This cohort study examines the implications of inadequate housing; financial difficulty; and alcohol, tobacco, or substance use as well as race/ethnicity and other covariates for veterans with symptomatic SARS-CoV-2 infection or COVID-19.
Key Points
Question
Are social and behavioral risk factors associated with mortality in US veterans with COVID-19?
Findings
In this cohort study of 27 640 veterans who received a positive test result for COVID-19, risk factors such as housing problems, financial hardship, alcohol use, tobacco use, and substance use were not associated with higher mortality.
Meaning
This study found no association between social and behavioral risk factors and death from COVID-19 in an integrated VA health system; such a system is known to transcend social vulnerabilities and has the potential to be a model of support services for households and at-risk populations in the US.
Abstract
Importance
The US Department of Veterans Affairs (VA) offers programs that reduce barriers to care for veterans and those with housing instability, poverty, and substance use disorder. In this setting, however, the role that social and behavioral risk factors play in COVID-19 outcomes is unclear.
Objective
To examine whether social and behavioral risk factors were associated with mortality among US veterans with COVID-19 and whether this association might be modified by race/ethnicity.
Design, Setting, and Participants
This cohort study obtained data from the VA Corporate Data Warehouse to form a cohort of veterans who received a positive COVID-19 test result between March 2 and September 30, 2020, in a VA health care facility. All veterans who met the inclusion criteria were eligible to participate in the study, and participants were followed up for 30 days after the first SARS-CoV-2 or COVID-19 diagnosis. The final follow-up date was October 31, 2020.
Exposures
Social risk factors included housing problems and financial hardship. Behavioral risk factors included current tobacco use, alcohol use, and substance use.
Main Outcomes and Measures
The primary outcome was all-cause mortality in the 30-day period after the SARS-CoV-2 or COVID-19 diagnosis date. Multivariable logistic regression was used to estimate odds ratios, clustering for health care facilities and adjusting for age, sex, race, ethnicity, marital status, clinical factors, and month of COVID-19 diagnosis.
Results
Among 27 640 veterans with COVID-19 who were included in the analysis, 24 496 were men (88.6%) and the mean (SD) age was 57.2 (16.6) years. A total of 3090 veterans (11.2%) had housing problems, 4450 (16.1%) had financial hardship, 5358 (19.4%) used alcohol, and 3569 (12.9%) reported substance use. Hospitalization occurred in 7663 veterans (27.7%), and 1230 veterans (4.5%) died. Housing problems (adjusted odds ratio [AOR], 0.96; 95% CI, 0.77-1.19; P = .70), financial hardship (AOR, 1.13; 95% CI, 0.97-1.31; P = .11), alcohol use (AOR, 0.82; 95% CI, 0.68-1.01; P = .06), current tobacco use (AOR, 0.85; 95% CI, 0.68-1.06; P = .14), and substance use (AOR, 0.90; 95% CI, 0.71-1.15; P = .41) were not associated with higher mortality. Interaction analyses by race/ethnicity did not find associations between mortality and social and behavioral risk factors.
Conclusions and Relevance
Results of this study showed that, in an integrated health system such as the VA, social and behavioral risk factors were not associated with mortality from COVID-19. Further research is needed to substantiate the potential of an integrated health system to be a model of support services for households with COVID-19 and populations who are at risk for the disease.
Introduction
The COVID-19 pandemic has exposed health disparities in the United States.1 In retracing the origins of the disease in the US, studies have found that the SARS-CoV-2 virus was introduced by individuals traveling around the world2 and that transmission chains eventually reached poor, vulnerable, and marginalized communities, which have been disproportionately affected and sustained community transmission.3 Although the pandemic has affected all lives in some way, it has also highlighted the health disparities in the US.4 Many people with low incomes are unable to work remotely because of their jobs as essential workers or to practice social distancing because of population density, making exposures to COVID-19 as well as transmission within families and social networks unavoidable.5,6 This situation has been associated with a substantial imbalance in case prevalence: socially vulnerable populations tend to have limited access to health care, less social support, and greater comorbidities, all of which contribute to worse outcomes and higher mortality from COVID-19.7,8,9,10
Social and behavioral risk factors have been found to be associated with COVID-19 outcomes.11,12,13,14 In poor, vulnerable, and marginalized communities, the prevalence of tobacco, alcohol, and drug use is high, and the various substances can be independent risk factors in COVID-19 outcomes.15 Veterans living throughout the US have diverse socioeconomic and behavioral backgrounds as well as diverse races/ethnicities.16,17 Although COVID-19 studies have increasingly reported that mortality is associated with race/ethnicity, US Department of Veterans Affairs (VA)–specific studies have shown no difference in mortality by race/ethnicity.18,19 The VA health system offers programs that are intended to reduce barriers to care for veterans as well as those with housing instability, poverty, and substance use disorder20,21,22,23; in this setting, it is unclear whether social and behavioral risk factors are associated with poor COVID-19 outcomes.
Juxtaposed with the structural inequity documented in the general US health care system is the structural equality cultivated within the VA system, with evidence of few racial disparities in health outcomes.24,25,26 The VA Office of Health Equity creates quality assurance metrics with health care teams to identify health inequities (eg, food insecurity); track them in the annual National Veteran Health Equity Report; and eliminate them through several personalized strategies, including tailoring outreach, earning trust, adapting treatment, and forming community partnerships.27
In this study, we used data from the VA to examine whether social and behavioral risk factors (housing problems; financial hardship; and tobacco, alcohol, and substance use) were associated with mortality among US veterans with COVID-19 and whether this association might be modified by race/ethnicity. We hypothesized that among veterans diagnosed with COVID-19, social and behavioral risk factors were not associated with mortality, even when the association was modified by race/ethnicity.
Methods
The institutional review board of the University of California, San Francisco approved this cohort study and waived the need for informed consent because the research involved no more than minimal risk to participants. Data were collected from March 2 to September 31, 2020. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Design, Setting, Participants, and Procedures
Using the VA Corporate Data Warehouse,28 we designed a cohort study of veterans who were diagnosed with COVID-19. The VA is a national health system for US veterans with localized services, including COVID-19 laboratory testing and reporting. The robust electronic health record system of the VA allows for a well-characterized cohort with mortality estimates that are updated on a quarterly basis. March 2, 2020, marked the earliest time point that a positive polymerase chain reaction test result for SARS-CoV-2 was seen in the VA laboratory system.
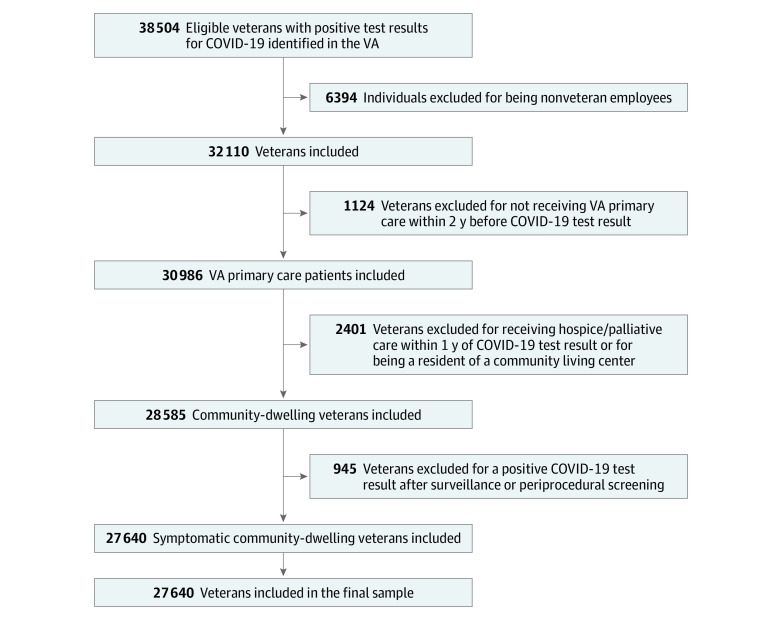
We assessed the eligibility of 38 504 individuals who received their first test result of RNA positivity for SARS-CoV-2 between March 2 and September 30, 2020, in a VA health care facility.28 We excluded 6394 nonveteran employees and 1124 veterans who did not receive VA primary care within 2 years before their SARS-CoV-2 test result to ensure that the study cohort included only those who obtained care in the VA. In addition, we did not include veterans who were tested outside of the VA because we may not have had access to all of their clinical information. By including only veterans who received primary care and were tested in the VA, we minimized missing baseline data. Because our focus was on identifying a veteran population living in the community, we excluded 2401 veterans who received hospice or palliative care within 1 year of the test result and those who were residents of a community living center (eg, VA nursing home). We also excluded 945 veterans with a positive COVID-19 test result after surveillance or screening before a procedure, as indicated by laboratory codes, to ensure that the study population was symptomatic.
All individuals who met the inclusion criteria were eligible to participate in the study and formed the analysis cohort. Veterans were followed up for 30 days after their first SARS-CoV-2 or COVID-19 diagnosis. September 30, 2020, was the end date of new diagnoses because VA mortality data are updated on a quarterly basis.
Data Sources and Measurements
All data on exposure, outcome, and covariate measurements were retrieved from the VA Corporate Data Warehouse.29 We used a combination of International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), procedure, outpatient diagnosis, and laboratory codes to extract these variables. We reviewed a random sample of 50 medical records to verify the capture of symptomatic individuals in the data set given that asymptomatic individuals by definition have zero probability of COVID-19–related mortality. Of the 50 medical records, we could not determine symptom status in 1 medical record, and no symptoms were reported for 1 medical record; the other 48 medical records identified symptoms among all veterans. For select variables (as described in the following paragraph), we used other sources of data. eTable 1 in the Supplement provides details on how each variable was constructed.
The exposure variables were social and behavioral risk factors. Social risk factors were defined as housing problems and financial hardship. We used a combination of ICD-10 codes on housing instability and receipt of VA housing services to identify veterans with evidence of housing problems. We identified an individual as having financial hardship according to ICD-10 codes that suggested poverty or financial hardship as well as the VA priority group. Income level, VA pension benefits, and receipt of Medicaid are considered in the assignment of veterans to priority groups. The VA adjusts annual income levels on the basis of resident zip code in consideration of priority groups, offering a measurement of financial hardship.30 Behavioral risk factors were defined as tobacco, alcohol, and substance use. Current tobacco use (eg, smoking within the past 1 year) was identified with an existing VA algorithm that was updated to include smoking-related ICD-10 diagnosis and clinic stop codes.31 Alcohol use was identified with a combination of ICD-10 codes and Alcohol Use Disorders Identification Test (Audit-C) scores.32 Substance use was identified according to ICD-10 codes. These ICD-10 codes were considered during the 2 years before the study period. We ascertained the presence or absence of a social and behavioral risk factor on the basis of a participant having at least 1 ICD-10 code during this 2-year period.
We reviewed a random sample of 25 medical records for each of the following variables: housing problems, current tobacco use, alcohol use, and substance use (a total of 100 records). We confirmed through medical record review that each social and behavioral risk factor identified using ICD-10 codes and other data sources was present in the 2 years before the index COVID-19 diagnosis. We did not conduct medical records review on the financial hardship variable because that was largely designated by the VA priority score after the VA conducted an in-depth assessment of veterans when they enrolled to receive care in the VA health system.
Primary Outcome and Covariates
The primary outcome was all-cause mortality in the 30-day period after the first test date of laboratory-confirmed SARS-CoV-2 infection or COVID-19 in a veteran. Mortality data were collected from the VA Corporate Data Warehouse and the VA Vital Status Files.29 When these available sources are combined, the resulting mortality data are comparable to the National Death Index in both accuracy and completeness. For the VA users, the combined data were 100% complete and 97.9% accurate to the date compared with the National Death Index.33 The final follow-up date was October 31, 2020. We considered other independent factors of mortality among veterans with COVID-19 and selected the following covariates: age, sex, race, ethnicity, marital status, comorbid conditions, body mass index, month of COVID-19 diagnosis, and hospitalization within 30 days. Race/ethnicity was self-reported by the individual, defined by the VA as a quality assurance mechanism for researchers, and assessed in the study because of the focus on health disparities.34 Hospitalization was identified using codes for inpatient admission (fee basis or VA) within 30 days of the first positive polymerase chain reaction test result for SARS-CoV-2 or COVID-19; otherwise, these covariates were baseline data that were collected before the test date.
Comorbid conditions included hypertension, ischemic heart disease, atrial fibrillation, stroke, diabetes or insulin use, heart failure, chronic kidney disease, chronic obstructive pulmonary disease or bronchiectasis, asthma, pneumonia, sleep apnea, deep venous thrombosis or pulmonary embolism, rheumatoid arthritis or other inflammatory conditions, cancer, HIV/AIDS, dementia, cirrhosis or hepatitis, home oxygen use in the past year, and mental health condition (depression, bipolar disorder, psychosis, and anxiety disorders). We used at least 1 inpatient ICD-10 code or 2 outpatient diagnosis codes in the 2 years before the test date to identify the presence or absence of comorbidities.35
Statistical Analysis
We performed descriptive analyses to estimate the prevalence of the covariates in the cohort. We assessed the prevalence of each social and behavioral risk factor by race/ethnicity, and we performed heterogeneity tests. Then, we assessed the association of social and behavioral risk factors with mortality. We fit multivariable logistic regression models, accounting for clustering through the addition of random effects for each VA health care facility, to estimate unadjusted and adjusted odds ratios (ORs). These assessments included iterative model building to understand the role of covariates (age, sex, race, ethnicity, marital status, clinical factors, health care facility, month of COVID-19 diagnosis) (eTable 2 in the Supplement). Clinical factors included body mass index and all comorbid conditions. These estimates were considered to be statistically significant if the CIs of the ORs did not cross the null value.
We tested the social and behavioral risk factors for interaction if race/ethnicity was associated with mortality. To this end, we took the product of each social and behavioral risk factor and race/ethnicity to create interaction terms. We assessed each possible interaction with a series of generalized linear models in which each model included the factor of interest (eg, housing problems) and its interaction term. Findings were considered to be statistically significant at a 2-sided P < .10 and if the factor was clinically relevant (eg, American Indian or Alaska Native vs White veterans). We used R, version 1.2.5019, including the glmm package (R Foundation for Statistical Computing), to conduct all analyses.
Results
The analysis cohort consisted of 27 640 veterans (Figure). Of these veterans, the mean (SD) age was 57.2 (16.6) years, and 24 496 were male (88.6%) and 3144 were female (11.4%) participants. Black (9745 [35.3%]) and Hispanic (3896 [14.1%]) veterans were well represented, and hypertension (14 693 [53.2%]) was the most common comorbid condition. The proportion of veterans with inadequate housing (3090 [11.2%]) and financial hardship (4450 [16.1%]) was comparable to the US poverty rate of 10.5% in 2019.36 Alcohol use was the most prevalent behavioral risk factor (5358 [19.4%]), but current tobacco use (4910 [17.8%]) and substance use (3569 [12.9%]) were also relatively common. We observed high levels of hospitalization (7663 [27.7%]) and death (1230 [4.5%]) (Table 1).
Figure. Flow Diagram of COVID-19 Cohort.
VA indicates US Department of Veterans Affairs.
Table 1. Characteristics of the US Veteran Cohort With COVID-19.
| Characteristic | No. (%) |
|---|---|
| No. | 27 640 |
| Age, y | |
| <55 | 11 444 (41.4) |
| 55-59 | 2811 (10.2) |
| 60-64 | 3197 (11.6) |
| 65-69 | 2791 (10.1) |
| 70-74 | 3869 (14.0) |
| 75-79 | 1651 (6.0) |
| ≥80 | 1877 (6.8) |
| Sex | |
| Female | 3144 (11.4) |
| Male | 24 496 (88.6) |
| Race | |
| White | 15 113 (54.7) |
| Black | 9745 (35.3) |
| Asian | 328 (1.2) |
| American Indian or Alaska Native | 283 (1.0) |
| Native Hawaiian or other Pacific Islander | 316 (1.1) |
| Unknown | 1855 (6.7) |
| Ethnicity | |
| Hispanic | 3896 (14.1) |
| Not Hispanic | 22 846 (82.7) |
| Unknown | 894 (3.2) |
| Marital status | |
| Married | 12 583 (45.5) |
| Social risk factors | |
| Inadequate housing | 3090 (11.2) |
| Financial hardship | 4450 (16.1) |
| No social risk factors | 21 151 (76.5) |
| Behavioral risk factors | |
| Current tobacco use | 4910 (17.8) |
| Alcohol use | 5358 (19.4) |
| Substance use | 3569 (12.9) |
| No behavioral risk factors | 18 492 (66.9) |
| Comorbid conditions | |
| Hypertension | 14 693 (53.2) |
| Ischemic heart disease, cardiac disease intervention, or myocardial infarction | 3989 (14.4) |
| Atrial fibrillation | 2054 (7.4) |
| Stroke | 757 (2.7) |
| Diabetes or insulin use | 8572 (31.0) |
| Congestive heart failure | 2184 (7.9) |
| Chronic kidney disease | 7233 (26.2) |
| Dialysis | 426 (1.5) |
| COPD or bronchiectasis | 3050 (11.0) |
| Asthma | 1487 (5.4) |
| Pneumonia | 893 (3.2) |
| Sleep apnea | 4872 (17.6) |
| Deep venous thrombus or pulmonary embolism | 672 (2.4) |
| Rheumatoid arthritis or other inflammatory conditions | 590 (2.1) |
| Cancer, including prostate cancer | 2080 (7.5) |
| HIV and AIDS | 332 (1.2) |
| Dementia | 1037 (3.8) |
| Cirrhosis or hepatitis | 2014 (7.3) |
| Home oxygen in past year | 818 (3.0) |
| No clinical conditions | 7318 (26.5) |
| Mental health conditions | |
| Depression | 7862 (28.4) |
| Bipolar disorder | 931 (3.4) |
| Psychosis | 885 (3.2) |
| Anxiety disorders | 4682 (16.9) |
| No mental health conditions | 17 470 (63.2) |
| BMI | |
| <18.5 | 119 (0.4) |
| 18.5-24.9 | 3369 (12.2) |
| 25.0-29.9 | 8110 (29.3) |
| ≥30 | 13 717 (49.6) |
| Unknown | 2325 (8.4) |
| VA region | |
| Northeast | 7454 (27.0) |
| Southeast | 10 889 (39.4) |
| Continental | 4905 (17.7) |
| Pacific | 4392 (15.9) |
| Mortality and hospitalization | |
| Died within 30 d | 1230 (4.5) |
| Hospitalized within 30 d | 7663 (27.7) |
| Month of COVID-19 diagnosis | |
| March | 1885 (6.8) |
| April | 2941 (10.6) |
| May | 1745 (6.3) |
| June | 4061 (14.7) |
| July | 8623 (31.2) |
| August | 4494 (16.3) |
| September | 3891 (14.1) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); COPD, chronic obstructive pulmonary disease; VA, US Department of Veterans Affairs.
Of the social and behavioral risk factors, housing problems (adjusted OR [AOR], 0.96; 95% CI, 0.77-1.19; P = .70), financial hardship (AOR, 1.13; 95% CI, 0.97-1.31; P = .11), current tobacco use (AOR, 0.85; 95% CI, 0.68-1.06; P = .14), alcohol use (AOR, 0.82; 95% CI, 0.68-1.01; P = .06), and substance use (AOR, 0.90; 95% CI, 0.71-1.15; P = .41) did not have statistically significant associations with mortality. Other factors in the model had statistically significant associations, including older age (eg, AOR, 75-79 years: 16.04; 95% CI, 11.24-22.91; P < .001), Asian (AOR, 2.02; 95% CI, 1.06-3.86; P = .03) and American Indian or Alaska Native (AOR, 2.41; 95% CI, 1.45-4.02; P = .001) races, diabetes (AOR, 1.40; 95% CI, 1.22-1.60; P < .001), chronic kidney disease (AOR, 1.82; 95% CI, 1.60-2.08; P < .001), dementia (AOR, 2.08; 95% CI, 1.73-2.51; P < .001), cirrhosis or hepatitis (AOR, 1.30; 95% CI, 1.05-1.61; P = .02), and home oxygen use in the past year (AOR, 1.38; 95% CI, 1.07-1.79; P = .01) (Table 2).
Table 2. Associations of Social and Behavioral Risk Factors With 30-Day Mortality Among US Veterans With COVID-19a.
| Variable | OR | P value | Adjusted OR | P value |
|---|---|---|---|---|
| Social and behavioral risk factors | ||||
| Housing problems | 0.86 (0.71-1.04) | .13 | 0.96 (0.77-1.19) | .70 |
| Financial hardship | 1.86 (1.63-2.12) | <.001 | 1.13 (0.97-1.31) | .11 |
| Current tobacco use | 0.63 (0.53-0.75) | <.001 | 0.85 (0.68-1.06) | .14 |
| Alcohol use | 0.53 (0.44-0.63) | <.001 | 0.82 (0.68-1.01) | .06 |
| Substance use | 0.83 (0.69-0.99) | .04 | 0.90 (0.71-1.15) | .41 |
| Age, y | ||||
| <55 | 1 [Reference] | 1 [Reference] | ||
| 55-59 | 0.30 (0.22-0.41) | <.001 | 2.75 (1.8-4.21) | <.001 |
| 60-64 | 0.67 (0.54-0.82) | <.001 | 5.12 (3.56-7.35) | <.001 |
| 65-69 | 1.04 (0.86-1.25) | .71 | 7.06 (4.94-10.08) | <.001 |
| 70-74 | 2.23 (1.96-2.55) | <.001 | 12.37 (8.86-17.29) | <.001 |
| 75-79 | 3.10 (2.63-3.65) | <.001 | 16.04 (11.24-22.91) | <.001 |
| ≥80 | 8.39 (7.37-9.55) | <.001 | 30.78 (21.74-43.57) | <.001 |
| Sex | ||||
| Female | 1 [Reference] | 1 [Reference] | ||
| Male | 4.42 (3.17-6.18) | <.001 | 1.31 (0.91-1.87) | .15 |
| Race | ||||
| White | 1 [Reference] | 1 [Reference] | ||
| Black | 1.09 (0.97-1.22) | .17 | 1.10 (0.95-1.28) | .20 |
| Asian | 0.81 (0.46-1.45) | .48 | 2.02 (1.06-3.86) | .03 |
| American Indian or Alaska Native | 1.83 (1.18-2.83) | .01 | 2.41 (1.45-4.02) | .001 |
| Native Hawaiian or other Pacific Islander | 0.68 (0.32-1.22) | .17 | 0.97 (0.48-1.99) | .94 |
| Unknown | 0.62 (0.47-0.81) | .001 | 0.99 (0.72-1.34) | .92 |
| Ethnicity | ||||
| Hispanic | 0.55 (0.45-0.68) | <.001 | 1.04 (0.82-1.31) | .76 |
| Marital status | ||||
| Married | 1.04 (0.93-1.17) | .48 | 0.88 (0.77-1.00) | .06 |
| Comorbid conditions | ||||
| Hypertension | 3.71 (3.22-4.27) | <.001 | 1.01 (0.85-1.20) | .89 |
| Ischemic heart disease, cardiac disease intervention, or myocardial infarction | 3.28 (2.90-3.71) | <.001 | 1.12 (0.96-1.30) | .14 |
| Atrial fibrillation | 3.52 (3.04-4.07) | <.001 | 1.11 (0.93-1.32) | .25 |
| Stroke | 2.53 (1.98-3.22) | <.001 | 0.98 (0.75-1.29) | .91 |
| Diabetes or insulin use | 2.76 (2.46-3.10) | <.001 | 1.40 (1.22-1.60) | <.001 |
| Congestive heart failure | 3.54 (3.07-4.09) | <.001 | 0.94 (0.78-1.13) | .50 |
| Chronic kidney disease | 3.96 (3.53-4.45) | <.001 | 1.82 (1.60-2.08) | <.001 |
| Dialysis | 3.72 (2.82-4.91) | <.001 | 1.18 (0.86-1.63) | .30 |
| COPD or bronchiectasis | 3.01 (2.63-3.44) | <.001 | 1.17 (0.99-1.39) | .06 |
| Asthma | 0.78 (0.59-1.04) | .09 | 0.88 (0.65-1.19) | .41 |
| Pneumonia | 3.32 (2.71-4.09) | <.001 | 1.18 (0.93-1.50) | .18 |
| Sleep apnea | 1.21 (1.05-1.39) | .009 | 1.10 (0.93-1.30) | .27 |
| Deep venous thrombus or pulmonary embolism | 2.00 (1.51-2.64) | <.001 | 1.07 (0.79-1.46) | .65 |
| Rheumatoid arthritis or other inflammatory conditions | 1.54 (1.11-2.14) | .01 | 1.16 (0.81-1.67) | .42 |
| Cancer, including prostate cancer | 2.42 (2.06-2.84) | <.001 | 1.07 (0.89-1.27) | .48 |
| HIV and AIDS | 0.95 (0.55-1.62) | .84 | 1.03 (0.58-1.83) | .92 |
| Dementia | 7.06 (6.01-8.29) | <.001 | 2.08 (1.73-2.51) | <.001 |
| Cirrhosis or hepatitis | 1.51 (1.25-1.82) | <.001 | 1.30 (1.05-1.61) | .02 |
| Home oxygen in past year | 3.17 (2.55-3.94) | <.001 | 1.38 (1.07-1.79) | .01 |
| BMI | ||||
| <18.5 | 2.88 (1.65-5.05) | <.001 | 1.16 (0.62-2.18) | .65 |
| 18.5-24.9 | 1 [Reference] | 1 [Reference] | ||
| 25.0-29.9 | 0.75 (0.67-0.84) | <.001 | 0.83 (0.68-1.00) | .05 |
| ≥30 | 1.72 (1.48-1.99) | <.001 | 1.01 (0.83-1.22) | .95 |
| Unknown | 1.01 (0.82-1.24) | .96 | 1.01 (0.77-1.32) | .95 |
| Month of positive COVID-19 test result | ||||
| March | 1 [Reference] | 1 [Reference] | ||
| April | 2.67 (2.33-3.07) | <.001 | 0.62 (0.50-0.77) | <.001 |
| May | 1.41 (1.15-1.73) | .001 | 0.35 (0.26-0.46) | <.001 |
| June | 0.74 (0.62-0.88) | .001 | 0.33 (0.25-0.42) | <.001 |
| July | 0.48 (0.41-0.55) | <.001 | 0.23 (0.18-0.29) | <.001 |
| August | 0.69 (0.58-0.82) | <.001 | 0.23 (0.18-0.30) | <.001 |
| September | 0.71 (0.59-0.85) | <.001 | 0.23 (0.18-0.30) | <.001 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); COPD, chronic obstructive pulmonary disease; OR, odds ratio.
Adjustment included age, sex, race, ethnicity, marital status, clinical factors, health care facility, and month of COVID-19 diagnosis.
Housing problems and substance use were higher in Black (1583 [16.2%] and 1482 [15.2%]) and American Indian or Alaska Native (46 [16.3%] and 50 [17.7%]) veterans compared with other racial/ethnic groups (eTable 3 in the Supplement). In contrast, Hispanic veterans had a lower prevalence of housing problems, financial hardship, current tobacco use, and substance use than non-Hispanic White veterans (eTable 4 in the Supplement). Given that Asian and American Indian or Alaska Native races were associated with mortality, we assessed these groups and found no evidence of an interaction with social and behavioral risk factors among these groups (eTable 5 in the Supplement).
Discussion
Despite relatively high levels of social and behavioral risk factors, no association with mortality from COVID-19 was found among individuals who obtained care through the VA, the largest integrated health care system in the US. Instead, we identified factors associated with mortality that were consistent with those reported in other studies, including older age, Asian and American Indian or Alaska or Alaska Native race, and certain comorbid conditions, such as diabetes and chronic kidney disease. Studies conducted outside of the VA health system have found that social risk factors were associated with mortality.37,38,39 Asking why we did not observe this association in the VA allows us to consider how the VA health system may be different from other US health care systems.
The VA has a portfolio of social and behavioral support programs that address housing instability, financial constraints, and substance use disorder.40,41 The US Department of Housing and Urban Development–VA Supportive Housing Program, for example, combines housing vouchers and supportive services to help veterans who are homeless and their families to find and sustain permanent housing.42 Case managers connect veterans with social and behavioral risk factors to other support services, including mental health treatment and substance use counseling. These services reduce barriers to care.43,44,45,46 The strong social and behavioral support programs in the VA may explain why we did not observe an association between social and behavioral risk factors and mortality. Studies that are designed to assess the potential reasons for this finding are needed.
In the general population of the US, concerns are widespread that social and behavioral risk factors may be associated with a much greater burden of disease and increased deaths from COVID-19, particularly among individuals with health disparities.13 Yet, we did not find a disproportionate association between these risk factors and mortality among a national cohort of socially vulnerable White, Black, or Hispanic veterans. Instead, the mitigating role may be attributed to the structural equities of the VA system. Further research is needed to substantiate the potential of an integrated system to be a model of support services to households with COVID-19 and populations who are at risk for this disease.
Limitations
This study has several limitations. First, veteran characteristics and access to support programs and integrated health care differ from those of the general population; thus, these findings should be extrapolated with caution. Second, veterans with poor health behaviors, such as heavy tobacco use, may have died before the pandemic from non–COVID-19 causes and thus were not included in the study, and those who were alive may have been less susceptible to the poor outcomes of their health behaviors; this situation presented the potential for selection bias (also called survivor bias). Third, social risk factors tend to be undercoded ICD-10 variables, which can lead to measurement error but not bias.47 However, we reviewed a random sample of medical records to confirm the classification of the measurements. In addition, the consistency of other findings from covariates, such as age, was reassuring, and we created iterative models to assess the association of age and other covariates with mortality. Fourth, although a large group of covariates were analyzed, certain covariates, such as occupational history, were not available from the VA data and may account for unmeasured confounding. Fifth, this study was not designed to explore the potential reasons for the observed findings.
Conclusions
This cohort study highlights the lack of association between death from COVID-19 and social and behavioral risk factors in an integrated VA health system. The VA health care system is known to transcend social vulnerabilities and has the potential to serve as a model of support services for households with COVID-19 and populations who are at risk for this disease in the US.
eTable 1. Codes Used to Define the Variables for the Social and Behavioral Risk Factors
eTable 2. Iterative Prediction Models to Assess Social and Behavioral Risk With 30-Day Mortality Among Veterans With COVID-19
eTable 3. Social and Behavioral Risk With COVID-19 Mortality, by Race
eTable 4. Social and Behavioral Risk With Mortality, by Ethnicity
eTable 5. Assessment of Interaction Between Social and Behavioral Risk and Race/Ethnicity
References
- 1.Centers for Disease Control and Prevention . Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Accessed April 29, 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
- 2.Worobey M, Pekar J, Larsen BB, et al. The emergence of SARS-CoV-2 in Europe and the US. bioRxiv. Preprint posted online May 2020. doi: 10.1101/2020.05.21.109322 [DOI]
- 3.Solis J, Franco-Paredes C, Henao-Martínez AF, Krsak M, Zimmer SM. Structural vulnerability in the U.S. revealed in three waves of COVID-19. Am J Trop Med Hyg. 2020;103(1):25-27. doi: 10.4269/ajtmh.20-0391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villarosa L. 'A terrible price': the deadly racial disparities of Covid-19 in America. The New York Times. April 29, 2020. Accessed April 29, 2021. https://www.nytimes.com/2020/04/29/magazine/racial-disparities-covid-19.html
- 5.Dyer O. Covid-19: Black people and other minorities are hardest hit in US. BMJ. 2020;369:m1483. doi: 10.1136/bmj.m1483 [DOI] [PubMed] [Google Scholar]
- 6.Rogers TN, Rogers CR, VanSant-Webb E, Gu LY, Yan B, Qeadan F. Racial disparities in COVID-19 mortality among essential workers in the United States. World Med Health Policy. August 5, 2020. doi: 10.1002/wmh3.358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayfield CA, Sparling A, Hardeman G, et al. Development, implementation, and results from a COVID-19 messaging campaign to promote health care seeking behaviors among community clinic patients. J Community Health. October 30, 2020. doi: 10.1007/s10900-020-00939-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Izzy S, Tahir Z, Cote DJ, et al. Characteristics and outcomes of Latinx patients with COVID-19 in comparison with other ethnic and racial groups. Open Forum Infect Dis. 2020;7(10):a401. doi: 10.1093/ofid/ofaa401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Page KR, Venkataramani M, Beyrer C, Polk S. Undocumented U.S. immigrants and Covid-19. N Engl J Med. 2020;382(21):e62. doi: 10.1056/NEJMp2005953 [DOI] [PubMed] [Google Scholar]
- 10.Oppel RA, Gebeloff R, Rebecca Lai KK, Wright W, Smith M. The fullest look yet at the racial inequity of coronavirus. The New York Times. July 5, 2020. Accessed April 29, 2021. https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html
- 11.Maroko AR, Nash D, Pavilonis BT. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Health. 2020;97(4):461-470. doi: 10.1007/s11524-020-00468-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nayak A, Islam SJ, Mehta A, et al. Impact of social vulnerability on COVID-19 incidence and outcomes in the United States. medRxiv. Preprint posted online April 17, 2020. doi: 10.1101/2020.04.10.20060962 [DOI]
- 13.Karaye IM, Horney JA. The impact of social vulnerability on COVID-19 in the U.S.: an analysis of spatially varying relationships. Am J Prev Med. 2020;59(3):317-325. doi: 10.1016/j.amepre.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freese KE, Vega A, Lawrence JJ, Documet PI. Social vulnerability is associated with risk of COVID-19 related mortality in U.S. counties with confirmed cases. J Health Care Poor Underserved. 2021;32(1):245-257. doi: 10.1353/hpu.2021.0022 [DOI] [PubMed] [Google Scholar]
- 15.Farhoudian A, Baldacchino A, Clark N, et al. COVID-19 and substance use disorders: recommendations to a comprehensive healthcare response. An International Society of Addiction Medicine Practice and Policy Interest Group position paper. Basic Clin Neurosci. 2020;11(2):133-150. doi: 10.32598/bcn.11.covid19.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wong MS, Steers WN, Hoggatt KJ, Ziaeian B, Washington DL. Relationship of neighborhood social determinants of health on racial/ethnic mortality disparities in US veterans—mediation and moderating effects. Health Serv Res. 2020;55(suppl 2):851-862. doi: 10.1111/1475-6773.13547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Griffin CL Jr, Stein MA. Self-perception of disability and prospects for employment among U.S. veterans. Work. 2015;50(1):49-58. doi: 10.3233/WOR-141929 [DOI] [PubMed] [Google Scholar]
- 18.Rentsch CT, Kidwai-Khan F, Tate JP, et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLoS Med. 2020;17(9):e1003379. doi: 10.1371/journal.pmed.1003379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ioannou GN, Locke E, Green P, et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US veterans with SARS-CoV-2 infection. JAMA Netw Open. 2020;3(9):e2022310. doi: 10.1001/jamanetworkopen.2020.22310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCreight MS, Gilmartin HM, Leonard CA, et al. Practical use of process mapping to guide implementation of a care coordination program for rural veterans. J Gen Intern Med. 2019;34(suppl 1):67-74. doi: 10.1007/s11606-019-04968-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leonard C, Gilmartin H, McCreight M, et al. Operationalizing an implementation framework to disseminate a care coordination program for rural veterans. J Gen Intern Med. 2019;34(suppl 1):58-66. doi: 10.1007/s11606-019-04964-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montgomery AE, Rahman AKMF, Chhabra M, Cusack MC, True JG. The importance of context: linking veteran outpatients screening positive for housing instability with responsive interventions. Adm Policy Ment Health. 2021;48(1):23-35. doi: 10.1007/s10488-020-01028-z [DOI] [PubMed] [Google Scholar]
- 23.Bell MD, Muppala B, Weinstein AJ, et al. Randomized clinical trial of cognitive remediation therapy with work therapy in the early phase of substance use disorder recovery for older veterans: 12-month follow-up. J Subst Abuse Treat. 2020;112:17-22. doi: 10.1016/j.jsat.2020.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peterson K, Anderson J, Boundy E, Ferguson L, McCleery E, Waldrip K. Mortality disparities in racial/ethnic minority groups in the Veterans Health Administration: an evidence review and map. Am J Public Health. 2018;108(3):e1-e11. doi: 10.2105/AJPH.2017.304246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong MS, Hoggatt KJ, Steers WN, et al. Racial/ethnic disparities in mortality across the Veterans Health Administration. Health Equity. 2019;3(1):99-108. doi: 10.1089/heq.2018.0086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kondo K, Low A, Everson T, et al. Prevalence of and Interventions to Reduce Health Disparities in Vulnerable Veteran Populations: A Map of the Evidence. Department of Veterans Affairs; 2017. [PubMed] [Google Scholar]
- 27.US Department of Veterans Affairs . Office of Health Equity. Accessed April 29, 2021. https://www.va.gov/healthequity/
- 28.DuVall S, Scehnet J. Introduction to the VA COVID-19 Shared Data Resource and its use for research. VA Informatics and Computing Infrastructure webinar. April 22, 2020. Accessed April 29, 2021. https://www.hsrd.research.va.gov/cyberseminars/catalog-upcoming-session.cfm?UID=3810
- 29.US Department of Veterans Affairs, Health Services Research & Development. Corporate Data Warehouse. Accessed April 29, 2021. https://www.hsrd.research.va.gov/for_researchers/vinci/cdw.cfm
- 30.US Department of Veterans Affairs . VA priority groups. Accessed April 29, 2021. https://www.va.gov/health-care/eligibility/priority-groups/
- 31.Barnett PG, Chow A, Flores NE. Using tobacco health factors data for VA Health Services Research. Technical Report 28. VA Palo Alto Health Economics Resource Center; 2014. Accessed April 29, 2021. https://www.herc.research.va.gov/files/RPRT_768.pdf
- 32.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking: Ambulatory Care Quality Improvement Project (ACQUIP)—alcohol use disorders identification test. Arch Intern Med. 1998;158(16):1789-1795. doi: 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- 33.Sohn MW, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:2. doi: 10.1186/1478-7954-4-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mor M. Assessing race and ethnicity in VA data. VIReC Database and Methods Seminar. April 5, 2021. Accessed April 29, 2021. https://www.hsrd.research.va.gov/cyberseminars/catalog-upcoming-session.cfm?UID=3965
- 35.Reaven PD, Emanuele NV, Wiitala WL, et al. ; VADT Investigators . Intensive glucose control in patients with type 2 diabetes—15-year follow-up. N Engl J Med. 2019;380(23):2215-2224. doi: 10.1056/NEJMoa1806802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.US Census Bureau . Income, poverty and health insurance coverage in the United States: 2019. September 15, 2020. Accessed April 29, 2021. https://www.census.gov/newsroom/press-releases/2020/income-poverty.html
- 37.Ahmad K, Erqou S, Shah N, et al. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS One. 2020;15(11):e0241327. doi: 10.1371/journal.pone.0241327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Siu JY. Health inequality experienced by the socially disadvantaged populations during the outbreak of COVID-19 in Hong Kong: an interaction with social inequality. Health Soc Care Community. October 2020. doi: 10.1111/hsc.13214 [DOI] [PubMed] [Google Scholar]
- 39.Dasgupta S, Bowen VB, Leidner A, et al. Association between social vulnerability and a county’s risk for becoming a COVID-19 hotspot—United States, June 1-July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1535-1541. doi: 10.15585/mmwr.mm6942a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi: 10.1097/MLR.0000000000000112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Edelman EJ, Maisto SA, Hansen NB, et al. The Starting Treatment for Ethanol in Primary Care Trials (STEP Trials): protocol for three parallel multi-site stepped care effectiveness studies for unhealthy alcohol use in HIV-positive patients. Contemp Clin Trials. 2017;52:80-90. doi: 10.1016/j.cct.2016.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.US Department of Veterans Affairs . Veterans experiencing homelessness. U.S. Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH) program. Accessed April 29, 2021. https://www.va.gov/homeless/hud-vash.asp
- 43.O’Mahen PN, Petersen LA. Effects of state-level Medicaid expansion on Veterans Health Administration dual enrollment and utilization: potential implications for future coverage expansions. Med Care. 2020;58(6):526-533. doi: 10.1097/MLR.0000000000001327 [DOI] [PubMed] [Google Scholar]
- 44.Tsai J, Link B, Rosenheck RA, Pietrzak RH. Homelessness among a nationally representative sample of US veterans: prevalence, service utilization, and correlates. Soc Psychiatry Psychiatr Epidemiol. 2016;51(6):907-916. doi: 10.1007/s00127-016-1210-y [DOI] [PubMed] [Google Scholar]
- 45.Ruggles KV, Fang Y, Tate J, et al. What are the patterns between depression, smoking, unhealthy alcohol use, and other substance use among individuals receiving medical care? a longitudinal study of 5479 participants. AIDS Behav. 2017;21(7):2014-2022. doi: 10.1007/s10461-016-1492-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O’Connell MJ, Kasprow WJ, Rosenheck RA. Differential impact of supported housing on selected subgroups of homeless veterans with substance abuse histories. Psychiatr Serv. 2012;63(12):1195-1205. doi: 10.1176/appi.ps.201000229 [DOI] [PubMed] [Google Scholar]
- 47.Ogilvie RP, MacLehose RF, Alonso A, et al. Diagnosed sleep apnea and cardiovascular disease in atrial fibrillation patients: the role of measurement error from administrative data. Epidemiology. 2019;30(6):885-892. doi: 10.1097/EDE.0000000000001049 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Codes Used to Define the Variables for the Social and Behavioral Risk Factors
eTable 2. Iterative Prediction Models to Assess Social and Behavioral Risk With 30-Day Mortality Among Veterans With COVID-19
eTable 3. Social and Behavioral Risk With COVID-19 Mortality, by Race
eTable 4. Social and Behavioral Risk With Mortality, by Ethnicity
eTable 5. Assessment of Interaction Between Social and Behavioral Risk and Race/Ethnicity