Abstract
BACKGROUND:
Historical information is limited on changes in procedures performed radiation safety practices by radiologic technologists during Fluoroscopically-guided interventional procedures (FGIPs).
METHODS:
Our study included 12,571 U.S. radiologic technologists who were certified for at least two years in 1926 – 1982 and reported in a 2012–13 survey that they ever performed or assisted with FGIPs and completed a mailed questionnaire in 2013–14 describing their detailed work practices for 21 FGIPs and associated radiation safety practices from the 1950’s through 2009.
RESULTS:
Overall, the proportion of technologists who reported working with therapeutic FGIPs, including percutaneous coronary interventions (PCI), increased over time, while the proportion of technologists who worked with diagnostic FGIPs, including diagnostic cardiovascular catheterization and neuroangiographic procedures, decreased. We also observed substantial increases in the median number of times per month that technologists worked with diagnostic cardiovascular catheterizations and PCI. In each time period, the majority of technologists reported consistently (≥ 75% of work time) wearing radiation monitoring badges and lead aprons during FGIPs. However, less than 50% of the technologists reported consistent use of thyroid shields, lead glasses and room shields during FGIPs, even in more recent time periods.
CONCLUSIONS:
This study provides a detailed historical assessment of FGIPs carried out and radiation safety practices employed by radiologic technologists from the 1950s through 2009. Results can be used in conjunction with badge dose data to estimate organ radiation dose for studies of radiation-related health risks in radiologic technologists who have worked with FGIPs.
Introduction
Fluoroscopically-guided interventional (FGI) procedures involve guidance of catheters and other small devices through blood vessels or other pathways (e.g. biliary or urinary tracts) with fluoroscopic imaging to localize and treat lesions [1–3]. Since the late 1970s, new devices including noncompliant balloon catheters, vascular stents, microcatheters and new guide wires have been developed and widely adapted for FGI procedures [1, 4, 5]. These technologies have allowed for smaller incisions, faster recovery and fewer complications than open surgical techniques [3]. As a result, an increasing number of diagnostic and therapeutic FGI procedures have been performed over last 30 years in the United States and elsewhere [6–13].
Although FGI procedures have provided benefits to patients, operators and those who assist the operators are potentially exposed to the primary x-ray beam or scattered radiation from the patient, as they are positioned close to the patient during the procedure [1, 2, 14]. Radiation exposure can be substantial over the career of medical radiation workers and place them at increased risk for radiation-related diseases [15–21].
Previous clinical reports have described the occurrence of brain tumors, breast cancers [15–17], and cataracts [18, 19] in medical workers who reported working with FGI procedures. However, these clinical reports were based on small numbers of workers and did not compare risks to medical radiation workers who did not perform FGI procedures. The studies also did not include historical information about changes in these work history practices over time. Data from the large U.S. Radiologic Technologists (USRT) cohort study suggested possible elevated risks of brain tumor, breast cancer, melanoma and cerebrovascular disease [20–22] in technologists who performed or assisted with FGI procedures in the mid - 1990s and follow-up of the technologists through 2008.
The USRT cohort study group did not collect substantial work history information about FGI procedures until 2013–14, when a detailed FGI work history survey was administered to a subset of the cohort who had previously reported having ever performed or assisted with FGI procedures. This survey inquired about a wide range of FGI procedures and radiation safety practices that technologists may have worked with or used since the 1950s.
To our knowledge, this is the first comprehensive historical assessment of FGI work practices among radiologic technologists.
Methods
Study overview
The USRT study of 146,022 radiologic technologists is a nationwide cohort study and described in detail elsewhere [23]. Eligible for inclusion in the nationwide cohort were technologists certified for at least 2 years by the American Registry of Radiologic Technologists between 1926 and 1982. Briefly, during follow- up which began in 1982, four different questionnaires were administered (during the periods 1983 – 89, 1994 – 98, 2003 – 05, and 2012 – 13) to collect information on health outcomes including specific types of cancer and benign tumors, circulatory diseases and other disorders, work history, demographic and lifestyle characteristics, medical history (e.g., history of personal medical diagnostic radiologic examinations and radiotherapy), reproductive characteristics, and other cancer risk factors.
Study population
In 2013 – 14, a detailed FGI work history survey was sent to technologists who responded positively to at least one of two screening questions in 2012–13 (response rate of 63%).
Of those who received the detailed FGI survey in 2013–14, 12,571 technologists reported that they ever performed or assisted with FGI procedures and were included in the current analytic study population.
Data collection
The screening question of the detailed FGI work history survey asked participants “Did you ever perform or assist with fluoroscopically-guided procedures such as those listed above at least once a month for a year or more?” FGI procedures were defined in the survey as “fluoroscopically-guided diagnostic or interventional procedures (cardiac, cardiac electrophysiology, interventional radiology endovascular, interventional neurosurgery, and GI/GU endoscopic procedures with fluoroscopy guidance for diagnosis or intervention)”, and participants were asked not to report on routine fluoroscopy exams (e.g., upper GI series, esophagram, barium enema). Participants were asked about 21 specific types of FGI procedures (see Supplementary Table 1) at the beginning of the survey. The term “perform or assist” was not specifically defined. The intent of the survey was to capture all activities conducted by radiologic technologists during the performance of FGI procedures. Radiologic technologists who responded positively to the screening question were asked how many years they performed or assisted with FGI procedures for five separate time periods (before 1970, 1970–79, 1980–89, 1990–99, and 2000–09), how many times per month for a year or more they had performed or assisted with 21 types of FGI procedures and the average percentage of time during each procedure that they were within three feet of the patient. For each time period, the technologist was also asked about the percentage of the time he or she wore radiation monitoring badges at specific anatomic locations (i.e. neck or chest, waist, and finger) or employed specific radiation protection practices while performing or assisting with FGI procedures.
The research protocol for the USRT cohort study of cancer risks has been approved annually by the National Cancer Institute Special Studies Institution Review Board (SSIRB Protocol OH97-C-N053) and the University of Minnesota Human Research Protection Program Institution Review Board (Federal Wide Assurance number 8005M02489).
Statistical Analyses
For each time period, we determined the proportion of technologists who performed or assisted with each specific FGI procedure. The denominators for this proportion were technologists who reported they performed or assisted with any FGI procedures during that period. Of those who reported that they ever performed or assisted with a specific procedure in a given time period, we calculated the median number of times per month the technologist performed or assisted with that procedure and the percentage of the time that the technologist was working within three feet of the patient. We further examined in each time period the proportion of technologists who consistently (75 – 100% of the time) employed specific radiation protection practices while performing or assisting with FGI procedures in that period. Again, the denominators for this proportion were technologists who reported they performed or assisted with any FGI procedures during that period.
All analyses were performed using the statistical software package SAS (release 9.3, SAS Institute, Cary, NC).
Results
Demographic characteristics of the 12,571 technologists who reported that they ever performed or assisted with FGI procedures are shown in Table 1. Of the technologists, 74% were female and 96% were Caucasian. At the completion of the fourth survey, two thirds (67%) of technologists were aged 60 or over, more than half were born in 1950 – 59 and a third in 1940 – 49. More than half of the technologists never smoked (55%), more than one-third (37%) completed a 2- year radiologic technologists program and one third (37%) completed college. These demographic characteristics were largely similar to those of the entire population of fourth survey responders (data not shown).
Table 1.
Demographic characteristics among radiologic technologists who ever performed or assisted with fluoroscopically guided interventional (FGI) procedures from before 1970 to 2009, US Radiologic Technologists Study
| Ever performed or assisted with FGI procedures (N=12, 571) | ||
|---|---|---|
| Characteristic | N | % |
| Gender | ||
| Male | 3167 | 25.2 |
| Female | 9393 | 74.7 |
| Unknown | 11 | 0.1 |
| Race | ||
| Caucasian | 12059 | 96.0 |
| African American | 256 | 2.0 |
| Asian/Pacific Islander | 93 | 0.7 |
| American Indian/Alaska Native | 37 | 0.3 |
| Others | 115 | 0.9 |
| Unknown | 11 | 0.1 |
| Age at follow - up at fourth survey completion (yrs) | ||
| < 60 | 4097 | 32.6 |
| 60 – 69 | 6112 | 48.6 |
| ≥ 70 | 2351 | 18.7 |
| Unknown | 11 | 0.1 |
| Birth cohort (yrs) | ||
| < 1940 | 1175 | 9.4 |
| 1940 – 49 | 4325 | 34.4 |
| 1950 – 59 | 6935 | 55.2 |
| ≥ 1960 | 125 | 1.0 |
| Unknown | 11 | 0.1 |
| Cigarette smoking status at fourth survey completion | ||
| Never smoker | 6909 | 55.0 |
| Former smoker | 4562 | 36.3 |
| Current smoker | 898 | 7.1 |
| Unknown | 202 | 1.6 |
| Education | ||
| Grade school | - | - |
| High school | 38 | 0.3 |
| 2 years radiologic technologist program | 4754 | 37.8 |
| College | 4751 | 37.8 |
| Graduate school | 878 | 7.0 |
| Others (e.g. vocational) | 335 | 2.7 |
| Unknown | 1815 | 14.4 |
| Body Mass Index (kg/m2) at fourth survey completion | ||
| <25 | 4131 | 32.9 |
| 25 – 29 | 4466 | 35.5 |
| ≥ 30 | 3730 | 29.7 |
| Unknown | 244 | 1.9 |
| Parity at fourth survey completiona | ||
| Nulliparous | 2061 | 22.3 |
| 1 | 1422 | 15.4 |
| 2 | 3543 | 38.4 |
| ≥3 | 2200 | 23.9 |
| Menopausal status at fourth survey completion a | ||
| Premenopausal | 246 | 2.7 |
| Postmenopausal | 8746 | 96.1 |
| Menstrual are irregular or using hormones | 112 | 1.2 |
: Only included female radiologic technologists
- : Not available
Shown in Table 2 is the frequency of selected work history characteristics of the 12,571 technologists. Most of the technologists (60%) became certified between 1970 and 1980. More than half of the technologists (53%) had worked with FGI procedures for more than 10 years, and most technologists (86%) were retired at survey completion. Of those completing the detailed FGI procedures survey, most technologists (86%) reported having ever performed or assisted with therapeutic FGI procedures, while a lower proportion (53%) had ever performed or assisted with diagnostic FGI procedures.
Table 2.
Work history characteristics among radiologic technologists who ever performed or assisted with fluoroscopically-guided interventional (FGI) procedures from before 1970 to 2009,US Radiologic Technologists Study
| Ever performed or assisted with FGI procedures (N=12,571) | ||
|---|---|---|
| Characteristic | N | % |
| Certification year as a technologist | ||
| < 1960 | 678 | 5.4 |
| 1960 – 1970 | 3417 | 27.2 |
| 1970 – 1980 | 7592 | 60.4 |
| > 1980 | 873 | 6.9 |
| Unknown | 11 | 0.1 |
| Year first worked as a technologist | ||
| < 1960 | 1096 | 8.7 |
| 1960 – 1969 | 3873 | 30.8 |
| 1970 – 1979 | 7092 | 56.4 |
| ≥ 1980 | 275 | 2.2 |
| Unknown | 235 | 1.9 |
| Duration of working as a technologist | ||
| < 5 | 409 | 3.3 |
| 5 – 10 | 1169 | 9.3 |
| 10 – 20 | 2585 | 20.6 |
| ≥ 20 | 7598 | 60.4 |
| Unknown | 810 | 6.4 |
| Years of performing or assisting FGI procedures | ||
| < 5 | 1644 | 13.1 |
| 5 – 10 | 2484 | 19.8 |
| 10 – 15 | 1807 | 14.4 |
| ≥ 20 | 4928 | 39.2 |
| Unknown | 1708 | 13.6 |
| Working status as a FGI procedure technologist | ||
| Retired when they completed the survey | 10824 | 86.1 |
| Currently working as rad tech | 1397 | 11.1 |
| Unknown | 350 | 2.8 |
| Working with | ||
| Diagnostic FG procedure | 6608 | 52.7 |
| Therapeutic FG procedures | 10726 | 85.6 |
| Both | 5907 | 47.1 |
- : Not available
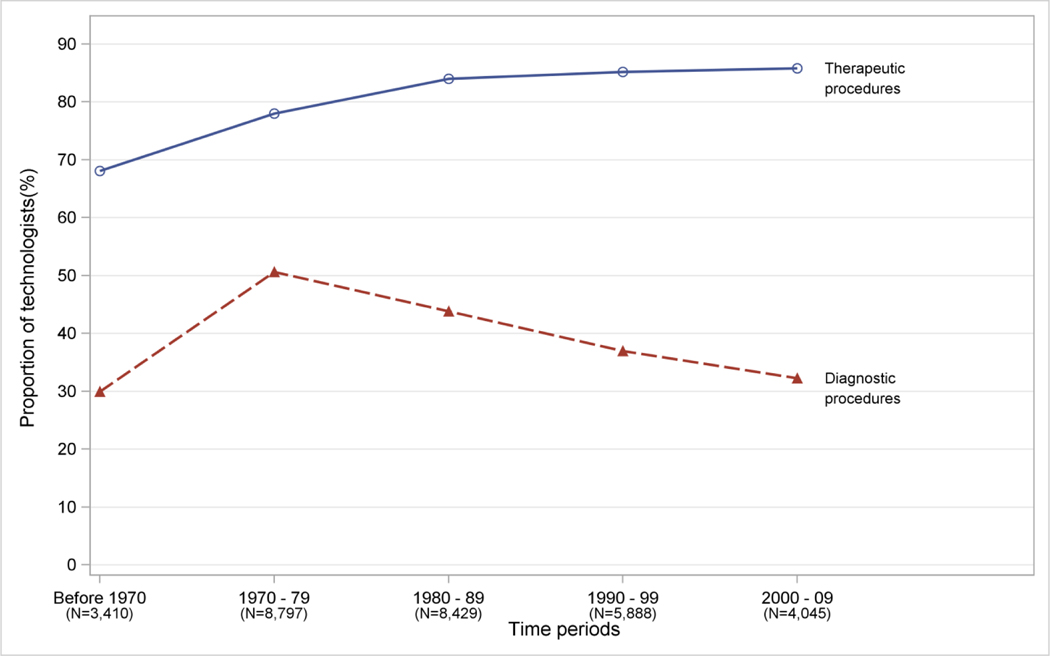
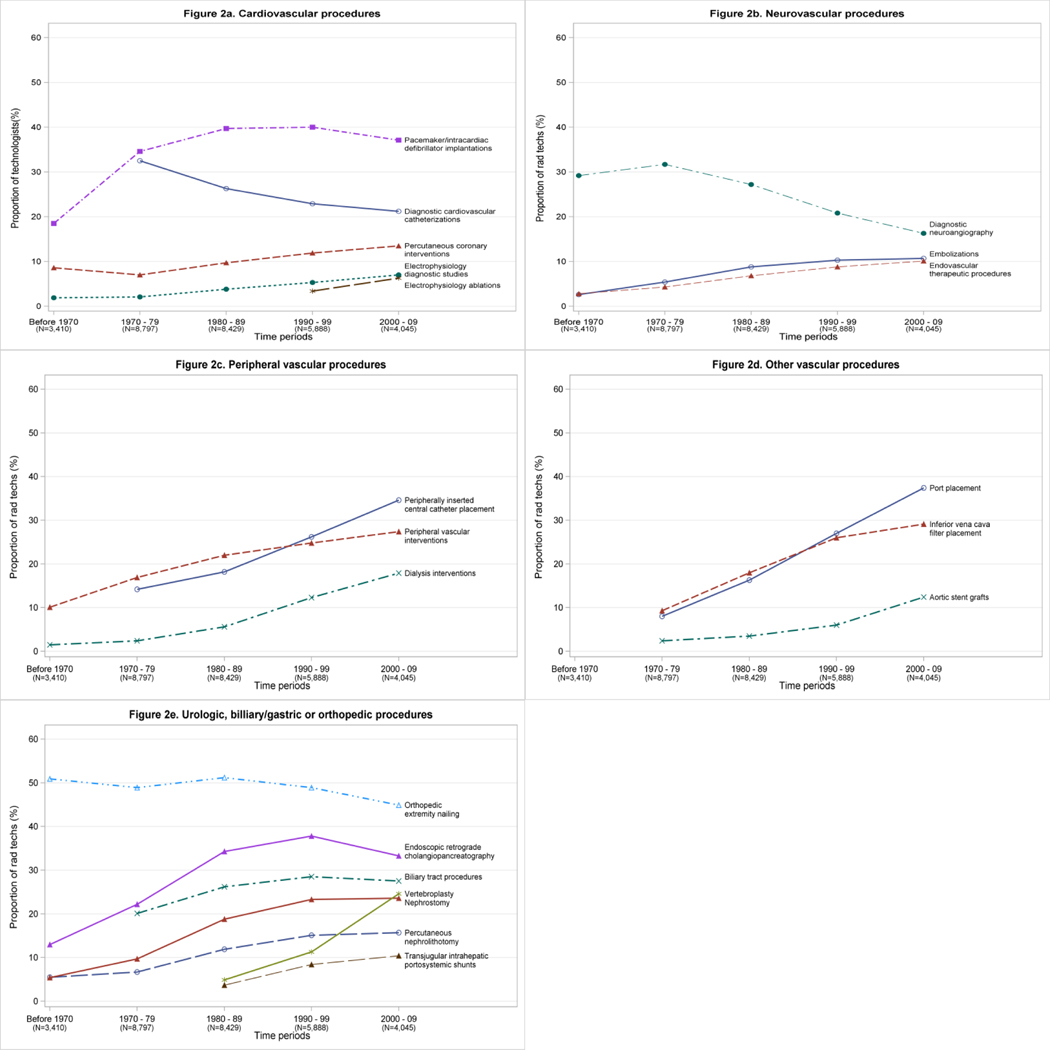
In general, among the 12,571 respondents the proportion performing or assisting with any FGI therapeutic procedures increased from 68% before 1970 to 85% in 1990 – 99 and then plateaued (Figure 1). This pattern was similar for technologists performing or assisting with embolizations (Figure 2b), endovascular therapeutic procedures (Figure 2b), peripheral vascular interventions (Figure 2c), inferior vena cava filter placement (Figure 2d), nephrostomy (Figure 2e), percutaneous nephrolithotomy (Figure 2e), transjugular intrahepatic portosystemic shunts (Figure 2e), and biliary tract procedures (Figure 2e). In contrast, the proportion of 12,571 technologists assisting with any diagnostic procedures in a given period increased from 30% before 1970 to 50% in 1970 – 79 but subsequently declined in later periods (Supplementary Table 1; Figure 1). This pattern was evident for technologists who performed or assisted with diagnostic cardiovascular catheterizations (Figure 2a) and diagnostic neuroangiography (Figure 2b).
Fig. 1-.
Proportion of radiologic technologists who performed or assisted with therapeutic or diagnostic fluoroscopically guided interventional (FGI) procedures from before 1970 to 2009, U.S. Radiologic Technologists Study. Supplementary Table 1 shows types of specific diagnostic and therapeutic FGI procedures.
Fig. 2-.
Proportion of radiologic technologists who performed or assisted with fluoroscopically guided interventional (FGI) procedures from before 1970 to 2009, U.S. Radiologic Technologists Study.
There was a steady increase over time in the proportion of technologists performing or assisting with electrophysiology diagnostic procedures (2% before 1970 to 7% in 2000 – 09; Figure 2a), peripherally inserted central catheter placement (14% in 1970 – 79 to 34% in 2000 – 09; Figure 2c), dialysis interventions (1% before 1970 – 79 to 17% in 2000 – 09; Figure 2c), port placement (8% in 1970 – 79 to 37% in 2000 – 09; Figure 2d), aortic stent grafts (2% in 1970 – 79 to 12% in 2000 – 09; Figure 2d), and vertebroplasty (5% in 1980 – 89 to 25% in 2000 – 09; Figure 2e) among those performing or assisting with FGI procedures in each time period. Among the technologists performing or assisting with any FGI procedure in a given period, the proportion of technologists performing or assisting with percutaneous coronary interventions decreased from 9% before 1970 to 7% in 1970 – 79 then increased (from 10% in 1980 – 89 to 14% in 2000 – 09; Figure 2a). A notable increase for pacemaker/intracardiac defibrillator implantation was observed from before 1970 through the 1990s followed by a decline in the 2000s (19% before 1970 to 40% in 1980 – 89 to 37% in 2000 – 09; Figure 2a) and endoscopic retrograde cholangipancreatography (13% before 1970 to 34% in 1980 – 89 to 38% in 1990 – 99 to 33% in 2000 – 09; Figure 2e). The proportion of technologists performing or assisting with orthopedic extremity nailing remained at a consistently high level of 45% to 50% throughout all time periods (Figure 2e).
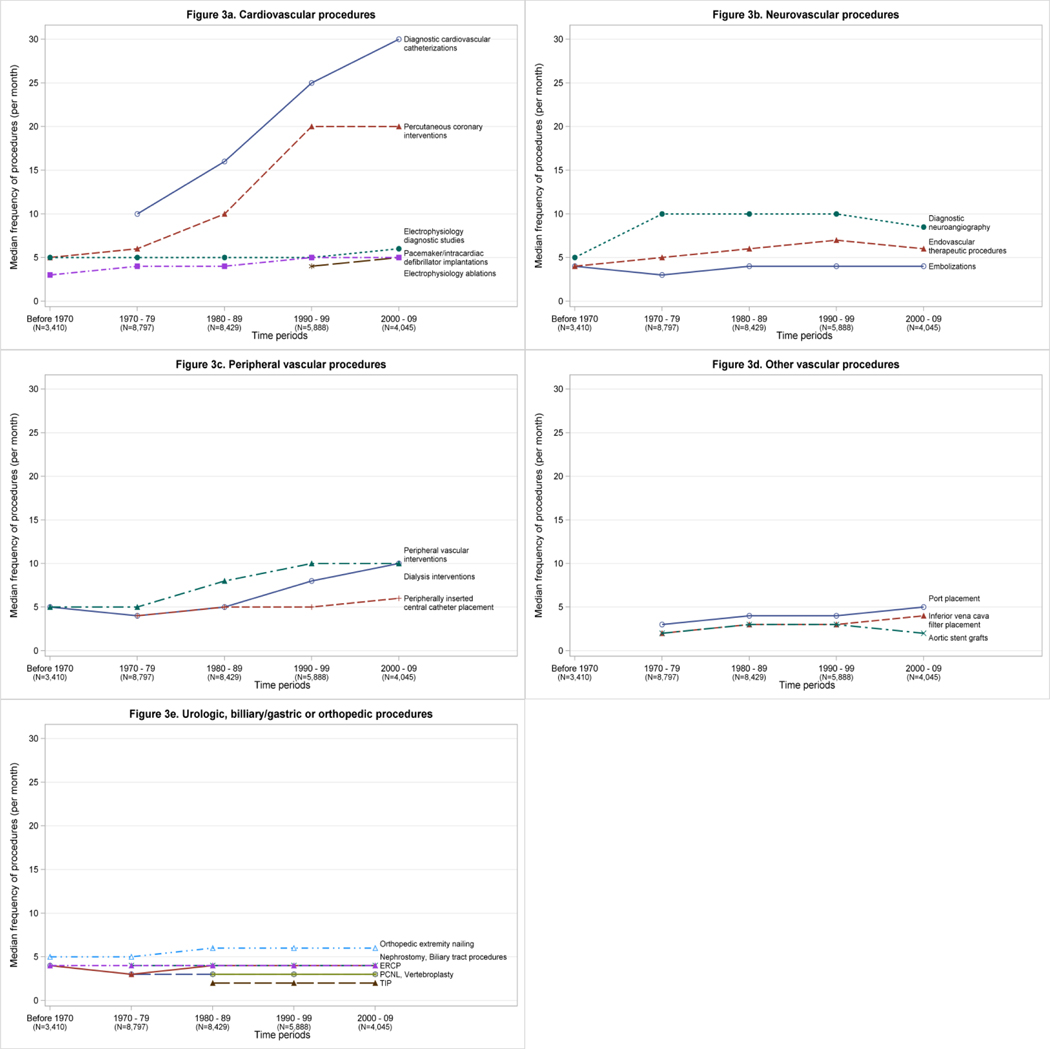
The median number of times per month that technologists performing or assisted with any FGI procedure rose consistently from 9 before 1970, to 15 in 1970 – 79, 20 in 1980 – 89, 24 in 1990 – 99, and to 26 in 2000 – 09 (data not shown). The median number of times per month that technologists performed or assisted with diagnostic cardiovascular catheterizations increased from 10 in 1970 – 79 to 30 in 2000 – 09 (Figure 3a) and similarly, percutaneous coronary interventions increased from a median of 5 per month before 1970 to 20 per month in 2000 – 09 (Figure 3a). The median number of times per month that technologists performed or assisted with diagnostic neuroangiography doubled from 5 before 1970 to 10 in 1970 – 79, but then decreased from 1990 – 99 onward (Figure 3b). The median number of peripheral vascular interventions that technologists carried out increased from 5 per month before the 1980s to 10 per month beginning in the 1990s (Figure 3c). The number of dialysis interventions that technologists performed or assisted with initially decreased slightly from 5 to 4 between before 1970 and 1970 – 79, but subsequently doubled from 1980 onward (from 5 to 10 between 1980 – 89 and 2000 – 09) (Figure 3c). Other procedures remained fairly constant with regard to frequency of performance (Figure 3).
Fig. 3-.
Median frequency of fluoroscopically guided interventional (FGI) procedures performed or assisted per month, among radiologic technologists who reported ever performing or assisting with the specific FGI procedure, before 1970 to 2009, US Radiologic Technologists Study. (ERCP: Endoscopic retrograde cholangiopancreatography, PCNL: Percutaneous nephrolithotomy, TIP: Transjugular intrahepatic portosystemic shunts)
The proportion of working time spent within three feet of the patients when performing or assisting with diagnostic cardiovascular catheterizations was 40 – 50% in each time period. After the 1970s, time spent within three feet of patients during percutaneous coronary interventions, endovascular therapeutic procedures, diagnostic neuroangiography, dialysis interventions, peripheral vascular interventions, and nephrostomy was also 40% - 50% (Table 3). For most other procedures, the median time spent within three feet of the patients was less than 40%.
Table 3.
Median percent of time technologists who performed or assisted with fluoroscopically guided interventional (FGI) procedures were located within three feet of the patient in five time periods from before 1970 to 2009, US Radiologic Technologists Study
| Before 1970 | 1970 – 79 | 1980 – 89 | 1990 – 99 | 2000 – 09 | |
|---|---|---|---|---|---|
| Cardiovascular procedures | |||||
| Diagnostic cardiovascular catheterizations | - | 45 | 50 | 50 | 50 |
| Percutaneous coronary interventions (PCI) | 40 | 30 | 40 | 50 | 50 |
| Electrophysiology (EP) diagnostic studies | 55 | 20 | 15 | 10 | 20 |
| Electrophysiology (EP) ablations | - | - | - | 9 | 10 |
| Pacemaker or intracardiac defibrillator implantations | 20 | 25 | 20 | 20 | 15 |
| Neurovascular procedures | |||||
| Embolizations | 10 | 34 | 30 | 40 | 35 |
| Endovascular therapeutic procedures | 20 | 30 | 40 | 40 | 40 |
| Diagnostic neuroangiography | 25 | 40 | 50 | 50 | 50 |
| Peripheral vascular procedures | |||||
| Peripherally inserted central catheter (PICC) placement | - | 25 | 25 | 30 | 34 |
| Dialysis interventions | 17 | 20 | 50 | 50 | 50 |
| Peripheral vascular interventions | 20 | 40 | 50 | 50 | 40 |
| Other vascular procedures | |||||
| Port placement | - | 20 | 15 | 15 | 20 |
| Inferior Vena Cava (IVC) filter placement | - | 20 | 30 | 25 | 25 |
| Aortic stent grafts | - | 10 | 20 | 20 | 15 |
| Urologic procedures | |||||
| Percutaneous nephrolithotomy (PCNL) | 20 | 15 | 20 | 25 | 20 |
| Nephrostomy | 20 | 25 | 40 | 50 | 40 |
| Biliary/gastric procedures | |||||
| Biliary tract procedures | - | 25 | 30 | 30 | 20 |
| Endoscopic retrograde cholangiopancreatography (ERCP) | 20 | 20 | 25 | 25 | 22 |
| Transjugular intrahepatic portosystemic shunts (TIPS) | - | - | 20 | 31 | 30 |
| Orthopedic procedures | |||||
| Vertebroplasty | - | - | 10 | 20 | 16 |
| Orthopedic extremity nailing | 20 | 20 | 20 | 20 | 12 |
- : Procedure not usually performed during the time period
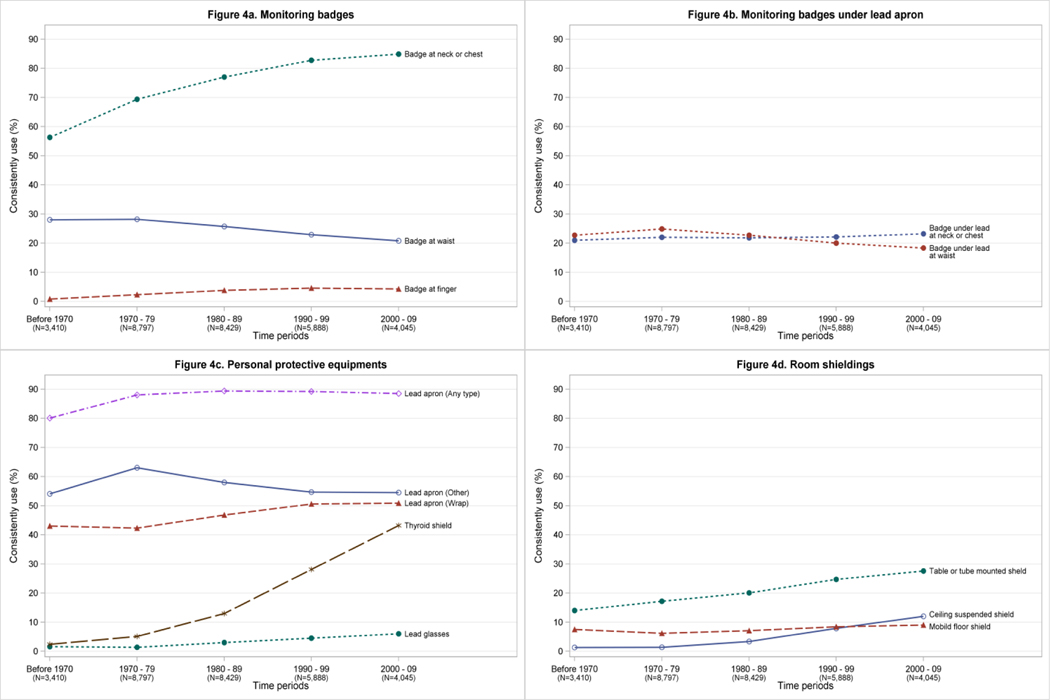
Consistent use (75% - 100% of the time) of radiation monitoring badges increased over time (Figure 4a). Technologists were substantially more likely to wear monitoring badges at the neck or chest than at the waist or on their fingers (Figure 4a). Only about 20% of technologists performing or assisting with FGI procedures consistently wore monitoring badges underneath their lead aprons at either the waist or neck/chest during each time period (Figure 4b). Most technologists (about 90%) consistently wore lead aprons in each time period (Figure 4c). Technologists were less likely to wear wrap- around lead aprons than other types of lead aprons in each time period, but the proportion of technologists who consistently wore wrap - around lead aprons rose somewhat over time from 42% before 1970 to 50% from 1990 onward (Figure 4c). The proportion of technologists who consistently used thyroid shields increased dramatically over time (from 2% before 1970 to 43% in 2000 – 09; Figure 4c).Only about 5% of technologists wore lead glasses consistently in each time period. The consistent use of room shields increased over time from 2 – 14% before 1970 to 8 – 29% in 2000 – 09, but remained less than 30% in each time period (Figure 4d).
Fig. 4-.
Proportion of radiologic technologists who consistently (75 – 100% of the time) used protective measurements during fluoroscopically guided interventional (FGI) procedures from before 1970 to 2009, US Radiologic Technologists Study.
Female technologists were more likely to wear monitoring badges at the waist over lead aprons than male technologists (females: 28%, males: 18% in 2000 – 09), and were slightly less likely to wear thyroid shields before 2000 (females: 26%, males: 28% in 1990 – 99). However, in 2000 – 09, use of thyroid shields in female technologists increased nearly two - fold and was notably higher than use of thyroid shields by male technologists (females: 56%, males: 41% in 2000 – 09) (data not shown).
Discussion
Overall, we found that the proportion of technologists who ever performed or assisted with therapeutic FGI procedures increased over the past several decades while the proportion of technologists who ever performed or assisted with diagnostic FGI procedures decreased. The median number of times per month that technologists performed or assisted with any FGI procedure tripled over the study period, with the most notable increases seen for diagnostic cardiovascular catheterizations and percutaneous coronary interventions. The median number of times per month that technologists performed other types of procedures remained fairly constant. The incorporation of radiation safety practices among technologists performing or assisting with FGI procedures has increased over time, but less than half of technologists reported use of thyroid shields and lead glasses during FGI procedures, and less than a third reported use of room shields even in the most recent decade.
The observed trend in the proportion of technologists performing therapeutic FGI procedures may be explained by the advent of newer technologies. Between 1970 and 1990, noncompliant balloon catheters and microcatheters, new guide wires and vascular stents were introduced and widely adopted for use in therapeutic FGI procedures because they provide a number of advantages over other procedures and allow an alternative to open surgery [1, 3–5]. The declines or stabilization in diagnostic FGI procedures, gastric and urologic FGI procedures, the latter having been observed in a previous study [6], can largely be explained by the introduction of non - invasive procedures in the 1980s and 1990s, such as computed tomography, computed tomography angiography, magnetic resonance imaging or magnetic resonance angiogram that provide much of the same information [5, 24, 25]. In addition, use of extracorporeal shockwave lithotripsy introduced in the 1980s for treatment for renal or bladder stones may have also contributed to the decline or stabilization of urologic FGI procedures [26].
Studies of interventional cardiology departments reported that the number of medical staff members has not proportionally increased along with the notable increase in the number of cardiac FGI procedures performed. As a result, the workload of the medical staff has increased [27, 28]. Our study similarly demonstrated a consistent increase in procedural volume for radiologic technologists who performed or assisted with diagnostic cardiovascular catheterizations or percutaneous coronary interventions.
Our findings suggest that technologists have increasingly followed the NCRP recommendation for use of placement of monitoring badges 1) at the neck outside the lead apron if one monitoring badge is provided and 2) at the neck outside the apron and at the waist or on the chest under the lead apron when two monitoring badges are provided [1]. In contrast, studies of medical staff in interventional laboratories have reported that approximately half of FGI operators had musculoskeletal problems and thus were using lighter weight aprons with a decreased lead equivalent thickness or replacement of lead by other elements, even though these may provide less protection [30–33].
Our study showed that relatively infrequent use of lead glasses and room shields consistently (defined as using 75–100% of the time during the procedure). It is similar to findings that fewer than 15% of 504 interventional radiation workers used such protective measures [17]. Either the lead glasses and room shields were not routinely provided to the radiologic technologists as an option, or they were not used, possibly because the radiologic technologists were not close to the radiation source or in the procedure room consistently during a typical FGI procedure. We did not specifically ask about radiation safety practices used within a certain distance of the beam or patient during the procedure. Neither the previous study nor ours inquired about the reasons for non-use of eyeglasses or ceiling suspended shielding.
Per-procedure radiation doses to interventional cardiologists have increased for certain procedures, such as percutaneous coronary interventions [28]. While less information is available on radiation exposure to technologists who performed or assist with FGI procedures, a small study found similar ranges of radiation exposure levels for interventional cardiologists and other medical staff (e.g., nurses/technicians) [40]. These observations, together with our results showing an increasing workload for technologists performing or assisting with therapeutic FGI procedures, suggests that occupational radiation exposure to radiologic technologists who performed or assisted with FGI procedures could have increased over time. Additional studies tracking monitoring badge doses over time could help to determine whether occupational doses of the radiologic technologists have indeed increased.
To our knowledge, this study is the first to provide comprehensive historical information about work history practices of radiologic technologists who performed or assisted with FGI procedures. However, there are limitations to our study. Although we inquired about FGI procedure – related work history practices between 2000 and 2009, all of the radiologic technologists in our study population were first certified before 1980. Our results, therefore, may not be applicable to all radiologic technologists who are currently working with these procedures. Some of the quantitative information provided to us may have been under- or overestimated by the participants, particularly for procedures that were performed several decades in the past, other literature on workers’ questionnaire responses suggests that the technologists provided reasonably accurate information on their work history practices. To our knowledge, there are no studies about the accuracy of self-reported work history information by medical workers. Other literature on workers’ questionnaire responses suggests that the technologists likely provided reasonably accurate information on their work history practices. Data from male chemical workers showed that about 71% of workers had provided information that agreed with company records for occupational histories up to 40 years in the past [40]. Furthermore, our findings were consistent with the 2009 American Heart Association report from 500 US hospitals showed an increasing number of cardiovascular FGI procedures being performed over time [28]. Finally, although we had data on radiation safety practices over several decades, we were not able to assess the variability in the use of safety practices of technologists specific to each FGI procedure.
Conclusion
This study provides a detailed historical assessment of FGI procedures carried out and radiation safety practices employed by radiologic technologists from the 1960s through 2009. Although technologists reported an increase in adherence to radiation safety practices over time, our findings suggest that workload of technologists who performed or assisted with certain FGI procedures has increased. Our results can be used in conjunction with badge dose data to estimate organ radiation dose for studies of radiation-related health risks in radiologic technologists who have worked with FGI procedures. A comprehensive assessment is needed of more recent practices and associated organ radiation dose estimates of workers in this field.
Supplementary Material
Acknowledgments
Funding: This work was supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics, National Cancer Institute, National Institutes of Health, U.S. Department of Health and Human Services
References
- 1.National Council on Radiation Protection and Measurements. Report No. 168 Radiation dose management for fluoroscopically-guided interventional medical procedures. In. Bethesda, MD: National Council on Radiation Protection and Measurements (NCRP), 2010 [Google Scholar]
- 2.Kim KP, Miller DL, De Gonzalez AB, et al. Occupational radiation doses to operators performing fluoroscopically-guided procedures. Health physics 2012; 103:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller DL. Overview of contemporary interventional fluoroscopy procedures. Health physics 2008; 95:638–644 [DOI] [PubMed] [Google Scholar]
- 4.Miller DL. Efforts to optimize radiation protection in interventional fluoroscopy. Health physics 2013; 105:435–444 [DOI] [PubMed] [Google Scholar]
- 5.Linet MS, Kim KP, Miller DL, Kleinerman RA, Simon SL, de Gonzalez AB. Historical review of occupational exposures and cancer risks in medical radiation workers. Radiation research 2010; 174:793–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhargavan M. Trends in the utilization of medical procedures that use ionizing radiation. Health physics 2008; 95:612–627 [DOI] [PubMed] [Google Scholar]
- 7.National Council on Radiation Protection and Measurements. Report No. 160 Ionizing radiation exposure of the population of the United States. In. Bethesda, MD: National Council on Radiation Protection and Measurements (NCRP), 2009 [Google Scholar]
- 8.Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics—2006 update a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2006; 113:e85–e151 [DOI] [PubMed] [Google Scholar]
- 9.United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2008 report, vol. I: sources of ionizing radiation. Annex A: medical radiation exposures. In: New York, NY: United Nations, 2010 [Google Scholar]
- 10.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics−−2014 update: a report from the American Heart Association. Circulation 2014; 129:e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manchikanti L, Cash KA, Moss TL, Rivera J, Pampati V. Risk of whole body radiation exposure and protective measures in fluoroscopically guided interventional techniques: A prospective evaluation. BMC anesthesiology 2003; 3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.IMV. IMV Medical Information Division. Benchmark Report, Cardiac Cath 2008 IMV Medical Information Division, Des Plaines,Illinois: 2009a; [Google Scholar]
- 13.IMV. IMV Medical Information Division. Benchmark Report, Interventional Angiography, 2008/2009. IMV Medical Information Division, Des Plaines, Illinois: 2009b; [Google Scholar]
- 14.Vano E, Ubeda C, Leyton F, Miranda P, Gonzalez L. Staff radiation doses in interventional cardiology: correlation with patient exposure. Pediatric cardiology 2009; 30:409–413 [DOI] [PubMed] [Google Scholar]
- 15.Finkelstein MM. Is brain cancer an occupational disease of cardiologists? The Canadian journal of cardiology 1998; 14:1385–1388 [PubMed] [Google Scholar]
- 16.Roguin A, Goldstein J, Bar O. Brain tumours among interventional cardiologists: a cause for alarm. Report of four new cases from two cities and a review of the literature EuroIntervention 2012; 7:1081–1086 [DOI] [PubMed] [Google Scholar]
- 17.Lynskey GE, Powell DK, Dixon RG, Silberzweig JE. Radiation protection in interventional radiology: survey results of attitudes and use. Journal of Vascular and Interventional Radiology 2013; 24:1547–1551. e1543 [DOI] [PubMed] [Google Scholar]
- 18.Vano E, Kleiman NJ, Duran A, Rehani MM, Echeverri D, Cabrera M. Radiation cataract risk in interventional cardiology personnel. Radiation research 2010; 174:490–495 [DOI] [PubMed] [Google Scholar]
- 19.Ciraj-Bjelac O, Rehani MM, Sim KH, Liew HB, Vano E, Kleiman NJ. Risk for radiation-induced cataract for staff in interventional cardiology: Is there reason for concern? Catheterization and Cardiovascular Interventions 2010; 76:826–834 [DOI] [PubMed] [Google Scholar]
- 20.Linet MS, Hauptmann M, Freedman DM, et al. Interventional radiography and mortality risks in US radiologic technologists. Pediatric radiology 2006; 36:113–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajaraman P DM, Doody MM, Yu CL, et al. Incidence and mortality risks for circulatory diseases in US radiologic technologists who worked with fluoroscopically guided interventional procedures, 1994–2008. Occupational and environmental medicine 2015:oemed-2015–102888 [DOI] [PubMed] [Google Scholar]
- 22.Rajaraman P DM, Yu CL, Preston DL, Miller JS, Sigurdson AJ, Freedman DM,, Alexander BH, Little MP, Miller DL, Linet MS.. Cancer risks in U.S. radiologic technologists working with fluoroscopically-guided interventional procedures, 1994–1998. Am J Roentgenol in press; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sigurdson AJ, Doody MM, Rao RS, et al. Cancer incidence in the US radiologic technologists health study, 1983–1998. Cancer 2003; 97:3080–3089 [DOI] [PubMed] [Google Scholar]
- 24.Feigenbaum H. The origin of echocardiography? Texas Heart Institute Journal 2008; 35:87. [PMC free article] [PubMed] [Google Scholar]
- 25.Fye WB. A history of the origin, evolution, and impact of electrocardiography. The American journal of cardiology 1994; 73:937–949 [DOI] [PubMed] [Google Scholar]
- 26.Cracco CM, Scoffone CM, Scarpa RM. New developments in percutaneous techniques for simple and complex branched renal stones. Current opinion in urology 2011; 21:154–160 [DOI] [PubMed] [Google Scholar]
- 27.Vano E, Gonzalez L, Fernandez J, Alfonso F, Macaya C. Occupational radiation doses in interventional cardiology: a 15-year follow-up. The British journal of radiology 2014; [DOI] [PubMed] [Google Scholar]
- 28.Kim KP, Miller DL, Balter S, et al. Occupational radiation doses to operators performing cardiac catheterization procedures. Health physics 2008; 94:211–227 [DOI] [PubMed] [Google Scholar]
- 29.Miller DL, Vañó E, Bartal G, et al. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Journal of Vascular and Interventional Radiology 2010; 21:607–615 [DOI] [PubMed] [Google Scholar]
- 30.Klein LW, Miller DL, Balter S, et al. Occupational health hazards in the interventional laboratory: time for a safer environment. Catheterization and Cardiovascular Interventions 2009; 73:432–438 [DOI] [PubMed] [Google Scholar]
- 31.Goldstein JA, Balter S, Cowley M, Hodgson J, Klein LW. Occupational hazards of interventional cardiologists: prevalence of orthopedic health problems in contemporary practice. Catheterization and cardiovascular interventions 2004; 63:407–411 [DOI] [PubMed] [Google Scholar]
- 32.Schlattl H, Zankl M, Eder H, Hoeschen C. Shielding properties of lead-free protective clothing and their impact on radiation doses. Medical physics 2007; 34:4270–4280 [DOI] [PubMed] [Google Scholar]
- 33.Venneri L, Rossi F, Botto N, et al. Cancer risk from professional exposure in staff working in cardiac catheterization laboratory: insights from the National Research Council’s Biological Effects of Ionizing Radiation VII Report. American heart journal 2009; 157:118–124 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.