Abstract
Objective:
Momentary negative affect has been shown to predict eating patterns in the laboratory, yet, more stable mood states have not been studied in relation to eating patterns in the laboratory among youth at high risk for binge-eating disorder and obesity.
Method:
One-hundred-eight adolescent girls (14.5±1.7y) with BMI between the 75th-97th percentile who reported loss-of-control (LOC)-eating completed measures of trait anxiety and depressive symptoms. Food-intake patterns were measured from a laboratory test meal (9,385 kcal). Latent factor analysis of depressive symptoms and trait anxiety was used to compute latent trait negative affect. Multivariate general linear models predicted total energy, snacks, and macronutrient intake from trait negative affect, adjusting for age, race, height, lean-mass, and percentage fat-mass.
Results:
Trait negative affect was significantly positively related to total energy-intake, and, specifically, snacks, sweet snacks, and percentage sweet fats (ps≤.03), and negatively related to percentage protein consumed (p=.04).
Discussion:
Expanding on affect theory, trait negative affect may relate to palatable food-intake among girls with LOC-eating. Further data are needed to determine whether those with LOC-eating and trait negative affect are at heightened risk for the development of binge-eating disorder and obesity.
Keywords: loss of control eating, negative affect, adolescents, obesity, binge-eating disorder
Introduction
Loss-of-control (LOC)-eating, a hallmark feature of binge-eating disorder (BED), involves the subjective experience of feeling out of control while eating. Common among youth with overweight and obesity, with rates of roughly 31% (He, Cai, & Fan, 2016), LOC-eating is predictive of partial- or full-syndrome BED (Hilbert, Hartmann, Czaja, & Schoebi, 2013; Tanofsky-Kraff et al., 2011) and excessive weight gain (Sonneville et al., 2013; Tanofsky-Kraff, Yanovski, et al., 2009). However, not all youth with LOC-eating develop pernicious outcomes, and roughly half of youth with LOC-eating later remit (Hilbert et al., 2013; Tanofsky-Kraff et al., 2011). A better understanding of LOC-eating is important to elucidate who is at greatest risk for adverse outcomes.
One mechanism for excess weight gain and BED in youth with LOC-eating is food-intake patterns. Compared to their counterparts, youth with LOC-eating tend to consume more energy (Hilbert, Tuschen-Caffier, & Czaja, 2010) and more highly-palatable foods (Goldschmidt, Tanofsky-Kraff, & Wilfley, 2011; Tanofsky-Kraff, McDuffie, et al., 2009). However, research is mixed regarding which factors may influence development of these intake patterns. Negative affect (NA) has been strongly and consistently associated with LOC-eating across the age spectrum (Goldschmidt, Aspen, Sinton, Tanofsky-Kraff, & Wilfley, 2008; Haedt-Matt & Keel, 2011). The relationship between NA and LOC-eating is consistent with affect theory, which proposes that LOC-eating may result from maladaptive coping with negative emotions (Heatherton & Baumeister, 1991; Kenardy, Arnow, & Agras, 1996). Affect theory is supported cross-sectionally (Goossens, Braet, & Decaluwé, 2007; Shomaker et al., 2010; Tanofsky-Kraff, Theim, et al., 2007) and is a prospective risk factor for LOC-eating onset in youth (Stice, 2002). Further, in a laboratory feeding study of youth at high risk for obesity and with reported LOC-eating, youth’s pre-prandial state NA related to greater consumption of highly-palatable foods (Ranzenhofer et al., 2013), suggesting momentary state NA may play a role in BED and obesity development.
Although there is consistent support for the role of state and trait NA in adults (Haedt-Matt & Keel, 2011; Smith et al., 2018), some naturalistic pediatric studies utilizing ecological momentary assessment have not found a direct relationship between state NA and LOC-eating (Goldschmidt et al., 2018; Hilbert, Rief, Tuschen-Caffier, de Zwaan, & Czaja, 2009; Ranzenhofer et al., 2014). Inconsistencies observed in the pediatric literature may be due to key differences in emotion regulation across the developmental spectrum (Swanson et al., 2014). Alternately, it is possible that trait NA masks state NA, such that youth experiencing consistent negative mood are less likely to endorse increased levels of state NA. Notably, more stable trait NA has not been well studied in relation to patterns of food-intake in developing youth at high risk for BED and adult obesity due to LOC-eating. Trait NA may be important, particularly in developing youth, for identifying who is at greatest risk for adverse outcomes.
Given the lack of laboratory data investigating these associations, we examined whether, among girls with reported LOC-eating, trait NA was associated with consumption of more highly-palatable, energy-dense food at a laboratory test meal designed to simulate a LOC-eating episode. Based on prior work (Tanofsky-Kraff, McDuffie, et al., 2009), it was hypothesized that greater trait NA would be associated with increased consumption of snack-type foods, a greater percentage of intake from sweet fats, and a lesser percentage of intake from protein.
Methods
Participants
A secondary analysis of data from girls ages 12–17 years with BMI between the 75th-97th percentile and reports of at least one episode of LOC-eating within the past month (ClinicalTrials.gov ID: NCT00680979) was conducted. Inclusion/exclusion criteria have been described (Tanofsky-Kraff et al., 2014), and other baseline data from this trial have been published (Glasofer et al., 2013; Jaramillo et al., 2018; Ranzenhofer et al., 2013; Shank et al., 2017) focusing on self-efficacy, family functioning, and state NA in relation to laboratory eating patterns. Data were collected from participants before initiating a prevention program.
Procedures
The study was IRB-approved and written informed consent from parents and assent from adolescents were obtained. At baseline, participants underwent the following:
Measures
Body Composition
Height was measured in triplicate by stadiometer and the average was used. Fasting weight was measured by scale calibrated to the nearest 0.1 kg. BMI (kg/m2) and BMI z-scores (Kuczmarski et al., 2002) were calculated. Lean and fat-mass were assessed by dual-energy x-ray absorptiometry (DXA; iDXA system, GE Healthcare, Madison WI).
Eating Disorder Examination (EDE)
The EDE (Fairburn & Cooper, 1993) was administered to determine presence of LOC-eating. The EDE has demonstrated very good interrater reliability in adolescents (Glasofer et al., 2007). EDE training/administration is described elsewhere (Tanofsky-Kraff et al., 2004).
Beck Depression Inventory (BDI-II)
The BDI-II (Beck, Steer, & Brown, 1996) is a self-report measure consisting of 21 depression-related statements rated on a 4-point scale ranging from 0 (not present) to 3 (very intense). Scores range from 0–63. The BDI-II has good psychometric properties in adolescents (Krefetz, Steer, & Kumar, 2003), and good internal consistency in this sample (Cronbach’s α = .86).
State-Trait Anxiety Inventory for Children (STAIC)–Trait Scale
The STAIC-trait scale (Spielberger, 1973) is a 20-item self-report measure of trait anxiety, defined as a personality trait capturing individual differences in the likelihood of experiencing anxiety across different situations. Scores range from 20–60. The STAIC has good reliability and construct validity (Papay & Hedl Jr, 1978), and good internal consistency in this sample (Cronbach’s α = .83).
Laboratory Test Meal
Energy-intake patterns were measured from a 9,385-kcal buffet test meal with an array of foods varying in macronutrients (51% carbohydrate, 37% fat, 12% protein) (Tanofsky-Kraff, McDuffie, et al., 2009). The test meal was consumed at 11:00 a.m. following an overnight fast. Participants received tape-recorded instructions to “Let yourself go and eat as much as you want.” Consumption was calculated by weighing each item before and after the meal. This LOC-eating paradigm is well-validated and has been successfully used in pediatric samples (Mirch et al., 2006; Tanofsky-Kraff, McDuffie, et al., 2009). Energy content and macronutrient composition for each food item were determined according to the U.S.D.A. Nutrient Database for Standard Reference standards and information supplied by food manufacturers.
Statistical Analyses
IBM SPSS Statistics 25 was used. Data were screened for outliers, skew, and kurtosis. Influential outliers were recoded to fall within 1.5 times the interquartile range above or below the 25th or 75th percentile (Behrens, 1997), which did not significantly alter the magnitude or direction of the results. Calories consumed from sweet snacks were not normally distributed and were logarithmically-transformed (base-10) to correct skew. Arcsine square-root transformations were conducted for percentage energy consumed from sweet fats (i.e. carbohydrates and fats combined) and protein.
A latent construct of trait NA was computed through latent factor analysis of depression symptoms and trait anxiety in order to capture the shared contribution of these constructs on eating (Elliott et al., 2010; Nelson, Aylward, & Steele, 2007). Three separate multivariate generalized linear models were conducted; with latent trait NA predicting 1) overall total energy-intake (kcal), adjusting for age, race (0=White, 1=Other), height (cm), lean-mass (kg), and percentage fat; 2) snack foods (i.e. kcal consumed from snack-type and sweet snack-type foods) adjusting for the same covariates and total energy-intake (kcal); and 3) percentage macronutrient intake (i.e. percentage of energy consumed from sweet fats and protein) adjusting for the same covariates as Model 1, given percentage intake adjusts for total energy-intake.
Results
Participants were 108 adolescent girls (14.5±1.7 years). The sample was 60.2% non-Hispanic White, 23.9% non-Hispanic Black, 16.0% Other race, and 8.8% Hispanic/Latina. Mean BMI percentile was 92.2%, BMIz 1.5±0.3, and fat 26.4±5.9kg; 40.7% of participants met criteria for obesity, 55.7% had overweight, while 3.5% had a BMI between the 75th-84th percentile. LOC-eating episodes in the past month ranged from 1–39 episodes. Thirty-seven participants (32.7%) reported objective binge-eating, and eight (7.4%) met criteria for BED.
In the model predicting total energy-intake, latent trait NA was significantly positively related to overall energy-intake (kcal) (p=.02), after adjusting for age, race, height, lean-mass, and fat (Table 1 displays complete models and effect sizes). In addition, trait NA was significantly positively related to snack-intake (p=.01), and sweet snack-intake (p=.01) after adjusting for the same covariates and total energy-intake. Lastly, latent trait NA was significantly positively related to percentage of energy consumed from sweet fats (p=.03), and negatively related to energy consumed from protein (p=.04) after adjusting for the same covariates as Model 1 (Figure 1).
Table 1.
Multivariate generalized linear model results of latent trait negative affect on total energy-intake (kcal), snack-intake (kcal), sweet snack-intake (kcal), percentage energy consumed from sweet fats, and percentage energy consumed from protein.
| Dependent variable(s) | Independent variables | F | β | p-value | ηp2 |
|---|---|---|---|---|---|
| Model 1: Total energy | |||||
| Total intake (kcal) | Latent Trait Negative Affect | 5.62 | 0.23 | .02* | .05 |
| Height (cm) | 0.59 | −0.12 | .44 | .01 | |
| Age (years) | 0.38 | −0.07 | .54 | <.01 | |
| Race | 0.20 | 0.05 | .67 | <.01 | |
| Lean mass (kg) | 2.15 | 0.24 | .15 | .02 | |
| % Fat mass | 0.02 | −0.02 | .88 | <.01 | |
| Model 2: Snacks | |||||
| Snack intake (kcal) | Latent Trait Negative Affect | 6.96 | 0.19 | .01* | .07 |
| Height (cm) | 0.28 | −0.06 | .60 | <.01 | |
| Age (years) | 0.42 | −0.05 | .52 | <.01 | |
| Race | 5.34 | −0.17 | .02* | .05 | |
| Lean mass (kg) | 0.16 | 0.05 | .69 | <.01 | |
| % Fat mass | 2.30 | −0.12 | .13 | .02 | |
| Total energy intake (kcal) | 71.39 | 0.62 | <.01* | .42 | |
| Sweet snack intake (kcal) | Latent Trait Negative Affect | 6.30 | 0.20 | .01* | .06 |
| Height (cm) | 0.02 | −0.02 | .90 | <.01 | |
| Age (years) | 1.96 | −0.12 | .17 | .02 | |
| Race | 7.53 | −0.22 | .01* | .07 | |
| Lean mass (kg) | 0.53 | −0.10 | .47 | .01 | |
| % Fat mass | 4.35 | −0.17 | .04* | .04 | |
| Total energy intake (kcal) | 40.14 | 0.50 | <.01* | .29 | |
| Model 3: % Macronutrient intake | |||||
| % Energy consumed sweet fats | Latent Trait Negative Affect | 4.63 | 0.20 | .03* | .04 |
| Height (cm) | 0.02 | 0.02 | .90 | <.01 | |
| Age (years) | 0.91 | −0.10 | .34 | .01 | |
| Race | 0.71 | −0.08 | .40 | .01 | |
| Lean mass (kg) | 0.18 | 0.07 | .68 | <.01 | |
| % Fat mass | 5.45 | −0.24 | .02* | .05 | |
| % Energy consumed protein | Latent Trait Negative Affect | 4.58 | −0.20 | .04* | .04 |
| Height (cm) | 0.02 | −0.02 | .89 | <.01 | |
| Age (years) | 0.91 | 0.10 | .34 | .01 | |
| Race | 0.74 | 0.09 | .39 | .01 | |
| Lean mass (kg) | 0.17 | −0.07 | .68 | <.01 | |
| % Fat mass | 5.35 | 0.24 | .02* | .05 | |
p<.05
Figure 1.
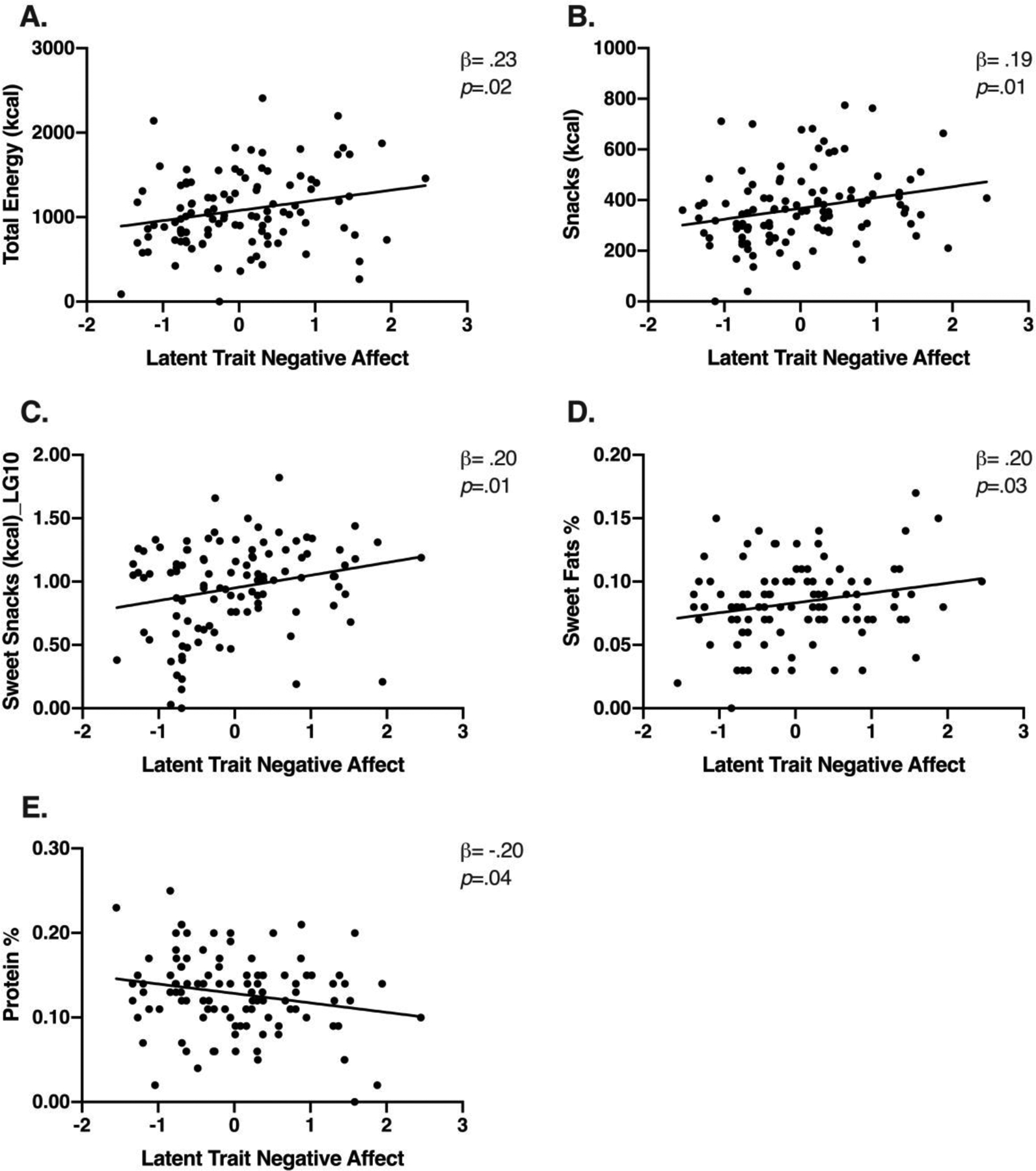
Latent trait negative affect in relation to food-intake patterns among girls with loss-of-control-eating. A) Trait negative affect positively relates to total energy-intake (kcal). B) Trait negative affect positively relates to snack-intake (kcal). C) Trait negative affect positively relates to sweet snack-intake (kcal). D) Trait negative affect positively relates to % energy consumed from sweet fats. E) Trait negative affect negatively relates to % energy consumed from protein.
Discussion
In a prevention-seeking sample of adolescent girls with LOC-eating, greater trait NA was positively related to greater consumption of total energy, snack-type and sweet snack-type foods, and percentage of sweet fats, and lesser percentage intake of protein at a meal modeled to simulate a LOC-eating episode. In line with affect theory (Kenardy et al., 1996), and consistent with studies examining self-reported LOC-eating and binge-eating (Goossens et al., 2007; Tanofsky-Kraff, Goossens, et al., 2007), more stable NA may be related to food-intake in the laboratory, which may subsequently influence risk for excess weight gain and BED development (Tanofsky-Kraff, Wilfley, et al., 2007). It is possible that trait NA masks aspects of state NA, particularly among healthy youth who do not meet criteria for clinical levels of anxiety or depression, such that those experiencing consistent negative mood are less likely to endorse increased levels of state NA. These data may clarify an important distinction in the pattern of eating among adolescent girls with LOC-eating and greater trait NA.
Interestingly, in contrast to one study of state NA that observed a link with palatable food-intake (Ranzenhofer et al., 2013), the current findings suggest that trait NA is also linked to greater total energy-intake, a more direct link to promotion of BED and obesity. Trait NA may exacerbate state negative mood, such that girls with greater trait NA may be at higher risk for consistent overeating compared to those who overeat only in response to momentary negative mood. One potential mechanism through which this pattern occurs may be explained by differences in food reward sensitivity, given that food-intake activates neurological reward pathways that reduce negative emotions (Adam & Epel, 2007). Those with LOC-eating and elevated trait NA may be chronically hypo-responsive to food reward, resulting in more consistent greater overall energy-intake as a maladaptive attempt to overcome a deficit in reward responsivity (Burger & Stice, 2011) compared to counterparts who have more regulated reward responsivity. Additionally, a pattern of lower protein consumption, as seen in the current study, has been associated with lower satiety, which may further increase overall energy-intake (Paddon-Jones et al., 2008). These cross-sectional data are a first step in supporting potential mechanisms.
Strengths include use of a racially diverse sample, a well-validated semi-structured interview to assess LOC-eating, and use of DXA rather than BMIz (Goran & Treuth, 2001; Kien & Ugrasbul, 2004). The laboratory test meal is a well-validated and well-controlled paradigm, and provides an objective measurement of intake. However, the laboratory buffet test meal may not accurately reflect eating in the natural environment, thus limiting the ecological validity of the findings. Additional limitations include the use of a restricted sample. Thus, findings cannot be extended to boys, those with lower or higher BMI, or youth without LOC-eating who have above average weight. Cross-sectional data limits the ability to draw causal relationships between trait NA and outcome. Finally, the effect sizes for significant results were small-to-medium (small effect size=.01; medium=.06) (Cohen, 1988) and thus should be interpreted with caution. Future research should consider other facets of eating patterns, such as length or sequence of eating episode, in relation to NA during LOC-eating episodes. Further, it could be of interest to analyze interactions of state and trait NA given the current study lacked adequate power, or examine anxiety and depressive symptoms separately, although it would increase the likelihood of Type 1 error and may provide limited clinical utility to screening efforts.
This study contributes to the understanding of LOC-eating, potentially identifying those with greater trait NA as a high-risk group. If trait NA is supported longitudinally as a clear mechanism for this relationship, findings could inform interventions that target both mood and eating for BED and adult obesity prevention.
CONFLICT OF INTEREST:
The authors have no conflicts of interest to declare. Dr. Yanovski reports grant support from Rhythm Pharmaceuticals, Inc. and Soleno Therapeutics, Inc. for work unrelated to the current submission.
DISCLAIMER:
J.A.Y. and M.K. are Commissioned Officers in the United States Public Health Service (PHS). The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the PHS, USUHS, or the United States Department of Defense. This research was supported by the Intramural Research Program of NICHD, NIH (ZIAHD00641 to JAY) and by R01DK080906 (to MTK).
The data that support the findings of this study are available from the corresponding author upon request.
References
- Adam TC, & Epel E (2007). Stress, eating and the reward system. Physiological Behavior, 91(4), 449–458. doi: 10.1016/j.physbeh.2007.04.011 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory-II (2 ed.). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Behrens JT (1997). Principles and procedures of exploratory data analysis. Psychological Methods, 2(2), 131–160. [Google Scholar]
- Burger KS, & Stice E (2011). Variability in reward responsivity and obesity: evidence from brain imaging studies. Current Drug Abuse Review, 4(3), 182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Elliott CA, Tanofsky-Kraff M, Shomaker LB, Columbo KM, Wolkoff LE, Ranzenhofer LM, & Yanovski JA (2010). An examination of the interpersonal model of loss of control eating in children and adolescents. Behaviour Research and Therapy, 48(5), 424–428. doi: 10.1016/j.brat.2009.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Cooper Z (1993). The Eating Disorder Examination (12th edition). In Fairburn CG & Wilson GT (Eds.), Binge eating: Nature, assessment, and treatment. (pp. 317–360). New York, NY, US: Guilford Press. [Google Scholar]
- Glasofer DR, Haaga DAF, Hannallah L, Field SE, Kozlosky M, Reynolds J, … Tanofsky-Kraff M (2013). Self-efficacy beliefs and eating behavior in adolescent girls at-risk for excess weight gain and binge eating disorder. International Journal of Eating Disorders, 46(7), 663–668. doi: 10.1002/eat.22160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasofer DR, Tanofsky-Kraff M, Eddy KT, Yanovski SZ, Theim KR, Mirch MC, … Yanovski JA (2007). Binge eating in overweight treatment-seeking adolescents. Journal of Pediatric Psychology, 32(1), 95–105. doi: 10.1093/jpepsy/jsl012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M, & Wilfley DE (2008). Disordered eating attitudes and behaviors in overweight youth. Obesity, 16(2), 257–264. doi: 10.1038/oby.2007.48 [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Smith KE, Crosby RD, Boyd HK, Dougherty E, Engel SG, & Haedt-Matt A (2018). Ecological momentary assessment of maladaptive eating in children and adolescents with overweight or obesity. International Journal of Eating Disorders, 51(6), 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Tanofsky-Kraff M, & Wilfley DE (2011). A laboratory-based study of mood and binge eating behavior in overweight children. Eating Behaviors, 12(1), 37–43. doi: 10.1016/j.eatbeh.2010.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens L, Braet C, & Decaluwé V (2007). Loss of control over eating in obese youngsters. Behaviour Research and Therapy, 45(1), 1–9. doi: 10.1016/j.brat.2006.01.006 [DOI] [PubMed] [Google Scholar]
- Goran MI, & Treuth MS (2001). Energy expenditure, physical activity, and obesity in children. Pediatric Clinics of North America, 48(4), 931–953. [DOI] [PubMed] [Google Scholar]
- Haedt-Matt AA, & Keel PK (2011). Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychological Bulletin, 137(4), 660–681. doi: 10.1037/a0023660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Cai Z, & Fan X (2016). Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis. International Journal of Eating Disorders, 50(2), 91–103. doi: 10.1002/eat.22661 [DOI] [PubMed] [Google Scholar]
- Heatherton TF, & Baumeister RF (1991). Binge eating as escape from self-awareness. Psychological Bulletin, 110(1), 86. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Hartmann AS, Czaja J, & Schoebi D (2013). Natural course of preadolescent loss of control eating. Journal of Abnormal Psychology, 122(3), 684–693. doi: 10.1037/a0033330 [DOI] [PubMed] [Google Scholar]
- Hilbert A, Rief W, Tuschen-Caffier B, de Zwaan M, & Czaja J (2009). Loss of control eating and psychological maintenance in children: An ecological momentary assessment study. Behaviour Research and Therapy, 47(1), 26–33. doi: 10.1016/j.brat.2008.10.003 [DOI] [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B, & Czaja J (2010). Eating behavior and familial interactions of children with loss of control eating: a laboratory test meal study. The American Journal of Clinical Nutrition, 91(3), 510–518. doi: 10.3945/ajcn.2009.28843 [DOI] [PubMed] [Google Scholar]
- Jaramillo M, Burke N, Shomaker L, Brady S, Kozlosky M, Yanovski J, & Tanofsky-Kraff M (2018). Perceived Family Functioning in Relation to Energy Intake in Adolescent Girls with Loss of Control Eating. Nutrients, 10(12), 1869. doi: 10.3390/nu10121869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenardy J, Arnow B, & Agras WS (1996). The aversiveness of specific emotional states associated with binge-eating in obese subjects. Australian and New Zealand Journal of Psychiatry, 30(6), 839–844. [DOI] [PubMed] [Google Scholar]
- Kien CL, & Ugrasbul F (2004). Prediction of daily energy expenditure during a feeding trial using measurements of resting energy expenditure, fat-free mass, or Harris-Benedict equations. The American Journal of Clinical Nutrition, 80(4), 876–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krefetz DG, Steer RA, & Kumar G (2003). Lack of Age Differences in the Beck Depression Inventory-II Scores of Clinically Depressed Adolescent Outpatients. Psychological Reports, 92(2), 489–497. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, … Johnson CL (2002). 2000 CDC Growth Charts for the United States: methods and development. Vital and Health Statistics, 11(246), 1–190. [PubMed] [Google Scholar]
- Mirch MC, McDuffie JR, Yanovski SZ, Schollnberger M, Tanofsky-Kraff M, Theim KR, … Yanovski JA (2006). Effects of binge eating on satiation, satiety, and energy intake of overweight children. The American Journal of Clinical Nutrition, 84(4), 732–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson TD, Aylward BS, & Steele RG (2007). Structural equation modeling in pediatric psychology: Overview and review of applications. Journal of Pediatric Psychology, 33(7), 679–687. doi: 10.1093/jpepsy/jsm107 [DOI] [PubMed] [Google Scholar]
- Paddon-Jones D, Westman E, Mattes RD, Wolfe RR, Astrup A, & Westerterp-Plantenga M (2008). Protein, weight management, and satiety. American Journal of Clinical Nutrition, 87. [DOI] [PubMed] [Google Scholar]
- Papay JP, & Hedl JJ Jr (1978). Psychometric characteristics and norms for disadvantaged third and fourth grade children on the State-Trait Anxiety Inventory for Children. Journal of Abnormal Child Psychology, 6(1), 115–120. [DOI] [PubMed] [Google Scholar]
- Ranzenhofer LM, Engel SG, Crosby RD, Anderson M, Vannucci A, Cohen LA, … Tanofsky-Kraff M (2014). Using ecological momentary assessment to examine interpersonal and affective predictors of loss of control eating in adolescent girls. International Journal of Eating Disorders, 47(7), 748–757. doi: 10.1002/eat.22333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranzenhofer LM, Hannallah L, Field SE, Shomaker LB, Stephens M, Sbrocco T, … Tanofsky-Kraff M (2013). Pre-meal affective state and laboratory test meal intake in adolescent girls with loss of control eating. Appetite, 68, 30–37. doi: 10.1016/j.appet.2013.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shank LM, Crosby RD, Grammer AC, Shomaker LB, Vannucci A, Burke NL, … Reynolds JC (2017). Examination of the Interpersonal Model of Loss of Control Eating in the Laboratory. Comprehensive Psychiatry, 76, 36–44. doi: 10.1016/j.comppsych.2017.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Elliott C, Wolkoff LE, Columbo KM, Ranzenhofer LM, … Yanovski JA (2010). Salience of loss of control for pediatric binge episodes: does size really matter? International Journal of Eating Disorders, 43(8), 707–716. doi: 10.1002/eat.20767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KE, Mason TB, Crosby RD, Engel SG, Crow SJ, Wonderlich SA, & Peterson CB (2018). State and trait positive and negative affectivity in relation to restraint intention and binge eating among adults with obesity. Appetite, 120, 327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, & Field AE (2013). Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA Pediatrics, 167(2), 149–155. doi: 10.1001/2013.jamapediatrics.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD (1973). Manual for the State-trait Anxiety Inventory for Children. Palo Alto: Consulting Psychologists Press. [Google Scholar]
- Stice E (2002). Risk and maintenance factors for eating pathology: a meta-analytic review. Psychological Bulletin, 128(5), 825. [DOI] [PubMed] [Google Scholar]
- Swanson SA, Horton NJ, Crosby RD, Micali N, Sonneville KR, Eddy K, & Field AE (2014). A latent class analysis to empirically describe eating disorders through developmental stages. International Journal of Eating Disorders, 47(7), 762–772. doi: 10.1002/eat.22308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, … Olsen C (2007). A multisite investigation of binge eating behaviors in children and adolescents. Journal of Consulting and Clinical Psychology, 75(6), 901–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky M, Schvey NA, Shomaker LB, … Yanovski JA (2009). Laboratory assessment of the food intake of children and adolescents with loss of control eating. The American Journal of Clinical Nutrition, 89(3), 738–745. doi: 10.3945/ajcn.2008.26886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, … Yanovski JA (2011). A prospective study of pediatric loss of control eating and psychological outcomes. Journal of Abnormal Psychology, 120(1), 108–118. doi: 10.1037/a0021406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Wilfley DE, Young JF, Sbrocco T, Stephens M, … Radin RM (2014). Targeted prevention of excess weight gain and eating disorders in high-risk adolescent girls: a randomized controlled trial. The American Journal of Clinical Nutrition, 100(4), 1010–1018. doi: 10.3945/ajcn.114.092536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Theim KR, Yanovski SZ, Bassett AM, Burns NP, Ranzenhofer LM, … Yanovski JA (2007). Validation of the emotional eating scale adapted for use in children and adolescents (EES-C). International Journal of Eating Disorders, 40(3), 232–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Wilfley DE, Young JF, Mufson L, Yanovski SZ, Glasofer DR, & Salaita CG (2007). Preventing excessive weight gain in adolescents: interpersonal psychotherapy for binge eating. Obesity, 15(6), 1345–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, & Yanovski JA (2009). A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders, 42(1), 26–30. doi: 10.1002/eat.20580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, & Yanovski JA (2004). Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of Consulting and Clinical Psychology, 72(1), 53–61. doi: 10.1037/0022-006X.72.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]


