Abstract
Ruptured vertebrobasilar dissecting aneurysms require urgent, often challenging treatment as they have with a high re-hemorrhage rate within the first 24 hours. The patient is a 57-year-old woman who presented with severe-sudden onset headache. Further work up showed a ruptured dissecting aneurysm of the caudal loop of the posterior inferior cerebellar artery (PICA) with associated narrowing distally, in the ascending limb. The aneurysm was immediately occluded with a Woven Endobridge (WEB) device (MicroVention, Tustin, CA, USA) while flow diversion treatment of the diseased ascending limb was postponed. Follow-up angiography three months later showed complete occlusion of the aneurysm, as well as healing of the diseased distal vessel, obviating the need for further intervention. WEB embolization of a ruptured dissecting posterior circulation aneurysm provided an excellent outcome for this patient.
Keywords: WEB device, dissection, aneurysm, PICA aneurysm
Introduction
Dissecting aneurysms of the vertebrobasilar circulation represent around 3% of all spontaneous subarachnoid hemorrhage.1,2 These aneurysms require expeditious treatment given their propensity to re-hemorrhage within the first 24 hours (71.4%) with a reported mortality ranging from 46 to 80%. 3 Endovascular treatment is often favored because of the higher risk of cranial nerve or brainstem injury associated with surgical clipping.4,5 Proximal occlusion, coil or stent-assisted coil embolization, and flow diversion are the primary endovascular options available for the treatment of dissecting aneurysms.1,2,6 Vessel sacrifice is the most durable option but is also associated with a high risk of ischemic stroke.1,4 Stent-assisted coiling and flow diversion mitigate the stroke risk but require the use of dual antiplatelet therapy.6,7 Woven Endobridge (WEB) (MicroVention, Tustin, CA, USA) is a novel intra-saccular flow-disruption device, that does not require antiplatelet therapy. 8 We report the first case of a posterior inferior cerebellar artery (PICA) dissecting aneurysm treated with WEB device with excellent results and suggest it may be well suited to this purpose.
Case report
History
A 57-year-old African American woman with a history of hypertension and previously treated breast cancer 10 years ago presented to the emergency department after experiencing a sudden-onset severe, persistent headache over the previous six hours with no associated neurological deficits. The patient reported nuchal rigidity and photophobia with no nausea, vomiting, or obvious motor deficits. Computed tomography (CT) imaging demonstrated hyperdensity in the third and fourth ventricles as well as along the posterior aspect of the upper spinal cord, consistent with acute subarachnoid hemorrhage. On arrival, the patient was awake and oriented to person, place, and time, complaining of a severe headache that was not relieved with analgesics. The patient had had a lumpectomy for the treatment of breast cancer with adjuvant chemotherapy ten years prior.
Physical examination
On admission, the patient was following commands and was appropriately alert and oriented. All cranial nerves were intact. No motor deficits were observed: strength was 5/5 in the upper and lower extremities and deep tendon reflexes were 2+ throughout. The Hoffman sign was negative bilaterally. Sensation to light touch was intact in all extremities. The only positive finding was a mild right-sided dysmetria.
Imaging and treatment
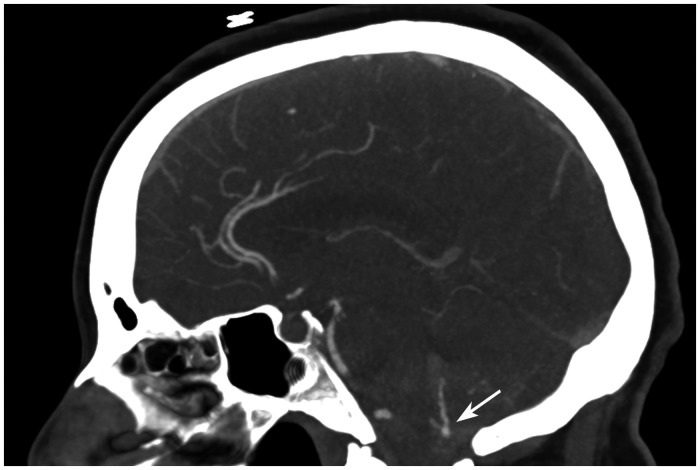
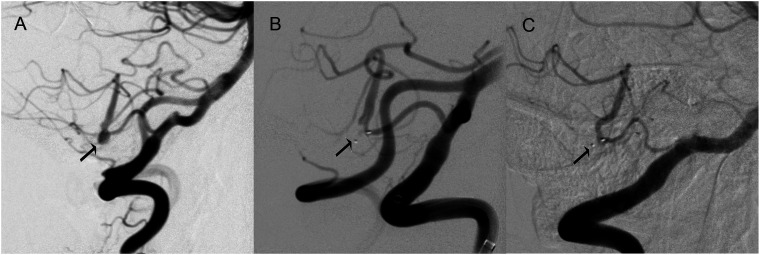
A CT of the head without contrast revealed a modified Fisher grade 4 subarachnoid hemorrhage within the third and fourth ventricles as well as along the posterior aspect of the cervical spinal cord. CT angiography showed a distal right-sided 5 mm PICA aneurysm with a possible dural arteriovenous fistula (Figure 1). Cerebral angiography showed evidence of significant angiopathy and irregularity of the ascending limb of the PICA with an associated dissection-related aneurysm (Figure 2(a)). Upon review of the 3-dimensional images, the decision was made to treat the dissection-related aneurysm with a 4x3 SL WEB device, with no additional treatment of the diseased segment of the PICA in the setting of an acute hemorrhage. Following appropriate sizing, the aneurysm was completely occluded with no residual neck remnant (Figure 2(b)).
Figure 1.
Sagittal computed tomography (CT) angiography of the brain showing the right posterior inferior cerebellar artery (PICA) with a 5 mm aneurysm along the caudal loop.
Figure 2.
Lateral digital subtraction angiography of the right vertebral artery. (a) 5 mm dissecting aneurysm of the PICA at the caudal loop associated with a diseased ascending limb of the vessel. (b) Immediate post-WEB embolization of the aneurysm showing intra-saccular stasis. (c) Three-month follow-up image showing complete obliteration of the aneurysm and resolution of the dissection-related disease of the ascending limb of the vessel.
Patient course
Post embolization, she was admitted to the neuro-intensive care unit, where a subarachnoid hemorrhage protocol was initiated that included systolic blood pressure control < 140 mmHg, daily transcranial Doppler ultrasound, nimodipine, euvolemia, and frequent neurological checks. Pain was well controlled with oral analgesics. Laboratory findings remained stable throughout the course of treatment. She remained stable in the intensive care unit, where her neurological exam was stable until discharge.
A follow-up angiogram performed 3 months after the SAH demonstrated complete occlusion of the dissection-related aneurysm as well as healing of the ascending loop of PICA diseased segment (Figure 2(c)). At follow-up, the patient remained neurologically intact.
Discussion
Ruptured dissecting aneurysms of the posterior circulation are rare and often challenging to treat. Although sometimes caused by traumatic unusual stretching of the arteries, atraumatic dissecting aneurysms are encountered in the setting of connective tissue and inflammatory diseases, smoking, and genetic predisposition. 9 Our patient was hypertensive and had previously received chemotherapy for the treatment of breast cancer. Mantia-Smaldone et al. reported a vertebral artery dissection, with secondary cerebral infarction associated with chemotherapeutic agent use. 10
Histopathologic study of the intradural vertebrobasilar system arteries show a thin media and adventitia, as compared to the extradural vertebral arteries, with diminished vasa vasora. 1 These characteristics likely limit the healing capabilities of these vessels in the setting of acute subarachnoid hemorrhage and diffuse inflammation 1 and may contribute to the early high re-rupture rate, making early treatment urgent.
The WEB device has revolutionized the treatment of wide neck bifurcation aneurysms, especially in the ruptured setting, given that no antiplatelet therapy is required. 8 In the setting of a dissecting aneurysm with an associated diseased vessel, the primary concern remains preventing early re-hemorrhage. Since the dissecting aneurysm was the most likely cause of the subarachnoid hemorrhage, we sought to direct initial therapy to aneurysmal occlusion. This was achieved immediately following deployment of the WEB device with intra-saccular stasis. In order to prevent any further dissections, the patient was planned to undergo subsequent flow diversion with a Pipeline flex (Medtronic, Dublin, Ireland) device, after the acute phase of the subarachnoid hemorrhage. However, this proved unnecessary as follow-up angiography showed the patient’s vessel had remodeled and healed. The origin of the dissection was likely associated with the aneurysm, and treatment of the aneurysm resolved the problem.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: The patient provided written informed consent for this publication and has reviewed the manuscript.
ORCID iD: Nicolas K Khattar https://orcid.org/0000-0002-5077-9804
References
- 1.Rabinov JD, Hellinger FR, Morris PP, et al. Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol 2003; 24: 1421–1428. [PMC free article] [PubMed] [Google Scholar]
- 2.Sedat J, Chau Y, Mahagne MH, et al. Dissection of the posteroinferior cerebellar artery: clinical characteristics and long-term follow-up in five cases. Cerebrovasc Dis 2007; 24: 183–190. [DOI] [PubMed] [Google Scholar]
- 3.Santos-Franco JA, Zenteno M, Lee A. Dissecting aneurysms of the vertebrobasilar system. A comprehensive review on natural history and treatment options. Neurosurg Rev 2008; 31: 131–140; discussion 140. [DOI] [PubMed] [Google Scholar]
- 4.Madaelil TP, Wallace AN, Chatterjee AN, et al. Endovascular parent vessel sacrifice in ruptured dissecting vertebral and posterior inferior cerebellar artery aneurysms: clinical outcomes and review of the literature. J Neurointerv Surg 2016; 8: 796–801. [DOI] [PubMed] [Google Scholar]
- 5.Lee JJ, Huang M, Guerrero J, et al. Operative treatment of a superior cerebellar artery perforator dissecting aneurysm. Oper Neurosurg (Hagerstown). Epub ahead of print 4 March 2020. DOI: 10.1093/ons/opz407. [DOI] [PubMed]
- 6.Wang J, Sun Z, Bao J, et al. Endovascular management of vertebrobasilar artery dissecting aneurysms. Turk Neurosurg 2013; 23: 323–328. [DOI] [PubMed] [Google Scholar]
- 7.Kurata A, Ohmomo T, Miyasaka Y, et al. Coil embolization for the treatment of ruptured dissecting vertebral aneurysms. AJNR Am J Neuroradiol 2001; 22: 11–18. [PMC free article] [PubMed] [Google Scholar]
- 8.Ozpeynirci Y, Braun M, Pala A, et al. WEB-only treatment of ruptured and unruptured intracranial aneurysms: a retrospective analysis of 47 aneurysms. Acta Neurochir (Wien) 2019; 161: 1507–1513. [DOI] [PubMed] [Google Scholar]
- 9.Linden MD, Chou SM, Furlan AJ, et al. Cerebral arterial dissection. A case report with histopathologic and ultrastructural findings. Cleve Clin J Med 1987; 54: 105–114. [DOI] [PubMed] [Google Scholar]
- 10.Mantia-Smaldone GM, Bagley LJ, Kasner SE, et al. Vertebral artery dissection and cerebral infarction in a patient with recurrent ovarian cancer receiving bevacizumab. Gynecol Oncol Case Rep 2013; 5: 37–39. [DOI] [PMC free article] [PubMed] [Google Scholar]