Abstract
Background and purpose
Thromboaspiration technology continues to evolve at an accelerated pace with increasing availability of larger and more navigable devices. Herein, we provide our initial experience with the intracranial navigation of a large-bore (.088" inner diameter) catheters during mechanical thrombectomy (MT).
Methods
Retrospective review of consecutive large vessel occlusion stroke patients in whom a TracStar™ or Zoom 88™ (Imperative Care, Campbell, CA) large-bore catheters were utilized in MT. The primary outcome was successful reperfusion (eTICI2b-3) at the end of the procedure. Safety measures included procedural complications and rates of symptomatic intracranial hemorrhage.
Results
Five patients (age,∼50–85 years; baseline NIHSS,17-23) were treated. The .088" catheters were used as the primary tool for contact aspiration in two patients (distal basilar artery and proximal MCA occlusions) with complete thrombus ingestion (eTICI3) during the first pass. In two patients, the .088" catheter was used for flow control where it was placed in the distal M1-segment of a patient with M2 occlusion treated with a combination of stent-retriever and .070" aspiration catheter and in the proximal M1 in a patient with distal M1 occlusion treated with .071" aspiration catheter resulting in eTICI3 reperfusion in both cases. In the fifth patient, the .088" catheter was navigated into the cavernous ICA to support .071" aspiration catheter treatment of an M2 occlusion resulting in eTCI2b67 reperfusion. Procedural duration ranged between 14 and 33 minutes. There were no adverse events.
Conclusion
Intracranial navigation of .088" large-bore catheters in MT appears technically feasible and safe. Larger prospective studies are warranted.
Keywords: Mechanical thrombectomy, aspiration, stroke, .088" catheter
Introduction
Mechanical thrombectomy (MT) is the standard care for large vessel occlusion strokes (LVOS). 1 Randomized controlled clinical trials have shown comparable efficacy between contact aspiration (CA) and stent-retriever (SR) thrombectomy in terms of successful reperfusion and functional outcomes.2–4 However, the thromboaspiration technology continues to evolve at an accelerated pace with the increasing availability of larger and more navigable devices. As both larger catheter inner diameter and larger catheter-to-vessel diameter ratio are known to be associated with better reperfusion and higher chances of complete thrombus ingestion,5–8 the advent of aspiration catheters that more closely approximate the dimeter of the larger proximal vessel represents one of the most promising clot retrieval technologies to improve the treatment of patients with LVOS.
The feasibility of navigating a .088" aspiration catheter (Millipede 088, Perfuze Ltd., Galway, Ireland) into the middle cerebral artery (MCA) and basilar artery was recently demonstrated in a fresh-frozen cadaveric model. 9 In this same study, the Millipede 088 system was compared with two commercially available aspiration catheters (SOFIA 070 Plus, Microvention, Aliso Viejo, CA and ACE 068, Penumbra, Alameda, CA) using different phenotypes of human blood clot analogues in a pulsatile-flow model based on a silicone replica of the human cerebrovasculature. Significantly higher rates of both complete revascularization and first-pass full clot ingestion were seen with the Millipede 088 system. Another in-vitro study using a similar set-up to evaluate the performance of a different .088" aspiration catheter (Route 92 Medical, Inc., San Mateo, CA) demonstrated higher rates of first-pass recanalization with the .088" system versus .070", .068" and .054" aspiration catheters regardless of clot type. In addition, this study showed that the rate of full clot ingestion was a function of catheter diameter (R2 = 0.994). 8 Herein, we describe the first case series of intracranial MT in LVOS patients using an aspiration catheter system with an inner luminal diameter of .088 inches.
Methods
We performed a retrospective review of our institutional database to identify all consecutive patients in whom a TracStar™ or Zoom 88™ (Imperative Care, Campbell, CA) large-bore catheters were utilized in MT. The primary efficacy outcome was successful reperfusion (eTICI 2 b-3) at the end of the procedure. Safety measures were procedure-related complications and rates of symptomatic intracranial hemorrhage (SICH). Secondary efficacy outcome included procedure duration (define as the time from arterial puncture to eTICI 2 b-3) and the modified Rankin scale at 7 days or discharge. The authors applied for and were granted an exempted status from their institutional review board for this research.
Device description
The TracStar™ and the Zoom 88™ Large Distal Platforms (LDP) are commercially available distal access catheters with a .088" inner diameter (ID) (2.24 mm), an 8 French (2.67 mm) outer diameter (OD) and a “bevel-shaped” soft atraumatic tip optimized for navigation through tortuous vasculature. The TracStar™ LDP is available in lengths 95 and 105 cm and has a 15 cm distal flexible segment. The Zoom 88™ LDP has a length of 110 cm and an 18 cm distal flexible segment designed to reach the MCA. Both catheters have Food and Drug Administration 510 (k) clearance and are indicated “for the introduction of interventional devices into the peripheral, coronary, and neuro vasculature” but do not yet have a specific indication for use in aspiration thrombectomy. The catheters are designed to have enough proximal support to allow for their transfemoral navigation as “solo” systems. Alternatively, an 8 F long sheath can be used for their cervical delivery.
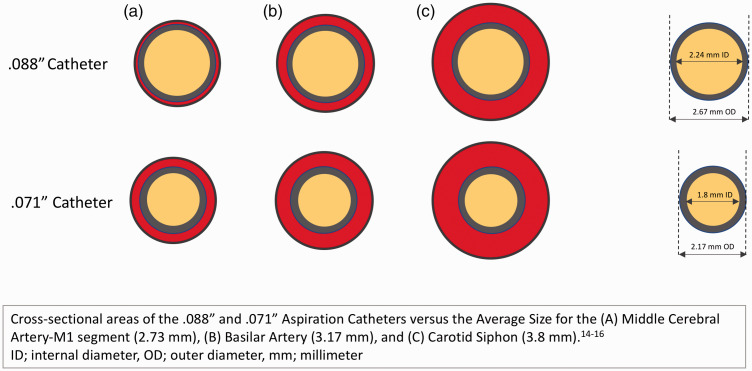
The TracStar™ and the Zoom 88™ LDP provide significantly larger ID and OD compared to the currently commercially available aspiration catheters (074 has ID of 1.88 mm and OD of 2.11 mm, 072 has ID of 1.83 mm and OD of 1.91 mm, 071 has ID of 1.80 and OD of 2.08-2.17 mm, 070 has ID of 1.78 and OD of 2.07, and 068 has ID of 1.73 mm and OD of 2.11 mm). An illustrative comparison of the OD and ID of a .071” versus .088" catheter in relation to the intracranial vessels is shown in Figure 1.
Figure 1.
demonstrates the relationship between the cross-sectional areas (CSA) of 0.071” and 0.088” catheters in relation to the average lumen sizes for the middle cerebral artery (MCA) M1 segment, basilar artery and cavernous segment of the internal carotid artery (ICA). The inner and outer CSAs of the 0.071” catheter cover 43.5% and 59.2%, 32.2% and 43.9%, and 22.4% and 30.5% of the lumen of the MCA-M1, basilar and cavernous ICA, respectively, versus 67.3% and 95.7%, 49.9% and 71%, and 34.7% and 49.4% coverage with the inner and outer CSAs of the 0.088” catheter.
Treatment technique
All procedures were performed in a biplane angiography suite (Philips Azurion) via a transfemoral approach with the aid of an 8 French 80 or 90 cm long sheath (Flexor® Shuttle® Guiding Sheath, Cook Medical, Bloomington, IN). The TracStar™ or Zoom 88™ LDP were navigated intracranially over a .021" microcatheter and .014" guidewire in the posterior circulation and coaxially over a Zoom 71 or Sofia Plus™ aspiration catheter plus a .021" microcatheter and .014" guidewire in the anterior circulation occlusion. Manual aspiration with a 60 cc Vac-Lok syringe was applied on the .088" catheters during the clot retrieval process in all five cases and also on the 070/071 catheters in the three cases where .088" catheter contact aspiration was not the single thrombectomy device.
Results
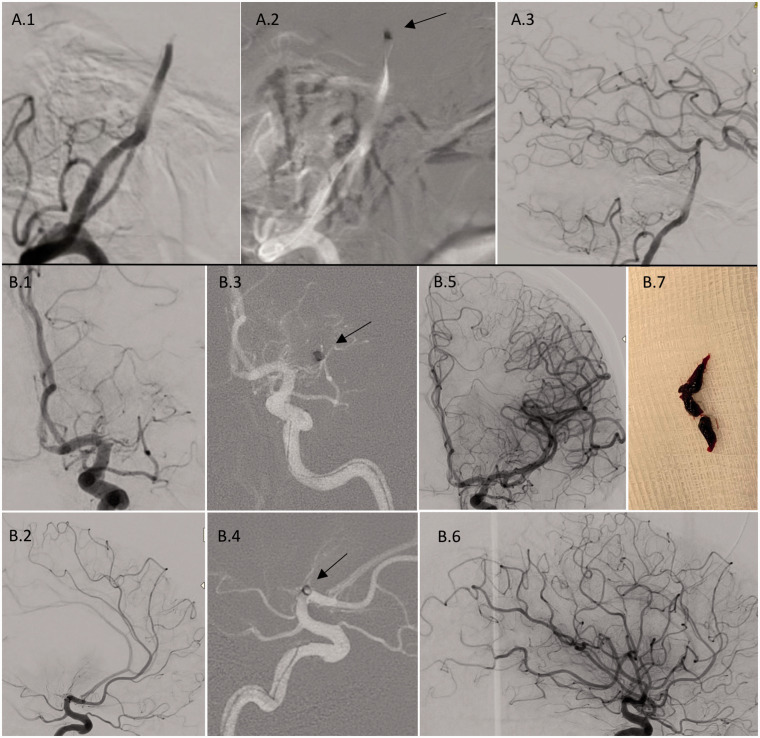
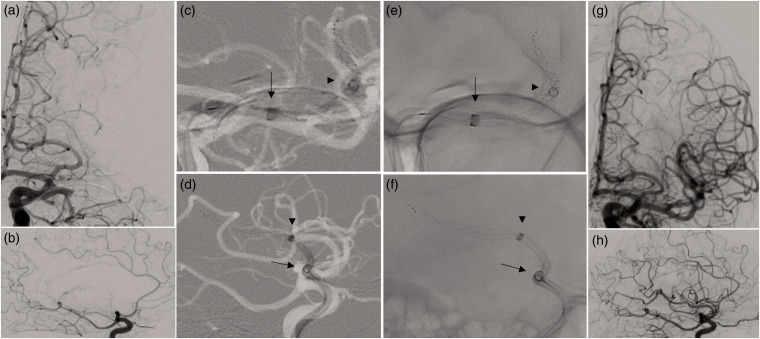
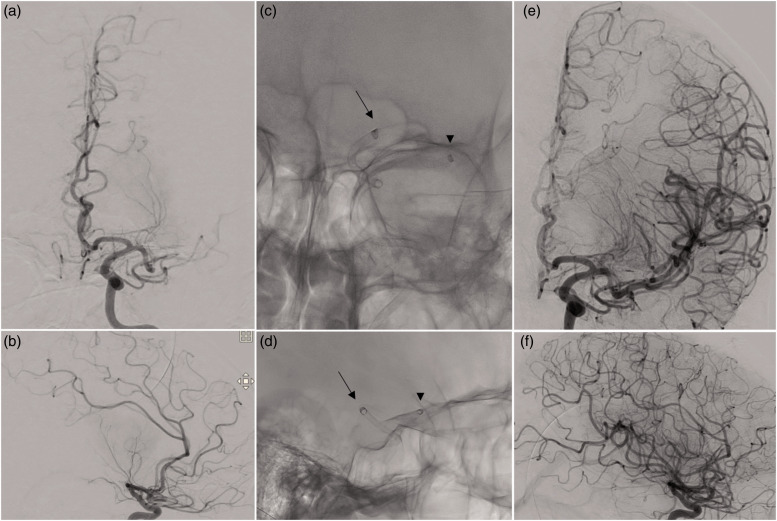
Five consecutive patients (age, range ∼50–85 years; range baseline NIHSS, 17–23, four males; IV tPA use: 4/5; premorbid mRS > 0: 2/5) were treated with the .088" catheters. The TracStar™ LDP became available in March 2020 and was used in posterior circulation case. The Zoom 88™ LDP became available in August 2020 and was used in four anterior circulation cases. The .088" catheters were used as the primary tool for contact aspiration in one patient with distal basilar artery occlusion (Figure 2(a)) and one patient with proximal MCA occlusion (Figure 2(b)) with complete thrombus ingestion (eTICI 3) in the first pass on both cases. In patient#3, there was clot migration from the MCA-M1 to the mid-distal M2 during microcatheter placement. This patient was treated with a combination of a Trevo ProVue™ XP 4.0 x 30 mm stent-retriever (Stryker Neurovascular, Fremont, CA) and a Sofia Plus aspiration catheter with the placement of the .088" catheter in the distal M1 segment for flow control resulting in eTICI 3 reperfusion (Figure 3). Similarly, in patient# 4 with distal left M1 occlusion, the .088" catheter was navigated to the proximal aspect of the M1 and used for flow control during contact aspiration with a .071" catheter resulting in eTICI 3 reperfusion after a single device pass (Figure 4). Notably, the navigation of the .088" catheter into the more distal aspects of the M1 segment was not possible due to the small vessel diameter (2.6 mm) in this case. In the fifth patient, the .088" catheter was navigated into the cavernous ICA to support the navigation of a Zoom 71™ aspiration catheter to treat a proximal superior division dominant M2 trunk occlusion. We were unable to navigate the .088" catheter across the carotid siphon due to excessive tortuosity. Contact aspiration was then performed via the Zoom 71™ catheter resulting in eTCI2b67 reperfusion (Supplemental Figure). Procedural duration ranged between 14 and 33 minutes. There were no adverse events. Specifically, there was no evidence of any significant vasospasm, vessel dissection or SICH. The details for each case are summarized on Table 1.
Figure 2.
A illustrates the lateral angiographic views for the baseline distal basilar artery occlusion (A.1) and the tip of the TracStar™.088" catheter (arrow) at the distal basilar artery on roadmap images (A2). Final angiography, lateral view shows full reperfusion (eTICI 3) (A.3). Figure 2B shows anterior-posterior and lateral views for the baseline angiography depicting a proximal MCA-M1 occlusion (B.1, 2) and the tip of the Zoom 88™ catheter (arrow) at the proximal to mid MCA-M1 segment on roadmap images (B.3, 4). Final angiography shows full reperfusion (eTICI 3) (B.5, 6). (B.7) shows the thrombus that was fully ingested by the.088" catheter.
Figure 3.
demonstrates anterior-posterior and lateral views for the baseline angiography showing complete occlusion of the proximal MCA-M1 segment (A, B) and the tips of the Zoom 88™ (arrow) and Sofia Plus (arrowhead) catheters in the mid MCA-M1 and distal M2, respectively, with a Trevo XP 4 x 30 mm extending into the M3 on roadmap (C, D) and native unsubtracted (E, F) images. Note that original occlusion migrated from the proximal M1 into the distal M2 after the initial microcatheterization. Final angiography shows full reperfusion (eTICI 3) (G, H).
Figure 4.
shows anterior-posterior and lateral views for the baseline angiography depicting an occlusion of the left distal MCA-M1 segment (A, B) and the tips of the Zoom 88™ (arrow) and Zoom 71™ (arrowhead) catheters in the proximal and distal MCA-M1 segment, respectively, on native unsubtracted images (C, D) images. Final angiography shows full reperfusion (eTICI 3) (E, F).
Table 1.
Baseline and procedural characteristic and outcomes.
| Case# | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Age, years | Mid 60 s | Mid 50 s | Mid 70 s | Mid 50 s | Mid 80 s |
| Baseline NIHSS score | 18 | 23 | 17 | 17 | 22 |
| Sex | Male | Male | Male | Male | Female |
| Pre-morbid mRS | 1 | 0 | 1 | 0 | 0 |
| Occlusion site | Distal basilar | Left M1 | Left M1 | Left distal M1 | Left M2 |
| ASPECTS | N/A | 8 | 7 | 7 | 10 |
| IV tPA | Yes | Yes | No | yes | Yes |
| Most Distal .088" Catheter Placement | Distal basilar | Mid M1 | Distal M1 | Proximal M1 | Cavernous ICA |
| Technique used with .088" Catheter | Primary CA | Primary CA | Support .070" CA Catheter/Flow Control | Support .071" CA Catheter/Flow Control | Support .071" CA Catheter |
| Adjunctive devicesa | None | .071" Catheter | .070" CatheterTrevo XP 4x30 mm | .071" catheter | .071" catheter |
| Number of passes | 1 | 1 | 4 | 1 | 2 |
| Arterial puncture to reperfusion, minutes | 14 | 19 | 26 (eTICI2b50)46 (eTICI3) | 15 | 33 |
| Final eTICI | 3 | 3 | 3 | 3 | 2b67 |
| SICH | No | No | No | No | No |
| Other complications | None | None | None | None | None |
| Discharge mRS | 1 | 2 | 4 | 2 | 3 |
a021" microcatheter and .014" guidewire used in all cases.
NIHSS: National Institute of Health Stroke Scale Score; mRS: modified Rankin Scale; CA: contact aspiration; MT: mechanical thrombectomy; eTICI: expanded thrombolysis in cerebral infarction; SICH: symptomatic intracerebral hemorrhage.
Discussion
The present case series provides preliminary data about the technical feasibility and safety of the intracranial navigation of .088" large bore aspiration catheters during MT in stroke. We were able to safely navigate into the distal aspects of the intracranial ICA, MCA-M1 segment and basilar artery in order to use the .088" system for either a primary aspiration or flow control and mechanical support strategy during clot retrieval with smaller ID aspiration catheters and/or stent-retriever. In one case, navigation across the carotid siphon was not possible due to excessive tortuosity. In another case, navigation into the more distal aspects of the MCA-M1 segment was not possible due to small vessel caliber in relation to the Zoom 88™ OD. Fast and successful reperfusion (eTICI 2 b-3) was achieved in all cases with full clot ingestion in a single pass in both of the cases where the .088" catheter was used for primary aspiration. There was no evidence of any significant vasospasm, vessel dissection or SICH.
The physics underlying aspiration thrombectomy are highly complex and influenced by multiple variables including the distorted flow profile due to the irregular geometry of the brain vessels, the nonlinear contact and frictional forces between the thrombus and the vessel wall, and the suction action produced by the aspiration procedure. 10 Notwithstanding, from a pragmatic standpoint, there are three main physical properties that seem to impact the likelihood of a successful aspiration: 1) suction force, 2) aspiration flow and 3) flow control; all of which are optimized by a larger catheter diameter. The laminar flow rate of an incompressible fluid along a cylindrical pipe is governed by Hagen-Poiseuille’s law, which states that flow is a function of radius to the fourth power, pressure, viscosity, and length. However, it is becoming progressively more clear that catheter aspiration flow has little impact on the initial clot retrieval particularly in the setting of a full occlusion as the aspirate is primarily drawn from the vessels proximal to the occlusion.10,11 Moreover, flow near completely or entirely ceases once the catheter tip is occluded by the thrombus. 12 Once antegrade flow is reestablished, aspiration flow probably plays an important role by minimizing distal embolization. Thus, suction force, which is defined by the summation of all the pressure forces acting on the proximal and the distal surfaces of the thrombus, 10 is likely the most important driver of aspiration success. As the retrieving force exerted on the clot by the catheter is a direct function of the vacuum pressure and the cross-sectional area of the catheter tip (i.e. F = P x A), it is not surprising that large bore catheters represent some of the most promising technologies in MT. A potential area of concern is that while high aspiration pressure may help to increase the suction force exerted on the thrombus, it may also increase the risk of the cerebral arteries to collapse and/or increase blood loss. New aspiration pump technologies with cyclical rather than static aspiration may help overcoming some of these limitations as cyclic aspiration may result in higher rates of recanalization and complete clot ingestion at lower magnitudes of pressure. 8
Flow control is important not only to prevent the embolization of debris once flow is reestablished but it also facilitates the actual clot removal process by neutralizing the antagonistic hydromechanical forces acting on the proximal surface of the thrombus. These forces are predominantly a function of the arterial blood pressure and the cross-sectional area of the residual vessel lumen which is defined by the difference between the cross-sectional areas of the original vessel lumen versus the outer aspect of the catheter (Figure 1). Moreover, flow control also affects the aspiration flow by mitigating the competing antegrade flow that originates proximally to the catheter tip and, as such, maximizing the reversed flow deriving distally to the tip. Indeed, balloon guide catheters (BGC) have been associated with better reperfusion outcomes in MT not only when used in conjunction with stent-retrievers but also with the use of contact aspiration as a primary modality. 13 As illustrated on cases #3 & 4, the .088" systems can be brought into the MCA to provide better flow control during the retrieval process of smaller aspiration catheters and/or stent-retrievers. This is achieved through three different mechanisms. First, there is greater obstruction to antegrade flow. For instance, assuming a 2.73 mm vessel diameter for the M1 segment of the MCA, 14 a .074" catheter (OD = 2.11 mm) obstructs only 59.7% of the cross-sectional area of the vessel lumen while a .088" catheter (OD = 2.67 mm) provides 95.7% luminal coverage. Second, as the aspiration flow is proportional to the fourth power of the catheter radius, increasing the ID to .088" dramatically increases the chances of flow reversal in the MCA. Finally, by placing the .088" catheter in the MCA-M1 segment, the operator bypasses the circle of Willis and, as such, can achieve better flow control as compared to the use of a balloon guide catheter where residual antegrade flow via the anterior and posterior communicating arteries into the MCA can, at least theoretically, increase the chances of distal clot embolization. This optimized flow control combined with the significantly higher chances of full clot ingestion with the .088" intracranial catheters should result in a dramatic reduction in the rates of distal embolization with MCA occlusions. However, it is important to acknowledge that the average diameter for the basilar artery (3.17 ± 0.73 mm at the level of the pons) 15 and the intracranial internal carotid artery (ICA, 3.8 ± 0.74 mm at the level of the second angle of the cavernous segment) 16 are typically substantially larger than the diameter of the MCA-M1 segment (2.73 ± 0.23 mm) 14 and, therefore, the overall efficacy of .088" catheters will likely vary according to the occluded vessel size. In this context, one must also consider that none of the currently available BGCs are compatible with .088" systems. This might represent a significant challenge in cases with large ICA clot burden.
Conclusion
In summary, the intracranial navigation of .088" large bore aspiration catheters during MT in stroke appears feasible and safe. As larger catheter platforms allow for both better and local flow control and higher aspiration forces, it is reasonable to expect higher rates of full clot ingestion and faster reperfusion with these systems. Larger prospective studies are needed to properly evaluate the safety and efficacy of this novel approach in relation to the current therapeutic modalities.
Supplemental Material
Supplemental material, sj-jpg-1-ine-10.1177_1591019920982219 for Preliminary experience with 088 large bore intracranial catheters during stroke thrombectomy by Raul G Nogueira, Mahmoud H Mohammaden, Alhamza R Al-Bayati, Michael R Frankel and Diogo C Haussen in Interventional Neuroradiology
Footnotes
Contributorship: RGN: Study conception, design of the work, acquisition of data, interpretation of data, drafting of the manuscript. MM, AA, MRF, DCH: critical revision of manuscript. All authors gave final approval of the version to be published and are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data sharing: All the data of this case series are presented in the manuscript.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: RGN reports consulting fees for advisory roles with Stryker Neurovascular, Cerenovus, Medtronic, Phenox, Anaconda, Genentech, Biogen, Prolong Pharmaceuticals, Imperative Care and stock options for advisory roles with Brainomix, Viz-AI, Corindus Vascular Robotics, Vesalio, Ceretrieve, Astrocyte and Cerebrotech. DCH is a consultant for Stryker and Vesalio and holds stock options at Viz.AI. The other authors have no conflict of interest.
Ethics approval: The authors applied for and were granted an exempted status from their institutional review board for this research.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Provenance and peer review: Not commissioned; externally peer reviewed.
ORCID iDs: Mahmoud H Mohammaden https://orcid.org/0000-0002-7393-9989
Alhamza R Al-Bayati https://orcid.org/0000-0001-8103-1930
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke 2019; 50: e344–e418. [DOI] [PubMed] [Google Scholar]
- 2.Lapergue B, Blanc R, Gory B, et al.; ASTER Trial Investigators. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. Jama 2017; 318: 443–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nogueira RG, Frei D, Kirmani JF, et al.; Penumbra Separator 3D Investigators. Safety and efficacy of a 3-dimensional stent retriever with aspiration-based thrombectomy vs aspiration-based thrombectomy alone in acute ischemic stroke intervention: a randomized clinical trial. JAMA Neurol 2018; 75: 304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turk AS, 3rd, Siddiqui A, Fifi JT, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet 2019; 393: 998–1008. [DOI] [PubMed] [Google Scholar]
- 5.Delgado Almandoz JE, Kayan Y, Wallace AN, et al. Larger ACE 68 aspiration catheter increases first-pass efficacy of ADAPT technique. J Neurointerv Surg 2019; 11: 141–146. [DOI] [PubMed] [Google Scholar]
- 6.Blanc R, Redjem H, Ciccio G, et al. Predictors of the aspiration component success of a direct aspiration first pass technique (ADAPT) for the endovascular treatment of stroke reperfusion strategy in anterior circulation acute stroke. Stroke 2017; 48: 1588–1593. [DOI] [PubMed] [Google Scholar]
- 7.Kyselyova AA, Fiehler J, Leischner H, et al. Vessel diameter and catheter-to-vessel ratio affect the success rate of clot aspiration. J Neurointerv Surg. Epub ahead of print 4 August 2020. DOI: 10.1136/neurintsurg-2020-016459. [DOI] [PubMed]
- 8.Arslanian RA, Marosfoi M, Caroff J, et al. Complete clot ingestion with cyclical ADAPT increases first-pass recanalization and reduces distal embolization. J NeuroIntervent Surg 2019; 11: 931–936. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgerald S, Ryan D, Thornton J, et al. Preclinical evaluation of Millipede 088 intracranial aspiration catheter in cadaver and in vitro thrombectomy models. J Neurointerv Surg. Epub ahead of print 30 January 2020 DOI: 10.1136/neurintsurg-2020-016218. [DOI] [PMC free article] [PubMed]
- 10.Shi Y, Cheshire D, Lally F, et al. Suction force-suction distance relation during aspiration thrombectomy for ischemic stroke: a computational fluid dynamics study. Physics Med 2017; 3: 1–8. [Google Scholar]
- 11.Lally F, Soorani M, Woo T, et al. In vitro experiments of cerebral blood flow during aspiration thrombectomy: potential effects on cerebral perfusion pressure and collateral flow. J Neurointerv Surg 2016; 8: 969–972. [DOI] [PubMed] [Google Scholar]
- 12.Froehler MT. Comparison of vacuum pressures and forces generated by different catheters and pumps for aspiration thrombectomy in acute ischemic stroke. Intervent Neurol 2017; 6: 199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang DH, Kim BM, Heo JH, et al. Effect of balloon guide catheter utilization on contact aspiration thrombectomy. J Neurosurg 2018; 131: 1494–500. DOI: 10.3171/2018.6.Jns181045. [DOI] [PubMed] [Google Scholar]
- 14.Schreiber SJ, Gottschalk S, Weih M, et al. Assessment of blood flow velocity and diameter of the Middle cerebral artery during the acetazolamide provocation test by use of transcranial Doppler sonography and MR imaging. AJNR Am J Neuroradiol 2000; 21: 1207–1211. [PMC free article] [PubMed] [Google Scholar]
- 15.Smoker WR, Price MJ, Keyes WD, et al. High-resolution computed tomography of the basilar artery: 1. Normal size and position. AJNR Am J Neuroradiol 1986; 7: 55–60. [PMC free article] [PubMed] [Google Scholar]
- 16.Pandey AS, Ringer AJ, Rai AT, et al.; Endovascular Neurosurgery Research Group (ENRG). Minimizing SARS-CoV-2 exposure when performing surgical interventions during the COVID-19 pandemic. J Neurointerv Surg 2020; 12: 643–647. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-jpg-1-ine-10.1177_1591019920982219 for Preliminary experience with 088 large bore intracranial catheters during stroke thrombectomy by Raul G Nogueira, Mahmoud H Mohammaden, Alhamza R Al-Bayati, Michael R Frankel and Diogo C Haussen in Interventional Neuroradiology