Abstract
Background
Most studies on the effects of SARS-CoV-2 infection have been conducted with adults and non-pregnant women. Thus, its impacts on maternal health are not yet fully established. This study aimed to verify the relationship between the maternal mortality ratio and the incidence of COVID-19 in the State of Bahia, Brazil, 2020.
Methods
This time-series study used publicly available information in Brazil, to obtain data on maternal deaths and live births in Bahia, State, from January 1, 2011, to December 31, 2020. The time trend of Maternal Mortality Ratio (MMR) was analysed through polynomial regression, of order 6. Expected MMR, monthly (Jan-Dec) and annual values for 2020, were predicted by the additive Holt-Winters exponential smoothing algorithm, with 95% confidence interval, based on the time series of the MMR from 2011 to 2019, and the accuracy of the forecasts for 2020 was assessed by checking the smoothing coefficients and the mean errors. According to the statistical forecast, the MMR values recorded in the year 2020 were compared to those expected.
Results
In 2020, the annual MMR in Bahia, Brazil, was 78.23/100,000 live births, 59.46% higher than the expected ratio (49.06 [95% CI 38.70–59.90]). The increase in maternal mortality ratio relative to expected values was observed throughout the 2020 months; however, only after May, when the COVID-19 epidemic rose sharply, it exceeded the upper limit of the 95% CI of the monthly prediction. Of the 144 registered maternal deaths in 2020, 19 (13.19%) had COVID-19 mentioned as the cause of death.
Conclusions
Our study revealed the increase in maternal mortality, and its temporal relationship with the incidence of COVID-19, in Bahia, Brazil, in 2020. The COVID-19 pandemic may be directly and indirectly related to this increase, which needs to be investigated. An urgent public health action is needed to prevent and reduce maternal deaths during this pandemic, in Brazil.
Introduction
The emergence and global spread of the novel coronavirus, SARS-CoV-2, from December 2019, caused a respiratory disease (COVID-19) pandemic which was already affected until February 11, 2021 107,818,965 individuals and 2,362,704 deaths in the world [1]. The COVID 19 pandemic hit Brazil in February 2020, and 1 year later 9,524,640 cases and 231,534 deaths were reported, corresponding to 2,4% case fatality rate, and mortality rate of 110.2 deaths per 100,000 inhabitants [2], being on that date, the third country with the highest number of cases worldwide [1].
The clinical and epidemiological profile observed, at the beginning of the epidemic in China, showed that elderly (60 years old or more) with comorbidities such as diabetes, hypertension, heart disease, obesity, pneumopathies and immunosuppressed individuals were at higher risk for complications and deaths for COVID19, as has been observed in many countries affected by this pandemic [3–6]. At earlier stages of the epidemic, pregnant women without comorbidities were not considered at greater risk for COVID-19 and its related complications. However, with the greater spread of this disease, some authors began to describe the occurrence of severe forms, as well as abortion and deaths, even among pregnant women without comorbidities [7, 8].
These findings have been reported in many countries such as the United States, United Kingdom, France, Mexico and Brazil [2, 9–12], and contributed to subsidise PAHO, to issue an Alert in August 2020, encouraging member countries to redouble efforts to ensure access and continuity of prenatal care, with special attention to the early detection of signs, symptoms, and severity of clinical manifestations of COVID-19 [13]. It is known that during pregnancy the women present a relative immunodeficiency and it could worsen the clinical evolution of COVID 19 and lead to negative outcomes in the mothers and foetus [14].
Brazil is a middle-income country where the maternal mortality is still high [15] although it has been presenting a slow declining trend [16, 17]. Since the 1990 s, improvements in the living and health conditions of the population in this country, which includes women of reproductive age, have contributed to an important reduction in maternal deaths [18], but not enough to reach the Brazilian government target of less than 30 maternal deaths for every 100,000 live births [19]. Then, the COVID-19 pandemic may negatively influence the evolution of this indicator in Brazil.
Given the uncertainties about the possible impact of the COVID-19 on maternal mortality, this study aimed to verify the relationship between the maternal mortality ratio and the incidence of COVID-19 in the State of Bahia, Brazil, 2020.
Methods
A retrospective time series study was carried out on maternal mortality during the COVID 19 pandemic in Bahia, Brazil, 2020. Maternal death was defined as established by the World Health Organization’s International Classification of Diseases (ICD-10) [20].
The website of the Bahia State Health Secretariat [21] was accessed to obtain the data for this study. Epidemiological bulletins [22] were the sources of data on the number of new cases of COVID-19 and population estimate, in Bahia. According to the month of occurrence, the number of maternal deaths and live births, from January 2011 to December 2020, were extracted from the public domain health open data, DATASUS [23, 24]. The DATASUS aggregates health data from different Brazilian official information systems. Data on maternal deaths come from the Mortality Information System (SIM), which in 2011 reached 96.1% nationwide coverage [25]. Data on live births come from the Live Birth Information System (SINASC), which in 2010 has coverage of 94,8% in Brazil, and most recent studies in large Brazilian cities point to 100% coverage [26, 27]. All maternal deaths occurred in 2020 were included in our analyses.
We estimated maternal mortality ratio (MMR) by dividing the number of maternal deaths by the number of live births, multiplied by 100,000, for each month and year [28]. Annual (from 2011 to 2020) and monthly (from January to December 2020) MMR were plotted on a time curve. The COVID-19 incidence in Bahia, per month in 2020, was calculated by the ratio between the number of new cases of this disease and the population estimate, followed by the multiplication by 100,000.
The time trend of MMR in the period from 2011 to 2020 was verified through polynomial regression analysis, of order 6. The additive Holt-Winters exponential smoothing model (ETS A, A, A), which considers the additive parameters error, trend and seasonality, was used to analyse the MMR time series 2011–2019 and predict the values for 2020, with a 95% confidence interval. Then, the real MMR values recorded in Bahia in 2020 were compared to those expected. The accuracy of the monthly and yearly MMR forecasts for 2020 was assessed by checking the Alpha, Beta and Gamma smoothing coefficients and the values of Scaled Mean Absolute Error (MASE), Symmetric Mean Percentage Absolute Error (sMAPE), Mean Absolute Error (MAE) and Root of the Mean Quadratic Simulation Error (RMSE).
As this study was carried out using public domain data, it was not necessary to submit it to the Research Ethics Committee.
Results
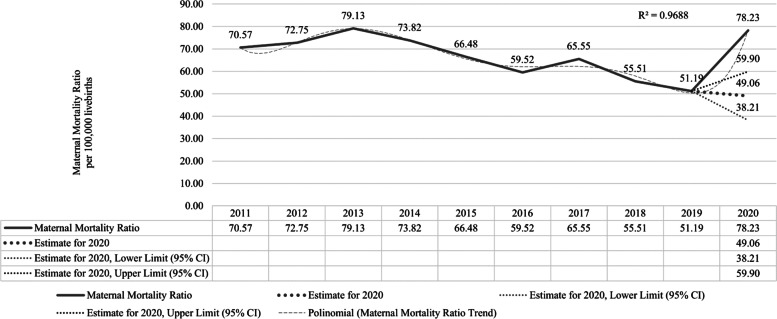
Between 2011 and 2013, the MMR in Bahia increased by 12.1%. From 2013 to 2019, it was decreasing (-35.13%) over the years. However, in 2020, the MMR was 78.23/100,000 live births (lb.), an excess of 59,46% from the expected for this year (49.06 [95% CI 38.70–59.90]) (Fig. 1).
Fig. 1.
Maternal Mortality Ratio time series (per 100,000 live births) 2011–2019, and recorded* versus predicted** values for 2020, with 95% confidence interval. Bahia, Brazil, 2011–2020. Source: Brazilian’s Mortality Information System (SIM/DATASUS) and Live Birth Information System (SINASC/DATASUS). *Data updated on February 04, 2021. ** Values for 2020 predicted by Holt-Winters additive exponential smoothing, based on the 2011–2019 yearly MMR time series. Smoothing coeficients: Alpha = 0.75; Beta = 0.00; Gamma = 0.00. Forecast Accuracy: Scaled Mean Absolute Error (MASE) = 0.75; Symmetric Mean Percentage Absolute Error (sMAPE) = 0.07; Mean Absolute Error (MAE) = 4.56; Root of the Mean Quadratic Simulation Error (RMSE) = 5.53
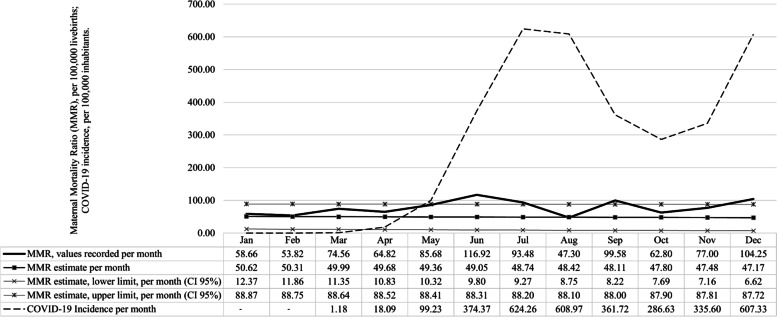
From January to April 2020, the predicted MMR values were not significantly different from the observed values for this period. Following a time pattern of increase and decrease like the COVID-19 incidence curve, in May the MMR increased and was close to the predicted maximum limit (Recorded MMR = 85.68/100,000 l.b.; Expected MMR = 49.36 [CI95% 10.32–88.41]). After that, the MMR exceeded the values expected for the period in June (Recorded MMR = 116.92/100,000 l.b.; Expected MMR = 49.05 [CI95% 9.80–88.31]), July (Recorded MMR = 93.48/100,000 l.b.; Expected MMR = 48.74 [CI95% 9.27–88.20]), September (Recorded MMR = 99.58/100,000 l.b.; Expected MMR = 48.11 [CI95% 8.22–88.00]) and December (Recorded MMR = 104.25/100,000 l.b.; Expected MMR = 47.17 [CI95% 6.62–87.72]) (Fig. 2).
Fig. 2.
Maternal Mortality Ratio (MMR) per 100,000 live births, and the incidence of COVID-19 per 100,000 inhabitants, per month 2020*, and predicted** MMR values with 95% confidence interval, for the same period. Bahia, Brazil, 2020. Source: Brazilian’s Mortality Information System (SIM/DATASUS) and Live Birth Information System (SINASC/DATASUS); COVID-19 Bahia Epidemiological Bulletins No. 01, 04, 35, 67, 98, 129, 160, 190, 221, 251 and 282/2020. *Data updated on February 04, 2021. **Values for 2020 predicted by Holt-Winters additive exponential smoothing, based on the 2011–2019 monthly MMR time series. Smoothing coefficients: Alpha = 0.10; Beta = 0.00; Gamma = 0.00. Forecast Accuracy: Scaled Mean Absolute Error (MASE) = 0.57; Symmetric Mean Percentage Absolute Error (sMAPE) = 0.28; Mean Absolute Error (MAE) = 14.16; Root of the Mean Quadratic Simulation Error (RMSE) = 16.53
From May to August, the COVID-19 pandemic rose sharply in Bahia, and its incidence per month reached 99.23, 374.37, 624.26, 608.97 / 100,000 inhabitants (inh.), respectively. A slight reduction in the incidence of COVID-19 was noted in September (361.72/100,000 inh.) and October (286.63/100,000 inh.), followed by a further increase in November (335.60/100,000 inh.) and December (607.33/100,000 inh.).
Of the 144 maternal death recorded in 2020, 19 (13.19%) were related to COVID-19 (Table 1) and occurred in the months April (01), May (02), June (05), July (06), September (02) and December (03). Of these, 15 death certificates contained mention of ICD-10 U071 (COVID-19, identified virus) among the causes of death, which means a SARS-CoV-2 infection diagnosed by laboratory examination, and 04 contained mention of ICD-10 U072 (COVID-19, unidentified virus), which represents diagnosis by clinical-epidemiological and imaging exams.
Table 1.
Number of maternal deaths according to the classification of underlying causes group, by ICD-10 and year of occurrence, Bahia, Brazil, 2011–2020
| ICD-10 | Underlying Causes Group | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year of occurrence | Total | With mention of COVID-19a | ||||||||||
| A30-A49 | Other bacterial diseases | - | - | 1 | - | - | - | - | - | - | - | - |
| B24 | Human immunodeficiency virus [HIV] disease | 3 | - | 1 | 2 | 1 | 2 | 4 | 1 | - | 1 | - |
| D37-D48 | Neoplasm of uncertain or unknown behavior | - | - | - | - | - | - | - | - | - | 1 | - |
| F50-F59 | Behavioral syndromes associated with physiological disorders and physical factors | - | - | 1 | 1 | - | - | - | - | - | - | - |
| O00-O08 | Pregnancy ending in abortion | 12 | 12 | 4 | 11 | 11 | 10 | 16 | 10 | 4 | 11 | 1 |
| O10-O16 | Edema, proteinuria, and hypertensive disorders in pregnancy, delivery and the puerperium | 25 | 30 | 33 | 38 | 35 | 23 | 25 | 25 | 30 | 32 | 2 |
| O20-O29 | Other maternal disorders predominantly related to pregnancy | 2 | 4 | 4 | 1 | 4 | 3 | 7 | 1 | 2 | 9 | - |
| O30-O48 | Assistance provided to the mother for reasons related to the fetus and amniotic cavity and for possible problems related to delivery | 12 | 9 | 9 | 9 | 6 | 13 | 7 | 9 | 8 | 18 | 1 |
| O60-O75 | Complications of labor and delivery | 24 | 29 | 30 | 23 | 27 | 17 | 24 | 19 | 18 | 17 | 1 |
| O85-O92 | Complications related predominantly to the puerperium | 14 | 18 | 23 | 26 | 14 | 12 | 14 | 12 | 11 | 12 | 1 |
| O94-O99 | Other obstetric conditions, not elsewhere classified | 60 | 51 | 55 | 40 | 40 | 39 | 37 | 37 | 28 | 43 | 13 |
| Total | 152 | 153 | 161 | 151 | 138 | 119 | 134 | 114 | 101 | 144 | 19 | |
Source: Brazilian’s Mortality Information System (SIM/DATASUS), data updated on February 04, 2021
aNumber of maternal deaths, according to the underlying cause group of the ICD-10, with mention of COVID-19 among the causes attested in the death certificate
Discussion
This study shows the rise in maternal mortality ratio in Bahia in 2020, insofar the officially recorded maternal deaths are far higher than the expected number for this year. A temporal relationship with COVID-19 pandemic was observed, since months in which the maternal mortality ratio exceeded the predicted value coincided with those with the highest incidence of COVID-19 in the state. The small number of maternal death certificates with COVID-19 diagnosed among the causes of death, which alone do not justify the excess of deaths observed in 2020, and leads us to consider the possibility of under diagnoses, since Brazil has not implemented universal testing of pregnant women [8] for COVID-19, and potential indirect effects of the pandemic. Maternal deaths attested due to not specified or ill-defined causes, related to ICD-10 O98.5—Other viral diseases complicating pregnancy, childbirth and the puerperium, for example, J18.9—Pneumonia, of unspecified aetiology or U04.9—Severe acute respiratory syndrome [SARS] unspecified, can mask undiagnosed cases of COVID-19.
Maternal deaths could result from maternal illness directly related to COVID-19 infection or an indirect effect of health service disruptions, and other indirect effects caused by the pandemic. First, maternal deaths directly related to COVID-19 in Brazil has been alarmed high [8]. However, it is also important to consider the possible indirect contributions of the pandemic in the occurrence of these deaths, as many pregnant women have stopped to attend antenatal appointments most likely because they did not feel protected against SARS-CoV-2 infection. Also, there may have been delay or resistance from some maternities with a lower level of complexity, to provide care to pregnant women with flu-like symptoms, or difficulty in the transportation of pregnant women to health units of a higher level of complexity located in other municipalities. In addition, some of these maternal deaths can still be under epidemiological investigation and analysis by the Epidemiological Surveillance Services and the State Maternal Mortality Studies Committee, so, the final cause of death can still be changed, and some deaths which COVID -19 has not been mentioned could emerge after evaluation. Lastly, the change in the organization of prenatal services during the pandemic, with a limited number of medical care provided to avoid crowding in the waiting rooms, may have caused delays in care, contributing to maternal deaths that could otherwise be avoided.
Maternal mortality is an indicator of access and quality of women’s health care [19], and this increase in maternal mortality showed in 2020 represents an unacceptable setback, that needs to be better clarified and faced. We understand that the public and private health sectors face many challenges in ensuring access and adequate care for all pregnant women. However, although the impact of the COVID-19 pandemic may affect many of them, it must be more remarkable for the poorest women, as occur already in the maternal mortality from other causes, to whom women of greater socioeconomic vulnerability are also more affected [18, 29, 30]. Therefore, the COVID-19 pandemic may exacerbate the social inequalities and injustices that already exist in Brazil [31, 32].
This study has limitations inherent to the use of i) secondary data; ii) relatively small number of maternal deaths, that makes the time series more susceptible to variations, and; iii) preliminary data on maternal deaths in 2020, due to possible delays in feeding official information systems. In addition, as time series studies correspond to a subtype of aggregate (or ecological) studies, they are vulnerable to ecological fallacy. Consequently, its results cannot be inferred for the individual level. Added to this the fact that it is a descriptive study, and thus a cause-effect relationship cannot be inferred from its results. Another limitation refers to the forecasting. In general, in the exponential smoothing of time series, the parameter ranges and initial values are arbitrary, and this can impair the accuracy of the forecast. In our study, it was possible to observe that the confidence interval for monthly forecasts was wider, indicating that there was less precision in these, when compared to the annual estimates. The model applied in our study use only the data from the series itself to project its forecasting, does not incorporate external variables, for example, environmental factors, or public policy interventions. Despite that, the Holt-Winters (ETS AAA) model is considered to be robust and has excellent performance for short-term forecasts [33, 34]. Notwithstanding these weaknesses, our study suggests devastating consequences for maternal mortality during the COVID-19 pandemic in Bahia, Brazil. It points to the need to conduct more research across the country during the pandemic to confirm these estimates and understand the long-term impacts of this disease on maternal health.
Acknowledgements
The authors would like to thank the anonymous reviewers. His comments and suggestions provided important improvements to the initial manuscript.
Abbreviations
- ICD
International Classification of Disease 10ª
- MMR
Maternal mortality ratio
- SIM
Mortality Information System
- SINASC
Live Births Information System
- inh.
Inhabitants
- l.b.
Live births
Authors’ contributions
RCOCS, MCNC and MGT conceived and designed the study, RCOCS, EMFS, MLAB, GRS, TPS collected the data, RCOCS, ESP, EMRN carried out the data analysis and interpretation. RCOCS, MCNC, EMRN, ESP and MGT wrote the first draft of the article. All authors critically revised the manuscript and approved the final version.
Funding
ESP is funded by the Wellcome Trust (grant number 213589/Z/18/Z), however, the funder of this study had no role in study design, data collection, data analysis, data interpretation, or the writing of the report.
Availability of data and materials
The data that support the findings of this study are available on request from the first author (email contact: ritacarvalhosauer@gmail.com). The data are publicly available.
Declarations
Ethics approval and consent to participate
The data is publicly available; therefore, ethical approval is not required for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Worldmeters. Coronavirus update (Live) COVID-19 virus pandemic. 2020. https://www.worldometers.info/coronavirus/. Accessed 11 Feb 2020.
- 2.Brasil. Ministério da Saúde. Painel Coronavírus: Síntese de casos, óbitos, incidência e mortalidade. OpenDATASUS. 2020. https://covid.saude.gov.br/. Accessed 11 Feb 2021.
- 3.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ejaz H, Alsrhani A, Zafar A, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health. 2020;13(12):1833–1839. doi: 10.1016/j.jiph.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiang G, Xie L, Chen Z, et al. Clinical risk factors for mortality of hospitalized patients with COVID-19: systematic review and meta-analysis. Ann Palliat Med. 2021;10(2):22–22. doi: 10.21037/apm-20-1278. [DOI] [PubMed] [Google Scholar]
- 6.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westgren M, Pettersson K, Hagberg H, Acharya G. Severe maternal morbidity and mortality associated with COVID-19: the risk should not be downplayed. Acta Obstet Gynecol Scand. 2020;99(7):815–816. doi: 10.1111/aogs.13900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takemoto MLS, Menezes MDO, Andreucci CB, et al. The tragedy of COVID‐19 in Brazil: 124 maternal deaths and counting. Int J Gynecol Obstet. 2020;151(1):ijgo.13300. doi: 10.1002/ijgo.13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lumbreras‐Marquez MI, Campos‐Zamora M, Lizaola‐Diaz de Leon H, Farber MK. Maternal mortality from COVID‐19 in Mexico. Int J Gynecol Obstet. 2020;150(2):266–267. doi: 10.1002/ijgo.13250. [DOI] [PubMed] [Google Scholar]
- 10.Kayem G, Lecarpentier E, Deruelle P, et al. A snapshot of the Covid-19 pandemic among pregnant women in France. J Gynecol Obstet Hum Reprod. 2020;49(7):101826. doi: 10.1016/j.jogoh.2020.101826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vallejo V, Ilagan JG. A postpartum death due to coronavirus disease 2019 (COVID-19) in the United States. Obstet Gynecol. 2020;136(1):52–55. doi: 10.1097/AOG.0000000000003950. [DOI] [PubMed] [Google Scholar]
- 12.Knight M, Bunch K, Vousden N, et al. Characteristics and outcomes of pregnant women hospitalised with confirmed SARS-CoV-2 infection in the UK: a national cohort study using the UK Obstetric Surveillance System (UKOSS). medRxiv. 2020:2020.05.08.20089268. 10.1101/2020.05.08.20089268
- 13.Organización Panamericana de la Salud. Alerta Epidemiológica: COVID-19 durante el embarazo- 13 de agosto de 2020 - OPS/OMS. 2020. https://www.paho.org/es/documentos/alerta-epidemiologica-covid-19-durante-embarazo-13-agosto-2020. Accessed 13 Oct 2020.
- 14.Liu H, Wang LL, Zhao SJ, Kwak-Kim J, Mor G, Liao AH. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139:103122. doi: 10.1016/j.jri.2020.103122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. The Global Health Observatory. World Health Data Platform. Maternal mortality ratio (per 100 000 live births). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/maternal-mortality-ratio-(per-100-000-live-births). Accessed 12 Feb 2021.
- 16.Ministério da Saúde. Portal da Secretaria de Atenção Primária a Saúde (SAPS). Brasil reduziu 8,4% a razão de mortalidade materna e investe em ações com foco na saúde da mulher. 2020. https://aps.saude.gov.br/noticia/8736. Accessed 12 Feb 2021.
- 17.Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the un Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387(10017):462–474. doi: 10.1016/S0140-6736(15)00838-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Victora CG, Aquino EM, Do Carmo Leal M, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: Progress and challenges. Lancet. 2011;377(9780):1863–1876. doi: 10.1016/S0140-6736(11)60138-4. [DOI] [PubMed] [Google Scholar]
- 19.BRASIL. Ministério da Saúde. Secretaria de Vigilância em Saúde. Bol Epidemiol 20. 2020;51. https://portalarquivos2.saude.gov.br/images/pdf/2020/janeiro/20/Boletim-epidemiologico-SVS-02-1-.pdf.
- 20.World Health Organization. Classificação Internacional de Doenças (CID-10): Décima Revisão, Vol. 1; 1200p. (Pub: Edusp). ISBN 13: 9788531401930. São Paulo; 2017.
- 21.Governo da Bahia. Secretaria Estadual de Saúde. http://www.saude.ba.gov.br/. Accessed 5 Feb 2021.
- 22.Governo da Bahia. Secretaria Estadual de Saúde. Boletins Epidemiológicos Diários – Covid-19 | Sesab. 2020. http://www.saude.ba.gov.br/temasdesaude/coronavirus/boletins-diarios-covid-19/. Accessed 5 Feb 2021.
- 23.Governo da Bahia. Secretaria Estadual de Saúde. DATASUS TabNet Win32 3.0: Óbitos de mulheres em idade fértil e óbitos maternos - Bahia. http://www3.saude.ba.gov.br/cgi/deftohtm.exe?sim/obitomat.def. Accessed 5 Feb 2021.
- 24.Governo da Bahia. Secretaria Estadual de Saúde. DATASUS TabNet Win32 3.0: Dados sobre Nascidos vivos - Bahia. http://www3.saude.ba.gov.br/cgi/deftohtm.exe?sinasc/nvba.def. Accessed 5 Feb 2021.
- 25.Brasil. Ministério da Saúde. Coordenação Geral de Informações e Análise Epidemiológica. Consolidação Do Sistema de Informações Sobre Nascidos Vivos. 2013. http://tabnet.datasus.gov.br/cgi/sinasc/Consolida_Sinasc_2011.pdf.
- 26.Bonilha EDA, Vico ESR, Freitas MD, et al. Cobertura, completude e confiabilidade das informações do Sistema de Informações sobre Nascidos Vivos de maternidades da rede pública no município de São Paulo, 2011. Epidemiol e Serv saude Rev do Sist Unico Saude do Bras. 2018;27(1):e201712811. doi: 10.5123/s1679-49742018000100011. [DOI] [PubMed] [Google Scholar]
- 27.Paiva Gabriel B, Morcillo M, do Carmo M, Gilberto IM, Daolio D, Lemos R. Avaliação das informações das Declarações de Nascidos Vivos do Sistema de Informação sobre Nascidos Vivos (Sinasc) em Campinas, São Paulo, 2009. Rev Paul Pediatr. 2009;32(3):183–188. doi: 10.1590/0103-0582201432306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brasil. Ministério da Saúde. Rede Interagencial de Informações para a Saúde RIPSA. TABNET/DATASUS. Razão de mortalidade materna (Taxa de mortalidade materna, coeficiente de mortalidade materna) C . 3 2010. Indicadores e Dados Básicos - Brasil - 2012. 2017. http://tabnet.datasus.gov.br/tabdata/LivroIDB/2edrev/c03.pdf. Accessed 6 Sept 2020.
- 29.Tatyana Maria Silva de Souza R, Angelo Giuseppe R. Near miss materno e iniquidades em saúde: Análise de determinantes contextuais no Rio Grande do Norte, Brasil. Cien Saude Colet. 2016;21(1):191–201. doi: 10.1590/1413-81232015211.20802014. [DOI] [PubMed] [Google Scholar]
- 30.Leal MDC, Gama SGND, Pereira APE, Pacheco VE, Carmo CND, Santos RV. The color of pain: racial iniquities in prenatal care and childbirth in Brazil. Cad Saude Publica. 2017;33:e00078816. doi: 10.1590/0102-311X00078816. [DOI] [PubMed] [Google Scholar]
- 31.Demenech LM, Dumith SDC, Vieira MECD, Neiva-Silva L. Desigualdade econômica e risco de infecção e morte por COVID-19 no Brasil. Rev Bras Epidemiol. 2020;23:e200095. doi: 10.1590/1980-549720200095. [DOI] [PubMed] [Google Scholar]
- 32.Campello T, Gentili P, Rodrigues M, Rizzo HG. Faces da desigualdade no Brasil: um olhar sobre os que ficam para trás Faces of inequality in Brazil: a look at those left behind. Saúde Debate. 2018;42(3):54–66. doi: 10.1590/0103-11042018S305. [DOI] [Google Scholar]
- 33.Gardner ES. Exponential smoothing: the state of the art. J Forecast. 1985;4(1):1–28. doi: 10.1002/for.3980040103. [DOI] [Google Scholar]
- 34.Hyndman RJ, Athanasopoulos G. Exponential smoothing. In: OTexts, ed. Forecasting: principles and practice. 3rd ed. Melbourne; 2021. https://otexts.com/fpp3/. Accessed 31 Mar 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the first author (email contact: ritacarvalhosauer@gmail.com). The data are publicly available.