Abstract
A 7-year 10-month-old boy was evaluated for mouth breathing and snoring habits. Examination revealed soft convex tissues, maxillary protrusion, mandibular retrusion, and a class II sagittal osteofascial pattern. The patient failed a water holding test. He was clinically diagnosed with skeletal class II malocclusion caused by mouth breathing. Under interceptive guidance of occlusion (iGo), the malocclusion improved with fixed maxillary expansion using functional appliances and interventional treatment of mouth breathing by lip closure exercises. These treatments enabled the patient to gradually return to nasal breathing and guided him to develop physiological occlusion for a coordinated jaw-to-jaw relation. At the 5-year 2-month post-correction follow-up visit (at the age of 13 years), the patient had stable occlusion, a coordinated osteofascial pattern, and normal dentition, periodontium, and temporomandibular joints.
Keywords: Interceptive guidance of occlusion, mouth breathing, mixed dentition children, skeletal class II malocclusion, lip closure exercise, fixed maxillary expansion, early treatment appliance, case report
Introduction
Long-term mouth breathing changes the temporomandibular joint structure and periarticular muscle groups, causing class II malocclusion and affecting the maxillofacial appearance and development.1–6 Interceptive guidance of occlusion (iGo) in pediatric patients allows for regular observation of the maxillofacial development and timely application of jaw correction, dental arch shaping, tooth alignment, and retainment of eruption induction-based occlusion development based on the patients’ functional occlusion development. This treatment enables children to develop physiological occlusion by the age of 12 years and realize stable occlusion and a coordinated facial appearance. We herein report a case of skeletal class II malocclusion caused by mouth breathing in pediatric patient undergoing iGo with fixed maxillary expansion using an early treatment appliance (ETA) and lip closure exercises.
Case report
A 7-year 10-month-old boy of Han nationality visited the Department of Pediatric Dentistry, College of Stomatology of Guangxi Medical University on 3 December 2013 because of lip and teeth exposure that affected his facial appearance. His mother denied systemic diseases or a history of drug allergy, but she noted that he had mouth breathing and snoring habits. The patient had a mandibular deficiency similar to that of his father. Facial and temporomandibular joint examinations showed a bilaterally symmetrical raised face and normal temporomandibular joints. Oral examination showed the stage of dentition replacement, a molar distal relationship, deep overbite, deep overjet, 11 and 21 tipping, 0.5-mm spaces in 11 and 21, a narrow upper dental arch, a highly arched palatal cover, crowded lower front teeth, and 3-mm offsetting of the mandibular midline to the right (Figure 1(a)–(e)).
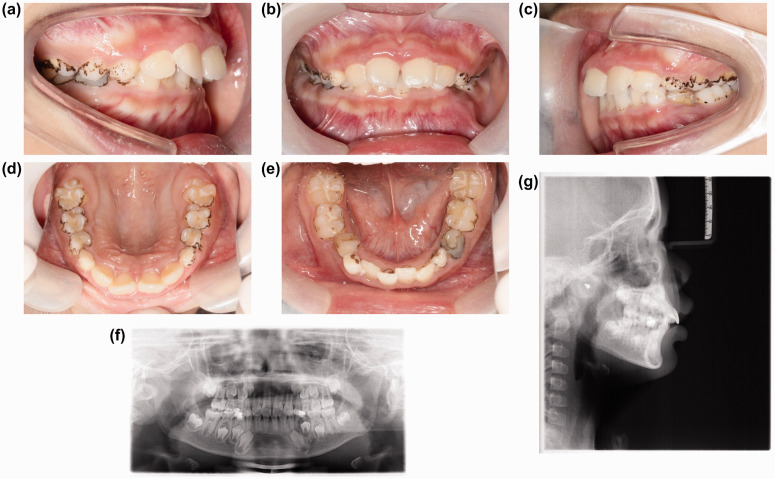
Figure 1.
Intraoral photographs, panoramic radiograph, and lateral cephalogram before treatment (captured on 6 December 2013). (a–e) Intraoral photographs. (f) Panoramic radiograph. (g) Lateral cephalogram.
A preoperative panoramic radiograph (Figure 1(f)) on 6 December 2013 showed the stage of mixed dentition; a normal number of teeth; a normal order of replaced teeth; caries of dental crowns at 55, 54, 74, 84, and 85; periapical lesions of 74; and disappearance of the dental follicle and ectopic tooth germ of 34. Cephalometric analysis (Figure 1(g)) showed maxillary excess (SNA of 85.8°), normal mandibular development (SNB of 79°), skeletal class II (ANB of 6.3°), even angles, protrusion of the upper anterior teeth, and lingual inclination of the lower anterior teeth. The adenoid-nasopharyngeal ratio was 0.69, suggesting moderate adenoid hypertrophy. Estimation from Moyers’ table showed moderate upper dentition crowding (−6 mm) and mild lower dentition crowding (−2 mm). The patient failed a water holding test. He was diagnosed with mouth breathing and skeletal class II malocclusion.
Treatment process
Odontotherapy: Necrotic tissue was removed and a filling was placed at 54, and 74 was removed (before the correction).
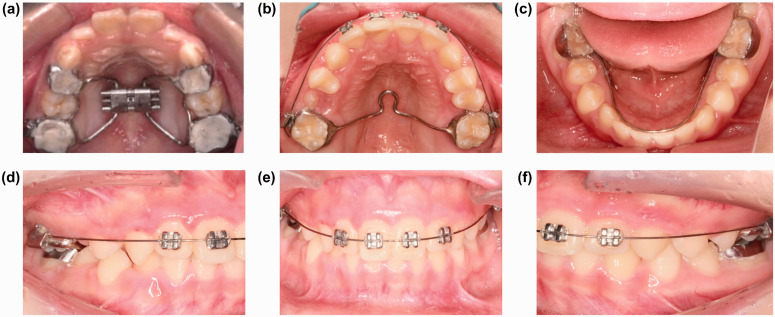
A maxillary spiral expander (Figure 2(a)) was used to improve crowding (for 3 months from December 2013 to March 2014), and lip closure exercises were intensified (15 minutes every day until the end of the correction).
Fixed correction using a 2 × 4 appliance (Figure 2(b)–(f)) was performed to align the front teeth, and a transpalatal arch was used to maintain the gaps between the front teeth and the lower hyoid arch (for 3 months from April 2014 to July 2014).
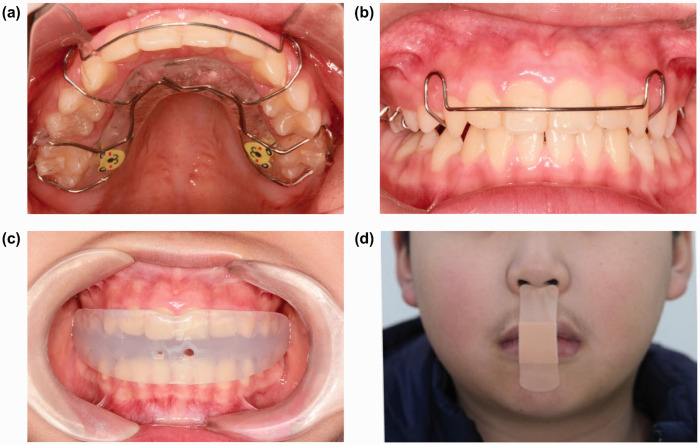
The ETA was worn at night, and lip stickers were used to help intervene in mouth breathing (for 6 months from August 2014 to January 2015).
Retaining stage: A Hawley retaining appliance (Figure 3(a), (b)) was worn in the daytime (for 6 months from February 2015 to September 2015), and the ETA (Figure 3(c), (d)) was worn during sleep at night to retain eruption induction-based occlusion development.
Figure 2.
Treatment process. (a) Fixed maxillary expansion; (b) Fixed correction using a 2 × 4 appliance + transpalatal arch. (c) Lower hyoid arch maintenance. (d) Right molar relation. (e) Centric occlusion. (f) Left molar relation.
Figure 3.
Eruption induction-based occlusion development and mouth breathing intervention. (a) Hawley retaining appliance. (b) Hawley retaining appliance (centric occlusion). (c) Early treatment appliance. (d) Lip sticker.
Treatment outcome
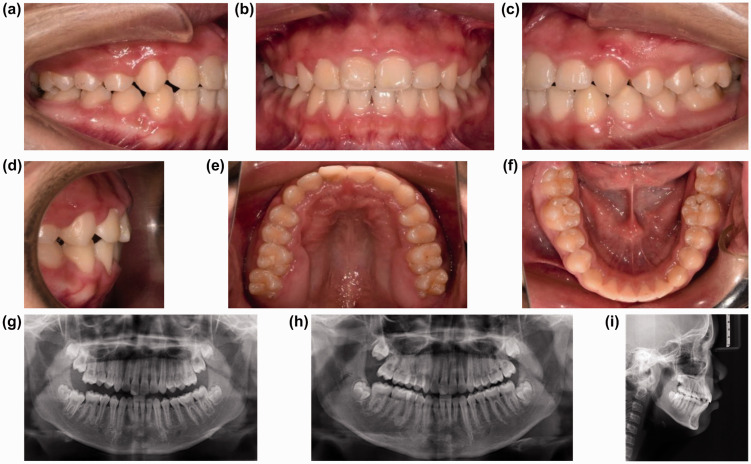
At the 5-year 2-month post-correction follow-up visit (when the patient was 13 years old), the patient had stable occlusion, a coordinated osteofascial pattern, and normal tooth bodies, periodontium, and temporomandibular joints (Figure 4). The lateral cephalometric superimposition before and after the correction is shown in Figure 5.
Figure 4.
Treatment outcome. (a–f) Intraoral photographs at the end of the correction (captured on 14 February 2019). (g, h) During the correction (captured on 5 April 2017) and intraoral photographs at the late stage (captured on 16 August 2018). (i) Lateral cephalogram after treatment (captured on 16 August 2018).
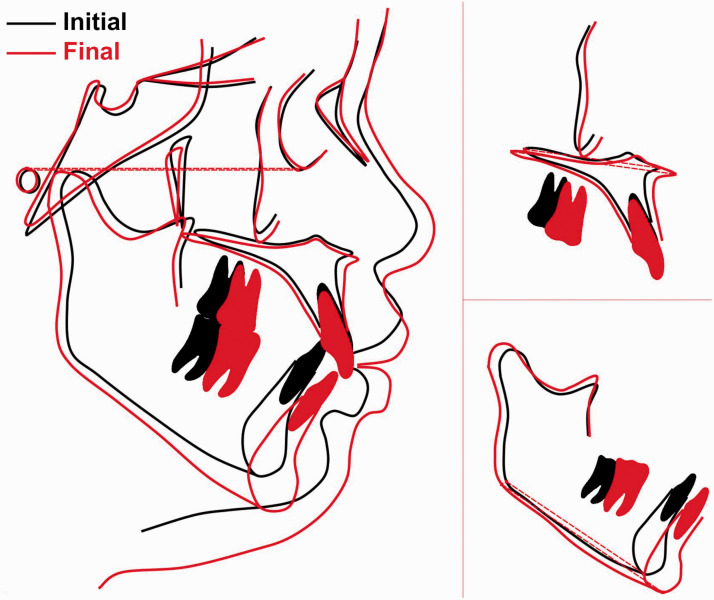
Figure 5.
Lateral cephalometric superimposition before and after the correction (black: before the correction; red: after the correction).
Discussion
Children are in the active growth and development stage; thus, their craniofacial bones, dental occlusions, and facial soft tissues are dynamically changing. Children with chronic rhinitis, adenoid hypertrophy, tonsil hypertrophy, and nasal septum deviation may develop mouth breathing because the upper airway is completely or partially obstructed, causing all or partial airflow to enter the lower airway through the mouth, oropharyngeal cavity, and laryngopharyngeal cavity rather than the nasal cavity. Mouth breathing changes the temporomandibular joint structure and periarticular muscle groups, resulting in regular mouth breathing. This causes malocclusion (often class II malocclusion) as well as changes in the maxillofacial soft and hard tissues, which in turn affects the maxillofacial appearance and development.3–6 The patient in the present case had mouth breathing and snoring habits, and examination showed soft convex tissues, a protruded maxilla, a retruded underjaw, and a class II sagittal osteofascial pattern; he was thus diagnosed with skeletal class II malocclusion caused by mouth breathing.
The available treatments for skeletal class II malocclusion caused by mouth breathing are early functional correction, camouflaged orthodontic treatment, and combined orthodontic and orthognathic treatment. Because of the growth potential in teenagers with skeletal class II diseases, the use of functional appliances can inhibit the growth of the maxilla and enhance the growth of the mandible.7,8 The patient in this case was 7 years 10 months old and at the stage of mixed dentition; thus, his dentition disorder was treated in a timely manner to lower the severity of malocclusion. We use iGo for pediatric occlusion induction to promptly intervene in oral problems in children via jaw correction, dental arch shaping, tooth alignment, and eruption induction-based occlusion development technologies from the time of primary occlusion (age of 3 years) to permanent occlusion replacement (age of 6 years) and to primary development of permanent dentition (age of 12 years). This intervention helps guide the development of physiological occlusion and realize stable occlusion and a coordinated facial appearance.
The skeletal class II malocclusion in our patient was mainly caused by changes in the maxillofacial soft and hard tissues due to long-term mouth breathing. Traditional appliances to intervene in mouth breathing are vestibular shields and lip bumpers. In this case, lip stickers were used to intervene in the patient’s habitual mouth breathing, and a fixed maxillary expander was used to improve crowding and broaden the dental arch. The width of the nasopharynx cavity subsequently increased, and the palatal vault was lowered while the median palatine suture was enlarged. This reduced the nasal ventilation resistance, and the patient gradually returned to nasal breathing. In addition, functional appliances were used to improve the malocclusion by guiding the development of physiological occlusion, which eventually realized jaw-to-jaw coordination. Common functional appliances include activators, the Twin Block, the Bionator, the Herbst appliance, the Forsus appliance, the Jasper Jumper, and muscle function trainers. 9
A muscle function trainer is a simple, convenient, and comfortable device that can effectively build oral muscle balance and adduct the upper incisor teeth. This appliance has been used to correct mouth breathing and treat skeletal class II malocclusion, and it has received widespread attention in recent years.10–12 For our patient, we used an ETA and lip closure exercises to restore and reshape the normal width of the upper and lower dental arches, improve the deep cover of the deep-overbite occlusion, and exercise the perioral muscle functions while correcting the jaw positions and abnormal tooth relationships. These measures established a balance between occlusal functions and perioral neuromuscular functions to realize respective physiological occlusion.
The success of such treatment is largely determined by the clinician’s adoption of a treatment regimen based on iGo according to the patient’s dentition, jawbone characteristics, facial soft tissue profile, and growth potential.
At the 5-year 2-month follow-up visit after the correction (when the patient was 13 years old), the patient had stable occlusion, a coordinated osteofascial pattern, and normal tooth bodies, periodontium, and temporomandibular joints.
Footnotes
Research ethics and patient consent: The study was performed in accordance with the World Medical Association Declaration of Helsinki. This study was approved by the Ethics Committee of College of Stomatology of Guangxi Medical University (approval no. 20210148). Written informed consent was obtained from the patient.
Data availability: The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Hua Huang https://orcid.org/0000-0003-0330-1995
References
- 1.Valera FC, Travitzki LV, Mattar SE, et al. Muscular, functional and orthodontic changes in pre school children with enlarged adenoids and tonsils. Int J Pediatr Otorhinolaryngol 2003; 67: 761–770. DOI: 10.1016/s0165-5876(03)00095-8. [DOI] [PubMed] [Google Scholar]
- 2.Franco LP, Souki BQ, Cheib PL, et al. Are distinct etiologies of upper airway obstruction in mouth-breathing children associated with different cephalometric patterns? Int J Pediatr Otorhinolaryngol 2015; 79: 223–228. DOI: 10.1016/j.ijporl.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Paolantonio EG, Ludovici N, Saccomanno S, et al. Association between oral habits, mouth breathing and malocclusion in Italian preschoolers. Eur J Paediatr Dent 2019; 20: 204–208. DOI: 10.23804/ejpd.2019.20.03.07. [DOI] [PubMed] [Google Scholar]
- 4.Cattoni DM, Fernandes FD, Di Francesco RC, et al. [ Characteristics of the stomatognathic system of mouth breathing children: anthroposcopic approach]. Pro Fono 2007; 19: 347–351. DOI: 10.1590/s0104-56872007000400004. [DOI] [PubMed] [Google Scholar]
- 5.Bakor SF, Enlow DH, Pontes P, et al. Craniofacial growth variations in nasal-breathing, oral-breathing, and tracheotomized children. Am J Orthod Dentofacial Orthop 2011; 140: 486–492. DOI: 10.1016/j.ajodo.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Bresolin D, Shapiro PA, Shapiro GG, et al. Mouth breathing in allergic children: its relationship to dentofacial development. Am J Orthod 1983; 83: 334–340. DOI: 10.1016/0002-9416(83)90229-4. [DOI] [PubMed] [Google Scholar]
- 7.Freitas B, Freitas H, Dos Santos PC, et al. Correction of Angle Class II division 1 malocclusion with a mandibular protraction appliances and multiloop edgewise archwire technique. Korean J Orthod 2014; 44: 268–277. DOI: 10.4041/kjod.2014.44.5.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalha AS. Early orthodontic treatment reduced incisal trauma in children with class II malocclusions. Evid Based Dent 2014; 15: 18–20. DOI: 10.1038/sj.ebd.6400986. [DOI] [PubMed] [Google Scholar]
- 9.Li X, Wang H, Li S, et al. Treatment of a Class II Division 1 malocclusion with the combination of a myofunctional trainer and fixed appliances. Am J Orthod Dentofacial Orthop 2019; 156: 545–554. DOI: 10.1016/j.ajodo.2018.04.032. [DOI] [PubMed] [Google Scholar]
- 10.Tallgren A, Christiansen RL, Ash M, Jr, et al. Effects of a myofunctional appliance on orofacial muscle activity and structures. Angle Orthod 1998; 68: 249–258. DOI: 0.1043/0003-3219(1998)068<0249:Eoamao>2.3.Co;2. [DOI] [PubMed] [Google Scholar]
- 11.Usumez S, Uysal T, Sari Z, et al. The effects of early preorthodontic trainer treatment on Class II, division 1 patients. Angle Orthod 2004; 74: 605–609. DOI: 10.1043/0003-3219(2004)074<0605:Teoept>2.0.Co;2. [DOI] [PubMed] [Google Scholar]
- 12.Uysal T, Yagci A, Kara S, et al. Influence of pre-orthodontic trainer treatment on the perioral and masticatory muscles in patients with Class II division 1 malocclusion. Eur J Orthod 2012; 34: 96–101. DOI: 10.1093/ejo/cjq169. [DOI] [PubMed] [Google Scholar]