Abstract
Background and Aims:
Pain perception and pain threshold vary from one individual to another and also differ in the right and left limbs leading to an inter-cerebral pain variability bias and inter-patient pain variability bias. To date, data comparing adductor canal block (ACB) with femoral nerve block (FNB) in the same patient who underwent bilateral total knee arthroplasty (TKA) remain limited.
Methods:
We performed a prospective, non-randomised, controlled study. Patients scheduled for bilateral TKA with central neuraxial anaesthesia received every 12-hourly intermittent boluses of 15 mL of ropivacaine 0.5% in two different peripheral nerve blocks (ACB and FNB) in either of the lower limbs postoperatively. The primary outcome was to assess postoperative VAS score, and the secondary outcomes were muscle strength of the quadriceps muscle and degree of flexion at the knee joint.
Results:
Among the 80 patients assessed for eligibility, 72 patients were enroled, and 69 were included in the final analysis. VAS scores after the two blocks during rest at 30 minutes, 6 hours, 12 hours and 48 hours post-operatively had no significant difference. VAS scores during rest at 24 hours and on doing exercise at 24 hours and 48 hours showed a significant difference. Quadriceps muscle strength and degree of flexion of knee at 24 hours and 48 hours post-operatively did show a significant difference in favour of the ACB over FNB.
Conclusion:
ACB provides equivalent analgesia in comparison with FNB at rest and during passive exercise up to 48 hours post-operatively. ACB significantly preserved motor power of quadriceps muscles when compared with FNB with no added complications.
Keywords: Acute pain management, adductor canal block, femoral nerve block, ropivacaine
INTRODUCTION
Total knee arthroplasty (TKA) is the treatment modality for osteoarthritis of knee, but it is associated with painful and prolonged post-operative recovery due to extensive tissue injury and bone destruction. Multimodal analgesic regimens, including systemic analgesics, local anaesthetic infiltration and peripheral nerve blocks (PNBs) provide effective pain relief after knee arthroplasty.[1,2]
Femoral nerve blocks (FNBs), were used successfully, but they had their own merits and demerits. FNB causes motor involvement in addition to the desired sensory blockade causing quadriceps muscle weakness and hence delayed mobilisation and increased incidence of falls in the post-operative period.[3] Adductor canal block (ACB) is a technique where sensory innervation of the knee (saphenous nerve, articular branch from vastus medialis and obturator nerve) are blocked and efferent branches to the quadriceps muscle are spared thereby preserving its motor strength.[2]
Few studies have compared ACB and FNB in patients undergoing bilateral TKA. Because pain perception and pain threshold vary from one individual to another, for instance, with gender and age, a significant inter-patient pain variability bias exists, and pain sensitivity also differs in the two cerebral hemispheres leading to an inter-cerebral pain variability bias.[4,5,6] To overcome this bias, we compared both these nerve blocks in the same individual undergoing the same surgical procedure in both the lower limbs. Till date, studies comparing effect of ACB and FNB in the same patient undergoing bilateral TKA are scarce.
With this background, in our study we planned to administer both ACB and FNB to all the patients undergoing bilateral TKA. We hypothesised that ACB would provide analgesia equivalent to FNB with preserved motor power of quadriceps muscles.
METHODS
After institutional ethical committee approval (AIIMS/IEC/18/88), and written informed consent, all patients of either gender classified as per American Society of Anesthesiologists (ASA) physical status classification as Classes I–III, aged >45 years, undergoing primary bilateral TKA under neuraxial anaesthesia were enroled in this non-randomised study (Clinical Trials Registry, India CTRI/2018/05/013680) from May 2018 to August 2019. Those with known allergy to the study drug, cognitive impairments and inability to understand the study protocol, intake of pain medications (use of opioids for >3 months in the past 1 year), any sensory motor deficit, coagulopathy, cognitive dysfunction and refusal to consent were excluded.
During the pre-operative visit, we detailed the study protocol and Visual Analogue Scale (VAS) scoring to all included patients. VAS is a 10-point objective score, where “0” indicates “no pain at all,” whereas “10” denotes “maximal possible pain.”[7] These patients underwent bilateral total knee arthroplasty under combined spinal–epidural anaesthesia (0.5% bupivacaine heavy, 2.5 mL intrathecally). Epidural top-up of bupivacaine 0.25% (5 mL) was administered for any intraoperative patient discomfort, at the discretion of the supervising anaesthetist. The surgical procedure was performed by the same surgeon throughout the study. After that, the patient was shifted to the post-anaesthesia care unit. Once a VAS score of 6/10 was reached, the peripheral nerve blocks including ACB and FNB were administered under aseptic precautions to the same patient on separate lower limbs, using the USG (ultrasonography)-guided in-plane technique (6–13 MHz linear probe, GE Healthcare Systems, Phoenix, US). The choice of left or right lower limb for performing ACB and FNB blocks alternated with each consecutive patient.
For FNB with perineural catheter insertion, the USG probe was inclined perpendicular to the femoral artery and in-line to the inguinal ligament. After that, an 18G Tuohy needle (10 cm in length) was inserted along the lateral border of the USG probe. With the needle tip positioned under the fascia iliaca around 1 cm lateral to the femoral nerve, 5 mL of saline was injected to facilitate further procedure. An epidural catheter (20G, triple orifice, Contiplex® Tuohy, B. Braun, Germany) was then threaded 5 cm beyond the needle tip. Thereafter, under real-time ultrasound view of saline spread, the catheter was slightly withdrawn, to ensure its proximity close to the femoral nerve. Then, the needle was withdrawn and a catheter was secured in place via transparent dressing.
For ACB with perineural catheter insertion, the USG probe was placed at the junction of middle and lower one third thigh level, the femur was identified, and the probe was moved medially until the boat-shaped sartorius muscle was visualised. The femoral artery and vein were identified beneath the sartorius muscle. The adductor canal was identified through the characteristic double contour of vaso adductor membrane. After that, an 18G Tuohy needle (10 cm in length) was inserted along the lateral border of the USG probe in a postero-lateral direction. With the needle tip positioned medial to the femoral artery in adductor canal, 5 mL of saline was injected to facilitate further procedure. An epidural catheter (20G, triple orifice, Contiplex® Tuohy, B. Braun, Germany) was then threaded 5 cm beyond the needle tip. Thereafter, under real-time ultrasound view of saline spread, the catheter was slightly withdrawn to ensure its proximity to the saphenous nerve. Then, the needle was withdrawn, and the catheter was secured in place via transparent dressing.[8]
Afterwards, 0.5% ropivacaine (15 mL) was injected every 12th hourly, through the FNB and ACB catheters for the next 48 hours. All PNB procedures were performed by the same anaesthesiologist. An independent nursing officer monitored the patients and collected the outcome data. The systemic analgesics, including paracetamol (15 mg/kg intravenous (IV), 6th hourly) and diclofenac (1 mg/kg IV, 8th hourly) were administered as a routine. Injection tramadol 50 mg IV was administered as a rescue analgesic for a VAS score >6, if desired. The epidural catheter was removed when the VAS score improved from 6/10 to 3/10 in both the limbs under the effect of PNB. In the event of block failure, epidural top-ups were given, and these patients were excluded from primary analysis. The patients were also monitored post-operatively for any untoward event.
The primary outcome included post-operative VAS score measured (at rest) at 30 minutes, 6 hours, 12 hours, 24 hours and 48 hours, and during exercise at 24 hours and 48 hours, after performing PNBs. The secondary outcome included quadriceps muscle strength and degree of knee flexion assessed at 24 hours and 48 hours, after performing PNBs. The quadriceps muscle strength (kilogram force) was measured in both legs, with the patient in supine position, knees flexed on a rolled pillow at 40°, bed angle between at 25° and knee extension against the Lafayette dynamometer placed over the base of the tibia, using Lafayette Manual Muscle Test System (Lafayette Instrument Company, Lafayette, Indiana, USA).[9] The degree of knee flexion was measured in both legs, with the patient in supine position. The limb support was attached to the table end (80°–90° bend), and kept in the popliteal fossa to provide support to the knee and maintain an angle for measuring the degree of knee flexion using goniometer. The position of the ankle was not fixed to reduce patient discomfort.
The sample size was calculated using G power software Version 3.1 (Germany). Using the two-sided hypothesis test, at an alpha error of 0.05, power of 80%, effect size of 0.53, allocation ratio of 1 and 10% drop-outs, we required 65 samples in each PNB. The effect size was based on the results of a previous study (mean ACB 4 ± 2.2; mean FNB 3 ± 1.48) for pain scores during activity at 48 hours.[10] The statistical analysis was performed using Statistical Package for Social Sciences statistical software, Version 21 (IBM, Armonk, NY, US). The data were presented as descriptive analysis. The primary and secondary outcomes were compared using the Wilcoxon signed-rank test. A P value <0.05 was considered significant.
RESULTS
Among the 80 patients assessed for eligibility, 72 (144 knees) were enrolled and 69 were included in the final analysis. Three were excluded: due to FNB failure in one patient and the catheter dislodgement from FNB site in the other two patients [Figure 1]. The mean age of the patients was 64 ± 8.4 years, mean weight was 75 ± 7.5 kg, and mean height was 162.9 ± 8.5 cm. Thirty-six male and 33 female patients were enrolled in which 49 (71%) patients were of ASA Class II.
Figure 1.
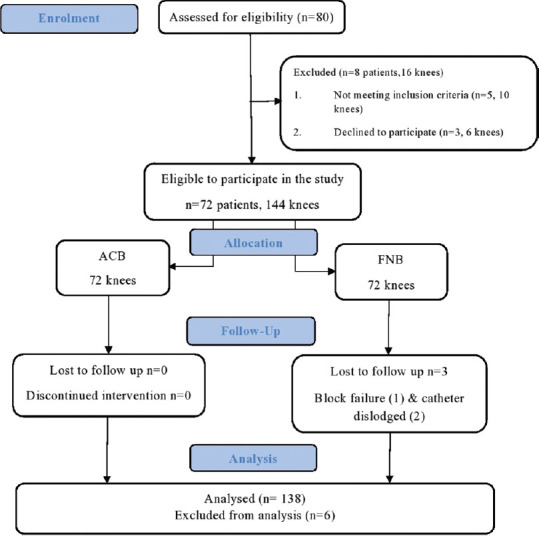
Flow chart depicting patient flow in the study
After administering the block, the VAS scores decreased significantly in both the blocks. The mean VAS scores in ACB were lower than in the FNB at most of the time points during both during rest and exercise. On intergroup comparison, the VAS scores at rest did not vary significantly between the blocks for most of the time points: at 0 minutes (ACB 7.6 ± 0.8; FNB 7.8 ± 0.8; P = 0.07), at 30 minutes (ACB 3.3 ± 0.7; FNB 3.4 ± 0.9; P = 0.32), at 6 hours (ACB 2.9 ± 0.6; FNB 3.1 ± 0.7; P = 0.19), at 12 hours (ACB 3.1 ± 0.6; FNB 3.2 ± 0.8; P = 0.10) and at 48 hours (ACB 3.3 ± 0.5; FNB 3.4 ± 0.6; P = 0.12). These values, however, attained statistical significance at 24 hours after initiating the block (ACB 3.2 ± 0.6; FNB 3.4 ± 0.6; P = 0.02). The VAS score while performing exercise was significantly higher in FNB compared with ACB: at 24 hours (ACB 3.8 ± 0.5; FNB 4.1 ± 0.5; P = 0.01) and at 48 hours (ACB 3.8 ± 0.5; FNB 4.3 ± 0.6; P < 0.001) after initiating the block, respectively.
The mean muscle strength values for ACB were significantly higher than that of FNB at 24 hours (ACB 2.2 ± 0.5; FNB 1.8 ± 0.4; P < 0.001) and at 48 hours (ACB 2.6 ± 0.5; FNB 2.3 ± 0.4; P < 0.001), respectively. The degree of knee flexion was significantly higher at 24 hours (ACB 85.4 ± 6.5; FNB 83.1 ± 6.6; P = 0.04) and 48 hours (ACB 105.5 ± 8.4; FNB 102.0 ± 8.0; P = 0.04) in ACB, compared with FNB [Table 1].
Table 1.
Comparison of primary and secondary outcomes of study population by Wilcoxon signed-rank test
| Outcome | Timeline | ACB | FNB | P |
|---|---|---|---|---|
| VAS score at | 0 min | 7.6±0.8 | 7.8±0.8 | 0.07 |
| rest | 30 min | 3.3±0.7 | 3.4±0.9 | 0.32 |
| 6 h | 2.9±0.6 | 3.1±0.7 | 0.19 | |
| 12 h | 3.1±0.6 | 3.2±0.8 | 0.10 | |
| 24 h | 3.2±0.6 | 3.4±0.6 | 0.02 | |
| 48 h | 3.3±0.5 | 3.4±0.6 | 0.12 | |
| VAS score | 24 h | 3.8±0.5 | 4.1±0.5 | 0.01 |
| during exercise | 48 h | 3.8±0.5 | 4.3±0.6 | <0.001 |
| Muscle strength | Baseline | 2.81±0.5 | 2.82±0.5 | 0.96 |
| (kgF) | 24 h | 2.2±0.5 | 1.8±0.4 | <0.001 |
| 48 h | 2.6±0.5 | 2.3±0.4 | <0.001 | |
| Degree of knee | 24 h | 85.4±6.5 | 83.1±6.6 | 0.04 |
| flexion (degrees) | 48 h | 105.51±8.4 | 102.0±8.0 | 0.04 |
Values are depicted as mean±SD; VAS=Visual Analogue Scale; time is taken from administration of block; kgF=kilogram force; P<0.05 is considered as statistically significant
There was no incidence of fall of patient up to 48 hours during recovery, and no significant catheter-related complication such as haematoma or displacement was found in either block.
DISCUSSION
The main findings of this study were that the VAS scores (primary outcome) in the two blocks at rest at different time points up to 48 hours post-operatively had no significant difference. VAS scores on passive exercise at 24 hours and 48 hours did show a significant statistical difference. Secondary outcomes, namely, quadriceps muscle strength and degree of knee flexion, were significantly better in ACB.
Not all patients showed a clinically significant difference in post-operative analgesia both at rest and during exercise which correlated with the findings of Elkassabany et al.[11] According to their study, pain scores, post-operative analgesic requirements and quality of recovery were similar between the two blocks. However, our findings were not consistent with the results of Memtsoudis et al. study,[9] which reported better qualitative pain relief in FNB compared with ACB 24 hours after TKA.
One reason for the differences in analgesic properties between the two blocks (ACB and FNB) could be that because FNB provided sensory block of the saphenous nerve, the nerve to vastus medialis and the medial femoral cutaneous nerve, it provided analgesia to the medial and anterior knee. ACB involves the nerve to vastus medialis and extra muscular sensory branch supply to the knee joint, medial femoral cutaneous nerve, articular branches from the obturator nerve, the medial retinacular nerve and saphenous nerve that innervate the medial, lateral and anterior aspects of the knee. In our study also, the mean VAS scores remained lower in ACB compared with FNB at all time intervals both at rest and during movement. Greater analgesic benefits of ACB can be attributed to the sensory block of the posterior branches of the obturator nerve.[12] Placement of tip of the perineural catheter distally in ACB spread local anaesthetic into the popliteal fossa causing anaesthesia of the posterior branch of the obturator nerve and the popliteal plexus, providing better analgesia compared with FNB.[13]
Each of the participants in the study was administered FNB on one lower limb and ACB on the other to reduce the bias due to inter-patient and inter-cerebral pain variability. Koh et al.[14] compared ACB and FNB in the same patient undergoing bilateral TKA comparing analgesic efficacy and quadriceps muscles strength up to 48 hours. Their results demonstrated that the patient's analgesic level remains the same between the knees that underwent either ACB or FNB. They also found statistical differences in terms of better quadriceps muscle strength recovery in the knee receiving ACB during the first 48 hours.
Quadriceps muscle strength assessed for knee extension post-operatively reflected that ACB showed statistically significant differences in sparing muscle power of quadriceps compared with FNB, correlating with previous studies.[11,12,14] This is due to the blockade of nerve to vastus medialis and its intramuscular and extra muscular sensory branch supplying the knee joint in the distal part of the adductor canal. ACB resulted in partial motor weakness of the vastus medialis only, sparing the motor function of the other three quadriceps components (rectus femoris, vastus lateralis and vastus intermedius) because their motor nerves do not traverse the adductor canal, whereas in FNB, nerve supply to all four muscles of femur is blocked.[13,15]
There are a few studies that found no significant differences in muscle strength between ACB and FNB, indicating that either pain or peri-surgical factors such as the use of tourniquet might be the reason for the outcome rather than the block per se. Jaeger et al.[15] did not find any difference in the quadriceps muscle strength between the two groups at 24 hours after TKA. They performed USG-guided ACB at the mid-thigh level and postulated that the large volumes applied (bolus and infusion) might have increased the risk of motor blockade. If the catheter is placed at the mid-thigh level, chances of the drug spreading into the apex of femoral triangle are more resulting in increased chances of quadriceps muscle weakness. In our study, we placed the catheter at the junction of middle one third and lower one third of the thigh after visualisation of vasoadductor membrane by USG, thus ruling out this possible bias.
In our study, the degree of knee flexion assessed with the help of goniometer at 24 hours and 48 hours post-operatively showed statistically significant differences between ACB and FNB, which correlated with the previous study done by Grevstad et al.[16] The leg receiving ACB showed better degrees of knee flexion compared with FNB; this may be due to the better analgesic effects of ACB at 24 hours and 48 hours on doing physical exercise and sparing of tibial nerve.
There was no incidence of patient fall due to weakness in any of the limbs, especially in the group receiving FNB.[17] In our study, no complications related to catheter placement such as catheter site infection, nerve injury, haematoma formation and displacements were seen while performing either of the PNBs (ACB and FNB).
There are certain possible limitations of our study. As we had given two different blocks in two limbs of a single patient, we were unable to accurately assess ambulation ability, gait trait and incidence of fall. Secondly, we did not monitor the catheter tip migration or drug migration in the adductor canal after its initial placement or drug administration. Lastly, the length of hospital stay could not be monitored because of logistic issues. Also, because all the participants of our study were admitted on the first outpatient department visit, no pre-operative rehabilitation for quadriceps muscle strengthening was done.[18]
CONCLUSION
Both FNB and ACB are equivalent only in providing post-operative analgesia in knee arthroplasty. ACB is superior to FNB with respect to the preservation of quadriceps muscle strength with no added complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Dr Suresh Sharma, College of Nursing, AIIMS Rishikesh; Dr Mridul Dhar, Department of Anaesthesia, AIIMS Rishikesh; Dr Namrata Gupta, Department of Anaesthesia, AIIMS Rishikesh; Arghya Kundu Choudhury, Department of Orthopaedics, AIIMS Rishikesh; and Dr Yogesh AB; Department of Community Medicine AIIMS Rishikesh.
REFERENCES
- 1.Mehdiratta L, Bajwa SJ, Malhotra N, Joshi M. Exploring cocktails, remixes and innovations in regional nerve blocks: The clinical research journey continues. Indian J Anaesth. 2020;64:1003–6. doi: 10.4103/ija.IJA_1517_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goyal R, Mittal G, Yadav AK, Sethi R, Chattopadhyay A. Adductor canal block for post-operative analgesia after simultaneous bilateral total knee replacement: A randomised controlled trial to study the effect of addition of dexmedetomidine to ropivacaine. Indian J Anaesth. 2017;61:903–9. doi: 10.4103/ija.IJA_277_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim DH, Lin Y, Goytizolo EA, Kahn RL, Maalouf DB, Manohar A, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: A prospective, randomized, controlled trial. Anesthesiology. 2014;120:540–50. doi: 10.1097/ALN.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 4.Bajwa SJ. Managing acute post-operative pain: Advances, challenges and constraints. Indian J Anaesth. 2017;61:189–91. doi: 10.4103/ija.IJA_110_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cole LJ, Farrell MJ, Gibson SJ, Egan GF. Age-related differences in pain sensitivity and regional brain activity evoked by noxious pressure. Neurobiol Aging. 2010;31:494–503. doi: 10.1016/j.neurobiolaging.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Ji G, Neugebauer V. Hemispheric lateralization of pain processing by amygdala neurons. J Neurophysiol. 2009;102:2253–64. doi: 10.1152/jn.00166.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15((Suppl 1)):S17–24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong WY, Bjørn S, Maria J, Strid C, Børglum J, Bendtsen TF. Defining the location of the adductor canal using ultrasound. Reg Anesth Pain Med. 2017;42:241–45. doi: 10.1097/AAP.0000000000000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Memtsoudis SG, Yoo D, Stundner O, Danninger T, Ma Y, Poultsides L, et al. Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop. 2015;39:673–80. doi: 10.1007/s00264-014-2527-3. [DOI] [PubMed] [Google Scholar]
- 10.Wiesmann T, Piechowiak K, Duderstadt S, Haupt D, Schmitt J, Eschbach D, et al. Continuous adductor canal block versus continuous femoral nerve block after total knee arthroplasty for mobilisation capability and pain treatment: A randomised and blinded clinical trial. Arch Orthop Trauma Surg. 2016;136:397–406. doi: 10.1007/s00402-015-2403-7. [DOI] [PubMed] [Google Scholar]
- 11.Elkassabany NM, Antosh S, Ahmed M, Nelson C, Israelite C, Badiola I, et al. The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block: A double-blinded randomized controlled study. Anesth Analg. 2016;122:1696–703. doi: 10.1213/ANE.0000000000001237. [DOI] [PubMed] [Google Scholar]
- 12.Gautier PE, Hadzic A, Lecoq J-P, Brichant JF, Kuroda MM, Vandepitte C. Distribution of injectate and sensory-motor blockade after adductor canal block. Anesth Analg. 2016;122:279–82. doi: 10.1213/ANE.0000000000001025. [DOI] [PubMed] [Google Scholar]
- 13.Thiayagarajan M, Kumar S, Venkatesh S. An exact localization of adductor canal and its clinical significance: A cadaveric study. Anesth Essays Res. 2019;13:284. doi: 10.4103/aer.AER_35_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh HJ, Koh IJ, Kim MS, Choi KY, Jo HU, In Y. Does patient perception differ following adductor canal block and femoral nerve block in total knee arthroplasty.A simultaneous bilateral randomized study? J Arthroplasty. 2017;32:1856–61. doi: 10.1016/j.arth.2017.01.025. [DOI] [PubMed] [Google Scholar]
- 15.Jaeger P, Koscielniak-Nielsen ZJ, Hilsted KL, Fabritius ML, Dahl JB. Adductor canal block with 10 ml versus 30 ml local anesthetics and quadriceps strength: A paired, blinded, randomized study in healthy volunteers. Reg Anesth Pain Med. 2015;40:553–8. doi: 10.1097/AAP.0000000000000298. [DOI] [PubMed] [Google Scholar]
- 16.Grevstad U, Mathiesen O, Lind T, Dahl JB. Effect of adductor canal block on pain in patients with severe pain after total knee arthroplasty: A randomized study with individual patient analysis. Br J Anaesth. 2014;112:912–9. doi: 10.1093/bja/aet441. [DOI] [PubMed] [Google Scholar]
- 17.Wahal C, Kumar A, Pyati S. Advances in regional anaesthesia: A review of current practice, newer techniques and outcomes. Indian J Anaesth. 2018;62:94–102. doi: 10.4103/ija.IJA_433_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jahic D, Omerovic D, Tanovic A, Dzankovic F, Campara M. The effect of prehabilitation on postoperative outcome in patients following primary total knee arthroplasty. Med Arch. 2018;72:439. doi: 10.5455/medarh.2018.72.439-443. [DOI] [PMC free article] [PubMed] [Google Scholar]


