Abstract
Context:
Chronic heat exposure promotes cardiovascular and cellular adaptations, improving an organism's ability to tolerate subsequent stressors. Heat exposure may also promote neural adaptations and alter the neural–hormonal stress response. Hot-temperature yoga (HY) combines mind–body exercise with heat exposure. The added heat component in HY may induce cardiovascular and cellular changes, along with neural benefits and modulation of stress hormones.
Aims:
The purpose of the present study is to compare the cardiovascular, cellular heat shock protein 70 (HSP70), neural, and hormonal adaptations of HY versus normal-temperature yoga (NY).
Settings and Design:
Twenty-two subjects (males = 11 and females = 11, 26 ± 6 years) completed 4 weeks of NY (n = 11) or HY (n = 11, 41°C, 40% humidity). Yoga sessions were performed 3 times/week following a modified Bikram protocol.
Subjects and Methods:
Pre- and posttesting included (1) hemodynamic measures during a heat tolerance test and maximal aerobic fitness test; (2) neural and hormonal adaptations using serum brain-derived neurotrophic factor (BDNF) and adrenocorticotropic hormone (ACTH), along with a mental stress questionnaire; and (3) cellular adaptations (HSP70) in peripheral blood mononuclear cells (PBMCs).
Statistical Analysis:
Within- and between-group Student's t-test analyses were conducted to compare pre- and post-VO2 max, perceived stress, BDNF, HSP70, and ACTH in HY and NY groups.
Results:
Maximal aerobic fitness increased in the HY group only. No evidence of heat acclimation or change in mental stress was observed. Serum BDNF significantly increased in yoga groups combined. Analysis of HSP70 suggested higher expression of HSP70 in the HY group only.
Conclusions:
Twelve sessions of HY promoted cardiovascular fitness and cellular thermotolerance adaptations. Serum BDNF increased in response to yoga (NY + HY) and appeared to not be temperature dependent.
Keywords: Brain-derived neurotrophic factor, heat acclimation, heat shock protein, hot yoga, yoga
Introduction
Yoga is defined as the combination of breathing exercises, meditation, and physical postures used to achieve a state of relaxation and balance of the mind, body, and spirit.[1] In the United States, yoga practice has become increasingly popular with 14.3% of adults using yoga as a form of complementary medicine.[1] The popularity of yoga is mirrored by a steady increase in the number of academic studies investigating the therapeutic impact of yoga.[2] Evidence suggests that yoga may provide health-related benefits for a wide variety of disease states including, but not limited to, depression,[3] schizophrenia,[4] type 2 diabetes mellitus,[5] and cancer-related fatigue.[6] Researchers have recently begun to explore the physiological mechanisms responsible for the physical and mental benefits obtained through yoga practice.[7]
One proposed mechanism that may partially explain the therapeutic benefits of yoga is through regulatory effects on the hypothalamic–pituitary–adrenal (HPA) axis, which is a core component for the maintenance of the stress response.[8] Upon exposure to physical (e.g., vigorous exercise) or mental (e.g., anxiety) stressors, the HPA axis activates neurons in the paraventricular nucleus, leading to downstream release of corticotrophin and vasopressin into portal circulation and further production of adrenocorticotropic hormone (ACTH). The synthesis and release of cortisol from the adrenal cortex is initiated by ACTH, promotes mobilization of stored energy, suppresses immune function,[9] and has mood altering effects.[10] Dysregulation of the HPA axis has been linked to numerous diseases including depression,[11] anxiety,[12] and schizophrenia.[13] Yoga has been shown to improve the regulatory control of the HPA axis among both healthy adults and those suffering from various disorders.[8,14]
A second mechanism that may explain beneficial impact of yoga is the increased expression of brain-derived neurotrophic factor (BDNF) following yoga therapy.[15] BDNF is a neuroregulatory protein that promotes neurogenesis, synaptic plasticity, and neuronal survival.[16] Decreased levels of BDNF have been observed in a number of neurodegenerative diseases[17] and mood disorders.[18] Evidence suggests that yoga practice promotes BDNF expression and this response may explain the therapeutic benefits (e.g., mood improvement and cognitive function) of yoga among individuals with neural disorders.[19]
While numerous styles of yoga exist, the most common form in academic literature is Hatha Yoga.[20] Hatha Yoga emphasizes physical postures, breathing techniques, and meditation. Hot-temperature yoga (HY) is another form which has been gaining popularity in the United States but is less commonly studied. Hot yoga combines the techniques used in Hatha Yoga with environmental heat stress. The addition of heat stress increases the cardiovascular demand during yoga which may augment yoga-induced adaptations.[21] Further, chronic exposure to environmental heat may promote increased tolerance to heat and cellular stress response adaptations.[22] This includes upregulation of key stress response proteins such as heat shock protein 70 (HSP70), which protects cells from a variety of insults (physical, bacterial, chemical, and environmental). In addition, heat intolerance is associated with HPA axis impairment,[23] and repetitive bouts of aerobic exercise in the heat have been shown to modulate both ACTH and cortisol levels among humans.[24] Further, heat exposure through hot water immersion has been shown to increase serum BDNF levels in healthy adult men.[25]
Based on these observations, several important questions are raised in regard to the benefits (and mechanisms) of adding a heat component to yoga practice. First, does participation in a hot yoga training program (3 times per week) cause cardiovascular adaptations and lead to thermoregulatory improvements? Second, does the heat exposure during hot yoga cause upregulation of key markers of cellular stress? Third, does hot yoga improve both HPA axis function and increase expression of BDNF beyond what has been reported in response to normal-temperature yoga (NY)? Given the limited research on the impact of hot yoga, the purpose of the present study is to compare the cardiovascular, cellular, and neural adaptations of normal-temperature and HY.
Subjects and Methods
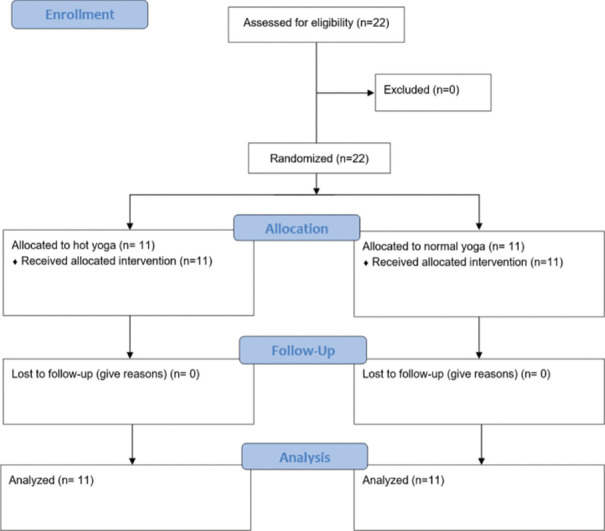
The present study was approved by the Institutional Review Board of the University of New Mexico. All data collection was in accordance with the ethical standards of the Helsinki Declaration. Twenty-two individuals (men: n = 11 and women: n = 11) aged 19–39 years were recruited in the study. All participants completed a health history questionnaire and written informed consent was obtained. Exclusion criteria included prior yoga experience; known cardiovascular, metabolic, viral, kidney, or liver disease; history of heat illness (e.g., heatstroke, heat exhaustion, heat cramps, and heat rash); or currently taking an antidepressant. Among 22 participants, no individuals were excluded from the study or lost to follow-up [Figure 1]. Participants were randomized, using block randomization, into either the HY group (n = 11) or the NY group (n = 11). All testing was performed in the Exercise Physiology Lab at the University of New Mexico. Data collection occurred from October to May to avoid environmental heat acclimatization [Figure 1].
Figure 1.
Flow chart of the study according to CONSORT statement
Protocol
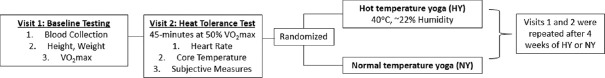
An outline of the experimental design is shown in Figure 2. Before the yoga intervention, subjects visited the lab on two occasions. At the first visit, baseline measures (aerobic capacity, body composition, and 20 ml venous blood draw) were obtained. At least 48 h following the first visit, subjects arrived to the lab to complete a written perceived stress scale (PSS)[26] and a heat tolerance test (HTT). After the first two visits, subjects completed three yoga sessions per week for 4 weeks (12 sessions total). Yoga sessions were scheduled between the hours of 5:00 am and 8:00 pm and efforts were made to keep the time consistent across all sessions. The baseline and postintervention data collection visits were scheduled between 5:00 am and 8:00 pm, with the visit time remaining consistent between the visits for each subject [Figure 2].
Figure 2.
Study protocol N = 22. VO2 max = Maximal aerobic fitness, HY = hot-temperature yoga, NY = normal-temperature yoga
Baseline measurements and aerobic fitness measurement
Subjects visited the lab on two occasions before beginning the yoga intervention. Subjects were asked to arrive after an overnight fast for the first baseline visit. Upon 10 min of seated rest, a 20 ml venous blood sample was collected from the antecubital vein. Peripheral blood mononuclear cells (PBMCs), plasma, and serum were collected from the whole blood sample for further analysis. Subject's height to the nearest centimeter (cm) and weight to the nearest 0.1 kilogram (kg) were recorded using a Harpenden stadiometer (Holtain Ltd., Crymych, U. K.) and an electronic scale (Detecto, model 6127/6126, Webb City, MO), respectively. Body density was estimated using 3-site skinfolds (Lange, Beta Technology Inc, Cambridge, MD, USA) and used to determine body fat percentage using the appropriate Jackson and Pollock equation for men and women.[27,28]
Subjects then performed a maximal exercise test on a motorized treadmill (Precor, C966, Woodinville, WA) to determine aerobic fitness by measuring maximal oxygen consumption (VO2 max). During the test, gases were sampled and continuously monitored breath-by-breath using a metabolic cart (Parvomedics, TrueOne 2400, Sandy, Utah). Treadmill speed and grade were increased every minute until participant reached volitional fatigue. Heart rate was continuously monitored during exercise by a Polar heart rate monitor (Polar Electro, model FS1, Lake Success, NY). The VO2 max value was recorded as the highest value using an 11-breath running average.
Heat tolerance test
Each subject performed a HTT at least 48 h after the baseline visit. Subjects were asked to arrive at least 2 h postprandial. Upon arrival, a small urine sample was collected to measure urine-specific gravity (USG) with a clinical refractometer (model A300; ATAGO Co, Tokyo, Japan) to assess hydration status. If USG was >1.025, subjects consumed 500 ml of water and USG was reassessed 30 min later. If USG was still >1.025, the visit was rescheduled. Once adequate hydration was confirmed, subjects recorded nude body weight and completed the PSS questionnaire.[26] Baseline heart rate, VO2, rating of perceived exertion (RPE),[29] and thermal sensation[30] were recorded. Subjects then entered an environmental chamber (42°C, 40% humidity) and walked at 50% of their previously recorded VO2 max for 45 min.[31] Heart rate, core temperature (temperature of internal organs), RPE, and thermal sensation were recorded every 5 min. VO2 was recorded every 10 min to evaluate exercise intensity. Subjects were allowed to drink water ad libitum and the amount of water consumed was recorded after the test. The test was terminated if subjects reached a core temperature of 40°C. Upon completion, subjects recorded a second nude body weight to determine the amount of body water lost during the HTT.
Yoga training
Subjects were randomized into the HY (37°C–40°C) or NY (18°C–22°C) group. Subjects completed 3 sessions of yoga per week for 4 weeks (12 total sessions). Each yoga session took place in an environmental heat chamber and followed a 75-min standardized yoga video. The yoga consisted of 24 specific bodily postures held for varying time combined with breathing and meditation [Appendix 1]. Specific poses included (1) standing deep breathing pose (Pranayama); (2) half-moon pose (Ardha Chandrasana); (3) awkward pose (Utkatasana); (4) sun salutations (Surya Namaskar); (5) eagle pose (Garurasana); (6) standing head-to-knee pose (Dandayamana–Janushirasana); (7) balancing stick pose (Tuladandasana); (8) standing bow pose (Dandayamana–Dhanurasana); (9) standing separate-leg stretch pose (Dandayamana–Bibhaktapada–Paschimotthanasana); (10) triangle pose (Trikanasana); (11) standing separate-leg head-to-knee pose (Dandayamana–Bibhaktapada–Janushirasana); (12) tree pose (Vrksasana); (13) corpse pose (Savasana); (14) wind-removing pose (Pavanamuktasana); (15) seated forward bend pose (Paschimottanasana); (16) cobra pose (Bhujangasana); (17) locust pose (Ardha Shalabhasana); (18) full locust pose (Salabhasana); (19) floor bow pose (Dhanurasana); (20) camel pose (Ustrasana); (21) childs pose (Balasana); (22) head-to-knee pose (Janu Sirsasana); (23) spine twist pose (Parivrtta Sukhasana); and (24) blowing in firm pose (Kapalbhati Pranayam). The first two yoga visits were performed with a yoga instructor to ensure that subjects were performing each yoga pose correctly, and all subsequent sessions were supervised by yoga instructors and research staff. Hydration status using USG was assessed before session 1 and 12. In addition, core temperature and heart rate were measured immediately after yoga sessions 1 and 12.
Post measures
After completion of 4-week yoga intervention, participants visited the lab on two additional occasions. The first (visit 1) included a second HTT, following the exact protocol used for the baseline HTT. The second session occurred at least 72 h later and included a blood draw (20 mL sample from the antecubital vein) and maximal aerobic fitness test, following the same protocol as the subject's baseline test.
Perceived stress scale
Perceived stress was measured using the 10-item PSS.[26] Participants were asked how often they felt or thought a certain way in the past month, using a visual analog scale (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often). Positively worded questions were reverse coded and all values were summed (high score = high perceived stress) with possible scores ranging from 0 to 40. Scores ranging from 0 to 13 were considered low stress, 14–26 were considered moderate stress, and 27–40 were considered high stress.[32]
Blood measurements
Adrenocorticotropic hormone
A portion of the blood sample (10 mL) was collected in Vacutainer tubes containing ethylenediaminetetraacetic acid (BD Biosciences, Franklin Lakes, NJ, USA). Whole blood was added to Histopaque (Sigma-Aldrich 1077, St. Louis, MO) in a 1:1 ratio and centrifuged (968 g, 25 min, 20°C). Plasma was pipetted into sterile microtubes and stored at -80°C until analysis of plasma ACTH. The concentration of ACTH in plasma was determined via an enzyme-linked immunosorbent assay (ELISA) with a detection range of 0.5–165 pg/mL (ENZ-KIT138, Enzo Life Sciences, Inc., East Farmingdale, New York). Undiluted samples were loaded onto a precoated 96-well microplate. All reagents were added and washed according to the manufacturer's instructions.
Brain-derived neurotrophic factor
A portion of the blood sample (10 mL) was collected in serum tubes (BD Biosciences, Franklin Lakes, NJ, USA) and centrifuged (968 g, 30 min, 4°C). The serum portion of the whole blood was transferred to sterile microtubes and stored at − 80°C until analysis of serum BDNF. Concentration was measured using an ELISA with a detection range of 15.6–1000 pg/mL (RandD Systems, Minneapolis, MN, USA). A 50-fold sample dilution was used and all manufacturer's directions were followed.
Heat shock protein 70
Following the previously described centrifugation of Histopaque and whole blood, the buffy coat containing the PBMCs was pipetted into a conical tube containing 10-mL of phosphate-buffered saline (Sigma-Aldrich 4417, St. Louis, MO). The mixture was centrifuged (968 g, 10 min, 20°C). The supernatant was disposed of and the pellet was stored at -80°C until analysis. HSP70 concentration in PBMCs was measured via ELISA with a detection range of 0.78–50 ng/mL (C92F3A-5, Enzo Life Sciences, Inc., East Farmingdale, New York). The pellet was resuspended in 1x extraction reagent, centrifuged (×21,000g, 10 min, 4°C), and the supernatant (cell lysate) was transferred to sterile microtubes, following the manufacturer's instructions. A 4-fold dilution was used and the samples were loaded onto a precoated 96-well microplate. All reagents were added and washed according to the manufacturer's instructions.
Statistical analysis
All data were presented as mean ± standard deviation unless otherwise specified. Sample size was determined based on a priori calculation with power of 0.80 and alpha level of 0.05 (G * power, Dusseldorf, Germany). The criterion for the selected studies was 4–8-week yoga interventions and changes in plasma BDNF levels. A power of 0.80 and alpha of 0.05 was used to calculate expected sample size for BDNF. The expected effect size for BDNF was 1.72, which estimates a minimum of 7 subjects per group. Within- and between-group Student's t-test analyses were conducted to compare pre- and post-VO2 max, perceived stress, BDNF, HSP70, and ACTH in the hot-temperature and normal-temperature groups. The change in core temperature (∆Tc) was evaluated by subtracting pre-HTT core temperature (resting core temperature) from post-HTT peak core temperature at both pre- and postyoga time points. The ∆ Tc during each HTT was evaluated within both the HY and NY groups using a paired t-test. The average ∆ Tc within each trial (HY and NY) was used to compare between group core temperature changes during HTTs. The data were analyzed using IBM SPSS Statistics (version 25.0, Chicago, IL, USA).
Results
Participant characteristics
Twenty-two participants (11 males and 11 females) participated in the present study. Twenty-three participants consented; however, one participant did not begin the study due to lack of time and no data was collected from this participant. The remaining 22 participants were randomized into the HY (n = 11) or NY (n = 11) group and completed all yoga sessions (12 sessions). Participant characteristics separated by sex are displayed in Table 1. Male subjects had an average VO2 max of 44.3 ml/kg/min, categorizing them into the “fair” category for age and sex according to the American College of Sports Medicine (ACSM) guidelines.[33] The average VO2 max among female participants was 39.7 ml/kg/min, indicating a “fair” fitness classification for age and sex according to the ACSM guidelines.[33]
Table 1.
Participant characteristics
| Characteristic | Mean±SD | ||
|---|---|---|---|
| n=22 | F (n=11) | M (n=11) | |
| Age (years) | 26±6 | 24±5 | 28±6 |
| Height (in) | 66.8±4.1 | 63.8±2.7 | 69.9±2.9 |
| Weight (kg) | 70.1±11.8 | 63.3±7.8 | 77.0±11.3 |
| Body fat percent (%) | 18.3±8.1 | 23.4±5.8 | 13.3±6.9 |
| Baseline VO2 max (ml/kg/min) | 44.3±8.1 | 39.7±6.7 | 48.9±6.7 |
VO2 max=Maximal oxygen consumption, SD: Standard deviation
Cardiorespiratory fitness
Absolute VO2 max values at baseline and post yoga intervention are displayed in Table 2. No significant difference was observed in baseline VO2 max between HY and NY groups (P > 0.05). A significant increase in VO2 max was observed within the HY group (3.22 ± 0.76 L/min vs. 3.46 ± 0.79 L/min,P < 0.05), but not in the NY group (3.00 ± 0.80 L/min vs. 3.05 ± 0.75 L/min,P > 0.05). No between-group differences were detected.
Table 2.
Cardiorespiratory fitness pre and post yoga intervention
| Intervention | Mean±SD | |
|---|---|---|
| Baseline VO2 max | Post VO2 max | |
| Hot temperature (L/min) | 3.22±0.76 | 3.46±0.79* |
| Normal temperature (L/min) | 3.00±0.80 | 3.05±0.75 |
*Significantly different from baseline, P<0.05. VO2 max=Maximal oxygen consumption
Heat tolerance
No within- or between-group differences were observed for average VO2, heart rate, RPE, or thermal sensation during the HTT from pre- to postyoga intervention. The change in core temperature (∆Tc) during baseline and postyoga HTT was evaluated within both the HY and NY groups [Figure 3]. No differences within each group were detected [Figure 3]. In addition, no difference was detected between (HY vs. NY) groups for average core temperature change from pre-HTT to post-HTT [Figures 3 and 4].
Figure 3.
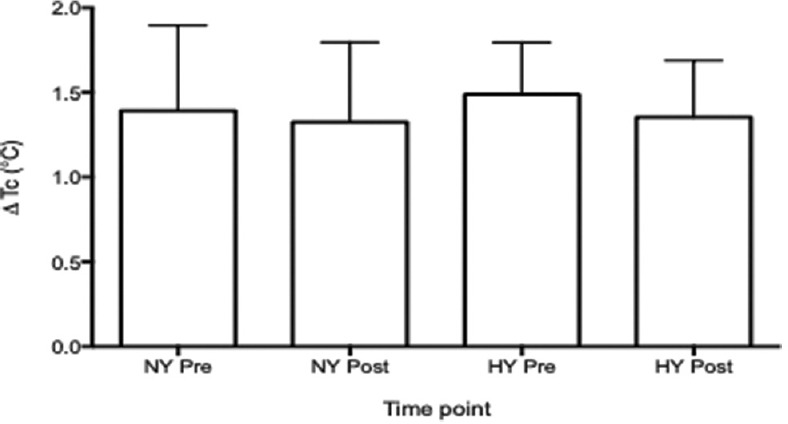
The change in core temperature was evaluated during both pre (baseline) and post (postyoga) heat tolerance trials. No differences were detected within each group. Mean ą standard deviation. N = 22. NY = Normal-temperature yoga, HY = Hot-temperature yoga
Figure 4.
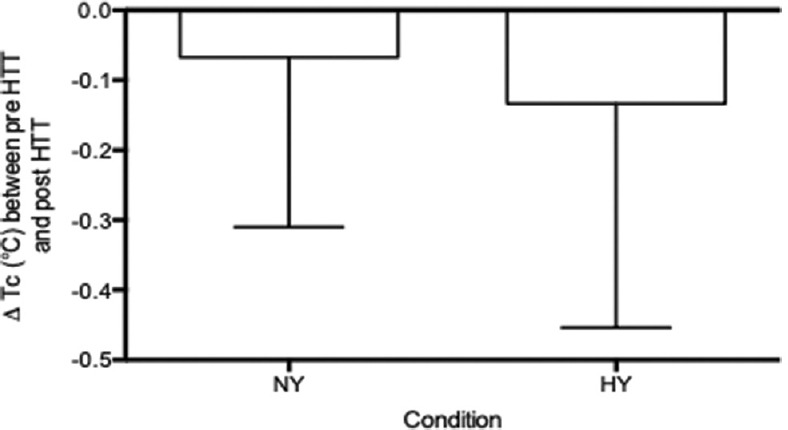
The core temperature difference between pre heat tolerance test and post heat tolerance test within each group (normal-temperature yoga and hot-temperature yoga) was used to compare the core temperature changes between trials. Mean ą standard deviation. N = 22. NY = Normal-temperature yoga, HY = Hot-temperature yoga
Perceived stress scale
Perceived stress scores at baseline and post yoga intervention are displayed in Table 3. Values indicate low perceived stress in both groups at pre and post intervention (low = 0–13). No significant difference was observed in pre and post perceived stress in either the hot-temperature (P > 0.05) or normal-temperature (P > 0.05) group.
Table 3.
Perceived stress scores pre- and post-yoga intervention
| Intervention group | Mean±SD | |
|---|---|---|
| Baseline PSS | Post-PSS | |
| Hot temperature | 13.0±7.1 | 13.7±6.5 |
| Normal temperature | 11.4±3.9 | 10.4±4.5 |
PSS=Perceived Stress Scale, SD=Standard deviation
Brain derived neurotrophic factor
No significant difference was observed in pre and post serum BDNF levels in either the hot-temperature or normal-temperature group (P > 0.05). When both groups were combined (n = 22), a significant difference was observed in pre and post serum BDNF levels (P < 0.05) as displayed in Figure 5.
Figure 5.
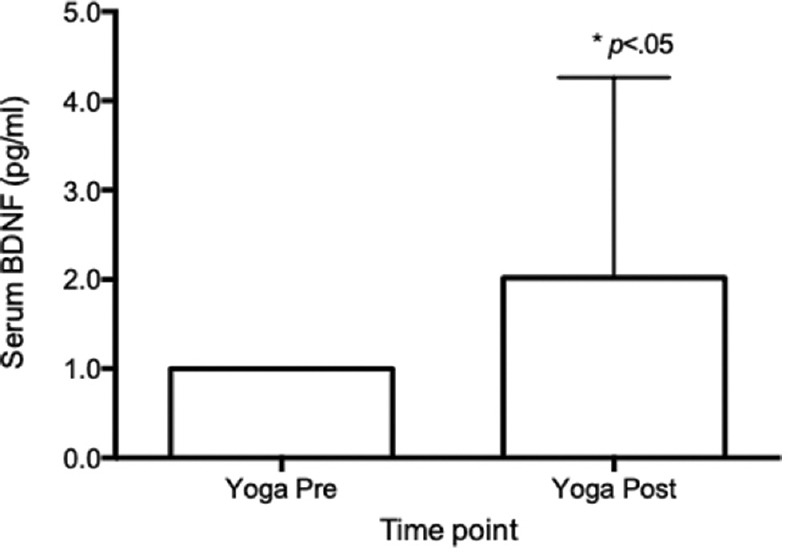
Serum brain derived neurotrophic factor (pg/ml) pre and post yoga intervention in combined groups N = 22. BDNF = Brain derived neurotrophic factor, pg/ml = picograms/milliliter
Heat shock protein 70
A significant increase in PBMC HSP70 was observed in the HY group, but not in the NY group following the yoga intervention (P < 0.05). After the yoga intervention, PBMC HSP70 was significantly higher in the HY versus NY groups [P < 0.05, Figure 6].
Figure 6.
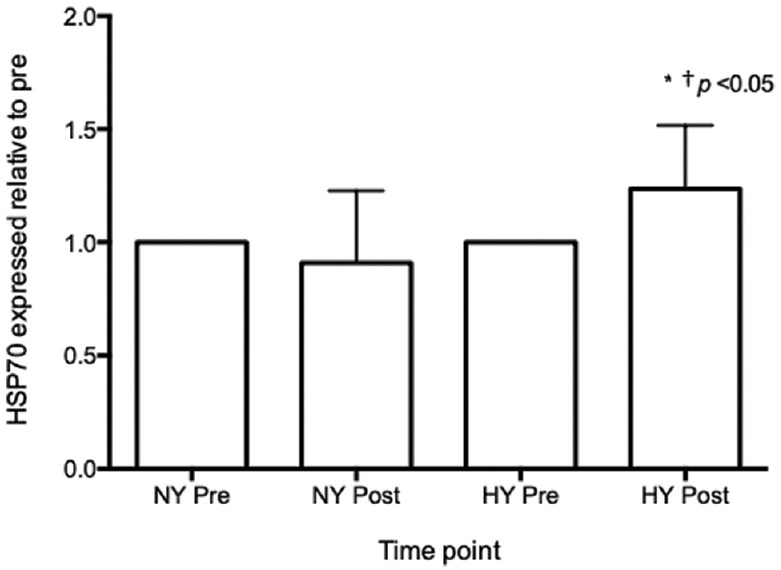
Basal heat shock protein 70 levels relative to pre-intervention in the normal- and hot-temperature group N = 22. HSP70 = heat shock protein 70, NY = normal-temperature yoga, HY = hot-temperature yoga. *Significantly different from baseline, P ≥ 0.05
Adrenocorticotropic hormone
ACTH expression relative to preintervention is displayed in Figure 7. No significant change in ACTH was observed in either the HY or NY group (P > 0.05).
Figure 7.
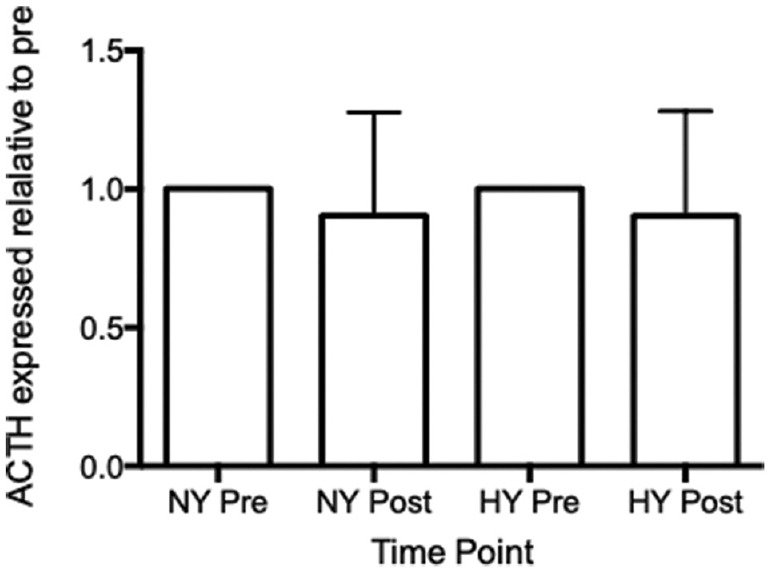
Plasma adrenocorticotropic hormone relative to preintervention in the hot and normal-temperature groups N = 22. ACTH = Adrenocorticotropic hormone, NY = normal-temperature yoga, HY = hot-temperature yoga
Discussion
The findings of the present study demonstrate that 12 sessions of HY, but not NY, improve cardiorespiratory fitness and resting expression of cellular stress response proteins (HSP70). In addition, yoga increased the levels of serum BDNF independent of the heat stress component. Results from this study also suggest that neither HY nor NY alters plasma ACTH, perceived stress, or heat tolerance.
The increase in cardiorespiratory fitness (aerobic capacity or VO2 max) observed in the current study indicates that the added heat stress was adequate to promote cardiovascular adaptation. One possible mechanism is the added cardiovascular strain that occurs during HY compared to yoga performed at room temperature.[21] The percentage of maximal heart rate and RPE of hot yoga participants has been reported to align with moderate intensity exercise according to exercise guidelines, which is able to elicit cardiovascular improvements among untrained humans.[34] Another explanation for the improvement in VO2 max is short-term plasma volume expansion that has been shown to occur in response to both heat acclimation (HA) and hot yoga.[35] Increased circulating volume creates a hypervolemic state and has been shown to augment cardiovascular performance.[36] Plasma volume expansion and improvements in aerobic capacity have been demonstrated after only 10 days of aerobic exercise training.[36] In addition, 16 days of HA (aerobic exercise in the heat) resulted in near immediate (day 8) and sustained plasma volume expansion (day 22).[37] Unfortunately, we did not measure plasma volume changes in the current study.
The aerobic capacity findings, herein, are in contrast to the results reported after a 6-day hot yoga intervention (60 min sessions) among female members of an elite field hockey team.[35] In addition, VO2 max did not increase after twenty-two 90-min hot yoga sessions spread across 8 weeks among healthy adults. Several factors may explain the differing results reported in the current study and those from previous research. The 6-day hot yoga intervention may not have been an adequate amount of cardiovascular strain. Moreover, the subjects recruited in the study were elite level and therefore may need a higher level of exercise training to promote cardiovascular adaptation. Interestingly, the authors reported an expansion of plasma volume 72 h after the last yoga session; however, they measured aerobic capacity at 24 h post yoga. It is more difficult to explain why aerobic capacity did not increase after 22 hot yoga sessions as reported by Tracy and Hart.[38] The majority of participants in the study ranged between 2.18 and 3.40 yoga sessions per week, which may have created a large variance in the aerobic capacity outcome. All participants in the current study were 100% compliant at 3 sessions per week. In addition, the authors did not report postyoga aerobic capacity, so direct comparisons cannot be made.
To investigate whether 12 sessions of HY lead to HA, a HTT technique was employed. Findings suggest that 12 sessions of HY did not lead to classic adaptations to heat stress (i.e., lower rise in core temperature). While no other studies have used the HTT model to explore whether HY results in HA, studies have examined the relationship between other forms of exercise in the heat and HA. For example, Magalhães Fde et al.,[39] reported that 11 one-h sessions of treadmill exercise in the heat (40°C ± 0°C) induced classic HA as observed during an HTT, thus contradicting the findings from the present study. The dissimilarity between results may be due to the difference in the timeline of protocols. Specifically, the protocol employed by Magalhães Fde et al.[39] required subjects to complete the 11 exercise visits in a 12–15 day period. Thus, the heat stimulus may not have been potent enough in the present study to induce similar adaptations.
Despite no change in HA from pre- to post intervention, our results suggest that HY, but not NY, induced cellular thermotolerance as evidenced by increased resting levels of HSP70 in PBMCs indicating enhanced ability to cope with cellular stress. Although the present study is the first to measure basal HSP70 levels in response to a yoga intervention, studies have reported increased HSP70 levels following different exercise interventions in the heat.[22,40] Studies that reported higher levels of HSP70 in PBMCs following HA have typically observed classic HA in addition to the cellular adaptation.[41] The magnitude of the HA is thought to be dependent on the intensity of the exercise performed in the heat.[42] In the present study, intensity of the yoga sessions was not recorded. Thus, it is possible that the intensity of the HY sessions was sufficient to promote cellular thermotolerance but not whole-body HA.
While several studies have investigated the impact of yoga on BDNF, no other studies to date have compared HY and NY effects on BDNF. We hypothesized that HY would increase BDNF expression as both NY and passive heat exposure have been shown to increase serum BDNF levels in humans.[25,43] Our results, however, suggest that 12 sessions of yoga, independent of temperature, may increase serum BDNF levels as significance was only observed when the groups were combined. These findings are in agreement with previous studies. For example, Cahn et al.[7] noted a significant increase in plasma BDNF levels in healthy adults following a 3-month yoga retreat in which NY was practiced daily. In addition, Lee M et al.[44] noted a significant increase in serum BDNF when NY was practiced × 3/week for 3-months in premenopausal women with low back pain. It is important to note that the intervention employed in the present study utilized a shorter intervention (×3/week for 4 weeks) than the studies described above, indicating that longer interventions may not be necessary to increase serum BDNF levels. Our findings disagree with Ikai et al.,[45] who reported no increases in plasma and salivary BDNF in individuals with schizophrenia after practicing NY ×1/week for 8 weeks. This study did not, however, control for use of antipsychotics which have been shown to decrease BDNF expression, which may explain the conflicting findings.[46]
No difference was observed in ACTH levels or perceived stress from pre to post intervention or between groups. To date, no other studies have compared the effect of HY versus NY on ACTH levels. Few studies have investigated the impact of NY on ACTH with inconsistent results observed. For example, Vedamurthachar et al.[47] reported reduced plasma ACTH after practicing Sudarshana Kriya Yoga ×1/week for 2 weeks in individuals rehabilitating from alcohol dependence. In contrast, Najafi and Moghadasi[14] observed an increase in plasma ACTH and reduction in cortisol after a yoga intervention in which women with multiple sclerosis performed yoga ×3/week for 8 weeks. These studies support the argument that yoga may modulate ACTH in clinical populations, as both multiple sclerosis and alcohol dependence have been linked to dysregulation of the HPA axis.[48,49] The present study comprised healthy subjects which may explain the disagreement in results. In addition, Vera et al.[50] found no difference in plasma ACTH levels between long-term yoga practitioners and a nonyoga practitioner control group, further supporting the idea that yoga may modulate ACTH activity in individuals prone to HPA-axis dysregulation but not healthy subjects.
Similarly, no difference in perceived stress was observed from pre to post intervention or between groups. These findings disagree with Hartfiel et al.,[51] who report reduced perceived stress following 8 weeks (×1/week, 50-min) of normal-temperature Dru Yoga (mean participation rate = 21 sessions). The type of yoga performed (Dru Yoga) may explain the conflicting results as Dru Yoga also includes affirmation and visualization relaxation techniques. Our findings also conflict with Hewett et al.,[52] who reported that 16 weeks (3–×5/week, 90-min) of HY at a Bikram yoga studio reduced perceived stress in sedentary adults. It is possible that the yoga studio environment and greater volume of yoga sessions explain the inconsistent findings with the present study. Our results are consistent with findings from Chu et al.,[53] who observed no change in perceived stress after 8-weeks (×2/week, 60 min) of NY. The conflicting results within the literature regarding the impact of yoga on stress reduction warrant further investigation.
Limitations
The present study was limited by the small sample size (n = 22), which may have limited the statistical power to detect changes in outcome measures outside of BDNF. Further, the impact of yoga on neural and hormonal markers may be more prevalent among populations experiencing cognitive/neural impairment, which may affect the external validity of the present study. In addition, hot yoga sessions are commonly 90 min in length; however, we modified duration as recruited subjects did not have prior yoga experience.
Conclusions
Our findings indicate that a short duration (4 weeks, ×3/week) HY intervention may provide a sufficient physiological stimulus to improve VO2 max and improve cellular thermotolerance (as evidenced by an increase in circulating PBMC HSP70) but not whole-body heat adaptations. Further, 12 sessions of yoga, regardless of environmental temperature, may increase serum BDNF levels. Results from the present study do not support an effect of hot or NY on HA, plasma ACTH, or perceived stress.
Although the present study was conducted in healthy participants, this research provides evidence that yoga may provide unique benefits for clinical populations. For example, HY may be a suitable way to improve fitness in clinical populations that are unable to tolerate high intensity exercise (i.e., obesity, chronic obstructive pulmonary disease, and cardiovascular disease), given that they are able to tolerate the hot environment. In addition, reduced expression of HSP70 is related to the progression of neurodegenerative disease, further supporting the clinical use of HY.[54] Similarly, hot and NY may be beneficial in populations that suffer from reduced BDNF expression including depression and schizophrenia.[55,56,57] Further research should explore the use of hot and NY in clinical populations with low cardiorespiratory fitness, altered HSP70 levels, and reduced BDNF.
Ethical clearance
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or ethics committee) of the University of New Mexico (IRB reference #1145197).
Financial support and sponsorship
Pure Action, Inc., Austin, Texas, USA, a 501c3 nonprofit organization.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank our yoga instructors: Valarie Maestas, Brenan Bitton-Foronda, and Jenna Sessions.
Appendix 1
Hot and Normal Temperature Yoga Protocol
| Pose name | Posture | Movement | Length of time |
|---|---|---|---|
| Standing deep breathing pose (Pranayama) | Standing with hands placed under chin and elbows extended to side | Inhalation while raising elbows, exhalation with elbows falling | 3-min |
| Half-moon pose (Ardha Chandrasana) | Standing with arms overhead (hands together) | Moving hips to right while tilting to the left (then opposite side) | 2x each side (hold 15s) |
| Awkward pose (Utkatasana) | Slight squatting position while on toes | Lower to comfortable position and then rise | 2x (hold 30s) |
| Sun salutations (Surya Namaskar) | A series of poses that move from standing to lunge, to plank, to downward dog | From standing, forward bend, move feet back and into a plank position, lower to ground, upward dog, then downward dog, then back to standing | Perform 5x |
| Eagle pose (Garurasana) | Standing on one foot with opposite foot curled over top of standing leg. Arms are crossed | Slight bend in standing leg, while holding pose | 2x with each leg (hold 30s) |
| Standing head-to knee-pose (Dandayamana-Janushirasana) | Standing on one foot with other leg extended in front | Hold extended foot while bending forward. Modified version is extending knee only | 2x each leg (hold 30s) |
| Balancing stick pose (Tuladandasana) | Standing on one foot | Bend forward with arms moving parallel to floor and nonstanding foot extending behind | 2x each leg (hold 30s) |
| Standing bow (Dandayamana-Dhanurasana) | While in balancing stick pose | Bend back leg and attempt to reach back to hold leg (various modifications to this pose) | 1x each leg (30s) |
| Standing separate leg stretch (Dandayamana-bibhaktapada-paschimotthanasana) | Feet spread wider than hip distance | Forward bend with grabbing outside of feet | 2x (hold 30s) |
| Triangle pose (Trikanasana) | Lunge position with back foot sideways (parallel to back of mat) | Left foot forward, extend left hand down to foot while reaching right arm up to ceiling. Slight twist in trunk | 1x each side (hold 30-60s) |
| Standing separate leg-head to knee pose (Dandayamana-bibhaktapada-janushirasana) | Standing with one foot about 2.5 feet back from front leg | Forward bend over the front leg while keeping back straight | 1x with each leg (30-60s) |
| Tree pose (Vrksasana) | Standing on one leg with hands together at chest | Bend non standing leg and place against shin or thigh and hold balance | 1x each leg (30-60s) |
| Corpse pose (Savasana) | Laying on back with arms at side and feet at mat width | Laying still while breathing | 3 min |
| Wind removing pose (Pavanamuktasana) | Laying on back | Bring right knee to chest and hug knees with arms, then left knee, then both knees | 1-2 min total |
| Seated forward bend pose (Paschimottanasana) | Sitting with feet in front | Forward bend and grab toes (modifications) | 2x (hold 30s) |
| Cobra pose (Bhujangasana) | Laying on stomach with hands under arm pits | Push down with hands while raising trunk | 2x (hold 30s) |
| Locust pose (Ardha Shalabhasana) | Laying on stomach with arms tucked under chest | Raise one leg at a time | 2x each leg (hold 15-30s) |
| Full locust (Salabhasana) | Laying on stomach with arms extended at sides | Raise feet and arms together | 2x (hold 15-30s) |
| Floor bow pose (Dhanurasana) | Laying on stomach arms at side and legs extended | Flex legs at knees and reach arms back to grab ankles | 2x (hold 15-30 s) |
| Camel pose (Ustrasana) | Kneeling upright | Place hands on buttocks or lower back while bending backwards. Some may be able to reach feet | 2x hold 15s |
| Childs pose (Balasana) | Kneeling upright | Curling head to knees while reaching hands back to feet | 2x hold 15s |
| Head to knee pose (Janu Sirsasana) | Sitting upright, one leg extended with other foot placed against inner thigh | Reach for extended leg with forward fold | 2x each leg (hold 30s) |
| Spine twist pose (Parivrtta Sukhasana) | One leg extended with other crossed over top | Twist trunk while placing elbow on other side of crossed leg | 1x each side (hold 30s) |
| Blowing in firm (Kapalbhati Pranayama) | Kneeling upright with hands on knees | Kneeling all while breathing | 2x 15s |
References
- 1.Clarke TC, Barnes PM, Black LI, Stussman BJ, Nahin RL. Use of yoga, meditation, and chiropractors among us adults aged 18 and over. NCHS Data Brief. 2018;325:1–8. [PubMed] [Google Scholar]
- 2.McCall MC. In search of yoga: Research trends in a western medical database. Int J Yoga. 2014;7:4–8. doi: 10.4103/0973-6131.123470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: A systematic review and meta-analysis. Depress Anxiety. 2013;30:1068–83. doi: 10.1002/da.22166. [DOI] [PubMed] [Google Scholar]
- 4.Vancampfort D, Vansteelandt K, Scheewe T, Probst M, Knapen J, De Herdt A, et al. Yoga in schizophrenia: A systematic review of randomised controlled trials. Acta Psychiatr Scand. 2012;126:12–20. doi: 10.1111/j.1600-0447.2012.01865.x. [DOI] [PubMed] [Google Scholar]
- 5.Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: A systematic review. Evid Based Complement Alternat Med. 2007;4:469–86. doi: 10.1093/ecam/nel103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadja J, Mills PJ. Effects of yoga interventions on fatigue in cancer patients and survivors: A systematic review of randomized controlled trials. Explore (NY) 2013;9:232–43. doi: 10.1016/j.explore.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cahn BR, Goodman MS, Peterson CT, Maturi R, Mills PJ. Yoga, meditation and mind-body health: Increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3-month yoga and meditation retreat. Front Hum Neurosci. 2017;11:315. doi: 10.3389/fnhum.2017.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross A, Thomas S. The health benefits of yoga and exercise: A review of comparison studies. J Altern Complement Med. 2010;16:3–12. doi: 10.1089/acm.2009.0044. [DOI] [PubMed] [Google Scholar]
- 9.Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. 2009;10:397–409. doi: 10.1038/nrn2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young AH. Cortisol in mood disorders. Stress. 2004;7:205–8. doi: 10.1080/10253890500069189. [DOI] [PubMed] [Google Scholar]
- 11.Varghese FP, Brown ES. The hypothalamic-pituitary-adrenal axis in major depressive disorder: A brief primer for primary care physicians. Prim Care Companion J Clin Psychiatry. 2001;3:151–5. doi: 10.4088/pcc.v03n0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kallen VL, Tulen JH, Utens EM, Treffers PD, De Jong FH, Ferdinand RF. Associations between HPA axis functioning and level of anxiety in children and adolescents with an anxiety disorder. Depress Anxiety. 2008;25:131–41. doi: 10.1002/da.20287. [DOI] [PubMed] [Google Scholar]
- 13.Bradley AJ, Dinan TG. A systematic review of hypothalamic-pituitary-adrenal axis function in schizophrenia: Implications for mortality. J Psychopharmacol. 2010;24:91–118. doi: 10.1177/1359786810385491. [DOI] [PubMed] [Google Scholar]
- 14.Najafi P, Moghadasi M. The effect of yoga training on enhancement of Adrenocorticotropic hormone (ACTH) and cortisol levels in female patients with multiple sclerosis. Complement Ther Clin Pract. 2017;26:21–5. doi: 10.1016/j.ctcp.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 15.Halappa NG, Thirthalli J, Varambally S, Rao M, Christopher R, Nanjundaiah GB. Improvement in neurocognitive functions and serum brain-derived neurotrophic factor levels in patients with depression treated with antidepressants and yoga. Indian J Psychiatry. 2018;60:32–7. doi: 10.4103/psychiatry.IndianJPsychiatry_154_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Binder DK, Scharfman HE. Brain-derived neurotrophic factor. Growth Factors. 2004;22:123–31. doi: 10.1080/08977190410001723308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zuccato C, Cattaneo E. Brain-derived neurotrophic factor in neurodegenerative diseases. Nat Rev Neurol. 2009;5:311–22. doi: 10.1038/nrneurol.2009.54. [DOI] [PubMed] [Google Scholar]
- 18.Hashimoto K, Shimizu E, Iyo M. Critical role of brain-derived neurotrophic factor in mood disorders. Brain Res Brain Res Rev. 2004;45:104–14. doi: 10.1016/j.brainresrev.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Balasubramaniam M, Telles S, Doraiswamy PM. Yoga on our minds: A systematic review of yoga for neuropsychiatric disorders. Front Psychiatry. 2012;3:117. doi: 10.3389/fpsyt.2012.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cramer H, Lauche R, Langhorst J, Dobos G. Is one yoga style better than another.A systematic review of associations of yoga style and conclusions in randomized yoga trials? Complement Ther Med. 2016;25:178–87. doi: 10.1016/j.ctim.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 21.Boyd CN, Lannan SM, Zuhl MN, Mora-Rodriguez R, Nelson RK. Objective and subjective measures of exercise intensity during thermo-neutral and hot yoga. Appl Physiol Nutr Metab. 2018;43:397–402. doi: 10.1139/apnm-2017-0495. [DOI] [PubMed] [Google Scholar]
- 22.Yamada PM, Amorim FT, Moseley P, Robergs R, Schneider SM. Effect of heat acclimation on heat shock protein 72 and interleukin-10 in humans. J Appl Physiol (1985) 2007;103:1196–204. doi: 10.1152/japplphysiol.00242.2007. [DOI] [PubMed] [Google Scholar]
- 23.Michel V, Peinnequin A, Alonso A, Buguet A, Cespuglio R, Canini F. Decreased heat tolerance is associated with hypothalamo-pituitary-adrenocortical axis impairment. Neuroscience. 2007;147:522–31. doi: 10.1016/j.neuroscience.2007.04.035. [DOI] [PubMed] [Google Scholar]
- 24.Tamm M, Jakobson A, Havik M, Timpmann S, Burk A, Ööpik V, et al. Effects of heat acclimation on time perception. Int J Psychophysiol. 2015;95:261–9. doi: 10.1016/j.ijpsycho.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Kojima D, Nakamura T, Banno M, Umemoto Y, Kinoshita T, Ishida Y, et al. Head-out immersion in hot water increases serum BDNF in healthy males. Int J Hyperthermia. 2018;34:834–9. doi: 10.1080/02656736.2017.1394502. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 27.Jackson AS, Pollock ML. Generalized equations for predicting body density of men. Br J Nutr. 1978;40:497–504. doi: 10.1079/bjn19780152. [DOI] [PubMed] [Google Scholar]
- 28.Jackson AS, Pollock ML, Ward A. Generalized equations for predicting body density of women. Med Sci Sports Exerc. 1980;12:175–81. [PubMed] [Google Scholar]
- 29.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81. [PubMed] [Google Scholar]
- 30.Young AJ, Sawka MN, Epstein Y, Decristofano B, Pandolf KB. Cooling different body surfaces during upper and lower body exercise. J Appl Physiol (1985) 1987;63:1218–23. doi: 10.1152/jappl.1987.63.3.1218. [DOI] [PubMed] [Google Scholar]
- 31.Kuennen M, Gillum T, Dokladny K, Bedrick E, Schneider S, Moseley P. Thermotolerance and heat acclimation may share a common mechanism in humans. Am J Physiol Regul Integr Comp Physiol. 2011;301:R524–33. doi: 10.1152/ajpregu.00039.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen S, Williamson G. Newbury Park (CA): Sage; 1988. Perceived stress in a probability sample of the United States. The social psychology of health. In: Claremont Symposium on Applied Social Psychology. [Google Scholar]
- 33.Riebe D, Ehrman J, Liguori G, Magal M. 10th ed. Philadelphia: Wolters Kluwer Heath; 2017. ACSM's Guidelines for Exercise Testing and Prescription. [Google Scholar]
- 34.Pescaltello LS, Arena R, Riebe D, Thompson PD. 9th ed. Philadelphia: Wolters Kluwer Heath; 2013. ACSM's Guidelines for Exercise Testing and Prescription. [DOI] [PubMed] [Google Scholar]
- 35.Perrotta AS, White MD, Koehle MS, Taunton JE, Warburton DE. Efficacy of hot yoga as a heat stress technique for enhancing plasma volume and cardiovascular performance in elite female field hockey players. J Strength Cond Res. 2018;32:2878–87. doi: 10.1519/JSC.0000000000002705. [DOI] [PubMed] [Google Scholar]
- 36.Mier CM, Domenick MA, Turner NS, Wilmore JH. Changes in stroke volume and maximal aerobic capacity with increased blood volume in men women. J Physiol. 2004;559:327–34. doi: 10.1152/jappl.1996.80.4.1180. [DOI] [PubMed] [Google Scholar]
- 37.Patterson MJ, Stocks JM, Taylor NA. Sustained and generalized extracellular fluid expansion following heat acclimation. J Physiol. 2004;559:327–34. doi: 10.1113/jphysiol.2004.063289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tracy BL, Hart CE. Bikram yoga training and physical fitness in healthy young adults. J Strength Cond Res. 2013;27:822–30. doi: 10.1519/JSC.0b013e31825c340f. [DOI] [PubMed] [Google Scholar]
- 39.Magalhães Fde C, Amorim FT, Passos RL, Fonseca MA, Oliveira KP, Lima MR, et al. Heat and exercise acclimation increases intracellular levels of Hsp72 and inhibits exercise-induced increase in intracellular and plasma Hsp72 in humans. Cell Stress Chaperones. 2010;15:885–95. doi: 10.1007/s12192-010-0197-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Amorim F, Yamada P, Robergs R, Schneider S, Moseley P. Effects of whole-body heat acclimation on cell injury and cytokine responses in peripheral blood mononuclear cells. Eur J Appl Physiol. 2011;111:1609–18. doi: 10.1007/s00421-010-1780-4. [DOI] [PubMed] [Google Scholar]
- 41.Amorim FT, Fonseca IT, Machado-Moreira CA, Magalhães Fde C. Insights into the role of heat shock protein 72 to whole-body heat acclimation in humans. Temperature (Austin) 2015;2:499–505. doi: 10.1080/23328940.2015.1110655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: Applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25:20–38. doi: 10.1111/sms.12408. [DOI] [PubMed] [Google Scholar]
- 43.Govindaraj R, Karmani S, Varambally S, Gangadhar BN. Yoga and physical exercise – A review and comparison. Int Rev Psychiatry. 2016;28:242–53. doi: 10.3109/09540261.2016.1160878. [DOI] [PubMed] [Google Scholar]
- 44.Lee M, Moon W, Kim J. Effect of yoga on pain, brain-derived neurotrophic factor, and serotonin in premenopausal women with chronic low back pain. Evid Based Complement Alternat Med. 2014;2014:1–7. doi: 10.1155/2014/203173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ikai S, Suzuki T, Uchida H, Saruta J, Tsukinoki K, Fujii Y, et al. Effects of weekly one-hour Hatha yoga therapy on resilience and stress levels in patients with schizophrenia-spectrum disorders: An eight-week randomized controlled trial. J Altern Complement Med. 2014;20:823–30. doi: 10.1089/acm.2014.0205. [DOI] [PubMed] [Google Scholar]
- 46.Favalli G, Li J, Belmonte-de-Abreu P, Wong AH, Daskalakis ZJ. The role of BDNF in the pathophysiology and treatment of schizophrenia. J Psychiatr Res. 2012;46:1–1. doi: 10.1016/j.jpsychires.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 47.Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna DK, Sureshbabu SV, et al. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006;94:249–53. doi: 10.1016/j.jad.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 48.Stephens MA, McCaul ME, Wand GS. The potential role of glucocorticoids and the HPA axis in alcohol dependence. Neurobiol Alcohol Depend. 2014:429–50. Doi: 10.1016/B978-0-12-405941-2.00021-3. [Google Scholar]
- 49.Huitinga I, Erkut ZA, Van Beurden D, Swaab DF. The hypothalamo-pituitary-adrenal axis in multiple sclerosis. Ann N Y Acad Sci. 2003;992:118–28. doi: 10.1111/j.1749-6632.2003.tb03143.x. [DOI] [PubMed] [Google Scholar]
- 50.Vera FM, Manzaneque JM, Maldonado EF, Carranque GA, Rodriguez FM, Blanca MJ, et al. Subjective Sleep Quality and hormonal modulation in long-term yoga practitioners. Biol Psychol. 2009;81:164–8. doi: 10.1016/j.biopsycho.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 51.Hartfiel N, Burton C, Rycroft-Malone J, Clarke G, Havenhand J, Khalsa SB, et al. Yoga for reducing perceived stress and back pain at work. Occup Med (Lond) 2012;62:606–12. doi: 10.1093/occmed/kqs168. [DOI] [PubMed] [Google Scholar]
- 52.Hewett ZL, Pumpa KL, Smith CA, Fahey PP, Cheema BS. Effect of a 16-week Bikram yoga program on perceived stress, self-efficacy and health-related quality of life in stressed and sedentary adults: A randomised controlled trial. J Sci Med Sport. 2018;21:352–7. doi: 10.1016/j.jsams.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 53.Chu IH, Lin YJ, Wu WL, Chang YK, Lin IM. Effects of yoga on heart rate variability and mood in women: A randomized controlled trial. J Altern Complement Med. 2015;21:789–95. doi: 10.1089/acm.2015.0138. [DOI] [PubMed] [Google Scholar]
- 54.Muchowski PJ, Wacker JL. Modulation of neurodegeneration by molecular chaperones. Nat Rev Neurosci. 2005;6:11–22. doi: 10.1038/nrn1587. [DOI] [PubMed] [Google Scholar]
- 55.Shimizu E, Hashimoto K, Okamura N, Koike K, Komatsu N, Kumakiri C, et al. Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants. Biol Psychiatry. 2003;54:70–5. doi: 10.1016/s0006-3223(03)00181-1. [DOI] [PubMed] [Google Scholar]
- 56.Laske C, Stransky E, Leyhe T, Eschweiler GW, Maetzler W, Wittorf A, et al. BDNF serum and CSF concentrations in Alzheimer's disease, normal pressure hydrocephalus and healthy controls. J Psychiatr Res. 2007;41:387–94. doi: 10.1016/j.jpsychires.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 57.Toyooka K, Asama K, Watanabe Y, Muratake T, Takahashi M, Someya T, et al. Decreased levels of brain-derived neurotrophic factor in serum of chronic schizophrenic patients. Psychiatry Res. 2002;110:249–57. doi: 10.1016/s0165-1781(02)00127-0. [DOI] [PubMed] [Google Scholar]