Abstract
Background
One of the constraints in containing the impact of the COVID-19 pandemic in Ecuador is limited testing capacity, especially in high-risk populations such as people living in humanitarian shelters.
Objectives
The “United Nations High Commissioner for Refugees” office in Ecuador in collaboration with “Universidad de Las Américas” performed surveillance screening at shelters for women victims of gender-based violence. They had been granted access to RT-qPCR tests for SARS-CoV-2 diagnosis since July 2020, a few weeks after the general population lockdown was lifted.
Results
From 411 people tested, 52 tests were SARS-CoV-2 positive, yielding an overall high attack rate of 12.65%. Moreover, COVID-19 outbreaks were found in nine of 11 shelters that were included in the study. While attacks rates varied among shelters, no association was found with occupancy.
Conclusion
This study is key to clarifying the epidemiological situation in this highly vulnerable population in Latin America. It highlights the importance of mass testing beyond the symptomatic population to prevent the spread of COVID-19.
Keywords: COVID-19, SARS-CoV-2, Shelters, Gender-based violence, Ecuador
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) raised alerts in the global scientific and health communities since the first 27 cases were reported in December 2019 from Wuhan, China. SARS-CoV-2 spread readily and quickly around the world, and the first cases in Latin America were reported just two months after the original report (PAHO, 2021). Until March 2021, more than 51 million COVID-19 cases and more than 1 million deaths were reported in the Americas region; and more than 290,000 cases were reported in Ecuador since the arrival of the first case in March 2020 (PAHO, 2021). However, with limited SARS-CoV-2 testing capacity and a positivity rate over 30%, those numbers are far from the real ones.
During the first months of the pandemic, a wide variety of recommendations were endorsed by the World Health Organization (including social distancing, mass testing, and isolation of confirmed cases) to slow down the spread of the disease. However, those measures are difficult to meet in some specific settings, including: refugee shelters, housing for victims of gender-based violence, prisons or provisional detention centres, among others. Confinement and prevention of spread in those settings is nearly impossible due to the lack of adequate infrastructure and the high occupation of some shelters (Peate, 2020, Wood et al., 2020). Moreover, confinement represents harm for the economic needs of the people living in those spaces. Testing capacity is also lower in those settings when compared with middle-income or high-income environments (Wang et al., 2020), and even worse with weak healthcare systems (e.g., in developing countries) (Inter-Agency Standing Committee (IASC), 2020).
Many humanitarian shelters are generally occupied to their full capacity at times of economic crisis, like the current one, making hotspots for SARS-CoV-2 infection and contagion. During the highest peak of the COVID-19 pandemic in Ecuador, the need for mass testing throughout the country was urgent to complement the effort of the public health system and to reach sectors of the population for whom PCR tests were inaccessible (Ortiz-Prado et al., 2021a,b, Freire-Paspuel et al., 2020). In this context, “Universidad de Las Américas” (UDLA) and the United Nations High Commissioner for Refugees (UNHCR) office in Ecuador coordinated efforts for granting access to SARS-CoV-2 PCR tests for the occupants of ten shelters for women victims of gender-based violence located across the country. By September 2020, when this study was finished, according to the official information from the Ecuadorian Ministry of Health (https://www.salud.gob.ec/wp-content/uploads/2020/09/Boletin-196_Nacional_MSP.pdf), a total number of 116,451 SARS-CoV-2-positives cases were reported in the country. However, with a positivity rate of 40.03%, the need to increase SARS-CoV-2 testing is mandatory.
This study aimed to highlight the epidemiological situation of those women’s shelters in Ecuador, the importance of testing in such humanitarian settings, and to assess whether the occupancy level of each shelter is related to the positivity rate. Thus, a description of the study population is provided, as well as a comparison between the attack rates at the different shelters and the occupation levels.
Methods
Study design and setting
A study to evaluate the burden of SARS-CoV-2 infection among all the occupants (women victims of gender-based violence and their children) and staff working (total number of 411 individuals) in 11 shelters was performed in nine different Ecuadorian cities from July to September 2020. The UNHCR office in Ecuador provided logistics for sampling in the different cities and the samples transportation to the UDLA Laboratory located in Quito, Ecuador. Also, UNHCR coordinated with “Red Nacional de Casas de Acogida” to select the shelters to be included in the study. The shelters considered were: “Casa de Acogida Manos Unidas Tejiendo Progreso” (Tulcan), “Casa Mama Zoila Espinoza” (Ibarra), “Casa Tránsito Amaguaña” (Cotacachi), “Casa Amiga” (Lago Agrio), “Casa Paula” (Francisco de Orellana), “Casa de la Mujer” and “Casa Matilde” (Quito), “Casa de Acogida Cotopaxi” (Salcedo), “Casa María Amor” (Cuenca), and “Hogar de Nazareth” (Guayaquil). Also, a group of 100 women refugees and their children who were migrating from Colombia and Venezuela were tested at a temporary shelter in Lago Agrio.
Sample collection, RNA extraction, and RT-qPCR for SARS-CoV-2 diagnosis using the CDC protocol
Nasopharyngeal swabs were collected on 0.5 mL TE pH 8 buffer for SARS-CoV-2 diagnosis by RT-qPCR following an adapted version of the Centers for Disease Control and Prevention (CDC) protocol by using “AccuPrep Viral RNA extraction kit” (Bioneer, South Korea) as an alternate RNA extraction method and CFX96 BioRad instrument (Freire-Paspuel and Garcia-Bereguiain, 2020, Freire-Paspuel et al., 2020b, Freire-Paspuel et al., 2020c, Freire-Paspuel et al., 2020d, Freire-Paspuel et al., 2021, Freire-Paspuel and Garcia-Bereguiain, 2021, CDC, 2021, Lu et al., 2020). Briefly, the CDC designed RT-qPCR FDA EUA 2019-nCoV CDC kit (IDT, USA) is based on N1 and N2 probes to detect SARS-CoV-2 and RNase P as an RNA extraction quality control (CDC, 2021, Lu et al., 2020). Negative controls (TE pH 8 buffer) were included as control for carryover contamination, one for each set of RNA extractions, to guarantee that only true positives were reported. For viral loads calculation, the 2019-nCoV N positive control (IDT, USA) was used, provided at 200.000 genome equivalents/μL, and a factor of 200 was applied to convert the viral loads to genome equivalents/mL and then converted to logarithmic scale.
Statistical analysis
For the statistical analysis of data, positivity rates were calculated for each shelter and occupancy rates were provided by UNHCR. To assess differences in the positivity rates among shelters, Chi-squared for comparison of proportions was applied, and a Pearson’s correlation test was performed to evaluate correlation between positivity rates and occupancy levels. All statistical analysis was carried out using R software.
Results
Overall SARS-CoV-2 attack rates and viral loads
A total of 411 people from refugee shelters were tested for SARS-CoV-2 using nasopharyngeal swabs. The shelters were distributed along the different geographical regions of Ecuador in nine cities: Cotacachi, Cuenca, Ibarra, Latacunga, Quito, and Tulcan in the Andean Region; Guayaquil in the Coastal Region; and Francisco de Orellana and Lago Agrio in the Amazon Region (Figure 1 A). Most of the samples were taken from females (283/411, 68.86%) aged between 30–40 years (mean 31.55 ± 0.73 years) inhabiting those shelters (Figure 1B,C). The overall attack rate of SARS-CoV-2 in all the shelters was 52/411 (12.65%) (Figure 1D). SARS-CoV-2 outbreaks were found in nine of the 11 shelters visited.
Figure 1.
Description of study population. (A) Number of SARS-CoV-2 RT-qPCR tests applied in different shelter locations. (B) Distribution of individuals tested by sex. (C) Distribution of individuals tested according to age. (D) Distribution of individuals who tested positive and negative.
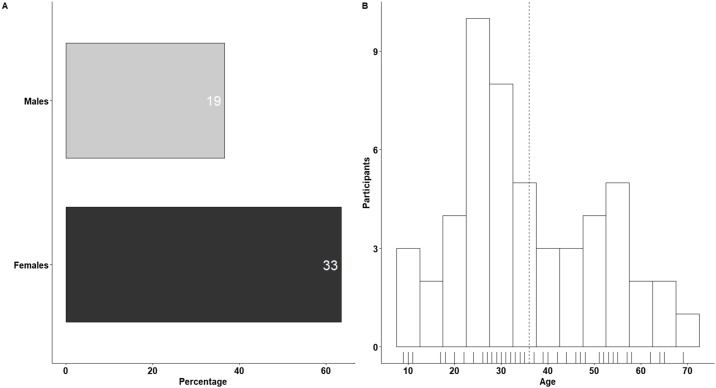
The subjects who tested positive for SARS-CoV-2 were distributed as shown in Figure 2, with a lower positivity ratio in females (33/283, 11.66%) than in males (19/128, 14.84%). Furthermore, more cases were distributed among the younger population (aged < 40 years) with an average age of 36.02 ± 2.11 years.
Figure 2.
Distribution of SARS-CoV-2 RT-qPCR-positive cases according to sex (A) and age (B) at the shelters for women victims of gender-based violence included in the study.
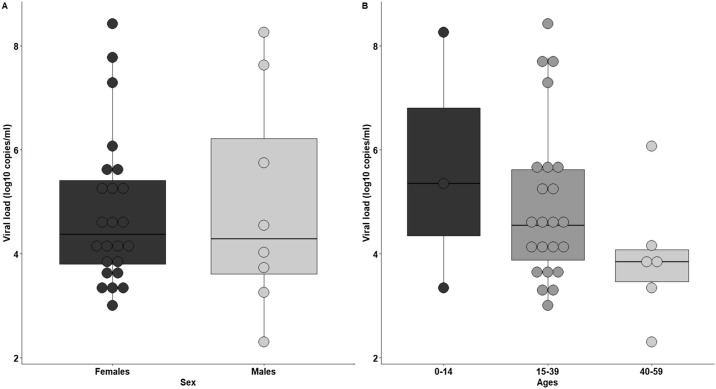
Data for viral loads (VL) were available for 32 of the 52 positive individuals in this study; thus, 32 individuals were considered for differences in VL between age groups and sex. There were no significant differences in the average VL among different sex or age groups (p > 0.05). However, higher VL were distributed within young adults (aged 15–39 years) and in females (Figure 3 ). The latter could be attributable to the fact that most of the occupants of different shelters were women and their children.
Figure 3.
SARS-CoV-2 viral load distribution according to sex (A) and age ranges (0–14: children, 15–39: young adults, 40–50: adults); (B) for the positive individuals included on the study (viral load is expressed as log10 copies/ml).
SARS-CoV-2 attack rates at different locations and shelters
The location of each shelter and its SARS-CoV-2 attack rate are detailed as follows and in Table 1:
-
‐
Lago Agrio city shelters (Sucumbios province, Amazonian Region). Two shelters were tested at Lago Agrio. First, a temporary shelter with 100 women refugees and their children coming from Colombia and Venezuela. In this sample, 100 RT-qPCR tests were performed on 56 females and 44 males. The SARS-CoV-2 attack rate was 20.0%. No occupation rate information was available for this refugee shelter. Second, the foster home “Casa Amiga” in Lago Agrio, with 72% capacity occupation was tested. Thirty-six individuals were sampled in this location and no SARS-CoV-2 positive cases were found.
-
‐
Francisco de Orellana shelter (Orellana province, Amazonian Region). In the capital city of Orellana province, “Casa Paula” shelter was considered for this study. Thirty-one people (27 females and four males) were tested, and seven had positive results, resulting in a SARS-CoV-2 attack rate of 22.6%. This shelter was occupied at 100% of its capacity.
-
‐
Tulcan city shelter (Carchi province, Andean Region). Twenty-one samples were taken in a shelter in Tulcán, distributed between 16 females and five males, with one male individual being positive, giving a SARS-CoV-2 attack rate of 4.8%. The shelter “Casa Manos Unidas Tejiendo Progreso” was occupied at 30% of its capacity.
-
‐
Quito city shelters (Pichincha province; Andean Region). Two shelters from the Ecuadorian capital city were considered in the study: “Casa de la Mujer” and “Casa Matilde”. “Casa de la Mujer” had an occupancy percentage of 55%, and 27 samples from 26 females and one male were considered: no SARS-CoV-2-positive individuals were found. In contrast, “Casa Matilde” was occupied at 73% of its capacity, and seven individuals of 28 living in the shelter (22 females and six males) had positive tests, giving a SARS-CoV-2 attack rate of 25.0%.
-
‐
Latacunga city shelter (Cotopaxi province, Andean Region). From “Casa de Acogida Cotopaxi” in Latacunga, 15 women and three men were tested for SARS-CoV-2, with three positive individuals, yielding an attack rate of 16.7%. This shelter was at 110% of its capacity.
-
‐
Ibarra city shelter (Imbabura province, Andean Region). Twenty-seven individuals were tested with four being positive, giving a SARS-CoV-2 attach rate of 14.8%. No shelter occupancy information was available.
-
‐
Cotacachi city shelter (Imbabura province, Andean region). Thirteen individuals were tested with four being positive, giving a SARS-CoV-2 attack rate of 30.8%. No shelter occupancy information was available.
-
‐
Cuenca city shelter (Azuay province; Andean region). “Casa María Amor” was overcrowded at 118% of its full capacity. Forty-nine women and 23 men were tested in this shelter, and three individuals were positive, giving an attack rate of 4.17% for this centre.
-
‐
Guayaquil city shelter (Guayas province, Coastal Region). From the 38 individuals sampled in “Casa Hogar de Nazareth” in Guayaquil, 26 were females and 12 were males, with three individuals being positive for SARS-CoV-2. The attack rate for this shelter was 7.89% and it was occupied at 37%.
Table 1.
SARS-CoV-2 attack rates, number of individuals tested, and occupation rates from the shelters for women victims of gender-based violence included in the study.
| Shelter | SARS-CoV-2 attack rate (%) | Sample size | Occupation (%) |
|---|---|---|---|
| Casa María Amor | 4.2 | 72 | 118 |
| Casa de Acogida Cotopaxi | 16.7 | 18 | 110 |
| Casa Paula | 22.6 | 31 | 100 |
| Casa Matilde | 25 | 28 | 73 |
| Casa Amiga | 0 | 36 | 72 |
| Casa de la Mujer | 0 | 27 | 55 |
| Casa Hogar de Nazareth | 7.9 | 38 | 37 |
| Casa Manos Unidas | 4.8 | 21 | 30 |
| Ibarra Shelter | 14.8 | 27 | NA |
| Cotacachi Shelter | 30.8 | 13 | NA |
| Refuges Lago Agrio | 20 | 100 | NA |
SARS-CoV-2 infection attack and shelter occupation rates
The occupation rates for the different shelters with the available information are detailed in Table 1. Although there are significant differences (p < 0.05) in the SARS-CoV-2 attack rates for different shelters, no significant linear correlation was found with the number of individuals at the shelter or the occupation rate (R = 0.36, p = 0.39, 95% CI −0.466, 0.848).
Discussion
Since the early stage of the COVID-19 pandemic in Ecuador, the strategy for prevention or mitigation of the impact of COVID-19 displayed by the Ministry of Health was limited to test symptomatic patients attending hospital facilities. Moreover, despite huge efforts from the National Reference Laboratories for SARS-CoV-2 surveillance from “Instituto Nacional de Salud Pública e Investigación” to keep up the diagnosis, a limited daily testing capacity below 200 PCR tests per million habitants was installed across the country (Ortiz-Prado et al., 2021c, Torres and Sacoto, 2020). However, the few reports about the epidemiological situation of SARS-CoV-2 among vulnerable populations suggest that community transmission has been happening since the population lockdown was lifted in June 2020 in Ecuador (Ortiz-Prado et al., 2021a, Ortiz-Prado et al., 2021b, Ortiz-Prado et al., 2021d, Freire-Paspuel et al., 2020a, Del Brutto et al., 2020). Under this scenario, in collaboration with UNHCR, this surveillance program was implemented at shelters for women victims of gender-based violence, and COVID-19 outbreaks were reported at nine out of 11 shelters visited. It is believed that this is the first publication to date addressing SARS-CoV-2 surveillance at shelters for women victims of gender-based violence.
After the arrival of the SARS-CoV-2 infection to Ecuador, a study revealed that women were less prone to acquire the infection compared with men (Ortiz-Prado et al., 2021c). This is in accordance with the findings in the overall SARS-CoV-2 attack rates for males and females in the current study. The overall high SARS-CoV-2 attack rate of 12.65% is also in agreement with other reports showing SARS-CoV-2 community transmission among community-dwelling individuals in Ecuador (Ortiz-Prado et al., 2021a, Ortiz-Prado et al., 2021b, Ortiz-Prado et al., 2021d, Freire-Paspuel et al., 2020a, Del Brutto et al., 2020).
A wide variety of studies sustain the idea that crowded household settings constitute an important site for COVID-19 outbreaks (Del Brutto et al., 2020, Leclerc et al., 2020, Ortiz-Prado et al., 2020, Rothan and Byrareddy, 2020, Madewell et al., 2020, Karb et al., 2020, Ly et al., 2021). The current study showed that nine of 11 shelters had active COVID-19 outbreaks, confirming that these kind of facilities are at high risk for SARS-CoV-2 transmission. However, a clear relationship between the occupancy level of each shelter and the attack rates was not found; those rates varied from 0 to 30.8%. The characteristics of the shelters could explain such variations in attack rates, as the majority of shelters participating in the screening were “long-stay shelters” and the rotation of housed people was low, the exposure of each resident or working-staff being lower in comparison with “short-stay shelters”. In fact, one study performed in Rhode Island (USA) found that homeless shelters in densely populated areas with more transient resident populations had more SARS-CV-2 incidences than shelters with stable residents. The same study recommended resident stability to reduce COVID-19 cases (Karb et al., 2020). Nevertheless, another study carried out at shelters in France also suggested the risk of collective housing for SARS-CoV-2 transmission and found a SARS-CoV-2 attack rate of 7% (Ly et al., 2021). Interestingly, the current study described how the occupation of some included shelters reached or even surpassed the shelter capacity, according to data provided by UNHCR. Considering that COVID-19 outbreaks were found at most of the shelters, recurrent screening for SARS-CoV-2 infection should be implemented.
Regarding the gender approach of this study, most of women included in this study were victims of gender-based violence, which increased during the strict lockdown implemented in the country. In addition to this, gender inequalities have deepened during COVID-19, which is reflected not only in the increase in gender-based violence, but also in worst posttraumatic stress effects after lockdown, or a deeper aftermath from SARS-CoV-2 infection (Silveira Campos et al., 2020, Ayittey et al., 2021). Studies like the current one have been recommended to prevent a deeper impact of the COVID-19 pandemic and guarantee health rights for women victims of gender-based violence (Ayittey et al., 2021).
The main limitation of this study is the fact that sampling took place only at one time point during the highest peak of the pandemic in Ecuador. Additional screening months after the first one would be useful to assess the dynamics of the infection in such humanitarian settings and implement control strategies to prevent the spread; however, a lack of funds did not allow this project to continue. Further prevention strategies in shelters for women and children could include: opportune case reports, mass testing for control of existing cases, proper isolation of affected residents wherever the infrastructure allows it as new residents are accepted, and testing for routine control of staff who are highly exposed (PAHO et al., 2020).
In conclusion, this study constitutes an important report to show the epidemiological situation of COVID-19 in humanitarian shelters in Latin America. Moreover, the findings endorse the importance of mass testing in the prevention of COVID-19 outbreaks, and the importance of closing the breach in SARS-CoV-2 testing, making them accessible to disadvantaged sectors of society.
Ethical approval and consent to participate
Written consent was obtained for all the individuals included in the surveillance. The study is included on a project that was approved by IRB from Universidad de Las Américas.
Consent for publication
Not applicable.
Availability of supporting data
Not applicable.
Competing interests
The authors declare no conflict of interest.
Funding
This study was supported by Fundación CRISFE (Fondo Sumar Juntos) and Universidad de Las Américas.
Authors’ contributions
All authors contributed to data collection and analysis. MAGB and PVJ wrote the manuscript.
Acknowledgments
We thank all the shelters residents and staff for the support to carry out this study. We also thanks to “Universidad de Las Américas” for their support to implement SARS-CoV-2 testing at our facilities.
Contributor Information
on behalf of the UDLA COVID-19 team:
Esteban Ortiz-Prado, Ismar Rivera-Olivero, Aquiles Rodrigo Henriquez, Tatiana Jaramillo, Daniela Santander Gordon, Gabriel Alfredo Iturralde, Julio Alejandro Teran, Karen Marcela Vasquez, Jonathan Dario Rondal, Genoveva Granda, Ana Cecilia Santamaria, Cynthia Lorena Pino, Oscar Lenin Espinosa, Angie Buitron, David Sanchez Grisales, Karina Beatriz Jimenez, Heberson Galvis, Barbara Coronel, Vanessa Bastidas, Dayana Marcela Aguilar, Ines Maria Paredes, Christian David Bilvao, Maria Belen Paredes-Espinosa, Angel S. Rodriguez, Juan Carlos Laglaguano, Henry Herrera, Pablo Marcelo Espinosa, Edison Andres Galarraga, Marlon Steven Zambrano-Mila, Ana Maria Tito-Alvarez, and Nelson David Zapata
References
- Ayittey F.K., Dhar B.K., Anani G., Chiwero N.B. Gendered burdens and impacts of SARS-CoV-2: a review. Health Care Women Int. 2021;41(11–12):1210–1225. doi: 10.1080/07399332.2020.1809664. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33616506. [cited 12 March 2021] [DOI] [PubMed] [Google Scholar]
- CDC . 2021. Interim guidelines for collecting and handling of clinical specimens for COVID-19 testing; pp. 3–8. [Google Scholar]
- Del Brutto O.H., Costa A.F., Mera R.M., Recalde B.Y., Bustos J.A., García H.H. Household clustering of SARS-CoV-2 in community settings: a study from rural Ecuador. Am J Trop Med Hyg. 2020;103(September (3)):1207–1210. doi: 10.4269/ajtmh.20-0688. Available from: https://www.ajtmh.org/view/journals/tpmd/103/3/article-p1207.xml. [cited 11 March 2021] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire-Paspuel B., Garcia-Bereguiain M.A. Poor sensitivity of “AccuPower SARS‑CoV‑2 real time RT‑PCR kit (Bioneer, South Korea)”. Virol J. 2020;17(178) doi: 10.1186/s12985-020-01445-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire-Paspuel B., Garcia-Bereguiain M.A. Analytical sensitivity and clinical performance of a triplex RT-qPCR assay using CDC N1, N2, and RP targets for SARS-CoV-2 diagnosis. Int J Infect Dis. 2021;102:14–16. doi: 10.1016/j.ijid.2020.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire-Paspuel B., Vega-Mariño P., Velez A., Castillo P., Masaquiza C., Cedeño-Vega R. “One health” inspired SARS-CoV-2 surveillance: the Galapagos Islands experience. One Health. 2020;11(December) doi: 10.1016/j.onehlt.2020.100185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire-Paspuel B., Vega-Mariño P., Velez A., Castillo P., Cruz M., Garcia-Bereguiain M.A. Evaluation of nCoV-QS (MiCo BioMed) for RT-qPCR detection of SARS-CoV- 2 from nasopharyngeal samples using CDC FDA EUA qPCR kit as a gold standard: an example of the need of validation studies. J Clin Virol. 2020;128(May):104454. doi: 10.1016/j.jcv.2020.104454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire-Paspuel B., Vega-Mariño P., Velez A., Cruz M., Garcia-Bereguiain M.A. Sample pooling of RNA extracts to speed up SARS-CoV-2 diagnosis using CDC FDA EUA RT-qPCR kit. Virus Res. 2020;290 doi: 10.1016/j.virusres.2020.198173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire-Paspuel B., Vega-Mariño P., Velez A., Castillo P., Gomez-Santos E.E., Cruz M. Cotton-tipped plastic swabs for SARS-CoV-2 RT-qPCR diagnosis to prevent supply shortages. Front Cell Infect Microbiol. 2020;10(June):1–4. doi: 10.3389/fcimb.2020.00356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire-Paspuel B., Vega-Mariño P., Velez A., Cruz M., Perez F., Garcia-Bereguiain M.A. Analytical and clinical comparison of Viasure (CerTest Biotec) and 2019-nCoV CDC (IDT) RT-qPCR kits for SARS-CoV2 diagnosis. Virology. 2021;553(October 2020):154–156. doi: 10.1016/j.virol.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inter-Agency Standing Committee (IASC) Inter-Agency Standing Committee; 2020. Interim guidance: public health and social measures for COVID-19 preparedness and response in low capacity and humanitarian settings - Version 1. [Google Scholar]
- Karb R., Samuels E., Vanjani R., Trimbur C., Napoli A. Homeless shelter characteristics and prevalence of SARS-CoV-2. West J Emerg Med. 2020;21(5):1048–1053. doi: 10.5811/westjem.2020.7.48725. [cited 12 March 2021] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leclerc Q.J., Fuller N.M., Knight L.E., Funk S., Knight G.M. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Res. 2020;5 doi: 10.12688/wellcomeopenres.15889.1. Available from: https://pubmed.ncbi.nlm.nih.gov/32656368/. [cited 11 March 2021] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu X., Wang L., Sakthivel S.K., Whitaker B., Murray J., Kamili S. US CDC real-time reverse transcription PCR panel for detection of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(8):1654–1665. doi: 10.3201/eid2608.201246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ly T.D.A., Nguyen N.N., Hoang V.T., Goumballa N., Louni M., Canard N. Screening of SARS-CoV-2 among homeless people, asylum-seekers and other people living in precarious conditions in Marseille, France, March–April 2020. Int J Infect Dis. 2021;105(April):1–6. doi: 10.1016/j.ijid.2021.02.026. Epub 2021 Feb 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madewell Z.J., Yang Y., Longini I.M., Halloran M.E., Dean N.E. Household transmission of SARS-CoV-2 A systematic review and meta-analysis + supplemental content. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31756. Available from: https://jamanetwork.com/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Prado E., Simbaña-Rivera K., Gómez- Barreno L., Rubio-Neira M., Guaman L.P., Kyriakidis N.C. Clinical, molecular, and epidemiological characterization of the SARS-CoV-2 virus and the Coronavirus Disease 2019 (COVID-19), a comprehensive literature review. Diagn Microbiol Infect Dis. 2020;98(September (1)):115094. doi: 10.1016/j.diagmicrobio.2020.115094. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0732889320304715. [cited 11 March 2021] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Prado E., Henriquez-Trujillo A.R., Rivera-Olivero I.A., Freire-Paspuel B., Vallejo-Janeta A.P., Lozada T. Massive SARS-CoV-2 RT-PCR testing on rural communities in Manabi Province (Ecuador) reveals severe COVID-19 outbreaks. Am J Trop Med Hyg. 2021:1–2. doi: 10.4269/ajtmh.20-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Prado Esteban, Rivera-Olivero Ismar A, Freire-Paspuel Byron, Lowe Rachel, Lozada Tannya, Henriquez-Trujillo Aquiles R. Testing for SARS-CoV-2 at the core of voluntary collective isolation: lessons from the indigenous populations living in the Amazon region in Ecuador. Int J Infect Dis. 2021;105(February):234–235. doi: 10.1016/j.ijid.2021.02.039. [DOI] [PubMed] [Google Scholar]
- Ortiz-Prado E., Simbaña-Rivera K., Gómez Barreno L., Diaz A.M., Barreto A., Moyano C. Epidemiological, socio-demographic and clinical features of the early phase of the COVID-19 epidemic in Ecuador. PLoS Negl Trop Dis. 2021;15(1):1–18. doi: 10.1371/journal.pntd.0008958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Prado Esteban, Henriquez-Trujillo Aquiles R., Rivera-Olivero Ismar A., Lozada Tannya, Garcia-Bereguiain Miguel Angel, on behalf of the UDLA-COVID-19 Team High prevalence of SARS-CoV-2 infection among food delivery riders. A case study from Quito, Ecuador. Sci Total Environ. 2021;770 doi: 10.1016/j.scitotenv.2021.145225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PAHO, UNFPA, Women U. 2020. COVID-19 infection prevention and control in shelters for women and children survivors of domestic and family violence in the Caribbean. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [cited 12 March 2021] [Google Scholar]
- PAHO. 2021. https://www.paho.org/es/documentos/actualizacion-epidemiologica-nuevo-coronavirus-covid-19-28-febrero-2020.
- Peate I. Self-isolation and the homeless population. Br J Nurs. 2020;29(7):2021. doi: 10.12968/bjon.2020.29.7.387. [DOI] [PubMed] [Google Scholar]
- Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109(May) doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silveira Campos L., Brigagão de Oliveira M., Peixoto Caldas J.M. COVID 19: sexual vulnerabilities and gender perspectives in Latin America. Health Care Women Int. 2020;41(11–12):1207–1209. doi: 10.1080/07399332.2020.1833884. Epub 2020 Nov 10. [DOI] [PubMed] [Google Scholar]
- Torres I., Sacoto F. Localising an asset-based COVID-19 response in Ecuador. Lancet. 2020;395(10233):1339. doi: 10.1016/S0140-6736(20)30851-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Ma H., Yiu K.C.Y., Calzavara A., Landsman D., Mph L.L. Heterogeneity in testing, diagnosis and outcome in SARS-CoV-2 infection across outbreak settings in the Greater Toronto Area, Canada: an observational study. Can Med Assoc J Open. 2020;8(4):627–636. doi: 10.9778/cmajo.20200213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood L.J., Davies A.P., Khan Z. COVID-19 precautions: easier said than done when patients are homeless. Med J Aust. 2020;212(8):384–385. doi: 10.5694/mja2.50571. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.