Supplemental Digital Content is available in the text.
Key Words: Affordable Care Act, Medicaid expansion, health care workforce, physician geographical distribution
Background:
Some states expanded Medicaid under the Affordable Care Act, boosting their low-income residents’ demand for health care, while other states opted not to expand.
Objective:
The objective of this study was to determine whether the Medicaid expansion influenced the states selected by physicians just completing graduate medical education for establishing their first practices.
Research Design:
Using 2009–2019 data from the American Medical Association Physician Masterfile and information on states’ Medicaid expansion status, we estimated conditional logit models to compare where new physicians located during the 6 years following implementation of the expansion to where they located during the 5 years preceding implementation.
Subjects:
The sample consisted of 160,842 physicians in 8 specialty groups.
Results:
Thirty-three states and the District of Columbia expanded Medicaid by the end of the study period. Compared with preexpansion patterns, we found that physicians in one specialty group—general internal medicine—were increasingly likely to locate in expansion states with time after the expansion. The Medicaid expansion influenced the practice location choices of men and international medical graduates in general internal medicine; women and United States medical graduates did not alter their preexpansion location patterns. Simulations estimated that, between 2014 and 2019, nonexpansion states lost 310 general internists (95% confidence interval, 156–464) to expansion states.
Conclusions:
The Medicaid expansion influenced the practice location choices of new general internists. States that opted not to expand Medicaid under the Affordable Care Act lost general internists to expansion states, potentially affecting access to care for all their residents irrespective of insurance coverage.
The Affordable Care Act (ACA) has increased health insurance coverage for working-age adults through 2 main provisions: the health insurance marketplaces, where individuals can purchase subsidized private insurance, and the expansion of Medicaid coverage to adults with incomes below 138% of the federal poverty line. Recent data indicate that 11.4 and 15.6 million Americans obtain coverage through the marketplaces and the Medicaid expansion, respectively.1,2
Initially intended to be mandatory for states, the Medicaid expansion was rendered optional by a Supreme Court decision in 2012.3 Twenty-four states and the District of Columbia expanded Medicaid in January 2014 and several others have expanded since, resulting in gains in insurance coverage and improved access to care and health status among their low-income, working-age residents.4–7 However, less is known about the ACA’s effects on physicians.
Of particular interest is whether the ACA’s effects on the demand for care have influenced the geographical distribution of physicians, which could have implications for access to care. Previous theoretical and empirical research has established that demand is the most important determinant of physicians’ practice location choices.8,9 Although both the insurance marketplaces and the Medicaid expansion increased demand, the former is unlikely to have affected physicians’ geographical distribution, since all states participated in the marketplaces. By contrast, the Medicaid expansion represented a “demand shock” that boosted demand in expansion states relative to nonexpansion states. A recent study documented how health care organizations in 5 Medicaid expansion states were responding to the increased demand for care by attempting to recruit additional primary care physicians and medical subspecialists.10
The objective of this study was to assess whether the Medicaid expansion influenced the choice of states where new physicians, defined as those just completing graduate medical education (GME), established their first practices. We hypothesized that new family physicians, general internists, and medical subspecialists were more likely to locate in Medicaid expansion states following the expansion. To our knowledge, this is the first study to examine the effects of the ACA on the geographical distribution of physicians.
MATERIALS AND METHODS
Study Population
We identified new physicians who established their first practices in the 50 states or the District of Columbia between 2009 and 2019 using the American Medical Association (AMA) Physician Masterfile. We used the physician-reported primary specialty in the Masterfile to classify physicians into 8 specialty groups: family medicine, general internal medicine, medical subspecialties (eg, cardiology, gastroenterology), general pediatrics, pediatric subspecialties, general surgery, surgical specialties (eg, ophthalmology, orthopedic surgery), and obstetrics and gynecology. We excluded hospital-based specialties (eg, hospital medicine, anesthesiology), psychiatry, dermatology, and neurology due to small numbers or to anticipated differences in the determinants of practice location.
Using the year-end data from the Masterfile for 2009–2019, we selected physicians whose main professional activity was direct patient care and who had completed their most recent GME (residency or fellowship) 2.5 years earlier. For example, among physicians in practice at the end of 2019, we selected those who had completed their most recent GME in 2017 (typically in June) and defined their practice at the end of 2019 as their first practice. The 2.5-year interval allowed time for more complete updating of practice address data (see below), served to exclude physicians who practiced for a brief period after residency but subsequently entered fellowships and enabled us to bypass the temporary jobs some new physicians may take while searching for stable practice opportunities.11
Next, we identified the state of each physician’s first practice using the most recently updated practice address in the Masterfile or the Center for Medicare and Medicaid Services National Plan and Provider Enumeration System, provided the update had occurred at most 3 years before the year of practice. If neither practice address was updated in this interval, we used the mailing address in the Masterfile. Of the assigned practice addresses, 34.3%, 62.8%, and 87.8% were updated within the prior year, 2, and 3 years, respectively. The remaining 12.2% were mailing addresses. About 0.4% of physicians were missing addresses and were excluded.
Other Data Sources
We obtained states’ Medicaid expansion dates from the Kaiser Family Foundation Web site.12 Twenty-four states and the District of Columbia implemented the Medicaid expansion on January 1, 2014, and 9 additional states on subsequent dates through 2019 (Online Appendix A, Supplemental Digital Content 1, http://links.lww.com/MLR/C193). We assigned the expansion year as the year of the expansion date if the date fell before July 1 and as the subsequent year if it fell after June 30.
We obtained state-level data on population characteristics from the 1-year American Community Survey (ACS) estimates,13 on states’ decisions to continue the “bump” in Medicaid primary care fees after the national bump expired in 2015 from a published report,14 and on malpractice reforms (caps on punitive and noneconomic damages) and nurse practitioner scope of practice laws from other sources.15,16
Statistical Methods
Our goal was to assess whether the probability that new physicians located in a Medicaid expansion state changed after the expansion while accounting for state characteristics and for the fact that states expanded in different years. Consequently, we used the conditional logit regression model, which was developed to analyze situations in which subjects make a single choice (eg, a state) from a set of alternatives.17 The estimated coefficients from the model can be used to predict the probability that each physician locates in each state.
We estimated separate models for each of the 8 specialty groups, with individual physicians as the unit of analysis and physicians’ choice of state as the dependent variable. The independent variables were state fixed effects (ie, an indicator variable for each state), which capture measurable and unmeasurable state characteristics that are constant over time; indicator variables for whether the physician was born, attended medical school, and completed GME in the state; and, for family medicine, general internal medicine, and general pediatrics, an indicator variable for whether the state continued the Medicaid primary care fee bump after 2014.
Because the expansion year varied across states, we captured Medicaid expansion effects by including, for each state that expanded Medicaid during the study period, separate indicator variables for each of the 5 (or more) years preceding the expansion year and each of the 6 years (or fewer) following the expansion. (The indicators were always zero for nonexpansion states.) To enable estimation, we constrained the average of the coefficients of the indicators for the 5 years preceding the expansion to equal zero. This “event study” specification provided full flexibility in the modeling. Further, each expansion state served as its own control; that is, the expansion effect was estimated by comparing the odds that physicians located in a state before and after the expansion. Specifically, the antilogarithm of the estimated coefficient of each year’s indicator can be interpreted as an odds ratio (OR), namely, the odds that physicians located in an expansion state in the particular year divided by the average odds that they located in the state during the 5 years preceding the expansion. Thus an OR=1.0 (>1.0) in a particular year means that physicians were equally likely (more likely) to locate in an expansion state in that year than they were, on average, during the preexpansion period (Online Appendix B has a detailed description of the model, Supplemental Digital Content 1, http://links.lww.com/MLR/C193).
To facilitate comparisons and statistical testing, we also estimated models in which we used a single indicator variable for the 6 years following the Medicaid expansion, rather than a separate indicator for each year. The antilogarithm of the estimated coefficient of this indicator can be interpreted as the average odds that physicians located in an expansion state during the 6 years following the expansion divided by the average odds that they located in an expansion state during the 5 years preceding the expansion. For brevity, we refer to this OR as the average 6-year postexpansion OR. We explored including state population characteristics in the models, but these variables were either relatively constant over the study period, and consequently collinear with the state fixed effects, or changed by similar amounts in every state (Online Appendix C, Supplemental Digital Content 1, http://links.lww.com/MLR/C193). The conditional logit model cannot estimate the effect of variables that change by a similar amount for every alternative because such changes do not affect the choice probabilities. We return to this point in the Results section.
We used the event study specification to conduct 3 sensitivity analyses: (1) using data for 2007–2019 to extend the preexpansion period; (2) adding indicators for caps on punitive and noneconomic damages, and for full nurse practitioner scope of practice to the models; and (3) ascertaining first practice addresses 1.5 years after GME completion (rather than 2.5 y). To facilitate comparisons, these models used a single indicator variable for the 6 years following the Medicaid expansion. Finally, we conducted stratified analyses to assess whether the effects of the Medicaid expansion differed between men and women and between physicians who graduated from the United States or Canadian medical school graduates (USMGs) and those who graduated from medical schools in other countries (international medical graduates, or IMGs). We estimated all models using Stata, version 14.2 and used the robust sandwich estimator to obtain SEs and confidence intervals (CIs).18 For the models that employed a single indicator variable for the 6 postexpansion years, we calculated adjusted P-values, accounting for multiple hypothesis testing across the 8 specialty groups, using the Hochberg method.19
Simulations
We used the estimated conditional logit regression coefficients to predict the number of new physicians who would establish their first practice in each state under 2 scenarios: (1) the observed patterns of Medicaid expansion across the states; and (2) a hypothetical alternative in which all states expanded on January 1, 2014. We aggregated the predicted numbers across actual expansion and nonexpansion states to determine how many physicians were gained or lost (Online Appendix G explains the simulation methods in detail, Supplemental Digital Content 1, http://links.lww.com/MLR/C193). We obtained SEs for the predictions using the delta method.20
RESULTS
Descriptive Data
Total sample sizes ranged from 6232 for general surgery to 39,288 for medical subspecialties (Table 1). Annual sample sizes declined from 2009 through 2019 for general pediatrics and obstetrics/gynecology but rose for the other 6 specialty groups, although at different rates (Online Appendix D, Supplemental Digital Content 1, http://links.lww.com/MLR/C193). The mean age was in the mid-30s for every specialty group, whereas the percentage of women and the percentage of IMGs varied substantially across groups (Table 1).
TABLE 1.
Sample Sizes and Descriptive Data for Study Sample, by Specialty Group
| Characteristic | Family Medicine | General Internal Medicine | Medical Subspecialties | General Pediatrics | Pediatric Subspecialties | General Surgery | Surgical Specialties | Obstetrics/Gynecology |
|---|---|---|---|---|---|---|---|---|
| Total sample size | 26,049 | 32,102 | 39,288 | 13,337 | 8712 | 6232 | 25,020 | 10,102 |
| Age [mean (SD)] | 35.9 (5.4) | 35.2 (4.6) | 36.8 (3.7) | 33.9 (3.8) | 36.8 (3.4) | 36.0 (3.9) | 35.9 (3.3) | 34.7 (3.6) |
| Gender (%) | ||||||||
| Men | 44.6 | 50.8 | 62.2 | 22.4 | 40.9 | 67.4 | 76.7 | 20.2 |
| Women | 55.4 | 49.2 | 37.8 | 77.6 | 59.1 | 32.6 | 23.3 | 79.8 |
| Country of medical school (%) | ||||||||
| USMG | 56.6 | 47.5 | 54.7 | 76.1 | 67.2 | 76.0 | 90.9 | 80.5 |
| IMG | 43.4 | 52.5 | 45.3 | 23.9 | 32.8 | 24.0 | 9.1 | 19.5 |
IMG indicates international medical graduate; USMG, United States medical school graduate.
About 57.2% of new physicians in the 8 specialty groups combined established their first practices in Medicaid expansion states in 2014, the first year of the expansion. This percentage rose gradually as additional states expanded, reaching 69.4% in 2019. The precise figures differed slightly across specialty groups, but the patterns were similar.
Effects of the Medicaid Expansion
The results of our event study models by specialty group are presented in Figure 1. The horizontal axis indexes years before (years −5 to −1) and after (years 1–6) the Medicaid expansion for each state that expanded during the study period. For example, the year “−1” is the year just before the expansion, that is, 2013 for states that expanded in 2014. Analogously, the year “1” is the first year of the expansion, that is, 2014 for states that expanded in 2014. The vertical axis indicates the OR, as defined earlier. The figure shows the point estimates for the ORs as well as 95% CIs.
FIGURE 1.
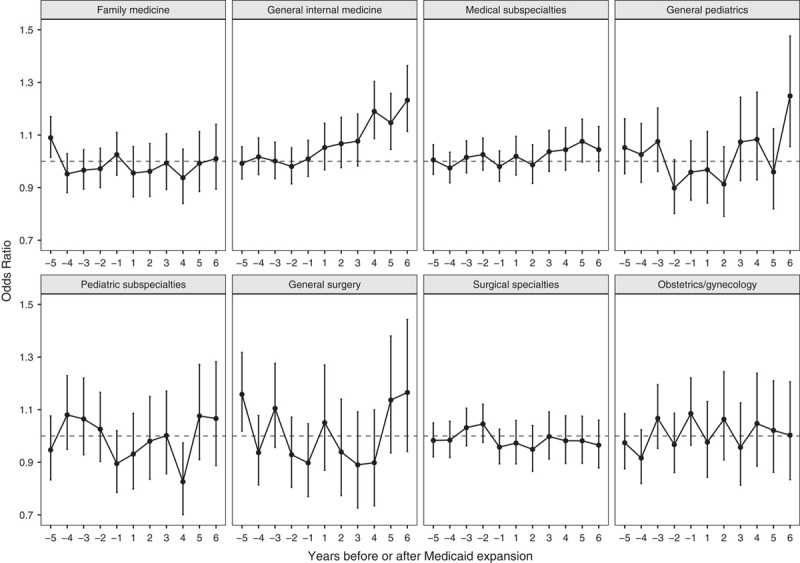
Odds of new physicians locating in a Medicaid expansion state in each preexpansion and postexpansion year relative to the average odds of locating in those states over 5 preexpansion years, by specialty group. Years −5 to −1 indicate preexpansion years and years 1–6 indicate postexpansion years. The graph shows the point estimate and 95% confidence interval for the odds ratio in each year. An odds ratio=1.0 in a particular year means that physicians were equally likely to locate in an expansion state in that year than they were, on average, during the preexpansion period. An odds ratio >1.0 in a particular year means that physicians were more likely to locate in an expansion state in that year than they were, on average, during the preexpansion period.
There was no discernible trend in ORs in the preexpansion years (years −5 to −1) for any of the 8 specialty groups (Fig. 1), and the null hypothesis that the 5 preexpansion ORs were simultaneously equal to 1.0 was not rejected for any specialty group (Online Appendix E, Supplemental Digital Content 1, http://links.lww.com/MLR/C193). Thus, before the Medicaid expansion, there were no trends toward either rising or declining numbers of new physicians locating in states that subsequently expanded.
Similarly, there was no consistent trend in ORs in the postexpansion years (years 1–6) for 7 of the 8 specialty groups (Fig. 1). By contrast, the postexpansion ORs progressively increased for general internal medicine, and the 95% CIs for the last 3 expansion years excluded 1.0. The ORs in the fourth, fifth, and sixth postexpansion years were 1.19 (95% CI, 1.09–1.30), 1.15 (95% CI, 1.05–1.26), and 1.23 (95% CI, 1.11–1.36), respectively. The 95% CI of the OR for general pediatrics in the sixth postexpansion year excluded 1.0 (Fig. 1), but this estimate does not appear to be part of a consistent postexpansion trend (Online Appendix E has full regression results, Supplemental Digital Content 1, http://links.lww.com/MLR/C193).
The average 6-year postexpansion OR for general internal medicine was 1.11 (95% CI, 1.05–1.17; P<0.001; adjusted P<0.001). The average 6-year postexpansion OR did not differ from 1.0 for any other specialty group including general pediatrics.
The findings of the 3 sensitivity analyses were qualitatively identical and quantitatively similar to the findings of our main analyses (Online Appendix F, Supplemental Digital Content 1, http://links.lww.com/MLR/C193).
Assessment of Confounding: Trends in Other Demand Determinants
As noted earlier, we could not control for state-level population characteristics in our models because of collinearity with the state fixed effects. Nonetheless, we were concerned that there may have been small differences in population trends between expansion and nonexpansion states that, while too small to mitigate collinearity, could have resulted in differential changes in demand and accounted for our findings that new general internists increasingly located in expansion states after 2014. Newhouse and colleagues8,9 have shown that population and population growth are key determinants of physician location. In fact, however, between 2013 and 2018 total population and every component thereof—whether defined by age, gender, race and ethnicity, educational attainment, poverty status, or nativity—either grew faster in nonexpansion than in expansion states, grew in nonexpansion states while declining in expansion states, or fell more slowly in nonexpansion states (Table 2). Similarly, the number of working-age adults with health insurance from sources other than Medicaid grew faster in nonexpansion states. (As expected, the number of working-age adults with Medicaid coverage grew much more quickly in expansion states.) Per capita income grew faster in expansion than in nonexpansion states, but the difference was negligible (Table 2). Therefore, aside from sharper increases in Medicaid coverage in expansion states, every other determinant of health care demand grew faster in nonexpansion states.
TABLE 2.
Percent Changes in Demand Determinants in Medicaid Expansion and Nonexpansion States, 2013–2018
| Variable | Expansion States (%) | Nonexpansion States (%) |
|---|---|---|
| Total population | 2.2 | 5.6 |
| By age (y) | ||
| <5 | −1.6 | 0.7 |
| 5–19 | −1.9 | 2.8 |
| 20–64 | 1.8 | 5.2 |
| >64 | 11.4 | 13.7 |
| By gender | ||
| Men | 2.3 | 5.5 |
| Women | 2.1 | 5.6 |
| By educational attainment (>24 y old) | ||
| No high school degree | −10.9 | −8.5 |
| High school degree, no college degree | −0.3 | 3.7 |
| Bachelor’s degree or higher | 12.5 | 16.6 |
| By race and ethnicity | ||
| Non-Hispanic White | −1.3 | 1.7 |
| Non-Hispanic Black | 2.2 | 5.6 |
| Hispanic | 8.4 | 14.5 |
| Other non-Hispanic minorities | 14.5 | 21.5 |
| By nativity | ||
| US-born | 1.6 | 4.6 |
| Foreign-born | 5.7 | 13.4 |
| By poverty status | ||
| Poor | −15.4 | −12.6 |
| Nonpoor | 5.4 | 9.2 |
| By age and insurance status | ||
| <20 y old | ||
| Uninsured | −35.2 | −11.2 |
| Insurance other than Medicaid | 3.9 | 11.6 |
| Medicaid | 8.6 | 6.2 |
| 20–64 y old | ||
| Uninsured | −50.1 | −25.0 |
| Insurance other than Medicaid | 3.3 | 10.9 |
| Medicaid | 44.8 | 5.5 |
| Per capita income | 20.6 | 19.4 |
Our descriptive findings imply that, in the absence of the Medicaid expansion, demand would have grown faster in nonexpansion than expansion states. They suggest that our results were not due to confounding from trends in demand determinants.
Differential Effects by Physician Gender and Country of Medical School
The effect of the Medicaid expansion on general internal medicine was driven by men and by IMGs, who showed progressively increasing ORs in the postexpansion years (Fig. 2). Women and USMGs, by contrast, showed no discernible trend in the postexpansion ORs. The average 6-year postexpansion OR for men was 1.15 (95% CI, 1.06–1.24; P<0.001; adjusted P<0.001), which differed significantly (P<0.001; adjusted P=0.005) from the average postexpansion OR for women of 1.07 (95% CI, 0.98–1.16; P=0.129). Analogously, the average 6-year postexpansion OR for IMGs was 1.13 (95% CI, 1.05–1.21; P<0.001; adjusted P=0.008), which differed significantly (P=0.001; adjusted P=0.011) from the OR for USMGs of 1.06 (95% CI, 0.97–1.16; P=0.205). Additional analyses found that the Medicaid expansion had similar effects on foreign-born and US-born IMGs.
FIGURE 2.
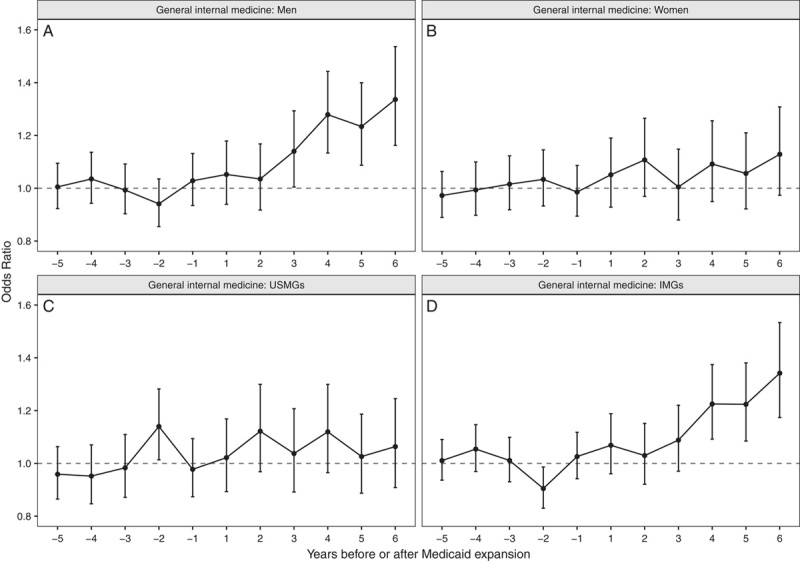
Odds of new general internists locating in a Medicaid expansion state in each preexpansion and postexpansion year relative to the average odds of locating in those states over 5 preexpansion years, by gender (A, B) and by country of medical school (C, D). IMG indicates international medical graduate; USMG, United States medical school graduate.
Other Regression Findings
The indicator variables for whether the physician was born, attended medical school and completed GME in a state had by far the strongest effects on physician location. In addition, general internists were more likely to locate in states that continued the Medicaid primary care fee bump after 2014 (Online Appendix E, Supplemental Digital Content 1, http://links.lww.com/MLR/C193).
Simulations
Our simulations found that, between 2014 and 2019, 310 general internists (95% CI, 156–464) who would have established practices in nonexpansion states if every state had expanded Medicaid in 2014 opted instead to establish practices in expansion states (Fig. 3). Further, their numbers generally rose through the postexpansion period. These figures represent 1.6% (95% CI, 0.8%–2.5%) of all new general internists who established practices between 2014 and 2019. For 2017, 2018, and 2019, the figures represent 2.3% (95% CI, 1.1%–3.5%), 1.9% (95% CI, 0.7%–3.1%), and 2.5% (95% CI, 1.4%–3.5%), respectively, of new general internists who established practices in those years.
FIGURE 3.
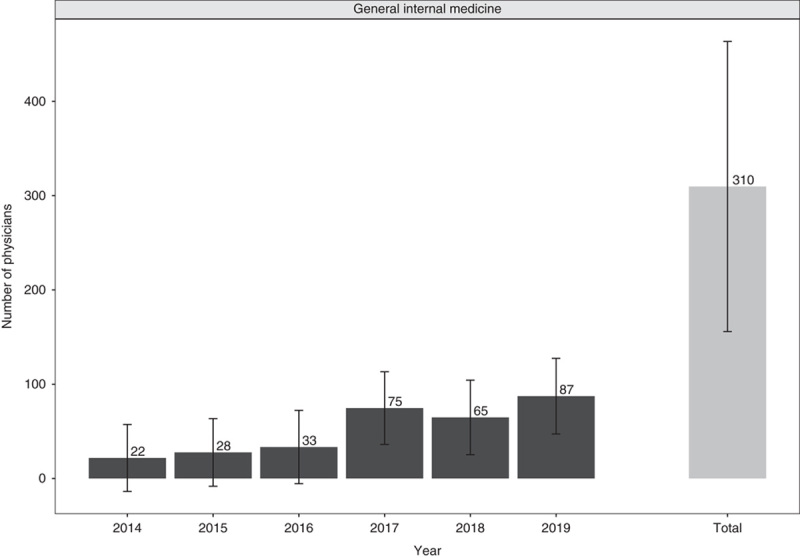
Simulated number of new general internists gained by Medicaid expansion states (and lost by nonexpansion states), by calendar year and total for 2014–2019. The graph shows point estimates and 95% confidence intervals for the simulated numbers of physicians.
DISCUSSION
Our study found that the decision of some states to expand Medicaid under the ACA, while other states rejected the expansion resulted in higher numbers of new general internists establishing their first practices in expansion states than if every state had expanded. The number of additional general internists who located in expansion states grew over time following 2014. Our findings are consistent with the documented impact of the ACA and the Medicaid expansion on health care providers and organizations and their responses. A 2016 national survey of physicians found that between 2012 and 2016 physicians‘ average share of Medicaid patients grew and their average share of uninsured patients declined in Medicaid expansion states but did not change in nonexpansion states.21 Many primary care physicians in Michigan, an expansion state, reported higher patient volume and increased patient complexity following ACA implementation. Nearly half said the time available to spend with patients had declined.22 These are the types of pressures that could lead health care organizations to recruit more clinicians.
Indeed, interviews in 2017 with stakeholders in 5 Medicaid expansion states found that both private health systems and community health centers responded to the increased demand for care by attempting to recruit more physicians and advanced practice clinicians, expanding facilities and hours, and opening new clinical sites. Physician recruitment focused on primary care physicians and medical specialists.10 On the basis of these reports, we had expected that family physicians and medical subspecialists would respond to the Medicaid expansion similarly to general internists. A possible explanation for our findings is that widespread physician shortages made it difficult to attract physicians to new locations since they are in high demand in many places.23 Under these circumstances, health care organizations might have opted to focus recruitment efforts on general internists, whose training includes significant experience in both primary care and medical subspecialties.24 Additional advanced practice clinicians recruited to provide primary care by health care organizations, and especially community health centers, in expansion states10 might have been stronger substitutes for family physicians than for general internists.25,26 These results warrant further research.
We found that the effect of the Medicaid expansion on general internists was driven by men and IMGs. Gendered responses to the expansion can be understood in the context of research findings that mixed-gender couples are more likely to move to improve the man’s occupational opportunities than the woman’s and that the man’s potential loss from a move deters the woman from capitalizing on job opportunities at a new location but not vice versa.27–29 These tendencies are enhanced when the man has a high-paying job or the couple has children.29 Notably, the spouses of female physicians have higher educational attainment, are much more likely to have paid employment, and earn much more than the spouses of male physicians.30 Female physicians also make more professional adjustments to accommodate household responsibilities and care for children.31 Our findings for IMGs in general internal medicine are consistent with these physicians’ long-standing propensity to care for underserved patients.32,33
Drawing causal inferences from observational data is challenging because of the possibility of omitted variable bias from unmeasured confounders. However, we believe our results are likely to represent a causal effect of the Medicaid expansion on the location choices of new general internists for several reasons. First, we found no trends before 2014 in the numbers of new physicians, including general internists, locating in what would subsequently become Medicaid expansion states. This suggests stable preexisting location patterns disrupted by the expansion. Second, the pattern of gradual growth after 2014 in the numbers of additional general internists locating in expansion states is consistent with expected real-world mechanisms. Specifically, this pattern probably reflects the gradual increase in Medicaid coverage following ACA implementation and the likelihood that the growing demand in expansion states and the ability of health care organizations to recruit more physicians took time to unfold.
Third, our descriptive analysis of trends in demand determinants in Medicaid expansion and nonexpansion states provides strong evidence against concerns that trends in unmeasured confounders favoring expansion states may be responsible for our findings. If anything, faster growth in demand determinants in nonexpansion states—aside from Medicaid coverage itself—suggests that if all states had expanded Medicaid in 2014 it is the nonexpansion states that would have attracted more physicians.
Finally, the only specialty group that showed a response was one of those cited as a recruitment target in the 2017 qualitative study of provider responses to the ACA.11 Unmeasured confounders having a generalized influence on new physicians’ location decisions should have resulted in responses by other specialty groups.
Several limitations of our study deserve mention. First, our models did not include variables to capture the diffusion of alternative payment models, a noteworthy recent trend in physician services markets. Nonetheless, we think it is unlikely that this trend is responsible for our findings. We are unaware of information on the effect of Accountable Care Organizations (ACOs) or other alternative payment models on the demand for care, physician incomes, or physician location, and the scant available information on provider experience suggests that it may be mixed.34 ACO penetration grew considerably between 2010 and 2019, but the rate of growth was slightly higher in the first half of this period, preceding implementation of the ACA, compared with the second half.35 Moreover, ACOs are present in every state, and our analysis of data presented in Muhlestein et al35 indicates that penetration differs only slightly between expansion and nonexpansion states (Online Appendix H, Supplemental Digital Content 1, http://links.lww.com/MLR/C193).
Second, most residents begin their job search before completing training,36 indicating that the optimal time interval for ascertaining the first practice location is likely to be shorter than 2.5 years. If so, our approach may have led us to attributing findings to 1 or 2 years later than the year to which they should have been attributed. However, we found no significant effects of the Medicaid expansion in the first 2 postexpansion years. The results of the sensitivity analysis using a 1.5-year interval are reassuring, but this analysis could not use the address updates that occurred between 1.5 and 2.5 years after GME completion.
Third, our specialty groups were based on physicians’ reported primary specialties. However, at least for internal medicine physicians, the reported primary specialty reflects the content of medical practice.37 Specifically, physicians who report general internal medicine as their primary specialty provide more primary care to their patients than those who report an internal medicine subspecialty. Fourth, we could only analyze allopathic physicians because the Masterfile collected limited data on osteopathic physicians during the study period.
We found that states that failed to expand Medicaid lost new general internists compared with the number they would have if they had expanded. To be sure, the number of lost physicians between 2014 and 2019 is modest. If the pace in 2017, 2018, and 2019 continues, however, this number will cumulate quickly, potentially having adverse spillover effects on access to care for residents regardless of insurance status. A remaining question is whether, over time, the Medicaid expansion will affect the practice location choices of new physicians in other specialty groups as well.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
Footnotes
Supported by Grant No. R01HS025750 from the Agency for Healthcare Research and Quality.
The findings and conclusions of this report are those of the authors and do not necessarily represent the views of the American Medical Association.
The authors declare no conflict of interest.
Contributor Information
José J. Escarce, Email: jjescarce@gmail.com.
Gregory D. Wozniak, Email: Greg.Wozniak@ama-assn.org.
Stavros Tsipas, Email: Stavros.Tsipas@ama-assn.org.
Joseph D. Pane, Email: josephp@rand.org.
Sarah E. Brotherton, Email: Sarah.Brotherton@ama-assn.org.
Hao Yu, Email: Hao_Yu@hphci.harvard.edu.
REFERENCES
- 1. Centers for Medicare and Medicaid Services. Health insurance exchanges 2020 open enrollment report; 2020. Available at: www.cms.gov/files/document/4120-health-insurance-exchanges-2020-open-enrollment-report-final.pdf. Accessed July 25, 2020.
- 2. The Henry J. Kaiser Family Foundation. State health facts: Medicaid expansion enrollment. Data source: The Centers for Medicare and Medicaid Services (CMS) Medicaid Budget and Expenditure System (MBES). Available at: www.kff.org/health-reform/state-indicator/medicaid-expansion-enrollment/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed July 25, 2020.
- 3. Crowley RA, Golden W. Health policy basics: Medicaid expansion. Ann Intern Med. 2014;160:423–425. [DOI] [PubMed] [Google Scholar]
- 4. Sommers BD, Gunja MZ, Finegold K, et al. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314:366–374. [DOI] [PubMed] [Google Scholar]
- 5. Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: a quasi-experimental study. Ann Intern Med. 2016;164:795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376:947–956. [DOI] [PubMed] [Google Scholar]
- 7. McMorrow S, Gates JA, Long SK, et al. Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Aff (Millwood). 2017;36:808–818. [DOI] [PubMed] [Google Scholar]
- 8. Newhouse JP, Williams AP, Bennett BW, et al. Does the geographical distribution of physicians reflect market failure? Bell J Econ. 1982;13:493–505. [Google Scholar]
- 9. Newhouse JP, Williams AP, Bennett BW, et al. Where have all the doctors gone? JAMA. 1982;247:2392–2396. [PubMed] [Google Scholar]
- 10. Wishner JB, Burton RA. How Have Providers Responded to the Increased Demand for Health Care Under the Affordable Care Act? Washington, DC: The Urban Institute; 2017. [Google Scholar]
- 11. Escarce JJ, Polsky D, Wozniak GD, et al. Health maintenance organization penetration and the practice location choices of new physicians: a study of large metropolitan areas in the United States. Med Care. 1998;36:1555–1566. [DOI] [PubMed] [Google Scholar]
- 12. The Henry J. Kaiser Family Foundation. Status of State Action on the Medicaid Expansion Decisions: Interactive Map; 2020. Available at: www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?activeTab=map¤tTimeframe=0&selectedDistributions=status-of-medicaid-expansion-decision&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed July 25, 2020. [PubMed]
- 13. United States Census Bureau. American Community Survey Data. Available at: www.census.gov/programs-surveys/acs/data.html. Accessed September 30, 2020.
- 14. Zuckerman S, Skopec L, Epstein M. Medicaid Physician Fees After the ACA Primary Care Fee Bump: 19 States Continue the Affordable Care Act’s Temporary Policy Change. Washington, DC: Urban Institute; 2017. [Google Scholar]
- 15. Avraham R. Database of State Tort Law Reforms (6.1). University of Texas School of Law, Law & Economics Research Paper Series No. e555; 2019. Available at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=902711. Accessed July 22, 2020.
- 16. The Policy Surveillance Program, Temple University Beasley School of Law. Nurse practitioner scope of practice. 2017. Available at: http://lawatlas.org/datasets/nurse-practitioner-scope-of-practice-1460402165. Accessed August 10, 2020.
- 17. McFadden DL. Zarembka P. Conditional logit analysis of qualitative choice behavior. Frontiers in Econometrics. New York, NY: Academic Press; 1973:105–142. [Google Scholar]
- 18. StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 19. Chen S-Y, Feng Z, Yi X. A general introduction to adjustment for multiple comparisons. J Thorac Dis. 2017;9:1725–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oehlert GW. A note on the delta method. Am Stat. 1992;46:27–29. [Google Scholar]
- 21. Gillis KD. Physicians’ Patient Mix—A Snapshot From the 2016 Benchmark Survey and Changes Associated With the ACA. Chicago, IL: American Medical Association; 2017. [Google Scholar]
- 22. Slowey M, Riba M, Udow-Phillips M. Changes in Primary Care Physicians‘ Patient Characteristics under the Affordable Care Act. Ann Arbor, MI: Center for Healthcare Research and Transformation; 2018. [Google Scholar]
- 23. Association of American Medical Colleges. The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. Washington, DC: IHS Markit Ltd; 2019. [Google Scholar]
- 24. American College of Physicians. Internal medicine vs. family medicine. Philadelphia, PA: ACP. Available at: www.acponline.org/about-acp/about-internal-medicine/career-paths/medical-student-career-path/internal-medicine-vs-family-medicine. Accessed August 2, 2020.
- 25. Laurant M, van der Biezen M, Wijers N, et al. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018;7:CD001271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Karimi-Shahanjarini A, Shakibazadeh E, Rashidian A, et al. Barriers and facilitators to the implementation of doctor-nurse substitution strategies in primary care: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019;4:CD010412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bielby WT, Bielby DD. I will follow him: family ties, gender-role beliefs, and reluctance to relocate for a better job. Am J Sociol. 1992;97:1241–1267. [Google Scholar]
- 28. Benson A. Rethinking the two-body problem: the segregation of women into geographically dispersed occupations. Demography. 2014;51:1619–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Baldridge DC, Eddleston KA, Veiga JF. Saying ‘no’ to being uprooted: the impact of family and gender on willingness to relocate. J Occup Organ Psychol. 2010;79:131–149. [Google Scholar]
- 30. Ly DP, Seabury SA, Jena AB. Characteristics of US Physician marriages, 2000-2015: an analysis of data from a US Census Survey. Ann Intern Med. 2018;168:375–376. [DOI] [PubMed] [Google Scholar]
- 31. Ly DP, Seabury SA, Jena AB. Hours worked among US dual physician couples with children, 2000 to 2015. JAMA Intern Med. 2017;177:1524–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hart LG, Skillman SM, Fordyce M, et al. International medical graduate physicians in the United States: changes since 1981. Health Aff (Millwood). 2007;26:1159–1169. [DOI] [PubMed] [Google Scholar]
- 33. Chen PG, Auerbach DI, Muench U, et al. Policy solutions to address the foreign-educated and foreign-born health care workforce in the United States. Health Aff (Millwood). 2013;32:1906–1913. [DOI] [PubMed] [Google Scholar]
- 34. Wildon M, Guta A, Waddell K, et al. The impacts of accountable care organizations on patient experience, health outcomes and costs: a rapid review. J Health Serv Res Policy. 2020;25:130–138. [DOI] [PubMed] [Google Scholar]
- 35. Muhlestein D Bleser WK Saunders RS, et al. Spread of ACOs and value-based payment models in 2019: gauging the impact of pathways to success. Health Affairs Blog; October 21, 2019. Available at: www.healthaffairs.org/do/10.1377/hblog20191020.962600/full/. Accessed October 5, 2020.
- 36. Hawkins M. 2019 Survey, Final-Year Medical Residents: A Survey Examining the Career Preferences, Plans and Expectations of Physicians Completing Their Residency Training. Dallas, TX: Merritt Hawkins; 2019. [Google Scholar]
- 37. Shea JA, Kletke PR, Wozniak GD, et al. Self-reported physician specialties and the primary care content of medical practice: a study of the AMA Physician Masterfile. Med Care. 1999;37:333–338. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


