Abstract
Background:
Parents play an important role in their children’s oral health behaviors, provide oral health access, initiate prevention, and coping strategies for health care.
Aim:
This paper develops a short form (SF) to assist parents to evaluate their children’s oral health status using Patient-Reported Outcome Measurement Information System (PROMIS) framework that conceptualized health as physical, mental, and social components.
Design:
Surveys of parents were conducted at dental clinics in Los Angeles County, together with an on-site clinical examination by dentists to determine clinical outcomes, Children’s Oral Health Status Index (COHSI), and referral recommendations (RRs). Graded response models in item response theory were used to create the SF. A toolkit including SF, demographic information, and algorithms was developed to predict the COHSI and RRs.
Results:
The final SF questionnaire consists of eight items. The square root mean squared error for the prediction of COHSI is 7.6. The sensitivity and specificity of using SF to predict immediate treatment needs (binary RRs) are 85% and 31%.
Conclusions:
The parent SF is an additional component of the oral health evaluation toolkit that can be used for oral health screening, surveillance program, policy planning, and research of school-aged children and adolescents from guardian perspectives.
1 |. BACKGROUND
Parents play an important role in the development of their children’s oral health, from using fluoridated toothpaste, choosing between a manual or powered toothbrush, and arranging dental appointments.1,2 A significant association has been identified between parental and child dental fear and dental anxiety, especially among younger children.3 Proxy-reported measures from parents provide information on the physical functioning and the mental and social experiences of children with respect to their oral health status.4,5 Parental responsiveness to children’s needs and the setting of clear expectations for their child’s behavior are associated with positive health outcomes.6
Although Patient-Reported Outcomes (PROs) from children and adolescents directly are the gold standard for the survey questions, Patient Proxy-Reported Outcome (PpRO) is useful when the child is too young or cognitively impaired for PRO self-assessment. PRO measures taken directly from children are limited by the children’s general cognition, self-awareness of symptoms, and understanding of oral health concepts.7 PpRO from parents provides supporting information to the PRO from children. For example, parents are the only appropriate source for questions such as ‘During the past 12 months, was there a time that your child needed dental care but did not get it?’ For children under seven, PpRO is the most effective way to access oral health-related quality of life (OHRQoL).4,5 There is literature that studied the validity and limitation for the efficacy of parent-proxy, especially for teenagers (age greater than 12).8 Therefore, it is necessary to develop a short form with valid psychometric properties.
The PpRO measures from parents or caregivers, however, are not simply designed to ask the same questions as those posed to their child. We have developed an oral health item bank,9,10 which is used to evaluate oral health status of children. The child version of the pediatric-calibrated items and the short form was presented in an earlier paper.11 The agreement of the answers between children and their parents is also discussed in another paper. The results in that paper show that in reporting the child’s oral health status, parents usually have worse scores than their children (S. Lee, M. Marcus, C. Maida, R.D. Hays, I. Coulter, J. Shen, Y. Wang, V. Spolsky, F. Ramos-Gomez, H. Liu, unpublished data).12 In this paper, we describe the development of a proxy-reported measure of oral health for 2–17 years old using the method of Patient-Reported Outcome Measurement Information System (PROMIS®).
To the best of our knowledge, there is no available questionnaire that focuses on the current oral health status of children and adolescents, with both PRO and PpRO independently compared to a dental exam result. The short forms use a small number of selected questions through a statistical approach to represent comparable information from the general, physical, mental, and social component of health.
2 |. METHODS
The item bank for parents’ PpRO was developed using PROMIS® methodology.9,10,12 These items were from the literature review of National Institute of Dental and Craniofacial Research (NIDCR) items, published questionnaires. In addition, the team used formative research, including focus groups and cognitive interviews9,10 to develop items. An expert panel (including pediatric dentists, general dentists, social scientists, and PROMIS® experts) reviewed the items before the cognitive interview, during which the items were reviewed on a one-on-one session between parents and dentists. Then, the survey items were administrated in a field test. Field test data were collected from twelve dental clinics in Los Angeles County10,11 from August of 2015 to September of 2017. The dental clinics were selected to cover the range of Los Angeles County, from Torrance (south) to Valencia (north), from Agoura Hills (west) to Whitter (east), and to represent children and adolescents who have a dental home in the county. The dental clinics targeted needed to be large enough to accommodate at least three dental chairs and have enough patients to enable recruiting at least 50 families in the community. In addition, the clinics needed to be open on a Saturday to conduct field testing. Parents answered the survey questions, whereas the children and adolescents were examined on-site by dentists for their current oral health status. The details of the study design and the development of children’s version short form are described elsewhere in the literature.9,10 This paper focuses on developing a short form of the parents’ version.
The conceptual model for parents was developed in parallel to the children’s version,11 except that it included some additional domains that can only be answered accurately by parents, for example, coping, prevention, and access to dental care. The conceptualized model included three components: physical, mental, and social health. Each component (orange in Figure 1) was further extended to subcomponents (green), domains (purple), and subdomains (blue). The colors of the block in Figure 1 indicate different levels of structure. The gray colored domains were not included in the further analysis because they did not directly measure oral health status.
FIGURE 1.
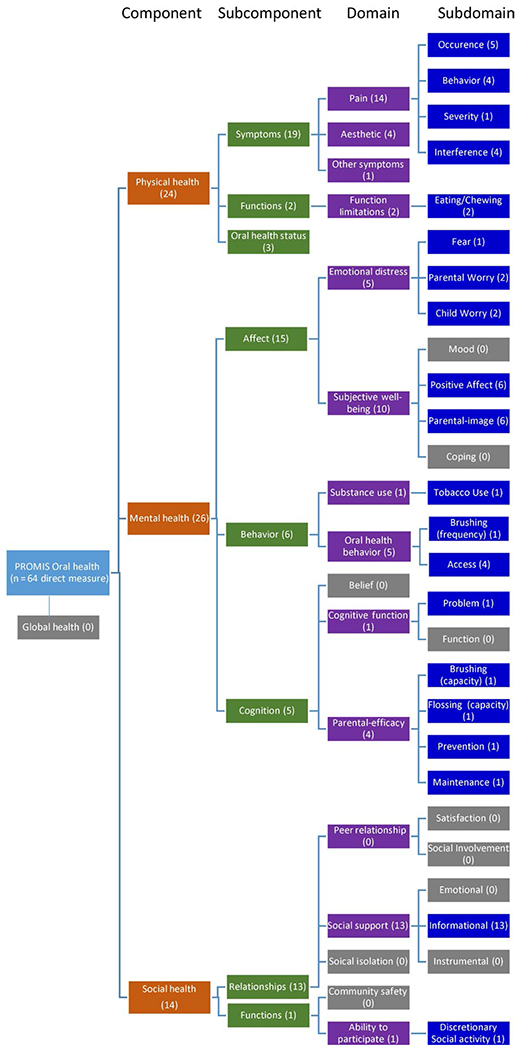
The domain structure of the parent oral health conceptual model using PROMTS approach
The clinical outcomes of the visual dental examination included Children’s Oral Health Status Index (COHSI) score and referral recommendation (RR). The COHSI was developed from a linear regression model that includes missing teeth adjusted for age, the decay of teeth, occlusion, and abnormal position13 to evaluate the overall oral health status. The RR criteria were developed from the guidelines for dental examination protocol of National Health and Nutrition Examination Survey Questionnaire (NHANES) to reflect the necessity for a future dental appointment. The criteria for the four levels of RRs, for example, emergency, urgent, earliest convenience, and routine dental conditions were described in detail in the pediatric oral health short form development paper.11
Items that directly measured oral health with responses from all 531 parents were included in the analysis. Each item was rescaled so that higher scores represented better oral health status. If a response option was endorsed by fewer than three parents, we combined the category with the adjacent worse scenario (lower score). Highly skewed items (defined as skewness less than −7.25) were excluded because of unstable estimation of parameters.11,14 Each survey item was further screened by evidence of relatively strong correlation (correlation coefficient greater than or equal to 0.2 or a significantly positive correlation) with one of the both clinical outcomes of the dental examination. After the correlation check, we included additional items so that each domain in Figure 1 is represented by at least one item. Exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) were performed to evaluate the structure of the conceptual model (Figure 1).11,15 Items with standardized loadings less than 0.3 in the EFA were excluded. In the CFA, we evaluated the goodness of fit of the model comparative fit index (CFI) (>0.90), the root mean square error (<0.06), and the standardized root mean square residual (SRMR) (<0.08).14
Samejima’s graded response model (GRM) in item response theory (IRT) was used to estimate the discrimination and threshold parameters11 for COHSI and RR separately. Four assumptions for GRM were checked. The monotonicity of items was checked by item characteristics curves to ensure that the probability of choosing response options representing more positive oral health increases with better latent oral health. The unidimensionality that the items described the latent oral health was confirmed by the GOF criteria in CFA.16,17 Differential item functioning (DIF) was evaluated using ordinal logistic regression.18–20 DIF provided evidence that the items are not measuring the latent oral health status in the same way across groups, for example, age, gender, and ethnicity. The assumption of local independence (conditional independence among items given the latent trait) was examined by to require its discrimination parameter did not exceeding 4. Another method used the diagonally weighted least square (WLSMV) method (residual correlation >0.3).14
The short form items were selected based on four criteria11: discrimination parameters, threshold parameters, the broadness of domain structure, and expert panel suggestions. The discrimination parameter (slope) should be at least greater than 1. The range of the threshold parameters should include a wide range of the latent trait. The items in the short form should represent a wide range of domains in the conceptual model. The agreement between long and short forms was compared by plots (shape of the curve) and intraclass correlations. Stata and M-plus21,22 were used to calibrate the items. The raw score and T-score conversion tables were generated for easy implementation of short form in practice.
T-scores generated from the parent’s short form were used to predict both COHSI and RR. We constructed the toolkit to mapping the short form results to the results from clinical examination directly, adjust for the demographic information and using machine learning techniques to train the algorithms. The demographic information was children’s age-group, gender, race or ethnicity, number of kids in the household, dental insurance, access to dental clinic, and parent-child relationship. We use naïve Bayesian method23 to validate the prediction result of short form for binary treatments needs. The entire database is divided into training sets and test sets. The training set was composed of randomly selected 70% of parents, and the rest are testing sets (30%).24 Naïve Bayesian methods are used on the training set to develop this prediction algorithm, which is then used on test set to report sensitivity, specificity, and area under the curve (AUC) for this prediction algorithm.
3 |. RESULTS
The sample included 531 parents of children 2-17 years old, recruited from general and pediatric dental clinics between August 2015 and September 2017 in the Los Angeles County. The characteristics of the sample (including both parents and children) are shown in Table 1. More than half of the children in the sample (58%) were recommended to follow their routine care, and 7% of children were recommended to see their dentist immediately. The overall COHSI score of the children was 90.6 (standard deviation 8.3). The sample was distributed approximately evenly among three age-groups 2-7, 8-12, and 13-17, and between boys and girls. The sample was 42% Latino, 20% White, 18% multiracial and others, 11% Asian, and 8% African American. Most of the proxy responses are obtained from female parents or guardians (71%), middle-aged (30-44) parents (56%), and Latinos (46%) as shown in Table 1. Most of the parents or guardians (75%) were married or living with a partner. The majority (72%) indicated that their primary language was English. Only 6% of the parents had less than a high school education. The average household size of the sample was about 4.8 persons per family. More than half of these families rented a place to live. There were 42% of families with household income above $60 000. The majority (80%) of the families had at least one parent with a full-time job.
TABLE 1.
Characteristics of the sample (children, parents, and household) in the field test
| Variables | Mean (SD) or No. (%) |
|---|---|
| Children’s Oral Health Status Index (COHSI) | 90.59 (8.3) |
| Clinical recommendation | |
| Continue your regular routine care | 306 (57.6%) |
| See a dentist at your earliest convenience | 62 (11.7%) |
| See a dentist within the next 2 wk | 126 (23.7%) |
| See a dentist immediately | 37 (7.0%) |
| Children’s mean age | 9.6 (4.2) |
| 2-7 | 179 (33.7%) |
| 8-12 | 206 (38.8%) |
| 13-17 | 146 (27.5%) |
| Children’s gender | |
| Male | 273 (51.4%) |
| Female | 257 (48.4%) |
| Female to male transgender | 1 (0.20%) |
| Children’s race/ethnicity | |
| Caucasian/White | 109 (20.5%) |
| Black/African American | 43 (8.1%) |
| Hispanic/Latino | 224 (42.2%) |
| Asian | 59 (11.1%) |
| Other | 96 (18.1%) |
| Parent’s gender | |
| Male | 156 (29.4%) |
| Female | 375 (70.6%) |
| Parent’s mean age | 40.4 (9.0) |
| Less than 30 | 64 (12.1%) |
| 30-44 | 295 (55.6%) |
| 45-59 | 157 (29.6%) |
| Above or equal to 60 | 15 (2.8%) |
| Parent’s race/ethnicity | |
| Caucasian/White | 130 (24.5%) |
| Black/African American | 45 (8.5%) |
| Hispanic/Latino | 246 (46.3%) |
| Asian | 67 (12.6%) |
| Other | 43 (8.1%) |
| Parent’s marital status | |
| Married/living w/partner | 398 (75.0%) |
| Single | 133 (25.1%) |
| Parent’s education level | |
| Did not finish high school | 31 (5.8%) |
| High school or equivalent | 153 (28.8%) |
| Some college | 273 (51.4%) |
| Graduate or professional school | 74 (13.9%) |
| Parent’s primary language | |
| English | 382 (71.9%) |
| Other | 149 (28.1%) |
| Household size | 4.8 (1.4) |
| Less than or equal to 3 | 89 (16.8%) |
| 4 | 176 (33.2%) |
| 5 | 121 (22.8%) |
| More than or equal to 6 | 145 (27.3%) |
| House status | |
| Own | 204 (38.4%) |
| Rent | 299 (56.3%) |
| Other arrangement | 28 (5.3%) |
| Household annual income level | |
| Less than $20 000 | 96 (18.1%) |
| $20 000-$39 999 | 141 (26.6%) |
| $40 000-$59 999 | 72 (13.6%) |
| $60 000-$89 999 | 83 (15.6%) |
| Over $100 000 | 139 (26.2%) |
| Family employment | |
| Full-time Job | 420 (79.1%) |
| Part-time Job | 59 (11.1%) |
| Not working | 52 (9.8%) |
The study questionnaire was completed by QDS™ (Questionnaire Development System). Subjects who did not complete the survey (<4%) were excluded at the beginning of analysis. We do not have missing data. The entire survey for parents included 256 items, including a literature review of published instruments, legacy items, and demographic items. The long form was developed from the 64 items, excluding 37 items that did not directly measure oral health; 94 branched items that were answered depending on the responses to previous questions; 17 items that are only answered by certain age-groups, 12 new items added in the middle of the field test; and 32 were demographic-related questions. One more item was excluded because of skewness. Thirty-six items were excluded because of small or negative correlations with clinical outcomes. Twenty- eight items remained in the item pool. Finally, seven items are added back after reviewing the completeness of the domain coverage in Figure 1. Thus, there were 37 candidate items for developing the long form, with 27 items associated with COHSI and 31 items for RRs. There were 21 items to both COHSI and RRs. Separate but similar procedures were performed for two sets of items that measured COHSI and RRs.
Seven items were excluded because of low EFA factor loadings (<0.3). The CFA confirmed the structure of the conceptual model; for COHSI, the overall CFI, SRMR, and RMSEA were 0.93, 0.04, and 0.06, respectively, and for RRs, these indices were 0.91, 0.05, and 0.06, respectively. These 30 proxy items covered the majority of domains in the conceptualized model, with five items only for COHSI, seven only for RRs, and 18 items in common. Two more items were excluded because of violation of the monotonicity assumption. Therefore, the calibrated long form included 28 items as shown in Table 2 for COHSI and RR. The results of calibration, with slopes (discrimination) and threshold (difficulty) parameters, are shown in Table 2A,B. In Table 2, the subcomponent of the items was indicated in the long form. The long form consists of a total of 28, with 22 items for COHSI and 24 items for RRs, including 18 items in common.
TABLE 2.
Item calibration statistics for Children’s Oral Health Status Index and referral outcomes for proxy PROs. (a) Item calibration statistics for Children’s Oral Health Status Index. (b) Calibration statistics for referral
| Threshold |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Subcomponent | Itemsa | Outcome | DIF | Slope | 1 | 2 | 3 | 4 | 5 |
| (A) | |||||||||
| PHY/Symptoms | It was hard for my child to eat because of pain in his or her mouth | Both | 2.22 | −6.80 | −4.71 | −2.98 | |||
| PHY/Symptoms | My child’s gums hurt. | Both | Parent Gender | 2.16 | −4.60 | −3.03 | |||
| MEN/Cognition | It was hard for my child to pay attention because of pain this or her mouth | Both | 2.15 | −6.49 | −5.39 | −4.10 | |||
| PHY/Symptoms | My child’s mouth hurts | Both | 1.89 | −6.54 | −4.22 | −2.17 | |||
| PHY/Symptoms | In the last 4 wk, how much of the time did your child have pain or discomfort? | Both | 1.78 | −6.80 | −5.67 | −3.14 | −1.64 | ||
| PHY/Symptoms | My child had a tooth that hurts. | Both | 1.78 | −6.12 | −3.38 | −2.09 | |||
| MEN/Affect | In the last 4 wk, how much of the time was your child worried or concerned about problems with his/her mouth, tongue, teeth, jaws, or gums? | Both | 1.74 | −6.62 | −5.91 | −5.32 | −3.43 | −1.76 | |
| MEN/Affect | In the last 4 wk, how much of the time were you pleased or happy with the look of your child’s mouth, teeth, jaws, or gums? | Both | Parent Age-groupb | 1.57 | −5.62 | −4.42 | −2.46 | −1.49 | 0.71 |
| MEN/Affect | When I look at my child’s teeth | Both | 1.48 | −2.80 | −0.16 | ||||
| MEN/Behavior | During the past 12 mo, was there a time that your child needed dental care but did not get it? | Both | 1.46 | −3.63 | |||||
| PHY/Oral Health Status | In general, would you say your child’s oral health is: | Both | 1.43 | −6.18 | −2.97 | −0.29 | 2.38 | ||
| MEN/Affect | How happy are you with the color of your child’s teeth? | Both | 1.27 | −3.29 | −2.23 | −0.69 | 1.40 | ||
| MEN/Affect | Does your child worry about problems with his or her teeth? | Both | Parent Education, Parent Language | 1.11 | −1.58 | ||||
| SOC/Functions | In the last 4 wk, how much of the time did your child’s oral health interfere with his/her social activities? | Both | Parent Education, Parent Language | 0.98 | −5.15 | −4.35 | −3.95 | −2.87 | −1.71 |
| MEN/Affect | Compared to other kids my child’s age: | Both | 0.85 | −3.21 | 0.10 | ||||
| PHY/Symptoms | My child’s teeth are straight | Both | 0.84 | −0.32 | |||||
| PHY/Symptoms | My child’s teeth has problems (ie, space, crooked, crowded.) | Both | Parent Education | 0.74 | 0.20 | ||||
| MEN/Cognition | I am able to help my child maintain good oral health | Index | 0.67 | −4.28 | −3.50 | −1.48 | |||
| MEN/Affect | How much is your child afraid to go to a dentist? | Both | Parent Age-groupb | 0.62 | −3.35 | −1.69 | −0.35 | ||
| PHY/Functions | In the last 4 wk, how much of the time was your child able to swallow comfortably? | Index | Parent education, parent language | 0.57 | −2.77 | −2.58 | −2.42 | −2.31 | −1.76 |
| MEN/Cognition | I can do many things to prevent oral health problems in my child | Index | 0.55 | −4.80 | −4.09 | −1.44 | |||
| MEN/Behavior | How often do you remind your child to brush his/her teeth before he/she goes to sleep? | Index | Parent age-group | 0.08 | 0.09 | 0.73 | 1.21 | 2.20 | 3.30 |
| (B) | |||||||||
| PHY/Symptoms | It was hard for my child to eat because of pain in his or her mouth | Both | 3.09 | −8.09 | −5.79 | −3.77 | |||
| PHY/Symptoms | It hurts my child’s teeth to chew. | Referral | Parent gender | 2.81 | −7.85 | −5.49 | −3.33 | ||
| MEN/Cognition | It was hard for my child to pay attention because of pain this or her mouth | Both | 2.72 | −7.27 | −6.11 | −4.74 | |||
| PHY/Symptoms | My child’s gums hurt | Both | 2.58 | −5.11 | −3.45 | ||||
| PHY/Symptoms | My child’s mouth hurts | Both | 2.54 | −7.48 | −4.99 | −2.65 | |||
| PHY/Symptoms | My child had a tooth that hurts | Both | Parent language | 2.36 | −6.93 | −3.98 | −2.51 | ||
| PHY/Symptoms | During the last school year, how many days of school did your child miss because of pain in his/her mouth, tongue, teeth, or gums? | Referral | Parent education | 2.04 | −5.67 | −4.22 | |||
| PHY/Symptoms | In the last 4 wk, how much of the time did your child have pain or discomfort | Both | 1.99 | −7.03 | −5.88 | −3.33 | −1.78 | ||
| MEN/Affect | In the last 4 wk, how much of the time was your child worried or concerned about problems with his/her mouth, tongue, teeth, jaws, or gums? | Both | 1.86 | −6.75 | −6.03 | −5.44 | −3.55 | −1.86 | |
| MEN/Behavior | During the past 12 mo, was there a time that your child needed dental care but did not get if? | Both | 1.47 | −3.64 | |||||
| MEN/Affect | In the last 4 wk, how much of the time were you pleased or happy with the look of your child’s mouth, teeth, jaws, or gums? | Both | 1.38 | −5.32 | −4.17 | −2.33 | −1.42 | 0.65 | |
| PHY/Oral Health Status | In general, would you say your child’s oral health is: | Both | 1.28 | −5.94 | −2.85 | −0.29 | 2.28 | ||
| MEN/Affect | When I look at my child’s teeth | Both | 1.25 | −2.62 | −0.17 | ||||
| MEN/Affect | How happy are you with the color of your child’s teeth? | Both | 1.10 | −3.14 | −2.12 | −0.66 | 1.32 | ||
| MEN/Affect | Does your child worry about problems with his or her teeth? | Both | Parent education, parent language | 1.07 | −1.57 | ||||
| SOC/Functions | In the last 4 wk, how much of the time did your child’s oral health interfere with his/her social activities? | Both | Parent education, parent language | 0.98 | −5.14 | −4.34 | −3.94 | −2.S6 | −1.71 |
| PHY/Oral Health Status | During the last 12 mo, did your child have an oral health problem? | Referral | 0.86 | −1.16 | |||||
| PHY/Symptoms | My child’s teeth are straight | Both | 0.72 | −0.32 | |||||
| MEN/Affect | Compared to other kids my child’s age: | Both | 0.72 | −3.13 | 0.09 | ||||
| MEN/Behavior | I take my child to the dentist | Referral | 0.70 | −4.09 | −2.53 | ||||
| PHY/Symptoms | How often does your child have bad breath? | Referral | Parent age-groupb | 0.67 | −4.06 | −3.11 | −2.38 | 0.22 | 2.07 |
| PHY/Symptoms | My child’s teeth has some problems (ie, space, crooked, crowded.) | Both | 0.63 | 0.19 | |||||
| MEN/Affect | How much is your child afraid to go to a dentist? | Both | Parent age-groupb | 0.62 | −3.35 | −1.70 | −0.35 | ||
| MEN/Cognition | By reminding my child to floss his or her teeth, I believe | Referral | 0.19 | −5.19 | −3.37 | ||||
Items in bold indicate being selected in the static short form.
No DIF with age if within age-group (<45 and ≥45).
The items for the short form are shown in bold in Table 2. These items were selected based on the slope (higher slope), threshold parameters (wider range), domain representation, and expert panel opinions. There were seven items in short form for COHSI and seven items for RRs. Six questions were commonly used to measure both clinical outcomes. The items represented the physical, mental, and social health components. The information curves for the short form and long form are compared in Figure 2 for both COHSI and RRs. The curves for short form preserved the shape of the curve for long form but with less comparable level of information. The Pearson correlation coefficients between the latent traits of the long form and short form were 0.90 for COHSI and 0.91 for RRs.
FIGURE 2.
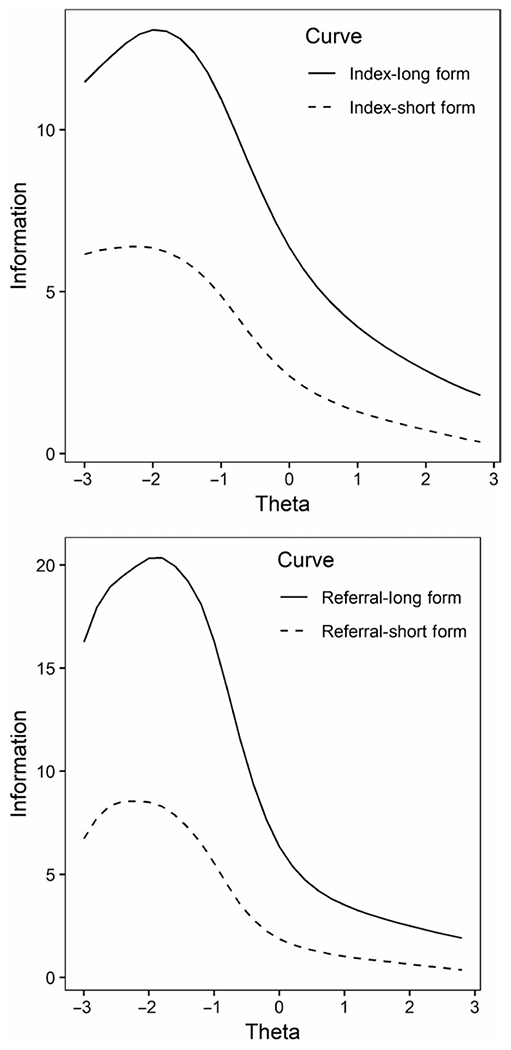
Information curve for both referral and Children’s Oral Health Status Index (long form vs short form)
The short form with detailed item questions and responses is shown in Table 3, and the form could be easily modified to be directly used in practice to evaluate both COHSI and RRs. Tables 4 and 5 linked the short form response to the T-score. The T-score has a mean of 50 and a standard deviation of 10, with higher scores indicating better oral health status. For example, if the T-score is 45.0 (raw score in the survey is 30), then the subject is 0.5 standard deviation below the U.S. general population mean. The conversion table is used when all the questions in the short form are answered. The 95% confidence interval is calculated by the formula T-score minus and plus the standard error in the table times 5.
TABLE 3.
PROMIS child oral health short form items
| Subcomponent | Items | Response |
|---|---|---|
| PHY/Symptoms | My child’s mouth hurts | Often (0); Sometimes (2); Almost Never (4); Never (5) |
| PHY/Symptoms | It was hard for my child to eat because of pain in his or her mouth | Always, Almost always, Often (0); Sometimes (2); Almost Never (4); Never (5) |
| PHY/Oral Health Status | In general, would you say your child’s oral health is: | Poor (0); Fair (2); Good (3); Very good (4); Excellent (5) |
| MEN/Cognition | It was hard for my child to pay attention because of pain this or her mouth | Always, Almost always, Often (0); Sometimes (2); Almost Never (4); Never (5) |
| MEN/Affect | In the last 4 wk, how much of the time was your child worried or concerned about problems with his/her mouth, tongue, teeth, jaws, or gums? | Always (0); Almost always (1); Often (2); Sometimes (3); Almost Never (4); Never (5) |
| MEN/Affect | In the last 4 wk, how much of the time were you pleased or happy with the look of your child’s mouth, teeth, jaws, or gums? | Never (0); Almost Never (1); Sometimes (2); Often (3); Almost always (4); Always (5) |
| SOC/Functions | In the last 4 wk, how much of the time did your child’s oral health interfere with his/her social activities? | Always (0); Almost always (1); Often (2); Sometimes (3); Almost Never (4); Never (5) |
| PHY/Symptoms | During the last school year, how many days of school did your child miss because of pain in his/her mouth, tongue, teeth, or gums? | 2 or more days (0); 1 d (3); Never (5) |
TABLE 4.
T-score conversion table for Children’s Oral Health Status Index
| Raw score | T-score | SE | N (%) | Average Index |
|---|---|---|---|---|
| 7 | 17.68 | 3.79 | 1 (0.2) | 96.54 |
| 14 | 24.37 | 3.09 | 2 (0.4) | 93.49 |
| 15 | 28.24 | 3.32 | 1 (0.2) | 84.69 |
| 18 | 29.02 | 3.07 | 2 (0.4) | 93.43 |
| 20 | 31.29 | 3.22 | 1 (0.2) | 80.08 |
| 21 | 31.29 | 3.22 | 4 (0.8) | 85.78 |
| 22 | 33.23 | 2.96 | 5 (0.9) | 84.20 |
| 23 | 33.23 | 2.96 | 4 (0.8) | 83.21 |
| 24 | 34.53 | 3.28 | 6 (1.1) | 83.39 |
| 25 | 37.75 | 3.66 | 11 (2.1) | 83.21 |
| 26 | 38.88 | 3.70 | 11 (2.1) | 85.99 |
| 27 | 39.41 | 3.74 | 15 (2.8) | 90.40 |
| 28 | 41.83 | 4.22 | 17 (3.2) | 88.67 |
| 29 | 44.10 | 4.55 | 40 (7.5) | 88.61 |
| 30 | 45.86 | 4.87 | 50 (9.4) | 86.76 |
| 31 | 48.22 | 5.36 | 56 (10.5) | 90.61 |
| 32 | 50.29 | 5.74 | 78 (14.7) | 91.45 |
| 33 | 53.66 | 6.39 | 95 (17.9) | 92.00 |
| 34 | 57.62 | 7.05 | 89 (16.8 | 93.08 |
| 35 | 62.16 | 7.82 | 43 (8.1) | 93.73 |
SE: standard error on T-score metric.
TABLE 5.
T-score conversion table for referral
| Raw score | T-score | SE | Category | N (%) | Average Index |
|---|---|---|---|---|---|
| 12 | 22.33 | 3.67 | Level 1—See dentist immediately | 2 (0.4) | 96.54 |
| 16 | 26.48 | 3.61 | 2 (0.4) | 90.16 | |
| 17 | 26.86 | 4.05 | 1 (0.2) | 91.35 | |
| 19 | 29.53 | 3.70 | 3 (0.6) | 85.37 | |
| 20 | 31.51 | 3.33 | 4 (0.8) | 83.26 | |
| 21 | 31.51 | 3.33 | 1 (0.2) | 75.67 | |
| 22 | 31.51 | 3.33 | 2 (0.4) | 95.42 | |
| 23 | 31.51 | 3.33 | 1 (0.2) | 87.89 | |
| 24 | 34.08 | 3.69 | 6 (1.1) | 87.85 | |
| 25 | 36.33 | 4.11 | Level 2—See dentist with the next two weeks | 10 (1.9) | 78.36 |
| 26 | 36.33 | 4.11 | 9 (1.7) | 88.50 | |
| 27 | 39.80 | 4.52 | 15 (2.8) | 88.32 | |
| 28 | 41.68 | 4.82 | 21 (4) | 88.20 | |
| 29 | 44.10 | 5.12 | 29 (5.5) | 87.41 | |
| 30 | 45.39 | 5.31 | Level 3—See dentist at your earliest convenience | 47 (8.9) | 88.87 |
| 31 | 47.56 | 5.63 | 66 (12.4) | 88.87 | |
| 32 | 49.82 | 5.92 | Level 4—See dentist at your regular routine | 76 (14.3) | 91.05 |
| 33 | 53.32 | 6.41 | 100 (18.8) | 91.86 | |
| 34 | 57.43 | 6.93 | 93 (17.5) | 93.49 | |
| 35 | 62.70 | 7.68 | 43 (8.1) | 93.73 | |
SE: standard error on T-score metric.
The toolkit is developed based on the above short form items, demographic information, and machine learning algorithms to predict clinical outcome, COHSI and RR (Figure 3). The validation of the toolkit indicated a good potential in prediction with AUC equal to 0.64. The potential cutoff with high sensitivity (ability to detect those who need treatment very soon) can yield a sensitivity of 85% with specificity 31%, from the 30% test data.
FIGURE 3.
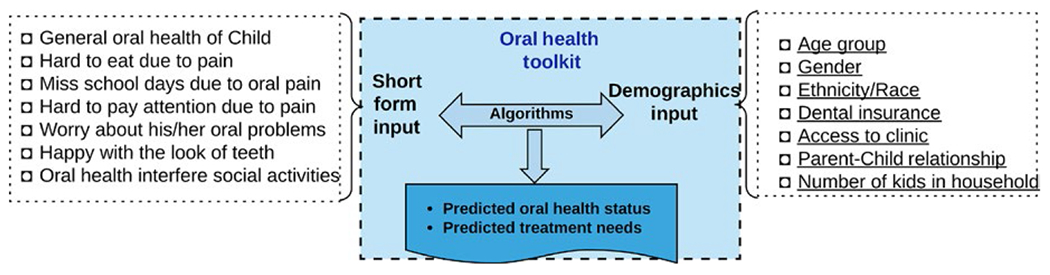
Parent toolkit to predict oral health outcomes
4 |. DISCUSSION
We used PROMIS® methods to develop the proxy-version short form from general health, and physical, mental, and social health perspectives. The proxy version was developed to compensate for or augment the child’s self-reported version. Children and parents’ perspectives may differ, and children may have limited ability to report on certain oral health-related issues. Certainly, when children are too young (less than 7 in our study) to answer the survey questions, only the parent’s responses can be relied upon. Parents and children were asked very similar questions for those concerns that have a small contextual effect, for example, in parent version, “How often does your child have bad breath,” as compared with the item in child version “How often do you have bad breath.” Certain items are only available in the child version, for example, “Do other students make jokes about the way your teeth look.” The accuracy of the response to these questions relies upon respondents’ perception of oral health and the degree of relationship between the respondents and their children. The parents’ perception of the factors that differentiate COHSI and RRs is not as clear as those gained directly from the children. The short form has a total of 15 items, with four items in common. As expected, the actual disease status and perceived need are associated with the parents’ perceptions of their children’s oral health status.2,25 The family relationship measure (“How often does your child feel that you listen to his or her ideas?”) is used to adjust for the variability in parent-proxy items.26 The validity and reliability of parent-proxy measurements can also be affected by the age of the children, items used in the PROs assessment, the oral health status of the child, the quality of parent-child relationship7; and the perception of oral health from parents’ perspective.2 The toolkit has high sensitivity and tolerable specificity to predict the COHSI and RRs.
It is estimated that by 2060, 34% of the US population under age of 18 will be Latino.27 The prevalence of dental caries is disproportionately higher for Latino children. The parents’ short form developed in this paper and the children’s short form together may help to find out the reasons for the disparities. The short form can be used to predict the COHSI score and RRs. It could be used for screening in large population settings with limited resources. The sample size in this study is more than 500, which is recommended28 for most two-parameter IRT models. To our knowledge, this is the first study that developed a proxy-version short form using PROMIS® methods to predict their children’s COHSI score and RRs. We evaluate the accuracy of the short form using outcomes from an on-site clinical exam. Parents can easily use the short form as a snapshot of their children’s oral health status, through RRs and the COHSI score. The short form could be used to evaluate the oral health programs from the parents’ perspectives. Additionally, it could be used to stratify samples for children’s oral health-related research using parental responses.
There are some limitations in this paper. Similar limitations are described in another paper, such as the sampling frame and data collection methods.11 The sample was recruited conveniently from dental clinics located in Los Angeles County. Given the complexity of residential mobility of the county, we did not take into account the variation in different areas, either demographic differences or oral health status from different clinics. We pooled the samples together to obtain sufficient sample size.28 We included some DIF questions in the short form. For example, for the reminder question, for example, “how often do you remind your child to brush his or her teeth before he or she goes to sleep,” DIF was found among and within age-groups. This item is age-specific as expected. Another item related to social activities has DIF with respect to the primary language and education level. This could potentially be the result of using the word “interfere” in the survey questions and respondent’s understanding of the meaning of “social activities.”
Future work includes comparing the consistency and agreement among items reported by both parent and child. The project is unique in the concurrent use of a clinical examination for all children and parents surveyed. Further analysis could be undertaken to develop a disease-specific parent-proxy version of the survey to address, for example, childhood active caries or caries experiences. This paper provides the foundation for the further development of children’s oral health toolkits that combine the short form responses from both children (self-reported) and parents (proxy-reported) to predict oral health outcomes effectively and accurately.
Why this paper is important to paediatric dentists.
The survey is developed using Patient-Reported Outcome Measurement Information System (PROMIS®) approach with validated psychometric properties.
To develop a short list of questions (short form) using item response theory (IRT) to predict children’s oral health status based on the parents’ view.
To provide a parent oral health toolkit that can evaluate and screen children’s oral health status and treatment needs.
ACKNOWLEDGMENTS
We thank the families for their participation in the study, which contributes to the enhancement of oral health item bank development. We also thank the field staff of the data collection and coordination sites. This research was supported by an NIDCR/NIH grant to the University of California, Los Angeles (UCLA) (U01DE022648).
Funding information
This research was supported by a National Institute of Dental and Craniofacial Research/NIH grant to the University of California, Los Angeles [U01DE022648].
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
To participate in the study, each family member provided active consent, as approved by the University of California, Los Angeles Institutional Review Board (Approval # 13-001330). All children gave consent to participate in the study. Moreover, each of their parents or guardians signed an informed consent form.
REFERENCES
- 1.Okada M, Kawamura M, Kaihara Y, et al. Influence of parents’ oral health behaviour on oral health status of their school children: an exploratory study employing a causal modelling technique. Int J Pediatr Dent. 2002;12(2):101–108. [DOI] [PubMed] [Google Scholar]
- 2.Talekar BS, Rozier RG, Slade GD, Ennett ST. Parental perceptions of their preschool-aged children’s oral health. J Am Dental Assoc. 2005;136(3):364–372. [DOI] [PubMed] [Google Scholar]
- 3.Olak J, Saag M, Honkala S, et al. Children’s dental fear in relation to dental health and parental dental fear. Stomatologija. 2013;15(1):26–31. [PubMed] [Google Scholar]
- 4.Varni JW, Thissen D, Stucky BD, et al. PROMIS(R) Parent Proxy Report Scales for children ages 5–7 years: an item response theory analysis of differential item functioning across age groups. Qual Life Res. 2014;23(1):349–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varni JW, Thissen D, Stucky BD, et al. PROMIS(R) Parent Proxy Report Scales: an item response theory analysis of the parent proxy report item banks. Qual Life Res. 2012;21(7):1223–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar S, Zimmer-Gembeck M, Kroon J, Lalloo R, Johnson N. The role of parental rearing practices and family demographics on oral health-related quality of life in children. Qual Life Res. 2017;26(8):2229–2236. [DOI] [PubMed] [Google Scholar]
- 7.Bevans KB, Riley AW, Moon J, Forrest CB. Conceptual and methodological advances in child-reported outcomes measurement. Expert Rev Pharmacoecon Outcomes Res. 2010; 10(4): 385–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Kooten JA, Terwee CB, Kaspers GJ, van Litsenburg RR. Content validity of the patient-r eported outcomes measurement information system sleep disturbance and sleep related impairment item banks in adolescents. Health Qual Life Outcomes. 2016;14:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maida CA, Marcus M, Hays RD, et al. Child and adolescent perceptions of oral health over the life course. Qual Life Res. 2015;24(11):2739–2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu H, Hays RD, Marcus M, et al. Patient-reported oral health outcome measurement for children and adolescents. BMC Oral Health. 2016;16(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu H, Hays R, Wang Y, et al. Short form development for oral health patient-reported outcome evaluation in children and adolescents. Qual Life Res. 2018;27:1599–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maida CA, Marcus M, Hays RD, et al. Qualitative methods in the development of a parent survey of children’s oral health status. J Patient Rep Outcomes. 2018;2(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koch AL, Gershen JA, Marcus M. A children’s oral health status index based on dentists’ judgment. J Am Dent Assoc. 1985;110: 36–42. [DOI] [PubMed] [Google Scholar]
- 14.Rose M, Bjorner JB, Gandek B, Bruce B, Fries JF, Ware JE. The PROMIS Physical Function item bank was calibrated to a standardized metric and shown to improve measurement efficiency. J Clin Epidemiol. 2014;67(5):516–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watt T, Bjorner JB, Groenvold M, et al. Development of a short version of the thyroid-related patient-reported outcome ThyPRO. Thyroid. 2015;25(10):1069–1079. [DOI] [PubMed] [Google Scholar]
- 16.Reliability Suhr D., exploratory & confirmatory factor analysis for the scale of athletic priorities. Diambil pada tanggal. 2003;2:274–228. [Google Scholar]
- 17.Suhr DD. Exploratory or confirmatory factor analysis? Cary, NC: SAS Institute; 2006. [Google Scholar]
- 18.Choi SW, Gibbons LE, Crane PK. Lordif: an R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and Monte Carlo simulations. J Stat Softw. 2011;39(8):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crane PK, Gibbons LE, Ocepek-Welikson K, et al. A comparison of three sets of criteria for determining the presence of differential item functioning using ordinal logistic regression. Qual Life Res. 2007;16(1):69. [DOI] [PubMed] [Google Scholar]
- 20.Paz SH, Spritzer KL, Reise SP, Hays RD. Differential item functioning of the patient-reported outcomes information system (PROMIS®) pain interference item bank by language (Spanish versus English). Qual Life Res. 2017;26(6):1451–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pope R Item response theory models in Stata. Paper presented at: 2015 Stata Conference 2015. [Google Scholar]
- 22.STATA. Stata Statistical Software Release 14. College Station, TX: Stata Press Publication; 2015. [Google Scholar]
- 23.Kohavi R Scaling up the accuracy of Naive-Bayes classifiers: a decision-tree hybrid. Paper presented at: KDD 1996. [Google Scholar]
- 24.McCallum A, Nigam K. A comparison of event models for naive bayes text classification. Paper presented at: AAAI-98 workshop on learning for text categorization 1998. [Google Scholar]
- 25.Oliveira ER, Narendran S, Williamson D. Oral health knowledge, attitudes and preventive practices of third grade school children. Pediatr Dent. 1999;22(5):395–400. [PubMed] [Google Scholar]
- 26.Bevans KB, Riley AW, Landgraf JM, et al. Children’s family experiences: development of the PROMIS® pediatric family relationships measures. Qual Life Res. 2017;26(11):3011–3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Population Estimates and Projections. Current Population Reports. P25–1143. US Census Bureau, 2015. [Google Scholar]
- 28.Cappelleri JC, Lundy JJ, Hays RD. Overview of classical test theory and item response theory for the quantitative assessment of items in developing patient-reported outcomes measures. Clin Ther. 2014;36(5):648–662. [DOI] [PMC free article] [PubMed] [Google Scholar]


