Abstract
One in 10 people die awaiting transplantation from donor shortage. Only half of Americans register as organ donors. In this cross-sectional study, we evaluated population-level associations of neighborhood socioeconomic deprivation and racial segregation on organ donor registration rates. We analyzed state identification card demographic and organ donor registration data from five states to estimate the association between a neighborhood socioeconomic deprivation index (range [0,1]; higher values indicate more deprivation) and a racial index of concentration at the extreme (ICE) (range [−1,1]; lower values indicate predominantly black neighborhoods, higher values indicate predominantly white neighborhoods) on organ donor registration rates within a specified geography (census tract or ZIP code tabulation area [ZCTA]). Among 26,720,738 registrants, 32% of the sample were registered organ donors. At the census tract level, with each 0.1 decrease in the deprivation index, the organ donor registration rate increased by 6.8% (95%CI: 6.6%, 7.0%). With each 0.1 increase in the racial ICE, the rate increased by 1.5% (95%CI: 1.5%, 1.6%). These associations held true at the ZCTA level. Areas with less socioeconomic deprivation and a higher concentration of white residents have higher organ donor registration rates. Public health initiatives should consider neighborhood context and novel data sources in designing optimal intervention strategies.
BACKGROUND
Currently, 114,411 people await life-saving organ transplants. In 2017, 12,093 people died or were removed from the waitlist for being too sick for transplantation, representing 11% of those waitlisted.1 There continue to be geographic,2 socioeconomic,3 and racial disparities4 among those who die. Disparities in organ allocation may contribute to disparities in outcomes. While organ donation rates have increased, demand continues to exceed supply.5 In the United States, approximately 70% of the population are willing to donate their organs,6,7 yet only 56% of eligible adults register as organ donors on their state driver’s license or identification card.5,8,9 Without clearly demarcated donor status, only half of families approached at the time of a potential donor’s death consent to donating their loved one’s organs.6 Identifying subgroups with low rates of organ donor registration may enable tailored public health initiatives to increase registration rates.10
At an individual level, those with lower socioeconomic status and African Americans are less likely to register as organ donors.7,11,12 Community-based interventions have been heralded as important tools for increasing organ donor registration,13,14 yet links between neighborhood contextual characteristics, enumerated using area-level data, and registration have been minimally explored.15–17 Ladin, et al.16 found that lower area-level social capital (i.e. “features of social organization, such as networks, norms, and trust, that facilitate coordination and cooperation for mutual benefit”18) and educational attainment were both associated with lower donor registration rates across Massachusetts. However, no other studies have evaluated the association between registration rates and additional ecological factors like socioeconomic deprivation and racial segregation, relevant characteristics at an individual level.
Geospatial methods, and area-level data, are routinely employed to target public health interventions to the correct demographic.19–24 They provide an opportunity to advance our understanding of how organ donor registration rates vary across populations. Building on the work of Ladin, et al.,16 and using data on ~27 million people from five state Bureau of Motor Vehicle (BMV) registries, we examined relationships between area-based rates of organ donor registration and area-level measures of socioeconomic deprivation and racial segregation. We hypothesized that areas with less deprivation and lower concentrations of African Americans would have higher registration rates.
METHODS
Study Design and Data Source
We conducted a cross-sectional study using data from driver’s license and state identification cardholders (N=27,077,020) from New York, Oregon, Tennessee, Vermont, and Wisconsin BMVs. We selected these states because they were geographically distributed across the country and had established mechanisms for sharing data with the research team. In all but one state (New York), we obtained cardholders’ residential address, age, sex, and organ donor registration status. New York did not release street addresses due to privacy concerns; however, they provided cardholders’ ZIP code, age, sex, and organ donor registration status. Across included states, data were discarded if cardholder’s listed age was >100 years or <16 years (N=356,282; 1.3%)—leaving 26,720,738 complete records.
The Cincinnati Children’s Hospital Institutional Review Board approved this study.
Geocoding
Street addresses and/or ZIP codes were geocoded into their containing census tract or ZIP code tabulation area (ZCTA) using DeGAUSS.25 Participants were excluded if their addresses could not be geocoded with enough precision to locate the address within a street or street segment (highest levels of precision) or if their matching score was less than 0.5.25 Census tracts are generally thought to be a better spatial resolution than ZIP codes for population-level health studies because of their officially-defined geographic boundaries and sociodemographic homogeneity.26 However, because New York only released ZIP codes, we could not identify census tracts for their cardholders. Instead, we matched ZIP codes to ZCTAs which provide geographical features to ZIP codes and enable connection to relevant U.S. Census Bureau data.27
Outcome
Our primary outcome was the percentage of organ donor registrants within a census tract and/or ZCTA. We calculated this by dividing the total number of organ donor registrants in a census tract/ZCTA by the total number of individuals who had registered with the BMV within that census tract/ZCTA, respectively.
Exposures
Our exposures were ecological measures of socioeconomic deprivation and racial segregation. They were measured via an index of area-based socioeconomic deprivation28–30 and a racial index of concentration at the extreme31 (ICE); both available at census tract and ZCTA levels. The socioeconomic deprivation index is composed of six measures from the U.S. Census Bureau’s 2015 5-year American Community Survey (ACS): median household income, and fraction of the population below the federal poverty level, adults with a high school education, households receiving public assistance, population with no health insurance, and housing units that are vacant.28 The index has a range of [0,1]; values closer to 1 indicate areas with more socioeconomic deprivation. The racial ICE assesses area-based racial heterogeneity. This measure, first conceived by Krieger, et al.19 was designed to measure health inequities within a specified geography by quantifying the relative composition of the most and least privileged groups across a specified social construct. In line with previous work by Krieger, et al.,31 “we conceptualized race as a social construct arising from inequitable race relations” that are different than socioeconomic class differences. The formula for determining the racial ICE within a specified geography is: the difference between the number of white non-Hispanic residents and the number of black non-Hispanic residents divided by the total number of white or black non-Hispanic residents. These two races were chosen because they are at the extremes of racial privilege across the U.S. and allow for monitoring inequities on the basis of race relations.31,32 The racial ICE has a range of [−1,1]. Values closer to −1 indicate areas that are predominantly black, and values closer to 1 indicate areas that are predominantly white, while values closer to zero represent areas that either have similar numbers of white and black residents or have mostly residents that are neither white nor black. Incorporating more than two races into a statistical model further complicates the interpretation of such models. Therefore, this measure does not capture Hispanic ethnicity, however, it provides important insight into health outcome gradients across different racial groups. Both the deprivation index and racial ICE were calculated at the census tract level using estimates from the 2015 5-year ACS. We calculated the ZCTA-level deprivation index by averaging values from all census tracts overlapping with that ZCTA. We derived ZCTA-level racial ICE directly from ZCTA-level data.
Statistical Analyses
We used descriptive statistics to characterize outcome and exposure variables. We used scatter plots to visualize relationships between outcomes and exposures at both spatial resolutions. To assess the relationship between organ donor rate and both deprivation index and racial ICE, we fit mixed-effects linear regression models with a random intercept for each state to account for state-level variation. We excluded New York from census tract-level analyses since we only had access to ZIP codes. All states were included in the ZCTA-level analyses.
Because we were unable to obtain street addresses from New York, we sought to determine if relationships between outcomes and exposures were different across spatial resolutions (i.e. census tract vs. ZCTA level) rather than because of inherent differences specific to New York. Therefore, as a sensitivity analysis, we assessed relationships at both the census tract and ZCTA levels for Oregon, Tennessee, Vermont, and Wisconsin.
Findings were considered significant with a p<0.05 and all hypothesis testing was 2-sided. We performed all analyses in R (v3.6.2; R Foundation for Statistical Computing). Mixed effects models were fit using the lme4 package (v1.1-21).
RESULTS
Roughly half the sample were female (50.6%) and the mean age was 47.7 years (SD: 18.7) (Table 1). About 32% of the sample were registered organ donors. New York had the lowest organ donor registration rate (22.7%), and Oregon the highest (56.7%). Across Oregon, Tennessee, Vermont, and Wisconsin, the mean census tract deprivation index was 0.38 (SD: 0.12) and racial ICE was 0.68 (SD: 0.44). Across all five states, the mean ZCTA deprivation index was 0.36 (SD: 0.09) and racial ICE was 0.80 (SD: 0.31).
Table 1.
Demographic characteristics by state
| New York | Oregon | Tennessee | Vermont | Wisconsin | |
|---|---|---|---|---|---|
| State-Level | N (%); mean±SD or median [IQR]a | ||||
| N | 15,793,754 | 3,369,741 | 5,487,594 | 489,144 | 1,580,505 |
| Female | 8,026,042 (50.8) | 1,696,111 (50.3) | 2,806,580 (51.1) | 245,406 (50.2) | 747,148 (47.3) |
| Age | 47.9±18.9 | 47.9±18.7 | 47.1±18.3 | 49.8±18.0 | 46.8±18.6 |
| Organ Donor Designation | 3,590,771 (22.7) | 1,911,506 (56.7) | 2,023,151 (36.9) | 252,505 (51.6) | 807,057 (51.1) |
| Census-tract Level | |||||
| N geocodedb | NA | 3,284,134 (97.5) | 5,208,888 (94.9) | 403,661 (82.5)c | 1,467,337 (92.8) |
| Number of tracts | NA | 825 | 1471 | 183 | 1389 |
| Deprivation Index | NA | 0.38±0.10 | 0.42±0.12 | 0.34±0.06 | 0.35±0.12 |
| Racial ICE | NA | 0.77±0.15 | 0.55±0.54 | 0.93±0.06 | 0.72±0.43 |
| Fraction Organ Donor Designation | NA | 0.57 [0.52,0.61] | 0.35 [0.28,0.42] | 0.51 [0.47,0.56] | 0.54[0.47,0.59] |
| ZCTA Level | |||||
| N matched to ZCTAd | 15,607,265 (98.8) | 3,273,679 (97.1) | 5,474,288 (99.8) | 474,902 (97.1) | 1,542,151 (97.6) |
| Number of ZCTAs | 1778 | 417 | 626 | 255 | 772 |
| Deprivation Index | 0.34±0.09 | 0.40±0.06 | 0.43±0.08 | 0.34±0.05 | 0.34±0.07 |
| Racial ICE | 0.76±0.35 | 0.84±0.13 | 0.77±0.38 | 0.94±0.06 | 0.88±0.21 |
| Fraction Organ Donor Designation | 0.28 [0.23,0.33] | 0.51 [0.46,0.67] | 0.33 [0.26,0.41] | 0.51 [0.46,0.67] | 0.53 [0.47,0.58] |
SD: standard deviation; IQR: interquartile range; ICE: index of concentration at the extreme; ZIP: Zone improvement plan
Continuous data presented as mean±SD when normally distributed and median [IQR] when non-normally distributed.
N geocoded refers to the total addresses that were successfully geocoded to a census tract within the state that had an associated deprivation index.
Of the 82,876 residents whose addresses were not geocoded, 73,465 (89%) were because the listed address was a post office box.
N matched to ZCTA refers to the total number of ZIP codes matched to a ZCTA within the respective state that had an associated deprivation index.
Census tract analyses
We geocoded 10,364,020 (94.8%) of available addresses from Oregon, Tennessee, Vermont, and Wisconsin to a census tract with valid deprivation index and racial ICE measures. This represents >95% of street addresses available from Oregon, Tennessee, and Wisconsin but just 83.1% of those from Vermont. Of Vermont records not geocoded, 89% were matched to Post Office boxes, which are not representative of a residential location.
Figure 1 depicts organ donor registration rates by census tract-level socioeconomic deprivation. For each 0.1 decrease in the deprivation index (i.e., 10% decrease in index-defined socioeconomic deprivation), the rate of organ donor registration increased by 6.8% (95%CI: 6.6%, 7.0%), adjusting for state. In other words, each 1 SD (i.e. 0.12) decrease in the deprivation index was associated with a 7.9% increase in the rate of organ donor registration. That is, less deprivation was associated with higher registration rates.
Figure 1. Organ donor registration by socioeconomic deprivation at the census tract level.
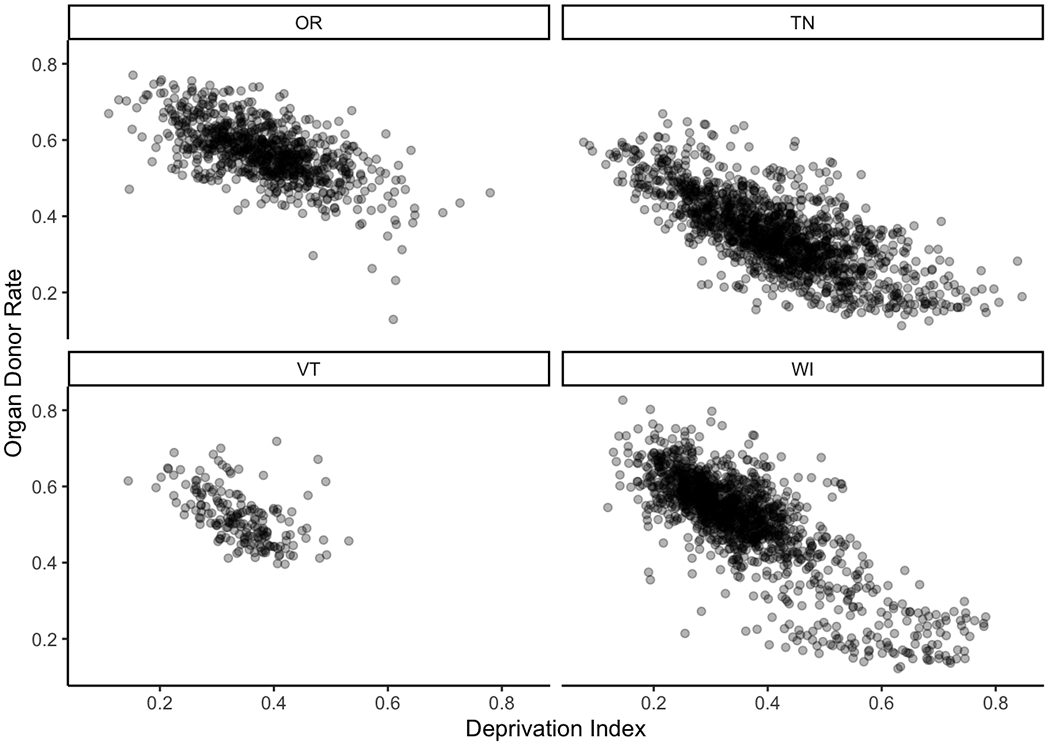
OR: Oregon; TN: Tennessee; VT: Vermont; WI: Wisconsin
There was a 6.8% (95%CI: 6.6%, 7.0%) increase in the rate of organ donor registration with each 0.1 decrease in the deprivation index, adjusting for the random effect of state. That is, with decreasing socioeconomic deprivation, organ donor registration rates increased.
Figure 2 depicts organ donor registration rates by census tract-level racial ICE. For each 0.1 increase in racial ICE, the adjusted organ donor registration rate increased by 1.5% (95%CI: 1.5%, 1.6%), adjusting for state. By extension, each 1 SD (i.e. 0.44) increase in the racial ICE was associated with a 6.7% increase in the rate of organ donor registration, illustrating that areas with predominately white residents had higher registration rates.
Figure 2. Organ donor registration by racial index of concentration at the extreme at the census tract level.
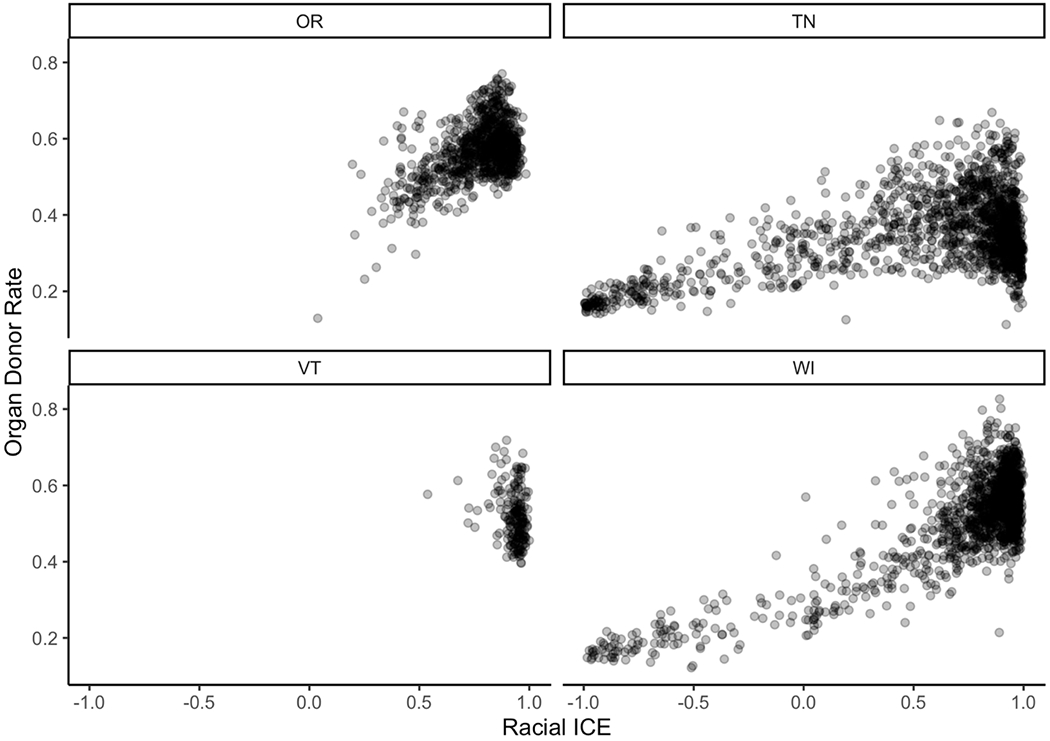
OR: Oregon; TN: Tennessee; VT: Vermont; WI: Wisconsin; ICE: Index of Concentration at the Extreme
There was a 1.5% (95%CI: 1.5%, 1.6%) increase in the rate of organ donor registration with each 0.1 increase in the racial ICE, adjusting for the random effect of state. That is, with increasing proportions of white residents, organ donor registration rates increased.
When both socioeconomic deprivation and racial ICE were included in the same state-adjusted model, each 0.1 decrease in socioeconomic deprivation was associated with a 5.2% (95%CI: 5.0%, 5.4%), and each 0.1 increase in racial ICE a 0.7% (95%CI: 0.7%, 0.8%), increase in organ donor registration, adjusting for state. In other words, each 1 SD (i.e. 0.12) decrease in the deprivation index was associated with a 6.2% increase in organ donor registration and each 1 SD (i.e. 0.44) increase in the racial ICE was associated with a 3.1% increase in organ donor registration.
ZCTA Analyses
Using data from all five states, we matched 26,372,285 (98.7%) of available ZIP codes to corresponding ZCTAs with valid deprivation index and racial ICE measures. Figure 3 depicts organ donor registration rates by ZCTA-level socioeconomic deprivation. Now including New York, we found that for each 0.1 decrease in the deprivation index, the organ donor registration rate increased by 3.8% (95%CI: 3.5%, 4.1%), adjusting for state. Thus, each 1 SD (i.e. 0.09) decrease in the deprivation index was associated with a 3.3% increase in the rate of organ donor registration.
Figure 3. Organ donor registration by socioeconomic deprivation at the ZCTA level.
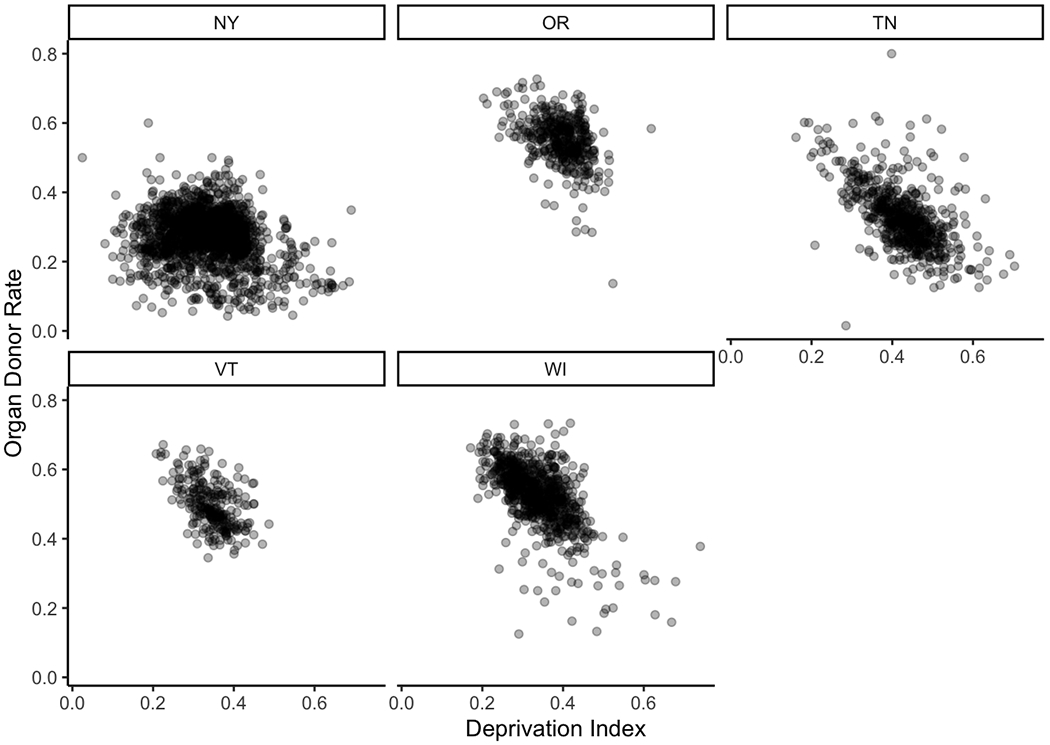
NY: New York; OR: Oregon; TN: Tennessee; VT: Vermont; WI: Wisconsin; ZCTA: ZIP code tabulation area
There was a 3.8% (95%CI: 3.5%, 4.1%) increase in the rate of organ donor registration with each 0.1 decrease in the deprivation index, adjusting for the random effect of state. That is, with decreasing socioeconomic deprivation, organ donor registration rates increased. When New York was excluded (to compare ZCTA analyses to census tract analyses), there was a 7.0% (95%CI: 6.6%, 7.5%) increase in the rate of organ donor registration with each 0.1 decrease in the deprivation index, adjusting for the random effect of state.
Similarly, Figure 4 depicts organ donor registration rates by racial ICE. Here, for each 0.1 increase in ZCTA-level racial ICE, the organ donor registration rate increased by 1.0% (95%CI: 1.0%, 1.1%), adjusting for state. Each 1 SD (i.e. 0.31) increase in the racial ICE was associated with a 3.2% increase in the rate of organ donor registration.
Figure 4. Organ donor registration by racial index of concentration at the extreme at the ZIP code level.
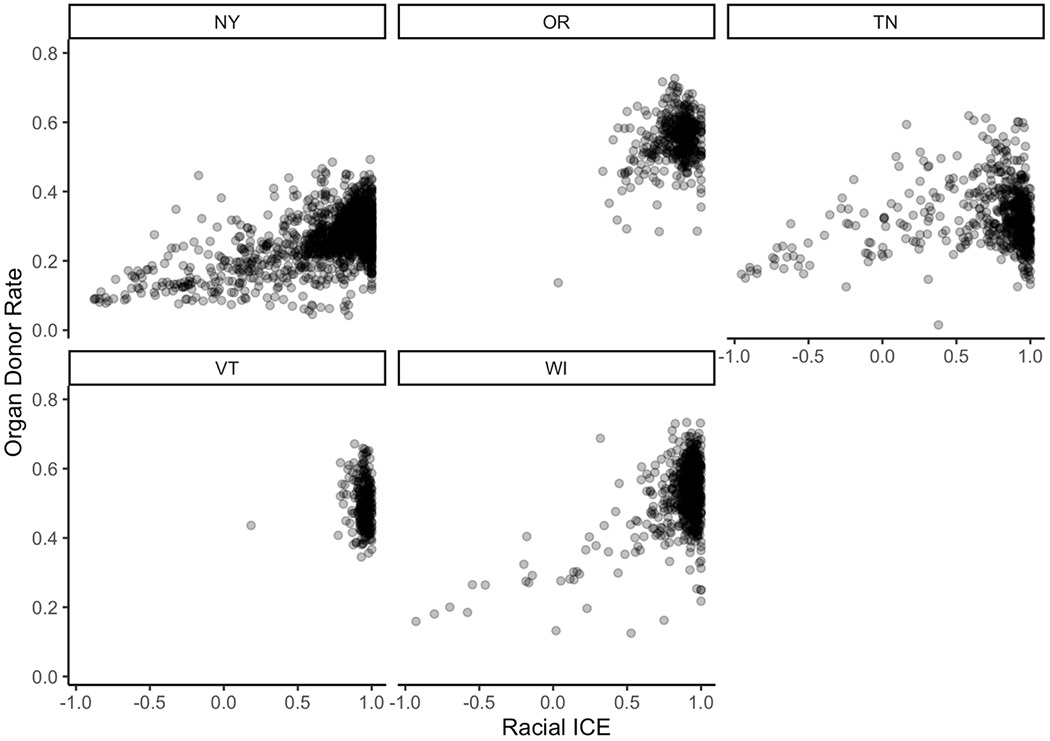
NY: New York; OR: Oregon; TN: Tennessee; VT: Vermont; WI: Wisconsin; ICE: Index of Concentration at the Extreme
There was a 1.0% (95%CI: 1.0%, 1.1%) increase in the rate of organ donor registration with each 0.1 increase in the racial ICE, adjusting for the random effect of state. That is, with increasing proportions of white residents, organ donor registration rates increased. When New York was excluded (to compare ZCTA analyses to census tract analyses), there was a 0.9% (95%CI: 0.7%, 1.0%) increase in the rate of organ donor registration with each 0.1 increase in the racial ICE, adjusting for the random effect of state.
When socioeconomic deprivation and racial ICE were both included in the ZCTA-level model, each 0.1 decrease in socioeconomic deprivation was associated with a 3.0% (95%CI: 2.7%, 3.3%), and each 0.1 increase in racial ICE a 0.8% (95%CI: 0.7%, 0.9%), increase in organ donor registration, adjusting for state. By extension, each 1 SD (i.e. 0.09) decrease in the deprivation index was associated with a 2.7% increase in organ donor registration; each 1 SD (i.e. 0.31) increase in the racial ICE was associated with a 3.1% increase in organ donor registration.
Sensitivity analyses
We repeated the above analyses at the ZCTA level for just Oregon, Tennessee, Vermont, and Wisconsin—excluding New York. In these state-adjusted models, our ZCTA- and census tract-level findings were quite similar. Indeed, we found that for each 0.1 decrease in the ZCTA-level socioeconomic deprivation index, the organ donor registration rate increased by 7.0% (95%CI: 6.6%, 7.5%). For each 0.1 increase in racial ICE, the registration rate increased by 0.9% (95%CI: 0.7%, 1.0%). Finally, when both socioeconomic deprivation and racial ICE were included in the same model, each 0.1 decrease in socioeconomic deprivation was associated with a 6.7% (95%CI: 6.3%, 7.1%), and each 0.1 increase in racial ICE a 0.3% (95%CI: 0.2%, 0.5%), increase in organ donor registration.
DISCUSSION
This is the first study to examine the relationship between ecological measures of socioeconomic deprivation and racial segregation on organ donor registration. Areas of lower socioeconomic deprivation and higher concentrations of white residents have higher rates of organ donor registration. Of note, in our multivariable analyses that included both the socioeconomic deprivation index and the racial ICE, the effect of racial ICE was decreased; suggesting that the effect of racial ICE on organ donor registration may be mediated, in part, by socioeconomic deprivation. While most previous studies focused on individual determinants of organ donor registration,6,7,12,33 these data add to our limited understanding of contextual, geospatial determinants of organ donor registration.15–17
If registration rates were equal to the top quartile ZCTAs in our sample, there would be an extra 2.4 million registered donors from these five states alone—representing a 28% increase in available donors across these states. Nationally, a 28% increase in organ donor registration rates would result in 42 million additional registered donors.8 Such an increase could begin to fill the substantial gap between organ need and supply. This possibility highlights an opportunity: increasing rates in low registration areas may lead to efficient increases in organ availability.
As we consider these public health-oriented implications, we acknowledge state-level variation in the relationship between socioeconomic deprivation and organ donor registration could exist given their relatively different socioeconomic and racial compositions. Since our findings using only Oregon, Tennessee, Vermont, and Wisconsin at both the tract- and ZCTA-level were not meaningfully different from one another, we conclude that the difference in findings after including New York was not due to differing spatial resolutions or ecological bias but might reflect inherent differences between New York and other states. Specifically, New York had lower rates of registration across all degrees of socioeconomic deprivation. Ladin, et al.16 demonstrated that decreased social capital partly explains geospatial variation in organ donor registration rates in Massachusetts. Thus, it is possible that differences in social capital across the states in our study could partially explain differences observed between models with and without New York. Indeed, in a recent report by the U.S. Congress Joint Economic Committee,34 Tennessee and New York had lower rates of social capital than Oregon, Vermont, and Wisconsin. In our sample, we observe that residents of Tennessee and New York had the lowest rates of organ donor registration. We posit that measures of area socioeconomic deprivation and social capital capture distinct but overlapping neighborhood characteristics.
Our findings align, in some ways, with those reported by Sasson, et al.35 who demonstrated that bystanders are less likely to initiate cardio-pulmonary resuscitation in poor, black neighborhoods compared to wealthy, white neighborhoods. Our findings may be driven by similar root causes, reasons that are likely multi-factorial and may include diminished trust in the healthcare system, misperceptions about organ donation,7 and alienation from the society to which they are donating.36 Indeed, in a qualitative study, African Americans expressed distrust in organ donation and the healthcare system writ large.7 Future studies evaluating why people from more deprived, segregated neighborhoods are less likely to register for organ donation may identify opportunities for interventions to improve registration rates. If we are to seek increased registration rates for organ donation that extend across populations, we must also demand that the health system build trust with and unravel generations of inequities felt by marginalized groups.37–39
Legislative policies and public health initiatives could be employed to increase registration rates across populations. One strategy could be to adopt ‘opt out’ legislation, the concept of registering all individuals as organ donors unless they explicitly decline.40 Alternatively, neighborhood context and geospatial data could inform tailored public health strategies to increase registration across communities. Prior research demonstrated that community-based organ donor registration interventions utilizing trusted community members and providing immediate opportunities to register have high rates of success.13 Still, such interventions require investment in training community leaders, and the cost-effectiveness of such investments is unclear.41 Such data may allow stakeholders (e.g., policy makers, local health departments, and DonateLife) to design public health campaigns to target segments of the population less likely to register as donors. Just as geospatial strategies are used by local public health officials to monitor chronic disease prevalence and morbidity locally,42 we suggest they could also be used to bolster organ donation rates. As we seek to improve organ availability, more granular and transparent public health data may inform targeted efforts to improve registration rates. Such public health interventions have successfully been applied to infectious disease and cancer surveillance.43–45 Previous studies utilizing state BMV data have only been single state11,15–17,46 and may not be generalizable. That this study identified population-level metrics strongly associated with organ donor registration across multiple, diverse states is a step closer towards implementing similar though novel strategies to improve organ availability. In line with precision public health (i.e., delivering the right intervention to the right population at the right time),10 geospatial-informed initiatives could realize meaningful increases in the number of organ donors, and transplantable organs, in the U.S., ultimately improving outcomes for those awaiting organ transplantation.
This study has several strengths. First, we utilized data from five geographically diverse states, making this, to our knowledge, the largest accrued dataset examining the geospatial distribution of organ donor registration rates. This allowed us to enumerate variation in organ donor registration across states and evaluate associations with underlying contextual factors. Previous work by Reibel, Olmo, Andrada, and Koertzen46 identified clusters of socio-cultural characteristics associated with areas with low rates of organ donors. While this study enumerated several important factors, including socioeconomic and racial measures, the authors acknowledged that their findings may not be generalizable to the rest of the U.S. Our study utilized indices available for every census tract in the United States and our use of mixed-effects regression models further strengthen the generalizability of our study. Second, many studies on organ donor registration use subjective assessments of ‘intent to register.’ Our study is strengthened by the use of an objective, legally binding indicator of donor status physically present on drivers’ licenses or state identification cards. Third, across four states, we were able to use geocoded street addresses to obtain census tract data, an ideal geospatial resolution to conduct area-based studies.26,47
Despite these strengths, we acknowledge limitations. First, we only included data from five states, and it is possible these findings may not generalize. That said, the included states are diverse geographically and demographically; the sample includes ~8% of the U.S. population. Furthermore, our models incorporate the random effect of state to account for state-level variation, providing further evidence that our results will extrapolate past these five states. Second, the BMVs in the included states do not provide data on an individual’s income, race, or ethnicity. Therefore, we cannot determine if the area-based socioeconomic deprivation index and the racial ICE are surrogate measures of individual/household characteristics (socioeconomic status and race, respectively) or if these findings are indicative of geospatial factors that affect organ donor registration. We posit that the deprivation index and racial ICE serve both as surrogates for individual/household characteristics while also providing data that contextualize the neighborhoods for BMV registrants.47 This study lays the groundwork for future studies that explore how both individual- and area-based measures influence organ donor registration. Third, our measure of racial ICE only includes non-Hispanic white and black residents. Admittedly, this measure does not incorporate Hispanic residents and may not adequately capture the effect of Hispanic enclaves on organ donor registration rates. Since we were primarily interested in the influence of race--as a social construct--on organ donor rates, our use of the two groups at the extremes of racial privilege provides powerful evidence that inequitable race relations contribute to variation in organ donor registration. Clearly, further investigation into the intersection of ethnicity and organ donor registration is necessary. Fourth, we were unable to obtain street addresses for New York BMV registrants. In sensitivity analyses, the results at the census tract and ZCTA levels for the other four states were similar; suggesting that the ZCTA analyses provide important insights into organ donor registration behaviors across states that may not have easily accessible address data. Fifth, we sought to determine if the differences by racial ICE were, in part, mediated by socioeconomic deprivation. However, these two constructs are closely related, therefore, these models may violate positivity assumptions. Supplemental Figure 1 depicts the relationship between socioeconomic deprivation and racial ICE for our sample. Sixth, it is possible that individuals may not register for organ donation at their state BMV but subsequently register through an alternate mechanism. Since the BMV is the most common source of new organ donor registration,48 we believe data on those alternative registration strategies would not fundamentally alter our findings.
Our data provide evidence that neighborhood socioeconomic deprivation and racial segregation influence the decision to register as an organ donor. Further work to characterize reasons for disparate rates of organ donor registration across areas may elucidate targets for intervention. Policies and public health initiatives aimed at increasing the number of donors should consider neighborhood context and seek tailored strategies to increase registration across populations.
Supplementary Material
Supplemental Figure 1. Scatterplots of neighborhood socioeconomic deprivation and racial index of concentration at the extreme (a) at the census tract level and (b) at the ZCTA level. ZCTA: zip code tabulation area
ACKNOWLEDGEMENTS
Funding:
NIH T32 DK 7727–24 (PI: L. Denson; support for S.I.W.); The research reported was partially supported by the Arnold W. Strauss Fellow Award at Cincinnati Children’s Hospital Medical Center. The funders had no role in study design, data analysis, or decision to publish these findings.
Abbreviations:
- ACS
American Community Survey
- BMV
Bureau of Motor Vehicles
- ICE
Index of concentration at the extreme
- ZCTA
ZIP Code Tabulation Area
Footnotes
DISCLOSURES
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
DATA AVAILABILITY STATEMENT
Research data are not shared.
REFERENCES
- 1.National Data - OPTN. Published September 24, 2019. Accessed September 24, 2019. https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/#
- 2.Goldberg DS, French B, Forde KA, et al. Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA. 2014;311(12):1234–1243. doi: 10.1001/jama.2014.2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braun HJ, Perito ER, Dodge JL, Rhee S, Roberts JP. Nonstandard Exception Requests Impact Outcomes for Pediatric Liver Transplant Candidates. Am J Transplant. 2016;16(11):3181–3191. doi: 10.1111/ajt.13879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ross K, Patzer RE, Goldberg DS, Lynch RJ. Sociodemographic Determinants of Waitlist and Posttransplant Survival Among End-Stage Liver Disease Patients. American Journal of Transplantation. 2017;17(11):2879–2889. doi: 10.1111/ajt.14421 [DOI] [PubMed] [Google Scholar]
- 5.Israni AK, Zaun D, Rosendale JD, Schaffhausen C, Snyder JJ, Kasiske BL. OPTN/SRTR 2017 Annual Data Report: Deceased Organ Donation. Am J Transplant. 2019;19 Suppl 2:485–516. doi: 10.1111/ajt.15280 [DOI] [PubMed] [Google Scholar]
- 6.Siminoff LA, Gordon N, Hewlett J, Arnold RM. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA. 2001;286(1):71–77. doi: 10.1001/jama.286.1.71 [DOI] [PubMed] [Google Scholar]
- 7.Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. Journal of general internal medicine. 2006;21(9):995–1000. doi: 10.1111/j.1525-1497.2006.00516.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donate Life America Annual Report. Donate Life America; 2019. [Google Scholar]
- 9.Traino HM, Siminoff LA. Attitudes and acceptance of First Person Authorization: A national comparison of donor and nondonor families. J Trauma Acute Care Surg. 2013;74(1):294–300. doi: 10.1097/TA.0b013e318270dafc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bayer R, Galea S. Public Health in the Precision-Medicine Era. New England Journal of Medicine. 2015;373(6):499–501. doi: 10.1056/NEJMp1506241 [DOI] [PubMed] [Google Scholar]
- 11.Sehgal NK, Scallan C, Sullivan C, et al. The Relationship Between Verified Organ Donor Designation and Patient Demographic and Medical Characteristics. Am J Transplant. 2016;16(4):1294–1297. doi: 10.1111/ajt.13608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldberg DS, Halpern SD, Reese PP. Deceased Organ Donation Consent Rates Among Racial and Ethnic Minorities and Older Potential Donors. Critical Care Medicine. 2013;41(2):496–505. doi: 10.1097/CCM.0b013e318271198c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deedat S, Kenten C, Morgan M. What are effective approaches to increasing rates of organ donor registration among ethnic minority populations: a systematic review. BMJ Open. 2013;3(12):e003453. doi: 10.1136/bmjopen-2013-003453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andrews AM, Zhang N, Magee JC, Chapman R, Langford AT, Resnicow K. Increasing donor designation through black churches: results of a randomized trial. Progress in Transplantation. 2012;22(2):161–167. doi: 10.7182/pit2012281 [DOI] [PubMed] [Google Scholar]
- 15.Grubesic TH. Driving donation: a geographic analysis of potential organ donors in the state of Ohio, USA. Soc Sci Med. 2000;51(8):1197–1210. doi: 10.1016/s0277-9536(00)00030-7 [DOI] [PubMed] [Google Scholar]
- 16.Ladin K, Wang R, Fleishman A, Boger M, Rodrigue JR. Does Social Capital Explain Community-Level Differences in Organ Donor Designation? Milbank Q. 2015;93(3):609–641. doi: 10.1111/1468-0009.12139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shacham E, Loux T, Barnidge EK, Lew D, Pappaterra L. Determinants of organ donation registration. American Journal of Transplantation. 2018;18(11):2798–2803. doi: 10.1111/ajt.15025 [DOI] [PubMed] [Google Scholar]
- 18.Putnam Robert D.. The Prosperous Community: Social Capital and Public Life. The American Prospect. 1993;(13):35–42. [Google Scholar]
- 19.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures--the public health disparities geocoding project. Am J Public Health. 2003;93(10):1655–1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping Neighborhood Health Geomarkers To Clinical Care Decisions To Promote Equity In Child Health. Health Aff (Millwood). 2017;36(6):999–1005. doi: 10.1377/hlthaff.2016.1425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miranda ML, Dolinoy DC, Overstreet MA. Mapping for prevention: GIS models for directing childhood lead poisoning prevention programs. Environ Health Perspect. 2002;110(9):947–953. doi: 10.1289/ehp.02110947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miranda ML, Ferranti J, Strauss B, Neelon B, Califf RM. Geographic health information systems: a platform to support the “triple aim.” Health Aff (Millwood). 2013;32(9):1608–1615. doi: 10.1377/hlthaff.2012.1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nicholas SW, Jean-Louis B, Ortiz B, et al. Addressing the Childhood Asthma Crisis in Harlem: The Harlem Children’s Zone Asthma Initiative. Am J Public Health. 2005;95(2):245–249. doi: 10.2105/AJPH.2004.042705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaufman S, Ali N, DeFiglio V, Craig K, Brenner J. Early Efforts to Target and Enroll High-Risk Diabetic Patients Into Urban Community-Based Programs. Health Promotion Practice. 2014;15(2_suppl):62S–70S. doi: 10.1177/1524839914535776 [DOI] [PubMed] [Google Scholar]
- 25.Brokamp C, Wolfe C, Lingren T, Harley J, Ryan PH. Decentralized and reproducible geocoding and characterization of community and environmental exposures for multi-site studies. Journal of American Medical Informatics Association. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krieger N, Waterman P, Chen JT, Soobader MJ, Subramanian SV, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and US census-defined geographic areas-the Public Health Disparities Geocoding Project. Am J Public Health. 2002;92(7):1100–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Census Bureau. Glossary. Published September 26, 2019. Accessed January 21, 2020. https://www.census.gov/programs-surveys/geography/about/glossary.html#par_textimage_13
- 28.Brokamp C, Beck AF, Goyal NK, Ryan P, Greenberg JM, Hall ES. Material community deprivation and hospital utilization during the first year of life: an urban population–based cohort study. Annals of Epidemiology. Published online November 29, 2018. doi: 10.1016/j.annepidem.2018.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wadhwani SI, Beck AF, Bucuvalas J, Gottlieb L, Kotagal U, Lai JC. Neighborhood socioeconomic deprivation is associated with worse patient and graft survival following pediatric liver transplantation. Am J Transplant. Published online January 20, 2020:ajt.15786. doi: 10.1111/ajt.15786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wadhwani SI, Bucuvalas JC, Brokamp C, et al. Association between neighborhood-level socioeconomic deprivation and the Medication Level Variability Index for children following liver transplantation. Transplantation. Published online January 19, 2020. doi: 10.1097/TP.0000000000003157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krieger N, Feldman JM, Waterman PD, Chen JT, Coull BA, Hemenway D. Local Residential Segregation Matters: Stronger Association of Census Tract Compared to Conventional City-Level Measures with Fatal and Non-Fatal Assaults (Total and Firearm Related), Using the Index of Concentration at the Extremes (ICE) for Racial, Economic, and Racialized Economic Segregation, Massachusetts (US), 1995–2010. J Urban Health. 2017;94(2):244–258. doi: 10.1007/s11524-016-0116-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beck AF, Riley CL, Taylor SC, Brokamp C, Kahn RS. Pervasive Income-Based Disparities In Inpatient Bed-Day Rates Across Conditions And Subspecialties. Health Aff (Millwood). 2018;37(4):551–559. doi: 10.1377/hlthaff.2017.1280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boulware LE, Ratner LE, Cooper LA, Sosa JA, LaVeist TA, Powe NR. Understanding disparities in donor behavior: race and gender differences in willingness to donate blood and cadaveric organs. Medical care. 2002;40(2):85–95. [DOI] [PubMed] [Google Scholar]
- 34.The Geography of Social Capital in America. US Congress Joint Economic Committee; 2018. Accessed March 11, 2020. https://www.jec.senate.gov/public/index.cfm/republicans/2018/4/the-geography-of-social-capital-in-america
- 35.Sasson C, Magid DJ, Chan P, et al. Association of Neighborhood Characteristics with Bystander-Initiated CPR. N Engl J Med. 2012;367(17):1607–1615. doi: 10.1056/NEJMoa1110700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Newton JD. How does the general public view posthumous organ donation? A meta-synthesis of the qualitative literature. BMC Public Health. 2011;11(1):791. doi: 10.1186/1471-2458-11-791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–365. doi: 10.1093/phr/118.4.358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wasserman J, Flannery MA, Clair JM. Raising the ivory tower: the production of knowledge and distrust of medicine among African Americans. J Med Ethics. 2007;33(3):177–180. doi: 10.1136/jme.2006.016329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fairchild AL, Bayer R. Uses and abuses of Tuskegee. Science. 1999;284(5416):919–921. doi: 10.1126/science.284.5416.919 [DOI] [PubMed] [Google Scholar]
- 40.Shepherd L, O’Carroll RE, Ferguson E. An international comparison of deceased and living organ donation/transplant rates in opt-in and opt-out systems: a panel study. BMC Med. 2014;12(1):131. doi: 10.1186/s12916-014-0131-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Golding SE, Cropley M. A Systematic Narrative Review of Effects of Community-Based Intervention on Rates of Organ Donor Registration. Prog Transplant. 2017;27(3):295–308. doi: 10.1177/1526924817715461 [DOI] [PubMed] [Google Scholar]
- 42.Miranda ML, Casper M, Tootoo J, Schieb L. Putting chronic disease on the map: building GIS capacity in state and local health departments. Prev Chronic Dis. 2013;10:E100. doi: 10.5888/pcd10.120321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dolley S Big Data’s Role in Precision Public Health. Front Public Health. 2018;6:68. doi: 10.3389/fpubh.2018.00068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dowell SF, Blazes D, Desmond-Hellmann S. Four steps to precision public health. Nature. 2016;540(7632):189–191. doi: 10.1038/540189a [DOI] [Google Scholar]
- 45.Khoury MJ, Iademarco MF, Riley WT. Precision Public Health for the Era of Precision Medicine. Am J Prev Med. 2016;50(3):398–401. doi: 10.1016/j.amepre.2015.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reibel M, Olmo C, Andrada S, Koertzen J. Deep Demographics: Understanding Local Variation in Donor Registration. Prog Transplant. 2016;26(2):191–198. doi: 10.1177/1526924816640670 [DOI] [PubMed] [Google Scholar]
- 47.Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: A multilevel analysis of Massachusetts births, 1989–1991. Am J Epidemiol. 2006;164(9):823–834. doi: 10.1093/aje/kwj313 [DOI] [PubMed] [Google Scholar]
- 48.Siegel JT, Tan CN, Rosenberg BD, et al. Anger, frustration, boredom and the Department of Motor Vehicles: Can negative emotions impede organ donor registration? Social Science & Medicine. 2016;153:174–181. doi: 10.1016/j.socscimed.2016.02.013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Scatterplots of neighborhood socioeconomic deprivation and racial index of concentration at the extreme (a) at the census tract level and (b) at the ZCTA level. ZCTA: zip code tabulation area


