Abstract
Background:
For many patients, health care needs increase toward the end of life, but little is known about the extent of outpatient physician care during that time. The objective of this study was to describe the volume and mix of outpatient physician care over the last 12 months of life among patients dying with different end-of-life trajectories.
Methods:
We conducted a retrospective descriptive study involving adults (aged ≥ 18 yr) who died in Ontario between 2013 and 2017, using linked provincial health administrative databases. Decedents were grouped into 5 mutually exclusive end-of-life trajectories (terminal illness, organ failure, frailty, sudden death and other). Over the last 12 months and 3 months of life, we examined the number of physician encounters, the number of unique physician specialties involved per patient and specialty of physician, the number of unique physicians involved per patient, the 5 most frequent types of specialties involved and the number of encounters that took place in the home; these patterns were examined by trajectory.
Results:
Decedents (n = 359 559) had a median age of 78 (interquartile range 66–86) years. The mean number of outpatient physician encounters over the last year of life was 16.8 (standard deviation [SD] 13.7), of which 9.0 (SD 9.2) encounters were with family physicians. The mean number of encounters ranged from 11.6 (SD 10.4) in the frailty trajectory to 24.2 (SD 15.0) in the terminal illness trajectory across 3.1 (SD 2.0) to 4.9 (SD 2.1) unique specialties, respectively. In the last 3 months of life, the mean number of physician encounters was 6.8 (SD 6.4); a mean of 4.1 (SD 5.4) of these were with family physicians.
Interpretation:
Multiple physicians are involved in outpatient care in the last 12 months of life for all end-of-life trajectories, with family physicians as the predominant specialty. Those who plan health care models of the end of life should consider support for family physicians as coordinators of patient care.
The aging of the population has resulted in a shift from most deaths being sudden and unexpected, to increasing numbers of people living with at least 1 progressive life-limiting illness for a period of months to years before dying.1–4 End-of-life health care patterns have typically been described in terms of the spike in acute care services and initiation of palliative care services late in the illness trajectory.5–9
For many patients, there is evidence of recognizable functional decline at least a year before death,10,11 necessitating comprehensive care from physicians in the community. 7,12 The patterns of physician care provided in the community have impacts on the use of higher-acuity health care. For example, higher continuity of physician care and home visits for older patients with complex health care needs or patients nearing end of life are associated with reduced acute care use and health care system costs.13–17 Medical specialists are often thought to provide care for the specific illness(es) that may be contributing to patients’ decline (e.g., oncologist for cancer or cardiologist for heart disease that may be life limiting), whereas family physicians may play the coordinating role.18 Medical specialists may step back as patients move closer to death and are transitioned to palliative and end-of-life care. These patterns vary by the illness trajectory. Patients dying of organ failure or dementia are less likely to receive palliative care services, or they receive them closer to the end of life, compared with patients with cancer.9,19
Given that end-of-life health care needs for most patients are relevant over the last year of life, and given the variability of palliative care services for different patient populations, it is important to understand the patterns of physician care in the community for health care system planning. The objective of this study was to describe the volume and mix of outpatient physician care over the last 12 and 3 months of life among patients dying with different end-of-life trajectories, including with cancer, organ failure, frailty and sudden (i.e., likely unforeseen) death.
Methods
Study design and data sources
We conducted a retrospective study using linked population-based health administrative databases in Ontario, Canada, held at ICES. ICES is an independent, nonprofit research institute; its holdings include databases from a comprehensive set of health care sectors in Ontario, which has a population of more than 14 million residents with publicly funded health care coverage. These data sets were linked using unique encoded identifiers and analyzed at ICES.
Study cohort
We created a cohort including all adult (aged ≥ 18 yr) decedents who died between Jan. 1, 2013, and Dec. 31, 2017. We excluded decedents who were older than 105 years at death (in case of administrative error), who were ineligible for insured health services through the Ontario Health Insurance Plan (OHIP) at any point in the last year of life, who had an address outside Ontario at the time of death, who had no health care encounters in the 5 years before death, who spent any days in a long-term care home in the last year of life, who had no outpatient encounters in the last year of life, or who had no cause of death listed. Deaths and cause of death were captured through the Ontario Office of the Registrar General — Deaths database (see Appendix 1 for a description of the databases, available at www.cmajopen.ca/content/9/2/E613/suppl/DC1).
We categorized decedents by the major trajectories of functional decline at end of life, defined by main cause of death, as per prior research.1,19,20 Using International Classification of Diseases, 10th Revision (ICD-10) codes, researchers conducted a modified Delphi process consisting of literature review (of studies describing clinically and functionally different end-of-life trajectories), expert opinion and cluster analysis to obtain consensus on which cause of death corresponded to the trajectories.21,22 The trajectory definitions demonstrated discriminant validity in that they were significantly different from each other in terms of health care utilization costs. They also discriminate in terms of initiation and intensity of palliative care services.9
Decedents were classified into the following trajectories: terminal illness (e.g., cancer), organ failure (e.g., chronic heart failure), frailty (e.g., Alzheimer disease), sudden death (i.e., unanticipated, such as an accident) and other. The top causes of death included cancers in the terminal illness trajectory; chronic respiratory- and cardiovascular-related causes in the organ failure trajectory; cardiovascular-, infection- and dementia-related causes in the frailty trajectory; accident-and injury-related causes in the sudden death trajectory; and infections, falls and ill-defined unspecified causes in the other trajectory. The top 15 causes of death in each trajectory can be found in Appendix 2, available at www.cmajopen.ca/content/9/2/E613/suppl/DC1.
Decedent characteristics
Demographic characteristics were determined using information in databases pertaining to the last year of life. Age at death and sex were obtained from the Registered Persons Database. Neighbourhood-level income quintile and rurality were estimated using the Postal Code Conversion File Plus, and patients’ postal codes were obtained from the Registered Persons Database.
A history of any comorbidities was determined looking back from 2008 up to death using previously developed algorithms that use diagnosis codes and medication data to assign conditions.23–32
Outcomes of interest
This study focused on physician encounters in the outpatient setting (as opposed to during a hospitalization) because we were interested in patterns of care in the community. These encounters were identified using physician claims to the OHIP database. Multiple billings by the same physician on the same visit date were considered 1 encounter. Management fee codes, which are codes used for care over a period of time, were not included, because the billing of the fee codes does not correspond 1-to-1 with an encounter.
We categorized physician specialty and identified unique physicians through OHIP billings. Billing codes are specific to each specialty, and billings also include a unique identifier for the submitting physician. In Ontario, any physician can bill palliative care fee codes, and in Canada, palliative care was not a designated specialty at the time of this study. Palliative care was not considered a separate specialty in analyses; however, most physicians who practise palliative care predominantly have certification as family physicians.33
Over the last 12 months and 3 months of life, we examined the number of physician encounters, the number of unique physician specialties involved per patient and specialty of physician, the number of unique physicians involved per patient, the 5 most frequent types of specialties involved and the number of encounters that took place in the home. These patterns were described across the 5 mutually exclusive illness trajectories. We also plotted the mean number of encounters for each month. The decision to describe different time horizons recognizes that care patterns may change closer to end of life as health worsens and needs increase.
Statistical analysis
Descriptive results are presented as proportions for categorical variables, and as means and standard deviations (SDs) or medians (with interquartile ranges for variables with skewed distribution) for continuous variables. Results are presented by end-of-life trajectory. All analyses were completed using SAS Enterprise Guide v. 7.15.
Ethics approval
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a research ethics board.
Results
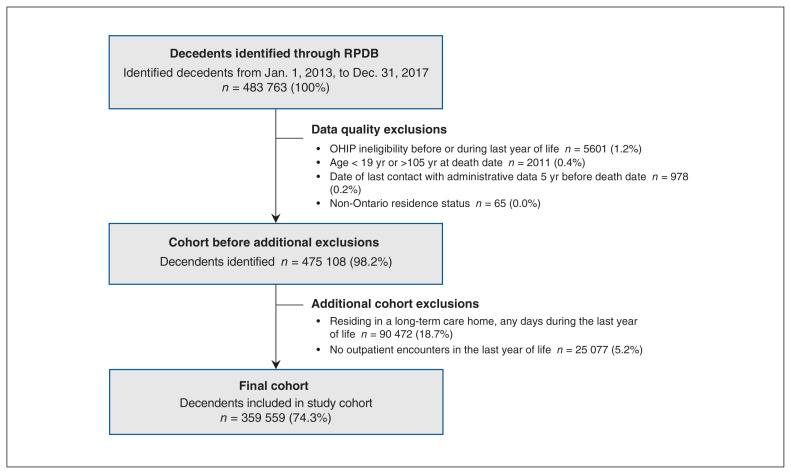
From Jan. 1, 2013, to Dec. 31, 2017, after 8655 exclusions owing to data quality, there were 475 108 deaths among individuals aged 18 years and older. After further exclusion of 90 472 (18.7%) residing in a long-term care home and 25 077 (5.2%) with no outpatient physician encounters in the last year of life, there were 359 559 decedents available for analysis (Figure 1). The mean age of decedents was 74.9 (SD 14.9) years, 46.4% were female and 13.5% resided in rural regions (Table 1). The distribution of illness trajectories was 34.8% terminal illness, 33.3% organ failure, 20.8% frailty, 5.3% sudden death and 5.8% other causes. Most decedents were older than 65 years in all trajectories except sudden death, in which 62.8% were younger than 65 years.
Figure 1:
Cohort creation flow diagram. Note: OHIP = Ontario Health Insurance Plan, RPDB = Registered Persons Database.
Table 1:
Profile of adult decedents who died between Jan. 1, 2013, and Dec. 31, 2017, in Ontario, Canada
| Characteristic | End-of-life trajectory; no. (%) of decedents* | Total cohort n = 359 559 |
||||
|---|---|---|---|---|---|---|
| Terminal illness n = 124 995 |
Organ failure n = 119 804 |
Frailty n = 74 750 |
Sudden death n = 19 023 |
Other n = 20 987 |
||
| Age at death, yr | ||||||
| 18–44 | 3031 (2.4) | 3120 (2.6) | 817 (1.1) | 5550 (29.2) | 997 (4.8) | 13 515 (3.8) |
| 45–54 | 8116 (6.5) | 5953 (5.0) | 2536 (3.4) | 3257 (17.1) | 1081 (5.2) | 20 943 (5.8) |
| 55–64 | 21 053 (16.8) | 13 978 (11.7) | 6861 (9.2) | 3145 (16.5) | 1978 (9.4) | 47 015 (13.1) |
| 65–74 | 32 901 (26.3) | 22 253 (18.6) | 11 903 (15.9) | 2247 (11.8) | 3068 (14.6) | 72 372 (20.1) |
| 75–84 | 35 864 (28.7) | 33 471 (27.9) | 20 006 (26.8) | 2291 (12.0) | 5416 (25.8) | 97 048 (27.0) |
| 85–94 | 22 000 (17.6) | 34 982 (29.2) | 26 472 (35.4) | 2204 (11.6) | 6923 (33.0) | 92 581 (25.7) |
| ≥ 95 | 2030 (1.6) | 6047 (5.0) | 6155 (8.2) | 329 (1.7) | 1524 (7.3) | 16 085 (4.5) |
| Mean ± SD | 72.6 ± 12.9 | 76.6 ± 14.1 | 79.8 ± 12.9 | 57.4 ± 21.0 | 77.2 ± 15.9 | 74.9 ± 14.9 |
| Median (IQR) | 74 (64–82) | 79 (68–87) | 83 (72–89) | 56 (41–75) | 82 (69–89) | 78 (66–86) |
| Sex, female | 59 222 (47.4) | 56 749 (47.4) | 33 795 (45.2) | 6671 (35.1) | 10 326 (49.2) | 166 763 (46.4) |
| Rural residence | 17 393 (13.9) | 17 033 (14.2) | 9209 (12.3) | 2427 (12.8) | 2346 (11.2) | 48 408 (13.5) |
| Neighbourhood income quintile | ||||||
| 1 (lowest) | 28 334 (22.7) | 31 063 (25.9) | 19 220 (25.7) | 5604 (29.5) | 5439 (25.9) | 89 660 (24.9) |
| 2 | 27 290 (21.8) | 26 817 (22.4) | 16 671 (22.3) | 4075 (21.4) | 4653 (22.2) | 79 506 (22.1) |
| 3 | 24 547 (19.6) | 22 890 (19.1) | 14 243 (19.1) | 3418 (18.0) | 4045 (19.3) | 69 143 (19.2) |
| 4 | 22 408 (17.9) | 20 171 (16.8) | 12 344 (16.5) | 2954 (15.5) | 3452 (16.4) | 61 329 (17.1) |
| 5 (highest) | 22 167 (17.7) | 18 555 (15.5) | 12 056 (16.1) | 2904 (15.3) | 3344 (15.9) | 59 026 (16.4) |
| Illness history | ||||||
| Cancer | 117 942 (94.4) | 30 615 (25.6) | 15 690 (21.0) | 2831 (14.9) | 5864 (27.9) | 172 942 (48.1) |
| CHF | 23 316 (18.7) | 53 610 (44.7) | 32 280 (43.2) | 2589 (13.6) | 7928 (37.8) | 119 723 (33.3) |
| COPD | 25 733 (20.6) | 38 608 (32.2) | 18 646 (24.9) | 2351 (12.4) | 5134 (24.5) | 90 472 (25.2) |
| Renal disease | 27 435 (21.9) | 41 726 (34.8) | 23 054 (30.8) | 2606 (13.7) | 6983 (33.3) | 101 804 (28.3) |
Note: CHF = congestive heart failure, COPD = chronic obstructive pulmonary disease, IQR = interquartile range, SD = standard deviation.
Unless stated otherwise.
The mean number of physician encounters in outpatient settings was 16.8 (SD 13.7) over the last 12 months of life, involving a mean of 3.9 (SD 2.2) unique specialties and 5.9 (SD 4.0) unique physicians (Table 2). In the last 12 months and 3 months of life, decedents in the terminal illness trajectory experienced the highest mean number of outpatient physician encounters and the highest mean number of unique specialties and unique physicians, whereas decedents in the frailty trajectory experienced the lowest mean number of encounters. Decedents in the sudden death trajectory also experienced a lower mean number of outpatient physician encounters, with 11.9 (SD 12.1) encounters. The mean number of encounters was highest for family physicians, which was greater than for all other specialties combined in the last 12 months and 3 months of life. This was the case for all trajectories except terminal illness over the entire last 12 months of life, in which mean encounters with family physicians and other specialties combined were similar. The mean numbers among these encounters that took place in the home were 1.4 (SD 4.5, median 0) and 1.0 (SD 2.9, median 0) over the last 12 and 3 months of life, respectively.
Table 2:
Outpatient physician encounters in last 12 months and last 3 months of life among decedents who died in Ontario, Canada, from 2013 to 2017 by end-of-life trajectory
| Outcome of interest | End-of-life trajectory | Total cohort n = 359 559 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Terminal illness n = 124 995 |
Organ failure n = 119 804 |
Frailty n = 74 750 |
Sudden death n = 19 023 |
Other n = 20 987 |
||||||||
|
|
|
|
|
|
|
|||||||
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | |
| Last 12 months of life | ||||||||||||
|
| ||||||||||||
| No. encounters with all physicians | 24.2 ± 15.0 | 22 (14–32) | 13.6 ± 11.2 | 11 (6–18) | 11.6 ± 10.4 | 9 (4–16) | 11.9 ± 12.1 | 8 (4–16) | 13.5 ± 11.3 | 11 (5–18) | 16.8 ± 13.7 | 14 (7–23) |
|
| ||||||||||||
| No. home encounters with all physicians | 2.4 ± 5.7 | 0 (0–3) | 1.0 ± 3.7 | 0 (0–0) | 1.0 ± 3.4 | 0 (0–0) | 0.3 ± 2.3 | 0 (0–0) | 0.8 ± 3.0 | 0 (0–0) | 1.4 ± 4.5 | 0 (0–1) |
|
| ||||||||||||
| No. encounters with a family physician | 12.1 ± 10.6 | 10 (5–16) | 7.7 ± 7.9 | 6 (3–10) | 6.9 ± 7.5 | 5 (2–9) | 7.4 ± 9.2 | 5 (2–9) | 7.3 ± 7.7 | 5 (2–10) | 9.0 ± 9.2 | 7 (3–12) |
|
| ||||||||||||
| No. encounters with other specialties | 12.1 ± 9.7 | 10 (5–17) | 5.9 ± 6.8 | 4 (1–8) | 4.8 ± 6.1 | 3 (1–7) | 4.5 ± 6.5 | 2 (0–6) | 6.2 ± 7.3 | 4 (1–9) | 7.8 ± 8.4 | 5 (2–11) |
|
| ||||||||||||
| No. unique specialties involved | 4.9 ± 2.1 | 5 (3–6) | 3.6 ± 2.1 | 3 (2–5) | 3.1 ± 2.0 | 3 (2–4) | 2.8 ± 1.9 | 2 (1–4) | 3.6 ± 2.1 | 3 (2–5) | 3.9 ± 2.2 | 4 (2–5) |
|
| ||||||||||||
| No. unique physicians involved | 8.0 ± 4.0 | 8 (5–10) | 5.0 ± 3.4 | 4 (2–7) | 4.3 ± 3.2 | 3 (2–6) | 4.2 ± 3.4 | 3 (2–6) | 5.1 ± 3.6 | 4 (2–7) | 5.9 ± 4.0 | 5 (3–8) |
|
| ||||||||||||
| Last 3 months of life | ||||||||||||
|
| ||||||||||||
| No. encounters with all physicians | 10.2 ± 7.8 | 9 (5–13) | 5.1 ± 4.6 | 4 (2–7) | 4.3 ± 4.0 | 3 (2–6) | 4.3 ± 4.3 | 3 (2–6) | 5.1 ± 4.2 | 4 (2–7) | 6.8 ± 6.4 | 5 (2–9) |
|
| ||||||||||||
| No. home encounters with all physicians | 1.9 ± 4.1 | 0 (0–2) | 0.6 ± 2.0 | 0 (0–0) | 0.5 ± 1.6 | 0 (0–0) | 0.2 ± 1.3 | 0 (0–0) | 0.4 ± 1.5 | 0 (0–0) | 1.0 ± 2.9 | 0 (0–1) |
|
| ||||||||||||
| No. encounters with a family physician | 6.4 ± 7.0 | 4 (2–8) | 3.0 ± 3.8 | 2 (1–4) | 2.7 ± 3.2 | 2 (1–3) | 2.6 ± 3.4 | 2 (1–3) | 2.7 ± 3.3 | 2 (1–3) | 4.1 ± 5.4 | 3 (1–5) |
|
| ||||||||||||
| No. encounters with other specialties | 3.9 ± 3.8 | 3 (1–6) | 2.1 ± 2.6 | 1 (0–3) | 1.7 ± 2.3 | 1 (0–2) | 1.7 ± 2.5 | 1 (0–2) | 2.3 ± 2.8 | 1 (0–3) | 2.7 ± 3.2 | 2 (0–4) |
|
| ||||||||||||
| No. unique specialties involved | 2.9 ± 1.5 | 3 (2–4) | 2.2 ± 1.3 | 2 (1–3) | 2.0 ± 1.2 | 2 (1–3) | 1.9 ± 1.2 | 2 (1–2) | 2.3 ± 1.3 | 2 (1–3) | 2.4 ± 1.4 | 2 (1–3) |
|
| ||||||||||||
| No. unique physicians involved | 4.4 ± 2.4 | 4 (3–6) | 2.8 ± 1.9 | 2 (1–4) | 2.5 ± 1.7 | 2 (1–3) | 2.5 ± 1.8 | 2 (1–3) | 2.9 ± 1.9 | 2 (1–4) | 3.4 ± 2.2 | 3 (2–5) |
Note: IQR = interquartile range, SD = standard deviation.
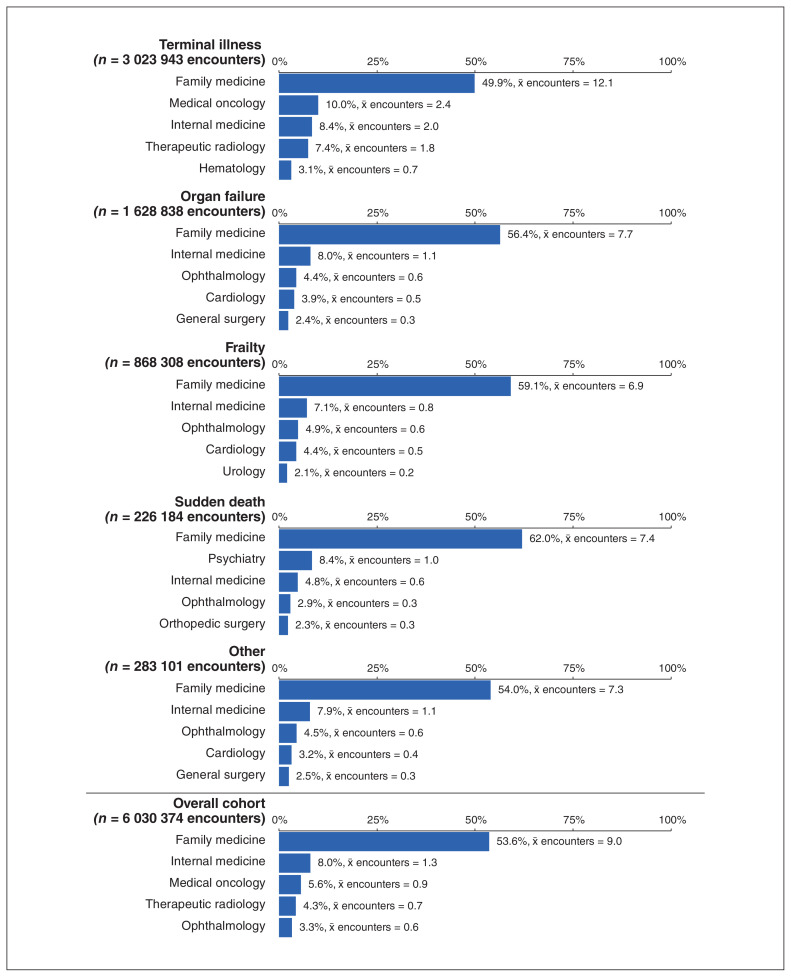
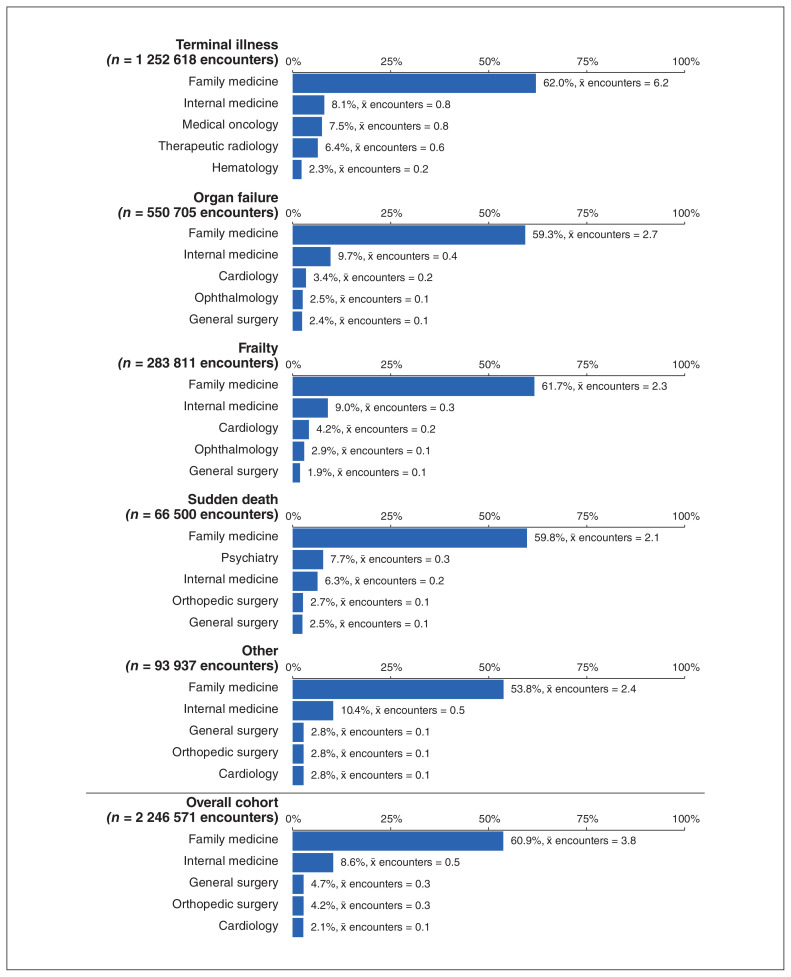
Figures 2 and 3 show the 5 physician specialties with the highest number of outpatient encounters across each trajectory in the last 12 and 3 months of life. Family medicine was the predominant specialty across all trajectories. In the last 12 months of life, internal medicine was the next most frequent for all trajectories except for the terminal illness trajectory, where medical oncology was the next most frequent, and sudden death, where psychiatry was second. Ophthalmology appeared in the top 5 specialties in all trajectories except for terminal illness. For the terminal illness trajectory, cancer-related specialties were predominant in the top 5.
Figure 2:
Proportion of outpatient physician encounters provided by the top 5 most common specialties and average number of encounters per patient provided by the specialty in last 12 months of life, among decedents who died in Ontario, Canada, from 2013 to 2017, by end-of-life trajectory. Note: χ̄ = mean.
Figure 3:
Proportion of outpatient physician encounters provided by the top 5 most common specialties and average number of encounters per patient provided by the specialty in last 3 months of life, among decedents who died in Ontario, Canada, from 2013 to 2017, by end-of-life trajectory. Note: χ̄ = mean.
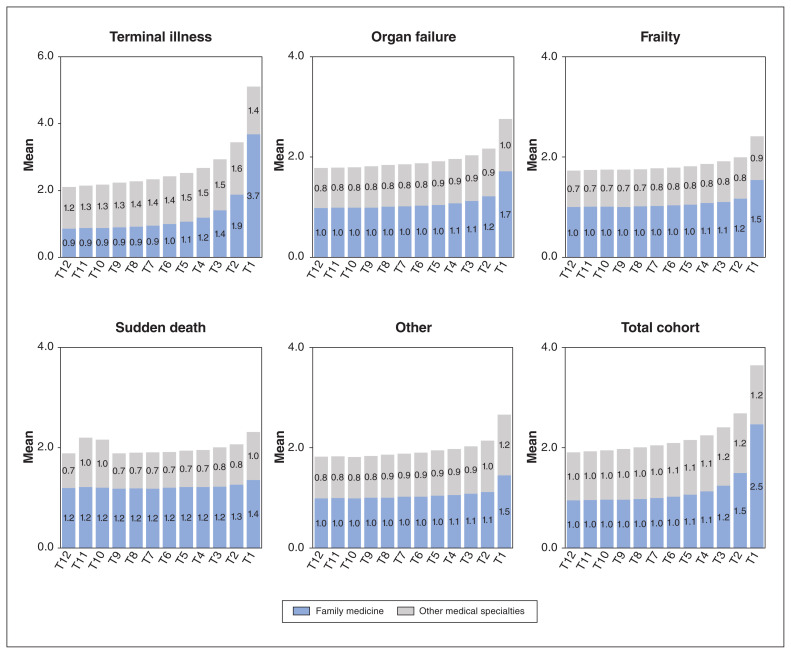
Figure 4 shows the monthly outpatient encounters with family physicians and all other specialty physicians over the last 12 months of life. The mean number of monthly outpatient encounters with family physicians was stable until about 4 months before the date of death, with the largest increase occurring during the second and last months of life. Decedents with terminal illness experienced slightly fewer family physician encounters until 4 months before death, when the mean number increased beyond the other trajectories.
Figure 4:
Monthly encounters with family physicians and other medical specialists in the last year of life, among decedents who died in Ontario, Canada, from 2013 to 2017, by end-of-life trajectory. Note: Months are defined as 30-day increments; T1 = 1–30 days before death date, T2 = 31–60 days before death date, etc.
Interpretation
In this retrospective study of outpatient physician care in the last year of life in Ontario, Canada, decedents had numerous encounters, predominantly with family physicians. The volume of outpatient physician encounters was, on average, nearly 2 per month and increased slightly in the last 4 months of life compared with earlier months. On average, fewer than 2 of the mean of 16 encounters in the last 12 months took place in the home. Decedents in the terminal illness trajectory experienced the highest number of outpatient physician encounters overall and the highest number of different physicians providing care, most of whom were cancer-related specialists.
Previous studies in Canada have described the use of hospitals and emergency departments as indicators of accessibility of end-of-life care in the community.8,34,35 Formal palliative care has also been described and is initiated for about half of decedents, mostly for patients with cancer and for a short time close to the end of life.8,36–38 By definition, palliative care should be initiated early and provided in the community;39 however, specialized palliative care teams in the community cannot meet all of the needs of the population. This necessitates viewing health care throughout the last year of life as an opportunity to address palliative needs. Therefore, it is important to understand overall patterns of care across the health care system when planning services for the end-of-life period, and in-patient hospital and palliative care services do not provide a full picture. This study fills a gap in knowledge regarding health care patterns over the end-of-life period, noting that across all end-of-life trajectories, family physicians provided most of the outpatient encounters alongside involvement of multiple other specialties.
Our results are consistent with descriptions of family physicians acting as the coordinators of care from multiple specialists, such as oncologists and internal medicine specialists. 40–42 In Canada, primary care is generally provided by a family physician, and other specialists can be accessed only through referral. It was surprising that family physician encounters remained generally consistent over time among decedents in the terminal illness trajectory, given reports that patients tend to see their physicians who specialize in cancer more than family physicians for much of their trajectory.43 Family physicians have important roles providing emotional support, management of other chronic conditions and health promotion.44
Consistent with other research, decedents with an organ failure trajectory in our study had the second highest number of encounters, as these individuals experience conditions such as heart, lung or renal disease, which require ongoing monitoring and management, and have high symptom burdens.45–47 Decedents in the frailty trajectory had the lowest volume of encounters, which may reflect the prolonged gradual decline1,48 and relative stability of frailty even in the last year of life.49 The variability in the rapidity and consistency of decline in noncancer compared with cancer end-of-life trajectories suggests that models of care need to be adaptable to accommodate different end-of-life trajectories.47,50 Decedents in the sudden death trajectory also had relatively fewer encounters, likely because they were younger, with a lower prevalence of serious health conditions, and their most frequent causes of death were accidental.
Our findings have implications for operationalizing Canada’s national palliative care framework, which has called for models of care led by primary care providers in a shared-care approach.51,52 The average number of outpatient specialties involved in care in the last year of life was nearly 4, with an average of 6 different physicians involved. With multiple physicians involved in care, it is possible that continuity of care, in the relational sense, could be disrupted. We did not examine the extent of shared care or communication among physicians, and the results do not suggest this is lacking. Our findings do suggest a need for understanding how best to organize care among multiple physicians to meet patients’ changing needs over the last year of life. Although home visits by physicians to patients who are at the end of life are associated with reduced likelihood of emergency department visits and hospital death,53 our results are consistent with other studies reporting that home visits are infrequent.6,53,54
Limitations
We did not include decedents who were living in a long-term care home in the last year of life, and our results may underestimate the amount of physician care provided to very frail people or those with severe dementia. Decedents who spent lengthy periods in hospital may have received fewer outpatient physician encounters, and we did not adjust for this factor. The health administrative data on physician encounters do not allow description of models of team care at the end of life that include key roles for other professionals, such as nurses. This study is based on 1 province of Canada (representing about 40% of the population), and health care systems are organized provincially; therefore, the results may not be generalizable to other jurisdictions. Owing to the timing of availability of cause-of-death data at ICES for creation of the trajectories, this study does not include recent years.
Conclusion
In the last year of life, patients have many encounters with various physicians in outpatient settings, and the volume and mix vary by end-of-life trajectory. Family physicians are the predominant specialty. Those who plan health care models of the end of life should consider support for family physicians to coordinate care and ways to optimize the complementary roles of different physicians while maintaining adequate continuity for patients.
Supplementary Material
Acknowledgements
The authors thank IQVIA Solutions Canada Inc. for the use of its Drug Information Database. Peter Tanuseputro is supported by a PSI Graham Farquharson Knowledge Translation Fellowship.
Footnotes
Competing interests: James Downar reports consulting fees from CMA Joule and honoraria from Boehringer Ingelheim (Canada), outside the submitted work. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Michelle Howard, Sarina Isenberg, Peter Tanuseputro and Abe Hafid conceived the study. All authors designed the study and interpreted the results. Michelle Howard wrote the manuscript. All authors revised the manuscript critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Funding: This study was funded by a grant from the Canadian Institutes of Health Research project #159771. This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care.
Data sharing: The data set from this study is held securely in coded form at ICES. While data sharing agreements prohibit ICES from making the data set publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at https://www.ices.on.ca/DAS. The full data set creation plan and underlying analytic code are available from the authors on request, understanding that the computer programs may rely on coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Disclaimer: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). Parts of this material are based on data and information compiled and provided by Canadian Institute for Health Information and the Ontario MOH. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. Parts of this material are based on the Ontario Office of the Registrar General information on deaths, the original source of which is Service Ontario. The views expressed therein are those of the authors and do not necessarily reflect those of the Ontario Office of the Registrar General or Ministry of Government and Consumer Services. Parts of this material are based on the Ontario Drug Benefit claims database.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/9/2/E613/suppl/DC1.
References
- 1.Lunney JR, Lynn J, Foley DJ, et al. Patterns of functional decline at the end of life. JAMA. 2003;289:2387–92. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 2.Fassbender K, Fainsinger RL, Carson M, et al. Cost trajectories at the end of life: the Canadian experience. J Pain Symptom Manage. 2009;38:75–80. doi: 10.1016/j.jpainsymman.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosella L, Kornas K, Huang A, et al. Accumulation of chronic conditions at the time of death increased in Ontario from 1994 To 2013. Health Aff (Millwood) 2018;37:464–72. doi: 10.1377/hlthaff.2017.1150. [DOI] [PubMed] [Google Scholar]
- 5.Rosella LC, Kornas K, Bornbaum C, et al. Population-based estimates of health care utilization and expenditures by adults during the last 2 years of life in Canada’s single-payer health system. JAMA Netw Open. 2020;3:e201917. doi: 10.1001/jamanetworkopen.2020.1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanuseputro P, Wodchis WP, Fowler R, et al. The health care cost of dying: a population-based retrospective cohort study of the last year of life in Ontario, Canada. PLoS One. 2015;10:e0121759. doi: 10.1371/journal.pone.0121759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown CR, Hsu AT, Kendall C, et al. How are physicians delivering palliative care? A population-based retrospective cohort study describing the mix of generalist and specialist palliative care models in the last year of life. Palliat Med. 2018;32:1334–43. doi: 10.1177/0269216318780223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tanuseputro P, Budhwani S, Bai YQ, et al. Palliative care delivery across health sectors: a population-level observational study. Palliat Med. 2017;31:247–57. doi: 10.1177/0269216316653524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seow H, O’Leary E, Perez R, et al. Access to palliative care by disease trajectory: a population-based cohort of Ontario decedents. BMJ Open. 2018;8:e021147. doi: 10.1136/bmjopen-2017-021147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Highet G, Crawford D, Murray SA, et al. Development and evaluation of the Supportive and Palliative Care Indicators Tool (SPICT): a mixed-methods study. BMJ Support Palliat Care. 2014;4:285–90. doi: 10.1136/bmjspcare-2013-000488. [DOI] [PubMed] [Google Scholar]
- 11.Murray SA, Kendall M, Mitchell G, et al. Palliative care from diagnosis to death. BMJ. 2017;356:j878. doi: 10.1136/bmj.j878. [DOI] [PubMed] [Google Scholar]
- 12.Quill TE, Abernethy AP. Generalist plus specialist palliative care — creating a more sustainable model. N Engl J Med. 2013;368:1173–5. doi: 10.1056/NEJMp1215620. [DOI] [PubMed] [Google Scholar]
- 13.Burge F, Lawson B, Johnston G, et al. Primary care continuity and location of death for those with cancer. J Palliat Med. 2003;6:911–8. doi: 10.1089/109662103322654794. [DOI] [PubMed] [Google Scholar]
- 14.Burge F, Lawson B, Johnston G. Family physician continuity of care and emergency department use in end-of-life cancer care. Med Care. 2003;41:992–1001. doi: 10.1097/00005650-200308000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Jones A, Bronskill SE, Seow H, et al. Associations between continuity of primary and specialty physician care and use of hospital-based care among community-dwelling older adults with complex care needs. PLoS One. 2020;15:e0234205. doi: 10.1371/journal.pone.0234205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almaawiy U, Pond GR, Sussman J, et al. Are family physician visits and continuity of care associated with acute care use at end-of-life? A population-based cohort study of homecare cancer patients. Palliat Med. 2014;28:176–83. doi: 10.1177/0269216313493125. [DOI] [PubMed] [Google Scholar]
- 17.Jones A, Bronskill SE, Seow H, et al. Physician home visit patterns and hospital use among older adults with functional impairments. J Am Geriatr Soc. 2020;68:2074–81. doi: 10.1111/jgs.16639. [DOI] [PubMed] [Google Scholar]
- 18.Beernaert K, Van den Block L, Van Thienen K, et al. Family physicians’ role in palliative care throughout the care continuum: stakeholder perspectives. Fam Pract. 2015;32:694–700. doi: 10.1093/fampra/cmv072. [DOI] [PubMed] [Google Scholar]
- 19.Murray SA, Kendall M, Boyd K, et al. Illness trajectories and palliative care. BMJ. 2005;330:1007–11. doi: 10.1136/bmj.330.7498.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gill TM, Gahbauer EA, Han L, et al. Trajectories of disability in the last year of life. N Engl J Med. 2010;362:1173–80. doi: 10.1056/NEJMoa0909087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fassbender K, Fainsinger RL, Carson M, et al. Cost trajectories at the end of life: the Canadian experience. J Pain Symptom Manage. 2009;38:75–80. doi: 10.1016/j.jpainsymman.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Health care use at the end of life in Atlantic Canada. Ottawa: Canadian Institute for Health Information; 2011. [Google Scholar]
- 23.Muggah E, Graves E, Bennett C, et al. The impact of multiple chronic diseases on ambulatory care use; a population-based study in Ontario, Canada. BMC Health Serv Res. 2012;12:452. doi: 10.1186/1472-6963-12-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lane NE, Maxwell CJ, Gruneir A, et al. Absence of a socioeconomic gradient in older adults’ survival with multiple chronic conditions. EBioMedicine. 2015;2:2094–100. doi: 10.1016/j.ebiom.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jaakkimainen RL, Bronskill SE, Tierney MC, et al. Identification of physician-diagnosed Alzheimer’s disease and related dementias in populationbased administrative data: a validation study using family physicians’ electronic medical records. J Alzheimers Dis. 2016;54:337–49. doi: 10.3233/JAD-160105. [DOI] [PubMed] [Google Scholar]
- 26.Mondor L, Cohen D, Khan AI, et al. Income inequalities in multimorbidity prevalence in Ontario, Canada: a decomposition analysis of linked survey and health administrative data. Int J Equity Health. 2018;17:90. doi: 10.1186/s12939-018-0800-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mondor L, Maxwell CJ, Bronskill SE, et al. The relative impact of chronic conditions and multimorbidity on health-related quality of life in Ontario long-stay home care clients. Qual Life Res. 2016;25:2619–32. doi: 10.1007/s11136-016-1281-y. [DOI] [PubMed] [Google Scholar]
- 28.Mondor L, Maxwell CJ, Hogan DB, et al. Multimorbidity and healthcare utilization among home care clients with dementia in Ontario, Canada: a retrospective analysis of a population-based cohort. PLoS Med. 2017;14:e1002249. doi: 10.1371/journal.pmed.1002249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gruneir A, Bronskill SE, Maxwell CJ, et al. The association between multi-morbidity and hospitalization is modified by individual demographics and physician continuity of care: a retrospective cohort study. BMC Health Serv Res. 2016;16:154. doi: 10.1186/s12913-016-1415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pefoyo AJ, Bronskill SE, Gruneir A, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015;15:415. doi: 10.1186/s12889-015-1733-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petrosyan Y, Bai YQ, Kone Pefoyo AJ, et al. The relationship between diabetes care quality and diabetes-related hospitalizations and the modifying role of comorbidity. Can J Diabetes. 2017;41:17–25. doi: 10.1016/j.jcjd.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 32.Thavorn K, Maxwell CJ, Gruneir A, et al. Effect of socio-demographic factors on the association between multimorbidity and healthcare costs: a population-based, retrospective cohort study. BMJ Open. 2017;7:e017264. doi: 10.1136/bmjopen-2017-017264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barbera L, Hwee J, Klinger C, et al. Development and validation of an algorithm to identify palliative care physicians among primary care physicians. CMAJ Open. 2015;3:E292–8. doi: 10.9778/cmajo.20150005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chaudhuri D, Tanuseputro P, Herritt B, et al. Critical care at the end of life: a population-level cohort study of cost and outcomes. Crit Care. 2017;21:124. doi: 10.1186/s13054-017-1711-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bekelman JE, Halpern SD, Blankart CR, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315:272–83. doi: 10.1001/jama.2015.18603. [DOI] [PubMed] [Google Scholar]
- 36.Hsu AT, Tanuseputro P. The delivery of palliative and end-of-life care in Ontario. Healthc Q. 2017;20:6–9. doi: 10.12927/hcq.2017.25232. [DOI] [PubMed] [Google Scholar]
- 37.Qureshi D, Tanuseputro P, Perez R, et al. Place of care trajectories in the last two weeks of life: a population-based cohort study of Ontario decedents. J Palliat Med. 2018;21:1588–95. doi: 10.1089/jpm.2018.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seow H, O’Leary E, Perez R, et al. Access to palliative care at the end-of-life by disease trajectory: a population-based cohort study of Ontario decedents. BMJ Open. 2018;8:e021147. doi: 10.1136/bmjopen-2017-021147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palliative care Fact sheet. Geneva: World Health Organization; 2017. [Google Scholar]
- 40.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Connecting the dots for patients: family doctors’ views on coordinating patient care in Ontario’s healthcare system. Toronto: Health Quality Ontario; 2016. [accessed 2021 May 21]. Available: https://www.hqontario.ca/Portals/0/documents/system-performance/connecting-the-dots-report-en.pdf. [Google Scholar]
- 42.Bodenheimer T, Ghorob A, Willard-Grace R, et al. The 10 building blocks of high-performing primary care. Ann Fam Med. 2014;12:166–71. doi: 10.1370/afm.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aubin M, Vezina L, Verreault R, et al. Family physician involvement in cancer care follow-up: the experience of a cohort of patients with lung cancer. Ann Fam Med. 2010;8:526–32. doi: 10.1370/afm.1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lawrence RA, McLoone JK, Wakefield CE, et al. Primary care physicians’ perspectives of their role in cancer care: a systematic review. J Gen Intern Med. 2016;31:1222–36. doi: 10.1007/s11606-016-3746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moens K, Higginson IJ, Harding R, et al. Are there differences in the prevalence of palliative care-related problems in people living with advanced cancer and eight non-cancer conditions? A systematic review. J Pain Symptom Manage. 2014;48:660–77. doi: 10.1016/j.jpainsymman.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 46.Claessens MT, Lynn J, Zhong Z, et al. Dying with lung cancer or chronic obstructive pulmonary disease: insights from SUPPORT. Study to understand prognoses and preferences for outcomes and risks of treatments. J Am Geriatr Soc. 2000;48:S146–53. doi: 10.1111/j.1532-5415.2000.tb03124.x. [DOI] [PubMed] [Google Scholar]
- 47.Aldridge MD, Bradley EH. Epidemiology and patterns of care at the end of life: rising complexity, shifts in care patterns and sites of death. Health Aff (Millwood) 2017;36:1175–83. doi: 10.1377/hlthaff.2017.0182. [DOI] [PubMed] [Google Scholar]
- 48.Amblas-Novellas J, Murray SA, Espaulella J, et al. Identifying patients with advanced chronic conditions for a progressive palliative care approach: a cross-sectional study of prognostic indicators related to end-of-life trajectories. BMJ Open. 2016;6:e012340. doi: 10.1136/bmjopen-2016-012340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stow D, Matthews FE, Hanratty B. Frailty trajectories to identify end of life: a longitudinal population-based study. BMC Med. 2018;16:171. doi: 10.1186/s12916-018-1148-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morin L, Aubry R, Frova L, et al. Estimating the need for palliative care at the population level: a cross-national study in 12 countries. Palliat Med. 2017;31:526–36. doi: 10.1177/0269216316671280. [DOI] [PubMed] [Google Scholar]
- 51.Morrison RS. A national palliative care strategy for Canada. J Palliat Med. 2018;21:S63–75. doi: 10.1089/jpm.2017.0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pereira J, Chary S, Moat JB, et al. Pallium Canada’s Curriculum Development Model: a framework to support large-scale courseware development and deployment. J Palliat Med. 2020;23:759–66. doi: 10.1089/jpm.2019.0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tanuseputro P, Beach S, Chalifoux M, et al. Associations between physician home visits for the dying and place of death: a population-based retrospective cohort study. PLoS One. 2018;13:e0191322. doi: 10.1371/journal.pone.0191322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Howard M, Chalifoux M, Tanuseputro P. Does primary care model effect healthcare at the end of life? A population-based retrospective cohort study. J Palliat Med. 2017;20:344–51. doi: 10.1089/jpm.2016.0283. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.