Abstract
Objectives
We aimed to develop a systematic synthesis of systematic reviews of health impacts of climate change, by synthesising studies’ characteristics, climate impacts, health outcomes and key findings.
Design
We conducted an overview of systematic reviews of health impacts of climate change. We registered our review in PROSPERO (CRD42019145972). No ethical approval was required since we used secondary data. Additional data are not available.
Data sources
On 22 June 2019, we searched Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, Cochrane and Web of Science.
Eligibility criteria
We included systematic reviews that explored at least one health impact of climate change.
Data extraction and synthesis
We organised systematic reviews according to their key characteristics, including geographical regions, year of publication and authors’ affiliations. We mapped the climate effects and health outcomes being studied and synthesised major findings. We used a modified version of A MeaSurement Tool to Assess systematic Reviews-2 (AMSTAR-2) to assess the quality of studies.
Results
We included 94 systematic reviews. Most were published after 2015 and approximately one-fifth contained meta-analyses. Reviews synthesised evidence about five categories of climate impacts; the two most common were meteorological and extreme weather events. Reviews covered 10 health outcome categories; the 3 most common were (1) infectious diseases, (2) mortality and (3) respiratory, cardiovascular or neurological outcomes. Most reviews suggested a deleterious impact of climate change on multiple adverse health outcomes, although the majority also called for more research.
Conclusions
Most systematic reviews suggest that climate change is associated with worse human health. This study provides a comprehensive higher order summary of research on health impacts of climate change. Study limitations include possible missed relevant reviews, no meta-meta-analyses, and no assessment of overlap. Future research could explore the potential explanations between these associations to propose adaptation and mitigation strategies and could include broader sociopsychological health impacts of climate change.
Keywords: public health, social medicine, public health
Strengths and limitations of this study.
A strength of this study is that it provides the first broad overview of previous systematic reviews exploring the health impacts of climate change. By targeting systematic reviews, we achieve a higher order summary of findings than what would have been possible by consulting individual original studies.
By synthesising findings across all included studies and according to the combination of climate impact and health outcome, we offer a clear, detailed and unique summary of the current state of evidence and knowledge gaps about how climate change may influence human health.
A limitation of this study is that we were unable to access some full texts and therefore some studies were excluded, even though we deemed them potentially relevant after title and abstract inspection.
Another limitation is that we could not conduct meta-meta-analyses of findings across reviews, due to the heterogeneity of the included systematic reviews and the relatively small proportion of studies reporting meta-analytic findings.
Finally, the date of the systematic search is a limitation, as we conducted the search in June 2019.
Introduction
The environmental consequences of climate change such as sea-level rise, increasing temperatures, more extreme weather events, increased droughts, flooding and wildfires are impacting human health and lives.1 2 Previous studies and reviews have documented the multiple health impacts of climate change, including an increase in infectious diseases, respiratory disorders, heat-related morbidity and mortality, undernutrition due to food insecurity, and adverse health outcomes ensuing from increased sociopolitical tension and conflicts.2–5 Indeed, the most recent Lancet Countdown report,2 which investigates 43 indicators of the relationship between climate change and human health, arrived at their most worrisome findings since the beginning of their on-going annual work. This report underlines that the health impacts of climate change continue to worsen and are being felt on every continent, although they are having a disproportionate and unequal impact on populations.2 Authors caution that these health impacts will continue to worsen unless we see an immediate international response to limiting climate change.
To guide future research and action to mitigate and adapt to the health impacts of climate change and its environmental consequences, we need a complete and thorough overview of the research already conducted regarding the health impacts of climate change. Although the number of original studies researching the health impacts of climate change has greatly increased in the recent decade,2 these do not allow for an in-depth overview of the current literature on the topic. Systematic reviews, on the other hand, allow a higher order overview of the literature. Although previous systematic reviews have been conducted on the health impacts of climate change, these tend to focus on specific climate effects (eg, impact of wildfires on health),6 7 health impacts (eg, occupational health outcomes),8 9 countries,10–12 or are no longer up to date,13 14 thus limiting our global understanding of what is currently known about the multiple health impacts of climate change across the world.
In this study, we aimed to develop such a complete overview by synthesising systematic reviews of health impacts of climate change. This higher order overview of the literature will allow us to better prepare for the worsening health impacts of climate change, by identifying and describing the diversity and range of health impacts studied, as well as by identifying gaps in previous research. Our research objectives were to synthesise studies’ characteristics such as geographical regions, years of publication, and authors’ affiliations, to map the climate impacts, health outcomes, and combinations of these that have been studied, and to synthesise key findings.
Methods
We applied the Cochrane method for overviews of reviews.15 This method is designed to systematically map the themes of studies on a topic and synthesise findings to achieve a broader overview of the available literature on the topic.
Research questions
Our research questions were the following: (1) What is known about the relationship between climate change and health, as shown in previous systematic reviews? (2) What are the characteristics of these studies? We registered our plan (CRD4201914597216) in PROSPERO, an international prospective register of systematic reviews and followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 202017 to report our findings, as a reporting guideline for overviews is still in development.18
Search strategy and selection criteria
To identify relevant studies, we used a systematic search strategy. There were two inclusion criteria. We included studies in this review if they (1) were systematic reviews of original research and (2) reported at least one health impact as it related (directly or indirectly) to climate change.
We defined a systematic review, based on Cochrane’s definition, as a review of the literature in which one ‘attempts to identify, appraise and synthesize all the empirical evidence that meets pre-specified eligibility criteria to answer a specific research question [by] us[ing] explicit, systematic methods that are selected with a view aimed at minimizing bias, to produce more reliable findings to inform decision making’.19 We included systematic reviews of original research, with or without meta-analyses. We excluded narrative reviews, non-systematic literature reviews and systematic reviews of materials that were not original research (eg, systematic reviews of guidelines.)
We based our definition of health impacts on the WHO’s definition of health as, ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’.20 Therefore, health impacts included, among others, morbidity, mortality, new conditions, worsening/improving conditions, injuries and psychological well-being. Included studies could refer to climate change or global warming directly or indirectly, for instance, by synthesising the direct or indirect health effects of temperature rises or of natural conditions/disasters made more likely by climate change (eg, floods, wildfires, temperature variability, droughts.) Although climate change and global warming are not equivalent terms, in an effort to avoid missing relevant literature, we included studies using either term. We included systematic reviews whose main focus was not the health impacts of climate change, providing they reported at least one result regarding health effects related to climate change (or consequences of climate change.) We excluded studies if they did not report at least one health effect of climate change. For instance, we excluded studies which reported on existing measures of health impacts of climate change (and not the health impact itself) and studies which reported on certain health impacts without a mention of climate change, global warming or environmental consequences made more likely by climate change.
On 22 June 2019, we retrieved systematic reviews regarding the health effects of climate change by searching from inception the electronic databases Medline, CINAHL, Embase, Cochrane, Web of Science using a structured search (see online supplemental appendix 1 for final search strategy developed by a librarian.) We did not apply language restrictions. After removing duplicates, we imported references into Covidence.21
bmjopen-2020-046333supp001.pdf (42.4KB, pdf)
Screening process and data extraction
To select studies, two trained analysts first screened independently titles and abstracts to eliminate articles that did not meet our inclusion criteria. Next, the two analysts independently screened the full text of each article. A senior analyst resolved any conflict or disagreement.
Next, we decided on key information that needed to be extracted from studies. We extracted the first author’s name, year of publication, number of studies included, time frame (in years) of the studies included in the article, first author’s institution’s country affiliation, whether the systematic review included a meta-analysis, geographical focus, population focus, the climate impact(s) and the health outcome(s) as well as the main findings and limitations of each systematic review.
Two or more trained analysts (RR, CB, RN, LC, LPB, RAPR) independently extracted data, using Covidence and spreadsheet software (Google Sheets). An additional trained analyst from the group or senior research team member resolved disagreements between individual judgments.
Coding and data mapping
To summarise findings from previous reviews, we first mapped articles according to climate impacts and health outcomes. To develop the categories of climate impacts and health outcomes, two researchers (RR and LC) consulted the titles and abstracts of each article. We started by identifying categories directly based on our data and finalised our categories by consulting previous conceptual frameworks of climate impacts and health outcomes.1 22 23 The same two researchers independently coded each article according to their climate impact and health outcome. We then compared coding and resolved disagreements through discussion.
Next, using spreadsheet software, we created a matrix to map articles according to their combination of climate impacts and health outcomes. Each health outcome occupied one row, whereas climate impacts each occupied one column. We placed each article in the matrix according to the combination(s) of their climate impact(s) and health outcome(s). For instance, if we coded an article as ‘extreme weather’ for climate and ‘mental health’ for health impact, we noted the reference of this article in the cell at the intersection of these two codes. We calculated frequencies for each cell to identify frequent combinations and gaps in literature. Because one study could investigate more than one climate impact and health outcome, the frequency counts for each category could exceed the number of studies included in this review.
Finally, we re-read the Results and Discussion sections of each article to summarise findings of the studies. We first wrote an individual summary for each study, then we collated the summaries of all studies exploring the same combination of categories to develop an overall summary of findings for each combination of categories.
Quality assessment
We used a modified version of AMSTAR-2 to assess the quality of the included systematic reviews (online supplemental appendix 2). The purpose of this assessment was to evaluate the quality of the included studies as a whole to get a sense of the overall quality of evidence in this field. Therefore, individual quality scores were not compiled for each article, but scores were aggregated according to items. Since AMSTAR-2 was developed for syntheses of systematic reviews of randomised controlled trials, working with a team member with expertise in knowledge synthesis (AT), we adapted it to suit a research context that is not amenable to randomised controlled trials. For instance, we changed assessing and accounting for risk of bias in studies’ included randomised controlled trials to assessing and accounting for limitations in studies’ included articles. Complete modifications are presented in online supplemental appendix 2.
bmjopen-2020-046333supp002.pdf (22.3KB, pdf)
Patient and public involvement
Patients and members of the public were not involved in this study.
Results
Articles identified
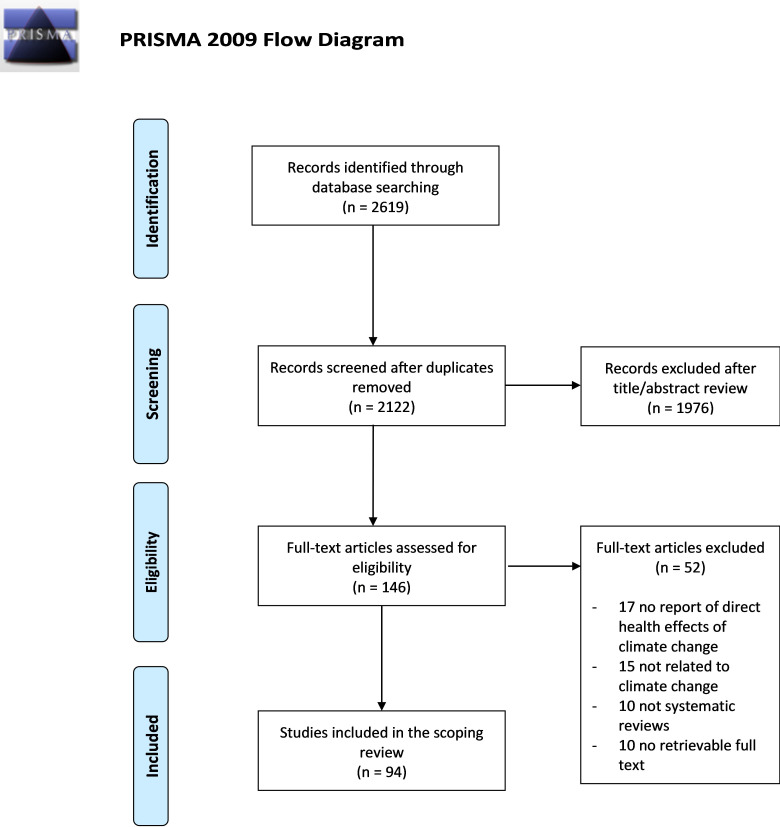
As shown in the PRISMA diagram in figure 1, from an initial set of 2619 references, we retained 94 for inclusion. More precisely, following screening of titles and abstracts, 146 studies remained for full-text inspection. During full-text inspection, we excluded 52 studies, as they did not report a direct health effect of climate change (n=17), did not relate to climate change (n=15), were not systematic reviews (n=10), or we could not retrieve the full text (n=10).
Figure 1.
The flow chart for included articles in this review.
Study descriptions
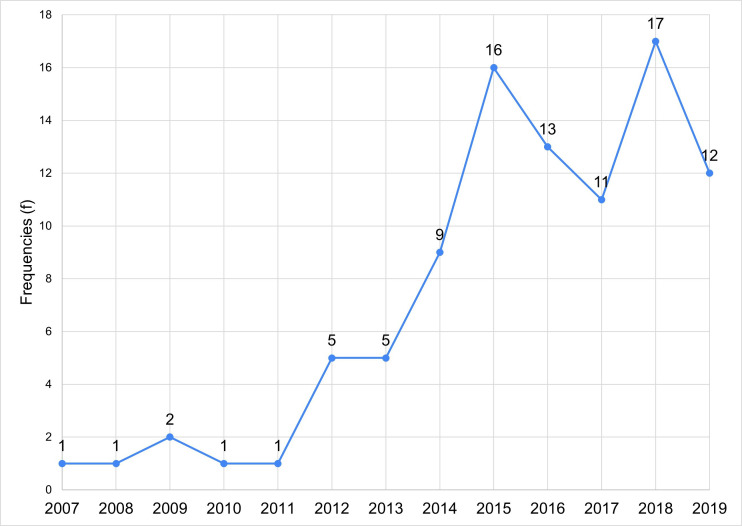
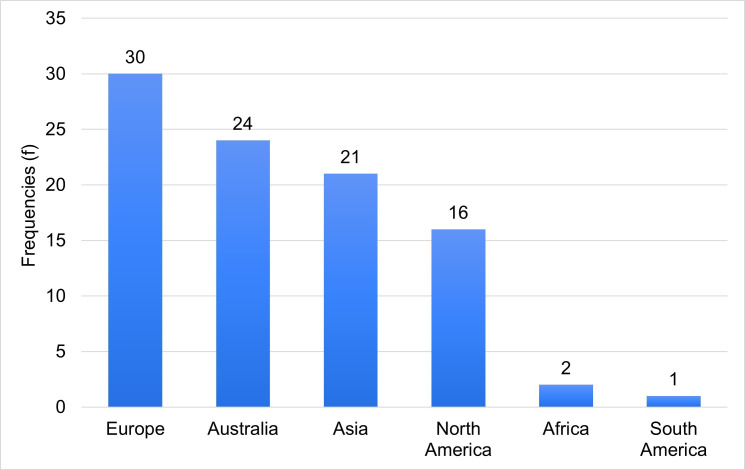
A detailed table of all articles and their characteristics can be found in online supplemental appendix 3. Publication years ranged from 2007 to 2019 (year of data extraction), with the great majority of included articles (n=69; 73%) published since 2015 (figure 2). A median of 30 studies had been included in the systematic reviews (mean=60; SD=49; range 7–722). Approximately one-fifth of the systematic reviews included meta-analyses of their included studies (n=18; 19%). The majority of included systematic reviews’ first authors had affiliations in high-income countries, with the largest representations by continent in Europe (n=30) and Australia (n=24) (figure 3). Countries of origin by continents include (from highest to lowest frequency, then by alphabetical order): Europe (30); UK (9), Germany (6), Italy (4), Sweden (4), Denmark (2), France (2), Georgia (1), Greece (1) and Finland (1); Australia (24); Asia (21); China (11), Iran (4), India (1), Jordan (1), Korea (1), Nepal (1), Philippines (1), Taiwan (1); North America (16); USA (15), Canada (1); Africa (2); Ethiopia (1), Ghana (1), and South America (1); Brazil (1).
Figure 2.
Number of included systematic reviews by year of publication.
Figure 3.
Number of publications according to geographical affiliation of the first author.
bmjopen-2020-046333supp003.pdf (185.2KB, pdf)
Regarding the geographical focus of systematic reviews, most of the included studies (n=68; 72%) had a global focus or no specified geographical limitations and therefore included studies published anywhere in the world. The remaining systematic reviews either targeted certain countries (n=12) (1 for each Australia, Germany, Iran, India, Ethiopia, Malaysia, Nepal, New Zealand and 2 reviews focused on China and the USA), continents (n=5) (3 focused on Europe and 2 on Asia), or regions according to geographical location (n=6) (1 focused on Sub-Saharan Africa, 1 on Eastern Mediterranean countries, 1 on Tropical countries, and 3 focused on the Arctic), or according to the country’s level of income (n=3) (2 on low to middle income countries, 1 on high income countries).
Regarding specific populations of interest, most of the systematic reviews did not define a specific population of interest (n=69; 73%). For the studies that specified a population of interest (n=25; 26.6%), the most frequent populations were children (n=7) and workers (n=6), followed by vulnerable or susceptible populations more generally (n=4), the elderly (n=3), pregnant people (n=2), people with disabilities or chronic illnesses (n=2) and rural populations (n=1).
Quality assessment
We assessed studies for quality according to our revised AMSTAR-2. Complete scores for each article and each item are available in online supplemental appendix 4. Out of 94 systematic reviews, the most commonly fully satisfied criterion was #1 (Population, Intervention, Comparator, Outcome (PICO) components) with 81/94 (86%) of included systematic reviews fully satisfying this criterion. The next most commonly satisfied criteria were #16 (potential sources of conflict of interest reported) (78/94=83% fully), #13 (account for limitations in individual studies) (70/94=75% fully and 2/94=2% partially), #7 (explain both inclusion and exclusion criteria) (64/94=68% fully and 19/94=20% partially), #8 (description of included studies in adequate detail) (36/94=38% fully and 41/94=44% partially), and #4 (use of a comprehensive literature search strategy) (0/94=0% fully and 80/94=85% partially). For criteria #11, #12, and #15, which only applied to reviews including meta-analyses, 17/18 (94%) fully satisfied criterion #11 (use of an appropriate methods for statistical combination of results), 12/18 (67%) fully satisfied criterion #12 (assessment of the potential impact of Risk of Bias (RoB) in individual studies) (1/18=6% partially), and 11/18 (61%) fully satisfied criterion #15 (an adequate investigation of publication bias, small study bias).
bmjopen-2020-046333supp004.pdf (75KB, pdf)
Climate impacts and health outcomes
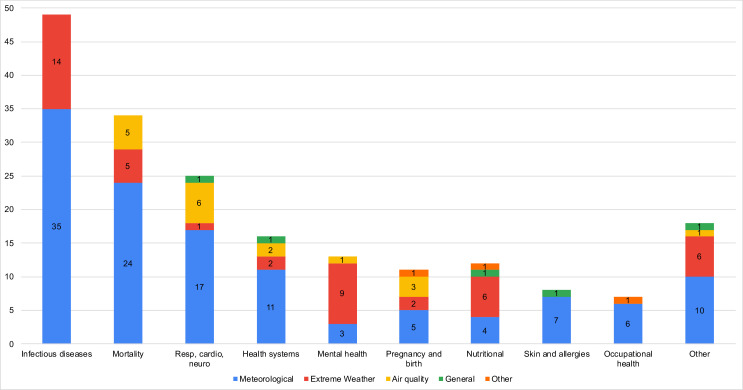
Regarding climate impacts, we identified 5 mutually exclusive categories, with 13 publications targeting more than one category of climate impacts: (1) meteorological (n=71 papers) (eg, temperature, heat waves, humidity, precipitation, sunlight, wind, air pressure), (2) extreme weather (n=24) (eg, water-related, floods, cyclones, hurricanes, drought), (3) air quality (n=7) (eg, air pollution and wildfire smoke exposure), (4) general (n=5), and (5) other (n=3). Although heat waves could be considered an extreme weather event, papers investigating heat waves’ impact on health were classified in the meteorological impact category, since some of these studies treated them with high temperature. ‘General’ climate impacts included articles that did not specify climate change impacts but stated general climate change as their focus. ‘Other’ climate impacts included studies investigating other effects indirectly related to climate change (eg, impact of environmental contaminants) or general environmental risk factors (eg, environmental hazards, sanitation and access to clean water.)
We identified 10 categories to describe the health outcomes studied by the systematic reviews, and 29 publications targeted more than one category of health outcomes: (1) infectious diseases (n=41 papers) (vector borne, food borne and water borne), (2) mortality (n=32), (3) respiratory, cardiovascular and neurological (n=23), (4) healthcare systems (n=16), 5) mental health (n=13), (6) pregnancy and birth (n=11), 7) nutritional (n=9), (8) skin diseases and allergies (n=8), (9) occupational health and injuries (n=6) and (10) other health outcomes (n=17) (eg, sleep, arthritis, disability-adjusted life years, non-occupational injuries, etc)
Figure 4 depicts the combinations of climate impact and health outcome for each study, with online supplemental appendix 5 offering further details. The five most common combinations are studies investigating the (1) meteorological impacts on infectious diseases (n=35), (2) mortality (n=24) and (3) respiratory, cardiovascular and neurological outcomes (n=17), (4) extreme weather events’ impacts on infectious diseases (n=14), and (5) meteorological impacts on health systems (n=11).
Figure 4.
Summary of the combination of climate impact and health outcome (frequencies). The total frequency for one category of health outcome could exceed the number of publications included in this health outcome, since one publication could explore the health impact according to more than one climate factor (eg, one publication could explore both the impact of extreme weather events and temperature on mental health).
bmjopen-2020-046333supp005.pdf (32.8KB, pdf)
For studies investigating meteorological impacts on health, the three most common health outcomes studied were impacts on (1) infectious diseases (n=35), (2) mortality (n=24) and (3) respiratory, cardiovascular and neurological outcomes (n=17). Extreme weather event studies most commonly reported health outcomes related to (1) infectious diseases (n=14), (2) mental health outcomes (n=9) and (3) nutritional outcomes (n=6) and other health outcomes (eg, injuries, sleep) (n=6). Studies focused on the impact of air quality were less frequent and explored mostly health outcomes linked to (1) respiratory, cardiovascular and neurological outcomes (n=6), (2) mortality (n=5) and (3) pregnancy and birth outcomes (n=3).
Summary of findings
Most reviews suggest a deleterious impact of climate change on multiple adverse health outcomes, with some associations being explored and/or supported with consistent findings more often than others. Some reviews also report conflicting findings or an absence of association between the climate impact and health outcome studied (see table 1 for a detailed summary of findings according to health outcomes).
Table 1.
Summary of findings from systematic reviews according to health outcome and climate impact
| Climate impact | n | Summary of findings |
| Infectious diseases (n=41) | ||
| Vector-borne infectious diseases (n=25) | ||
| Meteorological | 22 | Systematic reviews suggest that meteorological factors, such as temperature, precipitation, humidity, and wind, are associated with diverse vector-borne infectious diseases, including malaria and dengue.9 12 26 29 31 47–63 This association was mostly proportional (eg, higher temperature and increased rainfall associated with vector-borne diseases), although findings were at times conflicting, with some suggesting an inversely proportional association12 (eg, decreased rainfall) or no association at all52 (eg, with the human puumala hantavirus Infection.) Geographical location, seasonality and potential interaction with other climate-related factors may partly explain these inconsistencies.12 29 Temperature, humidity and rainfall were the most common and important meteorological factors reported by reviews and factors such as wind, air pressure and sunshine were reported less often. |
| Extreme weather | 7 | There are limited and conflicting findings concerning the association of extreme weather events with vector-borne diseases. Some reviews suggest water-related extreme events64 and flooding6 31 65 are associated with an increased risk of vector-borne diseases, while drought is associated with a reduction of dengue incidence.12 Other reviews focused specifically on Puerto Rico56 and Australia66 did not find an association between hurricanes and/or floods and mosquito-borne disease transmission. |
| Food and water borne infectious diseases (n=19) | ||
| Meteorological | 14 | Reviews suggest that meteorological factors, such as temperature, precipitation and humidity, are associated with diverse food-borne and water-borne infectious diseases, in particular, cholera, schistosomiasis, salmonella and E. coli gastroenteritis.11 31 53 55 58 61 67–74 Overall, higher temperatures and humidity,11 53 67 71 along with lower precipitation55 74 was associated with these infectious diseases. Directionality and strength of the association seemed to vary according to disease and pathogens,72 seasons and geographical region.69 |
| Extreme weather | 10 | Reviews suggest a proportional association between extreme water-related events,60 64 75 such as flooding6 53 65 and heavy rainfall,47 and food-borne and water-borne diseases, including diarrhoea, food contamination, cholera.6 31 47 53 58 60 64 65 70 75 Drought may also be proportionally associated with food-borne and water-borne disease,47 76 but these associations are less consistent than those with water-related extreme events.70 |
| Other infectious diseases (n=8) | ||
| Meteorological | 8 | Reviews suggest an association of most meteorological factors, such as temperature and humidity, with various other infectious diseases, including meningitis,24 47 Ebola,24 influenza,31 and paediatric infectious diseases such as hand-foot-and-mouth disease.7 8 30 62 68 This association was mostly proportional for meteorological factors such as temperature,7 8 62 diurnal temperature range30 and humidity,7 8 31 although some meteorological factors, such as air pressure8 and lower temperatures31 62 were inversely proportional to these diseases. Some conflicting evidence is reported concerning the association with some meteorological factors, such as sunshine with hand-foot-and-mouth disease,7 8 and humidity and paediatric infectious diseases.68 No association was found between some meteorological factors, such as precipitation, wind speed and sunshine with hand-foot-and-mouth disease.7 8 |
| Mortality (n=32) | ||
| Meteorological | 24 | Reviews suggest that temperature (high, low, or diurnal range) was consistently associated with all-cause and cause-specific mortality.24–26 30 33 34 55 58 60 62 77–89 A strong association was reported between heat (including heat waves) and mortality (all-cause),77 heat related,55 81 stroke related,24 82 cardiovascular related,33 60 and respiratory related,26 33 83 especially in rural,80 very young children62 and ageing populations.25 Mortality seems to be the most frequent health outcome studied in association with heatwaves.34 Inconsistent results are found concerning the association between heat and childhood mortality.87 Due to limited evidence, this association was weaker in some geographical regions.24 84 Also, heat wave intensity (compared with duration) was more strongly associated with heat-related mortality.88 Finally, although less studied, low temperature was also associated with mortality,62 89 specifically respiratory,77 stroke82 and cardiovascular mortality.60 79 83 |
| Extreme weather | 5 | Reviews suggest an association between extreme weather events such as floods,6 droughts,76 cyclones90 and other water-related events,26 64 with direct (eg, drowning) and indirect long-term mortality (eg, due to malnutrition, environmental toxin exposure, armed conflict, etc).6 64 76 90 |
| Air quality | 5 | Reviews suggest an association between exposure to air pollution26 91 or wildfire smoke92–94 and air pollution related-mortality, such as respiratory-specific mortality. There is currently limited evidence, but reviews suggest a potential association between wildfire smoke exposure and cardiovascular-specific mortality.92–94 |
| Respiratory, neurological and cardiovascular (n=23) | ||
| General | 1 | A review suggests a proportional association between climate change, in general, and ragweed pollen allergies in Europe.95 |
| Meteorological | 17 | Reviews suggest an association between meteorological factors, such as temperature and humidity, and cardiovascular, respiratory and neurological outcomes.24 26 30 33 35 49 58 62 68 77 79 81 82 86 87 96 97 Exposure to high temperatures and extreme heat are associated to cardiovascular and respiratory diseases,24 26 49 62 79 stroke,82 long-term neurological outcomes (due to heat strokes),81 myocardial infarction,33 35 and childhood asthma and paediatric respiratory diseases.87 97 A review also suggests a beneficial association between heat and the shortening of a respiratory virus season.58 Exposure to low temperature (cold), temperature drop, or diurnal temperature range was associated with cardiovascular and respiratory diseases,30 77 79 stroke,82 and myocardial infarctions.33 Humidity (most often high humidity, but also lower humidity) and low temperatures were also associated with respiratory diseases in children, including childhood asthma.68 96 97 |
| Extreme weather | 1 | A previous review suggests an association between drought and respiratory and cardiovascular outcomes, most likely due to droughts leading to increased dust in the air.76 |
| Air quality | 6 | Reviews suggest a proportional association between exposure to air pollution26 55 58 or wildfire smoke exposure92–94 and respiratory outcomes, including asthma, chronic obstructive pulmonary disease, coughing, wheezing and overall lung function. Although there is currently limited evidence,92 reviews also suggest a potential association between air pollution or wildfire smoke exposure and cardiovascular outcomes.58 93 94 |
| Health systems (n=16) | ||
| General | 1 | A previous review suggests that climate change in general puts a strain on public health resources, via population health issues and shows that using an integrated surveillance system may guide future adaptation to climate change.98 |
| Meteorological | 11 | Previous reviews suggest an association between temperature change30 extreme heat, aridity and cold temperatures and an increase in use of healthcare services (mostly linked to heat-related health impacts), such as an increase in emergency department visits, hospital admissions and use of ambulances.24 26 30 33–35 55 62 84 87 99 |
| Extreme weather | 2 | Reviews suggest that extreme weather events32 and flooding6 may be associated with an increase in use of healthcare services (eg, increased hospitalisations) and a compromised quality of care as extreme weather events may lead to power outages.32 |
| Air quality | 2 | Reviews suggest an association between wildfire smoke exposure and an increase in use of healthcare services, such as an increase in emergency department visits.92 94 |
| Mental health (n=13) | ||
| Meteorological | 3 | Reviews suggest an association of most meteorological factors such as temperature increase, aridity, heat and heat waves with mental health outcomes, including hospital admissions for mental health reasons,55 suicide,100 and exacerbation of pre-existing mental health conditions, difficulty sleeping and fatigue.35 No association was found between sunlight duration and suicide incidence.100 |
| Extreme weather | 9 | Most reviews reported a proportional association of extreme weather events,36 58 64 101 flooding6 26 102 and drought76 103 with diverse mental health issues, including, psychological distress, post-traumatic stress disorder, anxiety, depression, psychotropic medication use, alcohol consumption. There was conflicting evidence regarding the association of floods with suicide, tobacco, alcohol and substance abuse.102 No association was found between drought and suicide.76 |
| Air quality | 1 | A previous review suggests no association between wildfire smoke exposure and mental health, as measured by physician visits and hospitalizations for mental health reasons during wildfires.93 |
| Pregnancy and birth outcomes (n=11) | ||
| Meteorological | 5 | Reviews suggest that adverse birth outcomes may be higher among people exposed to meteorological factors such as high temperature, heat, sunlight intensity, cold and humidity.55 104–107 These outcomes include low birth weight, preterm birth, eclampsia and preeclampsia, hypertension and length of pregnancy.55 104–107 The association between heat and adverse birth outcomes seems to have stronger support than the association with cold temperatures.107 |
| Extreme Weather | 2 | Reviews suggest a potential association of extreme weather events36 and flooding6 with adverse birth outcomes, such as low birth weight, preterm birth and preeclampsia. It is suggested that extreme weather events may indirectly affect birth outcomes via the pregnant person’s well-being (eg, stress and worry during pregnancy.)6 36 |
| Air quality | 3 | There is limited and inconsistent evidence concerning the association between wildfire smoke exposure and adverse birth outcomes, but reviews suggest a potential proportional association between wildfire smoke exposure and lower birth weight.92–94 |
| Other | 1 | The association between environmental pollutants and adverse birth outcomes (ie, preterm birth) remains unclear due to conflicting evidence.28 |
| Nutritional (n=9) | ||
| General | 1 | A review suggests an association between climate change and obesity.108 |
| Meteorological | 4 | Reviews suggest an association between meteorological factors, such as changes in temperature, heat and precipitation, with diverse nutritional outcomes, including undernutrition, malnutrition and child stunting.24 27 55 84 This association may be explained by the impact of meteorological factors, such as temperature increase and precipitation decrease, on crop production and food insecurity.55 84 |
| Extreme Weather | 6 | Reviews suggest an association between extreme weather events, such as flooding and droughts,76 and diverse nutritional outcomes, including malnutrition and undernutrition in children and adults27 47 55 58 60 via, among others, crops production and food insecurity (eg, low food aid following flooding.55 |
| Other | 1 | A review suggests a potential association between certain environmental risk factors (eg, sanitation, cooking fuels and food-borne mycotoxins), and childhood stunting, which could be aggravated by climate change.109 |
| Skin diseases and allergies (n=8) | ||
| General | 1 | A review suggests a potential proportional association between climate change, in general, and skin and soft-tissue infections (eg, fatal vibrio vulnificus necrotising).110 |
| Meteorological | 7 | Reviews suggest an association of meteorological factors, such as ultraviolet light exposure, temperature and humidity, with diverse skin diseases and allergies, including skin cancer, sunburn, acute urticaria, eczema and paediatric skin irritabilities.24 35 58 60 62 68 111 Higher temperature and ultraviolet light exposure is proportionally associated with sunburn35 and skin cancer,58 111 while low humidity and low temperatures were associated with eczema and skin irritabilities in children.62 68 |
| Occupational health and injuries (n=6) | ||
| Meteorological | 6 | Reviews suggest that heat is associated with adverse occupational health outcomes, including injuries (eg, slips, trips, falls, wounds, lacerations and amputations), heat strain, dehydration and kidney diseases.103 112–117 This association was found in many occupational settings, including agriculture, construction, transport and fishing, and seems to affect both outdoor and indoor workers.112 This association may be explained by a combination of direct (eg, dehydration) and indirect factors (eg, impaired cognitive and physical performance.)116 |
| Other | 1 | A review suggests a potential association between environmental pollution (eg, heavy metals, fertilisers, etc) and occupational diseases, such as chronic kidney disease.117 This association is suggested to be affected by increasing temperatures. |
| Other (n=17) | ||
| General | 1 | A review suggests a potential association between climate change in general and disability-adjusted life years, which is an indicator that quantifies ‘the burden of disease attributable to climate change’.118 Authors suggest that the cost of disability-adjusted life years could be high, especially in low-income to middle-income countries. |
| Meteorological | 10 | Reviews suggests an association between increasing temperatures and temperature changes,30 and other various health outcomes, including acute gouty arthritis,119 unintentional injuries,120 diabetes,77 genitourinary diseases,30 77 impaired sleep time and quality,121 cataracts (indirectly associated via people spending more time outside and therefore increased exposure to ultraviolet light),58 60 heat stress, heat exhaustion and kidney failure,35 and renal diseases, fever and electrolyte imbalance in children.62 87 |
| Extreme weather | 6 | Reviews suggests an association between extreme weather events,101 such as flooding,6 cyclones,90 hurricanes121 and drought,76 and other various health outcomes including injuries (eg, debris, diving in water that is shallower than expected),6 76 90 101 impaired sleep,121 oesophageal cancer (likely linked to high salinity of water due to droughts),76 and exacerbation of chronic illnesses.6 36 |
| Air quality | 1 | There is limited evidence, but a systematic review suggests a potential association between wildfire smoke exposure and ophthalmic outcomes, such as eye irritation and cataracts.92 |
Reviews that covered multiple climate impacts are listed in each relevant category.
Notable findings of health outcomes according to climate impact include the following. For meteorological factors (n=71), temperature and humidity are the variables most often studied and report the most consistent associations with infectious diseases and respiratory, cardiovascular, and neurological outcomes. Temperature is also consistently associated with mortality and healthcare service use. Some associations are less frequently studied, but remain consistent, including the association between some meteorological factors (eg, temperature and heat) and some adverse mental health outcomes (eg, hospital admissions for mental health reasons, suicide, exacerbation of previous mental health conditions), and the association between heat and adverse occupational outcomes and some adverse birth outcomes. Temperature is also associated with adverse nutritional outcomes (likely via crop production and food insecurity) and temperature and humidity are associated with some skin diseases and allergies. Some health outcomes are less frequently studied, but studies suggest an association between temperature and diabetes, impaired sleep, cataracts, heat stress, heat exhaustion and renal diseases.
Extreme weather events (n=24) are consistently associated with mortality, some mental health outcomes (eg, distress, anxiety, depression) and adverse nutritional outcomes (likely via crop production and food insecurity). Some associations are explored less frequently, but these studies suggest an association between drought and respiratory and cardiovascular outcomes (likely via air quality), between extreme weather events and an increased use of healthcare services and some adverse birth outcomes (likely due to indirect causes, such as experiencing stress). Some health outcomes are less frequently studied, but studies suggest an association between extreme weather events and injuries, impaired sleep, oesophageal cancer and exacerbation of chronic illnesses. There are limited and conflicting findings for the association between extreme weather events and infectious diseases, as well as for certain mental health outcomes (eg, suicide and substance abuse). At times, different types of extreme weather events (eg, drought vs flood) led to conflicting findings for some health outcomes (eg, mental health outcomes, infectious diseases), but for other health outcomes, the association was consistent independently of the extreme weather event studied (eg, mortality, healthcare service use and nutritional outcomes).
The impact of air quality on health (n=7) was less frequently studied, but the few studies exploring this association report consistent findings regarding an association with respiratory-specific mortality, adverse respiratory outcomes and an increase in healthcare service use. There is limited evidence regarding the association between air quality and cardiovascular outcomes, limited and inconsistent evidence between wildfire smoke exposure and adverse birth outcomes, and no association is found between exposure to wildfire smoke and increase in use of health services for mental health reasons. Only one review explored the impact of wildfire smoke exposure on ophthalmic outcomes, and it suggests that it may be associated with eye irritation and cataracts.
Reviews which stated climate change as their general focus and did not specify the climate impact(s) under study were less frequent (n=5), but they suggest an association between climate change and pollen allergies in Europe, increased use of healthcare services, obesity, skin diseases and allergies and an association with disability-adjusted life years. Reviews investigating the impact of other climate-related factors (n=3) show inconsistent findings concerning the association between environmental pollutant and adverse birth outcomes, and two reviews suggest an association between environmental risk factors and pollutants and childhood stunting and occupational diseases.
Most reviews concluded by calling for more research, noting the limitations observed among the studies included in their reviews, as well as limitations in their reviews themselves. These limitations included, among others, some systematic reviews having a small number of publications,24 25 language restrictions such as including only papers in English,26 27 arriving at conflicting evidence,28 difficulty concluding a strong association due to the heterogeneity in methods and measurements or the limited equipment and access to quality data in certain contexts,24 29–31 and most studies included were conducted in high-income countries.32 33
Previous authors also discussed the important challenge related to exploring the relationship between climate change and health. Not only is it difficult to explore the potential causal relationship between climate change and health, mostly due to methodological challenges, but there are also a wide variety of complex causal factors that may interact to determine health outcomes. Therefore, the possible causal mechanisms underlying these associations were at times still unknown or uncertain and the impacts of some climate factors were different according to geographical location and specificities of the context. Nonetheless, some reviews offered potential explanations for the climate-health association, with the climate factor at times, having a direct impact on health (eg, flooding causing injuries, heat causing dehydration) and in other cases, having an indirect impact (eg, flooding causing stress which in turn may cause adverse birth outcomes, heat causing difficulty concentrating leading to occupational injuries.)
Discussion
Principal results
In this overview of systematic reviews, we aimed to develop a synthesis of systematic reviews of health impacts of climate change by mapping the characteristics and findings of studies exploring the relationship between climate change and health. We identified four key findings.
First, meteorological impacts, mostly related to temperature and humidity, were the most common impacts studied by included publications, which aligns with findings from a previous scoping review on the health impacts of climate change in the Philippines.10 Indeed, meteorological factors’ impact on all health outcomes identified in this review are explored, although some health outcomes are more rarely explored (eg, mental health and nutritional outcomes). Although this may not be surprising given that a key implication of climate change is the long-term meteorological impact of temperature rise, this finding suggests we also need to undertake research focused on other climate impacts on health, including potential direct and indirect effects of temperature rise, such as the impact of droughts and wildfire smoke. This will allow us to better prepare for the health crises that arise from these ever-increasing climate-related impacts. For instance, the impacts of extreme weather events and air quality on certain health outcomes are not explored (eg, skin diseases and allergies, occupational health) or only rarely explored (eg, pregnancy outcomes).
Second, systematic reviews primarily focus on physical health outcomes, such as infectious diseases, mortality, and respiratory, cardiovascular and neurological outcomes, which also aligns with the country-specific previous scoping review.10 Regarding mortality, we support Campbell and colleagues’34 suggestion that we should expand our focus to include other types of health outcomes. This will provide better support for mitigation policies and allow us to adapt to the full range of threats of climate change.
Moreover, it is unclear whether the distribution of frequencies of health outcomes reflects the actual burden of health impacts of climate change. The most commonly studied health outcomes do not necessarily reflect the definition of health presented by the WHO as, ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’.20 This suggests that future studies should investigate in greater depth the impacts of climate change on mental and broader social well-being. Indeed, some reviews suggested that climate change impacts psychological and social well-being, via broader consequences, such as political instability, health system capacity, migration, and crime,3 4 35 36 thus illustrating how our personal health is determined not only by biological and environmental factors but also by social and health systems. The importance of expanding our scope of health in this field is also recognised in the most recent Lancet report, which states that future reports will include a new mental health indicator.2
Interestingly, the reviews that explored the mental health impacts of climate change were focused mostly on the direct and immediate impacts of experiencing extreme weather events. However, psychologists are also warning about the long-term indirect mental health impacts of climate change, which are becoming more prevalent for children and adults alike (eg, eco-anxiety, climate depression).37 38 Even people who do not experience direct climate impacts, such as extreme weather events, report experiencing distressing emotions when thinking of the destruction of our environment or when worrying about one’s uncertain future and the lack of actions being taken. To foster emotional resilience in the face of climate change, these mental health impacts of climate change need to be further explored. Humanity’s ability to adapt to and mitigate climate change ultimately depends on our emotional capacity to face this threat.
Third, there is a notable geographical difference in the country affiliations of first authors, with three quarters of systematic reviews having been led by first authors affiliated to institutions in Europe, Australia, or North America, which aligns with the findings of the most recent Lancet report.2 While perhaps unsurprising given the inequalities in research funding and institutions concentrated in Western countries, this is of critical importance given the significant health impacts that are currently faced (and will remain) in other parts of the world. Research funding organisations should seek to provide more resources to authors in low-income to middle-income countries to ensure their expertise and perspectives are better represented in the literature.
Fourth, overall, most reviews suggest an association between climate change and the deterioration of health in various ways, illustrating the interdependence of our health and well-being with the well-being of our environment. This interdependence may be direct (eg, heat’s impact on dehydration and exhaustion) or indirect (eg, via behaviour change due to heat.) The most frequently explored and consistently supported associations include an association between temperature and humidity with infectious diseases, mortality and adverse respiratory, cardiovascular and neurological outcomes. Other less frequently studied but consistent associations include associations between climate impacts and increased use of healthcare services, some adverse mental health outcomes, adverse nutritional outcomes and adverse occupational health outcomes. These associations support key findings of the most recent Lancet report, in which authors report, among others, increasing heat exposure being associated with increasing morbidities and mortality, climate change leading to food insecurity and undernutrition, and to an increase in infectious disease transmission.2
That said, a number of reviews included in this study reported limited, conflicting and/or an absence of evidence regarding the association between the climate impact and health outcome. For instance, there was conflicting or limited evidence concerning the association between extreme weather events and infectious diseases, cardiorespiratory outcomes and some mental health outcomes and the association between air quality and cardiovascular-specific mortality and adverse birth outcomes. These conflicting and limited findings highlight the need for further research. These associations are complex and there exist important methodological challenges inherent to exploring the causal relationship between climate change and health outcomes. This relationship may at times be indirect and likely determined by multiple interacting factors.
The climate-health link has been the target of more research in recent years and it is also receiving increasing attention from the public and in both public health and climate communication literature.2 39–41 However, the health framing of climate change information is still underused in climate communications, and researchers suggest we should be doing more to make the link between human health and climate change more explicit to increase engagement with the climate crisis.2 41–43 The health framing of climate communication also has implications for healthcare professionals44 and policy-makers, as these actors could play a key part in climate communication, adaptation and mitigation.41 42 45 These key stakeholders’ perspectives on the climate-health link, as well as their perceived role in climate adaptation and mitigation could be explored,46 since research suggests that health professionals are important voices in climate communications44 and especially since, ultimately, these adverse health outcomes will engender pressure on and cost to our health systems and health workers.
Strengths and limitations
To the best of our knowledge, the current study provides the first broad overview of previous systematic reviews exploring the health impacts of climate change. Our review has three main strengths. First, by targeting systematic reviews, we achieve a higher order summary of findings than what would have been possible by consulting individual original studies. Second, by synthesising findings across all included studies and according to the combination of climate impact and health outcome, we offer a clear, detailed and unique summary of the current state of evidence and knowledge gaps about how climate change may influence human health. This summary may be of use to researchers, policy-makers and communities. Third, we included studies published in all languages about any climate impact and any health outcome. In doing so, we provide a comprehensive and robust overview.
Our work has four main limitations. First, we were unable to access some full texts and therefore some studies were excluded, even though we deemed them potentially relevant after title and abstract inspection. Other potentially relevant systematic reviews may be missing due to unseen flaws in our systematic search. Second, due to the heterogeneity of the included systematic reviews and the relatively small proportion of studies reporting meta-analytic findings, we could not conduct meta-meta-analyses of findings across reviews. Future research is needed to quantify the climate and health links described in this review, as well as to investigate the causal relationship and other interacting factors. Third, due to limited resources, we did not assess overlap between the included reviews concerning the studies they included. Frequencies and findings should be interpreted with potential overlap in mind. Fourth, we conducted the systematic search of the literature in June 2019, and it is therefore likely that some recent systematic reviews are not included in this study.
Conclusions
Overall, most systematic reviews of the health impacts of climate change suggest an association between climate change and the deterioration of health in multiple ways, generally in the direction that climate change is associated with adverse human health outcomes. This is worrisome since these outcomes are predicted to rise in the near future, due to the rise in temperature and increase in climate-change-related events such as extreme weather events and worsened air quality. Most studies included in this review focused on meteorological impacts of climate change on adverse physical health outcomes. Future studies could fill knowledge gaps by exploring other climate-related impacts and broader psychosocial health outcomes. Moreover, studies on health impacts of climate change have mostly been conducted by first authors affiliated with institutions in high-income countries. This inequity needs to be addressed, considering that the impacts of climate change are and will continue to predominantly impact lower income countries. Finally, although most reviews also recommend more research to better understand and quantify these associations, to adapt to and mitigate climate change’s impacts on health, it will also be important to unpack the ‘what, how, and where’ of these effects. Health effects of climate change are unlikely to be distributed equally or randomly through populations. It will be important to mitigate the changing climate’s potential to exacerbate health inequities.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the contributions of Selma Chipenda Dansokho, as research associate, and Thierry Provencher, as research assistant, to this project, and of Frederic Bergeron, for assistance with search strategy, screening and selection of articles for the systematic review.
Footnotes
Twitter: @RutNdjab, @ATricco, @hwitteman
Contributors: RN, CF, ACT, HOW contributed to the design of the study. CB, RN, LPB, RAPR and HOW contributed to the systematic search of the literature and selection of studies. RR, HOW, LC conducted data analysis and interpretation. RR and HOW drafted the first version of the article with early revision by CB, LC and RN. All authors critically revised the article and approved the final version for submission for publication. RR and HOW had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding: This study was funded by the Canadian Institutes of Health Research (CIHR) FDN-148426. The CIHR had no role in determining the study design, the plans for data collection or analysis, the decision to publish, nor the preparation of this manuscript. ACT is funded by a Tier 2 Canada Research Chair in Knowledge Synthesis. HOW is funded by a Tier 2 Canada Research Chair in Human-Centred Digital Health.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as supplementary information. Additional data are not available.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Portier C, Tart K, Carter S. A human health perspective on climate change a report Outlining the research needs on the human health effects of climate change. environmental health perspectives and the National Institute of environmental health sciences, 2010. [Google Scholar]
- 2.Watts N, Amann M, Arnell N, et al. The 2020 report of the Lancet countdown on health and climate change: responding to converging crises. Lancet 2021;397:129–70. 10.1016/S0140-6736(20)32290-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsiang SM, Burke M. Climate, conflict, and social stability: what does the evidence say? Clim Change 2014;123:39–55. 10.1007/s10584-013-0868-3 [DOI] [Google Scholar]
- 4.Hsiang SM, Burke M, Miguel E. Quantifying the influence of climate on human conflict. Science 2013;341:1235367. 10.1126/science.1235367 [DOI] [PubMed] [Google Scholar]
- 5.Patz JA, Frumkin H, Holloway T, et al. Climate change: challenges and opportunities for global health. JAMA 2014;312:1565–80. 10.1001/jama.2014.13186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alderman K, Turner LR, Tong S. Floods and human health: a systematic review. Environ Int 2012;47:37–47. 10.1016/j.envint.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 7.Coates SJ, Davis MDP, Andersen LK. Temperature and humidity affect the incidence of hand, foot, and mouth disease: a systematic review of the literature - a report from the International Society of Dermatology Climate Change Committee. Int J Dermatol 2019;58:388–99. 10.1111/ijd.14188 [DOI] [PubMed] [Google Scholar]
- 8.Duan C, Zhang X, Jin H, et al. Meteorological factors and its association with hand, foot and mouth disease in Southeast and East Asia areas: a meta-analysis. Epidemiol Infect 2019;147:1–18. 10.1017/S0950268818003035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Babaie J, Barati M, Azizi M, et al. A systematic evidence review of the effect of climate change on malaria in Iran. J Parasit Dis 2018;42:331–40. 10.1007/s12639-018-1017-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chua PL, Dorotan MM, Sigua JA, et al. Scoping review of climate change and health research in the Philippines: a complementary tool in research Agenda-Setting. Int J Environ Res Public Health 2019;16:2624. 10.3390/ijerph16142624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lal A, Lill AWT, Mcintyre M, et al. Environmental change and enteric zoonoses in New Zealand: a systematic review of the evidence. Aust N Z J Public Health 2015;39:63–8. 10.1111/1753-6405.12274 [DOI] [PubMed] [Google Scholar]
- 12.Li C, Lu Y, Liu J, et al. Climate change and dengue fever transmission in China: evidences and challenges. Sci Total Environ 2018;622-623:493–501. 10.1016/j.scitotenv.2017.11.326 [DOI] [PubMed] [Google Scholar]
- 13.Herlihy N, Bar-Hen A, Verner G, et al. Climate change and human health: what are the research trends? A scoping review protocol. BMJ Open 2016;6:e012022. 10.1136/bmjopen-2016-012022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosking J, Campbell-Lendrum D. How well does climate change and human health research match the demands of policymakers? A scoping review. Environ Health Perspect 2012;120:1076–82. 10.1289/ehp.1104093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pollock M, Fernandes RM, Becker LA. Chapter V: Overviews of Reviews. : Higgins JPT, Thomas J, Chandler J, . Cochrane Handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane, 2020. [Google Scholar]
- 16.Witteman HO, Dansokho SC, Ndjaboue R. Climate change and human health: an overview of systematic reviews, 2019. Available: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=145972 [Accessed 08 Aug 2020].
- 17.Page M, McKenzie J, Bossuyt P. Updating the PRISMA reporting guideline for systematic reviews and meta-analyses 2020.
- 18.Pollock M, Fernandes RM, Pieper D, et al. Preferred reporting items for Overviews of reviews (prior): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev 2019;8:335. 10.1186/s13643-019-1252-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.About Cochrane reviews. Available: https://www.cochranelibrary.com/about/about-cochrane-reviews [Accessed 14 Sept 2020].
- 20.World Health Organization . Preamble to the Constitution of WHO as adopted by the International Health Conference. New York, 19 June - 22 July 1946 signed on 22 July 1946 by the representatives of 61 States (Official Records of WHO, no. 2, p. 100) and entered into force on 7 April 1948. The definition has not been amended since 1948. Available: https://apps.who.int/gb/bd/pdf_files/BD_49th-en.pdf#page=7
- 21.Covidence systematic review software. Available: www.covidence.org
- 22.Watts N, Amann M, Arnell N, et al. The 2019 report of the Lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet 2019;394:1836–78. 10.1016/S0140-6736(19)32596-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boylan S, Beyer K, Schlosberg D, et al. A conceptual framework for climate change, health and wellbeing in NSW, Australia. Public Health Res Pract 2018;28. 10.17061/phrp2841826. [Epub ahead of print: 06 Dec 2018]. [DOI] [PubMed] [Google Scholar]
- 24.Amegah AK, Rezza G, Jaakkola JJK. Temperature-Related morbidity and mortality in sub-Saharan Africa: a systematic review of the empirical evidence. Environ Int 2016;91:133–49. 10.1016/j.envint.2016.02.027 [DOI] [PubMed] [Google Scholar]
- 25.Odame E, Li Y, Zheng S, et al. Assessing heat-related mortality risks among rural populations: a systematic review and meta-analysis of epidemiological evidence. Int J Environ Res Public Health 2018;15:1597. 10.3390/ijerph15081597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leyva EWA, Beaman A, Davidson PM. Health impact of climate change in older people: an integrative review and implications for nursing. J Nurs Scholarsh 2017;49:670–8. 10.1111/jnu.12346 [DOI] [PubMed] [Google Scholar]
- 27.Phalkey RK, Aranda-Jan C, Marx S, et al. Systematic review of current efforts to quantify the impacts of climate change on undernutrition. Proc Natl Acad Sci U S A 2015;112:E4522–9. 10.1073/pnas.1409769112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porpora MG, Piacenti I, Scaramuzzino S, et al. Environmental contaminants exposure and preterm birth: a systematic review. Toxics 2019;7:11. 10.3390/toxics7010011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bai L, Morton LC, Liu Q. Climate change and mosquito-borne diseases in China: a review. Global Health 2013;9:10. 10.1186/1744-8603-9-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng J, Xu Z, Zhu R, et al. Impact of diurnal temperature range on human health: a systematic review. Int J Biometeorol 2014;58:2011–24. 10.1007/s00484-014-0797-5 [DOI] [PubMed] [Google Scholar]
- 31.Phung D, Huang C, Rutherford S, et al. Climate change, water quality, and water-related diseases in the Mekong delta Basin: a systematic review. Asia Pac J Public Health 2015;27:265–76. 10.1177/1010539514565448 [DOI] [PubMed] [Google Scholar]
- 32.Klinger C, Landeg O, Murray V. Power outages, extreme events and health: a systematic review of the literature from 2011-2012. PLoS Curr 2014;6:ecurrents.dis.04eb1dc5e73dd1377e05a10e9edde673. 10.1371/currents.dis.04eb1dc5e73dd1377e05a10e9edde673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun Z, Chen C, Xu D, et al. Effects of ambient temperature on myocardial infarction: a systematic review and meta-analysis. Environ Pollut 2018;241:1106–14. 10.1016/j.envpol.2018.06.045 [DOI] [PubMed] [Google Scholar]
- 34.Campbell S, Remenyi TA, White CJ, et al. Heatwave and health impact research: a global review. Health Place 2018;53:210–8. 10.1016/j.healthplace.2018.08.017 [DOI] [PubMed] [Google Scholar]
- 35.Zuo J, Pullen S, Palmer J, et al. Impacts of heat waves and corresponding measures: a review. J Clean Prod 2015;92:1–12. 10.1016/j.jclepro.2014.12.078 [DOI] [Google Scholar]
- 36.Benevolenza MA, DeRigne L. The impact of climate change and natural disasters on vulnerable populations: a systematic review of literature. J Hum Behav Soc Environ 2019;29:266–81. 10.1080/10911359.2018.1527739 [DOI] [Google Scholar]
- 37.Clayton S. Climate anxiety: psychological responses to climate change. J Anxiety Disord 2020;74:102263. 10.1016/j.janxdis.2020.102263 [DOI] [PubMed] [Google Scholar]
- 38.Davenport L. Emotional Resiliency in the Era of Climate Change: A Clinician’s Guide. London: Jessica Kingsley Publishers, 2017. [Google Scholar]
- 39.Maibach EW, Nisbet M, Baldwin P, et al. Reframing climate change as a public health issue: an exploratory study of public reactions. BMC Public Health 2010;10:299. 10.1186/1471-2458-10-299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stoknes PE. What we think about when we try not to think about global warming: toward a new psychology of climate action. White River Junction, Vermont: Chelsea Green Publishing, 2015. [Google Scholar]
- 41.Ahmadi S, Schütte S, Herlihy N. Health as a key driver of climate change communication. A scoping review. Preprints 2020:2020100095. [Google Scholar]
- 42.Adlong W, Dietsch E. Environmental education and the health professions: framing climate change as a health issue. Environ Educ Res 2015;21:687–709. 10.1080/13504622.2014.930727 [DOI] [Google Scholar]
- 43.Myers TA, Nisbet MC, Maibach EW, et al. A public health frame arouses hopeful emotions about climate change. Clim Change 2012;113:1105–12. 10.1007/s10584-012-0513-6 [DOI] [Google Scholar]
- 44.Costello A, Montgomery H, Watts N. Climate change: the challenge for healthcare professionals. BMJ 2013;347:f6060. 10.1136/bmj.f6060 [DOI] [PubMed] [Google Scholar]
- 45.Gould S, Rudolph L. Challenges and opportunities for advancing work on climate change and public health. Int J Environ Res Public Health 2015;12:15649–72. 10.3390/ijerph121215010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang L, Liu C, Hess J, et al. Health professionals in a changing climate: protocol for a scoping review. BMJ Open 2019;9:e024451. 10.1136/bmjopen-2018-024451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Berhane K, Kumie A, Samet J. Health effects of environmental exposures, occupational hazards and climate change in Ethiopia: synthesis of situational analysis, needs assessment and the way forward. Ethiop J Health Dev 2016;30:50–6. [PMC free article] [PubMed] [Google Scholar]
- 48.Bernhardt V, Finkelmeier F, Verhoff MA, et al. Myiasis in humans—a global case report evaluation and literature analysis. Parasitol Res 2019;118:389–97. 10.1007/s00436-018-6145-7 [DOI] [PubMed] [Google Scholar]
- 49.de Sousa TCM, Amancio F, Hacon SdeS, et al. [Climate-sensitive diseases in Brazil and the world: systematic reviewEnfermedades sensibles al clima en Brasil y el mundo: revisión sistemática]. Rev Panam Salud Publica 2018;42:e85. 10.26633/RPSP.2018.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dhimal M, Ahrens B, Kuch U. Climate change and spatiotemporal distributions of vector-borne diseases in Nepal – a systematic synthesis of literature. PLoS One 2015;10:e0129869. 10.1371/journal.pone.0129869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fan J, Wei W, Bai Z, et al. A systematic review and meta-analysis of dengue risk with temperature change. Int J Environ Res Public Health 2015;12:1–15. 10.3390/ijerph120100001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roda Gracia J, Schumann B, Seidler A. Climate variability and the occurrence of human Puumala hantavirus infections in Europe: a systematic review. Zoonoses Public Health 2015;62:465–78. 10.1111/zph.12175 [DOI] [PubMed] [Google Scholar]
- 53.Hedlund C, Blomstedt Y, Schumann B. Association of climatic factors with infectious diseases in the Arctic and subarctic region – a systematic review. Glob Health Action 2014;7:24161. 10.3402/gha.v7.24161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hii YL, Zaki RA, Aghamohammadi N, et al. Research on climate and dengue in Malaysia: a systematic review. Curr Environ Health Rep 2016;3:81–90. 10.1007/s40572-016-0078-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Khader YS, Abdelrahman M, Abdo N, et al. Climate change and health in the eastern Mediterranean countries: a systematic review. Rev Environ Health 2015;30:163–81. 10.1515/reveh-2015-0013 [DOI] [PubMed] [Google Scholar]
- 56.Matysiak A, Roess A. Interrelationship between climatic, ecologic, social, and cultural determinants affecting dengue emergence and transmission in Puerto Rico and their implications for Zika response. J Trop Med 2017;2017:1–14. 10.1155/2017/8947067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Naish S, Dale P, Mackenzie JS, et al. Climate change and dengue: a critical and systematic review of quantitative modelling approaches. BMC Infect Dis 2014;14:167. 10.1186/1471-2334-14-167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nichols A, Maynard V, Goodman B, et al. Health, climate change and sustainability: a systematic review and thematic analysis of the literature. Environ Health Insights 2009;3:EHI.S3003–88. 10.4137/EHI.S3003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Racloz V, Ramsey R, Tong S, et al. Surveillance of dengue fever virus: a review of epidemiological models and early warning systems. PLoS Negl Trop Dis 2012;6:e1648. 10.1371/journal.pntd.0001648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Swynghedauw B. [Medical consequences of global warming]. Presse Med 2009;38:551–61. 10.1016/j.lpm.2008.02.022 [DOI] [PubMed] [Google Scholar]
- 61.Waits A, Emelyanova A, Oksanen A, et al. Human infectious diseases and the changing climate in the Arctic. Environ Int 2018;121:703–13. 10.1016/j.envint.2018.09.042 [DOI] [PubMed] [Google Scholar]
- 62.Xu Z, Etzel RA, Su H, et al. Impact of ambient temperature on children's health: a systematic review. Environ Res 2012;117:120–31. 10.1016/j.envres.2012.07.002 [DOI] [PubMed] [Google Scholar]
- 63.Yu W, Mengersen K, Dale P, et al. Projecting future transmission of malaria under climate change scenarios: challenges and research needs. Crit Rev Environ Sci Technol 2015;45:777–811. 10.1080/10643389.2013.852392 [DOI] [Google Scholar]
- 64.Veenema TG, Thornton CP, Lavin RP, et al. Climate Change-Related water disasters' impact on population health. J Nurs Scholarsh 2017;49:625–34. 10.1111/jnu.12328 [DOI] [PubMed] [Google Scholar]
- 65.Brown L, Murray V. Examining the relationship between infectious diseases and flooding in Europe: a systematic literature review and summary of possible public health interventions. Disaster Health 2013;1:117–27. 10.4161/dish.25216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tall JA, Gatton ML, Tong S. Ross River virus disease activity associated with naturally occurring Nontidal flood events in Australia: a systematic review. J Med Entomol 2014;51:1097–108. 10.1603/ME14007 [DOI] [PubMed] [Google Scholar]
- 67.Ghazani M, FitzGerald G, Hu W, et al. Temperature variability and gastrointestinal infections: a review of impacts and future perspectives. Int J Environ Res Public Health 2018;15:766. 10.3390/ijerph15040766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gao J, Sun Y, Lu Y, et al. Impact of ambient humidity on child health: a systematic review. PLoS One 2014;9:e112508. 10.1371/journal.pone.0112508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lal A, Fearnley E, Wilford E. Local weather, flooding history and childhood diarrhoea caused by the parasite Cryptosporidium spp.: a systematic review and meta-analysis. Sci Total Environ 2019;674:300–6. 10.1016/j.scitotenv.2019.02.365 [DOI] [PubMed] [Google Scholar]
- 70.Levy K, Woster AP, Goldstein RS, et al. Untangling the impacts of climate change on waterborne diseases: a systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ Sci Technol 2016;50:4905–22. 10.1021/acs.est.5b06186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Philipsborn R, Ahmed SM, Brosi BJ, et al. Climatic drivers of diarrheagenic Escherichia coli incidence: a systematic review and meta-analysis. J Infect Dis 2016;214:6–15. 10.1093/infdis/jiw081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Semenza JC, Herbst S, Rechenburg A, et al. Climate change impact assessment of food- and waterborne diseases. Crit Rev Environ Sci Technol 2012;42:857–90. 10.1080/10643389.2010.534706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stensgaard A-S, Vounatsou P, Sengupta ME, et al. Schistosomes, snails and climate change: current trends and future expectations. Acta Trop 2019;190:257–68. 10.1016/j.actatropica.2018.09.013 [DOI] [PubMed] [Google Scholar]
- 74.Welch K, Shipp-Hilts A, Eidson M, et al. Salmonella and the changing environment: systematic review using new York state as a model. J Water Health 2019;17:179–95. 10.2166/wh.2018.224 [DOI] [PubMed] [Google Scholar]
- 75.Cann KF, Thomas DR, Salmon RL, et al. Extreme water-related weather events and waterborne disease. Epidemiol Infect 2013;141:671–86. 10.1017/S0950268812001653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stanke C, Kerac M, Prudhomme C, et al. Health effects of drought: a systematic review of the evidence. PLoS Curr 2013;5:ecurrents.dis.7a2cee9e980f91ad7697b570bcc4b004. 10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bunker A, Wildenhain J, Vandenbergh A, et al. Effects of air temperature on Climate-Sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 2016;6:258–68. 10.1016/j.ebiom.2016.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Huang C, Barnett AG, Wang X, et al. Projecting future heat-related mortality under climate change scenarios: a systematic review. Environ Health Perspect 2011;119:1681–90. 10.1289/ehp.1103456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ghanizadeh G, Heidari M, Seifi B. The effect of climate change on cardiopulmonary disease-a systematic review. J Clin Diagn Res 2017;11:IE01–4.28658802 [Google Scholar]
- 80.Hajat S, Kosatky T. Heat-Related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health 2010;64:753–60. 10.1136/jech.2009.087999 [DOI] [PubMed] [Google Scholar]
- 81.Lawton EM, Pearce H, Gabb GM. Review article: environmental heatstroke and long‐term clinical neurological outcomes: a literature review of case reports and case series 2000–2016. Emerg Med Australas 2019;31:163–73. 10.1111/1742-6723.12990 [DOI] [PubMed] [Google Scholar]
- 82.Lian H, Ruan Y, Liang R, et al. Short-Term effect of ambient temperature and the risk of stroke: a systematic review and meta-analysis. Int J Environ Res Public Health 2015;12:9068–88. 10.3390/ijerph120809068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Moghadamnia MT, Ardalan A, Mesdaghinia A, et al. Ambient temperature and cardiovascular mortality: a systematic review and meta-analysis. PeerJ 2017;5:3574. 10.7717/peerj.3574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Salve HR, Parthasarathy R, Krishnan A, et al. Impact of ambient air temperature on human health in India. Rev Environ Health 2018;33:433–9. 10.1515/reveh-2018-0024 [DOI] [PubMed] [Google Scholar]
- 85.Sanderson M, Arbuthnott K, Kovats S, et al. The use of climate information to estimate future mortality from high ambient temperature: a systematic literature review. PLoS One 2017;12:e0180369. 10.1371/journal.pone.0180369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Witt C, Schubert AJ, Jehn M, et al. The effects of climate change on patients with chronic lung disease. A systematic literature review. Dtsch Arztebl Int 2015;112:878–83. 10.3238/arztebl.2015.0878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xu Z, Sheffield PE, Su H, et al. The impact of heat waves on children’s health: a systematic review. Int J Biometeorol 2014;58:239–47. 10.1007/s00484-013-0655-x [DOI] [PubMed] [Google Scholar]
- 88.Xu Z, FitzGerald G, Guo Y, et al. Impact of heatwave on mortality under different heatwave definitions: a systematic review and meta-analysis. Environ Int 2016;89:193–203. 10.1016/j.envint.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 89.Yu W, Mengersen K, Wang X, et al. Daily average temperature and mortality among the elderly: a meta-analysis and systematic review of epidemiological evidence. Int J Biometeorol 2012;56:569–81. 10.1007/s00484-011-0497-3 [DOI] [PubMed] [Google Scholar]
- 90.Doocy S, Dick A, Daniels A, et al. The human impact of tropical cyclones: a historical review of events 1980-2009 and systematic literature review. PLoS Curr 2013;5:ecurrents.dis.2664354a5571512063ed29d25ffbce74. 10.1371/currents.dis.2664354a5571512063ed29d25ffbce74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Madaniyazi L, Guo Y, Yu W, et al. Projecting future air pollution-related mortality under a changing climate: progress, uncertainties and research needs. Environ Int 2015;75:21–32. 10.1016/j.envint.2014.10.018 [DOI] [PubMed] [Google Scholar]
- 92.Liu JC, Pereira G, Uhl SA, et al. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ Res 2015;136:120–32. 10.1016/j.envres.2014.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Reid CE, Brauer M, Johnston FH, et al. Critical review of health impacts of Wildfire smoke exposure. Environ Health Perspect 2016;124:1334–43. 10.1289/ehp.1409277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Youssouf H, Liousse C, Roblou L, et al. Non-Accidental health impacts of Wildfire smoke. Int J Environ Res Public Health 2014;11:11772–804. 10.3390/ijerph111111772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lake IR, Jones NR, Agnew M, et al. Climate change and future pollen allergy in Europe. Environ Health Perspect 2017;125:385–91. 10.1289/EHP173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cong X, Xu X, Zhang Y, et al. Temperature drop and the risk of asthma: a systematic review and meta-analysis. Environ Sci Pollut Res 2017;24:22535–46. 10.1007/s11356-017-9914-4 [DOI] [PubMed] [Google Scholar]
- 97.Xu Z, Crooks JL, Davies JM, et al. The association between ambient temperature and childhood asthma: a systematic review. Int J Biometeorol 2018;62:471–81. 10.1007/s00484-017-1455-5 [DOI] [PubMed] [Google Scholar]
- 98.Sawatzky A, Cunsolo A, Jones-Bitton A, et al. Responding to climate and environmental change impacts on human health via integrated surveillance in the circumpolar North: a systematic realist review. Int J Environ Res Public Health 2018;15:30. 10.3390/ijerph15122706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wald A. Emergency department visits and costs for heat-related illness due to extreme heat or heat waves in the United States: an integrated review. Nurs Econ 2019;37:35–48. [Google Scholar]
- 100.Gao J, Cheng Q, Duan J, et al. Ambient temperature, sunlight duration, and suicide: a systematic review and meta-analysis. Sci Total Environ 2019;646:1021–9. 10.1016/j.scitotenv.2018.07.098 [DOI] [PubMed] [Google Scholar]
- 101.Rataj E, Kunzweiler K, Garthus-Niegel S. Extreme weather events in developing countries and related injuries and mental health disorders - a systematic review. BMC Public Health 2016;16:1020. 10.1186/s12889-016-3692-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fernandez A, Black J, Jones M, et al. Flooding and mental health: a systematic mapping review. PLoS One 2015;10:e0119929. 10.1371/journal.pone.0119929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Vins H, Bell J, Saha S, et al. The mental health outcomes of drought: a systematic review and causal process diagram. Int J Environ Res Public Health 2015;12:13251–75. 10.3390/ijerph121013251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Carolan-Olah M, Frankowska D. High environmental temperature and preterm birth: a review of the evidence. Midwifery 2014;30:50–9. 10.1016/j.midw.2013.01.011 [DOI] [PubMed] [Google Scholar]
- 105.Kuehn L, McCormick S. Heat exposure and maternal health in the face of climate change. Int J Environ Res Public Health 2017;14:29. 10.3390/ijerph14080853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Poursafa P, Keikha M, Kelishadi R. Systematic review on adverse birth outcomes of climate change. J Res Med Sci 2015;20:397–402. [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang Y, Yu C, Wang L. Temperature exposure during pregnancy and birth outcomes: an updated systematic review of epidemiological evidence. Environ Pollut 2017;225:700–12. 10.1016/j.envpol.2017.02.066 [DOI] [PubMed] [Google Scholar]
- 108.An R, Ji M, Zhang S. Global warming and obesity: a systematic review. Obes Rev 2018;19:150–63. 10.1111/obr.12624 [DOI] [PubMed] [Google Scholar]
- 109.Vilcins D, Sly PD, Jagals P. Environmental risk factors associated with child stunting: a systematic review of the literature. Annals of Global Health 2018;84:551–62. 10.29024/aogh.2361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Huang K-C, Weng H-H, Yang T-Y, et al. Distribution of fatal Vibrio vulnificus necrotizing skin and soft-tissue infections: a systematic review and meta-analysis. Medicine 2016;95:e2627. 10.1097/MD.0000000000002627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Augustin J, Franzke N, Augustin M, et al. Does climate change affect the incidence of skin and allergic diseases in Germany? J Dtsch Dermatol Ges 2008;6:632–8. 10.1111/j.1610-0387.2008.06676.x [DOI] [PubMed] [Google Scholar]
- 112.Binazzi A, Levi M, Bonafede M, et al. Evaluation of the impact of heat stress on the occurrence of occupational injuries: meta-analysis of observational studies. Am J Ind Med 2019;62:233–43. 10.1002/ajim.22946 [DOI] [PubMed] [Google Scholar]
- 113.Bonafede M, Marinaccio A, Asta F, et al. The association between extreme weather conditions and work-related injuries and diseases. A systematic review of epidemiological studies. Ann Ist Super Sanita 2016;52:357–67. 10.4415/ANN_16_03_07 [DOI] [PubMed] [Google Scholar]
- 114.Flouris AD, Dinas PC, Ioannou LG, et al. Workers' health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health 2018;2:e521–31. 10.1016/S2542-5196(18)30237-7 [DOI] [PubMed] [Google Scholar]
- 115.Levi M, Kjellstrom T, Baldasseroni A. Impact of climate change on occupational health and productivity: a systematic literature review focusing on workplace heat. Med Lav 2018;109:163–79. 10.23749/mdl.v109i3.6851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Varghese BM, Hansen A, Bi P, et al. Are workers at risk of occupational injuries due to heat exposure? A comprehensive literature review. Saf Sci 2018;110:380–92. 10.1016/j.ssci.2018.04.027 [DOI] [Google Scholar]
- 117.Wimalawansa SA, Wimalawansa SJ. Environmentally induced, occupational diseases with emphasis on chronic kidney disease of multifactorial origin affecting tropical countries. Ann Occup Environ Med 2016;28:33. 10.1186/s40557-016-0119-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang Y, Bi P, Hiller JE. Climate change and disability-adjusted life years. J Environ Health 2007;70:32–6. [PubMed] [Google Scholar]
- 119.Park KY, Kim HJ, Ahn HS, et al. Association between acute gouty arthritis and Meteorological factors: an ecological study using a systematic review and meta-analysis. Semin Arthritis Rheum 2017;47:369–75. 10.1016/j.semarthrit.2017.05.006 [DOI] [PubMed] [Google Scholar]
- 120.Otte im Kampe E, Kovats S, Hajat S. Impact of high ambient temperature on unintentional injuries in high-income countries: a narrative systematic literature review. BMJ Open 2016;6:e010399. 10.1136/bmjopen-2015-010399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rifkin DI, Long MW, Perry MJ. Climate change and sleep: a systematic review of the literature and conceptual framework. Sleep Med Rev 2018;42:3–9. 10.1016/j.smrv.2018.07.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-046333supp001.pdf (42.4KB, pdf)
bmjopen-2020-046333supp002.pdf (22.3KB, pdf)
bmjopen-2020-046333supp003.pdf (185.2KB, pdf)
bmjopen-2020-046333supp004.pdf (75KB, pdf)
bmjopen-2020-046333supp005.pdf (32.8KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as supplementary information. Additional data are not available.