Summary:
Prepectoral breast reconstruction through a small axillary incision during endoscopic-assisted nipple-sparing mastectomy or robotic nipple-sparing mastectomy is difficult. Cases involving implants covered with an acellular dermal matrix (ADM) are particularly difficult. Therefore, a new delivery technique for ADM-covered implants is needed. The ADM pocket for complete coverage of the implant is made with double-crossed ADMs. The pocket end is open and sutured at the funnel entry. After insetting the ADM pocket at the mastectomy site through an axillary incision, the implant is delivered from a funnel to the ADM pocket by squeezing. Prepectoral breast reconstruction with the new delivery technique for implants covered with ADM pockets proved easy and safe. Our new implant delivery technique could be a good option for prepectoral breast reconstruction after minimal breast surgery.
Minimally invasive surgery has become the mainstay breast cancer surgery, and innovative types of nipple-sparing mastectomy (NSM), such as endoscopic-assisted NSM, are being increasingly applied to treat breast cancer.1,2 A new minimally invasive surgery technique uses a single axillary incision for single-port endoscopic-assisted NSM3 and robotic NSM,4,5 which are feasible and safe procedures with good cosmetic results.
Prosthetic breast reconstruction became possible after the introduction and commercialization of the silicone gel breast implant in the 1960s. The ideal anatomical placement for prosthetic implants has been the subject of discussion, and opinions have changed over time. Prepectoral plane breast reconstruction is safe and effective, with complication rates comparable to standard techniques.6 In particular, the use of bioprosthetic material, such as acellular dermal matrix (ADM), has enabled surgeons to achieve a greater degree of soft-tissue support and hence improve outcomes.7
Prepectoral reconstruction, with complete or nearly complete implant coverage with ADM, is difficult in procedures using a small incision, such as endoscopic-assisted NSM, which has a single axillary incision, and in robotic NSM. Therefore, we suggest a new delivery technique for ADM-covered implants.
TECHNIQUE
Patient Selection
We selected breast cancer patients indicated for NSM. The other inclusion criteria were low risk of skin invasion, small-to-moderate-sized breast reconstruction, and adequate skin flap thickness and vascularity following mastectomy (Fig. 1A).
Fig. 1.
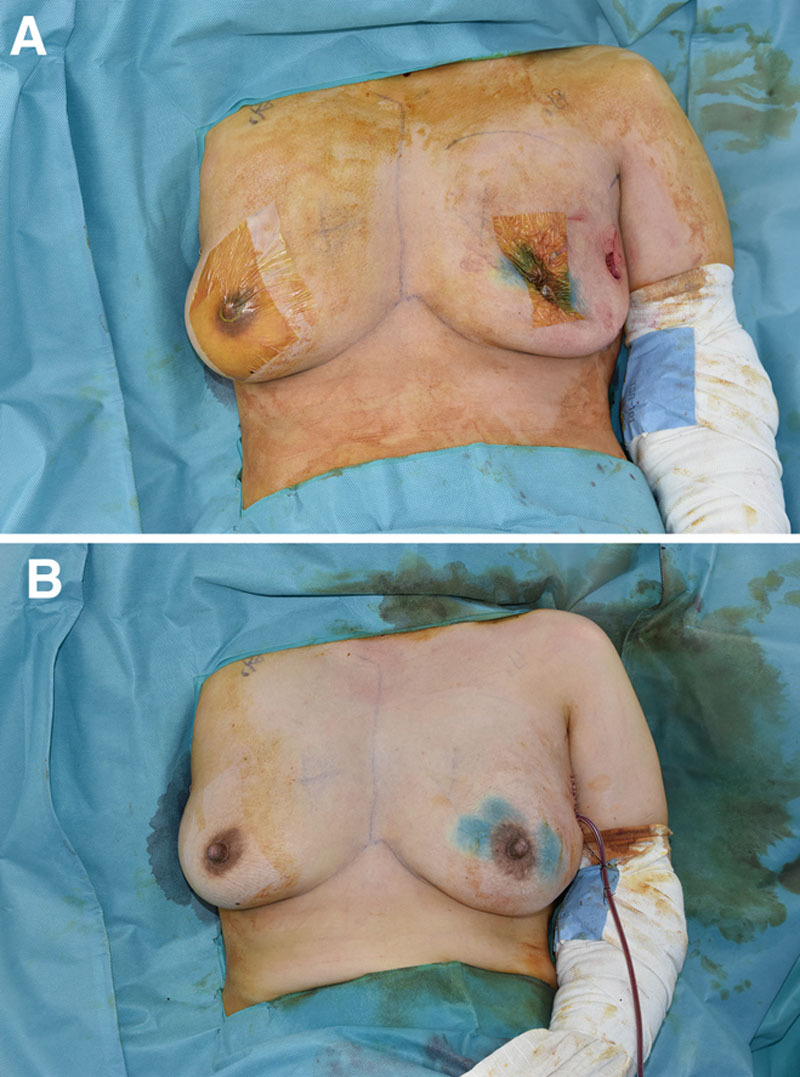
Images taken before and after breast reconstruction. A, Pre-reconstruction Image. B, Post-reconstruction image.
Delivery Technique
The horizontal and vertical circumferences of the implant were measured using a measuring tape, and 2 appropriately sized ADMs were applied. Pliable ADMs (CGDerm One-step; CGBio Co. Ltd., Hwaseong, South Korea) were used to fully cover the implant. The temporal sizer was completely covered with double-crossed ADMs, as described previously. The margins of the ADMs were sewed with interrupted suture using 2-0 Vicryl (Fig. 2A).7
Fig. 2.
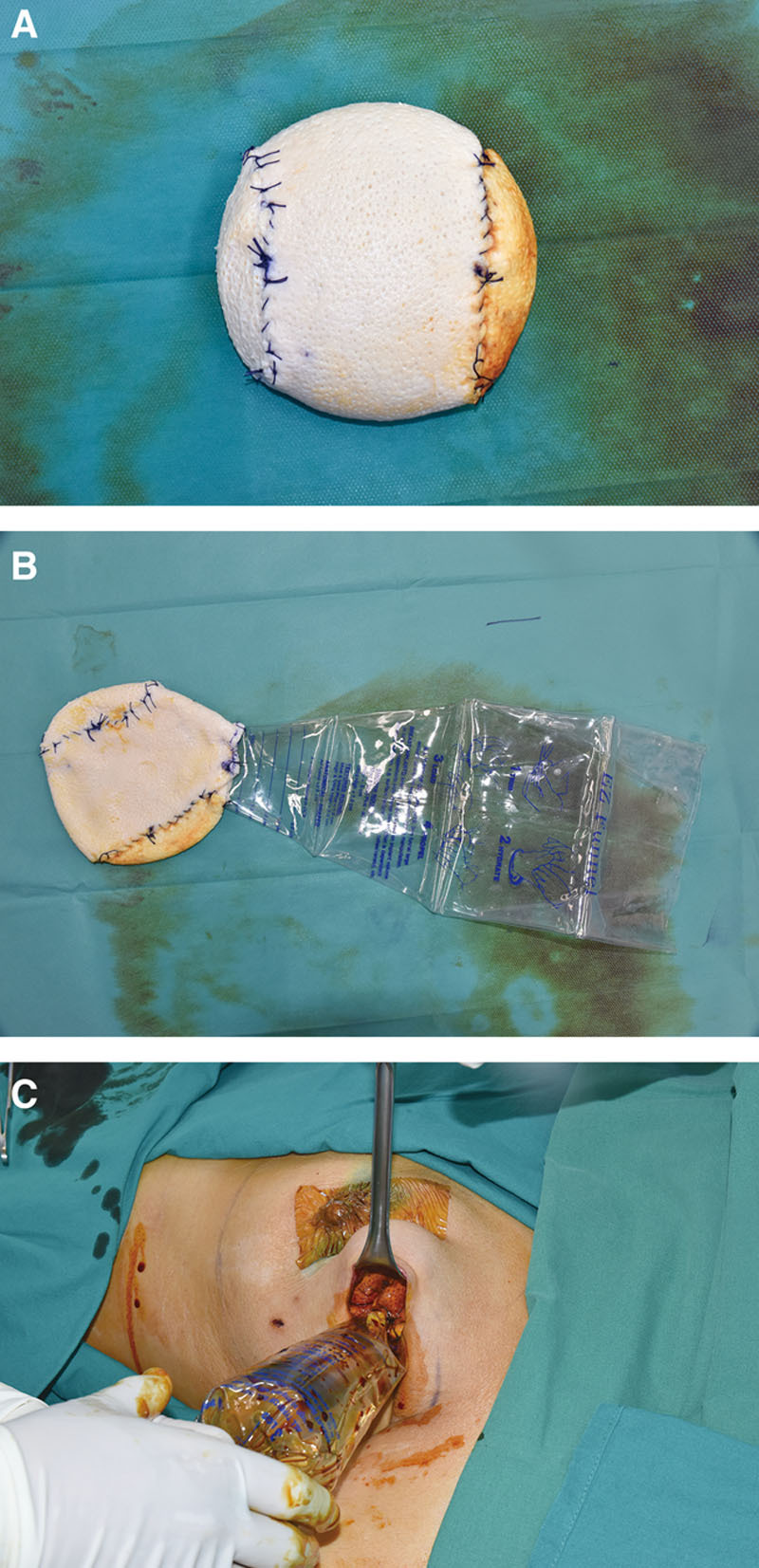
Operative process of implant delivery technique. A, An ADM pocket prepared with double-crossed ADMs completely covers the temporal sizer. B, After removing the temporal sizer, the funnel tip was sutured to the opening of the ADM pocket. C, After insetting the ADM pocket at the mastectomy site, the implant was delivered to the pocket via the funnel by squeezing.
After removing the temporal sizer through an opening in the ADM pocket, the opening was modified for compatibility with the tip size of a funnel (EZ funnel, UN Healthcare, Okcheon-gun, Chungcheongbuk-do, South Korea), and 4 fixation points were created to prevent slippage of the funnel (Fig. 2B). The pectoralis major muscle was left entirely intact, and wounds were irrigated with gentamicin and cetrazole. The ADM pocket was connected to the mastectomy site through an axillary incision. The smooth, round and 275 cc silicone-filled implant (Mentor Worldwide, Irvine, Calif.) was inserted into the ADM pocket at the mastectomy site via the funnel, and its position was then checked (Fig. 2C). After inserting the implant into the pocket with minimal manipulation, two absorbable sutures were used to bind the ADMs such that they completely covered the implant. The ADM was not secured in the breast pocket (Fig. 1B). The stability of the ADM-covered implant during consolidation was achieved through a postoperative compression garment.
DISCUSSION
Advances have been made over the past 20 years in the techniques, devices, and technology available to surgeons to reconstruct female breasts. Nearly 70% of breast reconstructions in the United States are implant-based.8 A 78% increase in immediate breast reconstruction and 203% rise in implant use were observed from 1998 to 2008.9 These increasing trends continue today, as advancements in technology have improved techniques and outcomes for prosthetic-based breast reconstruction. Refined ablative techniques, ADM, the latest generation of devices (tissue expanders and silicone implants), fat grafting, and tools for assessing intraoperative perfusion have enabled the use of totally ADM-covered devices in the subcutaneous (prepectoral) plane.6
The ideal anatomical position of prosthetic implants has been the subject of discussion and has changed over time. The advantages of prepectoral breast reconstruction are clear. The technique is less invasive and may be associated with less pain because the pectoralis major muscle remains undisturbed. Also, the simplicity of the procedure decreases the surgical and anesthesia times, resulting in less narcotic use.10 One particularly obvious advantage is the decreased risk of animation deformity. The long-term benefits of prepectoral reconstruction remain speculative; however, recent 2–3 year follow-up data are promising.6
In the 1990s, ADM was introduced to the reconstructive market and was quickly adopted for use during breast reconstruction. Surgeons were attracted to the shorter operating times and reduced postoperative pain. In addition, the pliability, biocompatibility, and off-the-shelf availability made ADM an excellent tool for covering the inferior pole of the reconstructed breast, helping ensure precise placement of the tissue expander or implant. The ADM is now used in the majority of implant-based reconstructions.11
The development of the funnel, a mechanical insertion device, in 2009 maximized a no-touch implant technique by giving an alternative to hand-placement of implants into breast pockets. The funnel is constructed of polymeric vinyl with a lubricous hydrophilic coating. The funnel is cut to implant size and then hydrated before the implant is poured directly from the packaging into the funnel. Finally, the funnel is placed about 1 cm inside the dissected pocket, and the implant is advanced through the funnel into the pocket as a no-skin touch technique.12
Minimally invasive surgeries for breast cancer, such as single-port endoscopic-assisted NSM and robotic NSM, use a single axillary incision. In previous studies, patients were satisfied with the location of the incision and the postoperative appearance of the scar.3,5 However, immediate breast reconstruction after single-port endoscopic-assisted NSM and robotic NSM is a difficult procedure. In particular, prepectoral breast reconstruction is more difficult if an ADM-covered implant is required. The new delivery technique presented herein overcomes these limitations of implant reconstruction after minimally invasive breast surgery.
ACKNOWLEDGMENTS
This work was supported by a research fund from Chungnam National University and by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI20C2088).
Footnotes
Published online 10 June 2021.
Disclosure: All the authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Sakamoto N, Fukuma E, Higa K, et al. Early results of an endoscopic nipple-sparing mastectomy for breast cancer. Ann Surg Oncol. 2009; 16:3406–.3413 [DOI] [PubMed] [Google Scholar]
- 2.Lai HW, Chen ST, Chen DR, et al. Current trends in and indications for endoscopy-assisted breast surgery for breast cancer: Results from a six-year study conducted by the Taiwan endoscopic breast surgery cooperative group. PLoS One. 2016; 11:e0150310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tukenmez M, Ozden BC, Agcaoglu O, et al. Videoendoscopic single-port nipple-sparing mastectomy and immediate reconstruction. J Laparoendosc Adv Surg Tech A. 2014; 24:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toesca A, Peradze N, Manconi A, et al. Robotic nipple-sparing mastectomy for the treatment of breast cancer: Feasibility and safety study. Breast. 2017; 31:51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarfati B, Struk S, Leymarie N, et al. Robotic prophylactic nipple-sparing mastectomy with immediate prosthetic breast reconstruction: A prospective study. Ann Surg Oncol. 2018; 25:2579–2586. [DOI] [PubMed] [Google Scholar]
- 6.Woo A, Harless C, Jacobson SR. Revisiting an old place: Single-surgeon experience on post-mastectomy subcutaneous implant-based breast reconstruction. Breast J. 2017; 23:545–553. [DOI] [PubMed] [Google Scholar]
- 7.Lee JS, Kim JS, Lee JH, et al. Prepectoral breast reconstruction with complete implant coverage using double-crossed acellular dermal matrixs. Gland Surg. 2019; 8:748–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng SK, Hare RM, Kuang RJ, et al. Breast reconstruction post mastectomy: Patient satisfaction and decision making. Ann Plast Surg. 2016; 76:640–644. [DOI] [PubMed] [Google Scholar]
- 9.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: Increasing implant rates. Plast Reconstr Surg. 2013; 131:15–23. [DOI] [PubMed] [Google Scholar]
- 10.Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral implant-based breast reconstruction: Rationale, indications, and preliminary results. Plast Reconstr Surg. 2017; 139:287–294. [DOI] [PubMed] [Google Scholar]
- 11.DeLong MR, Tandon VJ, Farajzadeh M, et al. Systematic review of the impact of acellular dermal matrix on aesthetics and patient satisfaction in tissue expander-to-implant breast reconstructions. Plast Reconstr Surg. 2019; 144:967e–974e. [DOI] [PubMed] [Google Scholar]
- 12.Newman AN, Davison SP. Effect of Keller Funnel on the rate of capsular contracture in periareolar breast augmentation. Plast Reconstr Surg Glob Open. 2018; 6:e1834. [DOI] [PMC free article] [PubMed] [Google Scholar]


