Abstract
Background:
Language barriers can influence the quality of healthcare and health outcomes of LEP patients with cancer. The use of medical interpretation services can be a valuable asset for improving communications in emergency care settings.
Objective:
To evaluate whether a mobile translation application increased call frequency to interpreter services among providers in an Urgent Care Center (UCC) at a comprehensive cancer center and to assess provider satisfaction of the mobile application.
Research Design:
Prospective pre-post non-randomized intervention of a mobile translation application with access to an over the phone interpreter (OPI) service at the push of a button and post-study satisfaction survey.
Subjects:
65 clinicians working at the UCC in a cancer center in New York City.
Measures:
Mean call frequency to OPI services, tested by the nonparametric Wilcoxon Mann Whitney test, and self-reported provider satisfaction descriptives.
Results:
The mobile application contributed to increasing the frequency of phone calls to OPI services during the intervention period (mean = 12.8; p = .001) as compared to the pre-intervention period (mean = 4.3), and showed continued use during the post-intervention period (mean = 5.7). Most clinicians were satisfied with the use of the mobile application and access to the OPI services.
Conclusions:
The results suggest that mobile application tools contribute to increasing the use and ease of access to language services. This has the potential to improve the quality of communication between medical providers and LEP patients in the delivery of cancer care in urgent care settings.
Keywords: Cancer, Communication, Health Information Technology, Language Barriers, Limited English Proficient
Introduction
The United States population is diverse, with more than 21% of people (62 million) five years and older speaking a language other than English at home (1). Language barriers lead to health disparities that hinder the quality of care for the growing US population with limited English proficiency (LEP), which increased 80% from 1990 to 2013 (2), and stood at 9% of the U.S. population in 2015 (3). Federal regulations regarding the provision of language services for patients with LEP exist (4) but there is wide variation in compliance with these mandates (5, 6). In addition, insurers do not reimburse for interpreters except in California, where private insurers reimburse for interpreter services (7), and the few states that allocate partial reimbursement for interpreter expenditures for Medicaid or Children’s Health Insurance Program LEP patients (8, 9). In one study, the majority of hospitals surveyed report that family members or untrained staff (ad-hoc interpreters) were used as interpreters instead of professional interpreters (6). Furthermore, 19% of hospitals were not in compliance with any of the language-related mandates (6). Although language assistance services are available at healthcare organizations, research has demonstrated that these services are often underused (10). Language barriers can lead to miscommunication between patients and their healthcare providers, particularly in the emergency department (ED) setting where timely and accurate responses to questions are essential. The number of visits to the ED by LEP patients are as much as 60% higher than English-speaking patients (11), and LEP patients are 24% more likely to return unplanned to the ED within 72 hours (12). Compared to English-speaking patients, LEP patients in the ED setting are more likely to report a poor understanding of their diagnoses and treatment plans (13), be admitted to the hospital for the same complaint (14), and have more laboratory testing or imaging (14). LEP patients are less likely to receive pain medications (15) and to be referred for follow-up appointments from the ED (16).
For cancer patients in the ED setting, communication can be especially challenging due to time constraints and the acuity of their medical issues. Without professional interpreters, LEP patients with cancer are less likely to receive adequate symptom control and optimal palliative care (17), are less likely to have appropriate information and understanding about diagnosis and prognosis (18, 19), and may have more miscommunications with their providers (20, 21). The presence of interpreters can improve the quality of palliative care services for LEP patients (22). The persistence of disparities experienced by LEP patients highlights the need for targeted interventions to improve the care for LEP patients.
Telephone interpreters can be a valuable resource for LEP patients when in-person interpreter services are limited. Telephone and video interpreting can also abate the costs of the system inefficiencies associated with in-person interpretation, in that the professional interpreters employed in these modalities can focus exclusively on interpreting rather than spending time traveling to clinical encounters (23). Emerging communication technologies can decrease communication barriers in clinical settings (24, 25). However, the use of technology to communicate with patients has obvious limitations, including the accuracy and applicability of the tools for patient care (26). Google Translate is an example of a real-time translation tool, offering web or mobile interface for iOS and Android (27). Online translation tools have been shown to reduce misunderstandings between medical providers and patients (25, 28). Additionally, when urgency and the cost of obtaining an in-person interpreter are a factor, the use of online translation tools may address communication barriers (29). Given that good quality language assistance services can contribute to effective physician-patient communication, quality healthcare, cost-effectiveness, patient satisfaction, and efficient resource utilization (30), the implementation of emerging interpretation tools, including mobile technology, could help when caring for LEP patients in emergency settings (31).
The primary aim of this study was to evaluate whether a mobile application increased the frequency of interpreter services use among providers at a comprehensive cancer center’s Urgent Care Center (UCC), which functions as an ED, in New York. We also assessed provider satisfaction with the application. The application had two main features, 1) the ability to directly call the institution’s over the phone interpreter (OPI) service and 2) a library of pre-translated medical phrases and questions that could be played as audio files and/or displayed as text. We hypothesized that use of the mobile application in the UCC would improve the workflow for accessing interpreters and thus, increase the frequency of use of interpreter services.
Methods
Study Design and Procedure
To evaluate the utility of the mobile application, we designed a prospective pre-post study, conducted from December 2014 to July 2015 in a large cancer center’s UCC. The UCC was selected because patients frequently present with new complaints that need to be explored in a timely manner (e.g., fever, pain, shortness of breath) and interpreter services cannot be arranged before the patient visit as can be done in the outpatient setting. The study was approved by the center’s IRB.
During the pre-intervention period, 2.5 months, interpreter services use was tracked for individual clinicians who worked in the UCC, including potential study participants. This served as the comparison group to the data collected during the intervention. Following the pre-intervention period, 65 UCC clinicians were recruited for the intervention and given access to the mobile application on their personal or hospital-provided mobile device. The use of interpreter services by enrolled participants and their use of the application were collected over a three-month period (intervention). After three months of application use, clinician participants were asked to complete a post-intervention feedback survey. Following the intervention period, participants were allowed to keep the application and their interpreter services use was tracked for an additional 2.5 months (post-intervention).
Recruitment and Participants
UCC clinicians were recruited through an informal study invitation via e-mail. All interested participants were contacted directly by a UCC clinician who was a co-investigator for the study. Participants were required to be UCC clinicians, defined as attending physicians, nurse practitioners, physician assistants, registered nurses, and patient care technicians. Participants were excluded if they: 1) did not work primarily in the UCC; 2) already used a language translation mobile application (with similar capabilities in providing pre-translated phrases or connecting to an OPI); or 3) had not been working in the UCC for two full months prior to study enrollment. Of the 65 participants who were interested, none met exclusion criteria. Informed consent was verbally obtained in-person.
Intervention
Providers were asked to download the application, were trained in a group on its functionality, and were asked to confirm the application was working. In the application, clinicians could choose from a library of pre-translated medical phrases and questions and/or use the application to call their institution’s OPI service directly (see Screenshots, Supplemental Digital Contents 1 and 2, displaying a list of phrases and a phrase being played in a different language, respectively; the option to call OPI is highlighted at the bottom), which provided another modality in addition to the landline telephone or Vocera. In this study, participants used a limited version, provided by commercial developers, of the application with a restricted list of 267 phrases, chosen by investigators, and were encouraged to use the application to call the OPI agency for comprehensive interactions with LEP patients. Phrases included introductions (e.g., “Hello, I’m your doctor today.”) and explanations (e.g., “I’m going to use this phone to get an interpreter.”) but excluded closed-ended questions which could be substituted for appropriate open-ended questions (e.g., “Does your chest hurt?” rather than “Can you describe your pain?”). Data on the mobile application use were collected weekly. Prior to the intervention, clinicians in the UCC had access to professional interpreters, in-person or telephone using the OPI via landline telephone or Vocera Badge. The Vocera Badge is a device worn primarily by nurses enabling instant, hands-free communication. The device is voice-controlled to direct calls to individuals or services using basic commands (e.g., “call interpreter”) regarding patient care needs. Interpreter access prior to the intervention was limited by a small number of both on-site, in-person interpreters and landline telephones in the UCC cubicles. Approximately, 70% in-patient as whole used OPI services compared to 30% in-person interpreters throughout the study time frame. The mobile application provided another means of accessing the same OPI used by the hospital. In an average week, 10% of patients who visit the UCC are LEP, suggesting a need for interpreter services. During the pre-intervention, intervention, and post-intervention, frequency of LEP patients each week remained on average at 9%, 10%, and 9%, respectively. A 2012 study found that 7% of patients who presented at another urban emergency department identified as LEP (12). The institution has quality assured patients’ reported preferred language with well-validated data on 92% of patients.
Measures
Use of the mobile application/interpreter services.
The information collected from the application included the frequency of phrases played and which languages were accessed. We collected data from the hospital’s interpreter services program, which tracks the use of in-person and telephone interpreters outside the use of the application. They reported the total number of calls to the OPI service (with and without the application) in the pre-, intervention, and post-intervention periods. We were able to distinguish whether calls to the OPI were made through the application, landline phone, or Vocera Badge.
Post-intervention survey
After the intervention, participants completed a feedback survey. The survey had 14 questions on perceived ease of use, efficiency, bidirectional communication improvement between clinician and LEP patients, satisfaction with using the application, and improvements to the application. Twelve questions were measured on a three-level ordinal scale (very much so, somewhat, and not at all) and 2 questions were open-ended.
Data Analysis
Descriptive analyses were performed on use of the pre-translated phrases: phrase played and phrase language; and on the clinicians’ post-study feedback survey. The percentage of calls by origin – mobile application, landline, and Vocera – during each intervention period was described. We hypothesized that calls made to the OPI via the mobile application would increase during the intervention period and remain elevated during the post-intervention period, compared to calls made via landline and Vocera Badge. To test this hypothesis, we compared the mean calls per week between the pre-intervention, intervention, and post-intervention periods. Significant differences in mean phone calls per week between study phases were tested using Wilcoxon Mann Whitney test assuming a type I error of 0.05 and were conducted using R statistical software version 3.1.1.
Results
Sixty-five physicians, physician assistants, and nurses participated in the study out of 89 UCC clinicians. A total of 918 phrases (897 during the intervention and 21 during the post-intervention) in 13 unique languages were used by participants via the mobile application. 82 unique phrases were accessed.
Table 1 lists the phrase languages, most frequently used phrases, and unique phrases played by clinicians in the application. Most of the phrases (53%) were in Spanish, 13% were in Russian, which is consistent with the commonly reported preferred languages at the institution, and less than 1% of phrases were in Japanese, Haitian Creole, or Portuguese. The most used phrase, “Hello, I am your nurse,” was accessed 109 times (12%) during the intervention and post-intervention periods. The phrase “I am going to do a physical exam” was used 64 (7%) times. Further phrases included actions being taken by clinicians, greetings, and follow-up (e.g., regarding pain). In comparing phrases versus OPI services accessed, 22% of the cases were providers who used the application to only access phrases, 29% used the phrases then transitioned to OPI services, and 49% used the application to only access OPI services.
Table 1.
Mobile Application Usage Characteristics
| Characteristic | |
|---|---|
| Count of phrases played per language, n (%)* | |
| Spanish | 485 (53%) |
| Chinese Mandarin | 40 (4%) |
| Chinese Cantonese | 60 (7%) |
| Arabic | 73 (8%) |
| Russian | 115 (13%) |
| Korean | 13 (1%) |
| Hindi | 41 (4%) |
| Japanese | 7 (0.8%) |
| Filipino | 12 (1%) |
| French | 41 (4%) |
| Haitian Creole | 7 (0.8%) |
| Vietnamese | 22 (2%) |
| Portuguese | 2 (0.2%) |
| Most common phrases played, n (%) | |
| Hello, I am your doctor | 68 (7%) |
| Hello, I am your nurse | 109 (12%) |
| I will use this device to communicate with you | 45 (5%) |
| Please point to what yours you or where it hurts | 44 (5%) |
| Are you feeling any pain | 37 (4%) |
| Do you have a list of medications you are taking | 53 (6%) |
| Please sit up | 55 (6%) |
| I am going to do a physical exam | 64 (7%) |
| We will now draw your labs | 31 (3%) |
| We are waiting for your results, and will let you know when they are available | 41 (4%) |
| Would you like me to call a translator | 6 (0.7%) |
Due to rounding, percentages may not add to 100%
During the intervention period, a mean of 12.8 (SD = 5.5) phone calls to the OPI service were made per week versus 4.3 (SD = 4.1) and 5.7 (SD = 4.7) calls per week for the pre- and post-intervention periods, respectively (Figure 1). During the intervention, there was a statistically significant increase of 8.5 calls per week on average compared to the pre-intervention period. There were no significant differences found in number of calls to the OPI when comparing the pre-intervention and post-intervention periods (Table 2). Two calls with excessive durations (50 and 161 minutes) were excluded as outliers.
Figure 1.
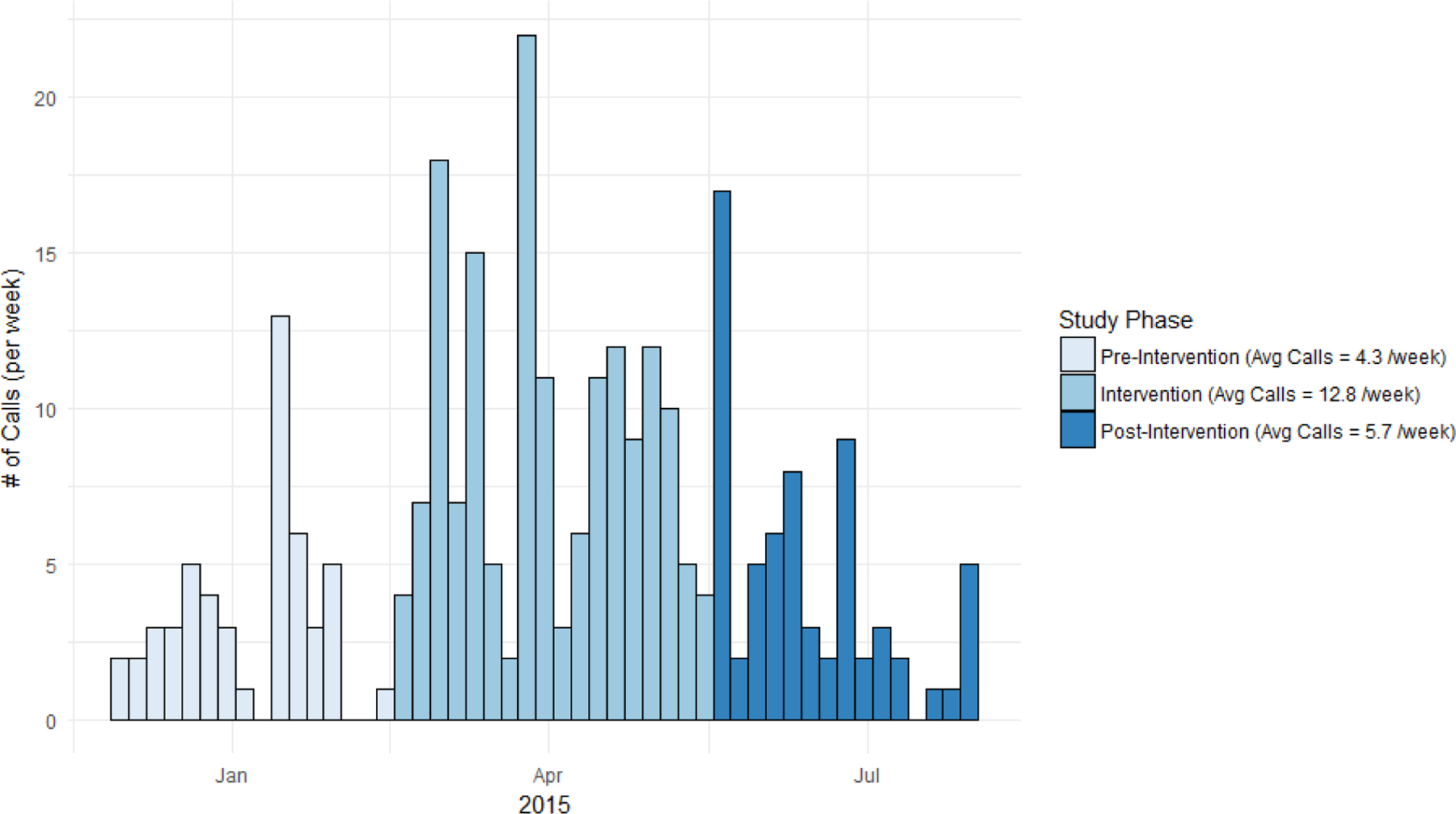
Number of Calls per Week by Study Phase
Table 2.
Mean Difference in Calls per Week
| Comparison | Call Differences Mean (SD) |
Wilcoxon Statistic |
p-value | |
|---|---|---|---|---|
| Intervention | Pre-Intervention | 8.5 (2.0) | 15.5 | 0.001 |
| Intervention | Post-Intervention | 7.1 (2.0) | 21.5 | 0.004 |
| Post-Intervention | Pre-Intervention | 1.4 (1.8) | 48.5 | 0.293 |
The proportion of calls to the OPI service compared to the volume of LEP patients was identified at each phase: 15%, 27%, and 18% at pre-intervention, intervention, and post-intervention, respectively. Origin of phone calls to the OPI service varied by the study phase (Figure 2). The frequency of phone calls to the OPI service more than tripled with 166 calls recorded during the intervention compared to 51 calls during the pre-intervention and 63 calls during the post-intervention period. During the pre-intervention period, 39 (75%) calls were placed to the OPI service using Vocera badges and 12 (25%) calls were made using landlines. In the intervention period 106 (65%) calls to the OPI service were placed using the mobile application, 48 (29%) via Vocera badges, and 9 (6%) using landlines. During the post-intervention period, 50 (76%) calls were placed using the application, 14 (21%) were made using Vocera badges, and 2 (3%) using landlines. The frequency of Vocera badge use remained almost equal from the pre-intervention to intervention period. Use of landline telephones to access the OPI steadily declined throughout the study period.
Figure 2.
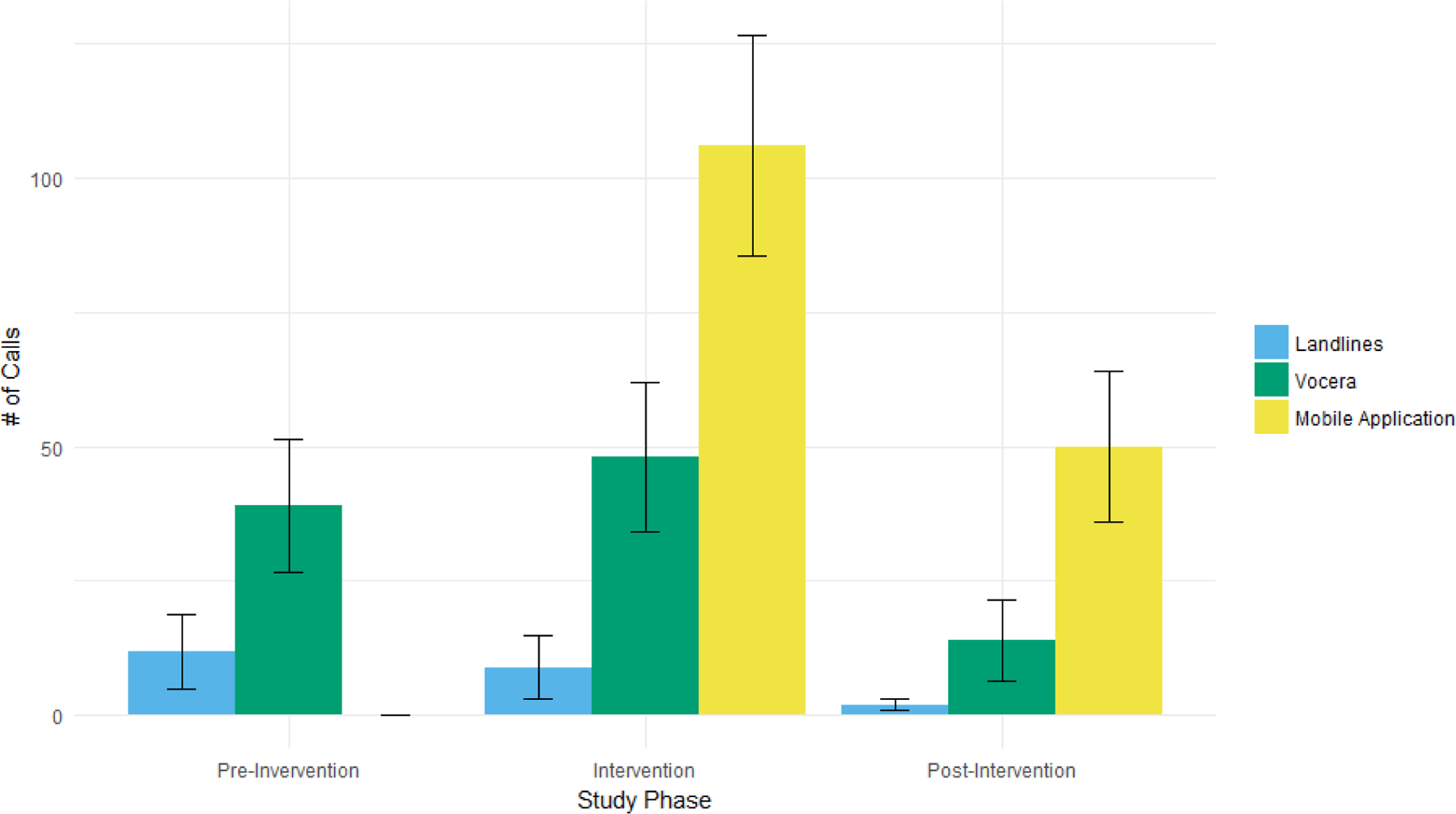
Number of Calls by Origin by Study Phase
Fifty participants (77%) completed the post-study feedback survey. The majority of respondents stated that the mobile application was very easy to use (82%), made calling interpreters easier (78%), and noted that it “very much” increased their likelihood of calling interpreter services (51%). Participants described the application as providing easier access with shorter waiting times to connect to an interpreter by telephone. Participants expressed interest in accessing more languages and phrases and using the application on a hospital-issued device, rather than their own device.
Discussion
Improving communication between LEP patients and clinicians is vital, regardless of the interpreting method. We tested the impact of using a mobile application on the use of telephone interpreters. The application increased the frequency and proportion of phone calls to the OPI service during the intervention period, which continued use during the post-intervention period. Most clinician participants were satisfied with the application, reporting that it was simple to use and efficient.
Our findings indicate that there is room to improve the communication between clinicians and LEP cancer patients in urgent care. The use of professional interpreter services is necessary for LEP cancer patients, particularly those at the end of life. Communication about end-of-life care is complicated in language-discordant encounters, including balancing word-for-word interpretation with cultural sensitivity (21). Relaying the complexity of information through an interpreter exacerbates this challenge (20, 32). Although we did not capture the content of the calls with interpreter services, discussions in oncology and palliative care can be difficult and include patients, families, and a multidisciplinary team of clinicians. Thus, the use of professional interpreters is essential to facilitate communication with LEP cancer patients and improve goals of care and symptom management discussions (22).
Our study suggests that the use of technology through mobile application tools has considerable potential to improve the frequency and quality of communication between providers and LEP patients. From a workflow perspective, clinicians are more likely to use interpreter services, including communication technology, if implemented at a systems-level with organizational commitment (33). Our institution’s workflow includes multiple modalities of interpreter access: OPI (landline, Vocera, or mobile application) and less-frequently used in-person or video services. Research shows that having multiple methods to access interpreter services can improve the feasibility and ease of language service delivery (34, 35). As smart devices become ubiquitous, the use of mobile applications as an optimal access point for services becomes more pertinent. In the ED/UCC, the immediacy and accessibility of interpreter services is critical because important, time-sensitive decisions are made by LEP patients and clinicians. Research has demonstrated that the use of interpreters in the ED significantly increases patients’ perceived knowledge of their diagnoses and treatments (36). In addition, language barriers increase use of ED resources (e.g., more frequent and expensive diagnostic testing; more frequent hospital admissions) (14, 37). One study noted that LEP patients who had professional interpreters had significantly fewer diagnostic tests, a shorter duration of stay in the ED, were more likely to attend follow-up visits and less likely to be readmitted to the ED (38). Thus, improving access to and use of professional interpreters for LEP patients may ultimately lower the cost of care (39).
Many cancer patients experience symptoms related to their underlying disease or side effects of treatment that require urgent hospital admission (40), but studies have shown that many of these visits could be avoided. One study showed that 23% of ED visits by patients with advanced cancer were potentially avoidable, suggesting that efforts to improve communication and support in the outpatient palliative care setting could eliminate unnecessary visits (41). Another study showed higher quality of life scores for advanced cancer patients who presented in an emergency setting and received palliative care services compared to those who received usual care (42). In a study of patients with advanced cancer, LEP patients were more likely to be unaware of their diagnosis, have worse symptom control, have mood disturbance, and die away from home compared to English-speaking patients (17). Professional interpreters may facilitate optimal palliative care for LEP cancer patients (43), and mobile applications can increase access to professional interpreters.
While Web- or mobile-based translation tools have the potential to improve communication between LEP patients and their clinicians (28), these applications have limitations. Before recent enhancements, Google Translate was often inaccurate in the medical setting (44). The prior translation method involved a statistical matching approach, and did not parse sentences grammatically (45). One study found that medical translations were frequently erroneous and nonsensical, and only 58% of translations were accurate (26). Recently, an artificial intelligence-rendered version of Google Translate was introduced, which handles language structure and pattern recognition in phrases (46). Although Google Translate and related technologies may be an improvement on those previously studied, it is unlikely that — at this point in time — they will be equipped to handle sensitive discussions, including end-of-life preferences, with the required nuance. Medical phrases translated via online or mobile translation tools have drawbacks in accuracy and context. Professional interpreters, either in-person or via telephone, provide superior accuracy, particularly in the setting of complex decision-making with LEP cancer patients. Further studies should investigate patient satisfaction with machine translation versus OPI, video interpreting, and/or in-person interpretation to elucidate LEP patient preferences for language assistance.
This study has limitations. This is a non-randomized, single-site study, with a small sample size. Thus, the findings have limited generalizability and are subject to confounding. Potential confounders to account for in future studies include: the amount of time clinicians spent with patients and whether an interpreter was used at each encounter, provider volume and scheduling, language concordance between LEP patients and providers, limited institutional tracking of providers who have confirmatory testing to provide bilingual care, content of calls, chief complaint, diagnosis, and provider demographics. Our study addressed some confounders, including call frequency, which limited provider recall bias on interpreter use. Second, our study data was collected in short periods, but our pre-post design allowed us to view temporal changes and the post-intervention analysis assessed the sustainability of the intervention. Most use of landlines and Vocera were replaced by continued mobile application use during the post-intervention period. A decrease in interpreter service use was seen in the post-intervention period, potentially due to technology acceptance waning after its introduction, which can be counteracted by cognitive factors (e.g., perceived ease of use) and social influences (subjective norm and image)(47). Furthermore, sustainability challenges exist in new health programs (48), yet research suggests that intervening at a national policy level (49), and factoring in organizational priority and benefits can yield continuity (48). Third, since the application uses closed-ended questions, its exclusive use prevented clinicians from obtaining in-depth information and could result in miscommunication. Our study allowed for providers to easily access an interpreter via the mobile application to assist in more complex conversations. Despite these limitations, our study suggests that there is a benefit to the mobile application, which led to increased access to interpreters for clinicians and to better communication for LEP cancer patients in an urgent care setting.
This research demonstrates that the use of a mobile application, as an additional workflow modality, increases the ease and frequency of use of telephone interpreters in a UCC setting. Facilities differ in their ability to access interpreter services and our study suggests mobile applications may help bridge this gap. Using multiple methods to access professional interpreter services, including mobile applications, telephone interpreters, and in-person interpreters, is consequential and can contribute to reducing disparities due to language barriers in cancer care settings. Increasing access to professional interpreters can improve the quality of communication between LEP patients and their clinicians and can increase patient and provider satisfaction. Health disparities due to language barriers are actionable and mobile applications are one potential solution to reducing these disparities.
Supplementary Material
1. Supplemental Digital Content 1. Screenshot that shows a list of phrases
2. Supplemental Digital Content 2. Screenshot showing a phrase being played in a different language
Footnotes
This was an unfunded study. One author has a potential conflict of interest as an employee with stock ownership of the mobile application we tested in our study, and is identified as such. Another author has stock ownership in Editas Medicine. The remaining authors have no conflicts of interest. The study design, data acquisition, data analysis, and manuscript preparation was completed entirely without bias. Dr. Diamond has maintained full control of the data and its presentation throughout this process.
References
- 1.U.S. Census Bureau. Language Spoken at Home: 2011–2015 American Community Survey 5-Year Estimates 2015. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml
- 2.Zong J, Batalova J. The limited English proficient population in the United States 2015. Available at: http://www.migrationpolicy.org/article/limited-english-proficient-population-united-states [Google Scholar]
- 3.Batalova J, Zong J. Language Diversity and English Proficiency in the United States 2016. Available at: https://www.migrationpolicy.org/article/language-diversity-and-english-proficiency-united-states [Google Scholar]
- 4.Office of Minority Health: U.S. Department of Health and Human Services. The National CLAS Standards 2016. Available at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=2&lvlid=53
- 5.VanderWielen LM, Enurah AS, Rho HY, et al. Medical interpreters: improvements to address access, equity, and quality of care for limited-English-proficient patients. Acad Med 2014;89:1324–1327 [DOI] [PubMed] [Google Scholar]
- 6.Diamond LC, Wilson-Stronks A, Jacobs EA. Do hospitals measure up to the national culturally and linguistically appropriate services standards? Medical care 2010;48:1080–1087 [DOI] [PubMed] [Google Scholar]
- 7.Chen AH, Youdelman MK, Brooks J. The Legal Framework for Language Access in Healthcare Settings: Title VI and Beyond. J Gen Intern Med 2007;22:362–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mann C. Increased Federal Matching Funds for Translation and Interpretation Services under Medicaid and CHIP Centers for Medicare & Medicaid Services; 2010 [Google Scholar]
- 9.Ku L, Flores G. Pay Now Or Pay Later: Providing Interpreter Services In Health Care. Health Affairs 2005;24:435–444 [DOI] [PubMed] [Google Scholar]
- 10.Diamond LC, Schenker Y, Curry L, et al. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med 2009;24:256–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Njeru JW, St Sauver JL, Jacobson DJ, et al. Emergency department and inpatient health care utilization among patients who require interpreter services. BMC Health Serv Res 2015;15:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ngai KM, Grudzen CR, Lee R, et al. The Association Between Limited English Proficiency and Unplanned Emergency Department Revisit Within 72 Hours. Ann Emerg Med 2016;68:213–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crane JA. Patient comprehension of doctor-patient communication on discharge from the emergency department. J Emerg Med 1997;15:1–7 [DOI] [PubMed] [Google Scholar]
- 14.Waxman MA, Levitt MA. Are diagnostic testing and admission rates higher in non-English-speaking versus English-speaking patients in the emergency department? Ann Emerg Med 2000;36:456–461 [DOI] [PubMed] [Google Scholar]
- 15.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a Risk Factor for Inadequate Emergency Department Analgesia. Jama-Journal of the American Medical Association 1993;269:1537–1539 [PubMed] [Google Scholar]
- 16.Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. J Gen Intern Med 2000;15:256–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan A, Woodruff RK. Comparison of palliative care needs of English- and non-English-speaking patients. Journal of palliative care 1999;15:26–30 [PubMed] [Google Scholar]
- 18.Butow PN, Sze M, Eisenbruch M, et al. Should culture affect practice? A comparison of prognostic discussions in consultations with immigrant versus native-born cancer patients. Patient Educ Couns 2013;92:246–252 [DOI] [PubMed] [Google Scholar]
- 19.Davies B, Contro N, Larson J, et al. Culturally-sensitive information-sharing in pediatric palliative care. Pediatrics 2010;125:e859–865 [DOI] [PubMed] [Google Scholar]
- 20.Butow PN, Lobb E, Jefford M, et al. A bridge between cultures: interpreters’ perspectives of consultations with migrant oncology patients. Support Care Cancer 2012;20:235–244 [DOI] [PubMed] [Google Scholar]
- 21.Norris WM, Wenrich MD, Nielsen EL, et al. Communication about end-of-life care between language-discordant patients and clinicians: insights from medical interpreters. Journal of palliative medicine 2005;8:1016–1024 [DOI] [PubMed] [Google Scholar]
- 22.Silva MD, Genoff M, Zaballa A, et al. Interpreting at the End of Life: A Systematic Review of the Impact of Interpreters on the Delivery of Palliative Care Services to Cancer Patients With Limited English Proficiency. J Pain Symptom Manage 2016;51:569–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacobs EA, Leos GS, Rathouz PJ, et al. Shared networks of interpreter services, at relatively low cost, can help providers serve patients with limited english skills. Health Aff (Millwood) 2011;30:1930–1938 [DOI] [PubMed] [Google Scholar]
- 24.Locatis C, Williamson D, Sterrett J, et al. Video medical interpretation over 3G cellular networks: a feasibility study. Telemed J E Health 2011;17:809–813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sciarra AM, Batigalia F, Oliveira MA. Technological Devices Improving System of Translating Languages: What About their Usefulness on the Applicability in Medicine and Health Sciences? Braz J Cardiovasc Surg 2015;30:664–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patil S, Davies P. Use of Google Translate in medical communication: evaluation of accuracy. BMJ 2014;349:g7392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hampshire S, Salvia CP. Translation and the Internet: evaluating the quality of free online machine translators. Quaderns: revista de traducció 2010:197–209 [Google Scholar]
- 28.Kaliyadan F, Gopinathan Pillai S. The use of Google language tools as an interpretation aid in cross-cultural doctor_patient interaction: a pilot study. Journal of Innovation in Health Informatics 2010;18:141–143 [DOI] [PubMed] [Google Scholar]
- 29.Chang DT, Thyer IA, Hayne D, et al. Using mobile technology to overcome language barriers in medicine. Ann R Coll Surg Engl 2014;96:e23–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Research AIf. Executive Summary: A Patient-Centered Guide to Implementing Language Access Services in Healthcare Organizations 2005. Available at: https://minorityhealth.hhs.gov/assets/pdf/checked/hc-lsig-executivesummary.pdf
- 31.Chan YF, Alagappan K, Rella J, et al. Interpreter services in emergency medicine. J Emerg Med 2010;38:133–139 [DOI] [PubMed] [Google Scholar]
- 32.Huang X, Butow P, Meiser B, et al. Attitudes and information needs of Chinese migrant cancer patients and their relatives. Australian and New Zealand journal of medicine 1999;29:207–213 [DOI] [PubMed] [Google Scholar]
- 33.Baurer D, Yonek JC, Cohen AB, et al. System-level factors affecting clinicians’ perceptions and use of interpreter services in California public hospitals. Journal of immigrant and minority health 2014;16:211–217 [DOI] [PubMed] [Google Scholar]
- 34.Burkle CM, Anderson KA, Xiong Y, et al. Assessment of the efficiency of language interpreter services in a busy surgical and procedural practice. BMC Health Serv Res 2017;17:456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Masland MC, Lou C, Snowden L. Use of communication technologies to cost-effectively increase the availability of interpretation services in healthcare settings. Telemed J E Health 2010;16:739–745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baker DW, Parker RM, Williams MV, et al. Use and effectiveness of interpreters in an emergency department. JAMA 1996;275:783–788 [PubMed] [Google Scholar]
- 37.Hampers LC, McNulty JE. Professional interpreters and bilingual physicians in a pediatric emergency department: effect on resource utilization. Archives of pediatrics & adolescent medicine 2002;156:1108–1113 [DOI] [PubMed] [Google Scholar]
- 38.Bernstein J, Bernstein E, Dave A, et al. Trained medical interpreters in the emergency department: effects on services, subsequent charges, and follow-up. Journal of immigrant health 2002;4:171–176 [DOI] [PubMed] [Google Scholar]
- 39.Jacobs EA, Shepard DS, Suaya JA, et al. Overcoming language barriers in health care: costs and benefits of interpreter services. American journal of public health 2004;94:866–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vandyk AD, Harrison MB, Macartney G, et al. Emergency department visits for symptoms experienced by oncology patients: a systematic review. Support Care Cancer 2012;20:1589–1599 [DOI] [PubMed] [Google Scholar]
- 41.Delgado-Guay MO, Kim YJ, Shin SH, et al. Avoidable and unavoidable visits to the emergency department among patients with advanced cancer receiving outpatient palliative care. J Pain Symptom Manage 2015;49:497–504 [DOI] [PubMed] [Google Scholar]
- 42.Grudzen CR, Richardson LD, Johnson PN, et al. Emergency Department-Initiated Palliative Care in Advanced Cancer: A Randomized Clinical Trial. JAMA Oncol 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith AK, Sudore RL, Perez-Stable EJ. Palliative care for Latino patients and their families: whenever we prayed, she wept. JAMA 2009;301:1047–1057, E1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khanna RR, Karliner LS, Eck M, et al. Performance of an online translation tool when applied to patient educational material. J Hosp Med 2011;6:519–525 [DOI] [PubMed] [Google Scholar]
- 45.Gomes L. Google Translate Tangles With Computer Learning 2010. Available at: https://www.forbes.com/forbes/2010/0809/technology-computer-learning-google-translate.html
- 46.Lewis-Kraus G. The great AI awakening. The New York Times Magazine 2016 [Google Scholar]
- 47.Venkatesh V, Davis FD. A theoretical extension of the Technology Acceptance Model: Four longitudinal field studies. Management Science 2000;46:186–204 [Google Scholar]
- 48.Scheirer MA. Is sustainability possible? A review and commentary on empirical studies of program sustainability. American Journal of Evaluation 2005;26:320–347 [Google Scholar]
- 49.Cutler DM. Behavioral health interventions: what works and why. Critical perspectives on racial and ethnic differences in health in late life 2004:643–674 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1. Supplemental Digital Content 1. Screenshot that shows a list of phrases
2. Supplemental Digital Content 2. Screenshot showing a phrase being played in a different language


