Abstract
Background:
We evaluated the effects of surgeon characteristics such as surgeon experience on differences in opioid prescribing after surgery.
Methods:
We evaluated a 20% national sample of Medicare beneficiaries ≥65 years old who underwent 15 different types of surgery to identify surgeon characteristics associated with opioid prescription size filled within seven days of discharge using a multi-level linear model.
Results:
174,141 patients and 13,828 surgeons met inclusion criteria. 53.8% of patients filled an opioid prescription within seven days postoperatively. The amount of opioids prescribed after surgery was highest for patients whose surgeons were early in practice (i.e. 0–7 years in practice). Surgeon credentials, type of surgery, and geographic region were associated with differing sizes of opioid fills postoperatively.
Conclusions:
Surgeon characteristics such as cumulative years of practice contribute to differences in prescribing behavior after surgery. These findings can help develop strategic interventions to enhance opioid stewardship.
Keywords: Opioid analgesics, opioids, surgery, prescribing, over, prescription
Introduction
Opioid medications are commonly prescribed after surgery, and for many opioid naïve patients, surgery may represent their first exposure to these effective, yet potentially harmful medications.(1) Across all different specialties, about 5–10% of opioid naïve patients meet criteria for new persistent opioid use after surgery.(2–4) Additionally, higher amounts of opioids prescribed in the perioperative period is strongly associated to prolonged opioid use after surgery.(2, 3) Although the etiology of the opioid epidemic in the United States is multifactorial and complex, overprescribing by physicians and other providers have contributed to the current public health problem and identifying these factors can help reduce the morbidity and mortality attributable to prescription opioids.
Patient factors associated with postoperative opioid analgesic fills after surgery have previously been identified.(1) Several studies have demonstrated that patient characteristics such as younger age, mental health disorders such as anxiety and substance abuse, and sociodemographic factors are associated with higher opioid prescription fills and new persistent opioid use after surgery.(1, 3) Beyond the associated patient level characteristics, less is known about prescriber level factors that may contribute to higher amounts of opioids being prescribed after surgery.
We sought to examine the relationship between surgeon level factors, such as years in practice, and the amount of opioid medications filled by patients after surgery. By leveraging national representative datasets, we tested our hypothesis that surgeon characteristics contributed to higher amounts of opioids filled after surgery. These insights can help develop prescriber-targeted interventions that can facilitate judicious opioid prescribing after surgery and ensure safe surgical care.
Methods
Data Sources and Study Population
Using a 20% Medicare national sample, we identified beneficiaries ≥65 years old who underwent elective surgery between January 1, 2009 through November 30, 2016 with continuous enrollment in Medicare Parts A, B, and D for at least 12 months prior to and 30 days after discharge. We examined the following surgical procedures: varicose vein removal, laparoscopic appendectomy, hemorrhoidectomy, laparoscopic cholecystectomy, transurethral prostate surgery, thyroidectomy, parathyroidectomy, carpal tunnel release, incisional hernia repair, anti-reflux surgery, total hip arthroplasty, and total knee arthroplasty. Procedures were identified using Current Procedural Terminology Fourth Edition (CPT-4) codes (Appendix Table 1).
We matched cases with providers using the American Medical Association (AMA) Physician Master file and any case without a matched record in the AMA Physician Master file was excluded. Any patient who did not have continuous enrollment in Medicare Parts A, B, and D at least 12 months prior to and 30 days after their surgical discharge date and who underwent a subsequent surgery within 30 days of their discharge date, identified by having another CPT-4 anesthesia code (Appendix Table 2), was also excluded. We examined opioid naïve patients, excluding individuals who filled one or more opioid prescriptions within 12 months prior to their admission date. Patients cared for by surgeons performing five or less procedures in the study population were excluded. We also excluded patients whose hospital stay was longer than 30 days or patients who were not discharged home. This study was deemed exempt by the Human Research Protection Office at the University of Michigan.
Outcomes of Interest
The primary outcome was the initial opioid prescription size filled within seven days of discharge. Medicare Part D pharmacy claims was used to obtain information on the opioid fills, and were converted to morphine milligram equivalent (OME) units by using a morphine equivalent conversion factor per milligram as previously published.(5) Prescription size was reported as total OMEs.
Surgeon factors
Surgeon characteristics were identified from data available in the AMA Physician Master File. Attributes included experience, which was defined by the number of years since medical school graduation (≤7, 8–15, 16–25, 26–35, >35 years), medical school training in the US or not, sex, geographic region based on surgeon’s mail address, credentials (i.e., MD versus DO), and specialty (i.e., General Surgery, Obstetrics/Gynecology, Orthopedics, Plastic Surgery, Others).
Statistical Analysis
Surgeon characteristics were analyzed via descriptive statistics. We used a multi-level linear model with natural log transformed prescription size as the outcome of interest and surgeon experience as the covariate of interest, while adjusting for patient and surgeon factors. The estimated coefficient was then back-transformed and interpreted as a multiplicative factor. Collinearity between covariates was assessed to determine the final list of variables in the model while controlling for clustering of patients within surgeons. Adjusted prescription size (in OME) by surgeon experience was estimated based on the model. Statistical analyses were performed using Stata version 15.1 (Stata-Corp) and statistical significance was set at two-tailed p< 0.05.
Results
Surgeon characteristics
Characteristics of surgeons caring for patients during the study period are identified in Table 1. In total, there were 13,828 surgeons who cared for all patients in the study population--including patients who did (n= 93,610; 53.8%) or did not (n= 80,531; 46.2%) fill an opioid prescription within the first seven days postoperatively. The average length of time from surgeon’s completion of undergraduate medical education to the study period was 25 years. The distribution of surgeon experience was as follows: ≤7 years: 1.3%; 8–15 years: 17.7%; 16–25 years: 33.4%; 26–35 years: 32.2%; >35 years: 15.4%. The majority of surgeons graduated from medical school in the US (88.6%), were male (93.7%), and had an allopathic medical degree (i.e., MD versus DO) (95.3%). The two most common types of surgeons in the dataset included General Surgeons (49.7%) and Orthopedic Surgeons (36.2%).
Table 1.
Surgeon characteristics
| All (n=13,828) | ||
|---|---|---|
| No. Surgeon | % Total | |
| Years after Graduated from Medical School | ||
| Mean (Std Dev) | 25.0 (9.7) | |
| ≤7 | 184 | 1.3% |
| 8 – 15 | 2,443 | 17.7% |
| 16 – 25 | 4,621 | 33.4% |
| 26 – 35 | 4,455 | 32.2% |
| >35 | 2,125 | 15.4% |
| Foreign Trained | ||
| Yes | 1,574 | 11.4% |
| No | 12,254 | 88.6% |
| Sex | ||
| Male | 12,961 | 93.7% |
| Female | 867 | 6.3% |
| Geographic Region (based on prescriber’s mail address) | ||
| East North Central | 2,415 | 17.5% |
| East South Central | 975 | 7.1% |
| Middle Atlantic | 1,834 | 13.3% |
| Mountain | 871 | 6.3% |
| New England | 852 | 6.2% |
| Pacific | 1,399 | 10.1% |
| South Atlantic | 2,691 | 19.5% |
| West North Central | 1,366 | 9.9% |
| West South Central | 1,412 | 10.2% |
| Unknown | 13 | 0.1% |
| MD or DO | ||
| MD | 13,173 | 95.3% |
| DO | 655 | 4.7% |
| Specialty | ||
| General Surgery | 6,874 | 49.7% |
| OB/GYN | 505 | 3.7% |
| Orthopaedics | 5,008 | 36.2% |
| Plastic Surgery | 457 | 3.3% |
| Others* | 984 | 7.1% |
including Neurological Surgery, Pediatric Surgery, Thoracic Surgery, Urological Surgery, Vascular Surgery, Head & Neck Surgery, Otolaryngology
Patient characteristics
Patient characteristics are presented in the Appendix. Of the 174,141 patients who met inclusion criteria, 93,610 patients (53.8%) filled an opioid prescription within seven days postoperatively and were cared for by 12,803 surgeons. More than one-third of patients (36.5%) belonged to the youngest cohort, 65–69 years old. Most patients were White (89.7%), female (63.6%), and resided in urban areas (62.4%). Additionally, most patients had at least one comorbid condition (none: 26.8%; mild 1–2: 38.7%; moderate 3–4: 19.7%; severe ≥5: 14.8%). The most common mental health disorders in our cohort were mood disorder (14.2%), anxiety (12.1%), and alcohol or substance abuse disorder (2.3%). About one-fifth of the cohort had a history of tobacco use (21.4%). Additionally, 5.6% of patients filled a benzodiazepine, sedative, hypnotic or anxiolytic within 30 days before their surgery date.
Characteristics associated with greater amounts of opioids filled after surgery
Surgeon
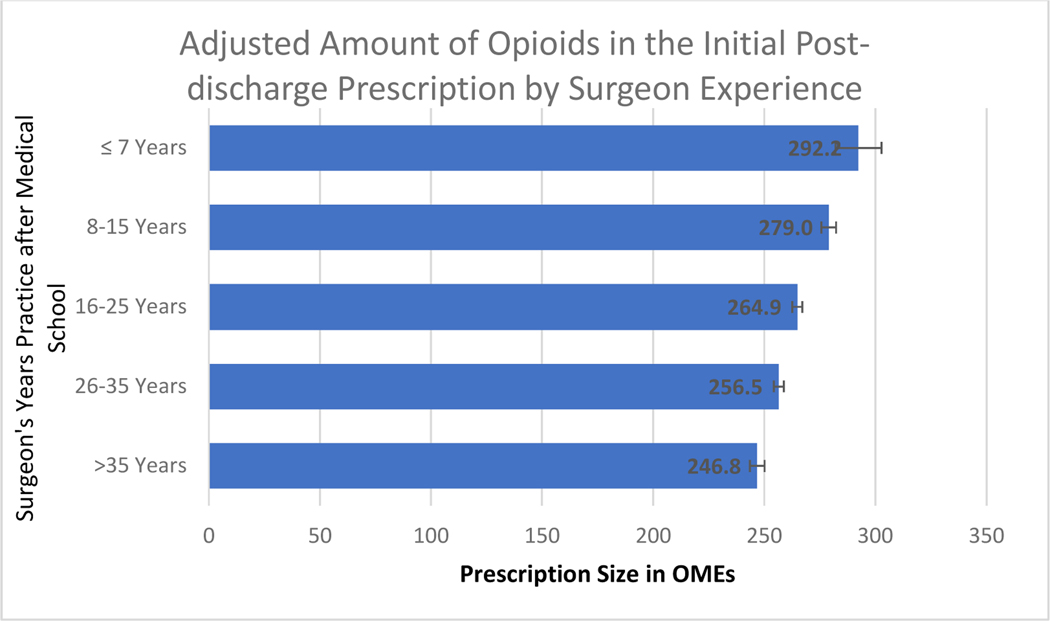
Results from our multi-level linear model are presented in Table 2. After controlling for patient and surgeon characteristics, and for procedure type, years of practice since medical school was significantly associated with initial opioid prescription size after surgery (Figure 1). The adjusted amount of opioids initially prescribed after surgery was highest for patients whose surgeons were early in practice (0–7 years: OME 292.2, 95% CI 282.0–302.8), with decreasing amounts of opioids filled among patients with surgeons who had been in practice longer (8–15 years: total OME 279.0, 95% CI 279.0– 275.7; 16–25 years: total OME 264.9, 95% CI 262.6–267.1; 26–35 years: total OME 256.5, 95% CI 254.2–258.7; >35 years, total OME 246.8, 95% CI 243.5–250.2).
Table 2.
Factors associated with amount of initial opioid prescriptions filled within 7 days of discharge
| Multiplicative Effect on the Size of Initial Post-discharge Opioid Prescription | ||||
|---|---|---|---|---|
| Multiplicative Factor | 95% CI LL | 95% CI UL | P Value | |
| Surgeon Characteristics | ||||
| Years after Medical School (Ref: 16 – 25 Years) | ||||
| 0–7 Years | 1.10 | 1.06 | 1.14 | <0.001 |
| 8–15 Years | 1.05 | 1.04 | 1.07 | <0.001 |
| 26–35 Years | 0.97 | 0.96 | 0.98 | <0.001 |
| >35 Years | 0.93 | 0.92 | 0.95 | <0.001 |
| Foreign Trained (Ref: U.S. Trained) | 1.01 | 0.99 | 1.03 | 0.311 |
| Other Surgeon Characteristics | ||||
| Surgeon - Female (Ref: Male) | 0.99 | 0.97 | 1.02 | 0.696 |
| Surgeon’s Credential: DO (Ref: MD) | 1.03 | 1.00 | 1.06 | 0.031 |
| Surgery (Ref: Laparoscopic Cholecystectomy) | ||||
| Varicose Vein Removal | 0.84 | 0.73 | 0.95 | 0.007 |
| Laparoscopic Appendectomy | 0.96 | 0.94 | 0.98 | <0.001 |
| Hemorrhoidectomy | 1.18 | 1.15 | 1.20 | <0.001 |
| Transurethral Prostate Surgery | 0.79 | 0.76 | 0.82 | <0.001 |
| Thyroidectomy | 0.93 | 0.90 | 0.96 | <0.001 |
| Parathyroidectomy | 0.86 | 0.83 | 0.89 | <0.001 |
| Carpal Tunnel Surgery | 1.02 | 1.01 | 1.04 | 0.010 |
| Bariatric Surgery | 1.04 | 0.98 | 1.09 | 0.185 |
| Colectomy | 1.10 | 1.08 | 1.12 | <0.001 |
| Incisional Hernia Repair | 1.08 | 1.07 | 1.09 | <0.001 |
| Anti-Reflux Surgery | 0.99 | 0.97 | 1.02 | 0.559 |
| Hysterectomy | 1.20 | 1.16 | 1.24 | <0.001 |
| Total Hip Arthroplasty | 2.19 | 2.16 | 2.23 | <0.001 |
| Total Knee Arthroplasty | 2.38 | 2.34 | 2.41 | <0.001 |
| Surgeon’s Location: Geographic Region (Ref: East North Central) | ||||
| East South Central | 1.02 | 0.99 | 1.05 | 0.115 |
| Middle Atlantic | 1.02 | 0.99 | 1.04 | 0.183 |
| Mountain | 1.08 | 1.05 | 1.11 | <0.001 |
| New England | 1.01 | 0.98 | 1.04 | 0.592 |
| Pacific | 1.10 | 1.07 | 1.13 | <0.001 |
| South Atlantic | 1.08 | 1.05 | 1.10 | <0.001 |
| West North Central | 0.96 | 0.94 | 0.99 | 0.003 |
| West South Central | 1.06 | 1.03 | 1.08 | <0.001 |
| Unknown | 0.73 | 0.58 | 0.90 | 0.004 |
Model also adjusted for patient characteristics including race, age, sex, rural vs. urban, Medicaid eligibility, filling of benzodiazepine, sedatives, hypnotics or anxiolytics within 30 days of surgery, Charlson Comorbidity Index, mental health disorders, pain disorders, and year of surgery.
Figure 1.
Adjusted amount of opioids in total OME in the initial post-discharge prescription by surgeon experience.
OME, oral morphine equivalent
Additionally, other surgeon characteristics were associated with greater amounts of opioids prescribed within the first seven days of surgery, such as surgeon credentials (ref= MD; DO: 1.03, 95% CI 1.00–1.06), type of surgery (ref= laparoscopic cholecystectomy; incisional hernia repair: 1.07, 95% CI 1.07–1.09; hysterectomy: 1.20, 95% CI 1.16–1.24; total hip arthroplasty: 2.18, 95% CI 2.16–2.23; total knee arthroplasty: 2.38, 95% CI 2.34–2.41) and certain surgeon locations (ref= East North Central; Pacific: 1.10, 95% CI 1.07–1.13; South Atlantic: 1.08, 95% CI 1.05–1.10; Mountain: 1.08, 95% CI 1.05–1.11, West South Central: 1.06, 95% CI 1.03–1.07). There were no associations found based on location of medical training (i.e., US versus foreign-trained) or sex of surgeon.
Patient
Patient characteristics associated with greater amounts of opioids filled after surgery were younger age (65–69 years) (ref= 65–69 years; 70–74 years: 0.97, 95% CI 0.96–0.97; 75–79 years: 0.93, 95% CI 0.93–0.94; 80–84 years: 0.89, 95% CI 0.88–0.90; ≥85 years: 0.85, 95% CI 0.84–0.86), male sex, history of tobacco use (1.02, 95% CI 1.00–1.02), and arthritis (1.06, 95% CI 1.05–1.08).
Discussion
Identifying the factors that are associated with post-operative opioid prescribing is important to design strategies to promote best practices in opioid stewardship. In addition to patient-level factors such as age, sex, comorbid conditions, and presence of mental health disorders, that have been previously defined,(1) surgeon-level factors also contribute to opioid prescribing habits after surgery. Our findings suggest differences in prescribing behavior based on the surgeon’s cumulative years of practice, and that surgeons in practice longer prescribe less than those earlier in practice. Other surgeon characteristics such as surgeon credentials, type of surgery, and location were also found to be associated with higher amounts of opioids prescribed after surgery. It is possible differences observed between surgery types reflect perception of the amount of pain associated with the procedure. Taken together, these insights can be used to inform policy and other strategic interventions to improve the safety of opioid prescribing after surgical care.
To understand why these factors may exist, we must first recognize that there have been major paradigm shifts in pain recognition and management in the United States.(7) Opioid medication for treatment of pain initially emerged for use in cancer pain, and subsequently, started to be used as treatment for other types of discomfort. Pain became a dominant influence in medicine through different movements. For example, in 1996, the American Pain Society raised awareness of the recognition of pain through its “Pain, The Fifth Vital Sign” campaign, prompting regulatory measures mandating pain assessments and treatments, and later used as quality metrics.(7, 8) In tandem, aggressive, and often misguided, pharmaceutical marketing strategies touting the safety of opioids prompted an increase in opioid prescribing.(9) Now, decades later, opioid-related morbidity and mortality have risen drastically in conjunction with excessive opioid prescribing for pain management.(8)
Our findings suggest that there are differences in prescribing behavior based on the surgeon’s cumulative years of practice. Interestingly, surgeons who began practicing during the time where pain was regarded as a fifth vital sign or afterwards prescribed higher amounts of opioids than surgeons who had already been in practice for several decades, which could be reflective of the influence of these campaigns. It is plausible to argue that more experienced surgeons, who cared for patients before the introduction of opioids for postoperative pain management, were less influenced by the pain and opioid campaigns, and better appreciate the ability to treat acute postoperative pain with non-opioid analgesic medications than their less experienced cohorts.
Another possibility is that less experienced surgeons such as residents and fellows may be less aware of the ability to treat postoperative pain with non-opioid analgesics due to a variety of reasons such as inadequate education on the topic,(10) lack of continuity of care contributing to a disconnect from a patient’s postoperative recovery,(11) and lack of prescribing guidelines.(12, 13) A recent statewide analysis in Michigan demonstrated that prescriptions originating from teaching hospitals were significantly larger than those from non-teaching hospitals.(11) The authors speculate that trainee involvement is likely a contributing factor to this as resident surgeons tend to prescribe greater total amounts of opioids compared to attending surgeons.(14) Although it is possible that trainees in our cohort were responsible for the larger amounts of opioids prescribed, it is also worth noting that similar analyses in other fields such as Emergency Medicine have not shown a difference in opioid prescribing between trainees and attending physicians.(15) Additionally, preliminary results from the Emergency Medicine literature also suggest that patients dispositioned by attending physicians were more likely to receive an opioid prescription compared to patients dispositioned by resident physicians.(16) These observations between Surgery and Emergency Medicine could be attributable to the differences in training structures and delegated responsibilities of trainees and attendings.
Despite these strengths, there are limitations that remain. First, as this was an analysis of claims data, we are only able to discuss the amounts of opioids that were filled by patients and cannot comment on what was consumed by the patient or prescriptions that were prescribed by surgeons and not filled by their patients. Second, these data are in advance of opioid prescribing guidelines for surgery and prior to the declaration of the opioid epidemic as a national emergency in 2017, after this study period. Given the introduction of prescribing recommendations for surgery in 2016 and increasing awareness of opioid misuse by the general public,(17) we hypothesize that less variability in opioid prescribing will be observed between surgeons with differing levels of experience compared to what our analysis demonstrated. Third, this analysis is limited to the 15 types of surgical procedures evaluated. Further investigations including other procedures spanning different surgical subspecialties that were not included in this study are warranted. Fourth, our analysis demonstrated a difference in opioid prescribing based on surgeon credentials (i.e. MD vs. DO). We felt it relevant to include this data as the degree type may reflect differences in opioid education and other prescribing habits first introduced to learners in their medical school curricula. However, it is worth noting that these findings preceded the merging of allopathic and osteopathic graduate medical education training programs. Fifth, we lacked details of treatments for other concomitant painful conditions (e.g. arthritis, back pain, neck pain, other pain conditions) during the follow-up period. Sixth, given the data available in the AMA Physician Master File, we were unable to determine the interaction between level of provider (i.e., resident surgeon versus attending surgeon) on opioid prescribing habits, which could have explained the findings. Finally, this cohort consisted of Medicare beneficiaries ≥65 years old, and may not be generalizable to younger cohorts.
Conclusions
While this data may not reflect the experiences of younger cohorts, it is worth noting that individuals ≥65 years old not only represent the fastest growing segment of the US population, but also have the greatest interaction with the US healthcare system. This nationwide analysis of older patients undergoing 15 different surgical procedures suggest that surgeon characteristics including experience (i.e., years since graduation of medical school), degree type (i.e., DO versus MD), procedure type and geographic location are associated with the size of the initial opioid prescription filled within the first week of surgery. With increasing awareness of the opioid epidemic and efforts to curb the public health crisis in the past several years, recognizing surgeon characteristics such as years in practice that are associated with variability in opioid prescribing will help target educational efforts and ensure that surgeons prescribe opioids judiciously and deliver the safest surgical care possible.
Supplementary Material
Study Highlights.
Surgeons early in practice prescribed more opioids for patients postoperatively.
Surgeon credentials (DO vs. MD) were associated with greater opioids prescribed.
Surgeons across all career levels should prescribe opioids judiciously.
Acknowledgments
Funding
This study was supported by the National Institutes of Health (NIH) National Institute on Drug Abuse (NIDA) (R01DA042859) awarded to J.F.W. and C.M.B. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the NIH. These funding sources had no role in study design, data collection or analysis, interpretation of data, writing the report, or the decision to submit the findings for publication. The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
Dr. Santosa reported no biomedical financial interests or potential conflicts of interest. Dr. Wang reported no biomedical financial interests or potential conflicts of interest. Dr. Hu reported no biomedical financial interests or potential conflicts of interest. Dr. Brummett reported no biomedical financial interests or potential conflicts of interest. Dr. Englesbe reported no biomedical financial interests or potential conflicts of interest. Dr. Waljee reported no biomedical financial interests or potential conflicts of interest.
References
- 1.Larach DB, Waljee JF, Hu HM, et al. Patterns of Initial Opioid Prescribing to Opioid-Naive Patients. Annals of surgery. 2020. February;271(2):290–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santosa KB, Hu HM, Brummett CM, et al. New persistent opioid use among older patients following surgery: A Medicare claims analysis. Surgery. 2020. April;167(4):732–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA surgery. 2017. June 21;152(6):e170504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson SP, Chung KC, Zhong L, et al. Risk of Prolonged Opioid Use Among Opioid-Naive Patients Following Common Hand Surgery Procedures. The Journal of hand surgery. 2016. October;41(10):947–57.e3. [DOI] [PubMed] [Google Scholar]
- 5.Waljee JF, Zhong L, Hou H, et al. The Use of Opioid Analgesics following Common Upper Extremity Surgical Procedures: A National, Population-Based Study. Plastic and reconstructive surgery. 2016. February;137(2):355e–64e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.USDA Rural-Urban Continuum Codes. [cited 2019 October 19, 2019]; Available from: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.
- 7.Tompkins DA, Hobelmann JG, Compton P. Providing chronic pain management in the “Fifth Vital Sign” Era: Historical and treatment perspectives on a modern-day medical dilemma. Drug and alcohol dependence. 2017. April 1;173 Suppl 1:S11–s21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levy N, Sturgess J, Mills P. “Pain as the fifth vital sign” and dependence on the “numerical pain scale” is being abandoned in the US: Why? Br J Anaesth. 2018. March;120(3):435–8. [DOI] [PubMed] [Google Scholar]
- 9.Haffajee RL, Mello MM. Drug Companies’ Liability for the Opioid Epidemic. New England Journal of Medicine. 2017;377(24):2301–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mezei L, Murinson BB. Pain Education in North American Medical Schools. The Journal of Pain. 2011 2011/December/01/;12(12):1199–208. [DOI] [PubMed] [Google Scholar]
- 11.Cron DC, Hwang C, Hu HM, et al. A statewide comparison of opioid prescribing in teaching versus nonteaching hospitals. Surgery. 2019. April;165(4):825–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiu AS, Freedman-Weiss MR, Jean RA, et al. No refills: The durable impact of a multifaceted effort by surgical trainees to minimize the prescription of postoperative opioids. Surgery. 2019. November;166(5):758–63. [DOI] [PubMed] [Google Scholar]
- 13.Chiu AS, Healy JM, DeWane MP, et al. Trainees as Agents of Change in the Opioid Epidemic: Optimizing the Opioid Prescription Practices of Surgical Residents. Journal of surgical education. 2018. Jan-Feb;75(1):65–71. [DOI] [PubMed] [Google Scholar]
- 14.Blay E, Nooromid MJ, Bilimoria KY, et al. Variation in post-discharge opioid prescriptions among members of a surgical team. The American Journal of Surgery. 2018 2018/July/01/;216(1):25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mazer-Amirshahi M, Mullins PM, Sun C, et al. Trends in Opioid Analgesic Use in Encounters Involving Physician Trainees in U.S. Emergency Departments. Pain medicine (Malden, Mass). 2016. December;17(12):2389–96. [DOI] [PubMed] [Google Scholar]
- 16.Androski CP Jr., Michael SS, Babu KM, Reznek MA. 255 Differences in Opioid Prescribing Patterns Among Emergency Medicine Independent Providers and Trainees. Annals of Emergency Medicine. 2016;68(4):S99. [Google Scholar]
- 17.Overton HN, Hanna MN, Bruhn WE, et al. Opioid-Prescribing Guidelines for Common Surgical Procedures: An Expert Panel Consensus. Journal of the American College of Surgeons. 2018;227(4):411–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.