Abstract
Objectives:
To compare tooth movement achieved, time required for alignment, root resorption, and alveolar bone thickness changes during initial dental alignment between groups treated with 0.012-inch preformed heat-activated or customized nickel titanium (NiTi) archwires.
Materials and Methods:
Thirty-two subjects (mean age 19.8 ± 1.7 years) with severe crowding of maxillary anterior teeth had premolar extractions and were randomly allocated into control and experimental groups receiving preformed heat-activated and customized NiTi archwires, respectively. Limited field of view cone-beam computed tomographies were taken initially (T0) and three months after final alignment (TF) to evaluate bone changes. Digital model analysis assessed tooth movement at monthly intervals. Time to achieve alignment was assessed in months. Wilcoxon signed-rank tests and Mann–Whitney U-tests were used to compare changes within and between groups, as appropriate.
Results:
Central incisor tooth movement was significantly different (all P ≤ .003) between groups at all time points. TF-T0 showed labial movement (0.75 ± 1.42 mm) in the control group and palatal movement (−0.96 ± 0.41 mm) in the experimental group. The experimental compared to control group showed significantly more canine distal movement (0.60 ± 0.28 mm; P ≤ .049), less labial bone thickness changes (P ≤ .004), less root resorption of the central and lateral incisors (P ≤ .007), and a longer time to achieve alignment (P = .01).
Conclusions:
The experimental group exhibited palatal movement of the central incisors, more canine distal movement with less bone thickness changes, and less root resorption but took more time to achieve alignment than the control group.
Keywords: Nickel titanium, Heat-activated NiTi, Alveolar bone thickness, Root resorption, Unfavorable tooth movement, Dental alignment
INTRODUCTION
Nickel titanium (NiTi) archwires have been widely used during the initial alignment phase of orthodontic treatment due to their shape memory and superelastic properties, which offer large working ranges and relatively low and constant applied force magnitudes.1,2 NiTi archwires are classified into two main types: superelastic austenite-active and heat-activated martensitic-active NiTi archwires.3 Heat-activated NiTi archwires have the advantage of producing lower force magnitudes than superelastic NiTi archwires of the same diameter and deflection.2,4,5
Relatively low force levels from NiTi archwires might reduce the risk of root resorption.6 However, even small diameter heat-activated NiTi archwires can produce force magnitudes that are higher2,4 than recommended,1 especially the 10–20 cN recommended for intrusion. Additionally, with greater amounts of crowding and malalignment, the more deflection of the archwire occurs, thus leading to higher magnitudes of forces and moments applied to the teeth7,8 and potentially greater undesirable side effects. Such side effects can include initial incisor proclination in extraction cases leading to incisor round-tripping,9 which may increase the time required to achieve alignment.7,8,10 Because initial dental alignment consists of many types and amounts of tooth movement, archwire selection and application are critical to minimize periodontal destruction.11 Preliminary laboratory studies using a three-bracket bending test showed that a NiTi wire bent close to the bracket produced deactivation forces ranging from 23 to 70 cN, which were lower than those of heat-activated NiTi wire at the same deflection (70–104 cN).
The purpose of customizing NiTi archwires would be to minimize the applied forces with the intent of moving teeth more efficiently with iatrogenic effects to the periodontium. No previous study has demonstrated a technique that diminishes the unfavorable side effects created by inserting a preformed archwire into malaligned brackets in continuous archwire treatment. Thus, this study aimed to compare tooth and alveolar bone changes after initial anterior dental alignment with 0.012-inch NiTi archwires of two types: preformed heat-activated (control group) and customized (experimental group). The null hypothesis was that there would be no difference between the groups with respect to tooth movement, bone thickness changes, root resorption, and time to achieve alignment.
MATERIALS AND METHODS
Subjects
This was a two-arm, parallel, randomized controlled trial approved by the Faculty of Dentistry, Prince of Songkla University Ethics Committee (0521.1.03/591). The sample size calculation was based on a previous study12 to detect a mean difference in the irregularity index of 0.8 mm. According to the power analysis, for an independent t-test with a significance level of 0.05 and power of 80%, the sample size required was 17 per group. One additional subject per group was recruited in case of subject attrition.
Thirty-six subjects were recruited and randomly allocated using a random number table into two groups: preformed heat-activated (control group) and customized superelastic NiTi archwire (experimental group). The inclusion criteria were: healthy adults aged 18–25 years with periodontal pockets ≤3 mm, crowding of the maxillary anterior teeth with an irregularity index13 score >6 mm, and upper lip protrusion to be treated with maxillary first premolar extractions. The exclusion criteria were: failure of a bonded bracket and use of nonsteroidal anti-inflammatory drugs during the study. Blinding of the subjects and operator was not possible due to the bends placed only in the customized archwires of the experimental group; however, outcome assessments were blinded and were performed by the same examiner for both groups who was not part of the clinical performance of the study.
Treatment Protocol
At the initial study visit (T0), all subjects had impressions and limited field of view (FOV) cone-beam computed tomographies (CBCT) made prior to bonding conventional appliances (pre-adjusted edgewise brackets: Roth system, Ormco, Glendora, Calif) with 0.018 × 0.025-inch slots for the incisors and 0.022 × 0.028-inch slots on canines and posterior teeth consistent with the bidimensional technique.14 0.012-inch NiTi archwires were used for both groups: the control group received preformed heat-activated wires (BioStarter, FORESTADENT, Straight-Arch-Form, Transition temperature range at 37° C), and the experimental group received customized superelastic wires (SuperElastic Regular Force, Highland Metals). The ends of the archwires were cinched in both groups. Subjects were seen monthly until the maxillary anterior teeth were aligned and the irregularity index equaled 0 (TF). The time between T0-TF was assessed in months. During each subject's visit, the archwire was removed and left at room temperature and a maxillary alginate impression was made. In the control group, the same archwire was reinserted. In the experimental group, the bending protocol was applied and then the archwire was reinserted. After TF, the same archwire remained in place for three months before performing a second CBCT (TF) scan.
Bending Protocol
Custom bends in the superelastic NiTi archwires were made chairside at room temperature, creating permanent deformation at the bending points (Figure 1). The bending protocol started from the midline landmark of the archwire. Each bend was created relative to the bracket slot to be engaged by the corresponding portion of the archwire. The bends were created with vertical and horizontal bias to produce a 1-mm activation of the archwire to be engaged in the corresponding bracket slots of all anterior teeth. At each visit, the same archwire was removed and existing bends were reduced, straightening the wire similar to the shape of a preformed archwire, to continue moving the teeth toward alignment (Figure 2) until the bends were nearly eliminated and the teeth were aligned.
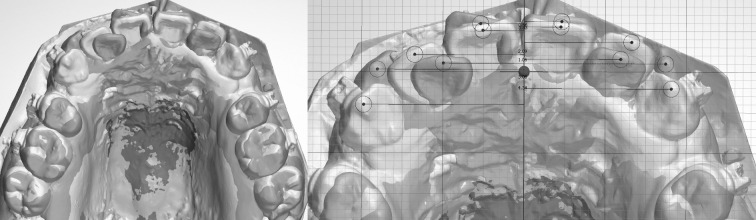
Figure 1.
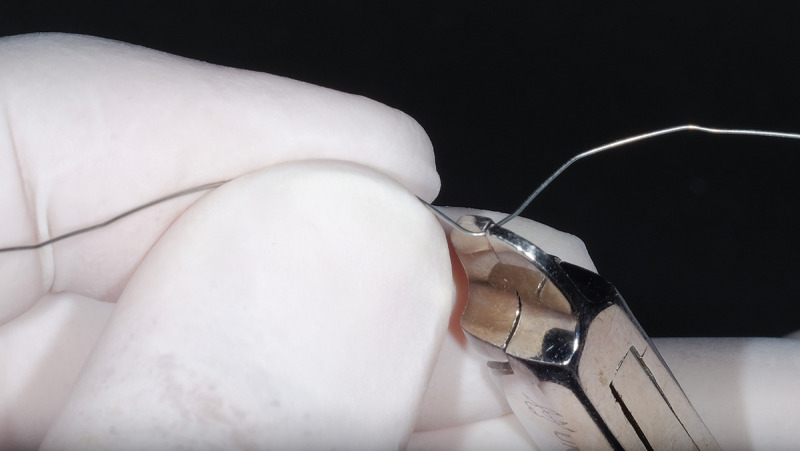
Tweed pliers were used to customize the NiTi archwires.
Figure 2.
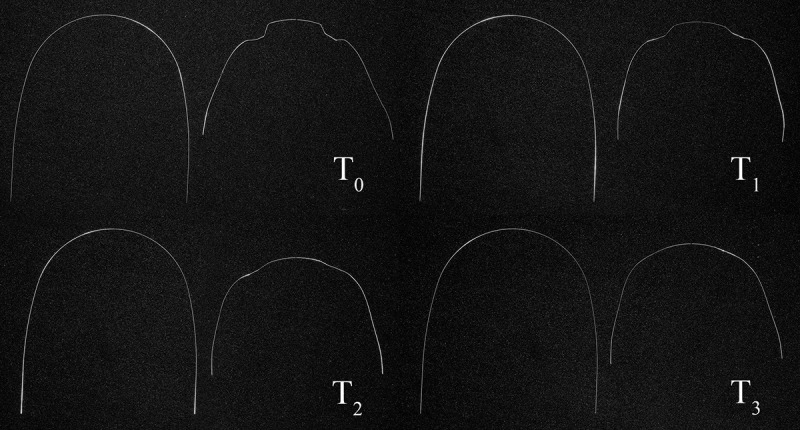
Appearance of a customized NiTi archwire from T0 to T3.
Assessment of Crowding
The amount of maxillary anterior dental crowding was evaluated twice on each dental model using Little's irregularity index13 by the same blinded examiner with the same Vernier caliper.
3D Digital Model Analysis
Dental models were made from maxillary impressions made at the initial (T0) and subsequent monthly visits (T1, T2, …, TF). The models were scanned using a calibrated scanner (R700 Orthodontic 3D Scanner, 3Shape, Copenhagen, Denmark). The rugae-palate superimposition method14 was employed with an analysis of superimpositions shown to be accurate and reliable15,16 and accomplished using commercial software (Ortho Analyzer, 3Shape, Copenhagen, Denmark). Dental change assessment focused on the movement of the maxillary anterior teeth in the anteroposterior and vertical dimensions by constructing X, Y, and Z axes as reference planes with the origin at the center of the incisive papilla of the initial cast. In the horizontal plane (X axis), the +/- signs indicated labial/palatal movement for incisors and distal/mesial movement of canines, respectively. In the vertical plane (Y axis), the +/- signs indicated extrusion/intrusion for all anterior teeth. The mean distance of right and left displaced canine cusp tips, middle of the incisal edges of maxillary central and lateral incisors, were measured relative to the 3D coordinate system at each time point (Figure 3).
Figure 3.
Tooth movement assessment via digital model analysis.
CBCT Analysis
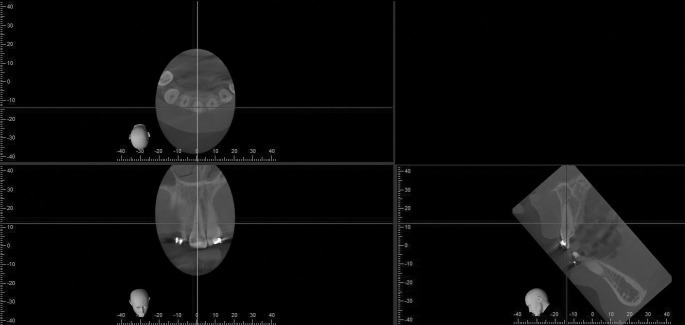
Bone thickness changes and root resorption of the maxillary anterior teeth were evaluated using limited field of view CBCT scans (80 kV, 5 mA, 80 × 40 mm with 0.125 mm voxel resolution; Veraviewepocs, J. Morita, Tokyo, Japan). The alveolar bone thicknesses were evaluated as previously described17 (Figures 4, 5, and 6). Each side and each level of each tooth were averaged to represent the mean thickness (mm) of the specific side and level. The data were paired and averaged between the right and left of the central and lateral incisors and the canines.
Figure 4.
Axial, sagittal, and coronal slices of CBCT images.
Figure 5.
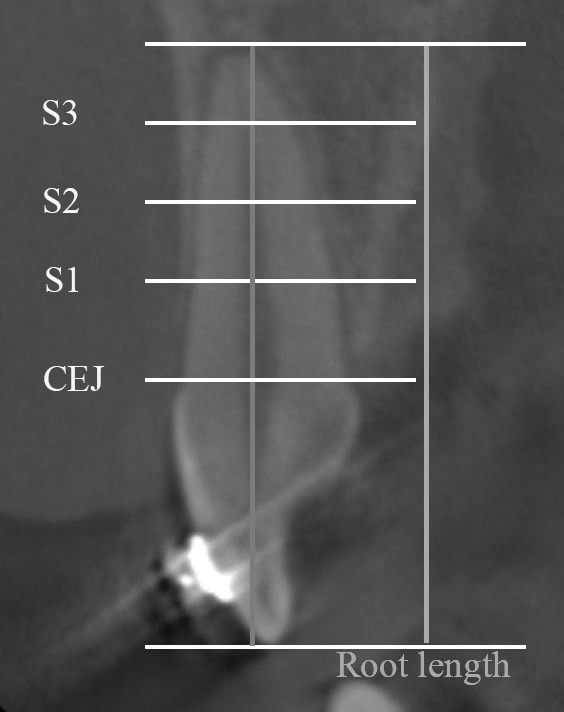
Levels of alveolar bone thickness measurement (S1, S2, and S3).
Figure 6.
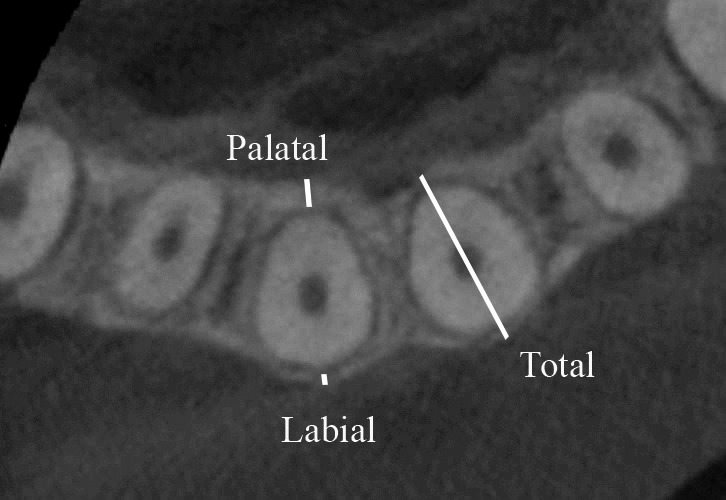
Labial, palatal, and total alveolar bone thicknesses.
Root length was assessed by means of axial, coronal, and sagittal slices18 (Figures 4 and 5). The root lengths (mm) at T0 and TF were then compared.
Statistical Analysis
Shapiro–Wilk tests revealed that all of the parameters were skewed. Wilcoxon signed-rank tests compared the changes between T0 and TF and Mann–Whitney U-tests evaluated between-group differences. The significance level of all tests was 0.05. The 3D-dental model and CBCT measurements, and four-week remeasurements performed by the same blinded examiner were used to evaluate the reliability of the Dahlberg formula.19 The measurement errors of the irregularity index, 3D-dental model, and CBCT measurements were 0.19, 0.15, and 0.14 mm, respectively. The Wilcoxon signed-rank test showed no significant differences (P > .05) between the two sets of measurements.
RESULTS
Four subjects were excluded: three because of bracket failures and one withdrew from the study, as shown in the CONSORT flowchart (Figure 7). Demographic characteristics of the two groups were not significantly different between the groups (Table 1).
Figure 7.
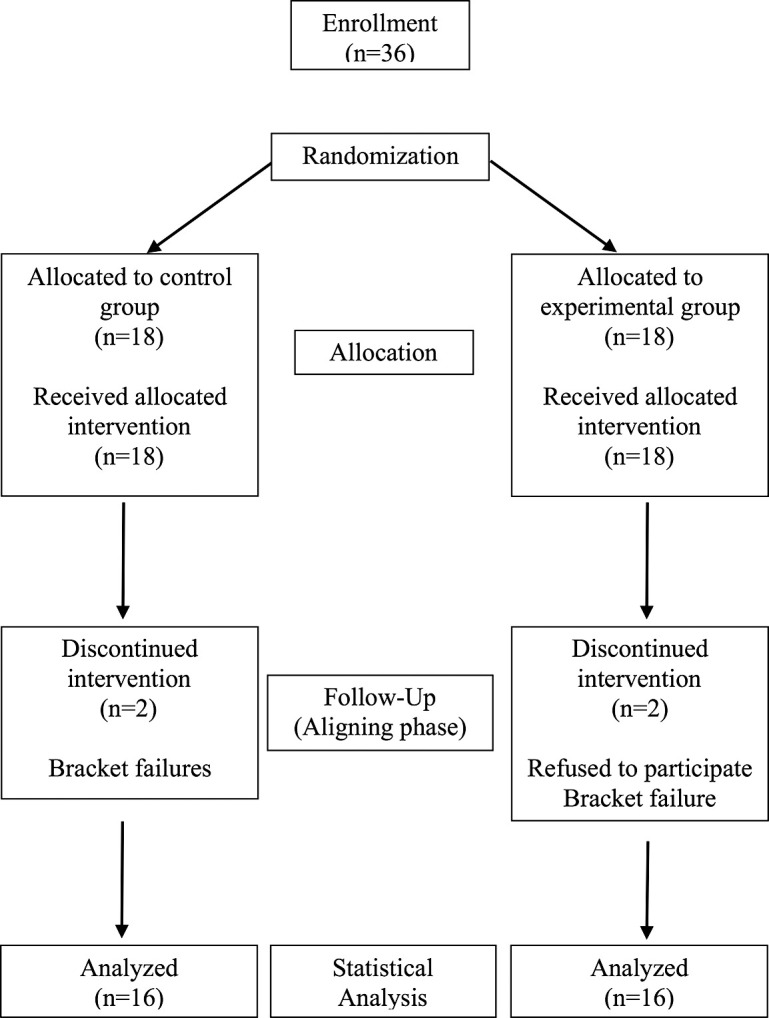
CONSORT flowchart of the study.
Table 1.
Demographics and Clinical Characteristics of the Patients at T0
| Variable |
Control n = 16 Mean or % |
SD |
Experimental n = 16 Mean or % |
SD |
Total | SD |
P Value |
| n = 32 Mean or % | |||||||
| Age (y) | 20.1 | 1.9 | 19.6 | 1.4 | 19.8 | 1.7 | .56 |
| Sex | |||||||
| Male | 25 | 19 | 22 | ||||
| Female | 75 | 81 | 78 | ||||
| Irregularity index (mm) | 14.0 | 2.1 | 13.9 | 2.2 | 13.9 | 2.1 | .56 |
Significant at P < .05.
SD indicates standard deviation.
The labiopalatal movements of the central incisors were different between the groups. The experimental group showed almost linear palatal (−) movement with a mean ± standard deviation (SD) of −0.96 ± 0.41 mm for TF-T0 and the control group showed labial (+) movement that peaked at T2-T0 (+0.91 ± 1.08 mm) and resulted in +0.75 ± 1.42 mm for TF-T0 (Figures 8 and 9). For the lateral incisors, labial movement peaked at T4 in both groups but the control group had a greater amount at all time points than the experimental group up to a maximum difference of +1.42 ± 0.29 mm for TF-T0 (Figures 8 and 9). For the canines, distal movement peaked at T4 in both groups and were larger at all time points for the experimental compared to the control group by up to 0.60 mm more at TF-T0 (Figures 8 and 9).
Figure 8.
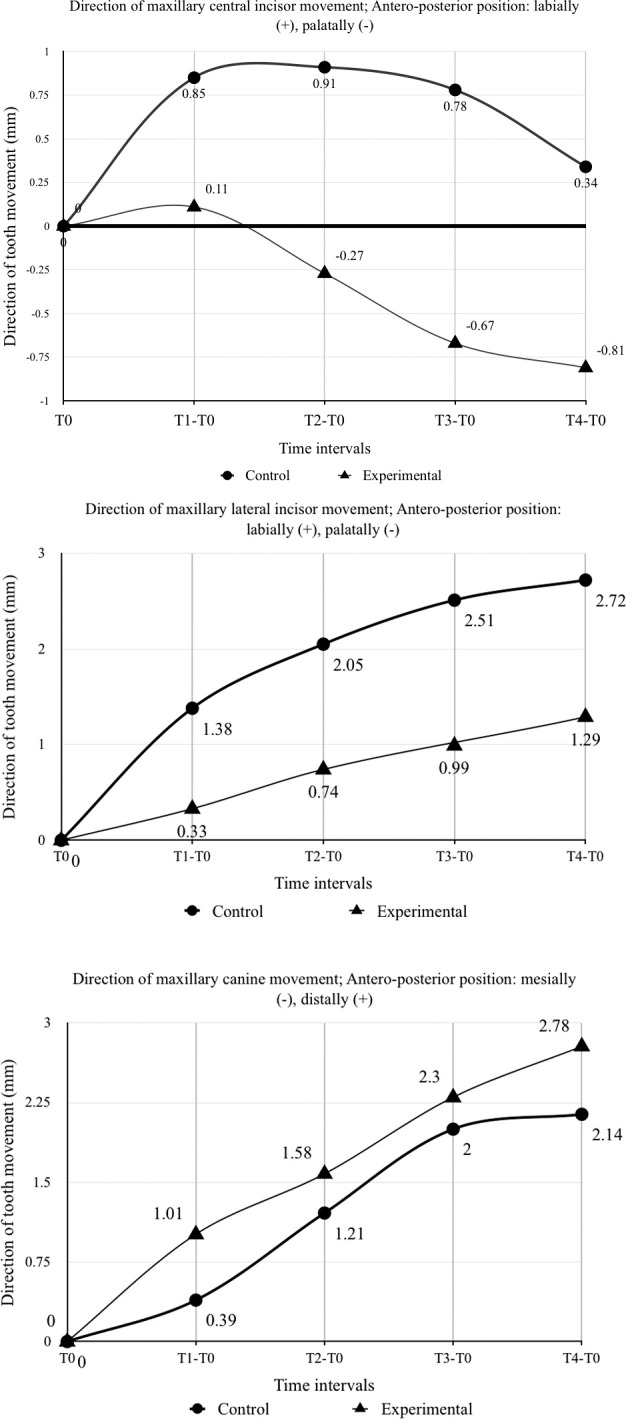
Comparisons of the direction of tooth movement at monthly intervals to T0 between groups.
Figure 9.
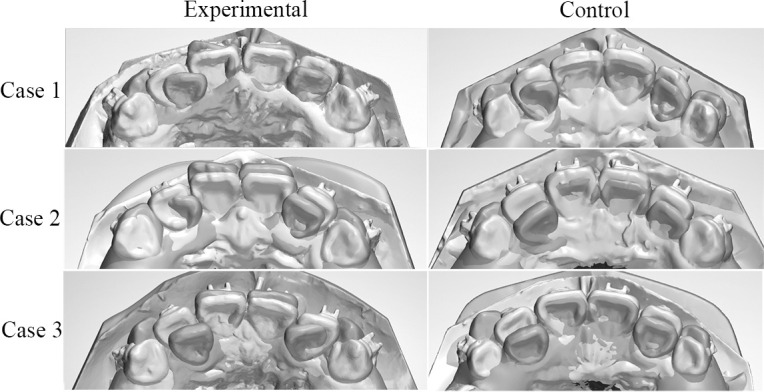
Model superimposition of cases between groups from T0 to TF.
Significant differences between the groups were found in the labiopalatal movement for the central and lateral incisors at each time point (all P ≤ .003) and in distal movement for the canines at T1-T0, T2-T0, and TF-T0 (all P ≤ .049). However, there was no significant difference in the amount of extrusion found in either group at any time point (all P > .05) (Table 2, Figure 9).
Table 2.
Comparison of the Differences in Amount of Tooth Movement at Monthly Intervals to T0 Between Groups
| Groups |
Tooth |
Direction |
Time Interval; Mean (SD) (mm) |
||||
| T1-T0 |
T2-T0 |
T3-T0 |
T4-T0 |
TF-T0 |
|||
| Control group | Central incisors | A-P | 0.85 (0.74) | 0.91 (1.08) | 0.78 (1.34) | 0.34 (1.18) | 0.75 (1.42) |
| V | 0.3 (0.42) | 0.44 (0.37) | 0.55 (0.5) | 0.74 (0.48) | 0.57 (0.52) | ||
| Lateral incisors | A-P | 1.38 (0.84) | 2.05 (1.08) | 2.51 (1.22) | 2.72 (1.1) | 2.65 (1.03) | |
| V | −0.16 (0.47) | 0 (5.4) | 0.31 (0.59) | 0.81 (0.94) | 0.68 (0.67) | ||
| Canines | A-P | 0.39 (0.22) | 1.21 (0.8) | 2 (0.78) | 2.14 (0.55) | 2.16 (0.8) | |
| V | 0.54 (0.54) | 0.98 (0.58) | 1.32 (0.82) | 1.42 (0.93) | 1.55 (0.73) | ||
| Experimental group | Central incisors | A-P | 0.11 (0.11) | −0.27 (0.19) | −0.67 (0.35) | −0.81 (0.5) | −0.96 (0.41) |
| V | 0.21 (0.26) | 0.37 (0.37) | 0.46 (0.31) | 0.49 (0.39) | 0.56 (0.38) | ||
| Lateral incisors | A-P | 0.33 (0.15) | 0.74 (0.26) | 0.99 (0.4) | 1.29 (0.5) | 1.22 (0.51) | |
| V | 0.11 (0.1) | 0.14 (0.11) | 0.3 (0.23) | 0.42 (0.33) | 0.41 (0.31) | ||
| Canines | A-P | 1.01 (0.34) | 1.58 (0.5) | 2.3 (0.73) | 2.78 (0.86) | 2.76 (0.81) | |
| V | 0.52 (0.28) | 0.86 (0.5) | 1.24 (0.67) | 1.48 (0.76) | 1.52 (0.74) | ||
| Between groups | Central incisors | A-P | 0.74 (1.87) | 1.18 (0.27) | 1.45 (0.35) | 1.15 (0.32) | 1.71 (0.37) |
| P value | < .001* | .001* | < .001* | < .001* | < .001* | ||
| V | 0.09 (0.12) | 0.07 (0.13) | 0.09 (0.15) | 0.15 (0.21) | 0.01 (0.16) | ||
| P value | .539 | .59 | .266 | .412 | .534 | ||
| Lateral incisors | A-P | 1.05 (0.21) | 1.31 (0.27) | 1.52 (0.32) | 1.43 (0.34) | 1.42 (0.29) | |
| P value | < .001* | < .001* | .001* | .003* | < .001* | ||
| V | −0.27 (0.12) | −0.14 (0.14) | 0 (0.16) | 0.39 (0.37) | 0.27 (0.18) | ||
| P value | .149 | .616 | .385 | .279 | .109 | ||
| Canines | A-P | 0.62 (0.1) | 0.37 (0.1) | 0.29 (0.27) | 0.63 (0.31) | 0.6 (0.28) | |
| P value | < .001* | .008* | .175 | .117 | .049* | ||
| V | 0.02 (0.15) | 0.12 (0.19) | 0.08 (0.26) | 0.06 (0.41) | 0.03 (0.26) | ||
| P value | .752 | .402 | .474 | .765 | .821 | ||
Significant at P < .05.
SD indicates standard deviation; TF, the final visit when achieved alignment;
Antero-posterior movement; + = labial movement of incisors, distal movement of canines, - = palatal movement of incisors, mesial movement of canines.
Vertical movement; + = extrusion, - = intrusion.
After alignment (TF-T0), at the S1 and S2 levels, significantly decreased bone thicknesses labial to the central and lateral incisors were found in both groups (P < .046) (Table 3). The changes in bone thickness labial to the central incisors were significantly different between the groups at the S1 and S2 levels, where the control group showed a two- to three-times greater decrease in labial bone thickness (−0.22 ± 0.06, −0.17 ± 0.11 mm, respectively) compared to the experimental group (−0.07 ± 0.08, −0.08 ± 0.10 mm, respectively; P ≤ .004) (Table 4). For the lateral incisors, the labial bone thickness changes between TF-T0 were significantly different between the groups at the S1 and S2 levels, where the control group showed a three- and five-times greater decrease (−0.31 ± 0.10, −0.23 ± 0.13 mm, respectively) compared to the experimental group (−0.10 ± 0.11, 0.04 ± 0.20 mm, respectively; P ≤ .001). Bone thicknesses palatal to the canines were decreased at the S1 and S2 levels in both groups. In a comparison between the two groups, no statistically significant differences were found (P > .076) (Table 4).
Table 3.
Mean Values and Differences in Bone Thickness Changes and Root Length at T0 and TF Within Each Group
| Variables |
Control Group |
Experimental Group |
||||||||
| T0 |
TF |
P Value |
T0 |
TF |
P Value |
|||||
| Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|||
| Bone thickness changes (mm) | ||||||||||
| Central incisors | ||||||||||
| S1L | 0.71 | 0.26 | 0.49 | 0.25 | < .001* | 0.72 | 0.18 | 0.65 | 0.15 | .007* |
| S1P | 1.74 | 0.55 | 1.46 | 0.56 | .004* | 1.49 | 0.42 | 1.33 | 0.43 | .066 |
| S1T | 8.42 | 0.69 | 7.96 | 0.62 | .001* | 8.36 | 0.58 | 8.07 | 0.63 | .006* |
| S2L | 0.58 | 0.2 | 0.4 | 0.16 | .001* | 0.63 | 0.19 | 0.55 | 0.17 | .009* |
| S2P | 2.3 | 0.59 | 2.1 | 0.52 | .023* | 2.18 | 0.52 | 2.05 | 0.57 | .078 |
| S2T | 7.99 | 0.85 | 7.54 | 0.79 | .001* | 8.13 | 0.6 | 7.84 | 0.64 | .008* |
| S3L | 0.9 | 0.8 | 0.64 | 0.34 | .07 | 0.93 | 0.44 | 0.7 | 0.43 | .001* |
| S3P | 3.14 | 0.99 | 2.91 | 0.96 | .034* | 3.4 | 0.79 | 3.48 | 1.06 | .438 |
| S3T | 7.72 | 1.59 | 7.07 | 1.44 | .002* | 8.06 | 0.78 | 7.9 | 0.99 | .485 |
| Lateral incisors | ||||||||||
| S1L | 0.61 | 0.21 | 0.3 | 0.2 | < .001* | 0.57 | 0.17 | 0.47 | 0.2 | .005* |
| S1P | 1.1 | 0.58 | 0.65 | 0.44 | < .001* | 0.98 | 0.39 | 0.78 | 0.4 | .002* |
| S1T | 7.71 | 0.78 | 6.97 | 0.74 | < .001* | 7.71 | 0.49 | 7.38 | 0.48 | .001* |
| S2L | 0.45 | 0.29 | 0.22 | 0.21 | < .001* | 0.32 | 0.13 | 0.37 | 0.22 | .438 |
| S2P | 1.99 | 0.59 | 1.2 | 0.71 | < .001* | 1.87 | 0.53 | 1.38 | 0.67 | .001* |
| S2T | 7.61 | 1.05 | 6.61 | 1.03 | < .001* | 7.42 | 0.66 | 6.94 | 0.83 | .001* |
| S3L | 0.42 | 0.23 | 0.62 | 0.52 | .046* | 0.44 | 0.26 | 0.59 | 0.3 | .004* |
| S3P | 3.26 | 0.97 | 1.98 | 1.02 | < .001* | 3.32 | 0.87 | 2.54 | 1.13 | < .001* |
| S3T | 7.49 | 1.28 | 6.38 | 1.29 | .001* | 7.47 | 0.83 | 6.78 | 1.09 | .001* |
| Canines | ||||||||||
| S1L | 0.56 | 0.3 | 0.54 | 0.33 | .66 | 0.55 | 0.25 | 0.59 | 0.25 | .649 |
| S1P | 1.61 | 0.74 | 1.03 | 0.77 | < .001* | 1.51 | 0.56 | 1.21 | 0.63 | .005* |
| S1T | 9.68 | 0.82 | 9.17 | 0.82 | .001* | 9.53 | 0.68 | 9.21 | 0.69 | .001* |
| S2L | 0.39 | 0.19 | 0.34 | 0.24 | .063 | 0.38 | 0.18 | 0.39 | 0.21 | .9 |
| S2P | 2.33 | 1.09 | 1.87 | 1.08 | .006* | 2.24 | 0.84 | 2.1 | 0.91 | .191 |
| S2T | 9.2 | 1.24 | 8.71 | 1.1 | .011* | 9.36 | 0.97 | 8.98 | 1.04 | .001* |
| S3L | 0.36 | 0.13 | 0.21 | 0.19 | .005* | 0.41 | 0.26 | 0.33 | 0.22 | .004* |
| S3P | 3.14 | 0.87 | 2.83 | 1.06 | .224 | 3.41 | 0.77 | 3.15 | 1.01 | .062 |
| S3T | 8.64 | 1.17 | 8.21 | 1.25 | .034* | 8.92 | 0.91 | 8.56 | 1.04 | .004* |
| Root length (mm) | ||||||||||
| Central incisors | 23.54 | 2.22 | 23.25 | 2.25 | < .001* | 23.79 | 0.98 | 23.55 | 0.97 | < .001* |
| Lateral incisors | 22.31 | 1.23 | 21.87 | 1.29 | < .001* | 22.76 | 0.93 | 22.52 | 0.96 | < .001* |
| Canines | 25.42 | 1.75 | 25.05 | 1.81 | < .001* | 25.9 | 1.4 | 25.69 | 1.44 | < .001* |
Significant at P < .05.
SD indicates standard deviation.
Table 4.
Comparison of Mean Values and Differences in Bone Thickness Changes and Root Length at TF –T0 Between Groups
| Variables |
Control group |
Experimental Group |
P Value |
||
| TF-T0 |
TF-T0 |
||||
| Mean Diff |
SD |
Mean Diff |
SD |
||
| Bone thickness changes (mm) | |||||
| Central incisors | |||||
| S1L | −0.22 | 0.06 | −0.07 | 0.08 | < .001* |
| S1P | −0.28 | 0.34 | −0.16 | 0.35 | .073 |
| S1T | −0.46 | 0.45 | −0.3 | 0.43 | .067 |
| S2L | −0.17 | 0.11 | −0.08 | 0.1 | .004* |
| S2P | −0.2 | 0.32 | −0.14 | 0.31 | .318 |
| S2T | −0.45 | 0.43 | −0.29 | 0.42 | .09 |
| S3L | −0.26 | 0.54 | −0.23 | 0.19 | .534 |
| S3P | −0.23 | 0.43 | 0.09 | 0.49 | .029* |
| S3T | −0.65 | 0.65 | −0.17 | 0.66 | .005* |
| Lateral incisors | |||||
| S1L | −0.31 | 0.1 | −0.1 | 0.11 | < .001* |
| S1P | −0.45 | 0.46 | −0.21 | 0.24 | .09 |
| S1T | −0.75 | 0.46 | −0.33 | 0.23 | .001* |
| S2L | −0.23 | 0.13 | 0.04 | 0.2 | < .001* |
| S2P | −0.79 | 0.64 | −0.49 | 0.49 | .169 |
| S2T | −1 | 0.6 | −0.48 | 0.44 | .006* |
| S3L | 0.2 | 0.34 | 0.15 | 0.18 | .806 |
| S3P | −1.28 | 0.96 | −0.78 | 0.73 | .083 |
| S3T | −1.11 | 0.65 | −0.7 | 0.58 | .062 |
| Canines | |||||
| S1L | −0.02 | 0.13 | 0.04 | 0.15 | .651 |
| S1P | −0.57 | 0.44 | −0.3 | 0.32 | .141 |
| S1T | −0.51 | 0.45 | −0.33 | 0.25 | .227 |
| S2L | −0.05 | 0.19 | 0 | 0.1 | .076 |
| S2P | −0.47 | 0.6 | −0.14 | 0.49 | .008* |
| S2T | −0.49 | 0.64 | −0.39 | 0.32 | .44 |
| S3L | −0.15 | 0.16 | −0.09 | 0.1 | .193 |
| S3P | −0.31 | 0.82 | −0.26 | 0.64 | .706 |
| S3T | −0.43 | 0.73 | −0.36 | 0.39 | .611 |
| Root length (mm) | |||||
| Central incisors | −0.3 | 0.09 | −0.24 | 0.15 | .007* |
| Lateral incisors | −0.44 | 0.2 | −0.24 | 0.18 | .002* |
| Canines | −0.36 | 0.25 | −0.21 | 0.1 | .083 |
Significant at P < .05.
SD indicates standard deviation.
Root resorption was noted in all anterior teeth between TF-T0 (P < .001). The experimental group had a lower amount of root resorption at the central and lateral incisors (−0.24 ± 0.15 and −0.24 ± 0.18 mm, respectively) compared to the control group (−0.30 ± 0.09 and −0.44 ± 0.20 mm, respectively; P ≤ .007).
The duration of TF-T0 was significantly shorter (P < .01) in the control (3.4 ± 0.5 months) compared to the experimental (3.9 ± 0.3 months) group. For the rate of alleviation of crowding, the control group had a significantly higher mean rate of 4.1 mm improvement per month compared with 3.6 mm per month in the experimental group (P = .01). Comparisons of the treatment times and reduction of the irregularity index between the groups are shown in Table 5.
Table 5.
Comparison of Treatment Times at Monthly Intervals and Reduction of the Irregularity Index Between Control and Experimental Groups
| Time Interval |
Irregularity Index |
||||||
| Control |
Experimental NiTi |
Between Groups |
|||||
| Mean |
SD |
Mean |
SD |
Mean |
SD |
P value |
|
| T0 | 14.0 | 2.1 | 13.9 | 2.2 | 0.1 | 0.8 | .556 |
| T0- T1 | 5.3 | 1.6 | 3.1 | 1.1 | 2.2 | 0.5 | .001* |
| T1-T2 | 3.9 | 1.1 | 3.4 | 1 | 0.4 | 0.4 | .251 |
| T2-T3 | 3.3 | 1.5 | 4.3 | 1.3 | −1 | 0.5 | .040* |
| T3-T4 | 1.5 | 1.9 | 3.1 | 1.4 | −1.6 | 0.6 | .029* |
Significant at P < .05.
SD indicates standard deviation.
DISCUSSION
In this study, crowding was relieved by incisor proclination to increase arch perimeter or canine distal movement into extraction spaces or both. Generally, incisor proclination is considered to be unfavorable since there is unnecessary round-tripping of teeth.9,10,20 To prevent this, canine distal movement should be initiated to gain sufficient space.9,21 From this study, there were statistically and clinically significant differences in the amount of canine distal movement between groups. In the experimental compared to the control group, more canine distal movement occurred in the first and second months leading to more total canine distal movement, while the central incisors moved labially, then progressively moved palatally (T0-TF). The increased amount of canine distal movement might have facilitated the central incisor retroclination observed in the experimental group. In the control group, the alignment achieved during the first two months was achieved, at least in part, because of increased arch perimeter due to incisor proclination20 from T0-T2 (Table 2).
Regarding lateral incisor movement, the amount of proclination was higher in the control group because space was lacking for the lateral incisors to align due to the lower amount of canine distal movement in that group. However, in the experimental group, more space was gained from canine distal movement. These findings corresponded with reduction in the irregularity index, which occurred mostly in the first month of treatment in the control group via incisor proclination. In the experimental group, reduction of the irregularity index occurred more steadily and with increased canine distal movement (Table 5).
One possible explanation for the lesser amount of canine distal movement observed in the control group could be due to the complexity of the forces and moments generated due to the wire-bracket angles7,8 created, which impeded canine movement into the extraction site. With the aim of decreasing the complexity of the forces and moments by decreasing the wire-bracket angle magnitudes, the experimental protocol may have promoted distal movement of the canines and gradual alignment of the incisors following the shape of the reduced bends.
Decreased bone thickness was observed in both groups. The reason might be related to the amount of extrusion observed in all anterior teeth. As the teeth extruded, they moved toward a narrower alveolar bone configuration, leading to decreased bone thickness around the teeth. A greater decrease in bone thickness labial to the central and lateral incisors was observed at the S1 and S2 levels in the control group. Changes in the bone thickness were consistent with the observed tooth movement. This was in agreement with previous studies that used CBCT to measure bone thickness changes.17,22 Decreased bone thickness labial to the central and lateral incisors may have been due to the amount of proclination and the magnitude of forces applied to the tooth. As the amount of proclination increased, the tooth tipped labially toward the labial cortical bone, leading to labial bone resorption. Furthermore, in the control group, incisor crowding and consequently small interbracket distances, combined with a lack of canine distal movement to create space for alignment, likely resulted in higher force levels exerted by the wire.
The finding that root resorption occurred in the early leveling phase using NiTi archwire is consistent with previous studies.23,24 If the assumed association between a greater risk of root resorption with higher magnitude of applied forces11 is true, the significantly higher mean root resorption of the central and lateral incisors in the control compared to the experimental group suggests that the applied forces in the control group were higher than the experimental group. However, the applied forces were not measured in this study.
The time required to achieve alignment in the control group was significantly shorter than in the experimental group at 0.4 months overall, or at a rate of 0.5 mm/mo faster. However, the control group experienced more incisor proclination, greater labial bone thickness decreases, and more root resorption.
The irregularity index was used in this study to evaluate and monitor crowding, but the index does not take into account tooth positions and changes in three dimensions. Therefore, the anteroposterior and vertical movements of the anterior teeth were evaluated and compared to provide more detailed data to explain how crowding was resolved within and between groups.
Limitations
Due to a loss of two subjects in each group, the sample sizes were lower than expected and the power of the study was reduced. However, several significantly different outcomes between the groups were still detected.
To evaluate bone and root changes occurring during the study, it would have been more ideal to wait six months for bone remodeling to occur before reassessment. However, for ethical reasons, a three-month resting period after complete alignment was used, which should have allowed reasonable time for the repair process to occur,17 while minimally delaying treatment progress.
To achieve the precision required to bend the wire accurately for the experimental group in this study, considerable clinical chair time was required for customizing the NiTi archwires used. The time for bending the wire was reduced with extra practice and experience. However, the amount of time used to bend the wire was not measured as part of this study. Similarly, it is acknowledged that the properties of the customized NiTi archwires might be altered by bending, thereby causing a decrease in elastic properties at the permanent deformation points. However, the mechanical property changes of the customized archwires were not evaluated as part of this study.
The customized NiTi archwire protocol used in this study reduced some of the undesirable side effects of orthodontic alignment in comparison to the control NiTi archwire protocol, but it required considerable clinical chair time and resulted in a longer time required for tooth alignment. Ultimately, the differences must be considered in a cost-benefit analysis for patients. From a long-term perspective, favorable tooth movement decreased the risk of bone and root resorption, which could be considerably beneficial to patients.
CONCLUSIONS
Use of customized NiTi archwires to align anterior teeth in the experimental group resulted in palatal movement of the central incisors compared to labial movement in the control group.
The experimental group experienced more canine distal movement with less bone thickness decreases at the incisors, and less root resorption.
It took more time to achieve alignment in the experimental than the control group.
ACKNOWLEDGMENTS
We would like to thank the Graduate School and the Faculty of Dentistry, Prince of Songkla University, for grant support.
REFERENCES
- 1.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics 5th ed. St. Louis, MO: Elsevier/Mosby;; 2013. [Google Scholar]
- 2.Lombardo L, Marafioti M, Stefanoni F, Mollica F, Siciliani G. Load deflection characteristics and force level of nickel titanium initial archwires. Angle Orthod. 2012;82:507–521. doi: 10.2319/032511-213.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wayman CM, Duerig TW. An introduction to martensite and shape memory. Engineering Aspects of Shape Memory Alloys. London, UK: Butterworth-Heinemann Ltd;; 1990. pp. 3–20. [Google Scholar]
- 4.Chan E, Darendeliler MA. Physical properties of root cementum: Part 5. Volumetric analysis of root resorption craters after application of light and heavy orthodontic forces. Am J Orthod Dentofacial Orthop. 2005;127:186–195. doi: 10.1016/j.ajodo.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 5.Mulligan TF. Common Sense Mechanics in Everyday Orthodontics. Pheonix, Ariz: CSM Publishing;; 2009. [Google Scholar]
- 6.Graber TM, Vanarsdall RL, Vig KWL. Orthodontics: Current Principles & Techniques 4th ed. St. Louis, Mo: Elsevier Mosby;; 2005. [Google Scholar]
- 7.Nanda RS, Tosun YS. Biomechanics in Orthodontics: Principles and Practice. 2010. Hanover Park, Ill.: Quintessence Publishing Co;
- 8.Shroff B LS. Leveling and aligning: challenges and solutions. Semin Orthod. 2001;7:16–25. [Google Scholar]
- 9.Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 10.Fansa M, Keilig L, Reimann S, Jager A, Bourauel C. The leveling effectiveness of self-ligating and conventional brackets for complex tooth malalignments. J Orofac Orthop. 2009;70:285–296. doi: 10.1007/s00056-009-9916-z. [DOI] [PubMed] [Google Scholar]
- 11.Montasser MA, El-Bialy T, Keilig L, Reimann S, Jager A, Bourauel C. Force levels in complex tooth alignment with conventional and self-ligating brackets. Am J Orthod Dentofacial Orthop. 2013;143:507–514. doi: 10.1016/j.ajodo.2012.11.020. [DOI] [PubMed] [Google Scholar]
- 12.Scott P, DiBiase AT, Sherriff M, Cobourne MT. Alignment efficiency of Damon3 self-ligating and conventional orthodontic bracket systems: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2008;134:470. doi: 10.1016/j.ajodo.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 13.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod Dentofacial Orthop. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 14.Gianelly AA. Bidimensional Technique: Theory and Practice. New York, NY: GAC International Inc;; 2000. p. 121. [Google Scholar]
- 15.Jang I, Tanaka M, Koga Y, et al. A novel method for the assessment of three-dimensional tooth movement during orthodontic treatment. Angle Orthod. 2009;79:447–453. doi: 10.2319/042308-225.1. [DOI] [PubMed] [Google Scholar]
- 16.Choi DS, Jeong YM, Jang I, Jost-Brinkmann PG, Cha BK. Accuracy and reliability of palatal superimposition of three-dimensional digital models. Angle Orthod. 2010;80:497–503. doi: 10.2319/101309-569.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarikaya S, Haydar B, Ciger S, Ariyurek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002;122:15–26. doi: 10.1067/mod.2002.119804. [DOI] [PubMed] [Google Scholar]
- 18.Castro IO, Alencar AHG, Valladares-Neto J, Estrela C. Apical root resorption due to orthodontic treatment detected by cone beam computed tomography. Angle Orthod. 2013;83:196–203. doi: 10.2319/032112-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dahlberg G. Statistical Methods for Medical and Biological Students. London, UK: Allen and Unwin;; 1940. [Google Scholar]
- 20.Fleming PS, DiBiase AT, Sarri G, Lee RT. Comparison of mandibular arch changes during alignment and leveling with 2 preadjusted edgewise appliances. Am J Orthod Dentofacial Orthop. 2009;136:340–347. doi: 10.1016/j.ajodo.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 21.McLaughlin RP, Bennett JC, Trevisi HJ. Systemized Orthodontic Treatment Mechanics. UK: Mosby Edinburgh;; 2001. [Google Scholar]
- 22.Yodthong N, Charoemratrote C, Leethanakul C. Factors related to alveolar bone thickness during upper incisor retraction. Angle Orthod. 2013;83:394–401. doi: 10.2319/062912-534.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramanathan C, Hofman Z. Root resorption during orthodontic tooth movements. Eur J Orthod. 2009;31:578–583. doi: 10.1093/ejo/cjp058. [DOI] [PubMed] [Google Scholar]
- 24.Makedonas D, Lund H, Grondahl K, Hansen K. Root resorption diagnosed with cone beam computed tomography after 6 months of orthodontic treatment with fixed appliance and the relation to risk factors. Angle Orthod. 2012;82:196–201. doi: 10.2319/112810-691.1. [DOI] [PMC free article] [PubMed] [Google Scholar]