Abstract
Objectives:
To evaluate changes in the volume and cross-sectional area of the nasal airway before and 1 year after nonsurgical miniscrew-assisted rapid maxillary expansion (MARME) in young adults.
Materials and Methods:
Fourteen patients (mean age, 22.7 years; 10 women, four men) with a transverse discrepancy who underwent cone beam computed tomography before (T0), immediately after (T1), and 1 year after (T2) expansion were retrospectively included in this study. The volume of the nasal cavity and nasopharynx and the cross-sectional area of the anterior, middle, and posterior segments of the nasal airway were measured and compared among the three timepoints using paired t-tests.
Results:
The volume of the nasal cavity showed a significant increase at T1 and T2 (P < .05), while that of the nasopharynx increased only at T2 (P < .05). The anterior and middle cross-sectional areas significantly increased at T1 and T2 (P < .05), while the posterior cross-sectional area showed no significant change throughout the observation period (P > .05).
Conclusions:
The results demonstrate that the volume and cross-sectional area of the nasal cavity increased after MARME and were maintained at 1 year after expansion. Therefore, MARME may be helpful in expanding the nasal airway.
Keywords: Airway, MARME, Nasal cavity
INTRODUCTION
Rapid maxillary expansion (RME) is an orthodontic treatment modality for correcting transverse discrepancy. However, in adults, conventional RME can produce side effects such as buccal crown tipping, root resorption, failure of suture separation, and marginal bone loss.1 To minimize these undesirable effects, expansion of the basal bone would be required.
Recently, successful expansion of the maxilla using miniscrews combined with an RME device was reported.2,3 The RME appliance maximizes skeletal expansion and minimizes dental side effects. According to a recent study,3 miniscrew-assisted rapid maxillary expansion (MARME) can be a clinically acceptable and stable treatment modality for maxillary constriction in young adults.
Patients with maxillary constriction tend to have narrow airways compared with normal individuals.4 As V-shaped expansion of the maxilla directly affects the nasal floor, the nasal cavity volume would change after the expansion.5,6 In previous studies, it was found that maxillary expansion through conventional RME contributed to an increase in the airway volume in children with obstructive sleep apnea (OSA).7,8 Adults with OSA have also shown maxillary constriction; however, it remains unclear whether maxillary constriction is a primary etiological factor for OSA.9
An increased upper airway volume has also been reported in adults treated with surgically assisted rapid maxillary expansion (SARME),10,11 although the clinical significance of this finding is considered questionable because of measurement errors associated with the acoustic rhinometry (AR) technique and variability in individual response.12 Furthermore, because a surgical procedure can affect the airway volume, the findings after SARME cannot be directly applied to MARME. Children are also different from adults in that they continue to grow. Therefore, additional studies are necessary for the accurate evaluation of airway changes after MARME in adults.
Even though the nasal cavity is directly affected by maxillary expansion, three-dimensional (3D) research is lacking, and most studies have focused on the pharyngeal airway because of technical difficulties in obtaining nasal cavity measurements.13 The complex structure of the nasal cavity is more accurately observed on 3D images than on two-dimensional (2D) images, because it is difficult to measure volumetric dimensions and changes in various cross-sectional areas on the basis of lateral or posteroanterior (PA) cephalograms.6 Cone beam computed tomography (CBCT) provides multiplanar images with low dose of radiation and high spatial resolution.14
From the aforementioned perspectives, CBCT was used to evaluate the null hypothesis that the volume and cross-sectional area of the nasal cavity and nasopharynx would not show significant differences before, immediately after, and 1 year after nonsurgical MARME.
MATERIALS AND METHODS
Subjects
Data for 14 patients (10 women, four men) who had undergone MARME at the Department of Orthodontics, Yonsei University Dental Hospital since January 2012 were collected retrospectively. The mean age of the patients was 22.7 ± 3.3 years (range, 18.3–26.5 years). The inclusion criteria were: young adults (>18 years of age) with a transverse discrepancy,15 successful opening of the midpalatal suture, non-extraction treatment, and availability of CBCT images obtained before expansion (T0), immediately after expansion (T1), and 1 year after expansion (retention period; T2), with a field of view (FOV) covering the entire nasal cavity. The exclusion criteria were: a history of orthodontic treatment, surgical procedure for the maxillary region including Le Fort I osteotomy during T0–T2, history of rhinitis during T0-T2, and presence of craniofacial anomalies or systemic diseases.
The MARME appliance was fabricated by modifying the conventional four-banded Hyrax RME appliance.2 Orthodontic miniscrews (Orlus, Ortholusion, Seoul, Korea) with a 1.8 mm collar diameter and 7 mm length were placed at the center of the helical hooks (Figure 1). Maxillary expansion was initiated the day after placement of the MARME appliance, which was activated once a day (0.2 mm/turn) until the required expansion was achieved. The mean duration of expansion was 28 days (range, 18–35 days), and the mean amount of expansion was 6.8 mm (range, 4.8–8.8 mm). CBCT was performed before expansion and within 5 weeks (mean, 10.71 days; range, 0–35 days) and approximately 14 months (mean, 14.0 months; range, 12.0–15.3 months) after the completion of expansion. The second CBCT images were obtained to determine if there was bone dehiscence after expansion, and the third CBCT images were obtained either for presurgical diagnosis or as post-treatment records. The MARME appliance was maintained for an average of 15.1 weeks after the completion of expansion. This study was approved by the institutional review board of Yonsei University dental hospital (IRB No. 2-2015-0020).
Figure 1.

Miniscrew-assisted rapid maxillary expander before (left) and immediately after (right) expansion.
Measurements
The CBCT device (Alphard VEGA, ASAHI Roentgen IND, Kyoto, Japan) was set at 8.0 mA and 80 kV, and images were captured for 17 s with a 0.3 mm voxel size (FOV, 100 × 100 mm2 or 154 × 154 mm2). In the lateral view, patients were scanned in an upright position with the Frankfort horizontal (FH) plane parallel to the ground and their midlines aligned with the vertical axis of the machine.16,17 In the frontal view, the head was oriented with the orbital floor parallel to the ground.
The 3D images were imported as Digital Imaging and Communications Medicine (DICOM) files using OnDemand3D software (Cybermed Co., Seoul, Korea). After reorientation with the FH plane parallel to the floor in the sagittal and coronal planes, 3 landmarks were identified [anterior nasal spine (ANS), choanae,18 and the third cervical vertebra (C3)] and 4 reference planes were used (two horizontal and two vertical) to obtain measurements (Table 1 and Figure 2).16 The volumes of the nasal cavity and nasopharynx were separately measured, and the total volume was calculated as the sum of the two volumes using the following procedure. The airway is a space bound by hard and soft tissues. The software used a sculpting procedure to eliminate the hard and soft tissues and preserved the required region by deleting unnecessary structures. Then, threshold values were adjusted to eliminate imaging artifacts and refine the selected region. Consequently, the airway volume could be measured in cubic millimeters. The nasal cavity was defined as the region bound superiorly by the FH plane, anteriorly by the ANS-perp. plane, laterally by the orifice of the maxillary sinus, and posteriorly by the choanae plane.19 The nasopharynx was bound superiorly by the choanae plane and inferiorly by the C3 plane.17 In addition, the cross-sectional area of the airway was measured in three different planes: ANS-perp. plane, choanae plane, and C3 plane (Figures 2C, D, and E). Each area was measured using the smart pen, which is a measuring tool provided by the software manufacturer and can automatically trace the border between soft tissue and airway.
Table 1.
Definition of Landmarks and Reference Planes Used for the Assessment of Changes in Dimensions of the Nasal Airway After Nonsurgical Miniscrew-Assisted Rapid Maxillary Expansion
| Definition |
Description |
| Landmark | |
| ANS | Anterior nasal spine: a bony protrusion extending forward at the base of the nasal aperture |
| Choanae | The choanae are bounded medially by the vomer, inferiorly by the horizontal plate of the palatine bone, laterally by the medial pterygoid plate, and superiorly by the body of the sphenoid bone1 |
| C3 | The most inferior and anterior point on the third cervical vertebra |
| Reference planes | |
| FH plane | Frankfort horizontal plane, which is determined by both porions and left orbitale |
| C3 plane | Parallel to the FH plane and passing through C3 |
| ANS-perp. plane | Perpendicular to the FH plane and passing through ANS |
| Choanae plane | The plane along the choanae |
ANS, choanae, C3, FH plane, C3 plane, ANS-prep. plane, and choanae plane were identified on two-dimensional lateral cephalograms reconstructed from three-dimensional cone beam computed tomography (CBCT) images.
Figure 2.
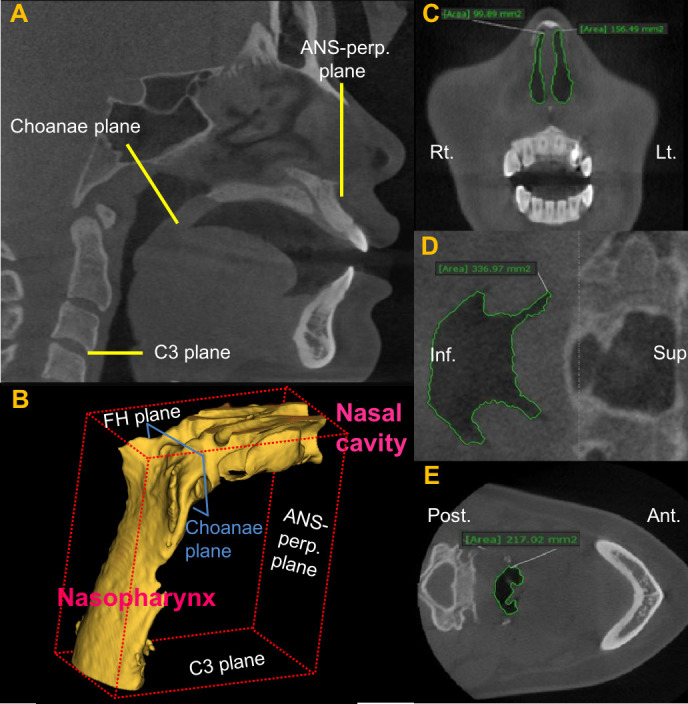
Measurements of the volume and cross-sectional area of the nasal airway using cone beam computed tomography in patients who underwent nonsurgical miniscrew-assisted rapid maxillary expansion. (A) Reconstructed two-dimensional lateral cephalogram for the identification of landmarks and reference planes. (B) Three-dimensional reconstructed nasal airway. (C), (D), (E) Cross-sectional area in the ANS-perp., choanae, and C3 planes, respectively. Please refer to Table 1 for definitions of each landmark and reference plane.
Statistical Analysis
One examiner performed all measurements. To estimate the intraexaminer reliability, seven randomly selected data sets were re-evaluated after a week. The intraclass correlation coefficient (ICC) showed high reliability (ICC > 0.90). The Shapiro–Wilk test was used to determine normality of the data. As all data showed normal distribution, paired t-tests were used to compare changes from T0 to T1, T1 to T2, and T0 to T2. A P-value <0.05 was considered statistically significant. SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
RESULTS
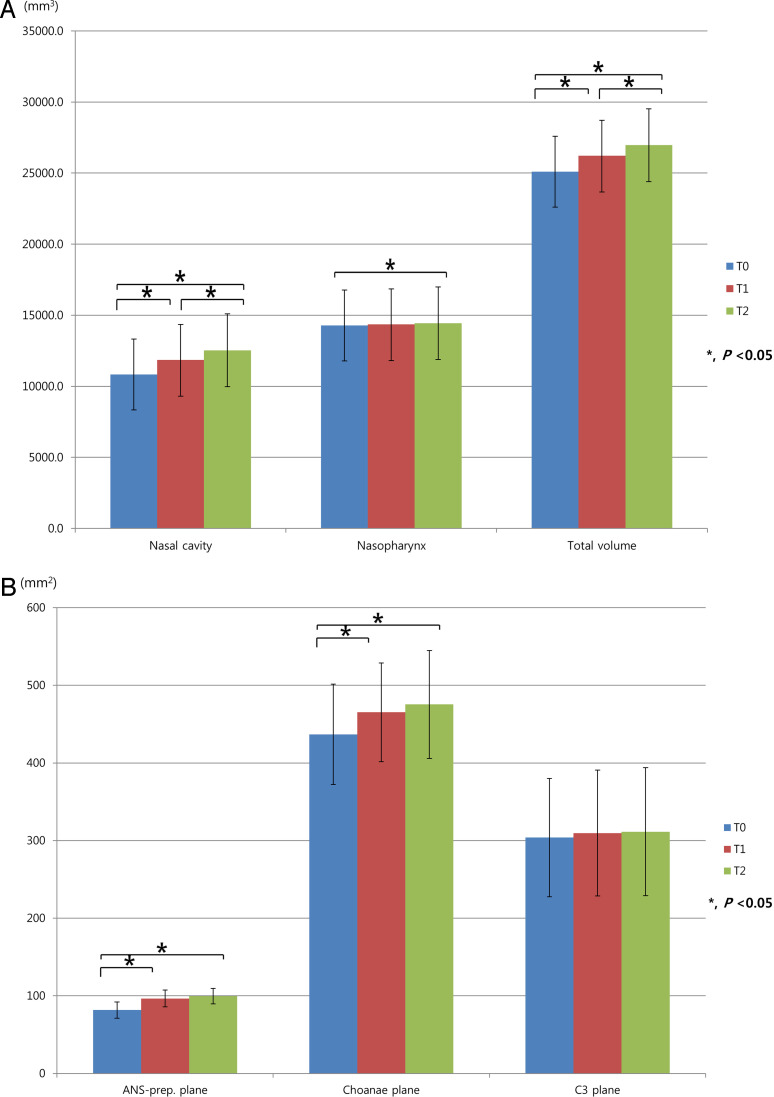
The average volume of the nasal cavity before MARME was 10,822.6 mm3, which increased by 1061.6 mm3 immediately after expansion (P < 0.05), with an additional increase of 648.6 mm3 during the 1 year after expansion (P < 0.05; Table 2 and Figure 3A). Consequently, the nasal cavity volume increased by 1710.2 mm3 from T0 to T2 (P < 0.05). The original volume of the nasopharynx was 14,277.0 mm3, and the total average volume was 25,099.6 mm3. Even though the nasopharynx volume did not show a statistically significant increase from T0 to T1 and from T1 to T2 (P > 0.05), the increase of 942.4 mm3 from T0 to T2 was statistically significant (P < 0.05). The total volume of the airway increased by 1575.0 mm3, 1077.7 mm3, and 2652.6 mm3 from T0 to T1, T1 to T2, and T0 to T2, respectively (P < 0.05).
Table 2.
Changes in the Volume and Cross-Sectional Area of the Nasal Airway Before (T0), Immediately After (T1), and 1 Year After (T2) Nonsurgical Miniscrew-Assisted Rapid Maxillary Expansiona*
| n = 14 |
T0 |
Δ T1–T0 |
Δ T2–T1 |
Δ T2–T0 |
| Volume (mm3) | ||||
| Nasal cavity | 10,822.6 ± 2700.5 | 1061.6 ± 613.9* | 648.6 ± 827.2* | 1710.2 ± 881.6* |
| Nasopharynx | 14,277.0 ± 2483.9 | 513.3 ± 727.8 | 429.1 ± 817.2 | 942.4 ± 821.0* |
| Total volume | 25,099.6 ± 3427.8 | 1575.0 ± 881.8* | 1077.7 ± 923.7* | 2652.6 ± 221.2* |
| Area (mm2) | ||||
| ANS-perp. plane | 81.6 ± 10.4 | 14.6 ± 17.5* | 7.4 ± 12.6 | 22.0 ± 15.4* |
| Choanae plane | 436.8 ± 64.6 | 31.6 ± 34.9* | 12.6 ± 45.5 | 44.2 ± 47.8* |
| C3 plane | 303.8 ± 76.2 | 9.0 ± 83.3 | 20.0 ± 49.6 | 29.0 ± 89.7 |
Figure 3.
Changes in the volume (A) and cross-sectional area (B) of the airway as measured using cone beam computed tomography before (T0), immediately after (T1), and 1 year after (T2) nonsurgical miniscrew-assisted rapid maxillary expansion in young adults. Please refer to Table 1 for definitions of each landmark and reference plane.
The average cross-sectional area of the airway on the anterior (ANS-perp.), middle (choanae), and posterior (C3) segments before MARME were 81.6, 436.8, and 303.8 mm2, respectively. The cross-sectional area of the airway in the anterior and middle segments showed a significant increase of 14.6 mm2 and 31.6 mm2, respectively, from T0 to T1 (P < 0.05; Table 2 and Figure 3B). The increase from T0 to T2 was also significant (P < 0.05; Table 2 and Figure 3B). The cross-sectional area of the posterior segment showed no significant changes throughout the observation period (P > 0.05).
DISCUSSION
MARME has been proven effective for skeletal and dental expansion in young adults, and the skeletal changes were maintained even after removal of the appliance.3,20 The present study demonstrated that nonsurgical maxillary expansion contributed to an increase in the volume and cross-sectional area of the nasal airway in young adults. The volume and area mainly increased in the nasal cavity, and this increase was maintained for 1 year after expansion; in contrast, the increase in the nasopharynx was not evident.
Maxillary constriction is a clinically significant factor for OSA because a low tongue position may cause narrowing of the pharynx.7,21,22 In previous studies, the apnea–hypopnea index values decreased after conventional RME in children, with a stable outcome at the 12-year follow-up.23,24 Several studies have shown that even minor changes in the anterior nasal volume can contribute to a decrease in the respiratory airway resistance.5,10 Furthermore, an increase in the cross-sectional area can facilitate easy breathing.25 MARME, which was performed for young adults in the present study, appeared to have similar effects on the nasal cavity and airway.
Previously, 2D analyses based on lateral cephalograms have been used to measure airway changes primarily in the pharyngeal area.26 With 2D modalities, volumetric measurement, which plays a crucial role with regard to airway flow, is not feasible. In addition, assessment of the anterior nasal airway is barely possible. Some studies have investigated changes in the volume and cross-sectional area of the nasal airway using AR.27,28 However, the data obtained by AR may not be reliable because of possible errors caused by temperature, surrounding noise, or decongestants.28 CBCT, which is not influenced by these factors, can demonstrate the structures of the nasal airway more accurately. Because of the complex structure of the nasal cavity, previous studies using CBCT images have evaluated changes in the posterior pharyngeal airway, not the anterior segment.13,17 Even though computed tomography (CT) images were used to measure the volume of the nasal cavity after SARME, the total volume was calculated by integration of each cross-sectional area,5 which may be a less accurate method compared with direct assessment. In the present study, the airway structures in the nasal cavity and nasopharyngeal area were delineated by manually deleting all hard tissues; this is probably more reliable than the previous methods.
In the present study, the volume of the nasal cavity and nasopharynx increased after MARME and was maintained during the retention period. While the nasal cavity volume increased by 9.9%, 5.5%, and 15.4% from T0 to T1, T1 to T2, and T0 to T2, respectively, that of the nasopharynx increased by 6.4%, 4.1%, and 10.5%, respectively. The additional increase during the retention period seems to be a result of adaptation of the lateral walls of the nasal cavity, which were displaced immediately after expansion.
It should be noted that the increase in volume was more evident in the nasal cavity than in the nasopharynx. This is probably because the position of the appliance, which was below the nasal cavity, would have directly influenced changes in the nasal cavity. Conversely, the nasopharynx volume would not be directly affected because of resistance from the zygomatic buttress and pterygomaxillary junction.29,30 The increase in the cross-sectional area showed a similar trend; the anterior segment showed a greater increase compared with the posterior segment, with a T0–T2 increase of 31.3%, 9.5%, and 6.1% in the anterior, middle, and posterior segments, respectively.
After SARME, the nasal cavity volume was found to increase by 17.9%–23.3% when measured using AR10,12 and 5.1% when measured using CT.5,27 In the present study, the increase measured on CBCT was 15.3% after MARME. These discrepancies can be attributed to differences in the expansion modality, measurement tool, definition of the nasal cavity volume, and duration of retention. Similar to that after MARME, the increase in the nasopharynx area after SARME was not significant.31,32 However, conventional RME led to a 25.9% increase in the pharynx volume,13 probably because of growth and differences in patient age.
The present study showed that MARME might be helpful in improving breathing through an increase in the airway dimensions, which are maintained even after removal of the appliance. However, a control group could not be enrolled in this study because of ethical issues. Also, the sample size was small, and measurements could not be analyzed according to age or sex, even though the data showed normal distribution. Last, morphometric changes in the airway were demonstrated which may not be directly related to functional aspects. Future studies should investigate the kinetic aspect of changes in the airway after nonsurgical maxillary expansion in young adults using computational fluid mechanics methods. Such simulations can predict the respiratory efficacy and detect inflammatory regions.33 It is planned to apply such analyses to MARME-treated patients to not only evaluate volumetric changes, but also to understand the patient-specific change in physics caused by the anatomical modification.
CONCLUSIONS
In conclusion, the null hypothesis was rejected. After nonsurgical maxillary expansion in young adults, the volume and cross-sectional area of the nasal cavity showed a significant increase, with an additional increase in volume during the 1-year retention period.
Moreover, the volume of the nasopharynx showed a significant increase at 1 year after the completion of expansion. The increase in the nasal cavity was larger than that in the nasopharynx throughout the observation period.
Collectively, these results suggest that MARME can be a helpful modality to improve breathing in young adults with maxillary constriction.
ACKNOWLEDGMENT
This study was supported by a faculty research grant of Yonsei University College of Dentistry for 6-2017-0018.
REFERENCES
- 1.Rungcharassaeng K, Caruso JM, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e421–428. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 2.Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010;137:830–839. doi: 10.1016/j.ajodo.2007.10.065. [DOI] [PubMed] [Google Scholar]
- 3.Choi SH, Shi KK, Cha JY, Park YC, Lee KJ. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016;86:713–720. doi: 10.2319/101415-689.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seto BH, Gotsopoulos H, Sims MR, Cistulli PA. Maxillary morphology in obstructive sleep apnoea syndrome. Eur J Orthod. 2001;23:703–714. doi: 10.1093/ejo/23.6.703. [DOI] [PubMed] [Google Scholar]
- 5.Deeb W, Hansen L, Hotan T, Hietschold V, Harzer W, Tausche E. Changes in nasal volume after surgically assisted bone-borne rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2010;137:782–789. doi: 10.1016/j.ajodo.2009.03.042. [DOI] [PubMed] [Google Scholar]
- 6.El H, Palomo JM. Three-dimensional evaluation of upper airway following rapid maxillary expansion: a CBCT study. Angle Orthod. 2014;84:265–273. doi: 10.2319/012313-71.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Villa MP, Rizzoli A, Miano S, Malagola C. Efficacy of rapid maxillary expansion in children with obstructive sleep apnea syndrome: 36 months of follow-up. Sleep Breath. 2011;15:179–184. doi: 10.1007/s11325-011-0505-1. [DOI] [PubMed] [Google Scholar]
- 8.Villa MP, Castaldo R, Miano S, et al. Adenotonsillectomy and orthodontic therapy in pediatric obstructive sleep apnea. Sleep Breath. 2014;18:533–539. doi: 10.1007/s11325-013-0915-3. [DOI] [PubMed] [Google Scholar]
- 9.Souki BQ, Pimenta GB, Souki MQ, Franco LP, Becker HM, Pinto JA. Prevalence of malocclusion among mouth breathing children: do expectations meet reality? Int J Pediatr Otorhinolaryngol. 2009;73:767–773. doi: 10.1016/j.ijporl.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Wriedt S, Kunkel M, Zentner A, Wahlmann UW. Surgically assisted rapid palatal expansion. An acoustic rhinometric, morphometric and sonographic investigation. J Orofac Orthop. 2001;62:107–115. doi: 10.1007/pl00001921. [DOI] [PubMed] [Google Scholar]
- 11.Nada RM, van Loon B, Schols JG, et al. Volumetric changes of the nose and nasal airway 2 years after tooth-borne and bone-borne surgically assisted rapid maxillary expansion. Eur J Oral Sci. 2013;121:450–456. doi: 10.1111/eos.12068. [DOI] [PubMed] [Google Scholar]
- 12.Kunkel M, Hochban W. Acoustic rhinometry: a new diagnostic procedure–experimental and clinical experience. Int J Oral Maxillofac Surg. 1994;23:409–412. doi: 10.1016/s0901-5027(05)80032-3. [DOI] [PubMed] [Google Scholar]
- 13.Chang Y, Koenig LJ, Pruszynski JE, Bradley TG, Bosio JA, Liu D. Dimensional changes of upper airway after rapid maxillary expansion: a prospective cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2013;143:462–470. doi: 10.1016/j.ajodo.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 14.Kiljunen T, Kaasalainen T, Suomalainen A, Kortesniemi M. Dental cone beam CT: A review. Phys Med. 2015;31:844–860. doi: 10.1016/j.ejmp.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Vanarsdall RL., Jr Transverse dimension and long-term stability. Semin Orthod. 1999;5:171–180. doi: 10.1016/s1073-8746(99)80008-5. [DOI] [PubMed] [Google Scholar]
- 16.Kim YJ, Hong JS, Hwang YI, Park YH. Three-dimensional analysis of pharyngeal airway in preadolescent children with different anteroposterior skeletal patterns. Am J Orthod Dentofacial Orthop. 2010. 137:306 e301-311; discussion 306-307. [DOI] [PubMed]
- 17.Park JW, Kim NK, Kim JW, Kim MJ, Chang YI. Volumetric, planar, and linear analyses of pharyngeal airway change on computed tomography and cephalometry after mandibular setback surgery. Am J Orthod Dentofacial Orthop. 2010;138:292–299. doi: 10.1016/j.ajodo.2009.10.036. [DOI] [PubMed] [Google Scholar]
- 18.Pagano AS, Laitman JT. Three-dimensional geometric morphometric analysis of the nasopharyngeal boundaries and its functional integration with the face and external basicranium among extant hominoids. Anat Rec (Hoboken) 2015;298:85–106. doi: 10.1002/ar.23076. [DOI] [PubMed] [Google Scholar]
- 19.Wetmore RF, Mahboubi S. Computed tomography in the evaluation of choanal atresia. Int J Pediatr Otorhinolaryngol. 1986;11:265–274. doi: 10.1016/s0165-5876(86)80038-6. [DOI] [PubMed] [Google Scholar]
- 20.Lin L, Ahn HW, Kim SJ, Moon SC, Kim SH, Nelson G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:253–262. doi: 10.2319/030514-156.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1–132. [PubMed] [Google Scholar]
- 22.Katyal V, Pamula Y, Daynes CN, et al. Craniofacial and upper airway morphology in pediatric sleep-disordered breathing and changes in quality of life with rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013;144:860–871. doi: 10.1016/j.ajodo.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 23.Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion in children with obstructive sleep apnea syndrome. Sleep. 2004;27:761–766. doi: 10.1093/sleep/27.4.761. [DOI] [PubMed] [Google Scholar]
- 24.Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion (RME) for pediatric obstructive sleep apnea: a 12-year follow-up. Sleep Med. 2015;16:933–935. doi: 10.1016/j.sleep.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 25.Warren DW, Hairfield WM, Seaton DL, Hinton VA. The relationship between nasal airway cross-sectional area and nasal resistance. Am J Orthod Dentofacial Orthop. 1987;92:390–395. doi: 10.1016/0889-5406(87)90259-9. [DOI] [PubMed] [Google Scholar]
- 26.Zhao Y, Nguyen M, Gohl E, Mah JK, Sameshima G, Enciso R. Oropharyngeal airway changes after rapid palatal expansion evaluated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137:S71–78. doi: 10.1016/j.ajodo.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 27.Babacan H, Sokucu O, Doruk C, Ay S. Rapid maxillary expansion and surgically assisted rapid maxillary expansion effects on nasal volume. Angle Orthod. 2006;76:66–71. doi: 10.1043/0003-3219(2006)076[0066:RMEASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Mitsuda ST, Pereira MD, Passos AP, Hino CT, Ferreira LM. Effects of surgically assisted rapid maxillary expansion on nasal dimensions using acoustic rhinometry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:191–196. doi: 10.1016/j.tripleo.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 29.Kilic E, Kilic B, Kurt G, Sakin C, Alkan A. Effects of surgically assisted rapid palatal expansion with and without pterygomaxillary disjunction on dental and skeletal structures: a retrospective review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:167–174. doi: 10.1016/j.oooo.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 30.Lim HM, Park YC, Lee KJ, Kim KH, Choi YJ. Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion. Korean J Orthod. 2017;47:313–322. doi: 10.4041/kjod.2017.47.5.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pereira-Filho VA, Monnazzi MS, Gabrielli MA, et al. Volumetric upper airway assessment in patients with transverse maxillary deficiency after surgically assisted rapid maxillary expansion. Int J Oral Maxillofac Surg. 2014;43:581–586. doi: 10.1016/j.ijom.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Seeberger R, Kater W, Davids R, Thiele OC. Long term effects of surgically assisted rapid maxillary expansion without performing osteotomy of the pterygoid plates. J Craniomaxillofac Surg. 2010;38:175–178. doi: 10.1016/j.jcms.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 33.Lintermann A, Meinke M, Schroder W. Fluid mechanics based classification of the respiratory efficiency of several nasal cavities. Comput Biol Med. 2013;43:1833–1852. doi: 10.1016/j.compbiomed.2013.09.003. [DOI] [PubMed] [Google Scholar]