Abstract
Objectives:
To compare palatal symmetry, dimensions, and molar angulations following early mixed-dentition slow maxillary expansion with parameters in normal controls.
Materials and Methods:
A total of 30 patients treated with a Haas-type expander for unilateral posterior crossbite with functional shift were compared with 30 controls matched for dental age, gender, and molar relationship. Records were taken before (T1) and after expansion (T2). Palatal width, surface area, volume, and molar angulations were measured on digitized models. Surface area and volume were split in half then divided into anterior, middle, and posterior segments to measure symmetry. Student's t-test was used to assess group differences.
Results:
Mean intercanine width increased 4.65 mm, and intermolar width increased 4.76 mm. The treated mean surface area increased 127.05 mm2 compared with 10.35 mm2 in controls. The treated palatal volume increased 927.55 mm3 compared with 159.89 mm3 for controls. At T1, the controls showed significant differences in surface area and volume between the anterior palatal segments. At T2, this difference occurred in surface area of middle palatal segments of the treated sample. First permanent molars showed an increased buccal and distal inclination after treatment, opposite to controls. The increase in buccal inclination was greater on the crossbite side.
Conclusions:
The Haas-type expander results in similar expansion across the canines and first molars. A palate that is symmetrical before expansion may become asymmetric after expansion but only in the middle segment. Changes in individual molar angulation following palatal expansion can be measured without radiation imaging.
Keywords: Slow expansion, Palatal dimensions, Posterior crossbite
INTRODUCTION
Posterior crossbite from a transverse discrepancy between arches occurs with a prevalence of 8% to 23%.1–3 It affects girls more often than boys and has been attributed to digit habits.4 The majority of unilateral crossbite cases show a functional shift of the lower jaw toward the crossbite side (UPXB).3,5,6 Primary canine interferences usually cause mandibular lateral forced guidance into maximum intercuspation.1,7 The lower midline shift to the crossbite side is associated with this shift.8 Antero-posterior molar relationship asymmetry is found with a Class II on the crossbite side and a Class I on the noncrossbite molar.8
Posterior crossbites with functional shifts should be treated once noticed.9 Untreated unfavorable changes include temporomandibular joint, skeletal and dental asymmetry.8,10,11 Early maxillary expansion treatment allows the permanent teeth to erupt into normal occlusion, eliminating interferences and providing favorable dental and skeletal changes during growth.3,12 Posterior crossbite correction by slow maxillary expansion (SME) in the mixed dentition has shown an 84% stability in the permanent dentition.13
Previous studies of palatal volume and surface area used rapid maxillary expansion (RME) during the mixed and permanent dentitions,14–18 and some mixed-dentition studies lacked controls.14,15 However, only primary dentition studies evaluated palatal changes after SME.19–21 Molar angle measurements on models have been carried out using either the intermolar angle or the buccal inclination of each molar.16,22
The purpose of this study was to evaluate changes in palatal dimensions, symmetry, and molar angulations following SME during the early mixed dentition when compared with untreated normal controls.
MATERIALS AND METHODS
This retrospective case-control study was approved by the ethics board at the University of British Columbia, Vancouver, Canada. A power calculation indicated a sample of 25 patients was required for each group. The calculation was based on a palatal volume assumption of a mean difference of 339.52 mm3 (standard deviation = 427.80) according to Primožič et al.19 using a power of 80% and α = 0.05.
The treatment sample consisted of 30 randomly selected patients from a private orthodontic office being treated for UPXB by a two-banded Haas-type appliance. Records were taken at two time intervals: T1 (before expansion) with a mean dental age of 8 years and T2 (after slow maxillary expansion and retention) with a mean dental age of 9 years. The untreated normal control sample consisted of 30 participants from a collection at the Oregon Health and Sciences University. The untreated control and treated samples were matched for gender, molar relationship, and dental age (Table 1) using the Demirjian and Goldstein method.23
Table 1.
Study Group Comparisonsa
| Group |
N |
Genderb |
Dental Agec |
||
| Male |
Female |
T1, Mean ± SD |
T2, Mean ± SD |
||
| Control sample | 30 | 11 | 19 | 8.30 ± 0.75 | 9.42 ± 0.92 |
| Treatment sample | 30 | 11 | 19 | 8.36 ± 0.70 | 9.47 ± 0.94 |
| Significance | P = 1.00 | P = .890 | P = .860 | ||
T1 indicates before expansion; T2, after expansion; SD, standard deviation.
Gender: male vs female.
Dental age as assessed by Demerjian.23
Treatment sample inclusion criteria were UPXB, mixed-dentition SME, and nonextraction. Exclusion criteria were growth-modification appliances, ectopic palatal lateral incisors, attrition affecting first molar cusps, craniofacial anomalies, eruption of permanent successors (canines and premolars) and poor-quality models.
The expansion protocol was one quarter-turn every 2 days until overcorrection with the maxillary lingual cusps contacting the mandibular buccal cusps. The expander was left passively for retention for a minimum of 6 months. The examiner was blinded for crossbite and noncrossbite sides until all data were collected.
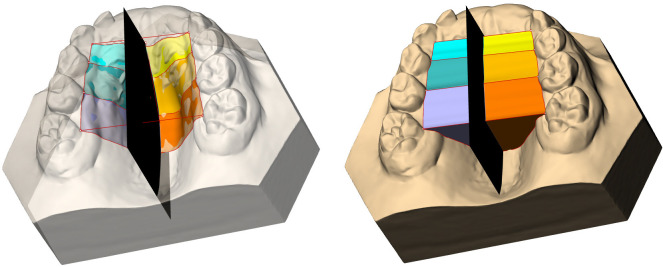
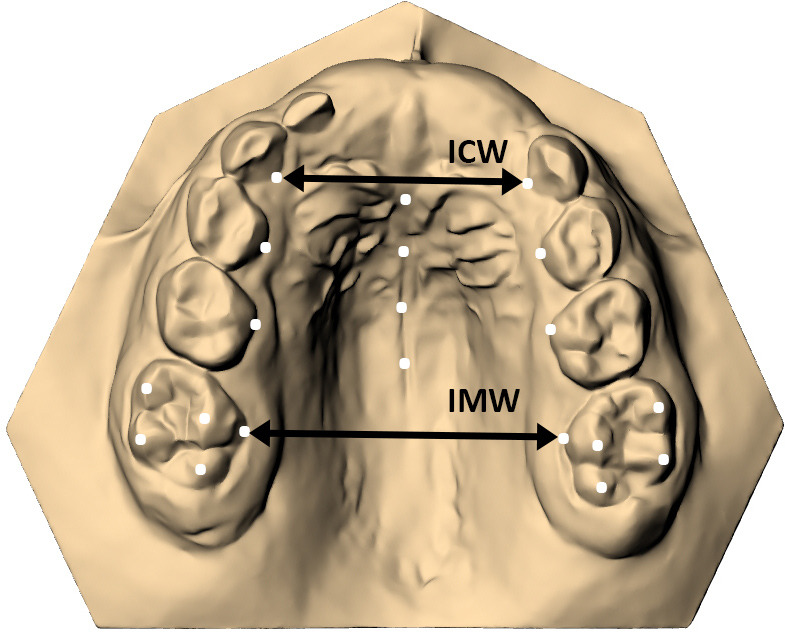
The maxillary models were digitally scanned and then imported and analyzed in Rhino3d v5.0 (Robert McNeel and Associates, Seattle, Wash). For each model, landmarks were identified at the lingual gingival margins of the greatest convexity: from the canines to the first permanent molars, on the four first permanent molar cusp tips, on the mid-distal surface of the incisive papilla, and along the mid-palatal raphe (Figure 1). Intercanine widths (ICWs) and intermolar widths (IMWs) were measured between the canine and first permanent molar landmarks (Figure 1). The palatal surface area was defined with curves through the lingual gingival margin points and on the palatal mesh between homologous dental landmarks. The palatal surface was created from this curve network and divided into six segments. These were defined by the locations of the first primary molar and second primary molars on each side as well as the palatal midline, together representing the anterior, middle, and posterior palatal areas on both sides of the midline (Figure 2). These areas were used to assess palatal symmetry. Palatal volume was derived from the region enclosed by the palatal surface as well as a horizontal plane through the points at the gingival margins of the teeth. This volume was divided in the same manner as the palatal surfaces (Figure 2). Each first molar's buccolingual and mesiodistal angulations were measured first by constructing the normal to a rectilinear planar surface fitted through its molar cusp tips, then by measuring its three-dimensional relationship to the normal of a best-fit horizontal plane through the points defining the palatal gingival margins of the maxillary teeth. Both normals were expressed relative to a common origin at the center of each molar's planar surface, then projected onto lateral and frontal reference planes orthogonal to the horizontal plane. This allowed measurement of the angular differences between the molar and palatal normals (Figure 3).
Figure 1.
Landmark identification on the digitized models and width measurements.
Figure 2.
Palatal surface area and volume divided into six parts.
Figure 3.
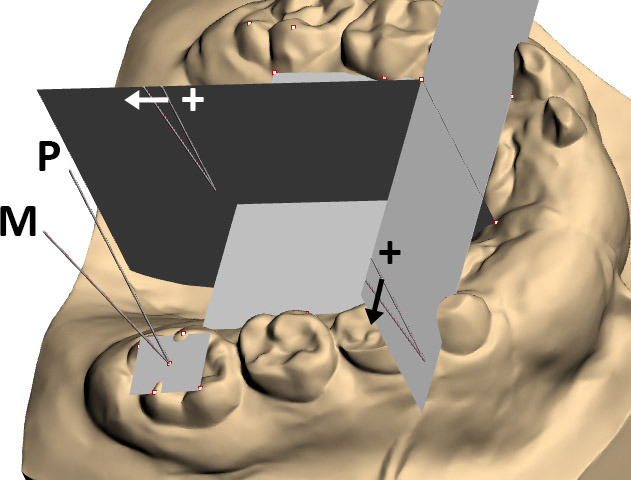
Molar angulations in anteroposterior and transverse planes.
Measurements for the 15 models were repeated 1 week apart to assess intraexaminer agreement. The agreement was examined by an independent sample t-test (P < .05) and intraclass correlation (P < .05). Data distribution was assessed statistically for normality; because the skewness and kurtosis values did not exceed ±1.96, parametric statistics were used thereafter. An independent sample t-test was used to assess the differences between the treatment and control groups; two-tailed dependent t-tests were used to compare sides and differences within the groups with a threshold for statistical significance of P < .05.
RESULTS
The results are summarized in Table 2. The range of intraclass correlation coefficients showed good to excellent intraexaminer agreement of 0.7 to 1.0. Similarly, a t-test showed no significant differences between the means of the first and second measurements.
Table 2.
Measurements Performeda
| Variable |
Treatment Group (n = 30) |
T2–T1 |
Control Group (n = 30b) |
T2–T1 |
Tx vs Control (P Valued) |
|||
| T1 | T2 |
P Valuec |
T1 | T2 |
P Valuec |
T1 |
T2 |
|
| Mean ± SD |
Mean ± SD |
Mean ± SD |
Mean ± SD |
|||||
| Intercanine width (mm) | 22.74 ± 2.15 | 27.39 ± 2.05 | <.001* | 24.35 ± 2.04 | 24.92 ± 2.17 | .294 | .004* | <.001* |
| Intermolar width (mm) | 30.32 ± 2.80 | 35.08 ± 3.03 | <.001* | 30.75 ± 2.20 | 31.22 ± 2.40 | .432 | .510 | <.001* |
| Total surface area (mm2) | 832.98 ± 88.90 | 960.03 ± 97.62 | <.001* | 858.33 ± 70.60 | 869.19 ± 84.23 | .602 | .227 | <.001* |
| Surface area anterior halves (mm2) | ||||||||
| Crossbite side | 103.3 ± 15.74 | 126.86 ± 21.88 | <.001* | 107.1 ± 18.77* | 107.5 ± 20.05 | .937 | .400 | .001* |
| Noncrossbite side | 103.83 ± 15.85 | 125.99 ± 20.42 | <.001* | 110.35 ± 18.80* | 109.17 ± 20.42 | .822 | .152 | .003* |
| Surface area middle halves (mm2) | ||||||||
| Crossbite side | 131.85 ± 18.43 | 146.98 ± 17.81* | <.001* | 134.83 ± 16.84 | 135.35 ± 16.59 | .907 | .517 | .013* |
| Noncrossbite side | 129.09 ± 17.22 | 143.46 ± 17.66* | .002* | 135.40 ± 17.8 | 136.23 ± 16.52 | .856 | .168 | .116 |
| Surface area posterior halves (mm2) | ||||||||
| Crossbite side | 183.14 ± 21.22 | 210.31 ± 22.62 | <.001* | 184.71 ± 16.30 | 191.26 ± 20.17 | .187 | .749 | .001* |
| Noncrossbite side | 180.67 ± 21.23 | 205.94 ± 18.38 | <.001* | 186.78 ± 17.00 | 189.46 ± 20.74 | .598 | .224 | .003* |
| Volume (mm3) | 3654.25 ± 726.32 | 4581.80 ± 838.76 | <.001* | 3922.20 ± 605.20 | 4082.76 ± 726.42 | .372 | .126 | .019* |
| Volume anterior halves (mm3) | ||||||||
| Crossbite side | 299.00 ± 95.00 | 414.60 ± 117.63 | <.001* | 326.50 ± 108.27* | 343.44 ± 112.44 | .566 | .300 | .023* |
| Noncrossbite side | 298.88 ± 85.55 | 414.99 ± 124.25 | <.001* | 337.15 ± 110.41* | 344.05 ± 116.11 | .819 | .139 | .030* |
| Volume middle halves (mm3) | ||||||||
| Crossbite side | 580.82 ± 154.83 | 714.23 ± 168.88 | .002* | 632.44 ± 126.48 | 648.60 ± 128.03 | .634 | .163 | .102 |
| Noncrossbite side | 576.36 ± 130.13 | 701.84 ± 153.74 | .001* | 642.06 ± 127.85 | 651.34 ± 132.44 | .789 | .053 | .188 |
| Volume posterior halves (mm3) | ||||||||
| Crossbite side | 958.18 ± 210.44 | 1191.28 ± 237.81 | <.001* | 983.99 ± 145.01 | 1047.76 ± 182.81 | .154 | .583 | .013* |
| Noncrossbite side | 940.59 ± 179.54 | 1154.04 ± 185.99 | <.001* | 1000.01 ± 146.13 | 1050.12 ± 192.62 | .278 | .165 | .044* |
| Molar angulation (°) | ||||||||
| Bucco-lingual angle (°) | ||||||||
| Crossbite side | 12.66 ± 5.77 | 17.08 ± 6.79* | .009* | 12.76 ± 3.77 | 12.04 ± 4.13 | .488 | .942 | .001* |
| Noncrossbite side | 11.16 ± 4.13 | 14.01 ± 5.72* | .031* | 12.93 ± 4.06 | 11.76 ± 5.11 | .338 | .101 | .117 |
| Mesio-distal angle (°) | ||||||||
| Crossbite side | 4.03 ± 4.05 | 8.40 ± 5.51 | .001* | 4.31 ± 3.31 | 2.90 ± 3.13 | .096 | .766 | <.001* |
| Noncrossbite side | 4.43 ± 4.25 | 8.93 ± 5.46 | .001* | 4.24 ± 4.06 | 2.58 ± 3.36 | .066 | .85 | <.001* |
T1 indicates before expansion; T2, after expansion; Tx, treatment; SD, standard deviation.
Control sample had n = 27 at T2 for the surface area and volume measurements and n = 29 for the molar angulation measurements.
Paired sample t-test.
Independent t-test.
Significant differences, P < .05.
The control sample was decreased to 27 cases at T2 for the palatal surface area and volume measurements due to one case with a large defect visible in the palate and first premolar eruption in two other cases. For the molar angle, one case was excluded because the first permanent molars were still erupting at T1.
The mean pretreatment ICW was significantly less in the treatment cases than in controls, whereas postexpansion it became significantly greater. The mean IMW in the treatment group at T1 was less than in controls, but not statistically significantly different; at T2, it became significantly greater.
The mean total surface area and volume in the treatment group at T1 was smaller than the controls, but not statistically significantly different. Postexpansion of the surface area and volume became significantly larger in the treatment group than controls.
When the palatal surface areas and volumes on the crossbite and noncrossbite sides (right and left sides for controls) were compared, there were significant differences for the anterior segments in the control group at T1 and the surface areas in the middle segments for the treatment group at T2.
The mean bucco-lingual angle (BLA) on the crossbite and noncrossbite sides pretreatment were not significantly different than the controls. After expansion, the mean BLA on the crossbite side was significantly larger than that in the controls, and the noncrossbite side showed no difference. The mean increase in the BLA from treatment on the crossbite and noncrossbite sides were 4.41° and 2.86°, respectively, which was statistically significantly different. In the control group from T1 to T2 there was a decrease in BLA on both sides, neither statistically significant.
The mean mesio-distal angles (MDA) on each side at T1 were similar between groups. After expansion, the mean MDA on both sides were significantly larger than the controls. The mean increase in MDA on the crossbite side from T1 to T2 in the treatment group was 4.38° on average, whereas on the noncrossbite side it changed by 4.51°; both increases were significant. In the control group, there was a nonsignificant decrease in the MDA on both sides. When the BLA and MDA were compared between the crossbite and noncrossbite sides for both time intervals, the only significant difference was observed in the BLA in the treatment group at T2.
DISCUSSION
The findings revealed changes in palatal dimensions and symmetry following early mixed-dentition SME with a Haas-type appliance.
The pretreatment ICW was significantly less than the control group. After expansion, the ICW increased by 4.65 mm, and this was significantly greater than controls, similar to Wong et al.24 The mean ICW increase was greater than that reported for other mixed-dentition unilateral posterior crossbite SME and RME patients treated with the RME Hyrax appliance, expansion plates, or a quadhelix.22,25–28 The current findings were similar to those reported for a mixed-dentition acrylic splint RME.29 In general, the ICW using SME is in accordance with previous studies with RME.
The pre-expansion IMW was not significantly less than the controls, whereas after expansion the IMW was statistically greater. The postexpansion IMW was slightly greater than other mixed-dentition SME using a removable appliance or quadhelix.26,30 The IMW was also greater than SME from quadhelix and expansion plates in the older age groups.25 The ICW and IMW increases from expansion were almost identical.
There were no significant differences in surface area between the treatment and control groups pretreatment. The postexpansion surface area was significantly greater than the controls. The treatment group showed smaller surface areas at both time intervals when compared with other studies, likely due to a different measurement method, appliances, and patient age.16,17 The surface area reported by Primožič et al.20 was less than the current study at both intervals. They also used an untreated control group, but at T2 the control group had slightly greater surface area than the treatment group, contrary to the current study observations. The appliance used, patient age, the timing of records, and methodology all differed from the current study.20 In another report by Primožič et al., the surface area was slightly greater in the treatment group than in the control group at T2.21
Palatal symmetry showed differences in the anterior halves of the control group at T1 and the middle halves of the treatment group postexpansion. Although statistically significant, the differences may not be clinically relevant as the mean difference was approximately 3 mm2. Primožič et al. assessed symmetry by measuring the percentage of overlap between the original surface area and a mirror image of the original surface area and reported symmetrical palates.20
The palatal volume before expansion was smaller, but not significantly different from the control group. After expansion, the volume was greater than the control group, similar to Primožič et al.21 Palatal volume for the treatment group was smaller than reported by De Felippe et al.17 and Gohl et al.18 The cause of these differences is likely similar to the factors affecting surface area. This study is the first to assess asymmetry by comparing the volumes of homologous palatal segments. It found no differences in the treatment group and a significant difference only in the anterior region of the control group at T1. This difference may be considered not clinically significant as the mean difference was approximately 11 mm3.
In the current study, individual buccolingual and mesiodistal molar angulations on the crossbite and noncrossbite sides were measured directly on the digitized models, which avoided use of Posteroanterior head films or Cone Beam Computed Tomography radiology. Although an independent reference such as the cranial base would be ideal for measuring changes in molar orientation, radiation hygiene suggests that it would be unethical to take consecutive CBCT scans in young children.31 Previously, molar buccolingual angulation measurements on models have included either the intermolar angle or the inclination of each molar defined by two cusp tips.16,22 The intermolar angle method, however, does not disclose any differences between homologous molars, and the use of two cusps as a reference line cannot reveal each molar's three-dimensional orientation. Both were possible in the present study.
The crossbite side increased its BLA more than the noncrossbite side. The significant increase in BLA for the treated crossbite side may be attributed to the elimination of the crossbite, freeing up potential pretreatment dental compensation. The Haas group in Oliveira et al.16 increased molar inclination from T1 to T2 by approximately 7°, which was greater than the current study.16 Kılıç et al.32 found an increase of approximately 7° for the acrylic-bonded group and 9° for the Hyrax group, which was greater than in this study. This difference can be attributed to differences in ages, appliances, activation rates, and methods used.16,32
Sari et al.33 measured mixed-dentition increases in intermolar angle of 5.5° per side, which is greater than the current study. For the permanent dentition group, the combined angle was 5° (2.5° for each molar) similar to the current findings on the noncrossbite side, but less than the crossbite side.33 Handelman et al.22 also measured the intermolar angle and noted in children an increase that was less than the current study; this is possibly due to age differences, different activation rates, and measurement methods. In early mixed-dentition unilateral crossbite cases, Wong et al.24 found a mean increase in the buccal angle of each molar about 2°, which was less than the current study. For the controls in this study, there was a decrease in the buccal angulation from T1 to T2, and this matches the report of maxillary molars uprighting with age from Marshall et al.34
No studies are available to compare the findings related to MDA angles. The increase in MDA following expansion was an unexpected finding, and the mechanism is unknown.
The retrospective nature of this study could be considered a limitation. A more reliable approach in the future would be a random prospective design.
CONCLUSIONS
Using SME with a Haas-type expander in the early mixed dentition resulted in the following:
Similar expansion was found across the canines and molars.
Pretreatment surface areas and volumes that were smaller than the untreated controls became significantly larger after expansion.
Surface areas in the palate were bilaterally similar, except for the central postexpansion region.
Increased inclination was noted of the first permanent molars buccally and distally, whereas the controls showed a decrease in both inclinations.
There was a greater mean increase in the buccal inclination of the treated first permanent molar on the crossbite side when compared with the noncrossbite side.
ACKNOWLEDGMENTS
We thank the staff who helped with the collection of the control sample (Oregon Health & Science University).
REFERENCES
- 1.Kutin G, Hawes RR. Posterior cross-bites in the deciduous and mixed dentitions. Am J Orthod. 1969;56:491–504. doi: 10.1016/0002-9416(69)90210-3. [DOI] [PubMed] [Google Scholar]
- 2.Thilander B, Myrberg N. The prevalence of malocclusion in Swedish schoolchildren. Scand J Dent Res. 1973;81:12–20. doi: 10.1111/j.1600-0722.1973.tb01489.x. [DOI] [PubMed] [Google Scholar]
- 3.Kurol J, Berglund L. Longitudinal study and cost-benefit analysis of the effect of early treatment of posterior cross-bites in the primary dentition. Eur J Orthod. 1992;14:173–179. doi: 10.1093/ejo/14.3.173. [DOI] [PubMed] [Google Scholar]
- 4.Johnson ED, Larson BE. Thumb-sucking: literature review. ASDC J Dent Child. 1993;60:385–391. [PubMed] [Google Scholar]
- 5.Thilander B, Wahlund S, Lennartsson B. The effect of early interceptive treatment in children with posterior cross-bite. Eur J Orthod. 1984;6:25–34. doi: 10.1093/ejo/6.1.25. [DOI] [PubMed] [Google Scholar]
- 6.Lindner A, Modéer T. Relation between sucking habits and dental characteristics in preschoolchildren with unilateral cross-bite. Eur J Oral Sci. 1989;97:278–283. doi: 10.1111/j.1600-0722.1989.tb01613.x. [DOI] [PubMed] [Google Scholar]
- 7.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics 4th ed. St. Louis, MO: Mosby Elsevier;; 2007. 437. [Google Scholar]
- 8.Hesse KL, Årtun J, Joondeph DR, Kennedy DB. Changes in condylar position and occlusion associated with maxillary expansion for correction of functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1997;111:410–418. doi: 10.1016/s0889-5406(97)80023-6. [DOI] [PubMed] [Google Scholar]
- 9.Binder RE. Correction of posterior crossbites: diagnosis and treatment. Pediatr Dent. 2004;26:266–272. [PubMed] [Google Scholar]
- 10.Nerder PH, Bakke M, Solow B. The functional shift of the mandible in unilateral posterior crossbite and the adaptation of the temporomandibular joints: a pilot study. Eur J Orthod. 1999;21:155–166. doi: 10.1093/ejo/21.2.155. [DOI] [PubMed] [Google Scholar]
- 11.O'Byrn BL, Sadowsky C, Schneider B, BeGole EA. An evaluation of mandibular asymmetry in adults with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1995;107:394–400. doi: 10.1016/s0889-5406(95)70092-7. [DOI] [PubMed] [Google Scholar]
- 12.Bell RA. A review of maxillary expansion in relation to rate of expansion and patient's age. Am J Orthod. 1982;81:32–37. doi: 10.1016/0002-9416(82)90285-8. [DOI] [PubMed] [Google Scholar]
- 13.Huynh T, Kennedy DB, Joondeph DR, Bollen A. Treatment response and stability of slow maxillary expansion using Haas, hyrax, and quad-helix appliances: a retrospective study. Am J Orthod Dentofacial Orthop. 2009;136:331–339. doi: 10.1016/j.ajodo.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 14.Marini I, Bonetti GA, Achilli V, Salemi G. A photogrammetric technique for the analysis of palatal three-dimensional changes during rapid maxillary expansion. Eur J Orthod. 2007;29:26–30. doi: 10.1093/ejo/cji069. [DOI] [PubMed] [Google Scholar]
- 15.Muchitsch AP, Winsauer H, Wendl B, et al. Remodelling of the palatal dome following rapid maxillary expansion (RME): laser scan-quantifications during a low growth period. Orthod Craniofac Res. 2012;15:30–38. doi: 10.1111/j.1601-6343.2011.01534.x. [DOI] [PubMed] [Google Scholar]
- 16.Oliveira NL, Da Silveira AC, Kusnoto B, Viana G. Three-dimensional assessment of morphologic changes of the maxilla: A comparison of 2 kinds of palatal expanders. Am J Orthod Dentofacial Orthop. 2004;126:354–362. doi: 10.1016/j.ajodo.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 17.De Felippe O, Nanci L, Da Silveira AC, et al. Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short- and long-term effects. Am J Orthod Dentofacial Orthop. 2008;134:370–382. doi: 10.1016/j.ajodo.2006.10.034. [DOI] [PubMed] [Google Scholar]
- 18.Gohl E, Nguyen M, Enciso R. Three-dimensional computed tomography comparison of the maxillary palatal vault between patients with rapid palatal expansion and orthodontically treated controls. Am J Orthod Dentofacial Orthop. 2010;138:477–485. doi: 10.1016/j.ajodo.2008.12.025. [DOI] [PubMed] [Google Scholar]
- 19.Primožič J, Ovsenik M, Richmond S, Kau CH, Zhurov A. Early crossbite correction: a three-dimensional evaluation. Eur J Orthod. 2009;31:352–356. doi: 10.1093/ejo/cjp041. [DOI] [PubMed] [Google Scholar]
- 20.Primožic J, Baccetti T, Franchi L, Richmond S, Farčnik F, Ovsenik M. Three-dimensional assessment of palatal change in a controlled study of unilateral posterior crossbite correction in the primary dentition. Eur J Orthod. 2013;35:199–204. doi: 10.1093/ejo/cjr125. [DOI] [PubMed] [Google Scholar]
- 21.Primožič J, Richmond S, Kau CH, Zhurov A, Ovsenik M. Three-dimensional evaluation of early crossbite correction: a longitudinal study. Eur J Orthod. 2013;35:7–13. doi: 10.1093/ejo/cjq198. [DOI] [PubMed] [Google Scholar]
- 22.Handelman CS, Wang L, BeGole EA, Haas AJ. Nonsurgical rapid maxillary expansion in adults: report on 47 cases using the Haas expander. Angle Orthod. 2000;70:129–144. doi: 10.1043/0003-3219(2000)070<0129:NRMEIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Demirjian A, Goldstein H. New systems for dental maturity based on seven and four teeth. Ann Hum Biol. 1976;3:411–421. doi: 10.1080/03014467600001671. [DOI] [PubMed] [Google Scholar]
- 24.Wong CA, Sinclair PM, Keim RG, Kennedy DB. Arch dimension changes from successful slow maxillary expansion of unilateral posterior crossbite. Angle Orthod. 2011;81:616–623. doi: 10.2319/072210-429.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bjerklin K. Follow-up control of patients with unilateral posterior cross-bite treated with expansion plates or the quad-helix appliance. J Orofac Orthop. 2000;61:112–124. doi: 10.1007/BF01300353. [DOI] [PubMed] [Google Scholar]
- 26.Petrén S, Bondemark L. Correction of unilateral posterior crossbite in the mixed dentition: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008;133:790.e7–790.e13. doi: 10.1016/j.ajodo.2007.11.021. [DOI] [PubMed] [Google Scholar]
- 27.Lamparski DG, Rinchuse DJ, Close JM, Sciote JJ. Comparison of skeletal and dental changes between 2-point and 4-point rapid palatal expanders. Am J Orthod Dentofacial Orthop. 2003;123:321–328. doi: 10.1067/mod.2003.10. [DOI] [PubMed] [Google Scholar]
- 28.Adkins MD, Nanda RS, Currier GF. Arch perimeter changes on rapid palatal expansion. Am J Orthod Dentofacial Orthop. 1990;97:194–199. doi: 10.1016/S0889-5406(05)80051-4. [DOI] [PubMed] [Google Scholar]
- 29.Spillane LM, McNamara Jr JA. Maxillary adaptation to expansion in the mixed dentition. Semin Orthod. 1995;1:176–187. doi: 10.1016/s1073-8746(95)80021-2. [DOI] [PubMed] [Google Scholar]
- 30.Moriyasu K, Kuriyama C, Kurihara K, Fujihashi A, Ohno K, Asada Y. Longitudinal clinical study on the effect of slow maxillary expansion with removable appliances. Pediatric Dental Journal. 2010;20:78–83. [Google Scholar]
- 31.What Parents Should Know about the Safety of Dental Radiology. Available at: http://www.imagegently.org/LinkClick.aspx?fileticket=2EUpQxTchIc%3d&portalid=6 Last accessed date: Copyright 2014.
- 32.Kılıç N, Kiki A, Oktay H. A comparison of dentoalveolar inclination treated by two palatal expanders. Eur J Orthod. 2008;30:67–72. doi: 10.1093/ejo/cjm099. [DOI] [PubMed] [Google Scholar]
- 33.Sari Z, Uysal T, Usumez S, Basciftci FA. Rapid maxillary expansion. Is it better in the mixed or in the permanent dentition? Angle Orthod. 2003;73:654–661. doi: 10.1043/0003-3219(2003)073<0654:RMEIIB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Marshall S, Dawson D, Southard KA, Lee AN, Casko JS, Southard TE. Transverse molar movements during growth. Am J Orthod Dentofacial Orthop. 2003;124:615–624. doi: 10.1016/s0889-5406(03)00630-9. [DOI] [PubMed] [Google Scholar]