Abstract
Backgrounds
Pregnancy related complications are major causes of maternal morbidity and mortality worldwide. Diversified food consumption is essential to produce hormones during pregnancy and it reduced complications. In Ethiopia, many researchers were investigated about the proportion of pregnant women with dietary diversity and its determinant factors. However, those studies are inconsistent and fragmented. Therefore, the aim of this study was to estimate the pooled proportion of pregnant women with dietary diversity practice and its associated factors in Ethiopia.
Methods
We conducted a systematic electronic web-based search of PubMed/ /MEDLINE, EMBASE, Web of Science, Google Scholar and Google online databases for identifying studies on proportion of pregnant women with dietary diversity practice and its associated factors in Ethiopia using pre-defined quality and inclusion criteria. STATA version 14 statistical software was used to analyze the data. We extracted relevant data and presented in tabular form. The I2 test was used to assess heterogeneity across studies. Funnel plot asymmetry and Begg’s test were used to check for publication bias. The final effect size was determined by applying a random-effects model.
Results
Our search identified 170 studies. Of which, 23 were included in the final analysis stage. The pooled proportion of dietary diversity among pregnant women in Ethiopia was 41% (95% CI: 33, 49). Mothers can read and write (OR = 1.82 (95% CI: 1.25, 2.64)), maternal primary school and above educated (OR = 2.11 (95% CI: 1.10, 4.05)), nutritional information (OR = 4.1 (95% CI: 2.1, 7.99), dietary diversity knowledge (OR = 3.4 (95% CI: 2.73, 4.73)) and household had rich wealth index (OR = 3.45 (95% CI: 1.19, 10.1)) were significantly associated with dietary diversity practice during pregnancy.
Conclusions
In this meta-analysis; we found that low proportion of pregnant women with adequate dietary diversity in Ethiopia (41%). Maternal education, nutritional information, dietary diversity knowledge and wealth index level of household were significantly associated factors of pregnant woman with dietary diversity practice. This finding implies that improving the awareness of woman about dietary diversity during pregnancy and empowering women economically would play a significant role to improve dietary diversity practice.
Background
Pregnancy related complications are a major public health problem in the world. To reduce it, diversified food consumption is essential during pregnancy. Dietary diversity intake fulfills the requirements of minerals and vitamins of a pregnant woman and the growing of the fetus. For healthy development of fetus taking Minerals and Vitamins are important. Dietary diversity is the consumption of a variety of food which is nutritionally adequate over a reference period [1–3].
Researchers suggested that nutrition information, education, monthly income, dietary knowledge, family size, age, ownership of radio, having an illness, and husband occupation as factors those affect the dietary practices of pregnant women [4–7].
The burden of inadequate dietary diversity intake among pregnant women is double which leads to poor fetus development, and increases pregnancy related complications [8]. Savy M et al (2007) indicated that maternal mortality, low birth weight, and childhood stunting are the major consequences of low diversified food intake during pregnancy [3]. Globally, 99% of maternal deaths are in developing countries, and most of them were related with inadequate food diversity intake and poor nutrition [9].
Ethiopia is one of the developing countries with high maternal mortality related with pregnancy complication. Annually, more than 10% pregnancies end in abortion, and 1 in 27 mothers die due to complications of pregnancy or childbirth [10]. By 2025, WHO planned to reduce low birth weight by 30% [11, 12], to fulfill this agenda, it needs to assess the status of dietary diversity intake among pregnant women during pregnancy [13]. The proportion of pregnant women with dietary diversity in Ethiopia scaled from 12.8 to 74.5% [14, 15].
In Ethiopia, many researchers were investigated about the proportion of pregnant women with dietary diversity and its determinant factors. However, those studies are inconsistent and fragmented. Hence, our concern was to have a comprehensive national estimate for the overall proportion of pregnant women with adequate dietary diversity and its associated factors. Therefore, the aim of this study was to estimate the pooled proportion of pregnant women with dietary diversity practice and its associated factors in Ethiopia. The findings of this study intended to improve the interventions of health care workers in dietary diversity of women during pregnancy, and to remained researchers for the future.
Methods
Search strategy and studies identification
Articles reviewed in this systematic review and meta-analysis was accessed through electronic web-based database searches, and reference list reviews. It is in accordance with the Preferred Reporting Items of Systematic Reviews and Meta-Analysis (PRISMA) protocols checklist guidelines. A comprehensive search was done from PubMed/ /MEDLINE, EMBASE, web of Science, Google Scholar and Google electronic international databases. We searched combining MeSH terms such as: “dietary diversity”, “pregnancy”, “associated or determinant factors” and “Ethiopia”. These search terms have pre-defined to allow a comprehensive search strategy that included all fields within records and Medical Subject Headings (MeSH terms). This study also used Boolean operator (within each axis we combined keywords with the "OR" operator and we then linked the search strategies for the two axes with the "AND" operator) to search dietary diversity. Searches were searched between January 1, 2020 and February 18, 2020. All articles done until April 20, 2020 were included. After identifying potentially relevant articles, studies were retrieved and managed using Endnote X8.
Eligibility criteria
In this systematic review and meta-analysis, studies were eligible based on the following criteria; 1. Only studies conducted in Ethiopia. 2. Only studies written in English language. 3. All observational (cohort, case-control and cross-sectional) studies conducted among pregnant woman. 4. Only studies estimated proportion or associated factors of dietary diversity practice. 5. Only published studies done until April 20, 2020 were included.
Outcome variable
Dietary diversity is the variety of foods which consumed by pregnant women out of the ten food groups. These food groups include starch staples, vitamin A-rich vegetables and fruits; dark green leafy v1egetables; other vegetables; other fruits; meat, poultry, and fish; eggs and pulses/legumes; nuts and seeds; and dairy products [16]. A good dietary diversity is considered a woman consumes five or more variety of food of the ten food groups used in this study. As a result, a primary outcome of this study was the proportion of mothers with dietary diversity during pregnancy, which was calculated as the number of women who experienced good dietary diversity during pregnancy among all pregnant women. The second outcome was associated factors conducted in Ethiopia. Odds ratio/ 2x2 contingency were extracted for associated factors.
Data extraction
The authors used two stages of screening. Primarily, we screened the titles and abstracts based on the inclusion criteria. Secondly, we identified potentially relevant articles using titles and abstracts for further re-screening of its full article document. The relevance of the articles was evaluated based on their topic, objectives, and methodology as listed in the abstract. The abstracts were also assessed for agreement with the inclusion criteria. When it was unclear whether an abstract was relevant, it was included for retrieval. Two authors (AG and AM) extracted all essential data independently. Data were extracted using predefined format. The format contains, primary author name, year of publication, regions where the study was conducted, study area, sample size, study design, proportion (%), and response rate (%). Furthermore, contingency tables were extracted from studies which reported associated factors. Any disagreement between the two authors due to inclusion and data collection was solved by third and fourth author (GT and GW) through discussion.
Risk of bias assessment
The risk of bias for the included studies were assessed using the 10-item rating scale developed by Hoy et al. for observational studies [17]. Sampling, data collection, reliability and validity of study tools, case definition, and study periods were assessed. Researchers categorized each study as having a low risk of bias (“yes” answers to domain questions) or high risk of bias (“no” answers to domain questions). Each study was assigned a score of 1 (Yes) or 0 (No) for each domain, and these domain scores were summed to provide an overall study quality score. Scores of 8–10 were considered as having a “low risk of bias”, 6–7 a “moderate risk”, and 0–5 a “high risk”. Two independent reviewers (AG and HD) critically appraised each paper. Disagreements between those reviewers were solved by (GT and GW) through discussion. If not, a third and fourth reviewer was involved to resolve the inconsistencies between the two independent reviewers. For the final risk of bias classification, discrepancies between the reviewers were resolved via consensus.
Data processing and analysis
After extracted all essential data, it was entered into Microsoft Excel, and then exported to STATA version 1 Software to determine the proportion of pregnant mothers with dietary diversity. Heterogeneity across studies was assessed using the inverse variance (I2) and Cochran Q statistics with 25% as low, 50% as moderate, and 75% as severe heterogeneity [18]. The value of I2 greater than 75 was considered as the existence of sever heterogeneity in the studies [19, 20]. Dersimonian and Liard random effect model was used for analysis due to high heterogeneity [21, 22]. Subgroup analysis were conducted using region, study design and sample size [23]. As a result, we used forest plot to show the findings. We used funnel plot asymmetry, and Egger’s and Begg’s test to check for publication bias [24].
Results
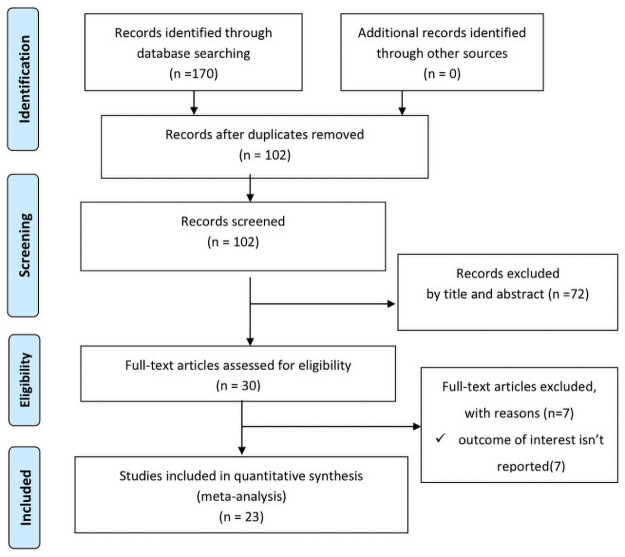
The database search and desk review yielded a total of 170 articles from the above listed electronic sources. After reviewing the titles and abstracts, we excluded 68 articles due to duplication. Seventy two articles were also excluded with a reason of irrelevance and seven additional articles were excluded due to lack of response on the outcome of interest [25–32]. Finally, 23 studies were included in this systematic review and meta-analysis [5–7, 14, 15, 33–50] (Fig 1).
Fig 1. PRISMA flowchart.
Flow diagram of studies included in meta-analysis.
Characteristics of included studies
Detail descriptions of the included studies were presented in Table 1. All studies were published between 2013 and 2020. Of all the included studies, nine studies [5, 7, 14, 33–35, 38, 40, 49] were community based cross-sectional (CBCS) and the rest; fourteen studies were institution based cross-sectional (IBCS) studies study design. Out of 23 studies, only 12 studies [5, 7, 14, 34–36, 38, 39, 42, 44, 48, 49] were reported essential associated factors of dietary diversity among pregnant woman in Ethiopia. The sample sizes in each study varies from 104 [51] to 1393 [15].
Table 1. Descriptive summary of 23 studies included in meta-analysis of dietary diversity during pregnancy in Ethiopia.
| Author name | Publication year | Region | Study design | Sample size | Proportion (%) | Response rate (%) |
|---|---|---|---|---|---|---|
| Abebe, et al [33] | 2014 | SNNP | CBCS | 104 | 50.0 | |
| Alemayehu, et al [34] | 2016 | Amhara | CBCS | 574 | 40.1 | 98.9 |
| Aliwo, et al [35] | 2019 | Amhara | CBCS | 647 | 31.4 | 97.4 |
| Demilew, et al [38] | 2020 | Amhara | CBCS | 694 | 19.9 | 97.5 |
| Desta, et al [39] | 2019 | Oromia | IBCS | 315 | 25.4 | 95.7 |
| Diddana [14] | 2019 | Amhara | CBCS | 604 | 74.5 | 100 |
| Daba, et al [36] | 2013 | Oromia | IBCS | 419 | 47.0 | 99.3 |
| Hailu, et al [42] | 2019 | Oromia | IBCS | 422 | 44.8 | 99.7 |
| Jemal, et al [44] | 2019 | Tigray | IBCS | 412 | 61.2 | 98 |
| Nana, et al [5] | 2018 | Amhara | CBCS | 616 | 39.3 | 100 |
| Hailu1, et al [43] | 2020 | Oromia | IBCS | 419 | 33.9 | 99.5 |
| Tenaw, et al [6] | 2018 | A.A | IBCS | 322 | 34.5 | 94.7 |
| Tolera, et al [7] | 2018 | Oromia | CBCS | 338 | 25.0 | 98.5 |
| Yeneabat, et al [49] | 2019 | Amhara | CBCS | 759 | 44.3 | 91 |
| Zerfu, et al [50] | 2019 | Oromia | IBCS | 432 | 49.7 | 100 |
| Samuel, et al [46] | 2020 | SNNP | IBCS | 423 | 20.1 | 97 |
| Gebreselassie, et al [40] | 2013 | SNNP | CBCS | 700 | 65.3 | 93.3 |
| Workicho, et al [15] | 2018 | Oromia | IBCS | 1393 | 12.8 | |
| Shenka, et al [47] | 2018 | Driedewa | IBCS | 380 | 43.0 | 98.2 |
| Tefera, et al [48] | 2020 | A.A | IBCS | 402 | 60.9 | 99 |
| Kobiro, et al [45] | 2020 | SNNP | IBCS | 303 | 42.6 | 99 |
| Gizahewu, et al [41] | 2019 | SNNP | IBCS | 211 | 31.8 | 100 |
| Delil, et al [37] | 2018 | SNNP | IBCS | 314 | 47.9 | 98.4 |
Moreover, four Ethiopian regions and two administrative cities were represented. Seven studies were in Oromia regions, six studies in Amhara region, six studies in South Nation Nationality People (SNNP) region, two studies in Addis Ababa (A.A), one study in Drie Dewa city and one study in Tigray. Furthermore, the proportion of dietary diversity varies from 12.8% [15] to 74.5% [14]. The smallest proportion was conducted institution based cross-sectional study, which was reported in Oromia region [15], while the largest was conducted community based cross-sectional study, which observed in Amhara region [14], (See Table 1).
Risk of bias assessment of included studies
In this review, we assessed the risk of bias for each of the original studies using Hoy, et al (2012) risk-of-bias assessment tool (S1 Table). Of the total included studies, our summary assessment showed that one (4.35%) study was at high risk of bias, 3 (13.04%) were medium risk, whereas the rest 19 (82.61%) were low risk of bias.
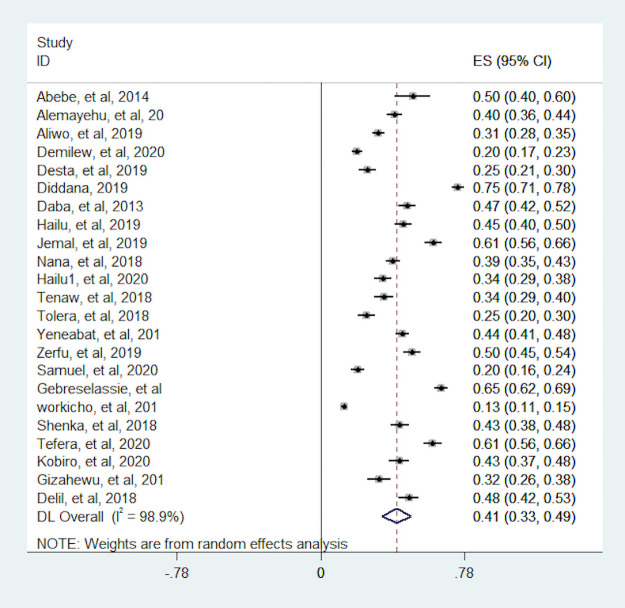
Proportion of dietary diversity among pregnant women
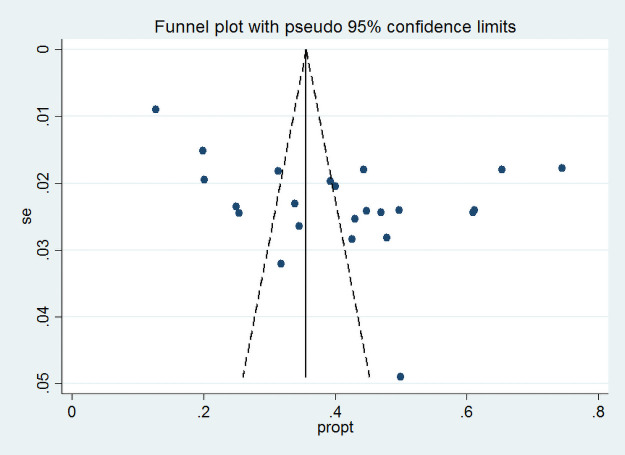
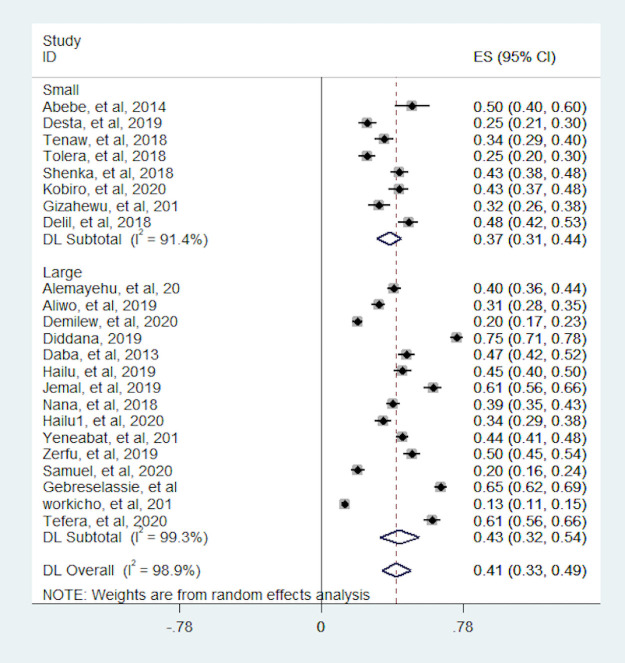
In this meta-analysis, we observed that the proportion of pregnant women with dietary diversity was varying across the included studies. The proportion was varying between 12.8% (15) and 74.5% (14). The I2 consistence test and Cochrane Q heterogeneity test statistics showed high heterogeneity (I2 = 98.9, p-value <0.001), which leads us Dersimonian and Liard random effect model. As a result of a random effect model, the pooled proportion of dietary diversity among pregnant women in Ethiopia was 41% (95% CI: 33, 49) (Fig 2). The funnel plot seems asymmetry but Begg’s rank correlation publication bias test was insignificant (p = 0.75) (Fig 3).
Fig 2. Forest plot the proportion of women with dietary diversity in Ethiopia.
Fig 3. Funnel plot for the proportion of adequate dietary diversity in Ethiopia.
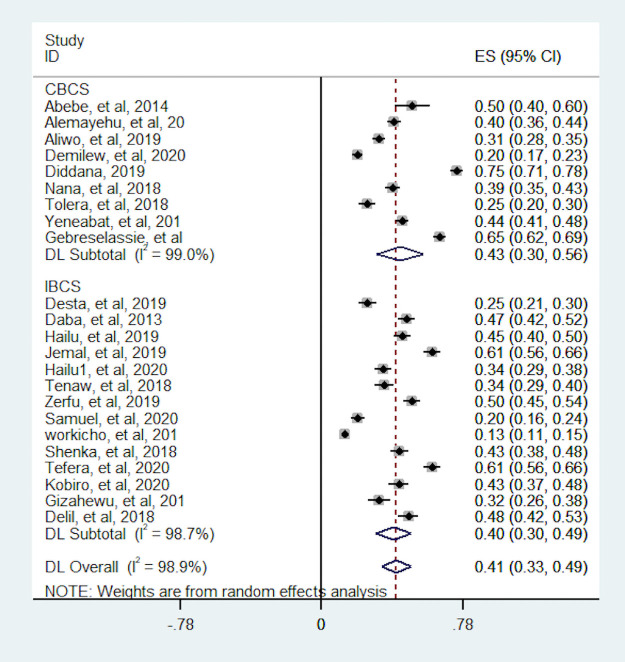
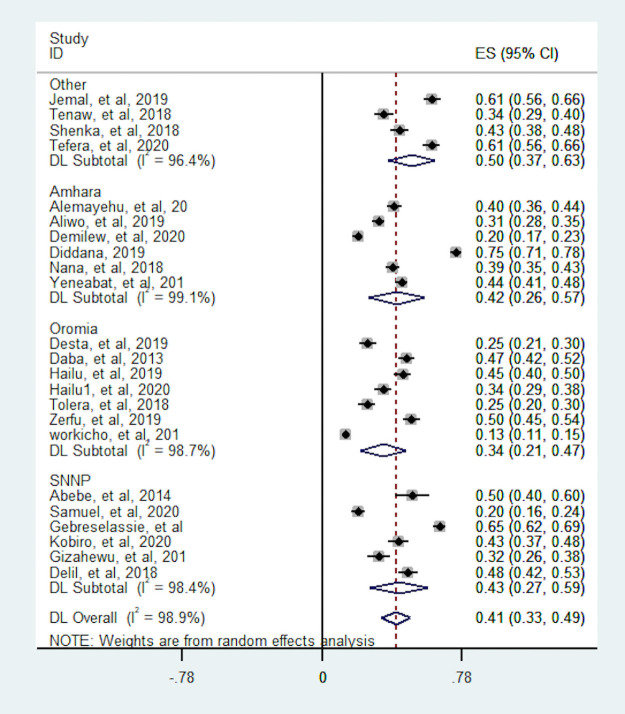
Subgroup analysis
In this meta-analysis, we conducted subgroup analyses to identify potential source of heterogeneity and the distribution of dietary diversity based on study design, region of the country where the study was conducted and sample size. As a result; the proportion of pregnant women with dietary diversity was higher for studies which conducted with CBCS design (43.3%) than IBCS (39.7%). Heterogeneity test between study design was statistically significant (p-value <0.001). The proportion of dietary diversity were more varies in studies which conducted in CBCS and which ranged from 20% to 75% whereas studies which was conducted in IBCS the proportion relatively consistent ranged from 13% to 61% (Fig 4). The subgroup analyses based on sample size showed the pooled proportion is robust over sample size. The heterogeneity test based on sample size also statistically insignificant (p-value = 0.970) (Fig 5). Moreover, the highest pooled proportion of pregnant women with dietary diversity was 49.9%, which was observed in other group (A.A, Dreie Dewa and Tigray) and the smallest pooled proportion was 34%, which was observed in Oromia region. We found a significant heterogeneity difference between regions (p-value <0.001). The heterogeneity of within studies in Amahara and SNNP region was high which may relate to study design (Fig 6).
Fig 4. Subgroup analysis of the proportion of pregnant women with dietary diversity by study design.
CBCS = Community based cross-sectional, IBCS = Institutional based cross-sectional.
Fig 5. Subgroup analysis of the proportion of pregnant women with dietary diversity by sample size.
Small = < = 400, large = >400.
Fig 6. Subgroup analysis of the proportion of pregnant women with dietary diversity by region.
Other = Addis Ababa, Drie Dewa and Tigray.
Associated factors of dietary diversity among pregnant women
In this meta-analysis, we assessed factors associated with dietary diversity. A separate analysis was conducted for each factor, which was considered in this study. Variables which assessed with the dietary diversity were: maternal education, husband education, place of residence, family size, nutritional information, dietary diversity related knowledge, income, and wealth index.
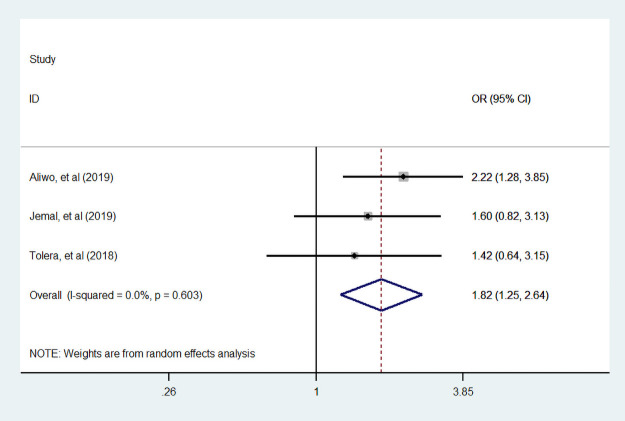
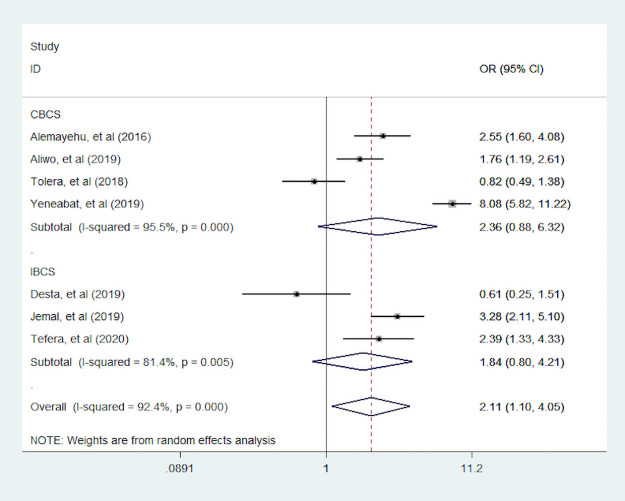
Maternal education
Three studies [7, 35, 44] assessed the association of a woman who can read and write with dietary diversity during pregnancy. Women who can read and write were 82% more likely to consumed diversified food than who cannot read and write (Fig 7). Seven studies [7, 34, 35, 39, 44, 48, 49] were assessed the primary school educated with dietary diversity. Of those seven studies, two studies reported the association between primary school educated women with dietary diversity during pregnancy is insignificant. In addition, four studies were conducted by CBCS study design. We found pregnant woman who are educated primary school and above were 2.11 times more likely to eat dietary diversity food compared to no educated women. The overall and within study design the value of I 2 was high, this heterogeneity may come do to study design variation (Fig 8).
Fig 7. The pooled odds ratio of the association between maternal can read and write and dietary diversity during pregnancy.
Fig 8. The pooled odds ratio of the association between maternal educated primary school and above with dietary diversity during pregnancy.
Husband education
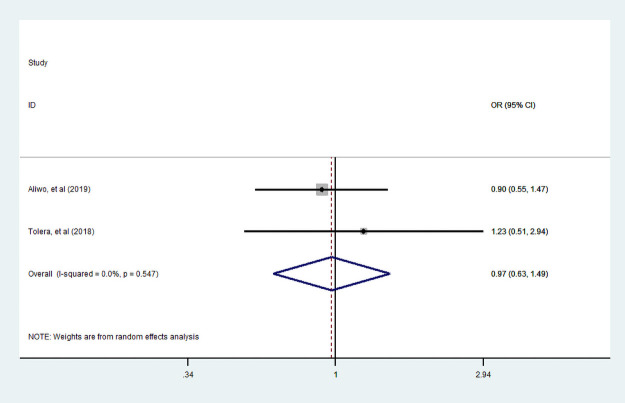
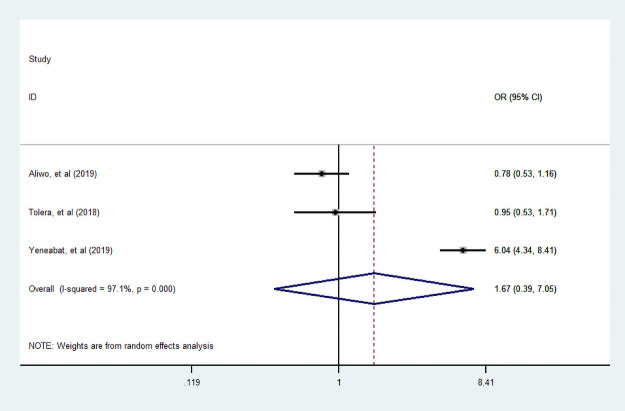
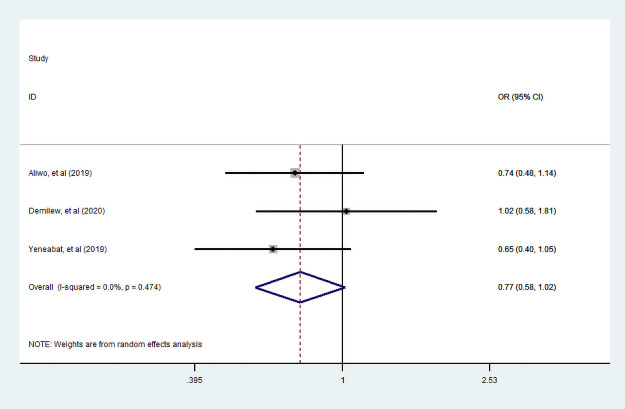
Of three studies [7, 35, 49] assessed the association between husband education and dietary diversity practice, only two studies [7, 35] examined the association between husband who can read and write with dietary diversity. Unfortunately, in this review, the association between a husband who can read and writes with dietary diversity during pregnancy was statistically insignificant. In addition, three studies [7, 35, 49] assessed husband educated primary and above with dietary diversified food practice. We observe that a woman who had primary and above educated husband had no statistically significant practice of diversified dietary food consumption during pregnancy (Figs 9 and 10).
Fig 9. The pooled odds ratio of the association between husbands can read and write with dietary diversity during pregnancy.
Fig 10. The pooled odds ratio of the association between husband educated primary school and above with dietary diversity during pregnancy.
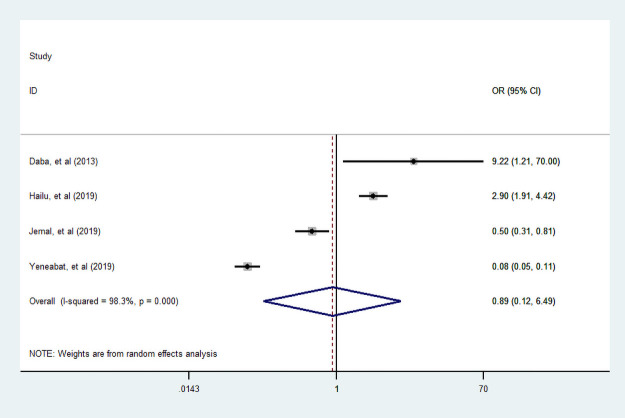
Place of residence
In this meta-analysis, four studies [36, 42, 44, 49] were assessed for the association between place of residence and dietary diversity food consumption. Consequently, the association was not statistically significant; it revealed that there is no dietary diversity practice variation among a woman living in rural and urban during pregnancy (Fig 11).
Fig 11. The pooled odds ratio of the association between place of residence and dietary diversity during pregnancy.
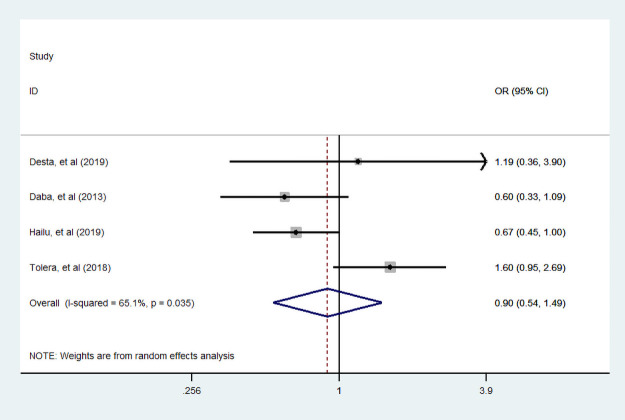
Family size
We assessed the association between family size and dietary practice during pregnancy. Four studies [7, 36, 39, 42] assessed its association. Only two studies showed a woman who had more than five family sizes is positively associated with diversified food practice. Our finding indicated that dietary diversity practice during pregnancy was not statistically associated with family size (Fig 12).
Fig 12. The pooled odds ratio of the association between family size and dietary diversity during pregnancy.
Nutritional information
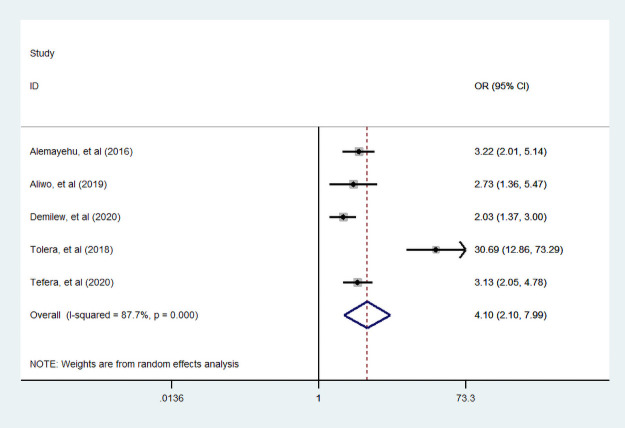
Furthermore, five studies [7, 34, 35, 38, 48] assessed the association between dietary diversity food and nutritional information. We found that statistically significant association between nutritional information and dietary diversity practice during pregnancy. A woman who had nutritional information was 4.1 times more likely practiced diversified food compared with a woman who had no nutritional information (Fig 13).
Fig 13. The pooled odds ratio of the association between maternal nutritional information and dietary diversity during pregnancy.
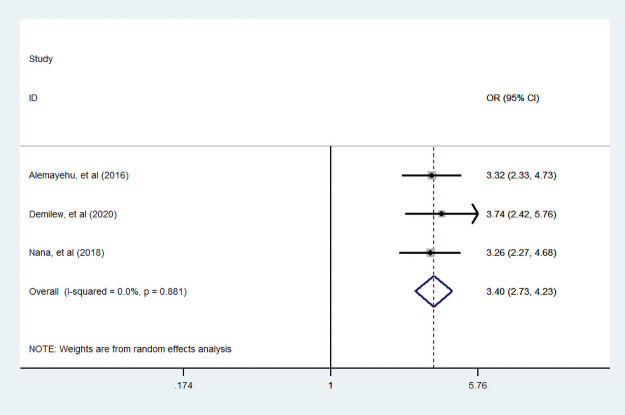
Knowledge about food diversity
In three studies [5, 34, 38], investigators examined the association between dietary diversity food knowledge with dietary diversity practice. We found that there was statistically significant association dietary diversity food knowledge and dietary diversity practice. A woman who had good knowledge about dietary diversity food consumption was 3.4 (95% CI: 2.73, 4.73) times more likely to experienced diversified food than who had no knowledge counter parts (Fig 14).
Fig 14. The pooled odds ratio of the association between knowledge about food diversity and dietary diversity during pregnancy.
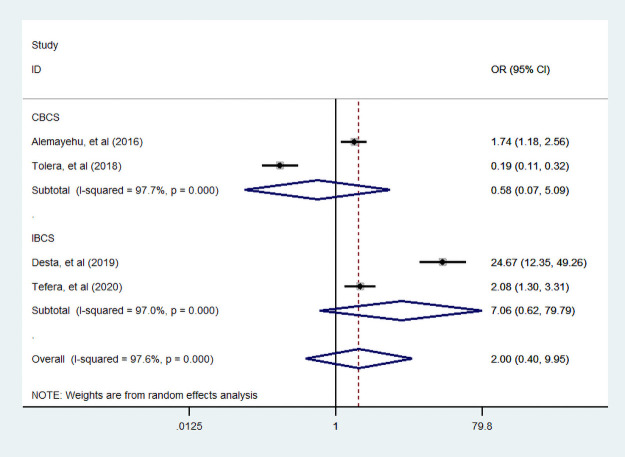
Income
In four articles [7, 34, 39, 48], researchers assessed the association of income with dietary diversity practice. Of those studies, two studies were conducted by CBCS. Moreover, one studies reported that income were negative association with dietary diversity during pregnancy. This meta-analysis suggested that income was not statistically associated with dietary diversified practice during pregnancy (Fig 15).
Fig 15. The pooled odds ratio of the association between income and dietary diversity during pregnancy.
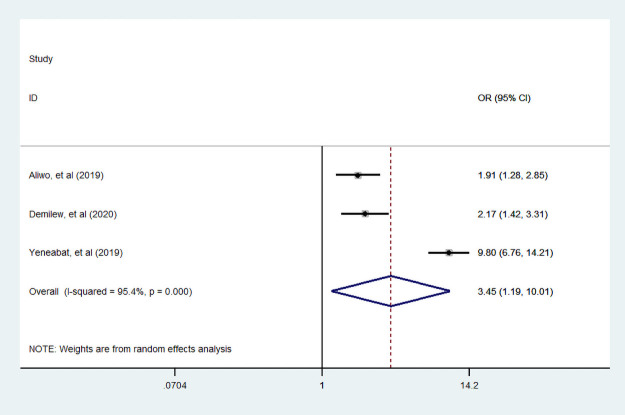
Wealth index
Three studies [35, 38, 49] were examined the association between household wealth index and dietary diversity practice. Accordingly those studies, we find that a woman from a household who had high wealth index was more likely practiced dietary diversity food compared to poor household. But, we found that a woman from a household with medium wealth index was not associated with dietary diversity practice compared to poor household (Figs 16 and 17).
Fig 16. The pooled odds ratio of the association between household high wealth index and dietary diversity during pregnancy.
Fig 17. The pooled odds ratio of the association between household medium wealth index and dietary diversity during pregnancy.
Discussion
Dietary diversity has a significant contribution for pregnancy outcome. Dietary diversity during pregnancy in developing countries is influenced by socio-demographic, culture, individual and health service-related factors [52, 53]. Therefore, this systematic review and meta-analysis was conducted to estimate the pooled proportion and associated factors of dietary diversity practice during pregnancy in Ethiopia.
This meta-analysis showed that the pooled proportion of dietary diversity among pregnant woman in Ethiopia was 41% (95% CI: 33, 49). This finding is almost half of the proportion dietary diversity reported from in Ghana [54], which was a minimum dietary diversity proportion five and above out of 11 food groups was 85% among pregnant woman. Moreover, this result also twice less than the result of a study conducted in Kenya [55], which reported that 85% of pregnant woman consumed more than four varieties of foods. The finding of this study is supported by a study conducted on Zinc deficiency in Ethiopia, which revealed that 59.9% women were faced zinc deficiency during pregnancy, which shows inadequate dietary diversity is high.
In addition, the subgroup analysis indicated that community based cross-sectional studies had (43.3%) more consumed variety of food than institution based cross-sectional study (39.7%). Similarly the highest proportion of dietary diversity was recorded in other group (Addis Ababa, Drie Dewa and Tigray) (49.9%) and the smallest was reported in Oromia (34%). This result has been supported by Ethiopian EDHS 2016 report which states that the highest proportion of normal BMI was observed in Addis Ababa and Drie Dewa city administrations (23.1 and 22.0%) respectively(EDHS,2016) [56]. The reason may be related to sampling issue means that studies which conducted in community based was included more representative participant than institution based studies because institution based studies consider only woman who attained at the selected institution unfortunately woman who left from the institution was not represent in the study. In addition woman who lived in Addis Ababa and Drie Dewa is more educated and have good knowledge relative to other regions.
We also assessed associated factors of proportion of dietary diversity practice in Ethiopia. We found that a woman who can read and write were 82% (95% CI: 1.25, 2.64) more likely to eat diversified food than who cannot read and write. In addition, more educated woman 2.11 (95% CI: 1.10, 4.05) times consumed a variety of food than non-educated woman. This finding is in line with a study conducted in Kenya [55], which showed that more educated woman was 2.78 (95% (CI: 1.06, 5.32)) times consumed minimum dietary diversity food than non-educated woman. We found that dietary diversity practice among pregnant woman was the same across residence and family size.
Moreover, the odds of a women having good nutritional information were 4.1 (95% CI: 2.1, 7.99) times than the odds of women hadn’t information. We also found that a women having knowledge about dietary diversity was 3.4 times more likely practiced diversified food during pregnancy. When women had information and knowledge on nutritional diversity they might have a chance to understand the benefits of consuming diversified food during pregnancy for their own babies’ health. In convention mothers are very egger to the better good of their babies which induces them to practice diversified food. However, husband education does not have significant association with wife’s dietary food consumption during pregnancy. Hence, husband should advise their wife’s to enhance mothers diversity food consumption practice during pregnancy.
Furthermore, this study found that a woman from a rich household was 3.45 (95% CI: 1.19, 10.1) times more likely consumed more diversified food groups compared to a woman from poor household. This finding consistent with a study conducted in Kenya [55], which reported that a women belongs in high income household 2.08 time more consumed a variety of food groups. Studies explain the reason could be related with rich households would have an access variety of foods in the household and it had positive contribution diversified food consumption [57].
Limitation of the study
This meta-analysis has some limitations. The first limitation of this study was solely studies written in English language were considered to estimate the proportion of dietary diversity among pregnant woman in Ethiopia. In addition, there were not enough studies of systematic reviews and meta-analysis for the problem to compare. Lastly, in this meta-analysis study only four Ethiopian regions and two administrative city of the country were represented, which may reflect non representation due to the limited number of articles included.
Conclusion
In this meta-analysis; we found that low proportion of dietary diversity among pregnant women in Ethiopia. Maternal education, nutritional information, dietary diversity knowledge and wealth index level of household were significantly associated with dietary diversity practice. Regardless of the current effort towards maternal and child health, this too low proportion of dietary diversity among pregnant women is not acceptable. This study implies the needs to develop interventions to improve house hold wealth by empowering women and improving awareness towards dietary diversity practice during pregnancy through exiting maternal health initiative strategies using health developmental army, policymakers, health extension workers and proper advising by health professionals during antenatal care visits. In addition, Husband education does not help wife’s dietary diversity practice. Hence, husband should advise their wife’s to enhance mothers diversity food consumption practice during pregnancy. Future studies should be given attention on clinical factors like nutritional consult and trimester of ANC during pregnancy.
Supporting information
(DOC)
(XLSX)
(XLSX)
(TXT)
Acknowledgments
We would like to acknowledge all authors of the studies which included in this review.
Data Availability
All relevant data are within the paper and its Supporting information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Cuco G, Arija V, Iranzo R, Vila J, Prieto M, Fernández-Ballart J. Association of maternal protein intake before conception and throughout pregnancy with birth weight. Acta obstetricia et gynecologica Scandinavica. 2006;85(4):413–21. doi: 10.1080/00016340600572228 [DOI] [PubMed] [Google Scholar]
- 2.Savy M, Martin-Prével Y, Sawadogo P, Kameli Y, Delpeuch F. Use of variety/diversity scores for diet quality measurement: relation with nutritional status of women in a rural area in Burkina Faso. European journal of clinical nutrition. 2005;59(5):703–16. doi: 10.1038/sj.ejcn.1602135 [DOI] [PubMed] [Google Scholar]
- 3.Savy M, Martin-Prével Y, Traissac P, Delpeuch F. Measuring dietary diversity in rural Burkina Faso: comparison of a 1-day and a 3-day dietary recall. Public health nutrition. 2007;10(1):71–8. doi: 10.1017/S1368980007219627 [DOI] [PubMed] [Google Scholar]
- 4.Gemeda D, Fekadu B, Wondu G, Habitamu F. Assessment of nutritional practices of pregnant mothers on maternal nutrition and associated factors in Guto Gida Woreda, East Wollega Zone, Ethiopia. Sci Technol Arts Res J. 2013;2:105–13. [Google Scholar]
- 5.Nana A, Zema T. Dietary practices and associated factors during pregnancy in northwestern Ethiopia. BMC pregnancy and childbirth. 2018;18(1):183. doi: 10.1186/s12884-018-1822-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tenaw Z, Arega M, Tachbele E. Nutritional knowledge, attitude and practices among pregnant women who attend antenatal care at public hospitals of Addis Ababa, Ethiopia. International Journal of Nursing and Midwifery. 2018;10(7):81–9. [Google Scholar]
- 7.Tolera B, Mideksa S, Dida N. Assessment of dietary practice and associated factors among pregnant mother in Ambo District, West Shoa, Oromia, Ethiopia, 2018. Ethiopian Journal of Reproductive Health. 2018;10(4). [Google Scholar]
- 8.Wu G, Imhoff-Kunsch B, Girard AW. Biological mechanisms for nutritional regulation of maternal health and fetal development. Paediatric and perinatal epidemiology. 2012;26:4–26. doi: 10.1111/j.1365-3016.2012.01291.x [DOI] [PubMed] [Google Scholar]
- 9.Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. The lancet. 2008;371(9608):243–60. doi: 10.1016/S0140-6736(07)61690-0 [DOI] [PubMed] [Google Scholar]
- 10.Moore AM, Gebrehiwot Y, Fetters T, Wado YD, Bankole A, Singh S, et al. The estimated incidence of induced abortion in Ethiopia, 2014: changes in the provision of services since 2008. International perspectives on sexual and reproductive health. 2016;42(3):111. doi: 10.1363/42e1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Organization WH. Global Nutrition Targets 2025: Low birth weight policy brief. World Health Organization; 2014. [Google Scholar]
- 12.Organization WH. Global nutrition targets 2025: Policy brief series. World Health Organization; 2014. [Google Scholar]
- 13.Grieger JA, Clifton VL. A review of the impact of dietary intakes in human pregnancy on infant birthweight. Nutrients. 2015;7(1):153–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diddana TZ. Factors associated with dietary practice and nutritional status of pregnant women in Dessie town, northeastern Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2019;19. doi: 10.1186/s12884-019-2649-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Workicho A, Belachew T, Ghosh S, Kershaw M, Lachat C, Kolsteren P. Burden and determinants of undernutrition among young pregnant women in Ethiopia. Maternal & child nutrition. 2019;15(3):e12751. doi: 10.1111/mcn.12751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.FAO F. Minimum dietary diversity for women: a guide for measurement. Rome: FAO. 2016;82. [Google Scholar]
- 17.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. Journal of clinical epidemiology. 2012;65(9):934–9. doi: 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 18.Hedges LV. Meta-analysis. Journal of Educational Statistics. 1992;17(4):279–96. [Google Scholar]
- 19.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cuijpers P. Meta-analyses in mental health research. A practical guide. Amsterdam, the Netherlands: Pim Cuijpers Uitgeverij. 2016. [Google Scholar]
- 21.Hoge EA, Friedman L, Schulz SC. Meta-analysis of brain size in bipolar disorder. Schizophrenia research. 1999;37(2):177–81. doi: 10.1016/s0920-9964(98)00149-2 [DOI] [PubMed] [Google Scholar]
- 22.Schwarzer G. meta: An R package for meta-analysis. R news. 2007;7(3):40–5. [Google Scholar]
- 23.Sterne JA, Egger M. Regression methods to detect publication and other bias in meta-analysis. Publication bias in meta-analysis: Prevention, assessment and adjustments. 2005:99–110. [Google Scholar]
- 24.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. Journal of clinical epidemiology. 2001;54(10):1046–55. doi: 10.1016/s0895-4356(01)00377-8 [DOI] [PubMed] [Google Scholar]
- 25.Bosha T, Lambert C, Riedel S, Melesse A, Biesalski HK. Dietary Diversity and Anthropometric Status of Mother–Child Pairs from Enset (False Banana) Staple Areas: A Panel Evidence from Southern Ethiopia. Int J Environ Res Public Health. 2019;16(12). doi: 10.3390/ijerph16122170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gebremedhin S, Enquselassie F, Umeta M. Prevalence of prenatal zinc deficiency and its association with socio-demographic, dietary and health care related factors in Rural Sidama, Southern Ethiopia: A cross-sectional study. BMC public health. 2011;11(1):898. doi: 10.1186/1471-2458-11-898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sonko A. Assessment of Dietary Practice and Anthropometric Status of Pregnant Women in Aleta Chuko Woreda Southern Nations, Nationalities and People’s™ Region /SNNPR/, Ethiopia: Descriptive Cross-Sectional Study. J Epidemiol Public Health Rev 1(1): http://dx.doi.org/1016966/2471-8211102.2016. [Google Scholar]
- 28.Zerfu TA, Biadgilign S. Pregnant mothers have limited knowledge and poor dietary diversity practices, but favorable attitude towards nutritional recommendations in rural Ethiopia: evidence from community-based study. BMC Nutr. 2018;4. doi: 10.1186/s40795-018-0251-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zerfu TA, Pinto E, Baye K. Consumption of dairy, fruits and dark green leafy vegetables is associated with lower risk of adverse pregnancy outcomes (APO): a prospective cohort study in rural Ethiopia. Nutr Diabetes. 2018;8(1):52. doi: 10.1038/s41387-018-0060-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zerfu TA, Umeta M, Baye K. Dietary habits, food taboos, and perceptions towards weight gain during pregnancy in Arsi, rural central Ethiopia: a qualitative cross-sectional study. J Health Popul Nutr. 2016;35(1):22. doi: 10.1186/s41043-016-0059-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zerfu TA, Umeta M, Baye K, Helion Belay AM, Tariku A, Woreta SA, et al. Dietary diversity during pregnancy is associated with reduced risk of maternal anemia, preterm delivery, and low birth weight in a prospective cohort study in rural Ethiopia, Am J Clin Nutr. 2016;103(6):1482–8. doi: 10.3945/ajcn.115.116798 [DOI] [PubMed] [Google Scholar]
- 32.Kuche D, Singh P, Moges D. Dietary practices and associated factors among pregnant women in Wondo Genet District, southern Ethiopia. J Pharm Sci Innov. 2015;4(5):270–5. [Google Scholar]
- 33.Abebe H, Abebe Y, Loha E, Stoecker BJ. Consumption of vitamin A rich foods and dark adaptation threshold of pregnant women at Damot Sore District, Wolayita, Southern Ethiopia. Ethiop J Health Sci. 2014;24(3):219–26. doi: 10.4314/ejhs.v24i3.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alemayehu MS, Tesema EM. Dietary practice and associated factors among pregnant women in Gondar town north west, Ethiopia, 2014. Int J Nutr Food Sci. 2015;4(6):707–12. [Google Scholar]
- 35.Aliwo S, Fentie M, Awoke T, Gizaw Z. Dietary diversity practice and associated factors among pregnant women in North East Ethiopia. BMC Res Notes. 2019;12(1):123. doi: 10.1186/s13104-019-4159-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Daba G, Beyene F, Garoma W, Fekadu H. Assessment of nutritional practices of pregnant mothers on maternal nutrition and associated factors in Guto Gida Woreda, east Wollega zone, Ethiopia. Science, Technology and Arts Research Journal. 2013;2(3):105–13. [Google Scholar]
- 37.Delil R, Tamiru D, Zinab B. Dietary Diversity and Its Association with Anemia among Pregnant Women Attending Public Health Facilities in South Ethiopia. Ethiop J Health Sci. 2018;28(5):625–34. doi: 10.4314/ejhs.v28i5.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Demilew YM, Alene GD, Belachew T. Dietary practices and associated factors among pregnant women in West Gojjam Zone, Northwest Ethiopia. BMC Pregnancy Childbirth. 2020;20(1):18. doi: 10.1186/s12884-019-2702-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Desta M, Akibu M, Tadese M, Tesfaye M. Dietary Diversity and Associated Factors among Pregnant Women Attending Antenatal Clinic in Shashemane, Oromia, Central Ethiopia: A Cross-Sectional Study. J Nutr Metab. 2019;2019:3916864. doi: 10.1155/2019/3916864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gebreselassie SG, Gase FE, Deressa MU. Prevalence and correlates of prenatal vitamin A deficiency in rural Sidama, Southern Ethiopia. J Health Popul Nutr. 2013;31(2):185–94. doi: 10.3329/jhpn.v31i2.16382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gizahewu A B B Y M. Under Nutrition and Associated Factors among Pregnant Women at ANC Clinic, Nigist Eleni Mohammad Memorial General Hospital, Hossana, Southern Ethiopia. Food Nutr Current Res, 2(2): 158–165. 2019. [Google Scholar]
- 42.Hailu S, Woldemichael B. Dietary diversity and associated factors among pregnant women attending antenatal care at public health facilities in Bale Zone, Southeast Ethiopia. Population. 2017;65(24). [Google Scholar]
- 43.Hailu SEG. Under Nutrition and Associated Factors among Pregnant Women Attending Antennal Care at Public Health Facilities on Bale Zone, South East Ethiopia. J Food Nutr Sci 7(1): 9–14. 2020. [Google Scholar]
- 44.Jemal K, Awol M. Minimum Dietary Diversity Score and Associated Factors among Pregnant Women at Alamata General Hospital, Raya Azebo Zone, Tigray Region, Ethiopia. J Nutr Metab. 2019;2019:8314359. doi: 10.1155/2019/8314359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kobiro D, Delil R, Tamiru D, Zinab B. Determinants of Dietary Diversity among Pregnant Women Attending Public Health Facilities in Hossana town, South Ethiopia. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Samuel S, Darebo T, Desta DT, Mulugeta A. Socio-economic and dietary diversity characteristics are associated with anemia among pregnant women attending antenatal care services in public health centers of Kembata Tembaro Zone, Southern Ethiopia. Food Science & Nutrition. 2020;8(4):1978–86. doi: 10.1002/fsn3.1485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shenka A, Damena M, Abdo M, Roba KT. Dietary Diversity and Nutritional Status of Pregnant Women Attending Public Hospitals in Dire Dawa City Administration, Eastern Ethiopia. East African Journal of Health and Biomedical Sciences. 2018;2(1):10–7. [Google Scholar]
- 48.Tefera W, Brhanie TW, Dereje M. Dietary diversity practice and associated factors among pregnant women attending ANC in Kolfe Keranyo sub city health centers, Addis Ababa, Ethiopia. medRxiv. 2020. [Google Scholar]
- 49.Yeneabat T, Adugna H, Asmamaw T, Wubetu M, Admas M, Hailu G, et al. Maternal dietary diversity and micronutrient adequacy during pregnancy and related factors in East Gojjam Zone, Northwest Ethiopia, 2016. BMC pregnancy and childbirth. 2019;19(1):173. doi: 10.1186/s12884-019-2299-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zerfu TA, Baye K, Faber M. Dietary diversity cutoff values predicting anemia varied between mid and term of pregnancy: a prospective cohort study. J Health Popul Nutr. 2019;38(1):44. doi: 10.1186/s41043-019-0196-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abebe Y, Bogale A, Hambidge KM, Stoecker BJ, Arbide I, Teshome A, et al. Inadequate intakes of dietary zinc among pregnant women from subsistence households in Sidama, Southern Ethiopia. Public health nutrition. 2008;11(4):379–86. doi: 10.1017/S1368980007000389 [DOI] [PubMed] [Google Scholar]
- 52.Oni OA, Tukur J. Identifying pregnant women who would adhere to food taboos in a rural community: a community-based study. African journal of reproductive health. 2012;16(3). [PubMed] [Google Scholar]
- 53.Zepro NB. Food taboos and misconceptions among pregnant women of Shashemene District, Ethiopia, 2012. Sci J Public Health. 2015;3(3):410–6. [Google Scholar]
- 54.Saaka M, Rauf AA. Role of dietary diversity in ensuring adequate haematological status during pregnancy. International Journal of Medical Research & Health Sciences. 2015;4(4):749–55. [Google Scholar]
- 55.Kiboi W, Kimiywe J, Chege P. Determinants of dietary diversity among pregnant women in Laikipia County, Kenya: a cross-sectional study. BMC Nutrition. 2017;3(1):12. [Google Scholar]
- 56.Agency CS, ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF. 2016.
- 57.Desyibelew HD, Dadi AF. Burden and determinants of malnutrition among pregnant women in Africa: A systematic review and meta-analysis. PloS one. 2019;14(9). doi: 10.1371/journal.pone.0221712 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(XLSX)
(XLSX)
(TXT)
Data Availability Statement
All relevant data are within the paper and its Supporting information files.