Abstract
Background
The emerging novel coronavirus disease 2019 (COVID-19) has become one of the leading cause of deaths worldwide in 2020. The present systematic review and meta-analysis estimated the magnitude of sleep problems during the COVID-19 pandemic and its relationship with psychological distress.
Methods
Five academic databases (Scopus, PubMed Central, ProQuest, ISI Web of Knowledge, and Embase) were searched. Observational studies including case-control studies and cross-sectional studies were included if relevant data relationships were reported (i.e., sleep assessed utilizing the Pittsburgh Sleep Quality Index or Insomnia Severity Index). All the studies were English, peer-reviewed papers published between December 2019 and February 2021. PROSPERO registration number: CRD42020181644.
Findings
168 cross-sectional, four case-control, and five longitudinal design papers comprising 345,270 participants from 39 countries were identified. The corrected pooled estimated prevalence of sleep problems were 31% among healthcare professionals, 18% among the general population, and 57% among COVID-19 patients (all p-values < 0.05). Sleep problems were associated with depression among healthcare professionals, the general population, and COVID-19 patients, with Fisher's Z scores of -0.28, -0.30, and -0.36, respectively. Sleep problems were positively (and moderately) associated with anxiety among healthcare professionals, the general population, and COVID-19 patients, with Fisher's z scores of 0.55, 0.48, and 0.49, respectively.
Interpretation
Sleep problems appear to have been common during the ongoing COVID-19 pandemic. Moreover, sleep problems were found to be associated with higher levels of psychological distress. With the use of effective programs treating sleep problems, psychological distress may be reduced. Vice versa, the use of effective programs treating psychological distress, sleep problems may be reduced.
Funding
The present study received no funding.
Keywords: COVID-19, Sleep problems, Healthcare workers, COVID-19 patients, General population, Meta-analysis
Research in context.
Evidence before this study
The novel coronavirus disease 2019 (COVID-19) pandemic has caused psychological problems and sleep problems in different populations, including healthcare professionals, COVID-19 infected individuals, and the general population.
Added value of this study
Patients with COVID-19 infection had the highest prevalence of sleep problems, and healthcare professions had the second highest prevalence of sleep problems. Moderate associations between sleep problems and psychological distress (including depression and anxiety) were found.
Patients with COVID-19 infection and health professions are at risk of having sleep problems, and that there are moderate associations between sleep problems and psychological distress.
Implications of all the available evidence
These data emphasize the need of programs and treatments to assist different populations in overcoming sleep problems and psychological distress, especially patients with COVID-19 infection and health professions.
Alt-text: Unlabelled box
1. Introduction
Prior to 2020, respiratory diseases were the fourth leading cause of death [1]. However, with the outbreak of the novel coronavirus disease 2019 (COVID-19) in December 2019, respiratory infections caused more deaths due to COVID-19 [2]. According to the World Health Organization (WHO) as of April 16, 2021, there were over 137,866,000 known cases of COVID-19 and over 2,965,000 cases of COVID-19 death worldwide [3].
Prior research has found that the prevalence of COVID-19 is associated with major psychological distress and significant symptoms of mental health illness [4], [5], [6], [7], [8]. The sudden onset of a threatening illness puts great pressure on healthcare workers [9]. Consequently, healthcare workers may have impaired sleep because they need to deal with the illness, suffer from the high risk of death, and adapt to irregular work schedules and frequent shifts [10], [11], [12], [13], [14], [15]. They may experience sleep problems, anxiety, depression, and stress when faced with this major public health threat [16], [17], [18]. Due to their job demands, they are in frequent contact with patients and therefore suffer from extremely high-level stress. Therefore, they may develop acute sleep problems, including poor sleep quality and experience too little sleep [19]. Given that healthcare professionals are the frontline workers who take care of patients, their health is extremely important. More specifically, if healthcare providers have any health issues that prevent them from taking care of patients, their local communities more specifically, and their country more generally, will encounter a huge challenge of healthcare burden and consequently impact on all residents’ health.
In addition to healthcare workers, the general population is likely to develop mental health and sleep problems due to the impacts of COVID-19 [20] because a substantial change in lifestyle is a huge stressor [21,22]. For example, individuals may need to self-isolate and quarantine at home, avoid social activities for leisure and recreation that they had participated in previously, and strictly obey the new policies to minimize spread of the virus (e.g., wearing a mask in public areas) [23,24]. The general population may also receive threatening information such as daily statistics concerning COVID-19 infection and deaths reported from the news or social media [25,26]. With the lifestyle changes and threatening information, the general population may avoid contact with other individuals due to great fear of infection, developing feelings of helplessness or suffering from panic [27]. In other words, the general population might experience psychological problems directly due to the COVID-19 pandemic [28].
Different factors contributing to insomnia and psychological problems have been reported. The most important risk factors for insomnia and mental health problems during the COVID-19 pandemic are being a healthcare worker, having an underlying illness, living in rural areas, being a woman, and being at risk of contact with COVID-19 infected patients. Among non-medical healthcare workers, having an underlying disease is a risk factor for insomnia and mental health problems [29]. Indeed, among the natural and non-natural disasters that can occur to humans, the COVID-19 pandemic has caused severe psychological distress due to the large number of individuals affected globally and the contagious and deadly nature of the virus [30]. The COVID-19 pandemic as a worldwide public health issue is a traumatic event that has affected both the sleep and mental health of the general public and healthcare providers [31], [32], [33], [34], [35]. Moreover, several policies implemented to reduce the spread of COVID-19 (e.g., quarantine) have been found to have some negative effects on an individuals’ psychological health [34].
Because sleep is important for human beings to maintain daily functions [36], several studies have focused on sleep problems all with the use of self-report data during the COVID-19 pandemic. Different findings regarding the sleep and psychological problems during COVID-19 in different populations have been reported among these studies. For example, Zhang et al. reported that the prevalence of insomnia was higher among non-medical healthcare workers (e.g., students, community workers, and volunteers) than among medical healthcare workers (prevalence rate of 38.4 vs. 30.5%, p<.01). Wang et al. reported higher prevalence of sleep problem among medical staff compared to non-medical staff comprising students, community workers, and volunteers (66.1% vs. 47.8, p<.01) and frontline healthcare providers compared to non-frontline medical workers (68.1 vs. 64.5, p=0.14) [37].
The quality of sleep during the COVID-19 pandemic and its related factors have been reported in an increasing number of studies. A recent study conducted a meta-analysis to understand the sleep problems during the COVID-19 pandemic [38]. The study found that the pooled prevalence rate of sleep problems globally was 35.7%, with the most affected group being patients with COVID-19 (74.8%), followed by healthcare providers (36.0%), and the general population (32.3%). In addition, sleep difficulties and psychological distress due to COVID-19 on those patients with COVID-19 were reported in a cohort study [39]. Patients with COVID-19 had sleep difficulties, depression, and anxiety at six months after acute infection. Another systematic review found the associations between COVID-19 and psychiatric symptoms among patients with mental illness, healthcare workers, and non-healthcare workers [40]. However, only the information on sleep difficulties has been well analyzed using robust meta-analysis method. Therefore, psychological distress and the associations between sleep problems and psychological distress have yet to be synthesized. Given the significant number of published studies on sleep quality, psychological distress, and related factors, and the importance of systematic reviews and meta-analyses in summarizing and analyzing the results of existing studies, the present study was designed and conducted with the aim of estimating sleep problems during the COVID-19 period (January to October, 2020) and its relationship with psychological distress.
2. Methods
The present systematic review was conducted utilizing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [41]. A systematic literature search was carried out utilizing five academic databases, and relevant studies were extracted and their methodological quality was assessed using the Newcastle Ottawa Scale (NOS) checklist. Findings were synthesized using a meta-analysis approach. The protocol was registered in the PROSPERO International prospective register of systematic reviews (ID code: CRD42020181644 [42]).
2.1. Search strategy
Five academic databases including Scopus, PubMed Central, ProQuest, ISI Web of Knowledge, and Embase were searched systematically between February 17 to 19, 2021. The search terms were extracted from published reviews and primary studies in addition to PubMed Medical Subject Headings (MeSH). The main search terms were ‘sleep’ and ‘COVID-19’. The Boolean search method (AND/OR/NOT) was used to develop the search. Search syntax was customized based on the advanced search attributes of each database. The full search strategy for each database is provided in Supplementary Table 1. Additionally, further sources (i.e., reference lists of included studies and systematic reviews of published papers) were searched to increase the likelihood of retrieving relevant empirical studies.
2.2. Inclusion criteria
Observational studies including case-control studies and cross-sectional studies were included if relevant data relationships were reported (i.e., sleep assessed using the Pittsburgh Sleep Quality Index or Insomnia Severity Index). More specifically, if the studies were included if they estimated the prevalence of sleep disorders and/or examined the relationship between sleep and psychological distress using Pearson's correlation coefficient (e.g., if the odds ratio [OR] information reported by the studies could be converted into Pearson's correlation coefficient; detailed information in 2.6 Data synthesis). English, peer-reviewed papers published between December 2019 and August 2020 were included. There were no limitations regarding participants’ characteristics.
2.2.1. Primary outcome
Estimation of sleep problems frequency was the primary outcome. Sleep problems were defined in a broad category of sleep disorders characterized by either hypersomnolence or insomnia. The three major subcategories of sleep problems were intrinsic (i.e., arising from within the body), extrinsic (secondary to environmental or pathological conditions), and disturbances of circadian rhythm. Sleep problems had to have been assessed using valid and reliable psychometric scales or confirmed with defined cut-off points for characterizing as sleep problems. More specifically, Pittsburgh Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI) were used to assess the primary outcomes because PSQI and ISI have items assessing the three major subcategories of the aforementioned sleep problems. For instance, a global score of 5 or more indicates poor sleep quality on the Pittsburgh Sleep Quality Index [43], or total score of 8 or more on the Insomnia Severity Index [44]
2.2.2. Secondary outcomes
There were three secondary outcomes: (i) association of sleep problems with psychological distress in the context of the COVID-19 pandemic; (ii) heterogeneity and its possible sources; and (iii) moderator variables in association of sleep problems and psychological distress related to COVID-19 pandemic. Ridner defined psychological distress (PD) as: “a state in response to stressors marked by perceived discomfort and inability to cope” [45]. In the present study, psychological distress was considered as either depression (defined as having depressed mood) and/or anxiety (defined as having excessive worry and being nervous). These had to have been assessed using valid and reliable psychometric scales. That is, studies were excluded if psychological distress was assessed using a non-psychometrically validated self-designed questionnaire. Moreover, in the present systematic review and meta-analysis, depression, and anxiety were treated as continuous variables.
2.3. Study screening and selection
In the first step, title and abstract of all retrieved papers were screened independently by two researchers based on the inclusion criteria. The full texts of potentially relevant studies were further examined based on the aforementioned criteria. In this process, relevant studies were selected.
2.4. Quality assessment
The Newcastle Ottawa Scale (NOS) was used to evaluate the methodological quality of the studies in observational studies. Three characteristics (i.e., selection, comparability, and outcome) were examined with the NOS checklist. The checklist has three versions for evaluating cross-sectional studies (seven items), case-control studies (eight items), and cohort studies (eight items). Despite a slight difference in number and content of items, each item is rated with a star, except comparability which can have two stars. This results in a maximum quality score of 9 for each study. Studies with less than 5 points are classified as having a high risk of bias [46]. No studies were excluded based on the quality rating. However, subgroup analysis was conducted to assess the impact of quality on pooled effect size
2.5. Data extraction
A pre-designed form was prepared to extract data from included studies. Data including first author's name, collection date, study design, country, number of participants, gender, mean age, scales used to assess psychological distress and sleep problems, numerical results regarding the frequency of sleep problems, and relationship between sleep problems and psychological distress. It should also be noted that study selection, quality assessment, and data extraction were processes performed independently by two reviewers. Disagreements were resolved through discussion.
2.6. Data synthesis
A quantitative synthesis using STATA software version 14 was conducted. Meta-analysis was run using random effect model because included studies were taken from different populations, and both within-study and between-study variances should be accounted for [47]. The Q Cochrane statistic was used to assess heterogeneity. Also, the severity of heterogeneity was estimated using the I2 index. Heterogeneity is interpreted as (i) mild when I2 is less than 25%, (ii) moderate when I2 is 25 to 50%, (iii) severe when I2 is 50 to 75%, and (iv) highly severe when I2 is greater than 75% [48].
Two key measures were selected for present study: (i) prevalence of sleep problems and (ii) correlation of sleep problem with psychological distress. The numerical findings regarding prevalence of sleep problems were reported consistently in 177 included studies. This key measure and its 95% confidence interval (CI) are reported. However, the association between sleep problems and psychological distress was reported differently in the included studies. Pearson's correlation coefficient was the selected effect size for meta-analysis. Due to the inconsistency in reporting numerical findings of this association, the other effect sizes of standardized mean difference and crude odds ratio were transformed into Pearson's correlation coefficients [49,50] using the Psychometrica website [51]. Also, Pearson's r correlation coefficient was converted to Fisher's z, due to the potential instability of variance. Consequently, all analyses were performed using Fisher's z values as effect size (ES) [52,53]. Fisher's z-transformation was applied using the following formula: z = 0.5 × ln(1+r-1-r). The standard error of z was calculated based on the following formula: SEz = 1/√ (n-3) [54]. Therefore, the selected measure of effect, selected for current meta-analysis, is expressed as Fisher's z score and its 95% CI.
For assessing moderator analysis and finding the possible sources of heterogeneity, subgroup analysis or meta-regression was carried out based on the number of studies in each group. Moreover, the three subgroups for synthesized analyses (i.e., general population, healthcare professionals, and patients) did not have any overlapping participants. More specifically, the general population did not include healthcare professionals or patients. If the number of studies in any group was less than four studies, meta-regression was used. Funnel plot and the Begg's Test were used to assess publication bias [55]. The Jackknife method was used for sensitivity analysis [56].
2.7. Role of the funding source
The present systematic review and meta-analysis did not receive any specific funding. However, one of the authors (Dr. C-Y Lin) received a grant on COVID-19 research to support his works on COVID-19. The grant that Dr. Lin received had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
3. Results
3.1. Study screening and selection process
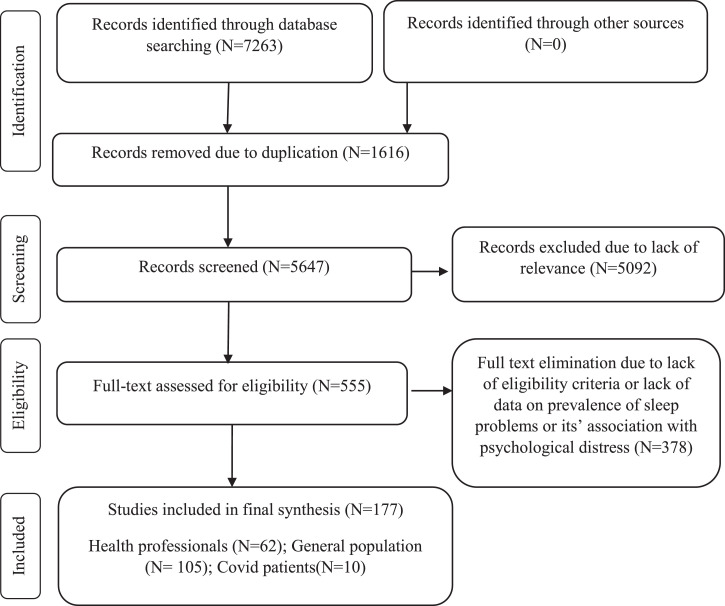
The initial search in five databases resulted in 7263 studies: Scopus (n=2518), ISI Web of Knowledge (n=474), PubMed (n=338), Embase (n=1426), and ProQuest (n=2507). After removing duplicate papers, a further 5647 papers were screened based on title and abstract. Finally, 555 papers appeared to be potentially eligible and their full-texts were reviewed. In this process, 177 studies met the eligibility criteria and were pooled in the meta-analysis. Figure 1 shows the search process based on the PRISMA flowchart.
Figure 1.
PRISMA Flowchart of selected studies
3.2. Study description
All the included studies (N=177) collected the data online and comprised 345,270 participants from 39 different countries (, Algeria, Argentine, Australia, Austria, Bahrain, Bangladesh, Belgium, Brazil, Canada, China, Colombia, Egypt, Ethiopia, Finland, France, Greece, India, Iran, Iraq, Israel, Italy, Lebanon, Malaysia, Morocco, Nepal, Netherlands, Nigeria, Oman, Pakistan, Palestine, Poland, Qatar, Saudi Arabia, Serbia, Spain, Sweden, Syria, Turkey, Tunisia, United Arab Emirates, UK, USA, and Vietnam). Of these, 28 studies collected data during the national lockdown period in the respective countries. The two countries with the highest number of eligible studies were China (N=76) and Italy (n=17). The smallest sample size was 20, and the largest sample size was 56,932. The mean age of participants varied from 15.26 years to 69.85 years. Approximately two-thirds of overall participants were females (63.5%) and one-third were married (35.33%). The most frequently used study design was cross-sectional (n=168). Four studies had a case-control design and five studies had a longitudinal design. In longitudinal studies, collected data during the COVID-19 pandemic were extracted. Various measures were used to assess sleep problems, with the Insomnia Severity Scale (ISI; n=93) and Pittsburgh Sleep Quality Index (PSQI; n=60) being the most frequently used scales in the studies. Psychological distress was also assessed with different measures, with the Patient Health Questionnaire (PHQ; n=73) and Generalized Anxiety Disorder Scale (GAD; n=75) being the most frequently used scales in the studies. Table 1 provides the summary characteristics of all included studies.
Table 1.
Data extraction- Summarized characteristics
| ID | Authors | Year | Country | Collection Date | Lock down Period | Design | Participant Group | Sample Size | Sex % Female | % Married | Mean Age/ Age range (Years) | NOS | Sleep Problem Scale | Psychological Distress Scale |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | Xiao [67] | 2020 | China | January and February 2020 | no | Cross-sectional | Medical Staff | 180 | 71.7 | 67.8 | 32.31 | 5 | PSQI | Self-Rating Anxiety Scale |
| 3 | Zhang [68] | 2020 | China | 29 January to 3 February 2020 | no | Cross-sectional | Medical staff | 1563 | 82.73 | 63.92 | 18 to above 60 | 5 | ISI | GAD-7 PHQ-9 |
| 5 | Huang [69] | 2020 | China | 3 February to 10 February 2020 | no | Cross-sectional | Volunteer population | 603 | 69 | 36.5 | 5 | PSQI | GAD-7 & CESD |
|
| 10 | Xiao [70] | 2020 | China | January 2020 | yes | Cross-sectional | Individuals who self-isolated | 170 | 40.5 | 64.7 | 37.78 | 4 | PSQI | Self-Rating Anxiety Scale |
| 12 | Zhang [29] | 2020 | China | February 19 to March 6, 2020 | no | Cross-sectional | Medical health workers | 2182 | 64.2 | 82 | less than 18 to above 60 | 5 | ISI | PHQ-4 |
| 16 | Wanqiu [71] | 2020 | China | 24 Feb to 25 Feb 2020 | no | Cross-sectional | Workforce | 673 | 25.6 | 54.4 | 30.8 | 5 | ISI | Impact of Event Scale-Revised, DASS-21 |
| 18 | Qi [32] | 2020 | China | February 2020 | no | Cross-sectional | Frontline medical workers | 1306 | 80.4 | 68.4 | 33.1 | 3 | PSQI | anxiety and depression VAS |
| 21 | Rossi [72] | 2020 | Italy | March 27th and April 6th 2020 | no | Cross-sectional | General population | 18147 | 79.5 | 38 | 5 | ISI | PHQ-9 GAD-7 |
|
| 23 | Tu [73] | 2020 | China | February 7 to 25, 2020 | no | Cross-sectional | Frontline nurses | 100 | 100 | 70 | 34.44 | 7 | PSQI | PHQ-9 GAD-7 |
| 24 | Jahrami [74] | 2020 | Bahrain | April 2020 | no | Cross-sectional | Frontline healthcare workers | 257 | 70 | 89.1 | 40.2 | 7 | PSQI | PSS (Perceived Stress Scale) |
| 25 | Lin [31] | 2020 | China | February 5 to 23, 2020 | no | Cross-sectional | Adults | 5461 | 70.1 | less than 18 to above 60 | 3 | ISI | PHQ-9 GAD-7 |
|
| 26 | Magnavita [75] | 2020 | Italy | March 2020 | no | Cross-sectional | Health care workers | 595 | 70.1 | 76.13 | less than 35 to above 55 | 7 | Sleep Condition Indicator (SCI) | Goldberg Anxiety and Depression Scale (GADS) |
| 27 | Romero-Blanco [76] | 2020 | Spain | 1 and 15 April, 2020 | yes | Cross-sectional | Nursing students/ post 4 weeks lockdown | 207 | 81.6 | 20.57 | 6 | PSQI | EQ-5D | |
| 28 | Fu [77] | 2020 | China | February 18 to 28, 2020 | no | Cross-sectional | Wuhan residents | 1242 | 69.73 | 33.7 | above 18 | 5 | AIS | PHQ-9 |
| 29 | Guo [78] | 2020 | China | 1–10 February 2020 | no | Cross-sectional | Adults | 2441 | 52.4 | 70.3 | 18 to above 51 | 6 | PSQI | CESD |
| 30 | Zhang [79] | 2020 | China | February 19 to March 20, 2020 | no | Longitudinal surveys | College students | 66 | 62.12 | 20.70 | 5 | PSQI | DASS-21 | |
| 32 | Li [80] | 2020 | China | 25 April to 9 May 2020 | no | Cross-sectional | Workers with income losses | 398 | 49.5 | 49.5 | 18 to above 40 | 9 | ISI | GAD-7 PHQ-9 |
| 34 | Wang [81] | 2020 | China | 30 January to 7 February 2020 | no | Cross-sectional | Medical workers | 123 | 90 | 30.08 | 33.75 | 6 | PSQI | SAS SDS |
| 35 | Hu [82] | 2020 | China | March 7 to 24, 2020 | no | Cross-sectional | COVID-19 inpatients | 85 | 49.4 | 85.9 | 48.8 | 6 | ISI | GAD-7 PHQ-9 |
| 36 | Yang [83] | 2020 | China | March 5 to 14, 2020 | no | Cross-sectional | General population | 2,410 | 49.2 | 76.55 | 36.3 | 5 | PSQI | GAD-7 PHQ-9 |
| 37 | Wang [68] | 2020 | China | 26 February and 3 March, 2020 | no | Cross-sectional | Medical staff |
274 | 77.4 | 81.8 | 37 | 5 | PSQI | GAD-7 PHQ-9 |
| 39 | Marelli [84] | 2020 | Italy | March 24 to May 3, 2020 | no | Cross-sectional | University students and staff |
400 | 75.8 | 29.93 | 5 | PSQI | Beck Anxiety Inventory/ Beck Depression Inventory- II |
|
| 42 | Wu [85] | 2020 | China | February 2020 | no | Case- control | Frontline vs. non frontline clinical staff |
120 | 74.15 | 33.65 | 4 | PSQI | Self-rating Anxiety Scale (SAS), Selfrating Depression Scale (SDS) |
|
| 45 | Gualano [86] | 2020 | Italy | April 19th and May 3rd 2020 | yes | Cross-sectional | General population | 1515 | 65.6 | 61.1 | 42 | 5 | ISI | GAD-7 PHQ-9 |
| 53 | Peng [87] | 2020 | China | February 14 to March 4, 2020 | yes | Cross-sectional | General population | 2237 | 41.66 | 68.44 | 35.93 | 5 | PSQI | Zung's Self-Rating Depression Scale (SDS) & self-rating anxiety scale |
| 57 | Pieh [88] | 2020 | Austria | April 15th to 30th, 2020 | yes | Cross-sectional | General population | 1005 | 52.7 | 18 to above 65 | 6 | ISI | GAD-7 PHQ-9 |
|
| 59 | Zhao [89] | 2020 | China | February 18 to 25, 2020 | no | Cross-sectional | General population | 1630 | 29.17 | 5 | PSQI | Self-Rating Anxiety Scale | ||
| 61 | Huang [90] | 2020 | China | February 3 to 17, 2020 | no | Cross-sectional | General public | 7236 | 54.6 | 35.3 | 4 | PSQI | GAD-7 CES_D |
|
| 63 | Assenza [91] | 2020 | Italy | April 11, 2020 | no | Cross-sectional | General population | 928 | 74.46 | 41.81 | 40.10 | 5 | PSQI | Beck Depression Inventory- II |
| 64 | Que [92] | 2020 | China | February 2020 | no | Cross-sectional | Healthcare workers | 2285 | 69.06 | 31.06 | 5 | ISI | GAD-7 PHQ-9 |
|
| 65 | Zhuo [67] | 2020 | China | March 2020 | no | Cross-sectional | Medical staff | 26 | 46.15 | 41.92 | 5 | ISI | Chinese version of the Self-Reporting Questionnaire (SRQ-20) |
|
| 67 | Mazza [93] | 2020 | Italy | April 6 to June 9, 2020 | no | Cross-sectional | COVID-19 survivors | 402 | 65.92 | 57.8 | 6 | Medical Outcomes Study Sleep Scale (MOS-SS) |
Zung Self-Rating Depression Scale/ 13-item Beck's Depression Inventory (BDI-13) /State-Trait Anxiety Inventory form Y (STAI-Y) |
|
| 68 | Song [94] | 2020 | China | 9–22 April, 2020 | no | Cross-sectional | People resuming Work |
709 | 74.2 | 35.35 | 5 | ISI | GAD-7 CESD |
|
| 69 | Wang [95] | 2020 | China | 2nd and 3rd February 2020 | no | Cross-sectional | Medical staff | 1045 | 85.8 | 7 | ISI | HADS | ||
| 70 | Shi [96] | 2020 | China | February 28 to March 11, 2020 | no | Cross-sectional | General population | 56932 | 52.1 | 77.2 | 35.97 | 7 | ISI | GAD PHQ |
| 71 | Hao [97] | 2020 | China | 19 to 22 February 2020 | yes | Case control | Psychiatric patients (n = 76); Healthy controls (n = 109) |
185 | 49.75 | 32.95 | 4 | ISI | DASS-21 | |
| 72 | Caballero-Domínguez [98] | 2020 | Colombia | March 30 to April 8, 2020 | yes | Cross-sectional | 700 | 68.0 | 48 | 37.1 | 6 | AIS | WHO-5 (depression) CESD |
|
| 73 | Liu [99] | 2020 | USA | April 13 to May 19, 2020 | no | Cross-sectional | Young adults with suspected and reported psychiatric diagnoses |
898 | 81.3 | 24.47 | 5 | MOS-Sleep Problems | PHQ-8 GAD-7 |
|
| 74 | Stojanov [100] | 2020 | Serbia | no | Cross-sectional | Healthcare professionals |
201 | 65.95 | 40.8 | 3 | PSQI | GAD-7, Self-rating Depression Scale | ||
| 76 | Cheng [101] | 2020 | China | February 9th to the 13th, 2020 | no | Cross-sectional | Medical staff | 534 | 82.4 | 20 to above 50 | 6 | PSQI | self-rating anxiety scale |
|
| 77 | Cellini [102] | 2020 | Italy | March 24 to 28, 2020 | yes | Cross-sectional | COVID-19 lockdown | 1310 | 67.18 | 23.91 | 3 | PSQI | DASS-21 | |
| 78 | Amerio [103] | 2020 | Italy | March 15 to April 15, 2020 | no | Cross-sectional | General practitioners |
131 | 48.1 | 70.2 | 52.31 | 3 | ISI | PHQ-9 GAD-7 |
| 79 | Cai [104] | 2020 | China | February 11 to 26, 2020 | no | Case-control | Frontline and non-frontline medical workers | 2346 |
70 | 83.2 | 30.55 | 5 | ISI | Beck Anxiety Inventory PHQ-9 |
| 82 | Wang [37] | 2020 | China | March 4 to 9, 2020 | no | Cross-sectional | Healthcare workers | 2737 | 64.5 | 70.9 | 18-65 | 6 | PSQI | HADS |
| 85 | Idrissi [105] | 2020 | Morocco | April 1, to May 1, 2020 | yes | Cross-sectional | General population | 846 | 52.2 | 35.9 | 5 | AIS, ESS | Hamilton Anxiety Rating Scale (HARS) and Beck Depression Inventory (BDI |
|
| 87 | Zhou [106] | 2020 | China | March 8 to March 15, 2020 | no | Cross-sectional | Adolescents and young adults | 11835 | 57.7 | 17.41 | 6 | PSQI | GAD-7 PHQ-9 |
|
| 96 | Juanjuan [107] | 2020 | China | February 16 to 19, 2020 | no | Cross-sectional | Breast cancer patients | 658 | 100 | less than 45 to above 65 | 6 | ISI | GAD-7 PHQ-9 |
|
| 97 | Huang [108] | 2020 | China | February 2 and March 5, 2020 | yes | Cross-sectional | Patients with epilepsy |
362 | 45.86 | 10 to above 60 | 7 | ISI | GAD-7 PHQ-9 |
|
| 98 | Mamun [63] | 2020 | Bangladesh | April 1-10, 2020 | no | Cross-sectional | General population | 10067 | 28.2 | 43.9 | 29.94 |
6 | ISI | PHQ-9 |
| 11 | Lai [109] | 2020 | China | January 29 to February 3, 2020 | no | Cross-sectional | Healthcare workers | 1257 | 76.7 | 66.7 | 18 to above 40 | 6 | ISI | GAD-7 PHQ-9 |
| 13 | Kang [110] | 2020 | China | January 29 to February 4, 2020 | no | Cross-sectional | Healthcare workers | 994 | 85.5 | 56.9 | 18 to above 50 | 6 | ISI | GAD-7 PHQ-9 |
| 38 | Zhan [111] | 2020 | China | March 3–10, 2020 | no | Cross-sectional | Healthcare workers | 1794 | 97 | less than 25 to above 65 | 6 | AIS | ||
| 43 | Wang [112] | 2020 | China | 23 March to 26 April 2020 | yes | Cross-sectional | General population | 2289 | 51.38 | 30 | 27.5 | 6 | PSQI | |
| 46 | Zhou [113] | 2020 | China | 24 March to 3 April 2020 | no | Cross-sectional | Healthcare workers | 1931 | 95.4 | 63.4 | 35.08 | 5 | PSQI | |
| 56 | Zhang [114] | 2020 | China | January 25 and March 15 | no | Retrospective cohort | Covid-19 patients | 136 | 42.2 | 95.6 | 63 | 6 | PSQI | |
| 554 | Wasim [115] | 2020 | Pakistan | 20th May to 3rd June 2020 | no | Cross-sectional | Tertiary care hospital dealing with corona patients | 356 | 52.00 | 51.40 | 20 to above 50 | 6 | ISI | DASS-21 |
| 553 | Lu [116] | 2020 | China | May 13 to 20 | no | Cross-sectional | Middle school students | 965 | 42.40 | 15.26 | 9 | Youth Self-Rating Insomnia Scales | PHQ-9 GAD-7 |
|
| 544 | Yitayih [117] | 2020 | Ethiopia | 22 and 28 March 2020 | no | Cross-sectional | Healthcare professionals | 249 | 52.60 | 27.40 | 6 | ISI | 0.00 | |
| 542 | Tselebis [118] | 2020 | Greece | half of May 2020 | no | Cross-sectional | Nursing Staff | 150 | 80.00 | 42.29 | 7 | AIS | 0.00 | |
| 541 | Liu [119] | 2021 | China | 7 to 17 March 2020 | no | Cross-sectional | Obstetrics staff | 2259 | 97.70 | 16–65 | 5 | ISI | PHQ-9 GAD-7 |
|
| 540 | Rossi [120] | 2020 | Italy | March 25th and April 7th. 2020 | no | Cross-sectional | General population + healthcare professionals | 24048 | 80.39 | 48.31 | 6 | ISI | PHQ-9 GAD-7 |
|
| 537 | Sharma [121] | 2020 | India | 0 | no | Cross-sectional | Obstetrics staff | 184 | 58.70 | 54.35 | 20 to above 50 | 5 | ISI | DASS-21 |
| 536 | Ammar [122] | 2020 | Multi country | April 11 to, 2020 | Data on both before and during lockdown period is provided | Cross-sectional | General population | 1047 | 53.80 | 53.70 | 18 to above 50 | 6 | PSQI | 0.00 |
| 535 | Tiete [123] | 2021 | Belgium | April 17th to May 25th, 2020 | no | Cross-sectional | Healthcare professionals | 647 | 78.40 | 80.50 | 20 to above 50 | 8 | ISI | DASS-21 |
| 511 | Franceschini [124] | 2020 | Italy | March 10 to May 4, 2020 | yes | Cross-sectional | General population | 6439 | 73.10 | 65.10 | 33.90 | 6 | Medical Outcomes Study–Sleep Scalbe (MOS-SS | DASS-21 |
| 507 | Huang [125] | 2020 | China | 0 | no | Cross-sectional | Nurses | 881 | 91.20 | 5 | PSQI | 0.00 | ||
| 506 | Elkholy [126] | 2020 | Egypt | April and May 2020 | no | Cross-sectional | Healthcare workers | 502 | 50.00 | 60 | 20 to above 40 | 8 | ISI | PHQ-9 GAD-7 |
| 502 | Yang [127] | 2020 | China | 6 to 8 June 2020 | no | Cross-sectional | Healthcare workers | 15000 | 57.10 | less than 18 to above 60 | 6 | ISI | PHQ-9 | |
| 495 | Yang [128] | 2020 | China | January to May 2020 | no | Cross-sectional | Young cancer patients | 197 | 54.82 | 36.50 | 5 | PSQI | self-rating Anxiety Scale | |
| 490 | Caballero‐Domínguez [129] | 2020 | Colombia | March 30 to April 8, 2020 | yes | Cross-sectional | General population | 700 | 68 | 48 | 37.10 | 8 | AIS | Well‐Being Index |
| 462 | Khamis [130] | 2020 | Oman | first two weeks of April 2020 | no | Cross-sectional | Healthcare professionals | 402 | 100 | 77.30 | 36.40 | 5 | SQS | GAD-7 |
| 472 | Sañudo [131] | 2020 | Spain | one-week period from February 2020 & 24 March to 3 April 2020 in locking period | data on both prior and during locking period | Cross-sectional | General population | 20 | 47 | 22.60 | 5 | PSQI | ||
| 460 | Jain [132] | 2020 | India | 12 to 22 May 2020 | no | Cross-sectional | Anesthesiologists | 512 | 44.30 | 64.70 | less than 30 to above 60 | 7 | ISI | GAD-7 |
| 454 | Agberotimi [133] | 2020 | Nigeria | March 20 to April 19, 2020 | yes | Cross-sectional | General population + healthcare professionals | 884 | 45.50 | 65.30 | 6 | ISI | PHQ-9 GAD-7 |
|
| 447 | Bhat [134] | 2020 | Kashmir | 4 to 10 April 2020 | no | Cross-sectional | General population | 264 | 27.70 | less than 18 to above 60 | 8 | PSQI | HADS | |
| 442 | McCracken [135] | 2021 | Sweden | 14th of May and the June 11, 2020 | no | Cross-sectional | General population | 1102 | 75.20 | 56.30 | 36.90 | 6 | ISI | PHQ-9 GAD-7 |
| 439 | Trabelsi [136] | 2021 | Multi country | 6 April to 28 June 2020 | data on both prior and during locking period | Cross-sectional | General population | 5056 | 59.40 | 50.20 | less than 18 to above 55 | 6 | PSQI | |
| 438 | Chi [137] | 2020 | China | May 13 and 20, 2020 | no | Cross-sectional | Adolescents | 1794 | 43.90 | 15.26 | 7 | YSIS | PHQ-9 GAD-7 |
|
| 420 | Liu [138] | 2021 | China | February 1 to 10th in 2020 | no | Cross-sectional | General population | 2858 | 53.60 | 60.20 | less than 18 to above 50 | 6 | PSQI | |
| 410 | Alamrawy [139] | 2021 | Egypt | 2 July to 23 July 2020 | no | Cross-sectional | Young adults of both genders aged between 14 and 24 years |
447 | 70.20 | 20.72 | 8 | ISI | PHQ-9 GAD-7 |
|
| 408 | Haravuori [140] | 2020 | Finland | 4 June to 26 June 2020 | no | Cross-sectional | General population + healthcare professionals | 4804 | 87.50 | 45 | 6 | ISI | PHQ-2 Overall Anxiety and Impairment Scale (OASIS) |
|
| 405 | Khaled [141] | 2021 | Qatar | Feb-20 | no | Cross-sectional | General population | 1160 | 53.20 | 79.30 | above 18 | 8 | Sleep Condition Indicator (SCI) | PHQ-9 GAD-7 |
| 403 | Alomayri [142] | 2020 | Saudi Arabia | July and August 2020 | no | Cross-sectional | Patients with atopic dermatitis | 400 | 86 | 18 to above 55 | 7 | PSQI | 0.00 | |
| 397 | Akıncı [143] | 2021 | Turkey | April and May of 2020 | no | Cross-sectional | Patients hospitalised with COVID-19 | 189 | 41 | 82.50 | 46.27 | 6 | PSQI | HADS |
| 394 | Barua [144] | 2021 | Bangladesh | 1st April to 30th May 2020 | no | Cross-sectional | Healthcare professionals | 370 | 39.70 | 66.80 | 30.50 | 8 | Sleep Condition Indicator (SCI-02) | PHQ-2 GAD-2 |
| 391 | Wang [145] | 2020 | China | February 3 to 7, 2020 | no | Cross-sectional | General population | 19372 | 51.96 | 11 or older | 6 | ISI | PHQ-9 GAD-7 |
|
| 389 | Fidanci [146] | 2020 | Turkey | May-20 | no | Cross-sectional | Healthcare professionals | 153 | 67.30 | 33.40 | 5 | PSQI | 0.00 | |
| 382 | Chouchou [147] | 2020 | France | 0 | data on both prior and during locking period | Cross-sectional | General population | 400 | 58.25 | 29.80 | 6 | PSQI | 0.00 | |
| 378 | Cheng [148] | 2020 | UK & US | 16 - 22 March 2020 & 18–24 May 2020 | no | Cross-sectional | General population | 2278 | 53.5 | 6 | PROMIS | State-Trait Anxiety Inventory | ||
| 376 | Gu [87] | 2020 | China | February 15 -22, 2020 | no | Cross-sectional | Patients with COVID-19 | 461 | 64.90 | 95.90 | 18 to above 50 | 5 | ISI | PHQ-9 GAD-7 |
| 371 | Pedrozo-Pupo [149] | 2020 | Colombia | 0 | no | Cross-sectional | Asthma and COPD patient |
227 | 64.70 | 60.40 | 5 | AIS | PHQ-9 | |
| 370 | Targa [150] | 2020 | Spain | April 28 to May 12, 2020 | no | Cross-sectional | General population | 71 | 75.00 | 40.70 | 5 | PSQI | Profile of mood states- depression | |
| 364 | Than [151] | 2020 | Vietnam | March and April 2020 | no | Cross-sectional | Healthcare professionals | 173 | 68.20 | 31.00 | 5 | ISI | DASS-21 | |
| 359 | Youssef [152] | 2020 | Egypt | Apr-20 | no | Cross-sectional | Healthcare professionals | 540 | 45.60 | 74.10 | 37.30 | 6 | ISI | DASS-21 |
| 357 | Ge [153] | 2020 | China | February 10th to 13th, 2020 | no | Cross-sectional | Undergraduate student | 2009 | 50.97 | 6 | ISI | GAD-7 | ||
| 348 | Almater [154] | 2020 | Saudi Arabia | March 28 to April 4 2020 | no | Cross-sectional | Ophthalmologists | 107 | 43.90 | 32.90 | 8 | ISI | GAD-7 | |
| 315 | Gupta [155] | 2020 | India | early May 2020 | no | Cross-sectional | General population + healthcare professionals | 958 | 41 | 67 | 37 | 6 | ISI | 0 |
| 4 | Varma [156] | 2021 | Australia | April 9 and May 25, 2020 | yes | Cross-sectional | General population | 1653 | 67.70 | 42.90 | 6 | PSQI | PHQ-9 State-Trait Anxiety Inventory |
|
| 5 | Li [157] | 2021 | China | May 22 and July 15, 2020 | no | Cross-sectional | Clinically stable older patients with psychiatric disorders |
1063 | 67.40 | 90.40 | 62.80 | 8 | ISI | PHQ-9 GAD-7 |
| 6 | Duran [158] | 2021 | Turkey | Oct-2020 | no | Cross-sectional | General population | 405 | 70.86 | 36.30 | 8 | PSQI | ||
| 7 | Yang [159] | 2021 | China | March 5 -9, 2020 | no | Cross-sectional | Healthcare providers | 1036 | 72.90 | 66.00 | 20 to above 50 | 8 | ISI | |
| 8 | Martínez-de-Quel- Before Lock down [160] | 2021 | Spain | March 16 and March 31, 2020 & April 30 and May 11, 2020 | data on both prior and during locking period | Longitudinal | General population | 161 | 37.00 | 35.00 | 6 | PSQI | ||
| 12 | Khoury [161] | 2021 | Canada | June 3 and July 31, 2020 | no | Cross-sectional | Pregnant individuals | 303 | 100.00 | 100.00 | 32.13 | 7 | ISI | CESD Cambridge Worry Scale (CWS) |
| 17 | Wang [162] | 2021 | China | January 28 to March 31, 2020 |
no | Cross-sectional | General population | 5676 | 71.40 | 68.90 | 6 | ISI | PHQ-9 GAD-7 |
|
| 25 | Zreik [163] | 2021 | Israel | 20 to 30April 2020 | yes | Cross-sectional | General population | 264 | 100 | 100 | 33.97 | 5 | ISI | Trait Anxiety Scale |
| 38 | Zhang [164] | 2021 | China | mid-February to late March 2020 | no | Cross-sectional | Medical Staff | 319 | 62.1 | 30.42 | 7 | PSQI | HADS | |
| 41 | Al Ammari [165] | 2021 | Saudi Arabia | 27 April to 4 May 2020 | no | Cross-sectional | Medical Staff | 720 | 64.17 | 35.14 | 18 to above 40 | 6 | ISI | PHQ-9 GAD-7 |
| 45 | Essangri [166] | 2021 | Morocco | April 8 to April 18, 2020 | no | Cross-sectional | Medical Students | 549 | 74 | 18.4 | 22 | 8 | ISI | PHQ-9 GAD-7 |
| 46 | Yitayih [167] | 2020 | Ethiopia | 22 to 28 March 2020 | no | Cross-sectional | General population | 247 | 23.5 | 63.2 | 30.47 | 7 | ISI | 0 |
| 47 | Xie [168] | 2020 | China | 0 | no | Cross-sectional | Pregnant individuals | 689 | 100 | 100 | 29.03 | 6 | PSQI | 0 |
| 48 | Zhang [169] | 2021 | China | January to February 2020 | no | Cross-sectional | Pregnant individuals | 456 | 100 | 100 | 6 | PSQI | 0 | |
| 57 | Massicotte [170] | 2021 | Canada | 28 April and 29 May 2020 | no | Cross-sectional | Breast Cancer Patients | 36 | 100 | 66.7 | 53.6 | 5 | ISI | HADS |
| 64 | Poyraz [171] | 2021 | Istanbul | March 16 and June 14, 2020 | no | Cross-sectional | Covid patient after initial treatment | 284 | 49.8 | 65 | 39.7 | 5 | ISI | HADS |
| 67 | Chen [172] | 2021 | China | March 14- 21, 2020 | no | Cross-sectional | Breast cancer patients | 834 | 100 | 86 | 5 | ISI | PHQ-9 GAD-7 |
|
| 69 | Lahiri [173] | 2021 | India | April 20 e May 19, 2020 | yes | Cross-sectional | General population | 1081 | 41.72 | 52.91 | 8 | ISI | GAD-7 | |
| 70 | Cellini [174] | 2021 | Italy & Belgium | April 1st to May 19th, 2020 | Data on both prior and during locking period | Cross-sectional | General population | 2272 | 75.25 | 38.55 | 6 | PSQI | ||
| 75 | Lin [119] | 2021 | Hong Kong | 20 February to 29 February 2020 | no | Cross-sectional | General population | 1897 | 43.6 | 36.6 | 7 | PSQI | 0 | |
| 80 | Sunil [175] | 2021 | India | June to july 2020 | no | Cross-sectional | Medical staff | 313 | 64.5 | Above 21 | 8 | ISI | PHQ GAD |
|
| 81 | Yadav [176] | 2021 | India | June to August 2020 | no | Cross-sectional | COVID-19 patients | 100 | 27 | 42.9 | 5 | ISI | PHQ GAD |
|
| 82 | Scotta [177] | 2020 | Argentina | 0 | yes | Cross-sectional | University students | 584 | 81 | 42 | 22.49 | 6 | ISI | 0 |
| 84 | He [178] | 2020 | China | 29 February 2020 to 1 May 2020 | no | Cross-sectional | General population, healthcare workers and quarantined population |
2689 | 70.1 | 42.84 | 56.84 | 6 | PSQI | PHQ GAD |
| 85 | Zhang [179] | 2020 | China | February 16th to 2020 March 2th. | no | Cross-sectional | Medical staff | 524 | 74.4 | 80 | 34.87 | 6 | ISI | PHQ GAD |
| 87 | Demartini [180] | 2020 | Italy | 24 to 31 March 2020 | no | Cross-sectional | General population + healthcare professionals | 432 | 72 | 35.9 | 6 | PSQI | DASS-21 | |
| 91 | Cui [181] | 2020 | China | February 1 to 19, 2020 | no | Cross-sectional | Breast cancer patients and female nurses |
891 | 100 | 74.21 | 18 to above 40 | 9 | ISI | PHQ GAD |
| 92 | Bacaro [182] | 2020 | Italy | 1st of April to 4th May 2020 | yes | Cross-sectional | General population | 1989 | 76.17 | 38.4 | 7 | ISI | HADS | |
| 93 | Gu [183] | 2020 | China | February 21 to28, 2020 | no | Cross-sectional | Healthcare workers | 522 | 77.6 | 62.1 | 18 to above 40 | 9 | ISI | PHQ GAD |
| 95 | Liu [184] | 2020 | China | February 14 to March 29, 2020 | no | Cross-sectional | Healthcare workers | 606 | 81.2 | 74.91 | 35.77 | 9 | ISI | 0 |
| 96 | Wang [185] | 2020 | China | February10-20, 2020 | no | Cross-sectional | General population | 4191 | 62 | 81.63 | 36.15 | 9 | ISI | PHQ BAI |
| 106 | Zhou [80] | 2020 | China | February 28–March 12, 2020 |
no | Cross-sectional | General population of pregnant and non-pregnant women | 859 | 100 | 93.25 | 33.25 | 9 | ISI | PHQ GAD |
| 109 | Abdulah [186] | 2020 | Iraq | 0 | no | Cross-sectional | Healthcare workers | 268 | 29.9 | 35.06 | 8 | Athens Insomnia Scale |
0 | |
| 112 | Zhou [106] | 2020 | China | February 14 to March 29, 2020. |
no | Cross-sectional | General population + healthcare professionals | 1705 | 73.61 | 50.85 | 32.5 | 9 | ISI | PHQ GAD |
| 113 | Ren [95] | 2020 | China | February 14 to March 29, 2020 |
no | Cross-sectional | General population | 1172 | 69.3 | 39.3 | 22 | 7 | ISI | PHQ GAD |
| 114 | Cai [187] | 2020 | China | January 29 to February 2 & February 26 to February 28, 2020 | no | Cross-sectional | Nurses | 1330 | 97 | 56.32 | 18 to above 40 | 9 | ISI | PHQ GAD |
| 116 | Giardino [82] | 2020 | Argentina | Jun-20 | no | Cross-sectional | healthcare workers | 1059 | 72.7 | 41.7 | 7 | ISI | 0 | |
| 118 | Kocevska [188] | 2020 | Netherlands | 0 | yes | Cross-sectional | General population | 667 | 7 | ISI | 0 | |||
| 119 | Zhang [189] | 2020 | China | February 5, 2020, to March 6, 2020 | no | Cross-sectional | COVID-19 patients | 30 | 50 | 80 | 42.5 | 9 | ISI | PHQ GAD |
| 120 | Fazeli [190] | 2020 | Iran | 2 May to 26 August 2020 |
no | Cross-sectional | Adolescents | 1512 | 43.6 | 15.51 | 9 | ISI | DASS-21 | |
| 123 | Bajaj [191] | 2020 | India | 25th March 2020-1st April 2020 | yes | Cross-sectional | General population | 391 | 53.45 | 18 to above 40 | 7 | ISI | 0 | |
| 125 | Kilani [192] | 2020 | Arab Countries | 17th–24th, April 2020. | no | Cross-sectional | General population | 1723 | 46.78 | 55 | 34.9 | 9 | PSQI | 0 |
| 126 | Necho [193] | 2020 | Ethiopia | July 15 to 30/2020 | no | Cross-sectional | individuals living with disabilities | 423 | 40.7 | 51.4 | 36.66 | 9 | ISI | PHQ GAD |
| 130 | Şahin [194] | 2020 | Turkey | 23 April and 23 May 2020 |
no | Cross-sectional | Healthcare workers | 939 | 66 | 65.7 | 18 to above 40 | 9 | ISI | PHQ GAD |
| 136 | McCall [195] | 2020 | USA | 15-May-20 | no | Cross-sectional | health care workers | 573 | 72 | 43.4 | 9 | RDC definition of insomnia disorder | PHQ GAD |
|
| 137 | Lai [196] | 2020 | UK | April 28 through May 12, 2020 | no | Cross-sectional | International university students | 124 | 63.7 | 9 | ISI | PHQ | ||
| 138 | Wang [197] | 2020 | China | February 21 to March 7, 2020 | no | Cross-sectional | College students | 3092 | 66.4 | 9 | Self-Rating Scale of Sleep (SRSS | GAD | ||
| 139 | Sagherian [198] | 2020 | USA | May–June 2020 | no | Cross-sectional | Nursing staff | 564 | 94.06 | 69.36 | 18 to above 40 | 9 | ISI | 0 |
| 150 | Magnavita [199] | 2020 | Italy | 27 April and 27 May 2020 | no | Cross-sectional | Anesthetists | 90 | 52.2 | 66.7 | 9 | Sleep Condition Indicator | Goldberg Anxiety and Depression Scale | |
| 155 | Casagrande [200] | 2020 | Italy | March 18th to April 2nd, 2020 | no | Cross-sectional | General population | 2291 | 74.6 | above 18 | 9 | PSQI | GAD | |
| 158 | Marroquín- sample 2 [201] | 2020 | USA | March 2020 sample | no | Cross-sectional | General population | 435 | 46.4 | 39.2 | 9 | ISI | CESD GAD |
|
| 159 | Wang [202] | 2020 | China | Mar-20 | no | Cross-sectional | COVID-19 inpatients | 484 | 50.2 | 91.7 | 52.5 | 9 | ISI | PHQ GAD |
| 161 | Herrero San Martin [203] | 2020 | Spain | March 1st to April 30th 2020 |
no | Cross-sectional | Healthcare workers | 170 | 58.82 | 36.4 | 9 | PSQI | 0 | |
| 162 | Florin [204] | 2020 | France | April 10 to April 19,2020 | yes | Cross-sectional | Healthcare workers | 1515 | 44.3 | 82.8 | 45.2 | 9 | ISI | HADS |
| 163 | Zhang [205] | 2020 | China | March 2 to 8, 2020 | no | Cross-sectional | General population | 3237 | 47.1 | 62.7 | 18 to above 64 | 9 | ISI | PHQ GAD |
| 164 | Xia [206] | 2020 | China | April 20 to 30, 2020 | no | Case- control | Patients with Parkinson's disease | 288 | 51.85 | 60.50 | 9 | PSQI | HADS | |
| 165 | Zanghì [207] | 2020 | Italy | 4 May to 22 May 2020 |
no | Cross-sectional | Multiple sclerosis patients | 432 | 64.1 | 70.3 | 40.4 | 9 | ISI | 0 |
| 169 | Saracoglu [208] | 2020 | Turkey | 0 | no | Cross-sectional | Healthcare workers | 220 | 27.9 | 29 | 9 | PSQI | PHQ | |
| 174 | Alnofaiey [209] | 2020 | Saudi Arabia | May 2020 to August 2020 | no | Cross-sectional | Healthcare workers | 340 | 49.1 | 20-60 | 9 | PSQI | 0 | |
| 176 | Saraswathi- During COVID-19 data [210] | 2020 | India | 0 | no | Longitudinal study |
Medical students in a COVID-19 treating | 217 | 64 | 20 | 9 | PSQI | DASS-21 | |
| 179 | Badellino [211] | 2020 | Argentine | March 29 to April 12, 2020 | no | Cross-sectional | General population | 1985 | 75.9 | 36.83 | 9 | ISI | PHQ GAD |
|
| 181 | Bigalke [212] | 2020 | USA | April 25 and May 18, 2020 |
Yes | Cross-sectional | General population | 103 | 59 | 38 | 6 | PSQI | 0 | |
| 182 | Alshekaili [213] | 2020 | Oman | 8-17 April 2020 | no | Cross-sectional | Healthcare workers | 1139 | 80 | 86.9 | 36.3 | 9 | ISI | DASS-21 |
| 190 | Juanjuan [214] | 2020 | China | February 16-19, 2020 | no | Cross-sectional | Patients with breast cancer |
658 | 100 | 88.9 | 9 | ISI | PHQ GAD |
|
| 198 | Yu [215] | 2020 | China | 6 - 20 April 2020 |
yes | Cross-sectional | General population | 1138 | 65.6 | 49.1 | 9 | ISI | 0 | |
| 201 | Wang [216] | 2020 | China | February 4 to February 18, 2020 | no | Cross-sectional | General population | 6437 | 56.13 | 38.99 | 9 | PSQI | 0 | |
| 213 | Blekas [217] | 2020 | Greek | April 10 until April 13, 2020. | no | Cross-sectional | Healthcare workers | 270 | 73.7 | 18 to above 75 | 9 | AIS | PHQ | |
| 218 | Khanal [218] | 2020 | Nepal | April 26 and May 12, 2020 | no | Cross-sectional | Healthcare workers | 475 | 52.6 | 37.1 | 28.2 | 8 | ISI | HADS |
| 231 | Liang [219] | 2020 | China | 14 February to 29 March 2020 | no | Cross-sectional | General population + healthcare professionals | 2003 | 74.79 | 52.32 | 18 to above 60 | 8 | ISI | PHQ GAD |
| 232 | Wankowicz [220] | 2020 | Poland | 3 to 17 May 2020. | no | Cross-sectional | Healthcare workers | 441 | 52.15 | 40 | 9 | ISI | PHQ GAD |
|
| 240 | Pieh [221] | 2020 | Austria | 10th of April 2020 for 10 days | yes | Cross-sectional | General population | 733 | 49.9 | 55 | 18 to above 65 | 9 | ISI | PHQ GAD |
| 272 | Alessi [222] | 2020 | Brazil | 0 | no | Cross-sectional | Patients with type 1 and type 2 diabetes | 120 | 55.8 | 54.8 | 9 | Mini Sleep Questionnaire (MSQ), | 0 | |
| 274 | Huang [223] | 2020 | China | February 14 to March 29, 2020 | no | Cross-sectional | General population | 1172 | 69.28 | 39.51 | 18-40 | 9 | ISI | 0 |
| 275 | McCracken [224] | 2020 | Sweden | May 14 and June 11, 2020 | no | Cross-sectional | General population | 1212 | 73.8 | 55.9 | 18 to 88 | 8 | ISI | PHQ GAD |
| 277 | Parlapani [225] | 2020 | Greece | 0 | no | Cross-sectional | General population | 103 | 61.17 | 69.85 | 9 | AIS | PHQ GAD |
|
| 278 | Barrea [226] | 2020 | Italy | January 2020 to 30 April 2020 | yes | Cross-sectional | General population | 121 | 65.5 | 44.9 | 9 | PSQI | 0 | |
| 283 | Wańkowicz [227] | 2020 | Poland | 3-17 May 2020 | no | Cross-sectional | People with/ without Systemic Lupus Erythematosus | 723 | 67.75 | 39.05 | 9 | ISI | PHQ GAD |
|
| 292 | Dai [228] | 2020 | China | February 23-26, 2020 | no | Cross-sectional | COVID-19 patients | 307 | 43.32 | 81.76 | 9 | PSQI | SDS SAA |
|
| 239 | Lin [57] | 2020 | Iran | February 15-30 2020 | no | Cross-sectional | General population | 1078 | 58.3 | 26.24 | 9 | ISI | HADS | |
| 375 | Ahorsu [229] | 2020 | Iran | 1- 30 April 2020 | no | Cross-sectional | General population | 413 | 38 | 87.9 | 57.72 | 9 | ISI | PHQ |
3.3. Quality assessment
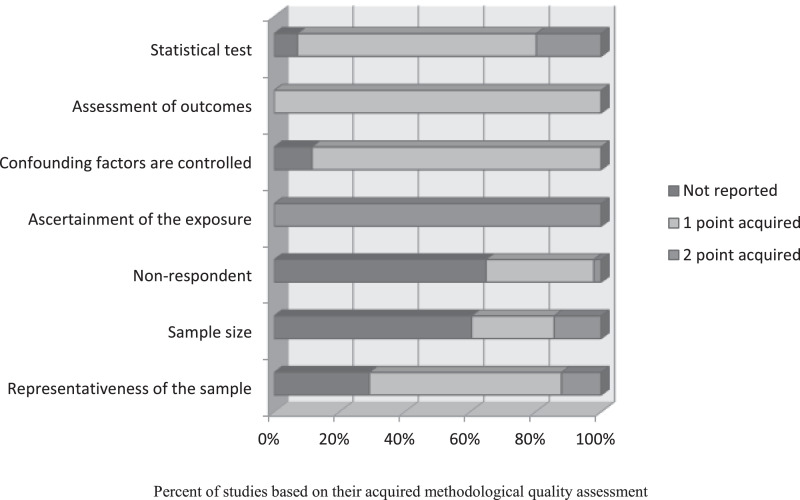
As aforementioned, the maximum score on the NOS is 9 and a score less than 5 is classified as having a high risk of bias [46]. Based on this criterion, 130 studies were categorized as being high quality studies. The impacts of study quality were further assessed and reported in subgroup analysis. The most common problems were in selection of participants. Online sampling leads to non-representativeness of the sample, sample size being not estimated or justified, and number of non-respondents being not reported. The results of the quality assessment are provided in Figure 2.
Figure 2.
Results of quality assessment
3.4. Outcome measures
Three target groups of participants were studied: healthcare professionals (n=62), general population (n= 105), and COVID-19 patients (n=10). Outcome measures are reported based on these target groups.
3.4.1. Sleep problems pooled prevalence based on participant target groups
3.4.1.1. Healthcare professionals
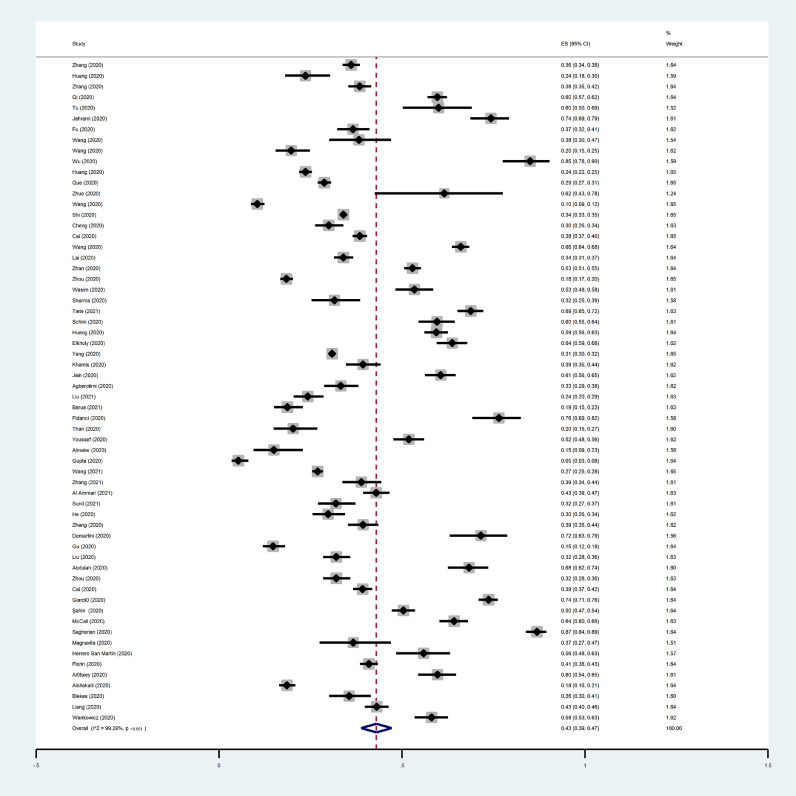
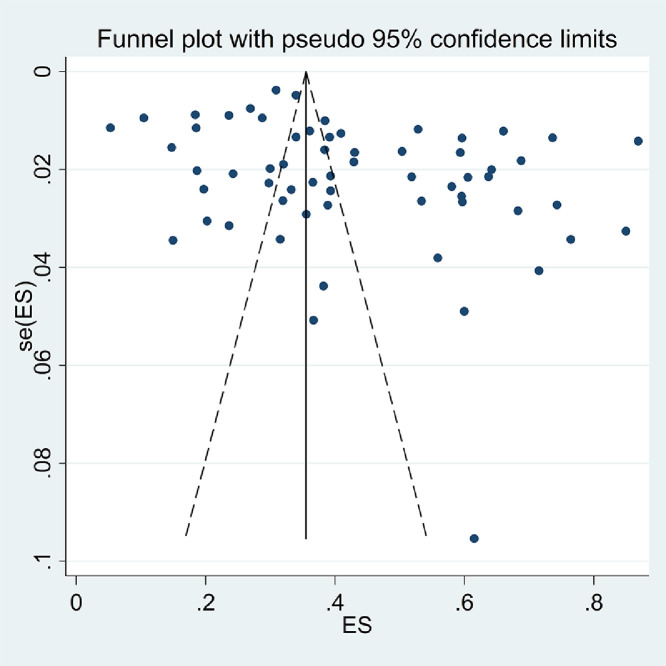
The pooled estimated prevalence of sleep problems among healthcare professionals was 43% [95% CI: 39-47%, I2:99.29%, Tau2:0.03]. Figure 3 provides the forest plot showing the pooled prevalence. Subgroup analysis (Table 2) and uni-variable meta-regression (Table 3), and multivariable meta-regression (Table 4) showed that none of the examined variables influenced the prevalence of sleep problems or heterogeneity. The probability of publication bias was assessed using Begg's test and funnel plot. Based on Begg's test (p=0.12) and funnel plot (Figure 4), the probability of publication bias was confirmed. Due to probability of publication bias in estimation of pooled prevalence of sleep problems in healthcare professions, the fill-and-trim method was used to correct the results. In this method, 20 studies were imputed and the corrected results based on this method showed that pooled prevalence of sleep problems among healthcare professions was 0.31 (95% CI: 0.27 to 0.36; p<.001). Funnel plot after trimming is provided in Figure 5. Also, sensitivity analysis showed that pooled effect size was not affected by a single study effect.
Figure 3.
Forest plot displaying the estimated pooled prevalence of sleep problems among health professionals
Table 2.
Results of subgroup analysis regarding estimated pooled prevalence
|
Healthcare professionals (N=62) |
General Population (N=105) |
Covid-19 patients (N=10) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | No. of studies | Pooled prevalence (95% CI) | I2 (%) | p for I2 | No. of studies | Pooled prevalence and 95% CI | I2 (%) | p for I2 | No. of studies | Pooled prevalence and 95% CI | I2 (%) | p for I2 | |
| Quality | Low quality | 17 | 41 (33-48) | 98.99 | 0.47 | 23 | 33 (27-39) | 99.61 | 0.10 | 3 | 42 (27-57) | 97.8 | 0.04 |
| High quality | 45 | 44 (39-49) | 99.37 | 82 | 38 (35-42) | 99.76 | 7 | 64 (49-71) | - | ||||
| Lockdown period | Yes | 3 | 45 (32-57) | - | 0.81 | 29 | 46 (37- 55) | 99.79 | 0.01 | - | - | - | - |
| No | 59 | 43 (39-47) | 99.32 | 76 | 34 (31-37) | 99.71 | 10 | 57 (42- 72) | 98.5 | ||||
| Gender group | Female only | 21 | 40 (34-47) | 99.33 | 0.34 | 32 | 34 (30-38) | 99.74 | 0.11 | 1 | 82 (78- 85) | - | <0.001 |
| Both gender | 41 | 44(39-50) | 99.28 | 73 | 39 (35- 43) | 99.75 | 9 | 54 (40 -69) | 98.10 | ||||
| Study design | Cross Sectional | 60 | 42 (38-47) | 99.3 | 0.96 | 99 | 36 (33-39) | 99.77 | <0.001 | 9 | 57 (41-73) | 98.67 | 0.80 |
| Case-control | 2 | 42 (41-44) | - | 2 | 50 (32-38) | - | - | - | - | ||||
| Longitudinal | - | - | - | 4 | 63 (52-74) | 86.86 | 1 | 55 (47-63) | - | ||||
| Measure of sleep | PSQI | 19 | 48 (38-58) | 99.29 | 0.24 | 38 | 45 (39-50) | 99.73 | <0.001 | 3 | 65 (42- 88) | - | <0.001 |
| ISI | 34 | 39 (34-45) | 99.37 | 53 | 31 (28-35) | 99.75 | 6 | 48 (38- 58) | 92.81 | ||||
| other | 9 | 46 (35-56) | 98.12 | 14 | 39 (29-49) | 99.68 | 1 | 82 (78-85) | - | ||||
| Overall estimated prevalence | 62 | 43 (39-47) | 99.29 | 105 | 37 (35-40) | 99.75 | 10 | 57 (42- 72) | 98.5 | ||||
95% CI=95% confidence interval. PSQI=Pittsburgh Sleep Quality Index. ISI=Insomnia Severity Index.
Table 3.
Results of Univariable meta-regression regarding estimated pooled prevalence
|
Healthcare professionals (N=62) |
General Population (N=105) |
Covid-19 patients (N=10) |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | No. of studies | Coeff. | S.E. | p | I2 res. (%) | Adj. R2 (%) | Tau2 | No. of studies | Coeff. | S.E. | p | I2 res. (%) | Adj. R2 (%) | Tau2 | No. of studies | Coeff. | S.E. | p | I2 res. (%) | Adj. R2 (%) | Tau2 |
| Country | 62 | 0.002 | 0.002 | 0.38 | 99.26 | -0.26 | 0.04 | 105 | 0.006 | 0.001 | <0.001 | 99.68 | 12.34 | 0.04 | 10 | -0.004 | 0.01 | 0.77 | 98.64 | -11.13 | 0.04 |
| Age | 34 | 0.005 | 0.007 | 0.46 | 99.2 | -1.5 | 0.04 | 69 | 0.002 | 0.002 | 0.48 | 99.8 | -0.7 | 0.04 | 8 | 0.0005 | 0.003 | 0.88 | 98.66 | -12.57 | 0.04 |
| Female % of participants | 62 | 0.001 | 0.001 | 0.72 | 99.29 | -1.45 | 0.04 | 103 | -0.0001 | 0.001 | 0.95 | 99.73 | -0.9 | 0.04 | 10 | -0.002 | 0.006 | 0.71 | 98.65 | -10.51 | 0.04 |
| Married % of participants | 39 | 0.001 | 0.002 | 0.51 | 99.30 | -1.54 | 0.04 | 52 | 0.001 | 0.001 | 0.37 | 99.74 | -0.4 | 0.04 | 8 | -0.002 | 0.007 | 0.80 | 98.46 | -16.04 | 0.04 |
Coeff.=coefficient. S.E.=standard error. I2 res.=I2 residual. Adj. R2=adjusted R2.
Table 4.
Results of multivariable meta-regression regarding estimated pooled prevalence
|
Healthcare professionals |
General Population |
|||||
|---|---|---|---|---|---|---|
| Variable | Coefficient | S.E. | p | Coefficient | S.E. | p |
| Country | -0.003 | 0.007 | 0.64 | 0.006 | 0.001 | <0.001 |
| Design | 0.06 | 0.24 | 0.81 | ⁎⁎ | ||
| Lockdown period (yes vs. no) | 0.23 | 0.17 | 0.21 | 0.08 | 0.04 | 0.03 |
| Study quality (low vs. high quality) | 0.12 | 0.13 | 0.40 | 0.04 | 0.04 | 0.39 |
| Age | -0.003 | 0.01 | 0.78 | 0.001 | 0.001 | 0.26 |
| % Female of participants | 0.03 | 0.003 | 0.39 | 0.001 | 0.001 | 0.30 |
| % Married of participants | 0.003 | 0.004 | 0.35 | -0.001 | 0.001 | 0.11 |
| Measure of sleep | -0.06 | 0.09 | 0.50 | -0.03 | 0.032 | 0.20 |
| Between-study variance (tau2) | 0.03 | 0.03 | ||||
| % Residual variation due to heterogeneity (I2 residual) | 99.27 | 99.68 | ||||
| Proportion of between-study variance explained (adjusted R2) | -26.23 | 26.33 | ||||
N.B. Due to insufficient observations, meta-regression was not conducted for COVID-19 patients subgroup.
Due to collinearity design was omitted.
Figure 4.
Funnel plot assessing publication bias in studies regarding prevalence of sleep problems among health professionals
Figure 5.
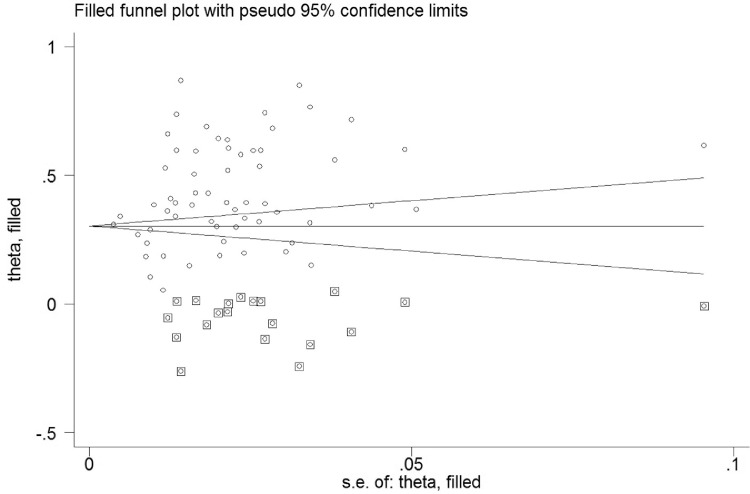
Corrected funnel plot assessing publication bias in studies regarding prevalence of sleep problems among health professionals
3.4.1.2. General population
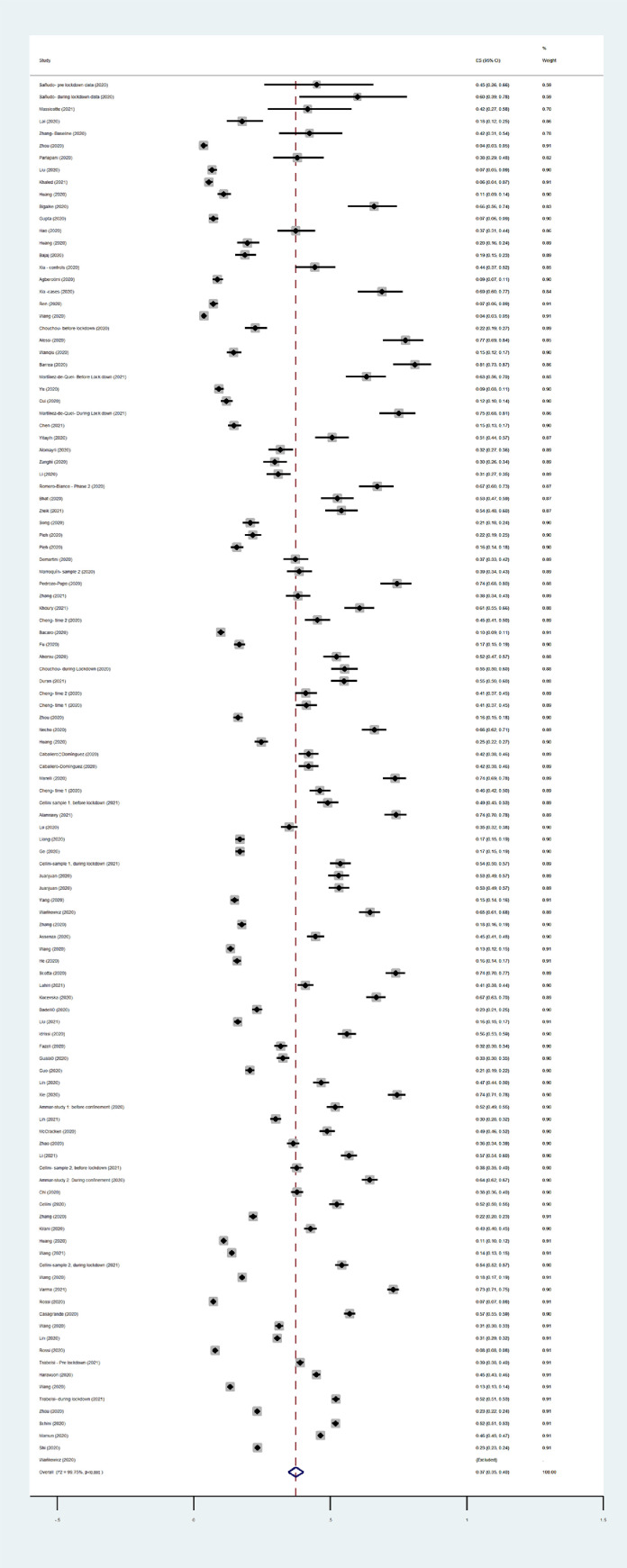
The pooled estimated prevalence of sleep problems among the general population was 37% [95% CI: 35-40%, I2:99.77%, Tau2:0.02]. Figure 6 provides the forest plot showing the pooled prevalence. Subgroup analysis (Table 2) showed that during lockdown, participants in longitudinal studies showed a significantly higher prevalence of sleep problems. Based on uni-variable meta-regression (Table 3), the country of residence was the other significant variable in prediction of prevalence of sleep problems among the general population. Also, multivariable meta-regression (Table 4) confirmed that country and lockdown period were significant influential factors on prevalence of sleep problems, explaining 26.32% of variance.
Figure 6.
Forest plot displaying the estimated pooled prevalence of sleep problems among general population
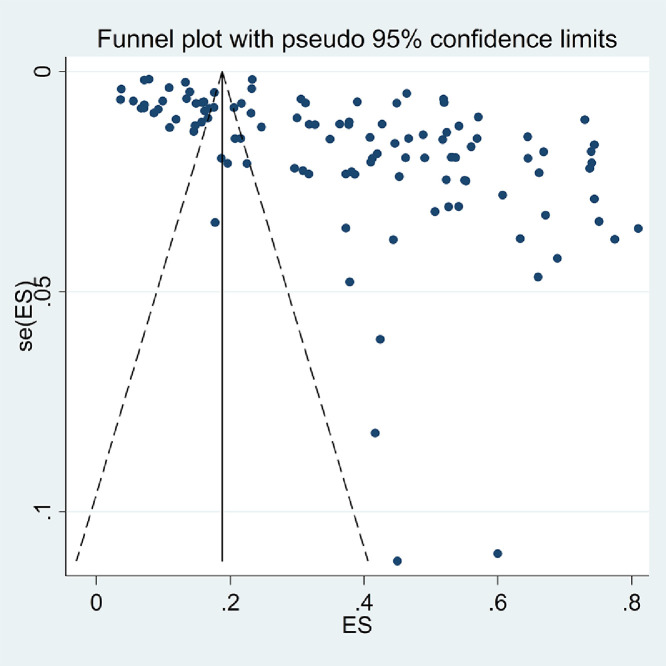
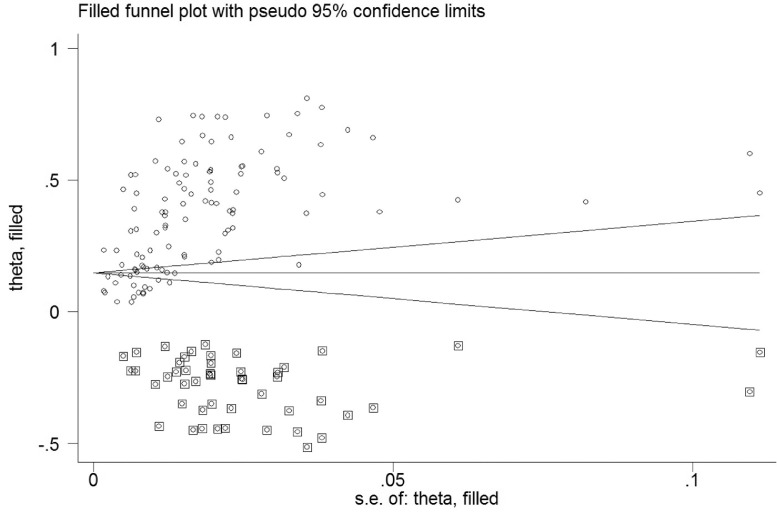
The probability of publication bias was assessed using Begg's test and funnel plot. Based on Begg's test (p=0.01) and funnel plot (Figure 7), the probability of publication bias was confirmed. Due to probability of publication bias in estimation of pooled prevalence of sleep problems among the general population, the fill-and-trim method was used to correct the results. In this method, 50 studies were imputed and the corrected results based on this method showed that pooled prevalence of sleep problems was 18% (95% CI: 15-21%; p<.001). Funnel plot after trimming is provided in Figure 8. Also, sensitivity analysis showed that pooled effect size was not affected by a single study effect.
Figure 7.
Funnel plot assessing publication bias in studies regarding prevalence of sleep problems among general population
Figure 8.
Corrected funnel plot assessing publication bias in studies regarding prevalence of sleep problems among general population
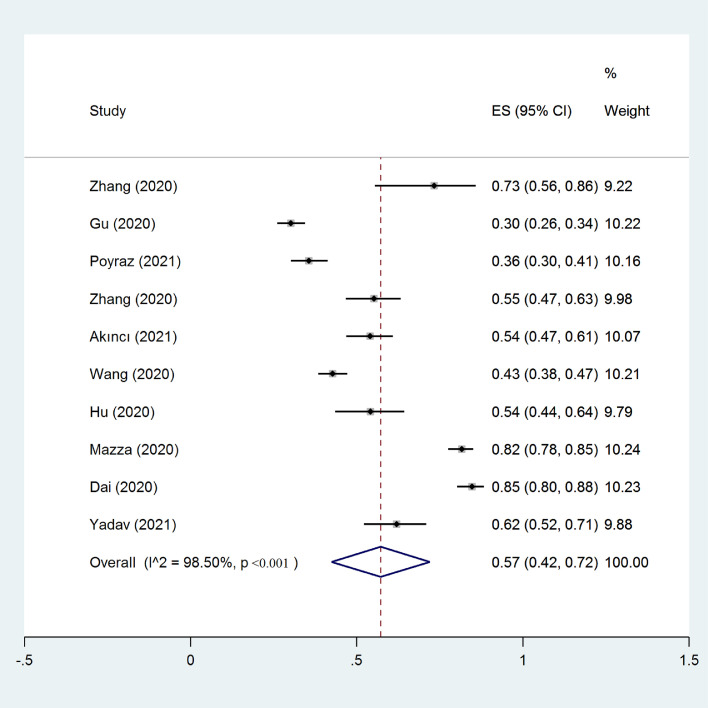
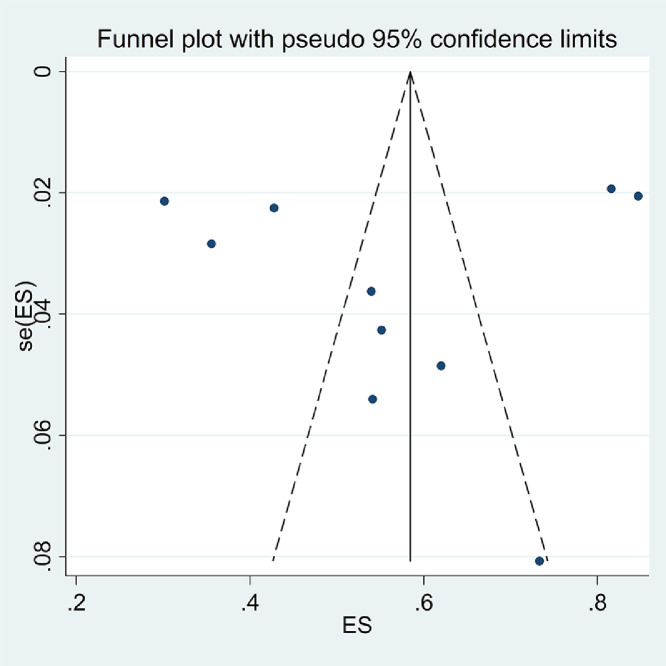
3.4.1.3. COVID-19 patients
The pooled estimated prevalence of sleep problems was 57% among COVID-19 patients [95% CI: 42 to 72%, I2:98.5%, Tau2:0.06]. Figure 9 provides the forest plot showing the pooled prevalence. Subgroup analysis (Table 2) showed studies with female-only participants had a higher prevalence of sleep problems significantly (82% vs. 54% respectively). Other variables did not influence heterogeneity or estimated pooled prevalence in this participants group. The probability of publication bias was assessed using Begg's test and funnel plot. Based on Begg's test (p=0.53) and funnel plot (Figure 10), the probability of publication bias was rejected. Also, sensitivity analysis showed that pooled effect size was not affected by a single study effect.
Figure 9.
Forest plot displaying the estimated pooled prevalence of sleep problems among COVID-19 patients
Figure 10.
Funnel plot assessing publication bias in studies regarding prevalence of sleep problems among Covid patients
Overall, the prevalence of sleep problems was significantly different in target participants considering 95% confidence interval of sleep prevalence. The corrected pooled estimated prevalence of sleep problems was 31% (95% CI: 27-36%), 18% (95% CI: 15-21%) and 57% (95% CI: 42-72%), among healthcare professional, general population and COVID-19 patients respectively. The highest prevalence of sleep problems was seen among COVID-19 patients.
3.4.2. Association of sleep problems with psychological distress
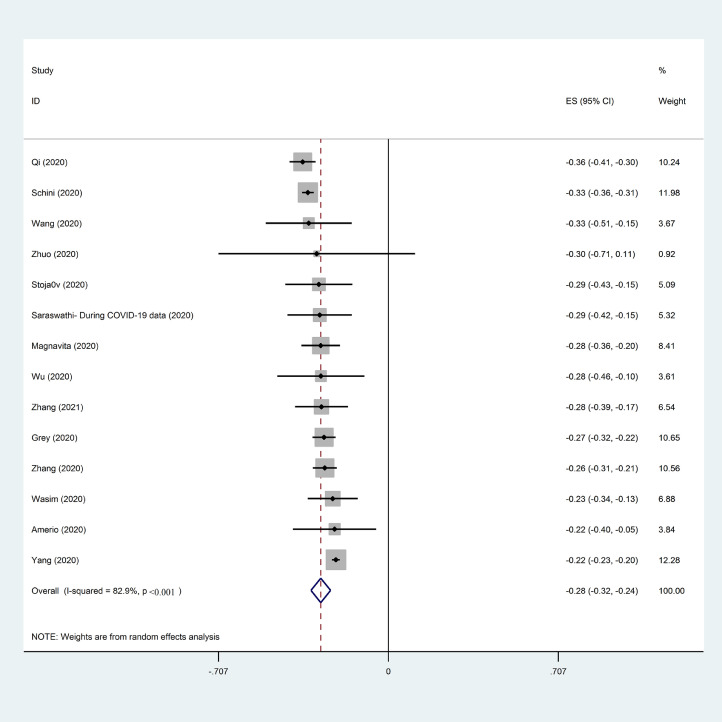
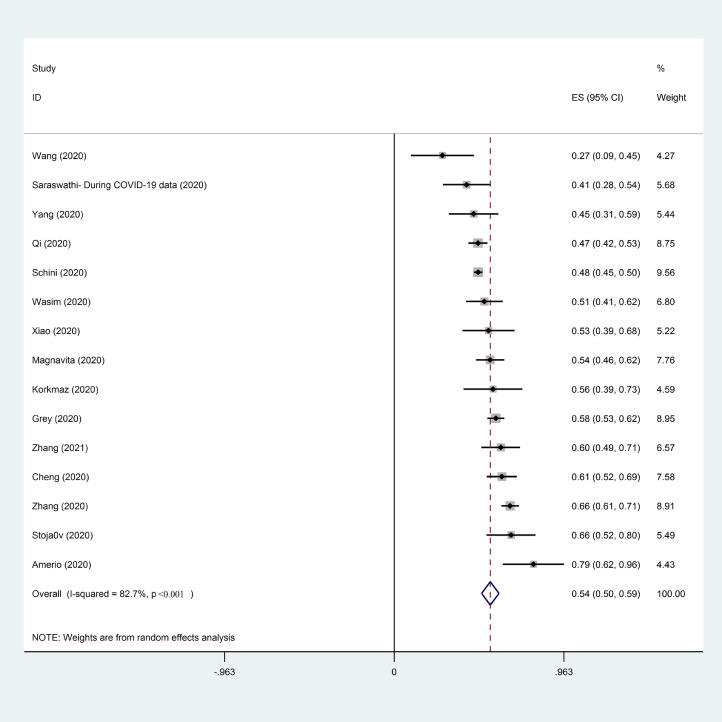
3.4.2.1. Healthcare professionals
The association of sleep problems with depression and anxiety among health professionals were reported in 14 and 15 studies respectively. The pooled estimated effect size showed poor correlation between sleep problems and depression with Fisher's z score of -0.28 [95% CI: -0.32 to -0.24, p<0.001, I2=82.9%; Tau2 = 0.004]. However, a moderate correlation was found between sleep problems and anxiety with Fisher's z score of 0.55 [95% CI: 0.49 to 0.59, p<0.001, I2=82.7%; Tau2 = 0.10]. The forest plots are shown in Figure 11, Figure 12.
Figure 11.
Forest plot displaying the estimated pooled Fishers’ Z score in association of sleep problems and depression among health professionals
Figure 12.
Forest plot displaying the estimated pooled fishers’ Z score in association of sleep problems and anxiety among health professionals
Based on subgroup analysis (Table 5), quality of studies (low vs. high), gender group of participants (female vs. both gender), and measure of sleep problems (PSQI vs. others) influenced heterogeneity of association of sleep problems and depression among health professionals. Meta-regression (Table 7) showed that age and marital status (married vs. others) significantly decreased the heterogeneity and explained substantial proportion of variance (72.8% and 43.85% respectively). Examined variables in subgroup analysis and meta-regression were not identified as possible source of heterogeneity or influential in the estimated pooled effect size in the association of sleep problems and anxiety (Table 6). Publication bias and small study effect was not found in association of sleep problems and depression/anxiety based on Begg's test (p=0.87 and p=0.81 respectively).
Table 5.
Results of subgroup analysis regarding estimated pooled correlation between sleep and Depression
|
Healthcare professionals (N=14) |
General Population(N=15) |
||||||
|---|---|---|---|---|---|---|---|
| Variable | No. of studies | ES (95% CI) | I2 (%) | No. of studies | ES (95% CI) | I2 (%) | |
| Quality | Low quality | 6 | -0.30 (-0.35; -0.25) | 28 | 4 | -0.32 (-0.37; -0.26) | 71.2 |
| High quality | 8 | -0.28 (-0.33; -0.22) | 88.9 | 11 | -0.29 (-0.32; -.27) | 76.2 | |
| Gender group | Female only | 6 | -0.30(-0.34; -0.26) | 23.8 | 4 | -0.32 (-0.39; -0.25) | 79.7 |
| Both gender | 8 | -0.27 (-0.32; -0.21) | 88.7 | 11 | -0.29 (-0.32; -0.27) | 74.7 | |
| Lockdown | Yes | 1 | -0.34 (-0.36; -0.31) | - | 4 | -0.33 (-0.38; -0.28) | 78.6 |
| No | 13 | -0.27 (-0.31; -0.24) | 60.8 | 11 | -0.29 (-0.31; -0.26) | 58.9 | |
| Study design | Cross-sectional | 12 | -0.28 (-0.32; -0.24) | 85.5 | 14 | -0.30 (-0.32; -0.27) | 75.5 |
| Case-control | 1 | -0.28 (-0.46; -0.1) | - | - | - | - | |
| Longitudinal | 1 | -0.29 (-0.42; -0.15) | - | 1 | -0.38 (-0.51; -0.24) | - | |
| Measure of sleep | PSQI | 7 | -0.30 (-0.34; -0.27) | 4.6 | 7 | -0.30 (-0.33; -0.27) | 64.6 |
| ISI | 5 | -0.22 (-0.24; -0.21) | - | 7 | -0.29 (-0.33; -0.25) | 72.9 | |
| other | 2 | -0.32 (-0.37; -0.28) | 35 | 1 | -0.34 (-0.36; -0.31) | - | |
| Overall estimated prevalence | 14 | -0.28 (-0.32; -0.24) | 82.9 | 15 | -0.30 (-0.32; -0.28) | 74.4 | |
Table 7.
Results of meta-regression regarding correlation between sleep and psychological distress
| Depression | Healthcare professionals (N=14) |
General Population(N=15) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | No of studies | Coeff. | S.E. | p | I2 res. (%) | Adj. R2 (%) | Tau2 | No of studies | Coeff. | S.E. | p | I2 res. (%) | Adj. R2 (%) | Tau2 |
| Country | 14 | 0.002 | 0.003 | 0.62 | 83.99 | -8.4 | 0.002 | 15 | -0.0004 | 0.001 | 0.64 | 75.9 | -7.49 | 0.002 |
| Age | 12 | -0.002 | 0.001 | 0.006 | 13.91 | 72.8 | 0.0004 | 13 | 0.002 | 0.001 | 0.21 | 77.65 | 1.88 | 0.002 |
| Female % of participants | 14 | -0.002 | 0.001 | 0.12 | 71.23 | 19.31 | 0.001 | 15 | -0.001 | 0.001 | 0.38 | 68.46 | 3.93 | 0.002 |
| Married % of participants | 12 | -0.001 | 0.0004 | 0.08 | 37.2 | 43.85 | 0.001 | 6 | -0.001 | 0.0004 | 0.52 | 72.16 | -3.47 | 0.002 |
| Anxiety |
Healthcare professionals (N=15) |
General Population (N=12) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Coeff. | S.E. | p | I2 res. (%) | Adj. R2 (%) | Tau2 | No of studies | Coeff. | S.E. | p | I2 res. (%) | Adj. R2 (%) | Tau2 | |
| Country | 15 | -0.002 | 0.005 | 0.73 | 83.61 | - 13.03 | 0.01 | 12 | -0.0005 | 0.003 | 0.89 | 95.62 | -10.62 | 0.02 |
| Age | 10 | 0.011 | 0.005 | 0.05 | 62.52 | 54.77 | 0.01 | 10 | 0.01 | 0.005 | 0.02 | 95.03 | 50.37 | 0.02 |
| Female % of participants | 15 | -0.002 | 0.002 | 0.38 | 83.37 | - 12.64 | 0.01 | 11 | 0.001 | 0.003 | 0.70 | 95.68 | -9.10 | 0.03 |
| Married % of participants | 9 | 0.006 | 0.003 | 0.46 | 87.86 | 21.25 | 0.01 | 5 | 0.0004 | 0.005 | 0.95 | 97.31 | -31.77 | 0.02 |
Table 6.
Results of subgroup analysis regarding estimated pooled correlation between sleep and Anxiety
|
Healthcare professionals (N=15) |
General Population(N=12) |
||||||
|---|---|---|---|---|---|---|---|
| Variable | No. of studies | ES (95% CI) | I2 (%) | No. of studies | ES (95% CI) | I2 (%) | |
| Quality | Low quality | 7 | 0.59 (0.49; 0.68) | 82.5 | 3 | 0.55 (0.48; 0.62) | 73.5 |
| High quality | 8 | 0.52 (0.46; 0.58) | 78.1 | 9 | 0.53 (0.46; 0.61) | 96.2 | |
| Lockdown period | Yes | 1 | 0.48 (0.45; 0.50) | - | 3 | 0.45 (0.32; 0.58) | 78.4 |
| No | 14 | 0.55 (0.50; 0.60) | 75.6 | 9 | 0.57 (0.49; 0.65) | 96.3 | |
| Gender group | Female only | 7 | 0.55 (0.47; 0.63) | 83.9 | 3 | 0.49 (0.31; 0.66) | 90.9 |
| Both gender | 8 | 0.54 (0.48; 0.60) | 76.8 | 9 | 0.56 (0.47; 0.64) | 95.8 | |
| Study design | Cross-sectional | 14 | 0.55 (0.50; 0.60) | 83.3 | 11 | 0.56 (0.49; 0.62) | 95.4 |
| Case-control | - | - | - | - | - | - | |
| Longitudinal | 1 | 0.41 (0.28; 0.55) | - | 1 | 0.28 (0.15; 0.42) | - | |
| Measure of sleep | PSQI | 10 | 0.53 (0.47; 0.58) | 68.1 | 6 | 0.51 (0.47; 0.57) | 88.7 |
| ISI | 2 | 0.64 (0.51; 0.77) | 60.1 | 5 | 0.60 (0.40; 0.80) | 97.7 | |
| Other | 3 | 0.50 (0.44; 0.56) | 78.1 | 1 | 0.48 (0.45; 0.50) | - | |
| Overall estimated prevalence | 15 | 0.55 (0.49 to 0.59) | 82.7 | 12 | 0.54 (0.48; 0.60) | 95.2 | |
3.4.2.2. General population
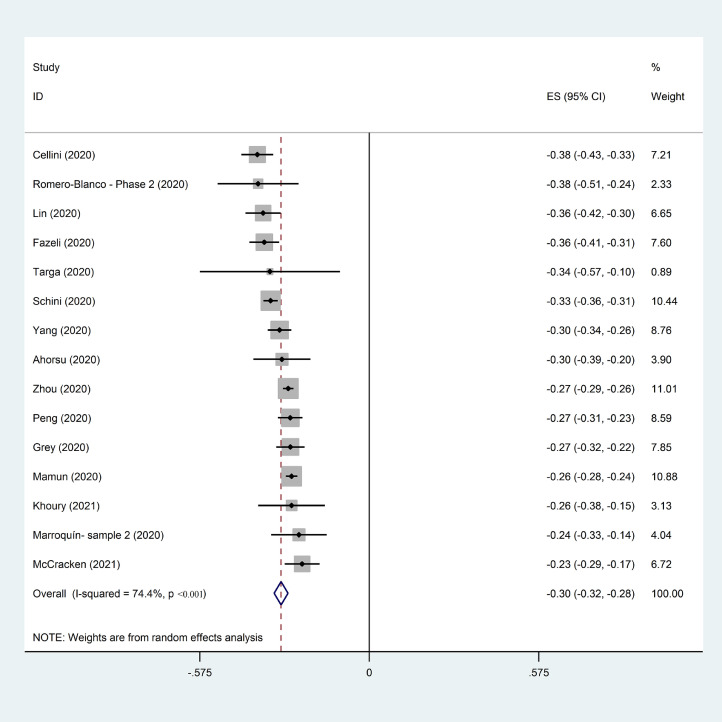
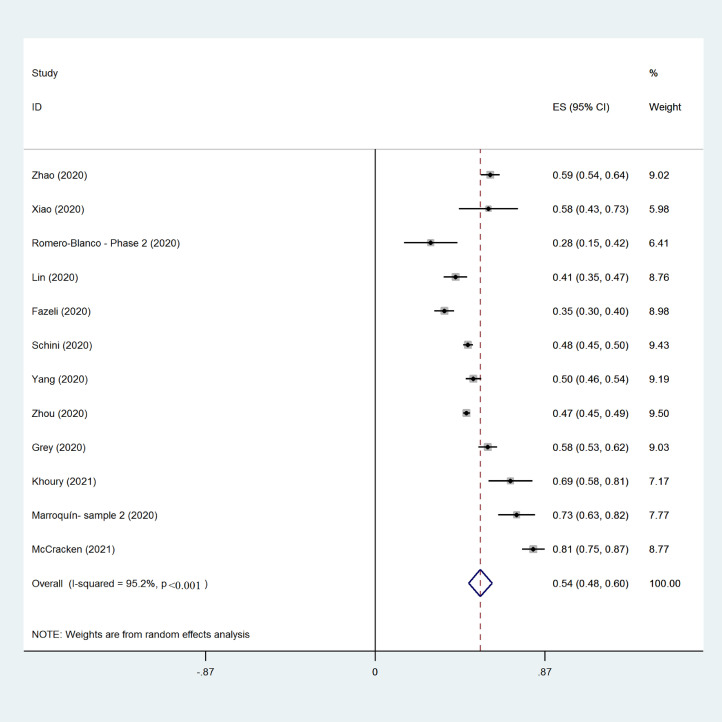
The association of sleep problems with depression and anxiety among the general population were reported in 15 and 12 studies respectively. The pooled estimated effect size showed moderate correlation between sleep problems and depression with Fisher's z score of -0.30 [95% CI: -0.32 to -0.28, p<0.001, I2=74.4%; Tau2 = 0.001]. Also, a moderate correlation was found between sleep problems and anxiety with Fisher's z score of 0.54 [95% CI: 0.48 to 0.60, p<0.001, I2=95.2%; Tau2 = 0.01]. The forest plots are shown in Figure 13, Figure 14. Based on subgroup analysis (Table 5 and 6), lockdown status (no vs. yes) reduced the heterogeneity in association of sleep problems and depression. Based on meta-regression (Table 7), age was a significant moderator in association between sleep problems and anxiety, which explained 50.37% of variance. However, the other examined variables were not identified as possible sources of heterogeneity or influential on the estimated pooled effect size in the association between sleep problems and depression/anxiety.
Figure 13.
Forest plot displaying the estimated pooled Fishers’ Z score in association of sleep problems and depression among general population
Figure 14.
Forest plot displaying the estimated pooled Fishers’ Z score in association of sleep problems and anxiety among general population
Based on Begg's test, publication bias and small study effect were not found in the association between sleep problems and depression (p=0.52). Although publication bias was not significant in association between sleep problems and anxiety (p=0.41), based on funnel plot, publication bias was probable. Consequently, fill and trim method was used to correct probable publication bias. After imputation of three studies, the association between sleep problems and anxiety was estimated as Fisher's z score of 0.48 (95% CI: 0.41 to 0.54).
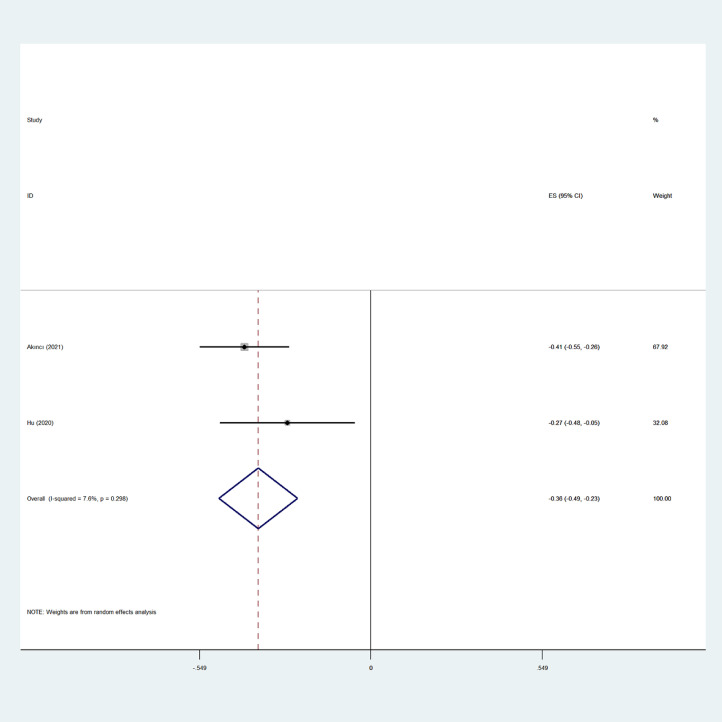
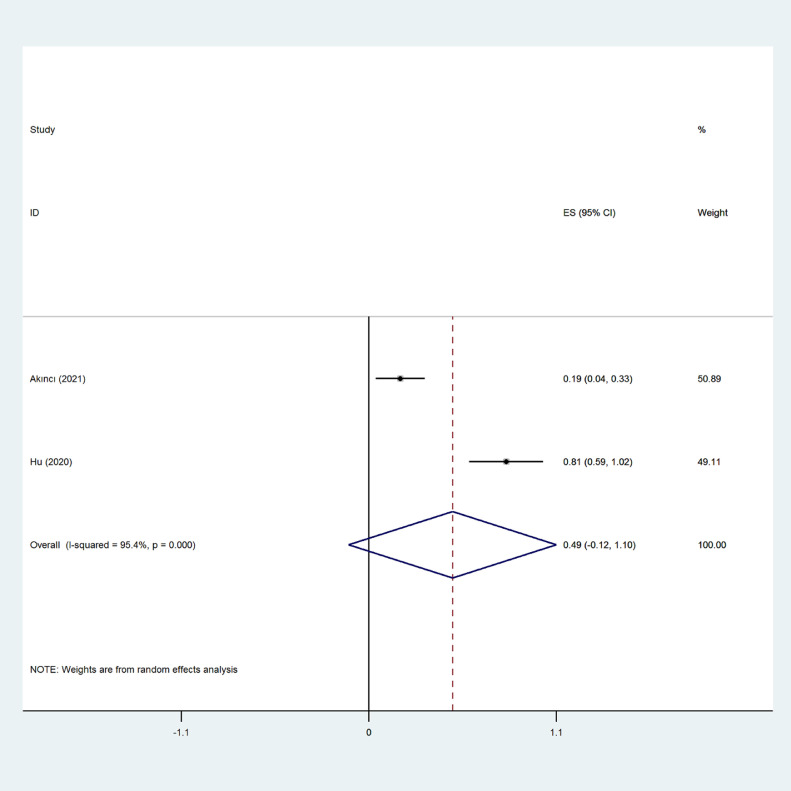
3.4.3. COVID-19 patients
The association of sleep problems with depression and anxiety among general population was reported in only two studies. The pooled estimated effect size showed moderate correlation between sleep problems and depression with Fisher's z score of -0.36 [95% CI: -0.49 to -0.24, p=0.0007, I2=7.4%; Tau2 = 0.001]. Also, a moderate correlation was found between sleep problems and anxiety with Fisher's z score 0.49 [95% CI: -0.12 to 1.1, p<0.001, I2=95.2%; Tau2 = 0.01]. The forest plots are shown in Figure 15, Figure 16. The number of studies was too few to conduct further secondary analysis including subgroup/meta-regression analysis, controlling publication bias, and small study effect.
Figure 15.
Forest plot displaying the estimated pooled Fishers’ Z score in association of sleep problems and depression among COVID-19 patients
Figure 16.
Forest plot displaying the estimated pooled fishers’ Z score in association of sleep problems and anxiety among Covid patients
4. Discussion
The present systematic review and meta-analysis synthesized data from 177 recently published studies on this topic to more rigorously investigate the prevalence of sleep problems and how sleep associated with psychological distress. The synthesized results showed that the pooled estimated prevalence of sleep problems regardless of gender and population was 37% during the COVID-19 outbreak. Additionally, a much higher prevalence rate of sleep problems was identified among patients with COVID-19 infection (55%) and healthcare professionals (43%). These findings concur with Jahrami et al. [38] who reported in their meta-analysis that the highest prevalence rate of sleep problems was found among COVID-19 patients. Meta-regression in the present review further indicated that country, age, gender, and marital status did not contribute to the estimated prevalence in sleep problems.
The nonsignificant finding for gender contradicts prior evidence showing that being female is a risk factor for insomnia and mental health problems [27, 56]. This may be explained by the samples recruited because the analyzed studies in the present review comprised a large proportion of females. The imbalanced gender distribution may have led to a reduced gender effect, which in turn, resulted in a nonsignificant finding. Regarding the association between sleep problems and psychological distress, sleep problems were found to be moderately correlated with depression (ES=0.54) and anxiety (ES=0.55). Subgroup analysis and meta-regression additionally showed that being a COVID-19 patient and being of older age were significant predictors of a higher association between sleep problems and psychological distress.
The high prevalence of sleep problems found in the present review can be explained by fear of COVID-19 and sleep-related factors (e.g., the changes in sleep-wake habits with delayed bedtime, lights off time, and sleep onset time due to quarantine and lockdown) [57]. The national and global COVID-19 death statistics are commonly and routinely reported by the social media and news [57]. Therefore, prior research has found the higher levels of psychological distress and significant symptoms of mental illness in various populations since the start of the pandemic [4], [5], [6]. Indeed, evidence prior to the pandemic has demonstrated that individuals may experience sleep problems when they experience major public health threats [16], [17], [18]. The higher prevalence of sleep problems found among healthcare professionals can be further explained by their job nature. Health professionals, especially those who are frontline workers dealing with COVID-19 infected patients on a daily basis, encounter much higher high risk of infection and irregular work schedules than those working in other occupations [10], [11], [12], [13], [14], [15].
Lockdown was found to be a significant factor in explaining sleep problems. However, this finding may be confounded by the different policies implemented to inhibit the spread of COVID-19 across the 39 countries analyzed in the present review. For example, mainland China launched a strict lockdown policy to prohibit almost all outdoor activities, while the lockdown policy in other countries was not as strict. Nevertheless, the present findings support prior evidence that lockdown negatively impacted individuals’ psychological health and sleep [57].
There are several clinical implications from the present study's findings. First, government and healthcare providers worldwide need to design and implement appropriate programs and treatments to assist different populations, including healthcare professionals, patients, and the general population, in overcoming sleep problems. For example, effective programs (e.g., cognitive behavioral therapy for insomnia and meditation) [58] reported in prior research can be embedded in smartphone apps and healthcare professional training to prevent or deal with the sleep problems for different populations. Second, the associations between sleep problems and psychological distress provide the empirical evidence that healthcare providers should simultaneously tackle sleep problems and psychological distress. Consequently, psychological distress can be reduced when an individual's sleep is improved (and vice versa). Third, special attention may need to be paid to COVID-19 patients and older individuals because the present review showed a higher association between their sleep problems and psychological distress. Moreover, specific populations such as children and their caregivers should not be ignored regarding their psychological needs and sleep issues. Although the present review did not provide evidence on pediatric populations, the present findings concerning the specific group of older individuals may generalize to other specific populations. It is recommended that programs comprising psychological support for family having children to overcome the difficulties during COVID-19 pandemic are implemented [60].
The present review has some strengths. First, the prevalence of sleep problems has been estimated across different populations and this information provides healthcare providers with a greater and more contextualized picture regarding the impacts of COVID-19 on sleep problems. Second, methodological quality of each analyzed study was assessed using the NOS checklist. Within the meta-analysis findings, subgroup analysis and meta-regression were used to provide thorough information and therefore the meta-analysis findings are robust. Third, generalizability of the present review's findings is good because the synthesized sample size was large (N=345,270) and the participants were recruited from 39 countries.
The present review has some limitations. First, most of the studies adopted a cross-sectional design (n=56) and only seven studies (three which used a case-control design and four which used a longitudinal design) considered the time effect in the causal relationship. Therefore, the relationships between sleep problems and psychological distress found in the present review do not have strong causality evidence. Diverse evidence in the causality has been proposed. Using longitudinal designs, Vaghela and Sutin [59] found that psychological distress might lead to poor sleep, while Mazzer and Linton [60] found that shorter sleep duration might lead to higher levels of psychological distress. Moreover, the lack of pre-COVID-19 pandemic information on sleep problems hinders the understanding of changes of sleep problems caused by COVID-19. Second, different measures were used in the studies that were evaluated (e.g., PSQI, ISI, and ASI for sleep problems). Given that different measures may have different features in capturing the severity of sleep problems, there may have some biases in estimating prevalence for sleep problems and effect sizes for the associations between sleep problem and psychological distress. All the studies evaluated here used self-report methods in assessing sleep problems and psychological distress. Therefore, findings in the present review cannot rule out social desirability and memory recall biases. Third, the impacts of COVID-19 on sleep and mental health problems are dynamic. That is, individuals may have different levels of sleep and mental health problems according to the severity of COVID-19 outbreak in their localities or countries. Moreover, the policies in controlling the COVID-19 outbreak are different across countries [57,[61], [62], [63], [64], [65], [66]]. Therefore, the estimated findings in the present review cannot represent the impacts of COVID-19 during a specific period. Fourth, the analyzed studies in the present review had a large proportion of Chinese and Italian populations. Similarly, the synthesized samples were mostly young adults. Therefore, the generalizability of the present review's findings to different ethnic populations and age groups (i.e., older people and children) is restricted. Given that China and Italy were the first two countries to be severely impacted by the COVID-19 pandemic, there is understandably more research carried out in these two countries. However, the contributions of other countries, especially the American and African populations, should not be ignored. Further research should be carried out in other ethnic populations and different countries to balance the findings and maximize the generalizability. Fifth, the present meta-analysis had very large heterogeneity (as shown in Fig. 3) and evidence of publication bias (as shown in Fig. 4). Therefore, the findings without removing the heterogeneity in the meta-regression and subgroup analysis might be biased. Finally, most of the studies included in the meta-analysis were not of high quality (as shown in Fig. 2). Therefore, future studies require higher quality designs to investigate sleep problems during COVID-19 pandemic.
In conclusion, sleep problems appear to have been common during the COVID-19 pandemic. One in every three individuals reported the sleep problems. Nearly half of the healthcare professionals (43%) encountered sleep problems during the pandemic period. Healthcare providers may want to design appropriate programs to help individuals overcome their sleep problems. Moreover, sleep problems were found to be associated with higher levels of psychological distress (including depression and anxiety). Therefore, with the use of effective programs treating sleep problems, psychological distress may be reduced. Vice versa, the use of effective programs treating psychological distress, sleep problems may be reduced. However, it is possible that the association between sleep problems and psychological distress found in the present review is contributed by confounders. In other words, causality may not be happened between sleep problems and psychological distress. Therefore, more longitudinal studies and randomized controlled trials are needed to investigate the causality between sleep problems and psychological distress.
Declaration of Competing Interest
Chung-Ying Lin was supported in part by a research grant from the Ministry of Science and Technology, Taiwan (MOST109-2327-B-006-005). All other authors have nothing to declare.
Acknowledgments
Data sharing statement
No additional unpublished data are available.
Funding
No funding was received.
Authors’ contributions
Conceptualisation: Amir H Pakpour, Zainab Alimoradi and Chung-Ying Lin; writing original draft: Amir H Pakpour, Zainab Alimoradi and Chung-Ying Lin; writing (review and edit): all authors; literature search: Amir H Pakpour, Zainab Alimoradi; data sourcing and collection: Amir H Pakpour, Zainab Alimoradi; Project administration: Amir H Pakpour; Statistical analysis: Zainab Alimoradi and Amir H Pakpour; access to data: Zainab Alimoradi and Amir H Pakpour; figures: Zainab Alimoradi; data interpretation: all authors.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.100916.
Contributor Information
Chung-Ying Lin, Email: cylin36933@gmail.com.
Amir H. Pakpour, Email: Pakpour_Amir@yahoo.com.
Appendix. Supplementary materials
References
- 1.Nowbar A.N., Gitto M., Howard J.P., Francis D.P., Al-Lamee R. Mortality from ischemic heart disease: Analysis of data from the World Health Organization and coronary artery disease risk factors From NCD Risk Factor Collaboration. Circulation: Cardiovascular Quality and Outcomes. 2019;12 doi: 10.1161/CIRCOUTCOMES.118.005375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . World Health Organization; Switzerland: 2020. Coronavirus disease 2019 (COVID-19): situation report, 72. [Google Scholar]
- 3.WHO . World Health Organization; Geneva, Switzerland: 2020. WHO Coronavirus Disease (COVID-19) Dashboard. [Google Scholar]
- 4.Stewart-Ibarra A.M., Hargrave A., Diaz A. Psychological distress and Zika, Dengue and Chikungunya symptoms following the 2016 earthquake in Bahía de Caráquez, Ecuador. International journal of environmental research and public health. 2017;14:1516. doi: 10.3390/ijerph14121516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tucci V., Moukaddam N., Meadows J., Shah S., Galwankar S.C., Kapur G.B. The forgotten plague: psychiatric manifestations of ebola, zika, and emerging infectious diseases. Journal of Global Infectious Diseases. 2017;9:151. doi: 10.4103/jgid.jgid_66_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International journal of environmental research and public health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin C.-Y., Hou W.-L., Mamun M.A. Fear of COVID-19 Scale (FCV-19S) across countries: Measurement invariance issues. Nursing open. 2021 doi: 10.1002/nop2.855. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu X., Kakade M., Fuller C.J. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry. 2012;53:15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caruso C.C. Negative impacts of shiftwork and long work hours. Rehabilitation Nursing. 2014;39:16–25. doi: 10.1002/rnj.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferri P., Guadi M., Marcheselli L., Balduzzi S., Magnani D., Di Lorenzo R. The impact of shift work on the psychological and physical health of nurses in a general hospital: a comparison between rotating night shifts and day shifts. Risk Management and Healthcare Policy. 2016;9:203. doi: 10.2147/RMHP.S115326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koinis A., Giannou V., Drantaki V., Angelaina S., Stratou E., Saridi M. The impact of healthcare workers job environment on their mental-emotional health. Coping strategies: the case of a local general hospital. Health Psychology Research. 2015;3 doi: 10.4081/hpr.2015.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar A., Bhat P.S., Ryali S. Study of quality of life among health workers and psychosocial factors influencing it. Industrial Psychiatry Journal. 2018;27:96. doi: 10.4103/ipj.ipj_41_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohanty A., Kabi A., Mohanty A.P. Health problems in healthcare workers: A review. Journal of Family Medicine and Primary Care. 2019;8:2568. doi: 10.4103/jfmpc.jfmpc_431_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jahrami H., Dewald-Kaufmann J., AlAnsari A.M., Taha M., AlAnsari N. Prevalence of sleep problems among medical students: a systematic review and meta-analysis. Journal of Public Health. 2019:1–18. [Google Scholar]
- 16.Cates D.S., Gomes P.G., Krasilovsky A.M. Bioemergency Planning. Springer; 2018. Behavioral health support for patients, families, and healthcare workers; pp. 195–214. [Google Scholar]
- 17.Lehmann M., Bruenahl C.A., Löwe B. Ebola and psychological stress of health care professionals. Emerging Infectious Diseases. 2015;21:913. doi: 10.3201/eid2105.141988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levin J. Psychiatry of Pandemics. Springer; 2019. Mental health care for survivors and healthcare workers in the aftermath of an outbreak; pp. 127–141. [Google Scholar]
- 19.Medic G., Wille M., Hemels M.E. Short-and long-term health consequences of sleep disruption. Nature and Science of Sleep. 2017;9:151. doi: 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiong J., Lipsitz O., Nasri F. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balanzá-Martínez V., Kapczinski F., de Azevedo Cardoso T. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Revista de Psiquiatria y Salud Mental. 2021;14(1):14–26. doi: 10.1016/j.rpsm.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodríguez-Rey R., Garrido-Hernansaiz H., Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Frontiers in Psychology. 2020;11:1540. doi: 10.3389/fpsyg.2020.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dul A.J. I am trying to avoid busy supermarkets. So, this morning, I was at the supermarket at 8 AM already. A qualitative research about the adaptive behaviour and quality of life of independently living older adults in the Northern Netherlands during the COVID-19 outbreak. 2020 [Google Scholar]
- 24.Mutz M., Gerke M. Sport and exercise in times of self-quarantine: how Germans changed their behaviour at the beginning of the COVID-19 pandemic. International Review for the Sociology of Sport. 2021;56(3):305–316. doi: 10.1177/1012690220934335. [DOI] [Google Scholar]
- 25.Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu C., Liu Y. Media exposure and anxiety during COVID-19: the mediation effect of media vicarious traumatization. International journal of environmental research and public health. 2020;17:4720. doi: 10.3390/ijerph17134720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID-19: mental health burden and strategies. Brazilian Journal of Psychiatry. 2020;42:232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee A. Wuhan novel coronavirus (COVID-19): why global control is challenging? Public Health. 2020;179:A1. doi: 10.1016/j.puhe.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang W.-r., Wang K., Yin L. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychotherapy and Psychosomatics. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanderson W.C., Arunagiri V., Funk A.P. The nature and treatment of pandemic-related psychological distress. Journal of Contemporary Psychotherapy. 2020;27:1–13. doi: 10.1007/s10879-020-09463-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin L.-y., Wang J., Ou-yang X.-y. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Medicine. 2021;77:348–354. doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qi J., Xu J., Li B.-Z. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Medicine. 2020;72:1–4. doi: 10.1016/j.sleep.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qiu D., Yu Y., Li R.-Q., Li Y.-L., Xiao S.-Y. Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Medicine. 2020;67:258–266. doi: 10.1016/j.sleep.2019.01.047. [DOI] [PubMed] [Google Scholar]
- 34.AlSaif H.I. Prevalence of and risk factors for poor sleep quality among residents in training in KSA. Journal of Taibah University Medical Sciences. 2019;14:52–59. doi: 10.1016/j.jtumed.2018.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zeng L.-N., Yang Y., Wang C. Prevalence of poor sleep quality in nursing staff: a meta-analysis of observational studies. Behavioral Sleep Medicine. 2020;18:746–759. doi: 10.1080/15402002.2019.1677233. [DOI] [PubMed] [Google Scholar]
- 36.Pakpour A.H., Griffiths M.D., Ohayon M.M., Broström A., Lin C.-Y. A Good Sleep: The Role of Factors in Psychosocial Health. Frontiers in Neuroscience. 2020;14:520. doi: 10.3389/fnins.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang W., Song W., Xia Z. Sleep disturbance and psychological profiles of medical staff and non-medical staff during the early outbreak of COVID-19 in Hubei Province, China. Frontiers in Psychiatry. 2020;11:733. doi: 10.3389/fpsyt.2020.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jahrami H., BaHammam A.S., Bragazzi N.L., Saif Z., Faris M., Vitiello M.V. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. Journal of Clinical Sleep Medicine. 2021;17:299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang C., Huang L., Wang Y. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 42.Alimoradi Z., Pakpour A. Sleep and Covid-19 related psychological distress. PROSPERO 2020 CRD42020181644. 2020 [Google Scholar]
- 43.Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 44.Morin C.M., Belleville G., Bélanger L., Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ridner S.H. Psychological distress: concept analysis. Journal of Advanced Nursing. 2004;45:536–545. doi: 10.1046/j.1365-2648.2003.02938.x. [DOI] [PubMed] [Google Scholar]
- 46.Luchini C., Stubbs B., Solmi M., Veronese N. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa Scale. World Journal of Meta-Analysis. 2017;5:80–84. [Google Scholar]
- 47.Hox J.J. and Leeuw E.D.d. Multilevel models for meta-analysis. 2003.
- 48.Huedo-Medina T.B., Sánchez-Meca J., Marín-Martínez F., Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods. 2006;11:193. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 49.Cohen J. Academic press; 2013. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 50.Rosenthal R., Cooper H., Hedges L. Parametric measures of effect size. The handbook of research synthesis. 1994;621:231–244. [Google Scholar]
- 51.Lenhard W., Lenhard A. Psychometrica; Dettelbach (Germany): 2016. Calculation of Effect Sizes. [Google Scholar]
- 52.Lipsey M.W., Wilson D.B. SAGE publications, Inc; 2001. Practical meta-analysis. [Google Scholar]
- 53.Alimoradi Z., Golboni F., Griffiths M.D., Broström A., Lin C.-Y., Pakpour A.H. Weight-related stigma and psychological distress: A systematic review and meta-analysis. Clinical Nutrition. 2020;39(7):2001–2013. doi: 10.1016/j.clnu.2019.10.016. [DOI] [PubMed] [Google Scholar]
- 54.Borenstein M., Hedges L., Higgins J., Rothstein H. Introduction to Meta-Analysis. John Wiley & Sons Ltd; West Sussex, UK: 2009. Complex data structures; pp. 215–245. [Google Scholar]
- 55.Rothstein H.R., Sutton A.J., Borenstein M. Publication bias in meta-analysis. Publication bias in meta-analysis: Prevention, assessment and adjustments. 2005:1–7. [Google Scholar]
- 56.Hedges L., Olkin I. Academic press; 2014. Statistical methods for meta-analysis. [Google Scholar]
- 57.Lin C.-Y., Broström A., Griffiths M.D., Pakpour A.H. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interventions. 2020;21 doi: 10.1016/j.invent.2020.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Majd N.R., Broström A., Ulander M. Efficacy of a Theory-Based Cognitive Behavioral Technique App-Based Intervention for Patients With Insomnia: Randomized Controlled Trial. Journal of Medical Internet Research. 2020;22:e15841. doi: 10.2196/15841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vaghela P., Sutin A.R. Discrimination and sleep quality among older US adults: the mediating role of psychological distress. Sleep Health. 2016;2:100–108. doi: 10.1016/j.sleh.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 60.Mazzer K., Boersma K., Linton S.J. A longitudinal view of rumination, poor sleep and psychological distress in adolescents. Journal of Affective Disorders. 2019;245:686–696. doi: 10.1016/j.jad.2018.11.053. [DOI] [PubMed] [Google Scholar]
- 61.Pramukti I., Strong C., Sitthimongkol Y. Anxiety and suicidal thoughts during COVID-19 pandemic: A cross-country comparison among Indonesian, Taiwanese, and Thai university students. Journal of Medical Internet Research. 2020;22(12):e24487. doi: 10.2196/24487. Accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen C.-Y., Chen I.-H., O’Brien K.S., Latner J.D., Lin C.-Y. Psychological distress and internet-related behaviors between schoolchildren with and without overweight during the COVID-19 outbreak. International Journal of Obesity. 2021;45:677–686. doi: 10.1038/s41366-021-00741-5. Accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mamun M.A., Sakib N., Gozal D. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. Journal of Affective Disorders. 2020;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chang K.-C., Strong C., Pakpour A.H., Griffiths M.D., Lin C.-Y. Factors related to preventive COVID-19 infection behaviors among people with mental illness. Journal of the Formosan Medical Association. 2020;119(12):1772–1780. doi: 10.1016/j.jfma.2020.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lin C.Y., Imani V., Majd N.R. Using an integrated social cognition model to predict COVID-19 preventive behaviours. British Journal of Health Psychology. 2020;25(4):981–1005. doi: 10.1111/bjhp.12465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen I.H., Chen C.Y., Pakpour A.H., Griffiths M.D., Lin C.Y. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. Journal of the American Academy of Child and Adolescent Psychiatry. 2020;159:1099–1102. doi: 10.1016/j.jaac.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhuo K, Gao C, Wang X, Zhang C, Wang Z. Stress and sleep: a survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID-19 pandemic. General Psychiatry. 2020;33(3) doi: 10.1136/gpsych-2020-100260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry research. 2020:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Medical science monitor: international medical journal of experimental and clinical research. 2020;26:e923921–1. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain, behavior, and immunity. 2020 doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N= 18147 web-based survey. medRxiv. 2020 doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tu Z-h, He J-w, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine. 2020;99(26) doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jahrami H, BaHammam AS, AlGahtani H, Ebrahim A, Faris M, AlEid K. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep and Breathing. 2020:1–9. doi: 10.1007/s11325-020-02135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. International journal of environmental research and public health. 2020;17(14):5218. doi: 10.3390/ijerph17145218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Romero-Blanco C, Rodríguez-Almagro J, Onieva-Zafra MD, Parra-Fernández ML, Prado-Laguna MdC, Hernández-Martínez A. Sleep Pattern Changes in Nursing Students during the COVID-19 Lockdown. International Journal of Environmental Research and Public Health. 2020;17(14):5222. doi: 10.3390/ijerph17145222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fu W, Wang C, Zou L, Guo Y, Lu Z, Yan S. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Translational psychiatry. 2020;10(1):1–9. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guo J, Feng XL, Wang XH, van IJzendoorn MH. Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults. International Journal of Environmental Research and Public Health. 2020;17(11):3857. doi: 10.3390/ijerph17113857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang Y, Zhang H, Ma X, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. International journal of environmental research and public health. 2020;17(10):3722. doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhou Y, Shi H, Liu Z, Peng S, Wang R, Qi L. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Translational psychiatry. 2020;10(1):1–7. doi: 10.1038/s41398-020-01006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occupational Medicine (Oxford; England: 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Giardino DL, Huck-Iriart C, Riddick M, Garay A. The endless quarantine: The impact of the COVID-19 outbreak on healthcare workers after three months of mandatory social isolation in Argentina. Sleep medicine. 2020;76:16–25. doi: 10.1016/j.sleep.2020.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Medical science monitor: international medical journal of experimental and clinical research. 2020;26:e923549–1. doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Marelli S, Castelnuovo A, Somma A, Castronovo V, Mombelli S, Bottoni D. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of Neurology. 2020:1–8. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wu K, Wei X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Medical Science Monitor Basic Research. 2020;26:e924085–1. doi: 10.12659/MSMBR.924085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. International journal of environmental research and public health. 2020;17(13):4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Peng M, Mo B, Liu Y, Xu M, Song X, Liu L. Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. Journal of affective disorders. 2020;275:119–124. doi: 10.1016/j.jad.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. Journal of psychosomatic research. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhou S-J, Wang L-L, Yang R, Yang X-J, Zhang L-G, Guo Z-C. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Medicine. 2020 doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Huang Y, Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian Journal of Psychiatry. 2020;51:102052. doi: 10.1016/j.ajp.2020.102052. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 91.Assenza G, Lanzone J, Brigo F, Coppola A, Di Gennaro G, Di Lazzaro V. Epilepsy care in the time of COVID-19 pandemic in Italy: risk factors for seizure worsening. Frontiers in neurology. 2020;11:737. doi: 10.3389/fneur.2020.00737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Que J, Le Shi JD, Liu J, Zhang L, Wu S, Gong Y. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. General psychiatry. 2020;33(3) doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain, behavior, and immunity. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Song L, Wang Y, Li Z, Yang Y, Li H. Mental health and work attitudes among people resuming work during the Covid-19 pandemic: A cross-sectional study in China. International journal of environmental research and public health. 2020;17(14):5059. doi: 10.3390/ijerph17145059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ren Y, Qian W, Li Z, Liu Z, Zhou Y, Wang R. Public mental health under the long-term influence of COVID-19 in China: Geographical and temporal distribution. Journal of Affective Disorders. 2020;277:893–900. doi: 10.1016/j.jad.2020.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shi L, Lu Z-A, Que J-Y, Huang X-L, Liu L, Ran M-S. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA network open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, behavior, and immunity. 2020 doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Caballero-Domínguez CC, Jiménez-Villamizar MP, Campo-Arias A. Suicide risk during the lockdown due to coronavirus disease (COVID-19) in Colombia. Death studies. 2020:1–6. doi: 10.1080/07481187.2020.1784312. [DOI] [PubMed] [Google Scholar]
- 99.Liu C, Stevens C, Conrad R, Hahm H. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among US young adults with suspected and reported psychiatric diagnoses. Psychiatry research. 2020;292:113345. doi: 10.1016/j.psychres.2020.113345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Stojanov J, Malobabic M, Stanojevic G, Stevic M, Milosevic V, Stojanov A. Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. The International journal of social psychiatry. 2020 doi: 10.1177/0020764020942800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cheng F-F, Zhan S-H, Xie A-W, Cai S-Z, Hui L, Kong X-X. Anxiety in Chinese pediatric medical staff during the outbreak of Coronavirus Disease 2019: a cross-sectional study. Translational pediatrics. 2020;9(3):231. doi: 10.21037/tp.2020.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID‐19 lockdown in Italy. Journal of Sleep Research. 2020 doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Amerio A, Bianchi D, Santi F, Costantini L, Odone A, Signorelli C. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio-medica: Atenei Parmensis. 2020;91(2):83–88. doi: 10.23750/abm.v91i2.9619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cai Q, Feng H, Huang J, Wang M, Wang Q, Lu X. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. Journal of affective disorders. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Idrissi AJ, Lamkaddem A, Benouajjit A, El Bouaazzaoui MB, El Houari F, Alami M. Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep medicine. 2020;74:248–253. doi: 10.1016/j.sleep.2020.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhou Y, Wang W, Sun Y, Qian W, Liu Z, Wang R. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: Workload should be concerned. Journal of affective disorders. 2020;277:510–514. doi: 10.1016/j.jad.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Juanjuan L, Santa-Maria CA, Hongfang F, Lingcheng W, Pengcheng Z, Yuangbing X. Patient reported outcomes of breast cancer patients during the COVID-19 outbreak in the epicenter of China: A cross sectional survey study. Clinical Breast Cancer. 2020 doi: 10.1016/j.clbc.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang H, Huang D, Huang H, Zhang J, Guo L, Liu Y. The psychological impact of COVID-19 pandemic on medical staff in Guangdong, China: a cross-sectional study. Psychological medicine. 2020:1–9. doi: 10.1017/S0033291720002561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kang L, Ma S, Chen M, Yang J, Wang Y, Li R. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, behavior, and immunity. 2020 doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhan Y, Liu Y, Liu H, Li M, Shen Y, Gui L. Factors associated with insomnia among Chinese front‐line nurses fighting against COVID‐19 in Wuhan: A cross‐sectional survey. Journal of nursing management. 2020;28(7):1525–1535. doi: 10.1111/jonm.13094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wang X, Lei SM, Le S, Yang Y, Zhang B, Yao W. Bidirectional influence of the COVID-19 pandemic lockdowns on health behaviors and quality of life among chinese adults. International journal of environmental research and public health. 2020;17(15):5575. doi: 10.3390/ijerph17155575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhou Y, Yang Y, Shi T, Song Y, Zhou Y, Zhang Z. Prevalence and Demographic Correlates of Poor Sleep Quality Among Frontline Health Professionals in Liaoning Province, China During the COVID-19 Outbreak. Frontiers in Psychiatry. 2020;11:520. doi: 10.3389/fpsyt.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang J, Xu D, Xie B, Zhang Y, Huang H, Liu H. Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: A retrospective cohort study. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wasim T, e Raana G, Bushra N, Riaz A. Effect of COVID-19 pandemic on mental wellbeing of healthcare workers in tertiary care hospital. Annals of King Edward Medical University. 2020;(26(Special Issue):):140–144. [Google Scholar]
- 116.Lu C, Chi X, Liang K, Chen S-T, Huang L, Guo T. Moving More and Sitting Less as Healthy Lifestyle Behaviors are Protective Factors for Insomnia, Depression, and Anxiety Among Adolescents During the COVID-19 Pandemic. Psychology research and behavior management. 2020;13:1223. doi: 10.2147/PRBM.S284103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yitayih Y, Mekonen S, Zeynudin A, Mengistie E, Ambelu A. Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. BJPsych Open. 2021;7(1) doi: 10.1192/bjo.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tselebis A, Lekka D, Sikaras C, Tsomaka E, Tassopoulos A. Ilias I. In: Insomnia, editor. Perceived Stress, and Family Support among Nursing Staff during the Pandemic Crisis. Healthcare; 2020: Multidisciplinary Digital Publishing Institute; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liu T, Zheng Z, Sha X, Liu H, Zheng W, Su H. Psychological impact in non-infectious disease specialists who had direct contact with patients with COVID-19. BJPsych open. 2021;7(1) doi: 10.1192/bjo.2020.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Rossi R, Socci V, Pacitti F, Mensi S, Di Marco A, Siracusano A. Mental Health Outcomes Among Healthcare Workers and the General Population During the COVID-19 in Italy. Frontiers in Psychology. 2020;11:3332. doi: 10.3389/fpsyg.2020.608986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sharma R, Seth S, Solanki HK, Mishra N, Srivastava A, Jakhar K. COVID-19 and Obstetrical Care: Coping With New Stress. Cureus. 2020;12(12) doi: 10.7759/cureus.12116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ammar A, Trabelsi K, Brach M, Chtourou H, Boukhris O, Masmoudi L. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: Insight from the “ECLB-COVID19” multi countries survey. Biology of Sport. 2021;28:9–21. doi: 10.5114/biolsport.2020.96857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Tiete J, Guatteri M, Lachaux A, Matossian A, Hougardy J-M, Loas G. Mental health outcomes in healthcare workers in COVID-19 and non-COVID-19 care units: a cross-sectional survey in Belgium. Frontiers in Psychology. 2020;11:3542. doi: 10.3389/fpsyg.2020.612241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Franceschini C, Musetti A, Zenesini C, Palagini L, Scarpelli S, Quattropani MC. Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy. Frontiers in psychology. 2020;11:3072. doi: 10.3389/fpsyg.2020.574475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Huang L, Lei W, Liu H, Hang R, Tao X, Zhan Y. Nurses’ Sleep Quality of “Fangcang” Hospital in China during the COVID-19 Pandemic. International Journal of Mental Health and Addiction. 2020:1–11. doi: 10.1007/s11469-020-00404-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Elkholy H, Tawfik F, Ibrahim I, Salah El-din W, Sabry M, Mohammed S. Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: A call for action. International Journal of Social Psychiatry. 2020 doi: 10.1177/0020764020960192. 0020764020960192. [DOI] [PubMed] [Google Scholar]
- 127.Yang BX, Xia L, Huang R, Chen P, Luo D, Liu Q. Relationship between eHealth literacy andpsychological status during COVID‐19 pandemic A survey of Chinese residents. Journal of nursing management. 2020 doi: 10.1111/jonm.13221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yang G, Xiao C, Li S, Yang N. The effect and mechanism of adverse childhood experience on suicide ideation in young cancer patients during coronavirus disease 2019 (COVID-19) pandemic. Risk management and healthcare policy. 2020;13:1293. doi: 10.2147/RMHP.S266269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Caballero‐Domínguez CC, De Luque‐Salcedo JG, Campo‐Arias A. Social capital and psychological distress during Colombian coronavirus disease lockdown. Journal of Community Psychology. 2020 doi: 10.1002/jcop.22487. [DOI] [PubMed] [Google Scholar]
- 130.Khamis F, Al Mahyijari N, Al Lawati F, Badahdah AM. The Mental Health of Female Physicians and Nurses in Oman during the COVID-19 Pandemic. Oman Medical Journal. 2020;35(6) doi: 10.5001/omj.2020.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sañudo B, Fennell C, Sánchez-Oliver AJ. Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns pre-and during-COVID-19 quarantine in young adults from spain. Sustainability. 2020;12(15):5890. [Google Scholar]
- 132.Jain A, Singariya G, Kamal M, Kumar M, Jain A, Solanki RK. COVID-19 pandemic: Psychological impact on anaesthesiologists. Indian journal of anaesthesia. 2020;64(9):774. doi: 10.4103/ija.IJA_697_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Agberotimi SF, Akinsola OS, Oguntayo R, Olaseni AO. Interactions between socioeconomic status and mental health outcomes in the nigerian context amid covid-19 pandemic: a comparative study. Frontiers in Psychology. 2020;11:2655. doi: 10.3389/fpsyg.2020.559819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bhat BA, Mir RA, Hussain A, Shah IR. Depressive and anxiety symptoms, quality of sleep, and coping during the 2019 coronavirus disease pandemic in general population in Kashmir. Middle East. Current Psychiatry. 2020;27(1):1–10. [Google Scholar]
- 135.McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. Journal of Contextual Behavioral Science. 2021;19:28–35. [Google Scholar]
- 136.Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, Bouaziz B. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biology of Sport. 2020;38:495–506. doi: 10.5114/biolsport.2021.101605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chi X, Liang K, Chen S-T, Huang Q, Huang L, Yu Q. Mental health problems among Chinese adolescents during the COVID-19: The importance of nutrition and physical activity. International Journal of Clinical and Health Psychology. 2020:100218. doi: 10.1016/j.ijchp.2020.100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Liu C, Liu D, Huang N, Fu M, Ahmed JF, Zhang Y. The Combined Impact of Gender and Age on Post-traumatic Stress Symptoms, Depression, and Insomnia During COVID-19 Outbreak in China. Frontiers in Public Health. 2020;8 doi: 10.3389/fpubh.2020.620023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Alamrawy RG, Fadl N, Khaled A. Psychiatric morbidity and dietary habits during COVID-19 pandemic: a cross-sectional study among Egyptian Youth (14–24 years). Middle East. Current Psychiatry. 2021;28(1):1–10. [Google Scholar]
- 140.Haravuori H, Junttila K, Haapa T, Tuisku K, Kujala A, Rosenström T. Personnel Well-Being in the Helsinki University Hospital during the COVID-19 Pandemic—A Prospective Cohort Study. International journal of environmental research and public health. 2020;17(21):7905. doi: 10.3390/ijerph17217905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Khaled SM, Petcu C, Al-Thani MA, Al-Hamadi AMH, Daher-Nashif S, Zolezzi M. Prevalence and associated factors of DSM-5 insomnia disorder in the general population of Qatar. BMC psychiatry. 2021;21(1):1–10. doi: 10.1186/s12888-020-03035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Alomayri W, Alanazi N, Faraj F. Correlation Between Atopic Dermatitis and Sleep Quality Among Adults in Saudi Arabia. Cureus. 2020;12(12) doi: 10.7759/cureus.12051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Akıncı T, Başar HM. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep medicine. 2021;80:167–170. doi: 10.1016/j.sleep.2021.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Barua L, Zaman MS, Omi FR, Faruque M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: a cross-sectional study. 2020;9 doi: 10.12688/f1000research.27189.1. F1000Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. European Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Fidanci İ, derinöz Güleryüz O, Fidanci İ. An analysis on sleep quality of the healthcare professionals during the covid-19 pandemic. Acta Medica. 2020;36:3797. [Google Scholar]
- 147.Chouchou F, Augustini M, Caderby T, Caron N, Turpin NA, Dalleau G. The importance of sleep and physical activity on well-being during COVID-19 lockdown: Reunion island as a case study. Sleep medicine. 2020 doi: 10.1016/j.sleep.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cheng C, Ebrahimi OV, Lau Yc. Maladaptive coping with the infodemic and sleep disturbance in the COVID‐19 pandemic. Journal of Sleep Research. 2020 doi: 10.1111/jsr.13235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pedrozo-Pupo JC, Campo-Arias A. Depression, perceived stress related to COVID, post-traumatic stress, and insomnia among asthma and COPD patients during the COVID-19 pandemic. Chronic respiratory disease. 2020;17 doi: 10.1177/1479973120962800. 1479973120962800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Targa AD, Benítez ID, Moncusí-Moix A, Arguimbau M, de Batlle J, Dalmases M. Decrease in sleep quality during COVID-19 outbreak. Sleep and Breathing. 2020:1–7. doi: 10.1007/s11325-020-02202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Than HM, Nong VM, Nguyen CT, Dong KP, Ngo HT, Doan TT. Mental Health and Health-Related Quality-of-Life Outcomes Among Frontline Health Workers During the Peak of COVID-19 Outbreak in Vietnam: A Cross-Sectional Study. Risk management and healthcare policy. 2020;13:2927. doi: 10.2147/RMHP.S280749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Youssef N, Mostafa A, Ezzat R, Yosef M, El Kassas M. Mental health status of health-care professionals working in quarantine and non-quarantine Egyptian hospitals during the COVID-19 pandemic. East Mediterr Health J. 2020:1155–1164. doi: 10.26719/emhj.20.116. [DOI] [PubMed] [Google Scholar]
- 153.Ge F, Di Zhang LW, Mu H. Predicting Psychological State Among Chinese Undergraduate Students in the COVID-19 Epidemic: A Longitudinal Study Using a Machine Learning. Neuropsychiatric Disease and Treatment. 2020;16:2111. doi: 10.2147/NDT.S262004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Almater AI, Tobaigy MF, Younis AS, Alaqeel MK, Abouammoh MA. Effect of 2019 coronavirus pandemic on ophthalmologists practicing in Saudi Arabia: A psychological health assessment. Middle East African. Journal of Ophthalmology. 2020;27(2):79. doi: 10.4103/meajo.MEAJO_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gupta R, Grover S, Basu A, Krishnan V, Tripathi A, Subramanyam A. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62(4):370–378. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2020:110236. doi: 10.1016/j.pnpbp.2020.110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Li W, Zhao N, Yan X, Zou S, Wang H, Li Y. The prevalence of depressive and anxiety symptoms and their associations with quality of life among clinically stable older patients with psychiatric disorders during the COVID-19 pandemic. Translational Psychiatry. 2021;11(1):1–8. doi: 10.1038/s41398-021-01196-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Duran S, Erkin Ö. Psychologic distress and sleep quality among adults in Turkey during the COVID-19 pandemic. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2021;107:110254. doi: 10.1016/j.pnpbp.2021.110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Yang G, Li C, Zhu X, Yan J, Liu J. Prevalence of and risk factors associated with sleep disturbances among HPCD exposed to COVID-19 in China. Sleep Medicine. 2021;80:16–22. doi: 10.1016/j.sleep.2020.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Martínez-de-Quel Ó, Suárez-Iglesias D, López-Flores M, Pérez CA. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: A longitudinal study. Appetite. 2020;158:105019. doi: 10.1016/j.appet.2020.105019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. COVID-19 and Mental Health During Pregnancy: The Importance of Cognitive Appraisal and Social Support. Journal of Affective Disorders. 2021;282 doi: 10.1016/j.jad.2021.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wang M, Zhao Q, Hu C, Wang Y, Cao J, Huang S. Prevalence of psychological disorders in the COVID-19 epidemic in China: A real world cross-sectional study. Journal of affective disorders. 2020;281:312–320. doi: 10.1016/j.jad.2020.11.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zreik G, Asraf K, Haimov I, Tikotzky L. Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID‐19) pandemic in Israel. Journal of sleep research. 2021;30(1) doi: 10.1111/jsr.13201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zhang X, Zou R, Liao X, Bernardo AB, Du H, Wang Z. Perceived Stress, Hope, and Health Outcomes Among Medical Staff in China During the COVID-19 Pandemic. Frontiers in Psychiatry. 2021;11:1646. doi: 10.3389/fpsyt.2020.588008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Al Ammari M, Sultana K, Thomas A, Al Swaidan L, Al Harthi N. Mental Health Outcomes Amongst Health Care Workers During COVID 19 Pandemic in Saudi Arabia. Frontiers in Psychiatry. 2021;11 doi: 10.3389/fpsyt.2020.619540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Essangri H, Sabir M, Benkabbou A, Majbar MA, Amrani L, Ghannam A. Predictive Factors for Impaired Mental Health among Medical Students during the Early Stage of the COVID-19 Pandemic in Morocco. The American journal of tropical medicine and hygiene. 2020;104(1):95–102. doi: 10.4269/ajtmh.20-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Yitayih Y, Lemu YK, Mekonen S, Mecha M, Ambelu A. Psychological impact of COVID-19 outbreak among Jimma University Medical Centere visitors in Southwestern Ethiopia: a cross-sectional study. BMJ open. 2021;11(1) doi: 10.1136/bmjopen-2020-043185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Xie M, Wang X, Zhang J, Wang Y. Alteration in the psychologic status and family environment of pregnant women before and during the Covid‐19 pandemic. International Journal of Gynecology & Obstetrics. 2021 doi: 10.1002/ijgo.13575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zhang X, Liu J, Han N, YinSocial Media Use J. Unhealthy Lifestyles, and the Risk of Miscarriage Among Pregnant Women During the COVID-19 Pandemic: Prospective Observational Study. JMIR Public Health and Surveillance. 2021;7(1) doi: 10.2196/25241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Massicotte V, Ivers H, Savard J. COVID-19 Pandemic Stressors and Psychological Symptoms in Breast Cancer Patients. Current Oncology. 2021;28(1):294–300. doi: 10.3390/curroncol28010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Poyraz BÇ, Poyraz CA, Olgun Y, Gürel Ö, Alkan S, Özdemir YE. Psychiatric morbidity and protracted symptoms after COVID-19. Psychiatry research. 2020;295:113604. doi: 10.1016/j.psychres.2020.113604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chen X, Wang L, Liu L, Jiang M, Wang W, Zhou X. Factors associated with psychological distress among patients with breast cancer during the COVID-19 pandemic: a cross-sectional study in Wuhan, China. Supportive Care in Cancer. 2020;1:1–10. doi: 10.1007/s00520-021-05994-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lahiri A, Jha SS, Acharya R, Dey A, Chakraborty A. Correlates of insomnia among the adults during COVID19 pandemic: evidence from an online survey in India. Sleep medicine. 2020;77:66–73. doi: 10.1016/j.sleep.2020.11.020. [DOI] [PubMed] [Google Scholar]
- 174.Cellini N, Conte F, De Rosa O, Giganti F, Malloggi S, Reyt M. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Medicine. 2020;77:112–119. doi: 10.1016/j.sleep.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Sunil R, Bhatt MT, Bhumika TV, Thomas N, Puranik A, Chaudhuri S. Weathering the Storm: Psychological Impact of COVID-19 Pandemic on Clinical and Nonclinical Healthcare Workers in India. Indian Journal of Critical Care Medicine: Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine. 2021;25(1):16. doi: 10.5005/jp-journals-10071-23702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Yadav R, Yadav P, Kumar SS, Kumar R. Assessment of Depression, Anxiety, and Sleep Disturbance in COVID-19 Patients at Tertiary Care Centre of North India. Journal of Neurosciences in Rural Practice. 2021 doi: 10.1055/s-0040-1722811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Scotta AV, Cortez MV, Miranda AR. Insomnia is associated with worry, cognitive avoidance and low academic engagement in Argentinian university students during the COVID-19 social isolation. Psychology, health & medicine. 2021:1–16. doi: 10.1080/13548506.2020.1869796. [DOI] [PubMed] [Google Scholar]
- 178.He Q, Fan B, Xie B, Liao Y, Han X, Chen Y. Mental health conditions among the general population, healthcare workers and quarantined population during the coronavirus disease 2019 (COVID-19) pandemic. Psychology, health & medicine. 2021:1–13. doi: 10.1080/13548506.2020.1867320. [DOI] [PubMed] [Google Scholar]
- 179.Zhang X, Zhao K, Zhang G, Feng R, Chen J, Xu D. Occupational Stress and Mental Health: A Comparison Between Frontline Medical Staff and Non-frontline Medical Staff During the 2019 Novel Coronavirus Disease Outbreak. Frontiers in Psychiatry. 2020;11:1543. doi: 10.3389/fpsyt.2020.555703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Demartini B, Nisticò V, D’Agostino A, Priori A, Gambini O. Early psychiatric impact of COVID-19 pandemic on the general population and healthcare workers in Italy: a preliminary study. Frontiers in psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.561345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Cui Q, Cai Z, Li J, Liu Z, Sun S, Chen C. The Psychological Pressures of Breast Cancer Patients During the COVID-19 Outbreak in China—A Comparison With Frontline Female Nurses. Frontiers in psychiatry. 2020;11:1462. doi: 10.3389/fpsyt.2020.559701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Bacaro V, Chiabudini M, Buonanno C, De Bartolo P, Riemann D, Mancini F. Insomnia in the Italian population during Covid-19 Outbreak: A snapshot on one major risk factor for Depression and Anxiety. Frontiers in psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.579107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Gu Y, Zhu Y, Xu G. Factors associated with mental health outcomes among health care workers in the Fangcang shelter hospital in China. International Journal of Social Psychiatry. 2020 doi: 10.1177/0020764020975805. 0020764020975805. [DOI] [PubMed] [Google Scholar]
- 184.Liu D, Liu S, Zhu L, Li D, Huang D, Deng H. Prevalence and related factors of insomnia among Chinese medical staff in the middle and late stage of COVID-19. Frontiers in psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.602315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Wang Q, Feng H, Wang M, Xie Y, Hou B, Lu X. Mental health and psychological responses during the coronavirus disease 2019 (COVID-19) epidemic: A comparison between Wuhan and other areas in China. Psychosomatic medicine. 2021 doi: 10.1097/PSY.0000000000000892. [DOI] [PubMed] [Google Scholar]
- 186.Abdulah DM, Musa DH. Insomnia and stress of physicians during COVID-19 outbreak. Sleep Medicine: X. 2020;2:100017. doi: 10.1016/j.sleepx.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. Journal of psychiatric research. 2020;131:132–137. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kocevska D, Blanken TF, Van Someren EJ, Rösler L. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep medicine. 2020;76:86–88. doi: 10.1016/j.sleep.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Zhang H, Qin S, Zhang L, Feng Z, Fan C. A psychological investigation of coronavirus disease 2019 (COVID-19) patients in mobile cabin hospitals in Wuhan. Annals of Translational Medicine. 2020;8(15) doi: 10.21037/atm-20-4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Fazeli S, Zeidi IM, Lin C-Y, Namdar P, Griffiths MD, Ahorsu DK. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addictive Behaviors Reports. 2020;12:100307. doi: 10.1016/j.abrep.2020.100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Bajaj S, Blair KS, Schwartz A, Dobbertin M, Blair RJR. Worry and insomnia as risk factors for depression during initial stages of COVID-19 pandemic in India. PloS one. 2020;15(12) doi: 10.1371/journal.pone.0243527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Kilani HA, Bataineh MaF, Al-Nawayseh A, Atiyat K, Obeid O, Abu-Hilal MM. Healthy lifestyle behaviors are major predictors of mental wellbeing during COVID-19 pandemic confinement: A study on adult Arabs in higher educational institutions. Plos one. 2020;15(12) doi: 10.1371/journal.pone.0243524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Necho M, Birkie M, Gelaye H, Beyene A, Belete A, Tsehay M. Depression, anxiety symptoms, Insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. PloS one. 2020;15(12) doi: 10.1371/journal.pone.0244530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Şahin MK, Aker S, Şahin G, Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. Journal of Community Health. 2020;45(6):1168–1177. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.McCall WV, Mensah-Bonsu D, Withers AE, Gibson RW. Short-term insomnia disorder in health care workers in an academic medical center before and during COVID-19: rates and predictive factors. Journal of Clinical Sleep Medicine. 2020;jcsm.:9034. doi: 10.5664/jcsm.9034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Lai AY-k, Lee L, Wang M-p, Feng Y, Lai TT-k, Ho L-m. Mental health impacts of the COVID-19 pandemic on international university students, related stressors, and coping strategies. Frontiers in Psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.584240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wang X, Chen H, Liu L, Liu Y, Zhang N, Sun Z. Anxiety and sleep problems of college students during the outbreak of COVID-19. Frontiers in Psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.588693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Sagherian K, Steege LM, Cobb SJ, ChoInsomnia H. fatigue and psychosocial well‐being during COVID‐19 pandemic: A cross‐sectional survey of hospital nursing staff in the United States. Journal of clinical nursing. 2020 doi: 10.1111/jocn.15566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Magnavita N, Soave PM, Ricciardi W, Antonelli M. Occupational Stress and Mental Health among Anesthetists during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2020;17(21):8245. doi: 10.3390/ijerph17218245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep medicine. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Marroquín B, Vine V, Morgan R. Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry research. 2020;293:113419. doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Wang Y, Zhu L-Y, Ma Y-F, Bo H-X, Deng H-B, Cao J. Association of insomnia disorder with sociodemographic factors and poor mental health in COVID-19 inpatients in China. Sleep Medicine. 2020;75:282–286. doi: 10.1016/j.sleep.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.San Martin AH, Serrano JP, Cambriles TD, Arias EMA, Méndez JM, del Yerro Álvarez MJ. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep medicine. 2020;75:388–394. doi: 10.1016/j.sleep.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Florin M, Pinar U, Chavigny E, Bouaboula M, Jarboui L, Coulibaly A. Socio-economic and psychological impact of the COVID-19 outbreak on private practice and public hospital radiologists. European journal of radiology. 2020;132:109285. doi: 10.1016/j.ejrad.2020.109285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Zhang Y, Wang S, Ding W, Meng Y, Hu H, Liu Z. Status and influential factors of anxiety depression and insomnia symptoms in the work resumption period of COVID-19 epidemic: A multicenter cross-sectional study. Journal of Psychosomatic Research. 2020;138:110253. doi: 10.1016/j.jpsychores.2020.110253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Xia Y, Kou L, Zhang G, Han C, Hu J, Wan F. Investigation on sleep and mental health of patients with Parkinson’s disease during the Coronavirus disease 2019 pandemic. Sleep medicine. 2020;75:428–433. doi: 10.1016/j.sleep.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Zanghì A, D’Amico E, Luca M, Ciaorella M, Basile L, Patti F. Mental health status of relapsing-remitting multiple sclerosis Italian patients returning to work soon after the easing of lockdown during COVID-19 pandemic: A monocentric experience. Multiple Sclerosis and Related Disorders. 2020;46:102561. doi: 10.1016/j.msard.2020.102561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Saracoglu KT, Simsek T, Kahraman S, Bombaci E, Sezen Ö, Saracoglu A. The psychological impact of Covid-19 disease is more severe on Intensive Care Unit healthcare providers: a cross-sectional study. Clinical Psychopharmacology and Neuroscience. 2020;18(4):607–615. doi: 10.9758/cpn.2020.18.4.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Alnofaiey YH, Alshehri HA, Alosaimi MM, Alswat SH, Alswat RH, Alhulayfi RM. Sleep disturbances among physicians during COVID-19 pandemic. BMC research notes. 2020;13(1):1–7. doi: 10.1186/s13104-020-05341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Saraswathi I, Saikarthik J, Kumar KS, Srinivasan KM, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8 doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Badellino H, Gobbo ME, Torres E, Aschieri ME. Early indicators and risk factors associated with mental health problems during COVID-19 quarantine: Is there a relationship with the number of confirmed cases and deaths? The International Journal of Social Psychiatry. 2020 doi: 10.1177/0020764020966020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Bigalke JA, Greenlund IM, Carter JR. Sex differences in self-report anxiety and sleep quality during COVID-19 stay-at-home orders. Biology of sex Differences. 2020;11(1):1–11. doi: 10.1186/s13293-020-00333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Alshekaili M, Hassan W, Al Said N, Al Sulaimani F, Jayapal SK, Al-Mawali A. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ open. 2020;10(10) doi: 10.1136/bmjopen-2020-042030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Juanjuan L, Santa-Maria CA, Hongfang F, Lingcheng W, Pengcheng Z, Yuanbing X. Patient-reported outcomes of patients with breast cancer during the COVID-19 outbreak in the epicenter of China: a cross-sectional survey study. Clinical Breast Cancer. 2020;20(5):e651–e662. doi: 10.1016/j.clbc.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Yu BY-M, Yeung W-F, Lam JC-S, Yuen SC-S, Lam SC, Chung VC-H. Prevalence of sleep disturbances during covid-19 outbreak in an urban Chinese population: a cross-sectional study. Sleep medicine. 2020;74:18–24. doi: 10.1016/j.sleep.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Wang J, Gong Y, Chen Z, Wu J, Feng J, Yan S. Sleep disturbances among Chinese residents during the Coronavirus Disease 2019 outbreak and associated factors. Sleep medicine. 2020;74:199–203. doi: 10.1016/j.sleep.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Blekas A, Voitsidis P, Athanasiadou M, Parlapani E, Chatzigeorgiou AF, Skoupra M. COVID-19: PTSD symptoms in Greek health care professionals. Psychological Trauma: Theory, Research, Practice, and Policy. 2020 doi: 10.1037/tra0000914. [DOI] [PubMed] [Google Scholar]
- 218.Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Globalization and health. 2020;16(1):1–12. doi: 10.1186/s12992-020-00621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. International journal of environmental research and public health. 2020;17(18):6550. doi: 10.3390/ijerph17186550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Wańkowicz P, Szylińska A, Rotter I. Assessment of mental health factors among health professionals depending on their contact with COVID-19 patients. International Journal of Environmental Research and Public Health. 2020;17(16):5849. doi: 10.3390/ijerph17165849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Pieh C, O´ Rourke T, Budimir S, Probst T. Relationship quality and mental health during COVID-19 lockdown. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0238906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Alessi J, De Oliveira GB, Franco DW, Amaral DoBB, Becker AS, Knijnik CP. Mental health in the era of COVID-19: prevalence of psychiatric disorders in a cohort of patients with type 1 and type 2 diabetes during the social distancing. Diabetology & metabolic syndrome. 2020;12(1):1–10. doi: 10.1186/s13098-020-00584-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Huang Y, Wang Y, Zeng L, Yang J, Song X, Rao W. Prevalence and correlation of anxiety, insomnia and somatic symptoms in a Chinese population during the COVID-19 epidemic. Frontiers in psychiatry. 2020;11:894. doi: 10.3389/fpsyt.2020.568329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.McCracken LM, Badinlou F, Buhrman M, Brocki KC. Psychological impact of COVID-19 in the Swedish population: Depression, anxiety, and insomnia and their associations to risk and vulnerability factors. European Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Parlapani E, Holeva V, Nikopoulou VA, Sereslis K, Athanasiadou M, Godosidis A. Intolerance of uncertainty and loneliness in older adults during the COVID-19 pandemic. Frontiers in psychiatry. 2020;11:842. doi: 10.3389/fpsyt.2020.00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Barrea L, Pugliese G, Framondi L, Di Matteo R, Laudisio D, Savastano S. Does Sars-Cov-2 threaten our dreams? Effect of quarantine on sleep quality and body mass index. Journal of translational medicine. 2020;18(1):1–11. doi: 10.1186/s12967-020-02465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Wańkowicz P, Szylińska A, Rotter I. Evaluation of mental health factors among people with systemic lupus erythematosus during the SARS-CoV-2 pandemic. Journal of clinical medicine. 2020;9(9):2872. doi: 10.3390/jcm9092872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Dai L-L, Wang X, Jiang T-C, Li P-F, Wang Y, Wu S-J. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. Plos one. 2020;15(8) doi: 10.1371/journal.pone.0238416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Ahorsu DK, Lin C-Y, Pakpour AH. The Association Between Health Status and Insomnia, Mental Health, and Preventive Behaviors: The Mediating Role of Fear of COVID-19. Gerontology and Geriatric. Medicine. 2020;6 doi: 10.1177/2333721420966081. 2333721420966081. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.