Abstract
Background
Acute kidney injury (AKI) is one of most prevalent and serious complications of leptospirosis, a prevalent zoonotic disease in tropical countries. Prompt diagnosis of the leptospirosis-associated AKI is a challenge as there are no proper diagnostic tools that can identify patients in the early stage. Kidney injury molecule-1 (KIM-1) and monocyte chemoattractant protein-1 (MCP-1) are widely used novel AKI biomarkers that are studied in various disease conditions with AKI, but not in leptospirosis. Thus, this study is aimed at seeking the importance of KIM-1 and MCP-1 in determining the leptospirosis-associated AKI.
Methods
Leptospirosis-suspected patients who were admitted to medical wards of two selected hospitals in the Western province of Sri Lanka were recruited. Leptospirosis was confirmed by three diagnostic tests: PCR, MAT, and culture, and the status of AKI was determined by Kidney Disease Improving Global Outcomes (KDIGO) criteria.
Results
Of 170 leptospirosis-suspected patients, 79 were leptospirosis confirmed, and among them, 24.05% of patients were diagnosed to have AKI according to KDIGO criteria. Median serum KIM-1 (p < 0.0001), urine KIM-1 (0.0053), serum MCP-1 (0.0080), and urine MCP-1 (0.0019) levels in those developing AKI were significantly higher than in patients not developing AKI. The biomarker levels associated with leptospirosis AKI had AUC-ROC of 0.8565, 0.7292, 0.7024, and 0.7282 for serum KIM-1, urine KIM-1, serum MCP-1, and urine MCP-1, respectively.
Conclusion
This study revealed serum KIM-1 as a promising marker for leptospirosis-associated AKI among the tested biomarkers. Thus, further validation is recommended with a larger study group.
1. Introduction
Acute kidney injury (AKI) in leptospirosis is one of the major complications causing high morbidity and mortality among the spectra of complications associated with leptospirosis [1]. Renal involvement in leptospirosis may range from uncomplicated mild symptoms characterized by slight proteinuria and urinary sediment deviations to severe AKI requiring dialysis [2]. Leptospirosis-associated AKI is a rare incidence in developed countries; nevertheless, in tropical countries, leptospirosis is one of the most common etiologies of AKI [3]. Leptospirosis was an etiology for 13% of AKI cases in India and more than 20% in Thailand and Singapore [4, 5]. In a recent study done in the Western and Southern provinces of Sri Lanka, AKI was reported in 35.7% of patients with confirmed leptospirosis while another study done in the North Central province and Central province in Sri Lanka reported 22% and 15% of patients with confirmed leptospirosis, respectively, highlighting its wide distribution in the country [6–8]. These studies done in Sri Lanka emphasize AKI as a major complication of leptospirosis in the country. It is important to identify patients likely to develop AKI during the course of infection, in order to prevent complications and mortality.
Although pathogenesis of AKI in leptospirosis has not been fully elucidated, studies conducted with this regard suggest immune-mediated damage [9–12]. While renal impairment in leptospirosis is characterized by the presence of interstitial nephritis and tubular damage [13], direct nephrotoxic action of the Leptospira and hemodynamic alterations as well as rhabdomyolysis is also considered as contributory factors [11, 14].
Complications of leptospirosis can be prevented by prompt diagnosis of the disease, thereby starting early antibiotic treatment and proper supportive therapy. However, early diagnosis of leptospirosis and early detection of renal complications are major challenges in the management of these patients [9, 15]. Serum creatinine levels are routinely used in the identification of patients developing renal complications [16]. Many criteria assessing AKI such as the Risk, Injury, Failure, Loss, End-stage renal disease (RIFLE) as well as its modification Acute Kidney Injury Network (AKIN) and Kidney Disease Improving Global Outcomes (KDIGO) guideline have been used by groups to diagnose AKI [17–19]. These criteria rely heavily upon the level of serum creatinine [16]. However, it is widely accepted that serum creatinine levels do not rise until around 50% of kidney function is lost [20]. In Sri Lanka, serum creatinine levels are a major consideration in the diagnosis of AKI due to unavailability of more appropriate and easily available markers in the local setting.
Kidney injury molecule-1 (KIM-1) and monocyte chemoattractant protein-1 (MCP-1) are among the serum novel biomarkers with emerging roles as potential early diagnostic markers expressed in AKI [21–23]. KIM-1 is involved in epithelial cell regeneration and phagocytosis of dead cells in the tubular lumen [24]. MCP-1 is a potent chemotactic factor for monocytes and has shown promising results as an early diagnostic marker in AKI in a murine model [25]. This study describes the levels of KIM-1 and MCP-1 in leptospirosis-confirmed patients. Further, we aimed to determine the usefulness of these two novel biomarkers as a diagnostic tool to predict AKI in leptospirosis.
2. Methods
2.1. Study Design and Study Sample
This was a prospective hospital-based study conducted in a tertiary care and base hospital in the Western province of Sri Lanka between January and December 2017. Patients presenting with clinically suspected leptospirosis admitted to the medical wards were recruited for the study following informed written consent. The inclusion criteria of this study were based on “suspected case definition” given in Communicable Disease Epidemiology Profile Sri Lanka, World Health Organization [26]. Patients less than 18 years of age were excluded from the study. The study population consisted of patients with fever between days 01 and 16 on admission.
Five milliliters of blood was collected following standard procedures and aliquoted to a plain tube for serum separation and to an ethylenediaminetetraacetic acid (EDTA) tube for DNA extraction. A urine sample was collected into a sterile wide mouth container. All samples were collected on the day of admission of the patient and transported at 4°C to the laboratory. Serum was separated and aliquoted, and all specimens were stored at -80°C until further processed.
2.2. Data Collection
All data including sociodemographic profile, clinical features, and risk factors were collected using a pretested interviewer-administered questionnaire. Clinical data and basic laboratory findings (complete blood count, serum electrolytes, renal profile, and liver profile) were collected from the Bed Head Ticket (BHT) of each patient. The serum creatinine levels were determined using a fully automated biochemical analyzer following the manufacturer's instructions. The outcome and complications of each patient were recorded.
2.3. Laboratory Confirmation of Leptospirosis
Microscopic agglutination test (MAT), culture isolation, and real-time polymerase chain reaction (PCR) were used to confirm leptospirosis in patients [27–29].
2.3.1. Microscopic Agglutination Test (MAT)
MAT was carried out using a panel of 15 reference Leptospira strains at the Medical Research Institute, Sri Lanka, which is the national reference laboratory (28).
2.3.2. Real-Time PCR for Detection of Leptospira
DNA was extracted from EDTA whole blood specimens using a QIAamp DNA blood mini kit (QIAGEN GmbH, Germany) following the manufacturer's instructions. Real-time PCR (Bio-Rad CFX96™ (Bio-Rad, USA)) based on EvaGreen technology was performed to detect pathogenic Leptospira spp., using secYIVF and secYIV [27].
2.3.3. Culture of Leptospira
Leptospira was isolated from patients' blood by inoculating into semisolid EMJH medium and confirmed by Leptospira flaB PCR as previously described [29, 30].
A patient was considered as “leptospirosis confirmed” if positive by one of the above three tests while patients who were enrolled into the study due to clinical suspicion of leptospirosis but were negative for any of these tests were considered as “leptospirosis unconfirmed.” The KDIGO AKI guideline was used to classify the AKI status of patients [19].
2.4. Enzyme-Linked Immunosorbent Assay (ELISA) for Renal Markers KIM-1 and MCP-1
Both serum and urine KIM-1 (R&D, Minneapolis, USA) and MCP-1 (BioLegend, San Diego, California, USA) expression levels were measured by ELISA following the manufacturers' instructions. ELISAs were validated by intra-run precision, inter-run precision, and dilution verification. Standard curves were generated following the manufacturer's instructions. KIM-1 and MCP-1 standards were prepared by reconstitution of the standard vials in the provided diluents. Serum and urine specimens for MCP-1 ELISA were used at the original concentration while samples were diluted by half for KIM-1 ELISAs. All standards and specimens were carried out in duplicate. Mean absorbance values were calculated, and data were analyzed using GraphPad Prism version 6.05 (GraphPad Software Inc.) to determine the level of biomarkers.
2.5. Statistical Analysis
Categorical variables were expressed as proportions and compared using a two-sample proportion test. Continuous variables were expressed as mean ± standard deviation (SD) (data with normal distribution) and compared using the unpaired t-test or were expressed as median ± interquartile range (IQR) (data with skewed distribution) and compared using Mann-Whitney U test, as appropriate. Spearman's coefficient test was performed to determine the correlation between serum creatinine and biomarkers. Receiver operating characteristic (ROC) curves were generated, and the area under the curve (AUC) was calculated to assess the predictive ability of each biomarker. Data were analyzed using Statistical Package for the Social Sciences (SPSS version 20) and GraphPad Prism version 6.05. p values < 0.05 were considered as statistically significant.
3. Results
3.1. Patients' Clinical and Demographic Characteristics
One hundred and seventy clinically suspected leptospirosis patients were recruited during the study period. Leptospirosis was confirmed in 79 patients (46.47%) by a positive MAT (n = 44), PCR (n = 49), or culture (n = 2) (Figure 1). Out of the 79 confirmed patients, 69 (87.34%) were males while 10 were females. The age range of the leptospirosis-confirmed population was between 18 and 94 years with an average age of 45.05 ± 16.19 years. The median duration of fever at the time of presentation to the hospital was 6 days (IQR: 2 and range: 1-16).
Figure 1.
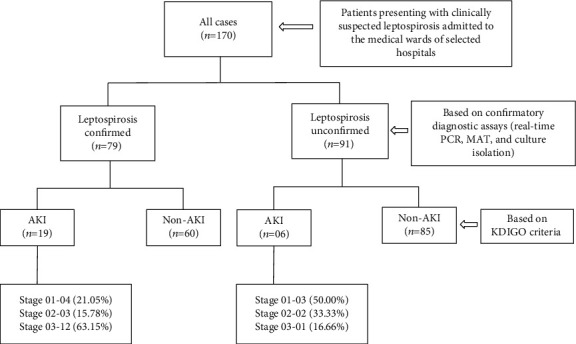
Classification of the study population.
Twenty-five patients (14.70%) were diagnosed with AKI, with 7 patients (28.00%) classified as KDIGO stage 1, 5 patients (20.00%) in KDIGO stage 2, and 13 patients (52.00%) in KDIGO stage 3. Among the leptospirosis-confirmed patients (n = 79), AKI was reported in 19 patients (24.05%), of whom 12 patients (63.15%) were classified as KDIGO stage 3. Two deaths were reported in the AKI patient population where all two were confirmed as having leptospirosis. Of the two deaths reported with AKI, both patients had KDIGO stage 3. Among the leptospirosis-unconfirmed patients (n = 91), only 6 (6.59%) developed AKI (Figure 1).
The clinical features of the leptospirosis-confirmed patient population and leptospirosis-unconfirmed patient population were compared based on the status of AKI. Among patients with confirmed leptospirosis (n = 79), fever (p = 0.0114), icterus (0.0063), anuria/oliguria (p = 0.0108), and hematuria (p = 0.0024) were found to be significantly different between patients with AKI and non-AKI. Clinical features were not found to be significantly different between AKI and non-AKI patients in the leptospirosis-unconfirmed group (Table 1).
Table 1.
Clinical features of patients based on AKI status.
| Clinical features | All cases (n = 170) | Confirmed diagnosis of leptospirosis (n = 79) | Without a confirmed diagnosis of leptospirosis (n = 91) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AKI (%) (n = 25) | Non-AKI (%) (n = 145) | p value∗ | AKI (%) (n = 19) | Non-AKI (%) (n = 60) | p value∗ | AKI (%) (n = 06) | Non-AKI (%) (n = 85) | p value∗ | |
| Fever | 92.00 | 97.93 | 0.1062 | 89.47 | 100.00 | 0.0114∗ | 100.00 | 96.47 | 0.6416 |
| Headache | 48.00 | 66.20 | 0.0817 | 52.63 | 61.66 | 0.4875 | 33.33 | 69.41 | 0.0708 |
| Myalgia | 88.00 | 80.00 | 0.3461 | 94.73 | 83.33 | 0.2139 | 66.66 | 77.64 | 0.5396 |
| Arthralgia | 48.00 | 53.10 | 0.6383 | 42.10 | 55.00 | 0.3298 | 66.66 | 51.76 | 0.4823 |
| Chills and rigors | 52.00 | 45.51 | 0.5491 | 52.63 | 35.00 | 0.1729 | 50.00 | 52.94 | 0.8897 |
| Lethargy | 28.00 | 19.31 | 0.3224 | 26.31 | 20.00 | 0.5622 | 33.33 | 18.82 | 0.3911 |
| Conjunctival suffusion | 28.00 | 17.93 | 0.2411 | 26.31 | 20.00 | 0.5622 | 33.33 | 16.47 | 0.2971 |
| Cough | 28.00 | 38.62 | 0.3113 | 26.31 | 38.33 | 0.3429 | 33.33 | 38.82 | 0.7905 |
| Dyspnea | 16.00 | 7.58 | 0.1716 | 15.78 | 8.33 | 0.3512 | 16.66 | 7.05 | 0.3956 |
| Nausea | 24.00 | 20.68 | 0.7083 | 26.31 | 23.33 | 0.7924 | 16.66 | 18.82 | 0.8962 |
| Vomiting | 56.00 | 43.44 | 0.2453 | 52.63 | 45.00 | 0.5638 | 66.66 | 42.35 | 0.2489 |
| Diarrhea | 48.00 | 37.24 | 0.3094 | 47.36 | 30.00 | 0.1671 | 50.00 | 42.35 | 0.7159 |
| Abdominal pain | 20.00 | 31.03 | 0.2650 | 21.05 | 33.33 | 0.3135 | 16.66 | 29.41 | 0.5064 |
| Icterus | 32.00 | 13.79 | 0.0238∗ | 36.84 | 10.00 | 0.0063∗ | 16.66 | 16.47 | 0.9904 |
| Anuria/oliguria | 60.00 | 30.34 | 0.0041∗ | 68.42 | 35.00 | 0.0108∗ | 33.33 | 27.05 | 0.7405 |
| Hematuria | 48.00 | 25.51 | 0.0222∗ | 63.15 | 25.00 | 0.0024∗ | 0.00 | 25.88 | 0.1547 |
∗ p < 0.05: two-sample proportion test.
The patient characteristics (age and gender) and hematological/biochemical parameters of patients based on the AKI status are compared and mentioned in Table 2. When considering leptospirosis-confirmed patients and leptospirosis-unconfirmed patients, there was no significance found with the gender and status of AKI. There was no significant difference in age between patients with AKI and those without AKI. Further, when considering the leptospirosis-confirmed patient population (n = 79), AKI patients had high WBC counts, elevated neutrophil percentage, reduced lymphocyte percentage, high BUN levels, higher SGPT value, elevated total bilirubin and direct bilirubin levels, increased CRP levels, lower platelet levels, and high K level compared to non-AKI patients. There was no significance found in levels of SGOT and hemoglobin between AKI and non-AKI of the leptospirosis-confirmed patient population. Further, Na ion levels of AKI and non-AKI patients did not show any significant difference in the two groups.
Table 2.
Patient characteristics by AKI status.
| Characteristics and hematological/biochemical parameter | All cases (n = 170) | Leptospirosis-confirmed patients (n = 79) | Leptospirosis-unconfirmed patients (n = 91) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AKI (n = 25) | Non-AKI (n = 145) | p value∗ | AKI (n = 19) | Non-AKI (n = 60) | p value∗ | AKI (n = 06) | Non-AKI (n = 85) | p value∗ | |
| Gender, male (%) | 88.00 | 91.03 | 0.6329 | 89.47 | 86.66 | 0.7498 | 83.33 | 94.11 | 0.3067 |
| Median | |||||||||
| Age (years) | 50.00 (29.50) | 43.00 (21.50) | 0.0275∗ | 50.00 (28.00) | 48.50 (22.75) | 0.1799 | 53.50 (40.75) | 42.00 (23.50) | 0.3817 |
| WBC (4‐11 × 103 mm3) | 14.20 (9.18) | 9.37 (6.09) | 0.0003∗ | 12.94 (7.07) | 9.61 (5.85) | 0.0030∗ | 16.47 (13.22) | 9.35 (6.44) | 0.0715 |
| Neutrophils (%) | 88.75 (10.28) | 80.10 (19.69) | <0.0001∗ | 89.35 (7.08) | 83.54 (20.38) | 0.0024∗ | 85.32 (9.63) | 78.92 (20.92) | 0.1087 |
| Lymphocytes (%) | 7.02 (7.52) | 11.90 (15.05) | <0.0001∗ | 4.88 (6.89) | 11.45 (15.74) | 0.0004∗ | 8.39 (5.16) | 12.89 (13.85) | 0.1874 |
| Creatinine (60-120 μmol/l) | 367.7 (313.10) | 98.00 (41.15) | <0.0001∗ | 443.40 (315.10) | 101.60 (52.20) | <0.0001∗ | 233.30 (168.42) | 94.85 (38.30) | <0.0001∗ |
| BUN (2.5-6.5 mmol/l) | 22.80 (17.73) | 7.30 (4.95) | <0.0001∗ | 26.96 (25.26) | 7.75 (6.72) | <0.0001∗ | 12.10 (11.97) | 7.22 (4.45) | 0.0495∗ |
| SGOT (10-40 U/l) | 69.00 (52.55) | 47.60 (53.80) | 0.0267∗ | 80.50 (53.80) | 59.30 (58.17) | 0.2384 | 52.40 (111.10) | 42.00 (36.75) | 0.3989 |
| SGPT (13-31 U/l) | 101.3 (119.47) | 50.75 (46.57) | 0.0092∗ | 106.90 (100.60) | 62.50 (50.65) | 0.0438∗ | 67.70 (124.00) | 47.50 (31.6) | 0.3107 |
| Na+ (136-145 mmol/l) | 133.20 (9.70) | 136.0 (6.00) | 0.4072 | 132.60 (10.9) | 135.80 (8.2) | 0.5106 | 136.50 (6.15) | 136.40 (4.90) | 0.8838 |
| Total bilirubin (5-21 μmol/l) | 35.72 (124.94) | 15.32 (25.40) | 0.0087∗ | 59.24 (176.69) | 13.33 (23.78) | 0.0063∗ | 17.30 (19.49) | 18.46 (29.77) | 0.9969 |
| Direct bilirubin (3.4 μmol/l) | 21.54 (85.83) | 7.440 (11.03) | 0.0050∗ | 34.65 (142.93) | 6.33 (9.69) | 0.0112∗ | 10.69 (7.92) | 7.80 (11.22) | 0.4573 |
| CRP (<0.5 mg/l) | 189.90 (99.90) | 131.40 (141.20) | 0.0003∗ | 189.90 (77.35) | 157.30 (155.32) | 0.0197∗ | 181.30 (153.95) | 114.90 (135.20) | 0.0737 |
| Mean | |||||||||
| Hemoglobin (14.0-17.5 g/dl) | 11.15 ± 0.42 | 12.19 ± 0.14 | 0.0098∗ | 11.10 ± 0.50 | 11.90 ± 0.25 | 0.1402 | 11.32 ± 0.82 | 12.41 ± 0.17 | 0.1107 |
| Platelet (150 − 450∗103/μl) | 79.42 ± 11.07 | 115.00 ± 5.25 | 0.0083∗ | 71.89 ± 13.75 | 106.3 ± 7.43 | 0.0277∗ | 102.0 ± 13.78 | 121.4 ± 7.24 | 0.4666 |
| K+ (3.5-5.2 mmol/l) | 4.71 ± 0.18 | 4.12 ± 0.07 | 0.0012∗ | 4.67 ± 0.17 | 4.08 ± 0.10 | 0.0040∗ | 4.80 ± 0.54 | 4.15 ± 0.10 | 0.0766 |
∗ p < 0.05: Mann-Whitney U test and unpaired t-test.
3.1.1. KIM-1 Expression
KIM-1 analysis among the patients with confirmed leptospirosis revealed a significant elevation of median serum (143.80 vs. 37.77, p < 0.0001) and urine (1497.00 vs. 463.60, p = 0.0053) KIM-1 in patients who developed AKI compared to patients without AKI. Serum KIM-1 expression was found to be 3.8-fold times higher in the leptospirosis AKI patients compared to non-AKI patients while urine KIM-1 levels showed a 3.2-fold increase. In the patients without confirmed leptospirosis, serum KIM-1 (44.94 vs. 13.71, p = 0.0233) showed a significant elevation among the six patients with AKI while urine KIM-1 (156.00 vs. 76.28, p = 0.4956) was not significantly elevated in this group (Table 3).
Table 3.
Serum and urine KIM-1 and MCP-1 concentration (ng/ml) stratified by AKI status.
| Renal biomarker [median, (IQR) (range)] | All cases (n = 170) | Leptospirosis-confirmed patients (n = 79) | Leptospirosis-unconfirmed patients (n = 91) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AKI (n = 25) | Non-AKI (n = 145) | p value∗ | AKI (n = 19) | Non-AKI (n = 60) | p value∗ | AKI (n = 06) | Non-AKI (n = 85) | p value∗ | |
| KIM-1 | |||||||||
| Serum | 115.37 (306.78) (10.75-1571.18) | 21.80 (48.89) (1.18-1161.02) | <0.0001∗ | 143.80 (283.17) (40.18-1571.18) | 37.77 (67.43) (2.51-493.48) | <0.0001∗ | 44.94 (149.83) (10.75-371.75) | 13.71 (31.47) (1.18-1161.02) | 0.0233∗ |
| Urine | 894.30 (1708.78) (21.50-3025.01) | 180.10 (922.48) (2.56-2729.61) | 0.0009∗ | 1497.00 (1771.52) (95.90-3025.01) | 463.60 (1088.34) (5.03-2713.26) | 0.0053∗ | 156.00 (617.49) (21.50-1996.05) | 76.28 (392.40) (2.56-2729.61) | 0.4956 |
| MCP-1 | |||||||||
| Serum | 257.70 (632.33) (17.72-1496.48) | 110.00 (176.44) (7.19-2508.52) | 0.0053∗ | 457.30 (676.81) (17.72-1496.48) | 120.90 (180.75) (7.19-1039.16) | 0.0080∗ | 132.60 (224.78) (67.13-367.28) | 94.09 (155.62) (7.69-2508.52) | 0.6178 |
| Urine | 399.80 (933.42) (1.07-2514.43) | 143.00 (318.93) (1.10-5017.05) | 0.0063∗ | 450.90 (912.35) (5.67-2514.43) | 133.30 (308.61) (1.19-2056.71) | 0.0019∗ | 209.50 (534.10) (1.07-734.56) | 144.60 (336.81) (1.10-5017.05) | 0.9036 |
∗ p < 0.05: Mann-Whitney U test.
When the expression of KIM-1 was compared between AKI patients with confirmed and unconfirmed leptospirosis, a significantly elevated serum (143.80 vs. 44.94, p = 0.0408) and urine (1497.00 vs. 156.00, p = 0.0092) KIM-1 expression was observed in patients in the confirmed leptospirosis group suggesting that KIM-1 expression could be useful in discriminating AKI patients with and without leptospirosis. Urine KIM-1 expression was found to be 9.6-fold times higher in the AKI patients with confirmed leptospirosis while serum KIM-1 levels showed a 3.2-fold increase. Furthermore, serum (37.77 vs. 13.71, p < 0.0001) and urine (463.60 vs. 76.28, p = 0.0002) KIM-1 levels were significantly raised in the leptospirosis-confirmed non-AKI group compared to the leptospirosis-unconfirmed non-AKI group (Figure 2).
Figure 2.
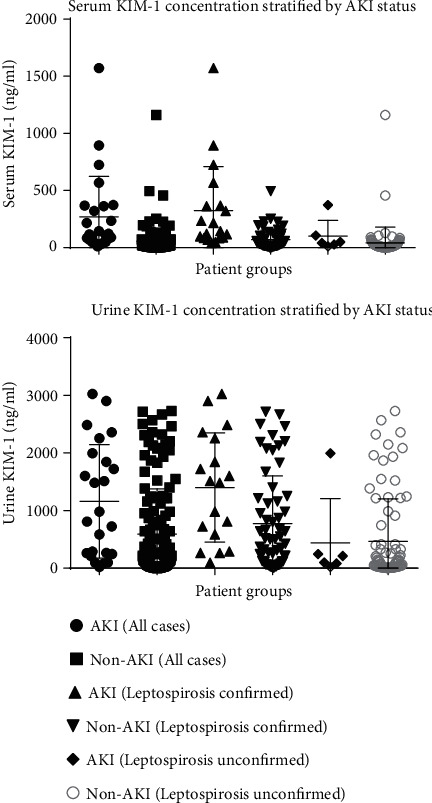
Serum and urine KIM-1 concentration stratified by AKI status.
3.1.2. MCP-1 Expression
Among patients with confirmed leptospirosis (n = 79), median serum (457.30 vs. 120.90, p = 0.0080) and urine (450.90 vs. 133.30, p = 0.0019) MCP-1 were also significantly higher in patients with AKI, whereas among leptospirosis-unconfirmed patients, the findings were not significant between the two groups in the serum (132.60 vs. 94.09, p = 0.6178) and urine (209.50 vs. 144.60, p = 0.9036) (Table 3). In terms of fold difference, serum MCP-1 showed 3.8 while urine MCP-1 showed 3.4 among leptospirosis AKI patients compared to non-AKI patients.
Further, serum (457.30 vs. 132.60, p = 0.1004) and urine (450.90 vs. 209.50, p = 0.1665) MCP-1 levels between leptospirosis-confirmed AKI and leptospirosis-unconfirmed AKI were not significantly different between the two groups. There was no significant elevation in serum (120.90 vs. 94.09, p = 0.1869) and urine (133.30 vs. 144.60, p = 0.7746) MCP-1 between leptospirosis-confirmed non-AKI and leptospirosis-unconfirmed non-AKI patients (Figure 3).
Figure 3.
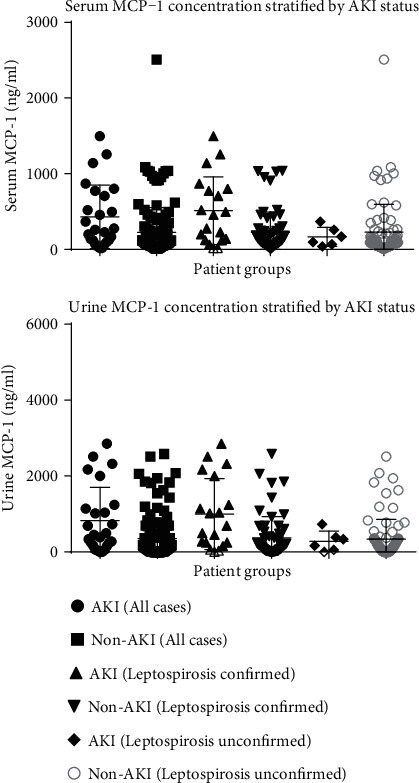
Serum and urine MCP-1 concentration stratified by AKI status.
3.2. Biomarkers for Diagnosis of AKI
To seek any correlation between serum creatinine and serum/urine KIM-1 and MCP-1 among leptospirosis-confirmed patients, Spearman's coefficient test was performed. The results of Spearman's coefficient test showed that levels of serum creatinine were significantly correlated with both serum (p < 0.000) and urine KIM-1 (p < 0.000) while serum (p = 0.002) and urine MCP-1 (p < 0.000) were also significantly elevated. The correlation coefficient (ρ) of serum and urine KIM-1 and MCP-1 was 0.594, 0.443, 0.359, and 0.401, respectively, suggesting a moderate positive correlation. The correlation between serum biomarkers and serum creatinine is shown in Figure 4.
Figure 4.
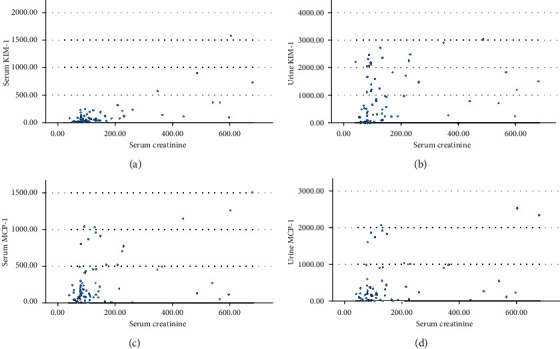
Scatter plots of (a) serum creatinine vs. serum KIM-1, (b) urine KIM-1, (c) serum MCP-1, and (d) urine MCP-1 among leptospirosis-confirmed patients.
For diagnosis of AKI in leptospirosis-confirmed patients, the area under the ROC curve (AUC) for serum and urine KIM-1 was 0.8565 (95% CI 0.7689-0.9440) and 0.7292 (95% CI 0.6030-0.8554), respectively. The AUC-ROC for serum and urine MCP-1 in leptospirosis-confirmed patients gave 0.7024 (95% CI 0.5498-0.8550) and 0.7282 (95% CI 0.5925-0.8640), respectively (Figure 5). The AUC-ROC for KIM-1 and MCP-1 for the leptospirosis-unconfirmed group had values less than 0.5.
Figure 5.
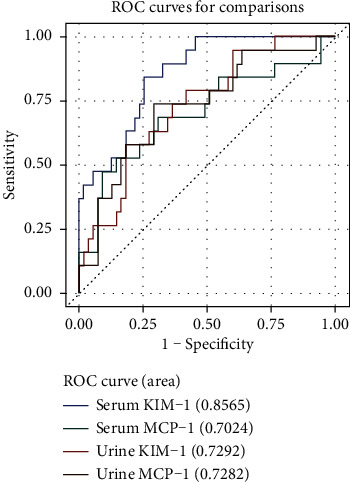
ROC curves for serum and urine KIM-1 and MCP-1 in leptospirosis-confirmed patients.
When the performed ROC DeLong AUC comparison analysis equated to serum KIM-1, there was a significant difference found between serum and urine KIM-1 (p = 0.0435) whereas no significant difference was found between serum KIM-1, serum MCP-1 (p = 0.0826), and urine MCP-1 (p = 0.0884).
For diagnosis of AKI, the cutoff values were determined by selecting the maximum point which gives high sensitivity and specificity. The cutoff for diagnosis of AKI among the leptospirosis-confirmed group was 82.45 ng/ml for serum KIM-1, 700.89 ng/ml for urine KIM-1, 196.48 ng/ml for serum MCP-1, and 243.58 ng/ml for urine MCP-1 (Table 4). The positive predictive value (PPV) and the negative predictive value (NPV) for each marker are mentioned in Table 4.
Table 4.
Renal biomarker concentration at the best cutoff values for AKI diagnosis.
| Biomarkers | Cutoff (ng/ml) | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| Serum KIM-1 | 82.45 | 0.789 | 0.750 | 0.894 | 0.633 |
| Urine KIM-1 | 700.89 | 0.722 | 0.633 | 0.736 | 0.466 |
| Serum MCP-1 | 196.48 | 0.684 | 0.695 | 0.684 | 0.566 |
| Urine MCP-1 | 243.58 | 0.737 | 0.729 | 0.736 | 0.733 |
In the leptospirosis-confirmed patients, serum KIM-1 had the highest odds ratio (26.667) and could strongly predict AKI compared to serum MCP-1, urine MCP-1, and urine KIM-1. High WBC count (6.861) was also found to be significantly associated with AKI among the leptospirosis-confirmed patient population (Table 5).
Table 5.
Association between biomarker/clinical findings and AKI.
| Biomarkers/clinical findings | Odds ratio (95% CI) unadjusted | p value |
|---|---|---|
| Serum KIM-1 | 26.667 (3.293-215.914) | 0.002∗ |
| Urine KIM-1 | 3.500 (0.903-13.563) | 0.070 |
| Serum MCP-1 | 2.400 (0.747-7.713) | 0.142 |
| Urine MCP-1 | 5.506 (1.677-18.074) | 0.005∗ |
| WBC | 6.861 (1.960-24.023) | 0.003∗ |
| Platelet | 2.500 (0.507-12.316) | 0.260 |
4. Discussion
AKI in leptospirosis is a major complication reported in Sri Lanka [6, 8, 31]. Diagnosis of AKI in the local setting is based on serum creatinine alone. The disadvantage of AKI diagnosis based on serum creatinine is that it is elevated when 50% of renal function is compromised. Further, several other factors may influence expression of serum creatinine such as volume overload and rhabdomyolysis. Identification of reliable diagnostic biomarkers in the early detection of leptospirosis-associated AKI can considerably contribute to the initiation of early management of these patients and reduce associated morbidity and mortality [5].
Few studies attempt to investigate the value of biomarkers such as syndecan-1, intercellular adhesion molecule-1, neutrophil gelatinase-associated lipocalin, and defensinα1 in leptospirosis-associated AKI [5, 32, 33]. Among the novel biomarkers of renal injury, KIM-1 and MCP-1 have been suggested to be useful in the identification of AKI [22, 23]. However, the value of KIM-1 and MCP-1 in the diagnosis of AKI due to leptospirosis has not been addressed.
In this study, we found that both serum and urine KIM-1 and MCP-1 concentrations were significantly higher in patients with confirmed leptospirosis, who developed AKI compared to patients without AKI. Human KIM-1 is not measureable in healthy individuals, but is present at very high concentrations in damaged proximal tubule epithelial cells after renal injury [24]. Several studies found that KIM-1 is useful as a biomarker for the diagnosis of kidney injury [34–36]. MCP-1 has been reported to be elevated following ischemia-induced AKI [23]. A comparative study conducted on murine model-induced intrarenal injury has shown a significant increase of both MCP-1 protein and its corresponding mRNA in contrast to other novel markers such as NGAL [25, 37].
When KIM-1 and MCP-1 expression was compared between leptospirosis-confirmed and leptospirosis-unconfirmed groups, serum and urine KIM-1 levels were found to be elevated among both leptospirosis-confirmed AKI and non-AKI patients compared to the leptospirosis-unconfirmed patient population. Investigation of serum and urine MCP-1 did not show a significant difference between the leptospirosis-confirmed and leptospirosis-unconfirmed patients with AKI and without AKI. During infection, Leptospira enters the body and spreads into renal tissue via the hematogenous route. Within the kidney, organisms enter into peritubular capillaries, move to the interstitium and renal tubules, and finally persist in the proximal tubular lumen [32]. Damage to the proximal tubular cells results in release of KIM-1 in leptospirosis patients which explains the significantly elevated KIM-1 levels compared to MCP-1. Thus, in leptospirosis-associated AKI, KIM-1 may have more discriminatory value compared to MCP-1.
In this study, most patients presented to the hospital on the sixth day of fever. Presenting on days 5–6 is a common practice in the Sri Lankan setting. The elevated serum KIM-1 on admission was observed in patients with AKI irrespective of the day of presentation. This suggests its usefulness in identifying renal injury at any time point of the illness in this patient group. In this study, it was not possible to gather sequential data on the pattern of KIM-1 expression with time. It was not possible to collect sequential samples to evaluate the dynamics of biomarker expression over time. This is due to early discharge of patients from hospitals in the local setting where a high number of patients present for treatment. Among the patients with a confirmed diagnosis of leptospirosis who developed AKI, the ability to detect KIM-1 was observed on day 3 of fever on admission while the highest KIM-1 expression was detected on day 9 of fever on admission. Therefore, KIM-1 can be suggested to be a suitable diagnostic marker in the local setting due to its ability to predict AKI at the time of admission.
In leptospirosis cases, based on cutoff values for each biomarker (KIM-1 and MCP-1), the highest sensitivity and specificity were reported for serum KIM-1. When comparing both urine and serum specimens, KIM-1 had higher sensitivity and specificity than MCP-1. In the presence of renal assault, KIM-1 is highly upregulated in proximal tubular cells of the kidney whereas MCP-1 is produced by many cell types as a result of inflammation [34, 38]. Thus, as a biomarker in leptospirosis-mediated renal injury, KIM-1 appears to be more specific than MCP-1.
Serum KIM-1 was found to have higher diagnostic sensitivity than urine KIM-1 in these patients. The shedding of the ectodomain of KIM-1 into the tubular lumen is marked by the high concentration of KIM-1 in urine following kidney injury. Further, KIM-1 may enter the blood through several mechanisms. Research suggests that KIM-1 may be released straight into the interstitium as a result of the absence of tubular cell polarity. Further, the elevated transepithelial permeability as a result of tubular injury leads to leakage of tubular contents into the circulation. Interrupted integrity of renal microvascular endothelial cells also facilitates the KIM-1 movement into the circulation. Therefore, these studies suggest that elevated levels of KIM-1 can be detected in the blood in addition to urine and may serve as a biomarker of kidney injury. Further use of serum is useful in complications like anuria where urine samples are totally unavailable for diagnosis.
Leukocytosis is a known risk factor for AKI in leptospirosis, and in our study, leukocytosis was an independent risk factor for AKI among leptospirosis patients. Similar findings were observed by other studies where they demonstrated an independent association between leukocytosis and AKI [5, 39]. Thrombocytopenia is another known risk factor for AKI in leptospirosis that has been mentioned in several studies; however, this association was not observed in our study even though there was a significant reduction of platelet counts among leptospirosis-associated AKI [40].
Limitations of the data from this study should be recognized. In the current study, patients presented to the hospital at a median of 6 days, which did not enable the collection of early samples from the patients. In order to determine the early diagnostic utility of these biomarkers, future studies should focus on collecting specimens at the primary care level or outpatient departments to include collection of early specimens. During the study, it was not possible to collect paired serum samples from the majority of the patients. This is due to patients' recovery and discharging from the hospital prior to convalescent sample collection and not reporting to follow-up clinics after discharge. As this is a general problem when collecting paired serum, this study was limited to interpretation of MAT by using a single sample of serum. Although initially it was planned to collect sequential samples to detect KIM-1 and MCP-1 expression, there were many practical difficulties doing this. Determination of novel biomarker expression over time has given valuable data; however, it was not possible to achieve this in this study due to late presentation, delayed diagnosis, and early discharge of patients from hospitals in the local setting where a high number of patients present for treatment.
5. Conclusions
This study revealed that both KIM-1 and MCP-1 were elevated in leptospirosis-associated AKI and highlighted the usefulness of serum KIM-1 as a potential biomarker for detection of AKI in leptospirosis patients. The early diagnostic utility of serum KIM-1 should be investigated in future studies.
Acknowledgments
This work was supported by the grants awarded by the University of Sri Jayewardenepura, Sri Lanka (ASP/01/RE/MED/2015/37, ASP/01/RE/MED/2016/48, and ASP/01/RE/MED/2017/29). We wish to acknowledge all patients, staff of relevant hospitals, and the Department of Microbiology, Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka.
Abbreviations
- AKI:
Acute kidney injury
- KIM-1:
Kidney injury molecule-1
- MCP-1:
Monocyte chemoattractant protein-1
- KDIGO:
Kidney Disease Improving Global Outcomes
- PCR:
Polymerase chain reaction
- MAT:
Microscopic agglutination test
- RIFLE:
Risk, Injury, Failure, Loss, End-stage renal disease
- AKIN:
Acute Kidney Injury Network
- EDTA:
Ethylenediaminetetraacetic acid
- BHT:
Bed Head Ticket
- ELISA:
Enzyme-linked immunosorbent assay
- IQR:
Interquartile range
- ROC:
Receiver operating characteristic
- AUC:
Area under the curve
- SPSS:
Statistical Package for the Social Sciences
- BUN:
Blood urea nitrogen
- SGOT:
Serum glutamic oxaloacetic transaminase
- SGPT:
Serum glutamic pyruvic transaminase
- CRP:
C-reactive protein
- WBC:
White blood cells
- CI:
Confidence interval
- PPV:
Positive predictive value
- NPV:
Negative predictive value.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
Ethical approval for the study was obtained from the Ethics Review Committee of the University of Sri Jayewardenepura (no. 02/17) and the respective Ethics Review committees of the hospitals.
Conflicts of Interest
The authors declare that they have no conflicts of interests.
Authors' Contributions
TN was involved in sample and data collection, laboratory work, data analysis and interpretation, and writing the manuscript. MW designed the study and was involved in proposal writing, data analysis, and writing the manuscript. NR and CM selected and recruited the patients for the study and were involved in drafting the article. CDG was involved in laboratory diagnosis and writing the manuscript. NF was involved in proposal writing, research question, data analysis, and writing the manuscript. CG was involved in proposal writing, designing the study, research question, data analysis, and writing the manuscript. All authors read and approved the final manuscript.
References
- 1.Al Hariri Y. K., Sulaiman S. A., Khan A. H., Adnan A. S., Al Ebrahem S. Q. Mortality of leptospirosis associated acute kidney injury (LAKI) & predictors for its development in adults: a systematic review. Journal of infection and public health. 2019;12(6):751–759. doi: 10.1016/j.jiph.2019.06.014. [DOI] [PubMed] [Google Scholar]
- 2.Seguro A. C., Andrade L. Pathophysiology of leptospirosis. Shock. 2013;39(Supplement 1):17–23. doi: 10.1097/SHK.0b013e31828fae49. [DOI] [PubMed] [Google Scholar]
- 3.Yaslianifard S., Hoseini M., Alimorad S. Renal failure due to human leptospirosis; an overview. Nephro-Urology Monthly. 2018;10(3) doi: 10.5812/numonthly.66503. [DOI] [Google Scholar]
- 4.Mehta K., Pajai A., Bhurke S., Shirkande A., Bhadade R., D'Souza R. Acute kidney injury of infectious etiology in monsoon season: a prospective study using acute kidney injury network criteria. Indian journal of nephrology. 2018;28(2):143–152. doi: 10.4103/ijn.IJN_355_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srisawat N., Praditpornsilpa K., Patarakul K., et al. Neutrophil gelatinase associated lipocalin (NGAL) in leptospirosis acute kidney injury: a multicenter study in Thailand. PLoS One. 2015;10(12, article e0143367) doi: 10.1371/journal.pone.0143367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bandara K. K., Weerasekera M., Gunasekara C. P., Ranasinghe N., Marasinghe C., Fernando N. Molecular characterisation and disease severity of leptospirosis in Sri Lanka. Memórias do Instituto Oswaldo Cruz. 2015;110(4):485–491. doi: 10.1590/0074-02760150070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agampodi S. B., Peacock S. J., Thevanesam V., et al. Leptospirosis outbreak in Sri Lanka in 2008: lessons for assessing the global burden of disease. The American journal of tropical medicine and hygiene. 2011;85(3):471–478. doi: 10.4269/ajtmh.2011.11-0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agampodi S. B., Dahanayaka N. J., Bandaranayaka A. K., et al. Regional differences of leptospirosis in Sri Lanka: observations from a flood-associated outbreak in 2011. PLoS neglected tropical diseases. 2014;8(1, article e2626) doi: 10.1371/journal.pntd.0002626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang C.-W. Leptospirosis renal disease: understanding the initiation by Toll-like receptors. Kidney international. 2007;72(8):918–925. doi: 10.1038/sj.ki.5002393. [DOI] [PubMed] [Google Scholar]
- 10.Cerqueira T. B., Athanazio D. A., Spichler A. S., Seguro A. C. Renal involvement in leptospirosis: new insights into pathophysiology and treatment. Brazilian Journal of Infectious Diseases. 2008;12(3):248–252. doi: 10.1590/S1413-86702008000300016. [DOI] [PubMed] [Google Scholar]
- 11.Daher E. D. F., KLSD A., GBDS J. Leptospirosis-associated acute kidney injury. Brazilian Journal of Nephrology. 2010;32(4):408–415. doi: 10.1590/S0101-28002010000400010. [DOI] [PubMed] [Google Scholar]
- 12.Visith S., Kearkiat P. Nephropathy in leptospirosis. Journal of postgraduate medicine. 2005;51(3):184–188. [PubMed] [Google Scholar]
- 13.Slocum J. L., Heung M., Pennathur S. Marking renal injury: can we move beyond serum creatinine? Translational Research. 2012;159(4):277–289. doi: 10.1016/j.trsl.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdulkader R. C., Silva M. V. The kidney in leptospirosis. Pediatric Nephrology. 2008;23(12):2111–2120. doi: 10.1007/s00467-008-0811-4. [DOI] [PubMed] [Google Scholar]
- 15.Goarant C. Leptospirosis: risk factors and management challenges in developing countries. Research and reports in tropical medicine. 2016;Volume 7:49–62. doi: 10.2147/RRTM.S102543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ostermann M., Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup. Critical Care. 2016;20(1):p. 299. doi: 10.1186/s13054-016-1478-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta R. L., Kellum J. A., Shah S. V., et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Critical care. 2007;11(2):p. R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bellomo R., Ronco C., Kellum J. A., Mehta R. L., Palevsky P. Acute renal failure–definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) group. Critical care. 2004;8(4):R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clinical Practice. 2012;120(4):c179–c184. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 20.Mårtensson J., Martling C.-R., Bell M. Novel biomarkers of acute kidney injury and failure: clinical applicability. British journal of anaesthesia. 2012;109(6):843–850. doi: 10.1093/bja/aes357. [DOI] [PubMed] [Google Scholar]
- 21.Han W. K., Bailly V., Abichandani R., Thadhani R., Bonventre J. V. Kidney injury molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney international. 2002;62(1):237–244. doi: 10.1046/j.1523-1755.2002.00433.x. [DOI] [PubMed] [Google Scholar]
- 22.Vaidya V. S., Ferguson M. A., Bonventre J. V. Biomarkers of acute kidney injury. Annual Review of Pharmacology and Toxicology. 2008;48(1):463–493. doi: 10.1146/annurev.pharmtox.48.113006.094615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deshmane S. L., Kremlev S., Amini S., Sawaya B. E. Monocyte chemoattractant protein-1 (MCP-1): an overview. Journal of interferon & cytokine research. 2009;29(6):313–326. doi: 10.1089/jir.2008.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bonventre J. V. Kidney injury molecule-1 (KIM-1): a urinary biomarker and much more. Oxford University Press; 2009. [DOI] [PubMed] [Google Scholar]
- 25.Munshi R., Johnson A., Siew E. D., et al. MCP-1 gene activation marks acute kidney injury. Journal of the American Society of Nephrology. 2011;22(1):165–175. doi: 10.1681/ASN.2010060641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Organization WH. Communicable Disease Epidemiological Profile. 2010.
- 27.Ahmed A., Engelberts M. F., Boer K. R., Ahmed N., Hartskeerl R. A. Development and validation of a real-time PCR for detection of pathogenic Leptospira species in clinical materials. PLoS One. 2009;4(9) doi: 10.1371/journal.pone.0007093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Herath N., Uluwattage W., Weliwitiya T., et al. Sequel and therapeutic modalities of leptospirosis associated severe pulmonary haemorrhagic syndrome (SPHS); a Sri Lankan experience. BMC infectious diseases. 2019;19(1):p. 451. doi: 10.1186/s12879-019-4094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nisansala G., Muthusinghe D., Gunasekara T., et al. Isolation and characterization of Leptospira interrogans from two patients with leptospirosis in Western Province, Sri Lanka. Journal of medical microbiology. 2018;67(9):1249–1252. doi: 10.1099/jmm.0.000800. [DOI] [PubMed] [Google Scholar]
- 30.Koizumi N., Muto M., Yamamoto S., et al. Investigation of reservoir animals of Leptospira in the northern part of Miyazaki prefecture. Japanese Journal of Infectious Diseases. 2008;61(6):465–468. [PubMed] [Google Scholar]
- 31.Herath N. J., Kularatne S. A., Weerakoon K. G., Wazil A., Subasinghe N., Ratnatunga N. V. Long term outcome of acute kidney injury due to leptospirosis? A longitudinal study in Sri Lanka. BMC research notes. 2014;7(1):p. 398. doi: 10.1186/1756-0500-7-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Libório A. B., Braz M. B. M., Seguro A. C., et al. Endothelial glycocalyx damage is associated with leptospirosis acute kidney injury. The American journal of tropical medicine and hygiene. 2015;92(3):611–616. doi: 10.4269/ajtmh.14-0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chagan-Yasutan H., Chen Y., Lacuesta T. L., et al. Urine levels of defensin α1 reflect kidney injury in leptospirosis patients. International journal of molecular sciences. 2016;17(10):p. 1637. doi: 10.3390/ijms17101637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khreba N. A., Abdelsalam M., Wahab A., et al. Kidney injury molecule 1 (KIM-1) as an early predictor for acute kidney injury in post-cardiopulmonary bypass (CPB) in open heart surgery patients. International journal of nephrology. 2019;2019:6. doi: 10.1155/2019/6265307.6265307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sun I. O., Shin S. H., Cho A. Y., Yoon H. J., Chang M. Y., Lee K. Y. Clinical significance of NGAL and KIM-1 for acute kidney injury in patients with scrub typhus. PloS one. 2017;12(4) doi: 10.1371/journal.pone.0175890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lei L., Li L. P., Zeng Z., et al. Value of urinary KIM-1 and NGAL combined with serum Cys C for predicting acute kidney injury secondary to decompensated cirrhosis. Scientific Reports. 2018;8(1):1–9. doi: 10.1038/s41598-018-26226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Urbschat A., Obermüller N., Haferkamp A. Biomarkers of kidney injury. Biomarkers. 2011;16(supplement 1):S22–S30. doi: 10.3109/1354750X.2011.587129. [DOI] [PubMed] [Google Scholar]
- 38.Brown Z., Strieter R. M., Neild G. H., Thompson R. C., Kunkel S. L., Westwick J. IL-1 receptor antagonist inhibits monocyte chemotactic peptide 1 generation by human mesangial cells. Kidney international. 1992;42(1):95–101. doi: 10.1038/ki.1992.266. [DOI] [PubMed] [Google Scholar]
- 39.Teles F., de Mendonça Uchôa J. V., Mendonça D. M. B., Costa A. F. P. Acute kidney injury in leptospirosis: the Kidney Disease Improving Global Outcomes (KDIGO) criteria and mortality. Clinical nephrology. 2016;86(12):303–309. doi: 10.5414/CN108865. [DOI] [PubMed] [Google Scholar]
- 40.Daher E. F., Silva G. B., Silveira C. O., et al. Factors associated with thrombocytopenia in severe leptospirosis (Weil's disease) Clinics. 2014;69(2):106–110. doi: 10.6061/clinics/2014(02)06. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


