Abstract
Background:
As adolescent girls and young women (AGYW) transition to adulthood, their interaction with their social context becomes a critical consideration for HIV prevention interventions. Few studies have examined what types of community groups and community spaces might be protective for AGYW HIV acquisition and related sexual behaviors.
Methods:
Data are from HIV Prevention Trials Network (HPTN) 068, a longitudinal study of AGYW (age 13–20) in rural South Africa. Survival analyses and generalized estimating equations were used to assess whether community group membership and time spent in community spaces were associated with HIV incidence and sexual behaviors (unprotected sex, transactional sex, and having an older partner).
Results:
A total of 2,245 AGYW were followed for up to four years. Membership in church groups (adjusted hazard ratio (aHR): 0.75, 95% CI: 0.53, 0.91), dance groups (aHR: 0.89, 95% CI; 0.80, 0.98), and spending time at church (aHR: 0.88, 95% CI: 0.79, 0.98) was protective for HIV infection. Conversely, spending time at taverns was associated with higher HIV incidence (aHR: 1.27, 95% CI: 1.15, 1.41). Membership in church groups and spending time at a family member’s home and at church was protective for all three sexual behaviors. Spending time at a boyfriend’s home and taverns was risky for all three sexual behaviors.
Conclusion:
Results suggest that community spaces and community groups that include an element of adult supervision are potentially protective, while spaces and groups that provide an opportunity for AGYW to interact unsupervised with boyfriends or meet new partners are potentially risky.
Keywords: adolescents, HIV incidence, sexual behaviors, social context
INTRODUCTION
Despite significant declines in new HIV infections over the last few decades, adolescent girls and young women (AGYW) (age 15–24) in sub-Saharan Africa (SSA) continue to bear a disproportionate burden of the HIV epidemic.1 This is particularly the case in rural South Africa, where HIV prevalence among AGYW is 16% and AGYW are three times more likely to acquire HIV than their age-matched male counterparts.2,3 The age and gender gap can be largely attributed to the biological, social, and structural factors that increase AGYW’s vulnerability to acquiring HIV through sexual transmission.4–7
Building on the premise that HIV risk differs between males and females, HIV prevention programs for young people have often employed gender-specific approaches.8–10 One such approach is the construction and maintenance of “safe spaces”. Safe spaces are typically gender specific support groups where adolescents and young adults can feel safe, respected, and comfortable speaking amongst peers. Through these groups, individuals work with mentors to develop skills, resources, and strong social networks that can aid in decision making and future life transitions.11–14 Safe space approaches are motivated by the well-established benefits of supportive social networks for adolescent health and wellbeing.15,16 In many countries, females, as well as LGBTQ individuals, are less likely than their male and heterosexual counterparts to have protective social connections.5,17–19 Taken together, safe space approaches are beneficial for AGYW HIV prevention because they potentially reduce social isolation, build positive social relationships, and encourage healthy behaviors.
Currently, safe space approaches create mentor-based, support groups which meet at mutually agreed upon community spaces such as halls, schools, youth centers, and even empty shipping containers.12,13,20 AGYW who participated in safe space programs were more likely to receive an HIV test, discuss HIV and STI topics with their partners, use family planning, and report having increased financial literacy as well as supportive social relationships.13,21,22 Few studies however, have examined what types of other community groups and community spaces might be similarly protective for AGYW HIV acquisition and related risky sexual behaviors. Current studies have largely focused on school as a safe space that occupies AGYW’s time and provides a connection to caring peers and adults, such that AGYW have fewer older partners, fewer partners overall and safer sexual behavior.23,24 Identifying similar types of naturally existing protective community spaces and groups has to the potential to provide leverage points for future HIV prevention interventions.
Little is also known about where AGYW spend their time, and the groups they belong to, after they graduate or leave school. Social Control Theory and the Social Development Model suggest that AGYW who are disconnected from prosocial contexts, such as school, might be particularly vulnerable as they are navigating the risks of young adulthood without consistent social connections, such as ones provided through an educational institution.25,26 Examining how group membership and engagement with community spaces changes after AGYW leave school provides an opportunity to understand the role of social environments for health during important life transitions.
Our analyses utilize data from a longitudinal conditional cash transfer study of AGYW in rural South Africa to examine three specific research aims. First, we document what types of community groups AGYW belong to and where they spend their time, outside of school and home. Second, we investigate the association among community group membership and time spent at community spaces with HIV incidence as well as related risky sexual behaviors. Third, we assess whether community group membership and time spent at community spaces differs between AGYW in school and AGYW out of school.
METHODS
HPTN 068 Overview and Setting
Data are from the HIV Prevention Trials Network (HPTN) 068 study (HPTN 068), a phase III randomized controlled trial to determine whether providing cash transfers, conditional on school attendance, reduced the risk of HIV acquisition among AGYW, age 13–20 years old. The parent study was conducted across 28 villages within the Medical Research Council/Wits Rural Public Health and Health Transition Research Unit (Agincourt) in rural Mpumalanga Province, South Africa. The study area is characterized by high levels of unemployment, poverty, migration for work, and HIV prevalence.27
HPTN 068 Data Collection and Ethics Approval
HPTN 068 enrolled 2533 AGYW in grades 8–12 who were not pregnant or married at the time of recruitment, able to read, enrolled in school, intending to reside in the study area until study completion, and had the necessary documentation to open a bank account. Enrolled AGYW were seen annually from baseline until one-year post study completion or graduation from high school, resulting in up to five assessments for each participant between 2011 and 2017. Each annual study visit included a behavioral questionnaire, administered through an audio computer-assisted self-interview, and HIV testing for those who were negative at the previous visit. Additional details on recruitment, data collection, and laboratory procedures are available in the parent publication of the trial.28,29 The parent study included five potential study visits: baseline and follow-up visits one to four. Our analytical sample did not include baseline data as our variables of interest were not captured at that time point. In total, our analytical sample included data from follow-up visits one through four. Furthermore, we only included participants who were HIV-negative at follow up visit one in our cohort (N=2245).
Institutional Review Board approval for this study was obtained from the University of North Carolina at Chapel Hill and the University of the Witwatersrand Human Research Ethics Committee. Each AGYW and her parent or guardian provided written informed consent at the home visit. Written assent was obtained for young women younger than 18 years. Consent and assent forms were available in English and Shangaan.
Measures
Our analysis included four time-varying outcome variables: HIV incidence, unprotected sex, transactional sex, and having an older male partner.
HIV incidence was determined using two HIV rapid tests performed in parallel followed by a confirmatory test, if one or both rapid results were HIV positive. We created a binary variable indicating whether the participant had experienced a new HIV infection for each study visit.
Unprotected sex in the previous three months was binary and defined at each visit as having reported any instance of condomless sex in the previous three months for each study visit.
Transactional sex in the previous three months was binary and defined as reporting feeling obligated to have sex with any of partners because they were given money or gifts in the previous three months.
Older partner was a binary indicator defined as whether the participant reported having had at least one sexual or nonsexual partner >5 years older for each study visit. Partners with whom there was no reported sexual relationship were included to account for potential misreporting about sexual behaviors.
Our analysis included two groups of time-varying exposures: membership in community groups and time spent in spaces outside of home and school.
Group membership was determined from a set of items on the behavioral questionnaire assessing whether the participants reported membership in any of the following community groups, which were not affiliated with school: church, health, HIV/AIDS, dance, sport, and finance/loan. We created separate binary variables indicating if the participant reported membership in any of the six groups for each study visit.
Time spent was determined from an item on the behavioral survey assessing the top three spaces that participants spent time outside of school and home from the following list: friend’s house, family member’s house, church, neighbor’s house, stokvel (savings and credit group), boyfriend’s house, work, shops, outside the community, and shebeen (tavern). We created separate binary variables indicating participant reported any time spent at each of the ten spaces for each study visit.
Data Analysis
First, we described participant characteristics, exposures, and outcomes at visit one and visit four. Second, we used separate Cox proportional hazard regression models to estimate adjusted hazard ratios (aHRs) for the relationship between community group membership, time spent in community spaces, and HIV infection. Third, we used separate log-binomial regression models to estimate adjusted prevalence ratios (aPRs) for the association between community group membership, time spent in community spaces, and sexual behaviors. We fit GEE models to account for the non-independent repeated measures from the same participant using an exchangeable correlation structure for the working correlation matrix. In our sexual behavior models, group membership and time spent exposures were lagged by one time point; the exposure was from the previous time point and the outcome was the sexual behavior in the past three months measured at the current time point. All models were adjusted for age, orphan status, HPTN 068 study intervention arm assignment, study visit number, current grade in school, and quartiles of per-capita household consumption. These variables were selected a priori and have been shown to be associated with incident HIV infection and HIV related sexual behaviors among adolescents in South Africa.4 All analyses were conducted using StataSE, version 14.2 (College Station, TX).
RESULTS
Population Characteristics, Group Membership, and Time Spent at Visit One (Table 1)
Table 1.
Participant Characteristics, Exposures, and Outcomes at Visit 1 and Visit 4*
| Visit 1 (N = 2245) | Visit 4 (N = 1931) | |||
|---|---|---|---|---|
| N or Median | (% or IQR) | N or Median | (% or IQR) | |
| Demographics | ||||
| Age | 16 | (15, 18) | 20 | (19, 21) |
| Enrolled in High School | 2234 | 99% | 377 | 20% |
| Any Orphanhood | 713 | 32% | 687 | 34% |
| Household Monthly Per Capita Expenditure (Rand) | 296 | (191, 473) | 310 | (202, 567) |
| CCT Intervention Arm | 1208 | 54% | 993 | 49% |
| Sexual Behaviors and HIV Infection | ||||
| Ever Had Sex | 740 | 33% | 1229 | 61% |
| Any Sex in Past 3 Months | 636 | 28% | 1114 | 55% |
| Unprotected Sex in Past 3 Months | 188 | 8% | 409 | 20% |
| Transactional Sex in Past 3 Months | 190 | 8% | 339 | 17% |
| Older Partner > 5 Years | 146 | 6% | 425 | 21% |
| HIV Infection | 0 | 0% | 174 | 9% |
| Group Membership | ||||
| Church/Religious | 1,077 | 48% | 863 | 43% |
| Health | 715 | 32% | 488 | 24% |
| HIV/AIDs | 414 | 18% | 276 | 14% |
| Dance | 364 | 16% | 203 | 10% |
| Sport | 220 | 10% | 80 | 4% |
| Finance/Loan | 102 | 5% | 51 | 3% |
| ≥ 2 Groups | 780 | 34% | 373 | 18% |
| Time Spent | ||||
| Friend’s House | 1,597 | 71% | 1,151 | 57% |
| Family Member’s House | 1222 | 54% | 731 | 36% |
| Church | 1218 | 54% | 984 | 49% |
| Neighbor’s House | 681 | 30% | 291 | 14% |
| Stokvel | 666 | 30% | 491 | 24% |
| Boyfriend’s House | 379 | 17% | 501 | 25% |
| Work | 282 | 13% | 171 | 8% |
| Shops | 259 | 12% | 258 | 13% |
| Outside the Community | 139 | 6% | 67 | 3% |
| Shebeen (Local Tavern) | 119 | 5% | 44 | 2% |
Totals do not sum to 100% due to missing data
A total of 2247 AGYW, who were HIV negative at visit one, were included in our cohort sample. Median age at visit one was 16 years (interquartile range 15–18 years). The majority of participants were in enrolled in school (99%), 32% reported being orphans, and 33% reported ever having had sex.
Almost all participants reported belonging to at least one type of social group at visit one (99%). Church groups had the highest proportion of membership (48%) followed by health groups (32%), HIV/AIDs groups (18%), dance groups (16%), sports groups (10%), and finance or loan groups (5%). Among these six groups, the proportion of participants reporting ever having had sex, versus not having had sex, differed by church group membership (36% vs. 54%, p < 0.001) and dance group membership (13% vs. 18%, p = 0.003).
The majority of participants reported friend’s homes (71%), family member’s homes (54%), and church (54%) among the top three places they spent time outside of school and home at visit one. Where participants reported spending their time differed by sexual history. A higher proportion of participants who reported ever having had sex spent time at friend’s homes (72% vs. 71%), stokvels (34% vs. 28%), boyfriend’s homes (27% vs. 12%), and shebeens (6% vs. 5%) [all p <0.01] than those who had never had sex. A lower proportion of participants reporting ever having had sex spent time at family member’s homes (52% vs. 56%), church (50% vs. 56%), neighbor’s homes (30% vs. 31%), work (12% vs. 13%), shops (10% vs. 12%), and outside of the community (5% vs. 6%) [all p <0.01].
HIV Infection and Sexual Behaviors Across Study Visits (Table 1)
Over the course of the study, there were 174 incident HIV infections between visit one and visit four. The proportion of participants reporting any unprotected sex in the past three months increased from 8% at visit one to 20% at visit four. The proportion of participants reporting any transactional sex in the past three months increased from 8% at visit one to 17% at visit four. The proportion of participants reporting having an older partner, five or more years older than them, increased from 6% at visit one to 21% at visit four.
Associations Among Group Membership, Time Spent, and HIV Incidence (Figures 1 and 2)
Figure 1.
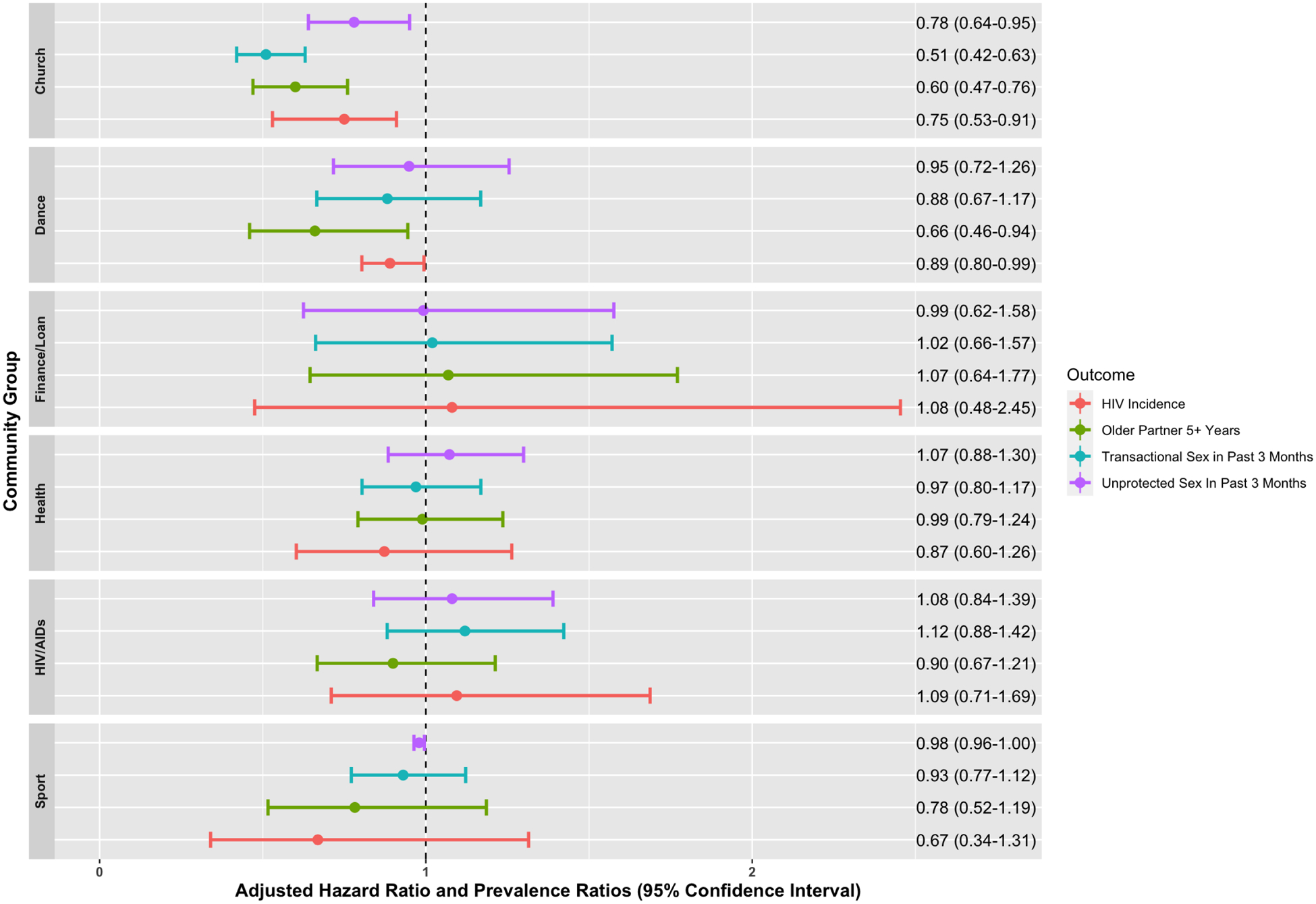
HIV Incidence and Sexual Behaviors by Community Group Membership
Figure 2.
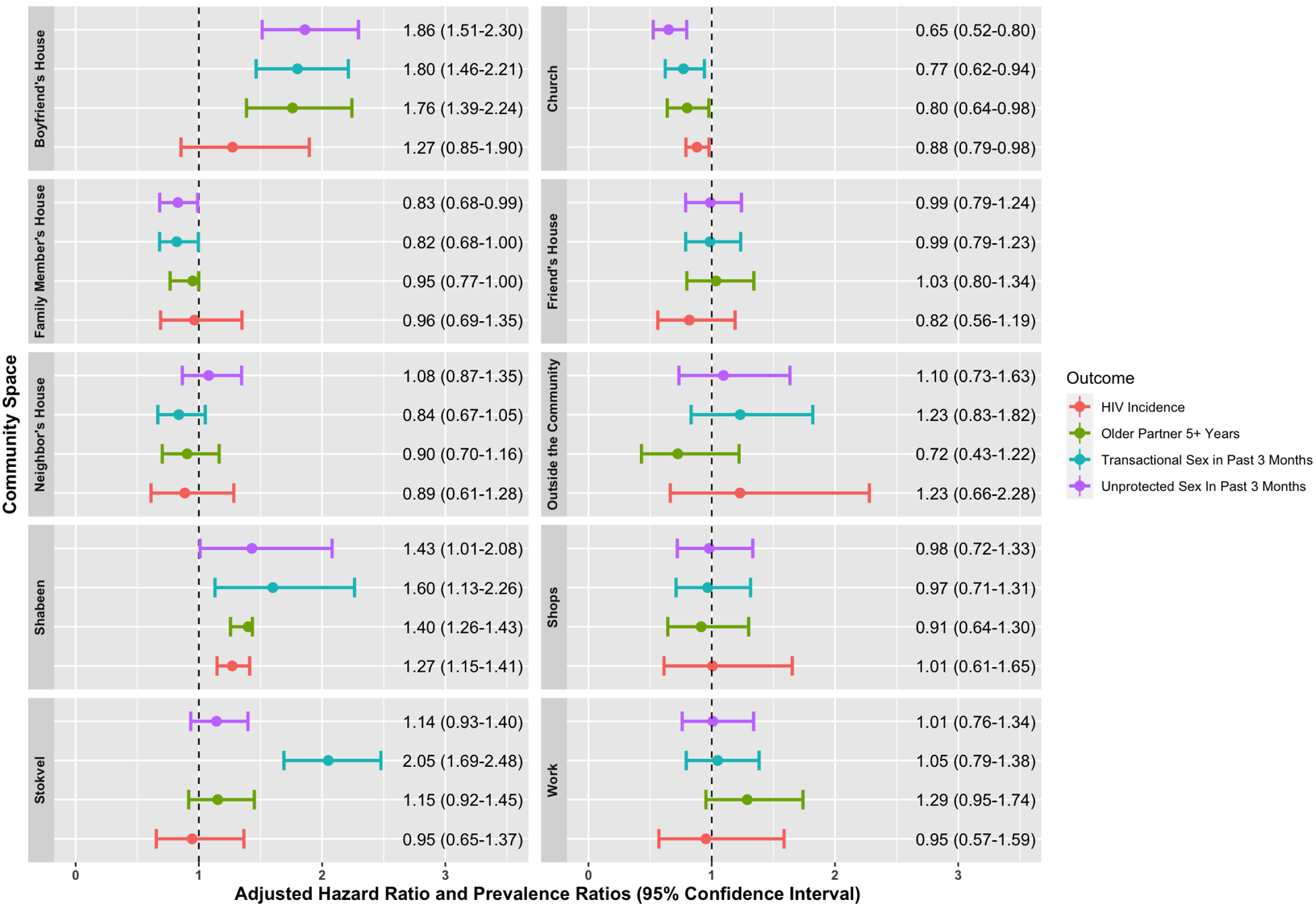
HIV Incidence and Sexual Behaviors by Time Spent at Community Spaces
We found membership in church groups (aHR: 0.75, 95% CI: 0.53, 0.91) and dance groups (aHR: 0.89, 95% CI; 0.80, 0.98) to be protective for HIV infection. Similarly, participants who reported spending time at church were at lower risk for HIV infection (aHR: 0.88, 95% CI: 0.79, 0.98). Among social group membership and time spent at social and community spaces, we only found spending time at shebeens to increase the risk of HIV acquisition (aHR: 1.27, 95% CI: 1.15, 1.41).
Associations Among Group Membership, Time Spent, and Unprotected Sex (Figures 1 and 2)
We found that participants who were part of church groups (aPR: 0.78, 95% CI: 0.64, 0.95) and spent time at church (aPR: 0.65, 95% CI: 0.52, 0.80) or family member’s homes (aPR: 0.83, 95% CI: 0.68, 0.99) were less likely to have engaged in unprotected sex in the past three months. Conversely, participants who spent time at their boyfriend’s house (aPR: 1.86, 95% CI: 1.51, 2.30) and at shebeens (aPR: 1.43, 95% CI: 1.01, 2.06) were more likely to have engaged in unprotected sex in the past three months.
Associations Among Group Membership, Time Spent, and Transactional Sex (Figures 1 and 2)
We found that participants who belonged to church groups (aPR: 0.51, 95% CI: 0.42, 0.63) and spent time at church (aPR: 0.77, 95% CI: 0.62, 0.94) or family member’s homes (aPR: 0.82, 95% CI: 0.68, 0.99) were less likely to have engaged in transactional sex in the past three months. Participants who spent time at stokvels (aPR: 2.05, 95% CI: 1.69, 2.48), boyfriend’s homes (aPR: 1.80, 95% CI: 1.46, 2.21), and shebeens (aPR: 1.60, 95% CI: 1.13, 2.26) were more likely to have engaged in transactional sex in the past three months.
Associations Among Group Membership, Time Spent, and Older Partnership (Figures 1 and 2)
We found that participants who were part of church groups (aPR: 0.60, 95% CI: 0.47, 0.76) and dance groups (aPR: 0.66, 95% CI: 0.46, 0.94), as well as those who spent time at church (aPR: 0.80, 95% CI: 0.64, 0.98) at neighbor’s homes (aPR: 0.95, 95% CI: 0.75, 0.99) were less likely to have an older partner. Participants who spent time at their boyfriend’s house (aPR: 1.76, 95% CI: 1.39, 2.24) or shebeens (aPR: 1.40, 95% CI: 1.26, 1.43) were more likely to have an older partner.
Differences in Group Membership and Time Spent by School Enrollment (Table 2)
Table 2.
Group Membership and Time Spent by School Enrollment at Visit 4*
| Currently Enrolled in High School (N = 377) | Graduated or Dropped Out of High School (N = 1554) | Chi-Square | |||
|---|---|---|---|---|---|
| N | % | N | % | p-value | |
| Groups | |||||
| Church/Religious | 133 | 35% | 729 | 47% | < 0.01 |
| Health | 71 | 19% | 386 | 25% | 0.024 |
| HIV/AIDs | 44 | 12% | 231 | 15% | 0.052 |
| Dance | 38 | 10% | 165 | 11% | 0.212 |
| Sport | 16 | 4% | 64 | 4% | 0.230 |
| Finance/Loan | 11 | 3% | 49 | 3% | 0.219 |
| Time Spent | |||||
| Friend’s House | 238 | 63% | 911 | 59% | 0.124 |
| Family Member’s House | 145 | 38% | 585 | 38% | 0.297 |
| Church | 185 | 49% | 833 | 54% | 0.042 |
| Neighbor’s House | 66 | 18% | 225 | 14% | 0.116 |
| Boyfriend’s House | 90 | 24% | 538 | 35% | 0.015 |
| Shops | 31 | 8% | 140 | 9% | 0.255 |
| Work | 36 | 10% | 222 | 14% | 0.012 |
| Outside the Community | 13 | 3% | 54 | 3% | 0.297 |
| Shebeen | 11 | 3% | 33 | 2% | 0.201 |
| Stokvel | 71 | 19% | 402 | 26% | < 0.01 |
Totals do not sum to 100% due to missing data
At visit four, the majority of participants were not enrolled in high school (N = 1554, 80%). Of those not enrolled, 84% had graduated high school (N = 1298) and 16% had dropped out of high school (N = 256). We found that participants not enrolled in school, compared to those who were still enrolled, were more likely to be members of church groups (47% vs. 35%, p < 0.01) and health groups (25% vs. 19%, p = 0.024). In addition, participants who were not enrolled in school were more likely to spend time at church (54% vs 49%, p < 0.01) their boyfriend’s house (35% vs. 24%, p = 0.015), work (14% vs. 10%, p = 0.012), and stokvels (26% vs. 19%, p < 0.01). However, school enrollment status did not significantly modify the association between group membership, time spent, and any HIV-related outcomes.
DISCUSSION
In this analysis, we investigated how community spaces and community group membership contribute to HIV acquisition and engagement in risky sexual behavior among AGYW in rural South Africa. Our results suggest that spending time in community spaces and group memberships that include an element of adult supervision (church and family members’ homes) may be protective while spaces and groups that provide an opportunity for AGYW to interact with boyfriends or meet new partners without supervision (boyfriend’s home, shebeens, and stokvels) may be risky.
Parental monitoring has been found to reduce risky sexual behaviors among AGYW in SSA.30,31 Studies suggest that parental monitoring limits time and opportunity to engage in sex and may change AGYW’s sexual attitudes by conveying parental beliefs. Our results, related to church group membership and spending time at church and family member’s homes, support these findings and additionally suggest that the impact of monitoring on AGYW risky sexual behaviors can be potentially extended to older adults as well as non-parental family members. We were not able to untangle whether spending time at church and family member’s homes simply limited opportunities to engage in sex or whether these spaces, and the adults in these spaces, imbued norms related to protective sexual behaviors. Exploring such differences is important if church and family member home contexts are to be utilized in HIV prevention efforts given previous literature. For example, studies conducted among AGYW in Zambia and South Africa found church membership to be associated with later sexual initiation and lower rates of pre-marital sex but the likelihood of condom use after sexual initiation was reduced.32,33 Additionally, studies in Zimbabwe found church membership to be associated with earlier marriage, which is has been found to be risk factor for HIV acquisition among AGYW.34–36 Identifying community spaces and groups that occupy AGYW’s time and facilitate protective norms related to HIV prevention is an important area for future research.
We found that spending time at stokvels increased AGYW’s risk of engaging in transactional sex, however there wasn’t a strong association between finance/loan group membership and transactional sex. Stokvels are mixed gender voluntary savings and credit groups comprised of older adults. Stokvel members meet regularly to contribute a fixed amount of money to a common pool which is then distributed amongst its members on a rotating basis. Meetings are also a form of social gathering and often include an element of merriment with alcohol.37,38 Previous studies have reported that while stokvels provide a platform for financial empowerment, social support, and fellowship, the alcohol consumption component increases the likelihood of risky sexual behaviors amongst members of both genders, including transactional sex.38–41 Given that a minimal number of participants reported belonging to a finance/loan group (5%) but almost a third of participants (30%) reported spending time at stokvels, it might be that AGYW frequent stokvels primarily for the opportunity to socialize or to meet financially solvent sexual partners. Future work that investigates motivations for spending time at stokvels and the potential for youth inclusive savings and loan groups is necessary, particularly among economically vulnerable AGYW.
Changes in where AGYW spent their time and the groups they belong to after leaving school aligned with expected milestones on the transition to adulthood. AGYW who were not in school were more likely to spend time at church, work, stokvels, and their boyfriend’s home. These spaces are reflective of AGYW potentially leaving parental homes, cohabitating, entering the workforce, or shouldering the financial responsibilities of their households. It is also possible that our list of the community groups and community spaces was not reflective of where AGYW in rural South Africa gather and spend their time, particularly after leaving school. Identifying these groups and spaces is important as we build our understanding of the structural, economic, and social needs of AGYW in the region to provide improved HIV prevention programing.
Despite the strengths of using longitudinal data and our large sample size of AGYW, this analysis also has a few limitations. First, we were not able to assess the temporal order of group membership, where AGYW spent time outside of home and school, and sexual behaviors. Second, information on sexual behaviors was self-reported, and there may have been some misreporting in the study despite the use of audio computer-assisted self-interview to minimize reporting bias. Third, we did not have any data on the age and gender composition of community groups and spaces or the frequency with AGYW engaged with the groups and spaces. In addition, participants may have conceptualized groups and spaces differently given that the survey questions did not include any descriptions. Fourth, it should be noted that the data are from a randomized controlled trial where all young women were already enrolled in school at study enrollment. As a result, findings from this population may not be generalizable to AGYW who are not in school or returned to school. Finally, there may also have been a Hawthorne effect of the trial where young women were less likely to drop out due to trial participation.42
CONCLUSION
Effective prevention interventions are needed to reduce HIV incidence among AGYW. Meaningful combinations of prevention interventions will be most effective when they are tailored to the social, biological, and structural needs of adolescent populations. This paper provides support for the notion that community context, particularly related to membership in community groups and engagement with community spaces, is associated with HIV incidence and risky sexual behaviors for AGYW in rural South Africa. Furthermore, community spaces and groups that include an element of adult supervision (church and family members’ homes) may be protective while spaces and groups that provide an opportunity for AGYW to interact with boyfriends or meet new partners without supervision (boyfriend’s home, shebeens, and stokvels) may be risky. Taken together, our results suggest that future HIV prevention intervention for AGYW consider the importance of existing safe spaces that include adult supervision or mentorship.
SOURCES OF FUNDING:
NLB was supported by the National Institute of Allergy and Infectious Diseases (T32 AI00700140). The HIV Prevention Trials Network is funded by the National Institute of Allergy and Infectious Diseases (UM1AI068619, UM1AI068613, and UM1AI1068617), with co-funding from the National Institute of Mental Health and the National Institute on Drug Abuse, all components of the US National Institutes of Health. This work was also supported by NIMH(R01MH087118) and the Carolina Population Center and its NIH Center Grant (P2C HD050924).
REFERENCES
- 1.UNAIDS. Global HIV & AIDS Statistics Factsheet. http://www.unaids.org/en/resources/fact-sheet (2019).
- 2.Simbayi L et al. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017. (2019).
- 3.Gómez-Olivé FX et al. Prevalence of HIV among those 15 and older in rural South Africa. AIDS Care 25, 1122–1128 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pettifor A, Stoner M, Pike C & Bekker L-G Adolescent lives matter: preventing HIV in adolescents. Curr. Opin. HIV AIDS 13, 265–273 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dellar RC, Dlamini S & Karim QA Adolescent girls and young women: key populations for HIV epidemic control. J. Int. AIDS Soc 18, 19408(2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viner RM et al. Adolescence and the social determinants of health. The Lancet 379, 1641–1652 (2012). [DOI] [PubMed] [Google Scholar]
- 7.Gray RH et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet Lond. Engl 357, 1149–1153 (2001). [DOI] [PubMed] [Google Scholar]
- 8.Jewkes R & Morrell R Gender and sexuality: emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and prevention. J. Int. AIDS Soc 13, 6(2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Exner TM, Dworkin SL, Hoffman S & Ehrhardt AA Beyond the male condom: the evolution of gender-specific HIV interventions for women. Annu. Rev. Sex Res 14, 114–136 (2003). [PubMed] [Google Scholar]
- 10.WHO. Integrating gender into HIV/AIDS programmes in the health sector. (2009).
- 11.Bruce J, Temin M & Hallman K Evidence-based approaches to protecting adolescent girls at risk of HIV. AIDSTAR-One Spotlight Gend. (2012). [Google Scholar]
- 12.Baldwin W Creating ‘safe spaces’ for adolescent girls. Promot. Healthy Safe Product. Transit. Adulthood 39, (2011). [Google Scholar]
- 13.Hallman K et al. Enhancing financial literacy, HIV/AIDS skills, and safe social spaces among vulnerable South African youth. N. Y. Popul. Counc. Transit. Adulthood Brief (2007). [Google Scholar]
- 14.Garcia J et al. ‘You’re Really Gonna Kick Us All Out?’ Sustaining Safe Spaces for Community-Based HIV Prevention and Control among Black Men Who Have Sex with Men. PloS One 10, e0141326(2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haas SA, Schaefer DR & Kornienko O Health and the structure of adolescent social networks. J. Health Soc. Behav 51, 424–439 (2010). [DOI] [PubMed] [Google Scholar]
- 16.Umberson D, Crosnoe R & Reczek C Social Relationships and Health Behavior Across the Life Course. Annu. Rev. Sociol 36, 139–157 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bruce J Girls left behind: Redirecting HIV interventions toward the most vulnerable. (2007).
- 18.Hallman K & Diers J Social isolation and economic vulnerability: Adolescent HIV and pregnancy risk factors in South Africa. in Poster presentation at the Annual Meeting of the Population Association of America, Boston 1–3 (2004). [Google Scholar]
- 19.LeGrand S, Muessig KE, Pike EC, Baltierra N & Hightow-Weidman LB If you build it will they come? Addressing social isolation within a technology-based HIV intervention for young black men who have sex with men. AIDS Care 26, 1194–1200 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fleischman J & Peck K Addressing HIV risk in adolescent girls and young women. CSIS Glob. Health Policy Cent (2015). [Google Scholar]
- 21.Austrian K, Soler-Hampejsek E, Hewett PC, Hachonda NJ & Behrman JR Adolescent girls empowerment programme: endline technical report. (2018).
- 22.Erulkar A Building the assets to thrive: Addressing the HIV-related vulnerabilities of adolescent girls in Ethiopia. (2014).
- 23.Stoner MCD et al. Effect of Schooling on Age-Disparate Relationships and Number of Sexual Partners Among Young Women in Rural South Africa Enrolled in HPTN 068. J. Acquir. Immune Defic. Syndr. 1999 76, e107–e114 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hargreaves JR et al. The association between school attendance, HIV infection and sexual behaviour among young people in rural South Africa. J. Epidemiol. Community Health 62, 113–119 (2008). [DOI] [PubMed] [Google Scholar]
- 25.Hirschi T A control theory of delinquency. Criminol. Theory Sel. Class. Read 1969, 289–305 (1969). [Google Scholar]
- 26.Hawkins JD & Weis JG The social development model: An integrated approach to delinquency prevention. in Developmental and Life-course Criminological Theories 3–27 (Routledge, 2017). [Google Scholar]
- 27.Collinson MA Striving against adversity: the dynamics of migration, health and poverty in rural South Africa. Glob. Health Action 3, 5080(2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pettifor A et al. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet Glob. Health 4, e978–e988 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pettifor A et al. HPTN 068: a randomized control trial of a conditional cash transfer to reduce HIV infection in young women in South Africa—study design and baseline results. AIDS Behav. 20, 1863–1882 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Biddlecom A, Awusabo-Asare K & Bankole A Role of Parents in Adolescent Sexual Activity and Contraceptive Use in Four African Countries. Int. Perspect. Sex. Reprod. Health 35, 72–81 (2009). [DOI] [PubMed] [Google Scholar]
- 31.Puffer ES et al. Individual- and Family-Level Psychosocial Correlates of HIV Risk Behavior Among Youth in Rural Kenya. AIDS Behav. 15, 1264–1274 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agha S, Hutchinson P & Kusanthan T The effects of religious affiliation on sexual initiation and condom use in Zambia. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med 38, 550–555 (2006). [DOI] [PubMed] [Google Scholar]
- 33.Garner RC Safe sects? Dynamic religion and AIDS in South Africa. J. Mod. Afr. Stud 38, 41–69 (2000). [DOI] [PubMed] [Google Scholar]
- 34.Hallfors DD et al. Preventing HIV by providing support for orphan girls to stay in school: does religion matter? Ethn. Health 18, 53–65 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.GREGSON S, ZHUWAU T, ANDERSON RM & CHANDIWANA SK Apostles and Zionists: The influence of religion on demographic change in rural Zimbabwe. Popul. Stud 53, 179–193 (1999). [DOI] [PubMed] [Google Scholar]
- 36.Clark S Early Marriage and HIV Risks in Sub-Saharan Africa. Stud. Fam. Plann 35, 149–160 (2004). [DOI] [PubMed] [Google Scholar]
- 37.Verhoef G Informal financial service institutions for survival: African women and stokvels in urban South Africa, 1930–1998. Enterp. Soc 2, 259–296 (2001). [Google Scholar]
- 38.Matuku S & Kaseke E The role of stokvels in improving people’s lives: The case in orange farm, Johannesburg, South Africa. Soc. Work 50, 504–515 (2014). [Google Scholar]
- 39.Wojcicki JM ‘ She drank his money’: survival sex and the problem of violence in taverns in Gauteng province, South Africa. Med. Anthropol. Q 16, 267–293 (2002). [DOI] [PubMed] [Google Scholar]
- 40.Wojcicki JM Commercial sex work or ukuphanda? Sex-for-money exchange in Soweto and Hammanskraal area, South Africa. Cult. Med. Psychiatry 26, 339–370 (2002). [DOI] [PubMed] [Google Scholar]
- 41.Campbell C, Williams B & Gilgen D Is social capital a useful conceptual tool for exploring community level influences on HIV infection? An exploratory case study from South Africa. AIDS Care 14, 41–54 (2002). [DOI] [PubMed] [Google Scholar]
- 42.Rosenberg M et al. Evidence for sample selection effect and Hawthorne effect in behavioural HIV prevention trial among young women in a rural South African community. BMJ Open 8, e019167(2018). [DOI] [PMC free article] [PubMed] [Google Scholar]


