Abstract
Background:
Youth with perinatal HIV exposure have demonstrated high rates of emotional-behavioral problems. Few studies have longitudinally examined racial/ethnic disparities in such functioning across adolescence, a critical time for targeting prevention/intervention efforts.
Setting:
The PHACS Adolescent Master Protocol, one of the largest US-based cohort studies of youth with perinatal HIV infection (YPHIV) or HIV-exposed but uninfected (YPHEU).
Methods:
Youth and caregivers individually completed the Behavior Assessment System for Children, 2nd edition every two years between ages 7–19. We used adjusted mixed effect models to evaluate whether mean youth-reported emotional concerns and caregiver-reported behavioral concerns differed by race/ethnicity. We used Group-based trajectory models (GBTMs) to identify groups having similar emotional-behavioral trajectories, followed by multinomial models to determine which factors predicted group membership.
Results:
391 YPHIV and 209 YPHEU (7% White non-Hispanic, 21% White Hispanic, 66% Black non-Hispanic, 6% Black Hispanic) completed a median of 4 assessments over follow-up. Adjusted models showed more caregiver-reported behavioral concerns for Black non-Hispanic YPHEU than Black non-Hispanic YPHIV, White Hispanic YPHIV, and White Hispanic YPHEU, particularly later in adolescence. Race/ethnicity did not predict membership in subgroups of youth-reported emotional or caregiver-reported behavioral functioning identified using GBTMs. However, factors predicting membership in vulnerable youth-reported emotional and caregiver-reported behavioral groups included experiencing a stressful life event and living with a caregiver who was married or screened positive for a psychiatric condition.
Conclusion:
Our study revealed that Black non-Hispanic YPHEU are a vulnerable subgroup. Contributing factors that could inform interventions include the caregiver’s health, household characteristics, and psychiatric status.
Keywords: perinatal HIV, neurodevelopment, emotional-behavioral functioning, racial disparities, group-based trajectory model
Introduction
Youth born to women with HIV have demonstrated greater emotional-behavioral problems than the general US youth population.1 Gadow et al. and others found that youth living with perinatal HIV infection (YPHIV) and youth perinatally HIV-exposed but uninfected (YPHEU) had higher rates of psychiatric disorders than the general population.1–9 However, the role of PHIV has been mixed. Some studies observed higher risk of emotional-behavioral problems among YPHEU than YPHIV;4,7 others showed higher rates of psychiatric disorders in YPHIV than YPHEU;3,8 yet others found similar rates of psychiatric disorders among both groups.2,9 Regardless of mental health prevalence, several studies reported that YPHIV were more likely to receive psychotropic or non-pharmacological mental health treatment than YPHEU, likely because of closer monitoring within routine PHIV-related medical care.10–12
Social determinants of health (SDOH) may be associated with emotional-behavioral functioning among YPHIV and YPHEU. SDOH is defined as “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect health, functioning, and quality-of-life outcomes and risks.”13 Additionally, studies of YPHIV and YPHEU indicate that caregiver characteristics play a significant role in children’s emotions and behavior. These characteristics include the caregiver relationship (i.e., biological mother or other), the caregiver’s health (i.e., HIV status and psychiatric conditions), and life stressors within the family or household.3,4,6,11 Importantly, since youth in this population often live in low-income neighborhoods, with increased risk for stressful events in childhood and adolescence, SDOH may exacerbate emotional-behavioral challenges.3,14
Additionally, underrepresented individuals from low-income neighborhoods may experience race-based discrimination.15–17 A meta-analysis by Williams and colleagues highlighted that race-based discrimination predicts adverse mental and physical outcomes. Specifically, marginalized racial groups experience elevated disease and mortality rates, race-based differences persist in health even after adjustment for socioeconomic status, and the general health of Hispanics is declining over time.15
In the US, YPHIV and YPHEU are now reaching adulthood, allowing examination of their emotional-behavioral functioning over time. To provide targeted interventions, it is crucial to understand how the lived experience of those in minority racial and ethnic groups contribute to the emotional-behavioral health of youth affected by HIV throughout adolescence.1,3–6,18–20 While a limited number of studies have evaluated behavior longitudinally in YPHIV, none have specifically addressed racial/ethnic disparities in emotional-behavioral functioning.21
We used data from one of the largest prospective cohort studies of YPHIV and YPHEU in the US, providing a unique opportunity to examine racial/ethnic differences in emotional-behavioral trajectories from mid-childhood through late adolescence, spanning critical, dynamic periods of development. The availability of youth self- and caregiver reports about youth emotions and behavior provide unique perspectives on youth’s psychological adjustment.22 We evaluated the impact of membership in particular racial/ethnic groups on trends in emotional-behavioral functioning during adolescence, identifying potentially vulnerable subgroups of youth with poorer functioning.
Methods
Study Population
The Pediatric HIV/AIDS Cohort Study (PHACS) (https://phacsstudy.org) Adolescent Master Protocol (AMP) was designed to evaluate the impact of perinatally acquired HIV and antiretroviral therapy on YPHIV. From March 2007 to October 2009, AMP enrolled 678 children and youth with perinatal HIV exposure (YPHIV and YPHEU) at fifteen sites in the US, including Puerto Rico. Eligibility criteria included perinatal HIV infection or exposure, age 7–16 at enrollment, engaged in care, and recorded antiretroviral history. AMP study visits occurred every six months until 2010, then annually thereafter. Data collection included physical examination, medical chart review, structured demographic and psychosocial interviews, and neurodevelopmental evaluations. Trained psychologists evaluated youth and caregiver mental health and psychosocial well-being through a biopsychosocial assessment protocol. Institutional Review Boards at participating sites and the Harvard T.H. Chan School of Public Health approved the study. Written informed consent and age-appropriate assent were obtained according to institutional guidelines. Given the epidemiology of HIV in women and children, analyses focused on youth with race reported as either Black/African American or White, ethnicity as either Hispanic or non-Hispanic, and at least one obtained emotional-behavioral assessment between the ages of 7 and 19 years.
Emotional-behavioral functioning
A standard in child and adolescent psychology and psychiatry, we utilized a multi-informant approach—youth and caregiver reports—to capture unique perspectives on youth psychological adjustment.22 Youth are likely to report more accurately on their internalizing states (i.e., depression and anxiety) while caregivers are considered more reliable reporters of youth externalizing behaviors.23 In contrast, caregivers are considered more reliable reporters of youth’s externalizing behaviors.23 PHACS psychologists administered the Behavior Assessment System for Children-Second Edition (BASC-2) every two years through independent interviews with youth and caregivers at the same visit.24 A standardized, validated and reliable multidimensional questionnaire, the BASC-2 contains two summary measures of interest. The Emotional Symptoms Index (ESI), a youth-reported summary measure, reflects emotional functioning by measuring social stress, anxiety, depression, sense of inadequacy, self-esteem, and self-reliance domains. The Behavioral Symptoms Index (BSI), a caregiver-reported summary measure, reflects caregiver perceptions of the youth’s behavior, including hyperactivity, aggression, depression, attention problems, atypicality, and withdrawal. Higher ESI and BSI scores indicate poorer emotional-behavioral functioning. T-score classifications are: <60 “Average Range,” 60–69 “At-Risk,” and >69 “Clinically Significant.”24 ESI or BSI assessments >85 were excluded as outliers.
Race/Ethnicity
Although race-based discrimination is not currently assessed, self-reported race was used as a proxy, allowing this analysis to inform future PHACS analyses on race-based discrimination. Caregivers reported their child’s race as Black/African American, White, Asian, American Indian, Multiracial, or Unknown. The following racial groups were excluded due to small subsets: American Indian (0.4%), Asian (0.9%), Multiracial (1.9%), and Unknown/not reported (4.3%). Caregivers also reported their child’s ethnicity (Hispanic/non-Hispanic). Four racial/ethnic subgroups were evaluated: White non-Hispanic, White Hispanic, Black non-Hispanic, and Black Hispanic.
Covariates and Potential Confounders
Demographic data were obtained through independently administered youth and caregiver interviews. Youth information included age at each study visit, biological sex, socioeconomic status (household income, caregiver education, and household density reported at study entry), and family structure (whether the biological mother was born in the US, whether the caregiver is the youth’s biological mother, change in primary caregiver during study follow-up, caregiver’s marital status, and geographic region of the enrollment site). Number of stressful life events experienced by the youth as measured by the Quality of Life Assessment25 at baseline also was included (i.e., caregiver lost job, death of a family member, caregiver went to jail). Caregiver information included HIV status and positive screen from the initial Client Diagnostic Questionnaire (CDQ) for any psychiatric disorder including: depression, panic attacks, Generalized Anxiety Disorder (GAD), alcohol abuse, substance abuse, trauma, or any psychiatric condition, obtained from the earliest assessment.26,27 Of the 600 caregivers in the sample, 219 (37%) were biological mothers. These SDOH were considered as potential confounders. Less than 5% of youth were missing SDOH information except for family structure variables (≤16%) and caregiver health variables (≤14%, not evaluated); missing indicators were used for these measures.
Statistical Methods
To summarize emotional-behavioral functioning, two longitudinal approaches were implemented: a traditional mixed effects model, and a novel group-based trajectory model (GBTM). These two complimentary approaches allow a robust investigation of potential race-based disparities in emotional-behavioral functioning over time.
Mixed Effects Models
We fit mixed effects models to evaluate whether mean ESI and BSI T-scores differed across the 4 racial/ethnic groups as youth transitioned through adolescence. To allow a potential non-linear relationship of T-scores with age, we included squared terms for age. We also evaluated possible effect modification of racial/ethnic associations by HIV status using stratified analyses. Models included a random effect for each youth to account for correlation in repeated assessments. An exponential spatial correlation structure with a nugget effect,28–30 was utilized.
Initial ESI and BSI models were fit adjusting for youth age (centered at mean age at first assessment = 11.6 years), HIV status, and sex. We included interactions of racial/ethnic group with age, age2, and HIV status. Final models additionally included any SDOH that changed any of the racial/ethnic group estimates by >10%. Mixed effects model results were used to generate predicted trajectories for mean emotional-behavioral functioning by racial/ethnic group and HIV status. Contrasts of least-square means were used to test pairwise differences in emotional-behavioral functioning across the four racial/ethnic groups at each age.
Group-Based Trajectory Models
GBTMs were fit to identify groups of youth following similar emotional-behavioral trajectories between ages 7 to 19 years. This approach uses multinomial density functions rather than continuous multivariate density functions to model variation in developmental trajectory parameters.31 The maximized function is a product of the probability of belonging to a specific group, and the conditional probability of the outcome as a function of age given group membership. The model selection process consisted of two iterative steps. First, we held the quadratic form constant and used the Bayesian information criterion (BIC) to identify the optimal number of groups.32 Then, keeping this number constant, we used the BIC to determine the optimal polynomial function of the model. This process yielded a predicted probability of belonging to each group for each youth, and assigned each youth to the group with maximum probability. Finally, we modeled the groups as dependent variables in a multinomial logistic regression model to determine which of the covariates described previously, including race and ethnicity, predicted group membership. GBTM results were summarized through plots of predicted trajectories with 95% confidence intervals (CIs). We summarized baseline characteristics by group membership. Statistical analyses were conducted using Stata (version 16, StataCorp LLC., College Station, TX) and R (R Core Team, 2019).
Results
Study Population
The AMP study enrolled 678 youth between 2007 and 2009, including 451 YPHIV and 227 YPHEU. Among these, 600 (88%) were included in the analysis of BSI scores and 588 (87%) in the analysis of ESI scores. Within the BSI sample, about half were male (49%), and the average age at first behavioral assessment was 11.6 years (Table 1). Overall, 72% identified as Black and 27% as Hispanic. Table 1 shows baseline characteristics of the four racial/ethnic groups. Baseline youth characteristics of the ESI sample (n=588) were similar (Supp. Table 1), and characteristics of those included in each sample were similar to the AMP study as a whole (Supp. Table 2).33 As of June 2019, AMP participants had up to eight youth and caregiver emotional-behavioral assessments (median = 4, IQR = 3–5), allowing for characterization of longitudinal trajectories. The median number of repeated measurements (4) was the same across racial/ethnic groups.
Table 1.
Baseline Characteristics of Caregiver-reported BSI Study Population by Racial/ethnic Group
| Racial/ethnic Group | |||||
|---|---|---|---|---|---|
| Characteristic | Total (n=600) |
White non-Hispanic (n=44) |
White Hispanic (n=127) |
Black non-Hispanic (n=396) |
Black Hispanic (n=33) |
| Median Assessments (IQR) | 4 (3–5) | 4 (2–5) | 4 (3–5) | 4 (3–5) | 4 (3–4) |
| Mean Age (SD) | 11.6 (2.7) | 12.1 (2.8) | 11.5 (2.7) | 11.6 (2.7) | 11.5 (2.7) |
| Male vs Female | 296 (49.3%) | 19 (43.2%) | 70 (55.1%) | 190 (48.0%) | 17 (51.5%) |
| YPHIV vs YPHEU | 391 (65.2%) | 28 (63.6%) | 69 (54.3%) | 276 (69.7%) | 18 (54.5%) |
| Socioeconomic Status | |||||
| Household income ≤ $20,000 | 302 (50.3%) | 10 (22.7%) | 88 (69.3%) | 185 (46.7%) | 19 (57.6%) |
| Caregiver education <HS | 166 (27.7%) | 2 (4.5%) | 59 (46.5%) | 91 (23.0%) | 14 (42.4%) |
| Household income supports ≤4 people | 362 (60.3%) | 35 (79.5%) | 69 (54.3%) | 236 (59.6%) | 22 (66.7%) |
| Family Structure | |||||
| Mother born in US | 459 (76.5%) | 40 (90.9%) | 80 (63.0%) | 319 (80.6%) | 20 (60.6%) |
| Caregiver is biological mother | 219 (36.5%) | 18 (40.9%) | 58 (45.7%) | 131 (33.1%) | 12 (36.4%) |
| Primary caregiver change | 58 (9.7%) | 5 (11.4%) | 15 (11.8%) | 36 (9.1%) | 2 (6.1%) |
| Caregiver is married | 201 (33.5%) | 21 (47.7%) | 41 (32.3%) | 132 (33.3%) | 7 (21.2%) |
| Experienced stressful life event | 442 (73.7%) | 36 (81.8%) | 90 (70.9%) | 291 (73.5%) | 25 (75.8%) |
| Site location | |||||
| South | 209 (34.8%) | 7 (15.9%) | 16 (12.6%) | 184 (46.5%) | 2 (6.1%) |
| Northeast | 193 (32.2%) | 12 (27.3%) | 35 (27.6%) | 130 (32.8%) | 16 (48.5%) |
| Midwest | 87 (14.5%) | 14 (31.8%) | 5 (3.9%) | 65 (16.4%) | 3 (9.1%) |
| West | 59 (9.8%) | 11 (25.0%) | 30 (23.6%) | 17 (4.3%) | 1 (3.0%) |
| Puerto Rico | 52 (8.7%) | 0 (0.0%) | 41 (32.3%) | 0 (0.0%) | 11 (33.3%) |
| Caregiver Health | |||||
| Living with HIV | 282 (47.0%) | 22 (50.0%) | 84 (66.1%) | 160 (40.4%) | 16 (48.5%) |
| Positive CDQ screening for | |||||
| Alcohol abuse | 28 (4.7%) | 1 (2.3%) | 10 (7.9%) | 15 (3.8%) | 2 (6.1%) |
| Panic or GAD | 62 (10.3%) | 3 (6.8%) | 13 (10.2%) | 40 (10.1%) | 6 (18.2%) |
| Major or other depression | 66 (11.0%) | 3 (6.8%) | 11 (8.7%) | 43 (10.9%) | 9 (27.3%) |
| Drug abuse | 15 (2.5%) | 1 (2.3%) | 3 (2.4%) | 10 (2.5%) | 1 (3.0%) |
| Any psychiatric condition | 168 (28.0%) | 11 (25.0%) | 36 (28.3%) | 106 (26.8%) | 15 (45.5%) |
BSI: Behavioral Symptoms Index; SD: Standard Deviation; YPHIV: Youth with perinatally-acquired HIV infection; YPHEU: Youth who are perinatally HIV-exposed but uninfected; HS: High School; CDQ: Client Diagnostic Questionnaire; GAD: Generalized Anxiety Disorder; Missingness for Socioeconomic Status (range: 0–5%), Family Structure (range: 0–16%), Caregiver Health (range: 10–14%)
Differences in Emotional-Behavioral Functioning: Mixed Effect Model Results
The final adjusted mixed effects model for ESI (child-reported emotional functioning) controlled for youth HIV status, sex, age, site location, and caregiver psychiatric condition (Supp. Table 3). Predicted trajectories for mean emotional functioning for each cross-classification of racial/ethnic group and HIV status are shown in Figure 1 (upper panel). A Likelihood Ratio Test showed no overall racial/ethnic differences across age in ESI T-scores; pairwise contrast tests of least-square means showed no difference in ESI T-scores between racial/ethnic groups at each age. The final model for BSI (caregiver-reported behavioral functioning) controlled for youth HIV status, sex, age, household density, stressful life event, having a caregiver living with HIV, and any caregiver psychiatric condition. In contrast to the ESI model, there was greater evidence of overall racial/ethnic differences in BSI T-scores. Pairwise contrasts tests showed that Black non-Hispanic YPHEU had significantly more caregiver-reported behavioral concerns than three other groups at specific ages. Specifically, their mean scores were approximately five points higher (0.5 SD) than Black non-Hispanic YPHIV from age 7 to 19, five points higher than White Hispanic YPHIV from age 13 to 17, and five points higher than White Hispanic YPHEU from age 15 and 17 (Figure 1, lower panel).
Figure 1. Predicted Mean ESI and BSI T-scores from Adjusted Mixed Effects Models.
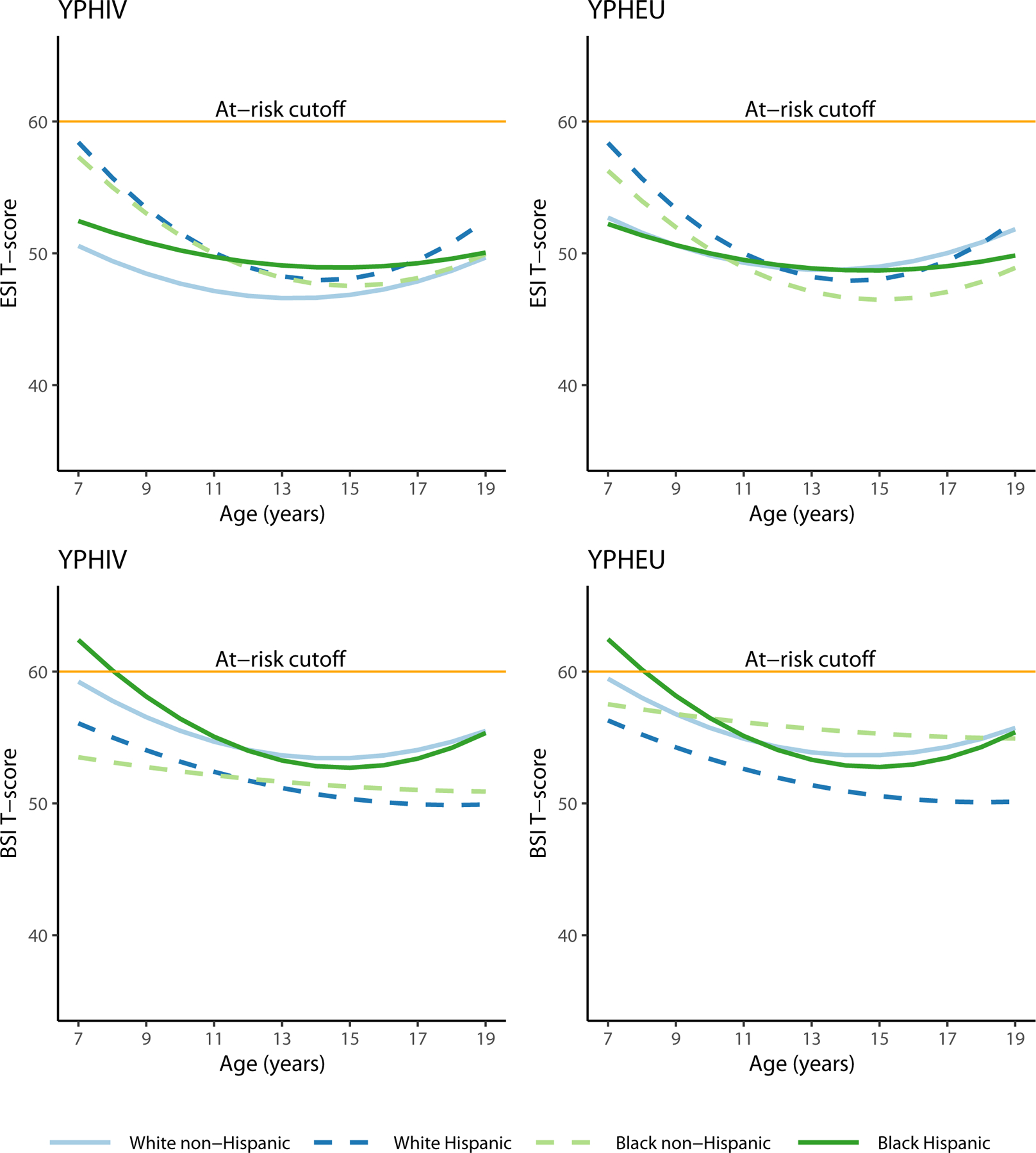
YPHIV: Youth with perinatally-acquired HIV infection; YPHEU: Youth who are perinatally HIV-exposed but uninfected; ESI: Emotional Symptoms Index; BSI: Behavioral Symptoms Index
Differences in Emotional-Behavioral Functioning: GBTM Results
Application of the GBTM approach for the ESI sample resulted in four groups, each with a quadratic trajectory (Supp. Table 4). We denoted Group 1 (43.8% of the population) as the ‘Best’ functioning group, having the lowest mean ESI T-scores at every age (Figure 2a). Group 2 (21.8%) was denoted as the ‘Average’ functioning group because ESI T-scores were higher than the ‘Best’ group, but within the Average range according to BASC-2 classifications. Group 3 (27.8%) was denoted as the ‘Improving’ group because their ESI T-scores showed a decreasing trend, reflecting fewer self-reported emotional concerns through adolescence. Group 4 (6.7%) was denoted as the ‘At-Risk’ group due to consistent mean ESI T-scores in the At-Risk range from ages 7 to 18. Both ‘Best’ and ‘Average’ groups, representing nearly 66% of the AMP population, had mean ESI T-scores within the Average range during follow-up. However, 63.9% of ‘Average’ youth had at least one ESI score in the At-Risk or Clinically Significant range during follow-up, as compared to only 4.7% of ‘Best’ youth.
Figure 2a. Group-Based Trajectory Modeling Plot of ESI Trajectories over age.
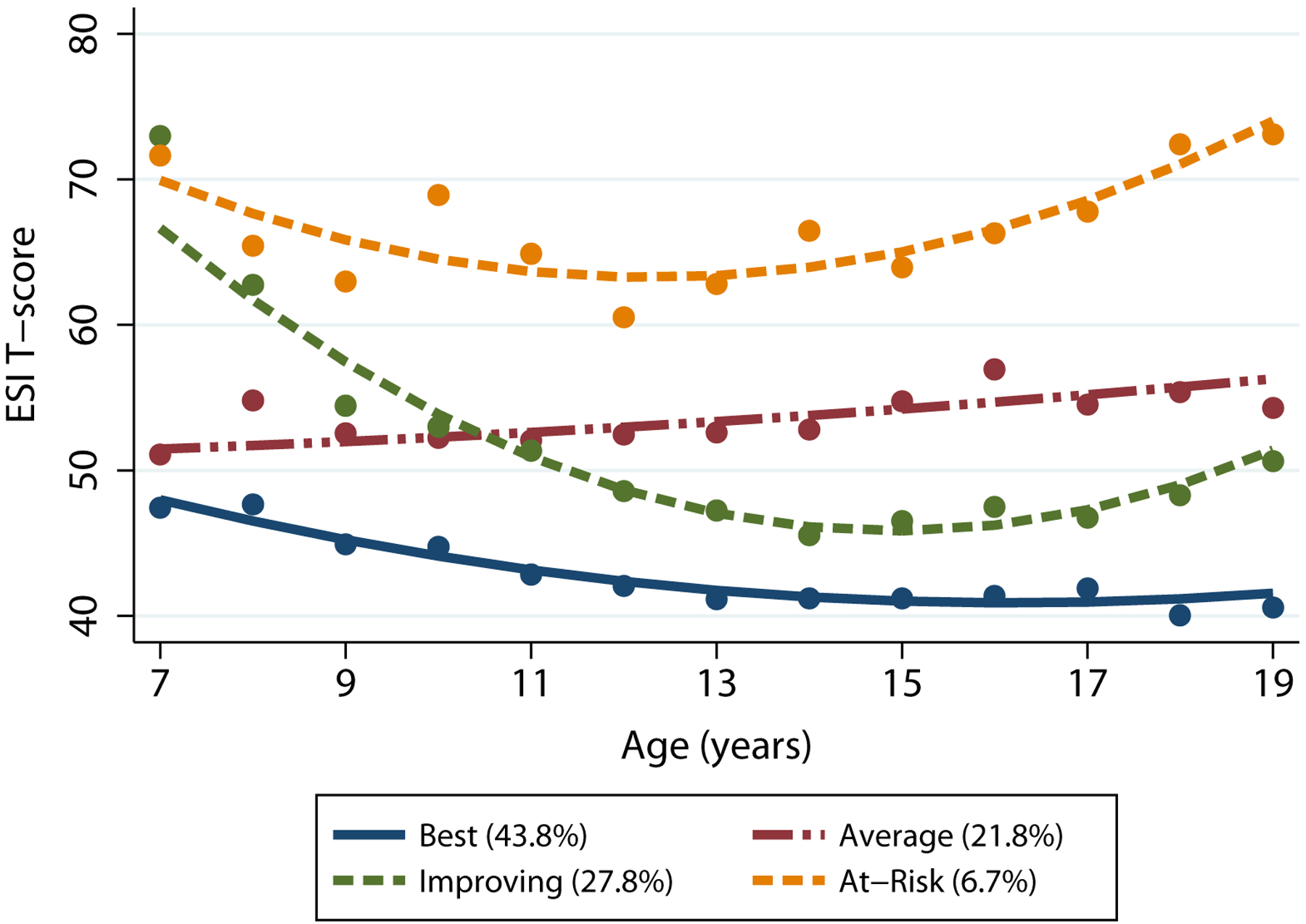
Higher ESI scores reflect worse emotional functioning (<60: Normal; 60–69: At-Risk, 70+: Clinically Significant). Points represent the observed mean score for each group at each age. Smooth curves represent fitted lines from the GBTM. Mean scores for groups 1 and 2 are considered within normal limits.
The distribution of racial/ethnic groups was relatively similar across the emotional functioning groups (Supp. Table 5). Based on multinomial logistic regression models, we found no association of racial/ethnic group or HIV status with membership in any emotional functioning group compared to the ‘Best’ group. However, males were less likely than females to be in the ‘Average’ group than the ‘Best’ group (RR 0.52; 95% CI 0.34, 0.81). After adjusting for SDOH, the lack of racial/ethnic differences remained, but youth who experienced a change in primary caregiver were nearly three times more likely to be in the ‘At-Risk’ group than the ‘Best’ group than those without a change (RR 2.85; 95% CI 1.08, 7.51) (Table 3). Youth with a married caregiver were more likely to be in the ‘Improving’ group than the ‘Best’ group (RR 1.60; 95% CI 1.05, 2.43). Youth who experienced a stressful life event vs. no stressful life event were three times more likely (RR 3.23; 95% CI 1.20, 8.68) to be in the ‘Average’ group than the ‘Best’ group. Lastly, youth whose caregiver screened positive for a psychiatric condition vs. not were more likely (RR 1.69; 95% CI 1.07, 2.68) to be in the ‘Improving’ group than the ‘Best’ group. When comparing each group to the ‘At-Risk’ group, no associations with racial/ethnic group or HIV status were observed.
Table 3.
Multinomial Analysis of Youth-reported ESI and Caregiver-reported BSI Trajectory Groups Adjusting for Social Determinants of Health
| ESI Trajectory Group (Ref = Best) | ||||
|---|---|---|---|---|
| Characteristic |
Average RR (95% CI) |
Improving RR (95% CI) |
At-Risk RR (95% CI) |
|
| Racial/ethnic Group (Ref. White non-Hispanic) | ||||
| White Hispanic | 1.48 (0.56, 3.89) | 1.47 (0.61, 3.53) | 1.00 (0.23, 4.41) | |
| Black non-Hispanic | 1.24 (0.52, 2.96) | 1.37 (0.62, 3.05) | 0.78 (0.21, 2.91) | |
| Black Hispanic | 2.20 (0.67, 7.17) | 0.94 (0.27, 3.23) | 0.54 (0.05, 5.93) | |
| YPHIV vs YPHEU | 1.32 (0.82, 2.14) | 0.96 (0.63, 1.46) | 1.56 (0.65, 3.74) | |
| Male vs Female | 0.50 (0.32, 0.79) | 1.04 (0.69, 1.55) | 0.48 (0.22, 1.06) | |
| Primary caregiver changed | 0.96 (0.46, 2.03) | 0.87 (0.43, 1.78) | 2.85 (1.08, 7.51) | |
| Married caregiver | 1.07 (0.66, 1.73) | 1.60 (1.05, 2.43) | 1.57 (0.70, 3.49) | |
| Experienced stressful life event | 3.23 (1.20, 8.68) | 1.20 (0.63, 2.28) | 0.74 (0.25, 2.17) | |
| Positive psychiatric syndrome | 1.42 (0.85, 2.35) | 1.69 (1.07, 2.68) | 1.76 (0.73, 4.20) | |
| BSI Trajectory Group (Ref = Best) | ||||
| Characteristic |
Average RR (95% CI) |
Improving RR (95% CI) |
At-Risk RR (95% CI) |
Problematic RR (95% CI) |
| Black vs White | 0.79 (0.45, 1.39) | 0.81 (0.35, 1.89) | 4.11 (0.73, 23.19) | 1.99 (0.54, 7.38) |
| Hispanic vs non-Hispanic | 0.55 (0.31, 0.98) | 0.52 (0.21, 1.26) | 0.52 (0.12, 2.31) | 2.04 (0.58, 7.15) |
| YPHIV vs YPHEU | 0.87 (0.58, 1.30) | 0.47 (0.26, 0.85) | 0.80 (0.34, 1.88) | 0.82 (0.32, 2.08) |
| Male vs Female | 0.90 (0.62, 1.31) | 1.29 (0.72, 2.29) | 1.23 (0.55, 2.76) | 0.64 (0.26, 1.56) |
| Married caregiver | 1.12 (0.75, 1.67) | 1.17 (0.63, 2.17) | 1.08 (0.45, 2.56) | 4.34 (1.72, 10.93) |
| Experienced stressful life event | 1.90 (1.03, 3.50) | 4.86 (1.12, 21.06) | 2.28 (0.51, 10.26) | 1.07 (0.28, 4.10) |
| Positive psychiatric syndrome | 2.62 (1.68, 4.10) | 1.97 (1.01, 3.83) | 2.49 (1.03, 6.04) | 6.26 (2.51, 15.63) |
RR: Relative Risk; CI: Confidence Interval; ESI: Emotional Symptoms Index; BSI: Behavioral Symptoms Index; YPHIV: Youth with perinatally-acquired HIV infection; YPHEU: Youth who are perinatally HIV-exposed but uninfected; Bold indicates statistical significance at the 0.05 level
The GBTM for the BSI sample resulted in five groups, again, each with a quadratic trajectory (Supp. Table 6). Similar to the ESI sample, we denoted Group 1 (40.3% of the population) as ‘Best’ (Figure 2b), Group 2 (38.2%) as ‘Average’, Group 3 (11.2%) as ‘Improving’, Group 4 (6.4%) as ‘At-Risk’, and Group 5 (3.9%) as ‘Problematic’. Both ‘Best’ and ‘Average’ groups, representing nearly 80% of the AMP population, had mean T-scores that were within the Average range during adolescence. However, 41.6% of ‘Average’ youth had at least one BSI score in the At-Risk or Clinically Significant range during follow-up, as compared to only 1.7% of ‘Best’ youth. The distribution of racial/ethnic groups across the behavioral functioning groups are shown in Table 2.
Figure 2b. Group-Based Trajectory Modeling Plot of BSI Trajectories over age.
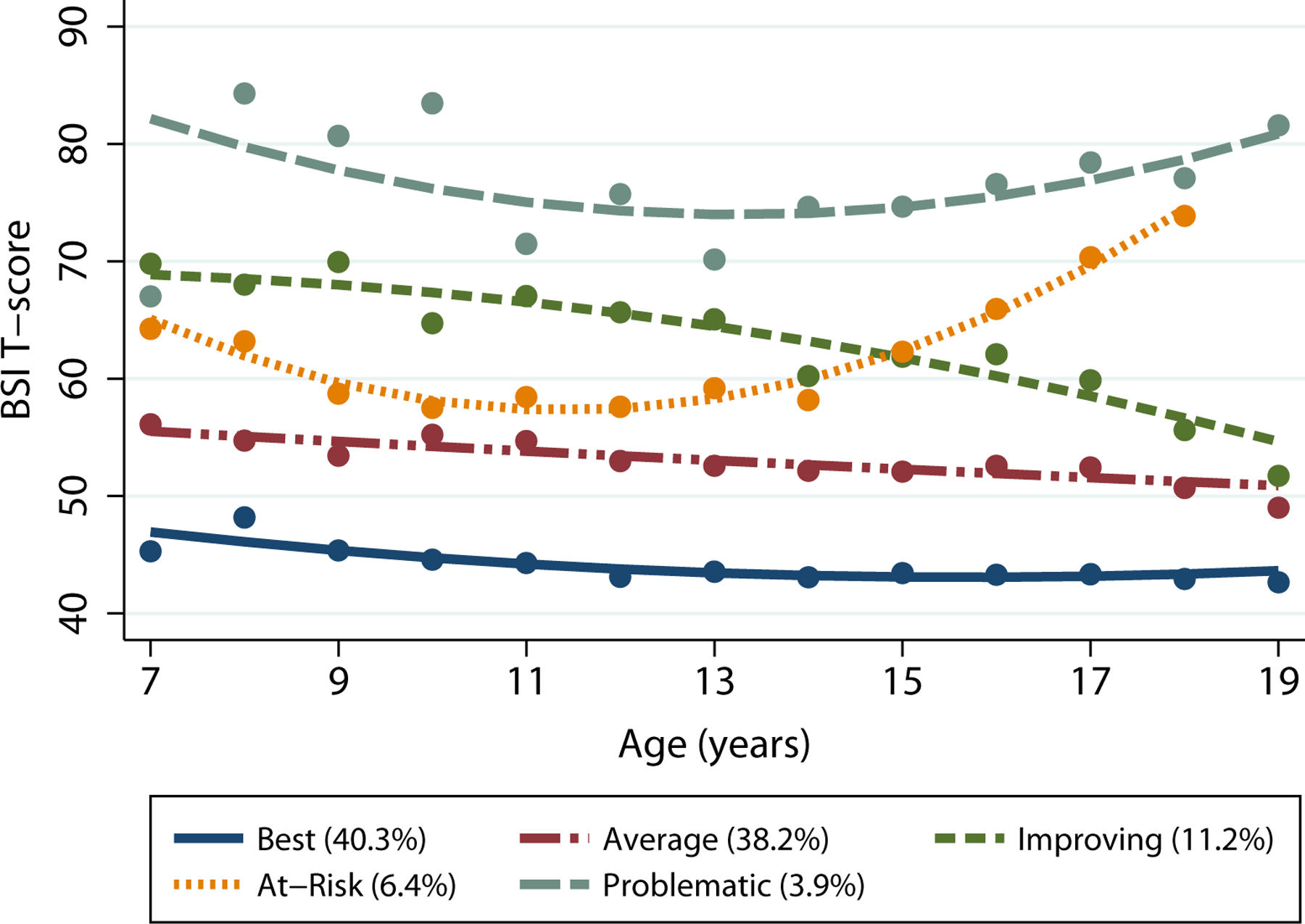
Higher BSI scores reflect worse behavioral functioning (<60: Normal; 60–69: At-Risk, 70+: Clinically Significant). Points represent the observed mean score for each group at each age. Smooth curves represent fitted lines from the GBTM. Mean scores for groups 1 and 2 are considered within normal limits.
Table 2.
Baseline Characteristics of Caregiver-reported BSI Study Population by Trajectory Group
| Trajectory Group | |||||
|---|---|---|---|---|---|
| Characteristic | Best (n=243) |
Average (n=243) |
Improving (n=62) |
At-Risk (n=28) |
Problematic (n=24) |
| Racial/ethnic Group | |||||
| White non-Hispanic | 12 (4.9%) | 21 (8.6%) | 6 (9.7%) | 2 (7.1%) | 3 (12.5%) |
| Black Hispanic | 12 (4.9%) | 10 (4.1%) | 3 (4.8%) | 3 (10.7%) | 5 (20.8%) |
| White Hispanic | 64 (26.3%) | 47 (19.3%) | 12 (19.4%) | 0 (0.0%) | 4 (16.7%) |
| Black non-Hispanic | 155 (63.8%) | 165 (67.9%) | 41 (66.1%) | 23 (82.1%) | 12 (50.0%) |
| Male vs Female | 121 (49.8%) | 114 (46.9%) | 35 (56.5%) | 15 (53.6%) | 11 (45.8%) |
| YPHIV vs YPHEU | 167 (68.7%) | 160 (65.8%) | 31 (50.0%) | 18 (64.3%) | 15 (62.5%) |
| Socioeconomic Status | |||||
| Household income ≤ $20,000 | 124 (51.0%) | 122 (50.2%) | 33 (53.2%) | 14 (50.0%) | 9 (37.5%) |
| Caregiver education <HS | 65 (26.7%) | 65 (26.7%) | 22 (35.5%) | 7 (25.0%) | 7 (29.2%) |
| Household income supports ≤ 4 people | 152 (62.6%) | 148 (60.9%) | 36 (58.1%) | 13 (46.4%) | 13 (54.2%) |
| Family Structure | |||||
| Mother born in US | 180 (74.1%) | 188 (77.4%) | 51 (82.3%) | 21 (75.0%) | 19 (79.2%) |
| Caregiver is biological mother | 89 (36.6%) | 91 (37.4%) | 24 (38.7%) | 8 (28.6%) | 7 (29.2%) |
| Primary caregiver change | 21 (8.6%) | 25 (10.3%) | 6 (9.7%) | 5 (17.9%) | 1 (4.2%) |
| Caregiver is married | 77 (31.7%) | 80 (32.9%) | 21 (33.9%) | 9 (32.1%) | 14 (58.3%) |
| Experienced stressful life event | 171 (70.4%) | 177 (72.8%) | 52 (83.9%) | 24 (85.7%) | 18 (75.0%) |
| Site location | |||||
| South | 76 (31.3%) | 85 (35.0%) | 26 (41.9%) | 17 (60.7%) | 5 (20.8%) |
| Northeast | 77 (31.7%) | 86 (35.4%) | 15 (24.2%) | 5 (17.9%) | 10 (41.7%) |
| Midwest | 34 (14.0%) | 35 (14.4%) | 8 (12.9%) | 4 (14.3%) | 6 (25.0%) |
| West | 29 (11.9%) | 19 (7.8%) | 8 (12.9%) | 1 (3.6%) | 2 (8.3%) |
| Puerto Rico | 27 (11.1%) | 18 (7.4%) | 5 (8.1%) | 1 (3.6%) | 1 (4.2%) |
| Caregiver Health | |||||
| Living with HIV | 117 (48.1%) | 117 (48.1%) | 29 (46.8%) | 9 (32.1%) | 10 (41.7%) |
| Positive CDQ screening for | |||||
| Alcohol abuse | 4 (1.6%) | 14 (5.8%) | 4 (6.5%) | 3 (10.7%) | 3 (12.5%) |
| Panic or GAD | 20 (8.2%) | 24 (9.9%) | 8 (12.9%) | 3 (10.7%) | 7 (29.2%) |
| Major or other depression | 22 (9.1%) | 25 (10.3%) | 9 (14.5%) | 6 (21.4%) | 4 (16.7%) |
| Drug abuse | 4 (1.6%) | 6 (2.5%) | 3 (4.8%) | 1 (3.6%) | 1 (4.2%) |
| Any psychiatric condition | 42 (17.3%) | 83 (34.2%) | 19 (30.6%) | 10 (35.7%) | 14 (58.3%) |
BSI: Behavioral Symptoms Index; YPHIV: Youth with perinatally-acquired HIV infection; YPHEU: Youth who are perinatally HIV-exposed but uninfected; HS: High School; CDQ: Client Diagnostic Questionnaire; GAD: Generalized Anxiety Disorder
Based on multinomial logistic regression models, we found no association between the racial/ethnic group and membership in any behavioral group relative to the ‘Best’ group. However, YPHIV were less likely than YPHEU (RR 0.47; 95% CI 0.26, 0.85) to be in the ‘Improving’ group than the ‘Best’ group. After adjusting for SDOH, these findings remained consistent (Table 3). Youth whose caregivers were married were four times more likely to be in the ‘Problematic’ group than the ‘Best’ group (RR. 4.34; 95% CI 1.72, 10.93). Youth who experienced a stressful life event were more likely to be in the ‘Average’ (RR 1.90; 95% CI 1.03, 3.50) and ‘Improving’ (RR 4.86; 95% CI 1.12, 21.06) groups than the ‘Best’ group. Lastly, youth whose caregiver screened positive for a psychiatric condition were at least twice more likely to be in each of the four other groups than the ‘Best’ group. We observed no racial/ethnic or HIV status associations when comparing any other group to the ‘Problematic’ group.
Discussion
We used two methods to assess the relationship between membership in racial/ethnic group and emotional-behavioral functioning among youth with perinatal HIV exposure. Using a mixed effects model approach that compared mean scores over time, caregivers of Black non-Hispanic YPHEU reported more behavioral concerns than caregivers of Black non-Hispanic YPHIV, White Hispanic YPHIV, and White Hispanic YPHEU, across various ages. The GBTM approach based on caregiver report identified clusters of youth with similar behavioral trajectories but did not suggest strong racial/ethnic differences given our sample size. Interestingly, neither approach demonstrated racial/ethnic differences based on youth self-report of emotional functioning. However, other factors predicted membership in vulnerable youth-reported emotional and caregiver-reported behavioral functioning groups including youth experiencing a stressful life event, living with a married caregiver, experiencing a change in caregiver, and/or having a caregiver who screened positive for a psychiatric condition.
Some studies have indicated that YPHEU, experience higher rates of mental health problems compared to YPHIV.2,4,8,11 Given their chronic health condition, YPHIV have increased access to comprehensive care than YPHEU, given YPHIV are monitored every 3–4 months for HIV-specific care, while YPHEU may be seen only annually or less often for research purposes. As a result, emotional-behavioral problems in YPHIV may be identified earlier, given increased opportunities for monitoring and referral for intervention. Our results indicated that a change in caregiver contributed to more behavioral concerns, highlighting the important role of stability in home environment. Black non-Hispanic caregivers who may experience a higher prevalence of racial discrimination, including historical negative biases, intergenerational attitudes, and beliefs, may be more likely to observe and/or express concerns about their child’s behaviors when asked.34 However, due to stigma, cultural beliefs about psychiatry and mental health, and inconsistent access to health insurance, these caregivers may also be less likely to seek professional attention for their child’s emotional-behavioral concerns.35
There are several possible reasons why we did not identify strong evidence of racial/ethnic disparities in our study. The number of White non-Hispanic and Black Hispanics was small, reducing the power to detect subtle differences for these two specific subgroups. The existing literature provides substantial evidence of a relationship between racial inequality, environmental exposures, social conditions, and child behavior.36–40 Beginning in utero and throughout early childhood, children from disadvantaged backgrounds are vulnerable to neurodevelopmental and emotional impact of environmental injustice.38,41 Longitudinal studies are needed to examine the interrelation between environmental exposures, including social conditions, on developmental and behavioral health outcomes in adolescents from minority backgrounds in substandard environments that place them at increased risk.
This study is not without limitations. Although standardized measures were administered individually in an interview format, BASC-2 assessments may be subject to biases of social desirability, recall, and the mental/emotional state of the respondent.42 BASC-2 youth self-report and caregiver evaluations do not assess identical clinical constructs, thus prohibiting direct comparison across global functioning indicators. Some of our youth were lost to follow-up. These youth may have been at higher risk for emotional-behavioral problems or greater fluctuations in emotional-behavioral functioning over time than those who remained on study. Differing ages at enrollment and loss to follow up yielded varied numbers of assessments per participant; however, there was no evidence of imbalance in the number of repeated assessments across subgroups defined by race-ethnicity and HIV status. HIV disproportionately impacts people of color, particularly Blacks and Hispanics, who comprised our study.43 Due to limited representation, other racial and ethnic groups could not be examined. Also, we did not have available a validated measure of race-based discrimination. Such measures are needed within this and similar cohort studies to better understand the impact of structural racism on health disparities.15,44 The GBTM approach yielded low counts of racial and ethnic subgroups among the ‘At-Risk’ and ‘Problematic’ functioning groups, making it challenging to identify race and ethnicity as predictors of a group membership. Thus the GBTM model has inherent limitations for handling small samples and assumptions made about missing data.31
Despite these limitations, our study findings are noteworthy. This study utilized a novel application of GBTM, illustrating developmental trajectories among one of the largest cohorts of YPHIV and YPHEU in the US. This approach revealed underlying behavioral patterns, that while not highly dependent on race or ethnicity, did differ by other youth and caregiver characteristics. We examined emotional-behavioral including multiple factors that may influence youths’ emotional-behavioral trajectory over time. This study demonstrates utility of this method in life-course epidemiology to objectively identify population trajectories and determine predictors of trajectory membership.
Additionally, our analysis included sufficient sample sizes of racial and ethnic representation of Black non-Hispanics and White Hispanics, indicating high statistical power to detect smaller differences in emotional-behavioral functioning within these groups. Rather than a snapshot of mental health problems, we described unique groups of youth following similar emotional-behavioral trajectories over time. This study also highlights that the majority of adolescents affected by PHIV are resilient with respect to their emotional-behavioral functioning, despite living with a chronic illness. For those youth with emotional-behavioral challenges, especially when persistent over time, early identification and access to targeted intervention services are necessary. Identification of SDOH that predicted vulnerable subgroups illuminates opportunities for targeted prevention and intervention services for YPHIV and YPHEU.
Supplementary Material
Acknowledgments
We thank the children and families for their participation in PHACS, and the individuals and institutions involved in the conduct of PHACS. The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development with co-funding from the National Institute on Drug Abuse, the National Institute of Allergy and Infectious Diseases, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, the National Institute on Deafness and Other Communication Disorders, the National Institute of Dental and Craniofacial Research, the National Cancer Institute, the National Institute on Alcohol Abuse and Alcoholism, the Office of AIDS Research, and the National Heart, Lung, and Blood Institute through cooperative agreements with the Harvard T.H. Chan School of Public Health (HD052102) (Principal Investigator: George R Seage III; Program Director: Liz Salomon) and the Tulane University School of Medicine (HD052104) (Principal Investigator: Russell Van Dyke; Co-Principal Investigator: Ellen Chadwick; Project Director: Patrick Davis). Data management services were provided by Frontier Science and Technology Research Foundation (PI: Suzanne Siminski), and regulatory services and logistical support were provided by Westat, Inc (PI: Julie Davidson).
The following institutions, clinical site investigators and staff participated in conducting PHACS AMP and AMP Up in 2018, in alphabetical order: Ann & Robert H. Lurie Children’s Hospital of Chicago: Ellen Chadwick, Margaret Ann Sanders, Kathleen Malee, Yoonsun Pyun; Baylor College of Medicine: William Shearer, Mary Paul, Chivon McMullen-Jackson, Mandi Speer, Lynnette Harris; Bronx Lebanon Hospital Center: Murli Purswani, Mahboobullah Mirza Baig, Alma Villegas; Children’s Diagnostic & Treatment Center: Lisa Gaye-Robinson, Sandra Navarro, Patricia Garvie; Boston Children’s Hospital: Sandra K. Burchett, Michelle E. Anderson, Adam R. Cassidy; Jacobi Medical Center: Andrew Wiznia, Marlene Burey, Ray Shaw, Raphaelle Auguste; Rutgers - New Jersey Medical School: Arry Dieudonne, Linda Bettica, Juliette Johnson, Karen Surowiec; St. Christopher’s Hospital for Children: Janet S. Chen, Maria Garcia Bulkley, Taesha White, Mitzie Grant; St. Jude Children’s Research Hospital: Katherine Knapp, Kim Allison, Megan Wilkins, Jamie Russell-Bell; San Juan Hospital/Department of Pediatrics: Midnela Acevedo-Flores, Heida Rios, Vivian Olivera; Tulane University School of Medicine: Margarita Silio, Medea Gabriel, Patricia Sirois; University of California, San Diego: Stephen A. Spector, Megan Loughran, Veronica Figueroa, Sharon Nichols; University of Colorado Denver Health Sciences Center: Elizabeth McFarland, Carrie Chambers, Emily Barr, Mary Glidden; University of Miami: Gwendolyn Scott, Grace Alvarez, Juan Caffroni, Anai Cuadra
Note: The conclusions and opinions expressed in this article are those of the authors and do not necessarily reflect those of the National Institutes of Health or US Department of Health and Human Services.
Sources of Funding:
The Pediatric HIV/AIDS Cohort Study (PHACS) was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) with co-funding from the National Institute of Dental and Craniofacial Research (NIDCR), the National Institute of Allergy and Infectious Diseases (NIAID), the National Institute of Neurological Disorders and Stroke (NINDS), the National Institute on Deafness and Other Communication Disorders (NIDCD), Office of AIDS Research (OAR), the National Institute of Mental Health (NIMH), the National Institute on Drug Abuse (NIDA), and the National Institute on Alcohol Abuse and Alcoholism (NIAAA), through cooperative agreements with the Harvard T.H. Chan School of Public Health (HD052102) and the Tulane University School of Medicine (HD052104). JRB is also supported by a grant from the National Institute of Allergy and Infectious Diseases (2T32AI007358-31). The conclusions and opinions expressed in this article are those of the authors and do not necessarily reflect those of the National Institutes of Health or US Department of Health and Human Services.
Footnotes
Conflicts of Interest: None reported.
References
- 1.Mellins CA, Malee KM. Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. J Int AIDS Soc. 2013;16(1):18593. doi: 10.7448/IAS.16.1.18593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gadow KD, Chernoff M, Williams PL, et al. Co-Occuring Psychiatric Symptoms in Children Perinatally Infected With HIV and Peer Comparison Sample: J Dev Behav Pediatr. 2010;31(2):116–128. doi: 10.1097/DBP.0b013e3181cdaa20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mellins CA, Brackis‐Cott E, Leu C-S, et al. Rates and types of psychiatric disorders in perinatally human immunodeficiency virus-infected youth and seroreverters. J Child Psychol Psychiatry. 2009;50(9):1131–1138. doi: 10.1111/j.1469-7610.2009.02069.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malee KM, Tassiopoulos K, Huo Y, et al. Mental health functioning among children and adolescents with perinatal HIV infection and perinatal HIV exposure. AIDS Care. 2011;23(12):1533–1544. doi: 10.1080/09540121.2011.575120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith R, Wilkins M. Perinatally acquired HIV infection: Long-term neuropsychological consequences and challenges ahead. Child Neuropsychol. 2015;21(2):234–268. doi: 10.1080/09297049.2014.898744 [DOI] [PubMed] [Google Scholar]
- 6.Hermetet-Lindsay KD, Correia KF, Williams PL, et al. Contributions of Disease Severity, Psychosocial Factors, and Cognition to Behavioral Functioning in US Youth Perinatally Exposed to HIV. AIDS Behav. 2017;21(9):2703–2715. doi: 10.1007/s10461-016-1508-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mellins CA, Tassiopoulos K, Malee K, et al. Behavioral Health Risks in Perinatally HIV-Exposed Youth: Co-Occurrence of Sexual and Drug Use Behavior, Mental Health Problems, and Nonadherence to Antiretroviral Treatment. AIDS Patient Care STDs. 2011;25(7):413–422. doi: 10.1089/apc.2011.0025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mellins CA, Elkington KS, Leu C-S, et al. Prevalence and change in psychiatric disorders among perinatally HIV-infected and HIV-exposed youth. AIDS Care AIDSImpact 10th Int Conf Spec Issue St Fe N M. 2012;24(8):953–962. doi: 10.1080/09540121.2012.668174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gadow KD, Angelidou K, Chernoff M, et al. Longitudinal Study of Emerging Mental Health Concerns in Youth Perinatally Infected With HIV and Peer Comparisons: J Dev Behav Pediatr. 2012;33(6):456–468. doi: 10.1097/DBP.0b013e31825b8482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chernoff M, Nachman S, Williams P, et al. Mental health treatment patterns in perinatally HIV-infected youth and controls. Pediatrics. 2009;124(2):627–636. doi: 10.1542/peds.2008-2441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith R, Huo Y, Tassiopoulos K, et al. Mental Health Diagnoses, Symptoms, and Service Utilization in US Youth with Perinatal HIV Infection or HIV Exposure. AIDS Patient Care STDs. 2019;33(1):1–13. doi: 10.1089/apc.2018.0096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abrams EJ, Mellins CA, Bucek A, et al. Behavioral Health and Adult Milestones in Young Adults With Perinatal HIV Infection or Exposure. Pediatr Evanst. 2018;142(3):e20180938-. doi: 10.1542/peds.2018-0938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Office of Disease Prevention and Health Promotion. Social Determinants of Health. Accessed October 2, 2019. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health
- 14.Kang E, Mellins CA, Ng WYK, et al. Standing between two worlds in Harlem: A developmental psychopathology perspective of perinatally acquired human immunodeficiency virus and adolescence. J Appl Dev Psychol. 2008;29(3):227–237. doi: 10.1016/j.appdev.2008.02.001 [DOI] [Google Scholar]
- 15.Williams DR, Lawrence JA, Davis BA. Racism and Health: Evidence and Needed Research. Annu Rev Public Health. 2019;40(1):105–125. doi: 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Priest N, Williams DR. Racial discrimination and racial disparities in health. In: The Oxford Handbook of Stigma, Discrimination, and Health. Major B, Dovidio JF, & Link BG (Eds.), Oxford library of psychology. Oxford University Press; 2018:163–182. [Google Scholar]
- 17.Yearby R Racial Disparities in Health Status and Access to Healthcare: The Continuation of Inequality in the United States Due to Structural Racism: Continuing Racial Health Disparities. Am J Econ Sociol. 2018;77(3–4):1113–1152. doi: 10.1111/ajes.12230 [DOI] [Google Scholar]
- 18.Tassiopoulos K, Patel K, Alperen J, et al. Following young people with perinatal HIV infection from adolescence into adulthood: the protocol for PHACS AMP Up, a prospective cohort study. BMJ Open. 2016;6(6):e011396. doi: 10.1136/bmjopen-2016-011396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alegría M, Green JG, McLaughlin KA, et al. Disparities in child and adolescent mental health and mental health services in the U.S. Published online 2015:26. [Google Scholar]
- 20.Marrast L, Himmelstein DU, Woolhandler S. Racial and Ethnic Disparities in Mental Health Care for Children and Young Adults: A National Study. Int J Health Serv. 2016;46(4):810–824. doi: 10.1177/0020731416662736 [DOI] [PubMed] [Google Scholar]
- 21.Nguyen N, Choi CJ, Robbins R, et al. Psychiatric trajectories across adolescence in perinatally HIV-exposed youth: the role of HIV infection and associations with viral load. AIDS. Published online April 13, 2020. doi: 10.1097/QAD.0000000000002529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychol Bull. 1987;101(2):213–232. doi: 10.1037/0033-2909.101.2.213 [DOI] [PubMed] [Google Scholar]
- 23.De Los Reyes A, Augenstein TM, Wang M, et al. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull. 2015;141(4):858–900. doi: 10.1037/a0038498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds CR, Kamphaus RW. BASC-2: Behavior Assessment System for Children. Published online 2004.
- 25.Gortmaker SL, Lenderking WR, Clark C, et al. Development and use of a pediatric quality of life questionnaire in AIDS clinical trials: Reliability and validity of the General Health Assessment for Children. In: Measuring Health-Related Quality of Life in Children and Adolescents: Implications for Research and Practice. Mahwah, NJ: Lawrence Erlbaum Associates Publishers, 219–235. [Google Scholar]
- 26.Aidala A, Havens J, Mellins CA, et al. Development and validation of the Client Diagnostic Questionnaire (CDQ): A mental health screening tool for use in HIV/AIDS service settings. Psychol Health Med. 2004;9(3):362–380. [Google Scholar]
- 27.Mellins CA, Kang E, Leu C-S, et al. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care STDs. 2003;17(8):407–416. doi: 10.1089/108729103322277420 [DOI] [PubMed] [Google Scholar]
- 28.Littell RC, Milliken GA, Stroup WW, et al. SAS for Mixed Models. 2nd ed. SAS Institute, Inc; 2006. [Google Scholar]
- 29.Venables WN, Ripley BD. Modern Applied Statistics with S-PLUS. 4th ed. Springer Science & Business Media; 2013. [Google Scholar]
- 30.Diggle PJ, Tawn JA, Moyeed RA. Model-based geostatistics. J R Stat Soc Ser C Appl Stat. 1998;47(3):299–350. [Google Scholar]
- 31.Nagin DS. Group-Based Modeling of Development. Harvard University Press; 2005. [Google Scholar]
- 32.Jones BL, Nagin DS, Roeder K. A SAS Procedure Based on Mixture Models for Estimating Developmental Trajectories. Sociol Methods Res. 2001;29(3):374–393. doi: 10.1177/0049124101029003005 [DOI] [Google Scholar]
- 33.Siberry GK, Leister E, Jacobson DL, et al. Increased risk of asthma and atopic dermatitis in perinatally HIV-infected children and adolescents. Clin Immunol. 2012;142(2):201–208. doi: 10.1016/j.clim.2011.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kang S, Harvey EA. Racial Differences Between Black Parents’ and White Teachers’ Perceptions of Attention-Deficit/Hyperactivity Disorder Behavior. J Abnorm Child Psychol. 2019;48(5):661–672. doi: 10.1007/s10802-019-00600-y [DOI] [PubMed] [Google Scholar]
- 35.Burgess DJ, Ding Y, Hargreaves M, et al. The Association between Perceived Discrimination and Underutilization of Needed Medical and Mental Health Care in a Multi-Ethnic Community Sample. J Health Care Poor Underserved. 2008;19(3):894–911. doi: 10.1353/hpu.0.0063 [DOI] [PubMed] [Google Scholar]
- 36.Gee GC, Payne-Sturges DC. Environmental Health Disparities: A Framework Integrating Psychosocial and Environmental Concepts. Environ Health Perspect. 2004;112(17):1645–1653. doi: 10.1289/ehp.7074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Landrigan PJ, Rauh VA, Galvez MP. Environmental Justice and the Health of Children. Mt Sinai J Med J Transl Pers Med. 2010;77(2):178–187. doi: 10.1002/msj.20173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rauh VA, Margolis AE. Research Review: Environmental exposures, neurodevelopment, and child mental health – new paradigms for the study of brain and behavioral effects. J Child Psychol Psychiatry. 2016;57(7):775–793. doi: 10.1111/jcpp.12537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grandjean P, Landrigan PJ. Developmental neurotoxicity of industrial chemicals. The Lancet. 2006;368(9553):2167–2178. doi: 10.1016/S0140-6736(06)69665-7 [DOI] [PubMed] [Google Scholar]
- 40.Grandjean P, Landrigan PJ. Neurobehavioural effects of developmental toxicity. Lancet Neurol. 2014;13(3):330–338. doi: 10.1016/S1474-4422(13)70278-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grandjean P Only One Chance: How Environmental Pollution Impairs Brain Development -- and How to Protect the Brains of the Next Generation. Oxford University Press, Oxford University Press, Incorporated; 2013. doi: 10.1093/acprof:oso/9780199985388.001.0001 [DOI] [Google Scholar]
- 42.Najman JM, Williams GM, Nikles J, et al. Bias influencing maternal reports of child behaviour and emotional state. Soc Psychiatry Psychiatr Epidemiol. 2001;36(4):186–194. doi: 10.1007/s001270170062 [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2018. (Preliminary). HIV Surveill Rep. Published online 2019:30. [Google Scholar]
- 44.Krieger N Methods for the Scientific Study of Discrimination and Health: An Ecosocial Approach. Am J Public Health 1971. 2012;102(5):936–945. doi: 10.2105/AJPH.2011.300544 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


