Abstract
This study identified a shared pathophysiological mechanism of pediatric anxiety and irritability. Clinically, anxiety and irritability are common, co-occurring problems, both characterized by high-arousal negative affective states. Behaviorally, anxiety and irritability are associated with aberrant threat processing. To build on these findings, we examined eye-tracking measures of attention bias in relation to the unique and shared features of anxiety and irritability in a transdiagnostic sample of youth (n=97, 58% female, Mage=13.03, SDage=2.82). We measured attention bias to negative versus non-negative emotional faces during a passive viewing task. We employed bifactor analysis to parse the unique and shared variance of anxiety and irritability symptoms from self- and parent-report questionnaires. Negative affectivity is the derived latent factor reflecting shared variance of anxiety and irritability. We found that higher negative affectivity was associated with looking longer at negative versus non-negative faces, reflecting a shared mechanism of anxiety and irritability. This finding suggests that modification of elevated attention to negative emotional faces may represent a common potential treatment target of anxiety and irritability.
Keywords: Anxiety, attention bias, eye-tracking, irritability, negative affectivity
Introduction
Anxiety and irritability are highly common (Brotman et al., 2017; LeDoux and Pine, 2016; Merikangas et al., 2010) and often comorbid (Cornacchio et al., 2016; Shimshoni et al., 2020; Stoddard et al., 2014). Both anxiety and irritability are characterized by high-arousal negative affective states (Kircanski et al., 2018; Rothbart, 2007; Watson and Clark, 1984) and aberrant threat processing (Brotman et al., 2017; Kircanski et al., 2018; LeDoux and Pine, 2016). Specifically, behavioral and neuroimaging tasks indicate that anxiety and irritability are both associated with an attention bias towards threatening stimuli, such as negative faces (Dudeney et al., 2015; Hommer et al., 2014). Studying anxiety and irritability using dimensional methods is essential to probe more precise pathophysiological targets for treatment and prevention. Here, we examined if attention bias relates to unique and shared features of anxiety and irritability in a transdiagnostic sample of youth.
One way of parsing unique and shared features of psychopathology is using bifactor analysis. Bifactor analysis is a type of latent variable analysis in which observed data is used to estimate underlying constructs (Flagel et al., 2016; Friston et al., 2017; Kircanski et al., 2018). It is well-suited to handle correlated data, such as anxiety and irritability (Kircanski et al., 2018). Bifactor analysis parses such correlated data (e.g. anxiety and irritability) in a shared or overarching latent variable (e.g., “negative affectivity”), and unique, orthogonal latent variables (e.g., “anxiety”, “parent-reported irritability”, and “child-reported irritability”) (Cardinale et al., 2019; Kircanski et al., 2018). This approach provides the opportunity to disentangle unique and shared mechanisms underlying anxiety and irritability by testing if behavioral and neural measures are related to the shared negative affectivity latent variable or the unique latent variables. While negative affectivity was related to behavioral measures of attention bias, unique anxiety and irritability latent variables were related to differential neural correlates of attention bias (Kircanski et al., 2018).
Attention bias towards threat, or focusing attention on threatening stimuli, is associated with both anxiety and irritability. Attention bias towards threat is typically measured with tasks using reaction times (RT) to respond to probes appearing after negative versus non-negative faces, such as in the dot-probe task. However, eye-tracking tasks provide more reliable and direct measures of attention bias than RT-based paradigms (Lisk et al., 2020). In one free-viewing eye-tracking task, participants look at matrices consisting of negative and non-negative faces. In this paradigm, socially anxious adults gazed longer at negative than non-negative faces than non-anxious controls (Lazarov et al., 2016). Similarly, children with anxiety disorders (AD), compared to healthy controls, looked longer at negative faces versus non-negative faces (Abend et al., 2020). Here, we examined eye-tracking measures of attention bias in relation to the unique and shared features of anxiety and irritability in a transdiagnostic sample of youth. Since negative affectivity is related to behavioral measures of attention bias variability (Kircanski et al., 2018), we hypothesized that attention bias towards negative faces as measured with eye-tracking would be associated with negative affectivity, representing a shared mechanism of anxiety and irritability.
Methods
Participants
Ninety-seven youth between 8 and 17 years (58% female, Mage=13.03, SDage=2.82; Table 1) were recruited from the community to participate in studies of pediatric psychopathology at the National Institute of Mental Health (NIMH). This transdiagnostic sample was enriched for symptoms of anxiety and irritability to provide a wide range of symptom severity. Primary diagnoses included: AD, attention-deficit/hyperactivity disorder (ADHD), disruptive mood dysregulation disorder (DMDD), and oppositional defiant disorder (ODD) (n=68 with Axis-I disorder). We included 29 healthy controls without any present or lifetime psychiatric diagnoses. Masters and doctoral-level clinicians administered the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (Kaufman et al., 1997) with the DMDD module (Wiggins et al., 2016) and primary diagnosis was confirmed in a clinical consensus meeting. 13 youth were on psychotropic medication1. Youth and their parents provided written informed assent and consent, respectively, after the nature of the procedures had been fully explained. Study procedures were approved by the Institutional Review Board of the NIMH and were in accordance with the Declaration of Helsinki. Data of 27 youth with AD and 13 healthy controls were included in (Abend et al., 2020).
Table 1.
Descriptive statistics of the transdiagnostic sample.
| Mean | SD | Min | Max | |
|---|---|---|---|---|
| Age | 13.03 | 2.82 | 8.24 | 17.97 |
| IQ | 112.53 | 12.88 | 77 | 143 |
| ARI child | 2.82 | 2.89 | 0 | 11 |
| ARI parent | 3.2 | 3.01 | 0 | 10 |
| SCARED child | 21.24 | 15.83 | 0 | 55 |
| SCARED parent | 19.25 | 14.69 | 0 | 54 |
| Primary diagnosis | n (% female) | Mage | SDage | |
| AD | 45 (60%) | 13.13 | 2.84 | |
| ADHD | 8 (25%) | 12.89 | 1.60 | |
| DMDD | 14 (71%) | 12.59 | 2.83 | |
| ODD | 1 (100%) | 11.89 | ||
| HC | 29 (55%) | 13.18 | 3.19 |
Note: ARI = Affective Reactivity Index; SCARED = Screen for Child Anxiety Related Emotional Disorders; AD = anxiety disorders; ADHD = attention-deficit/hyperactivity disorder; DMDD = disruptive mood dysregulation disorder; ODD = oppositional defiant disorder; HC = healthy control.
Bifactor modeling of behavioral data
The Screen for Child Anxiety Related Emotional Disorders (SCARED; (Birmaher et al., 1997)) was used to assess anxiety and the Affective Reactivity Index (ARI; (Stringaris et al., 2012)) was used to assess irritability. All youth and their parents completed these measures within 3 months of testing.
We used a bifactor analysis on these questionnaires to parse shared versus unique variance of anxiety and irritability (Cardinale et al., 2019; Kircanski et al., 2018). We combined questionnaire data of the current sample (n=97) with a large transdiagnostic sample of youth (n=331, 54.08% female, Mage=13.57, SDage=2.69) (Cardinale et al., 2019) to obtain a larger sample. Eight participants from the current sample were already included in the (Cardinale et al., 2019) dataset. The bifactor model included six child-report and six parent-report ARI items (categorical), and five child-report and five parent-report SCARED subscales (continuous). ARI data were missing for 1 participant. All items were indicators of a ‘negative affectivity’ latent factor. Additionally, all SCARED subscales were modeled by an anxiety latent factor, all self-report ARI items were modeled by an irritability-child latent factor, and all parent-report ARI items were modeled by an irritability-parent latent factor (Figure 1). The analysis included separate irritability-child and irritability-parent factor scores, as previous studies (Cardinale et al., 2019; Kircanski et al., 2018) showed that this fits the data better than including one irritability factor score.
Figure 1.
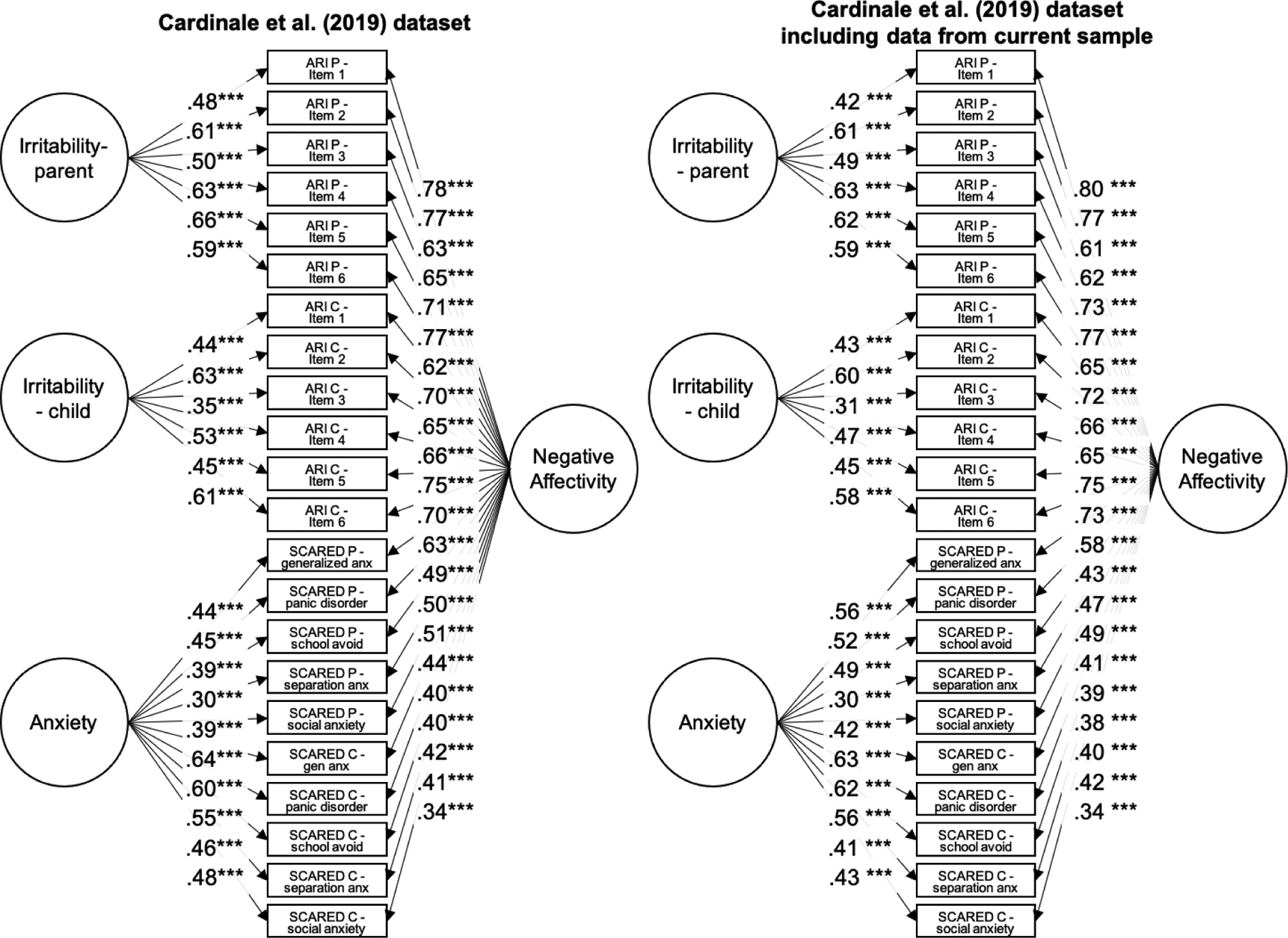
Factor loadings for the bifactor model from the (Cardinale et al., 2019) dataset with and without data from the current sample. Adapted from (Cardinale et al., 2019).
Note: ARI P = parent-reported Affective Reactivity Index; ARI Y = child-reported Affective Reactivity Index; SCARED P = parent-reported Screen for Child Anxiety Related Emotional Disorders; SCARED C = child-reported Screen for Child Anxiety Related Emotional Disorders; It. = item; Gen. = generalized anxiety; Pan. = panic disorder; Sch. = school avoidance; Sep. = separation anxiety; Soc. = social anxiety.
We used the weighted least square mean and variance adjusted estimator because categorical variables were included. All analyses were run with Mplus Version 8.4. As the fit statistics (Supplementary Table 1) and factor loadings (Figure 1) were very similar between the (Cardinale et al., 2019) dataset (n=331) and the dataset including the current sample (n=420), we used the latent factor scores in the subsequent analyses. The distribution of the latent factor scores was very similar in the full dataset (n=420) and in the current sample (n=97; Supplementary figure 1). Correlations between the derived factor scores and raw questionnaire data from are shown in Supplementary Table 2. The omega for the bifactor model as a whole was 0.93, and the hierarchical omega for the negative affectivity factor was 0.642.
Eye-tracking task
We used the eye-tracking task and analysis from (Abend et al., 2020) (Figure 2). Internal consistency (Cronbach’s alphas >0.89) and one-week test-retest reliability (rs>0.62) have been reported for this task in adults (Lazarov et al., 2016). Participants observed matrices with 4×4 faces in three conditions with breaks in between: Happy-Angry, Happy-Sad, and Neutral-Disgust. Half of the actors in each matrix presented the negative expression and half presented the non-negative expression. Images were taken from the NimStim stimulus set (Tottenham et al., 2009). Participants were instructed to look at the faces however they liked. Each trial began with a fixation cross presented until the eye-tracker registered a 1000 ms fixation on the fixation cross, to ensure that participants’ eye-gaze began in the center of the matrix. Following this fixation, a matrix (900×900 pixels) was presented for 6000 ms, followed by an inter-trial interval of 2000 ms. The presentation of the matrices and conditions was randomized. Overall, each condition lasted approximately 8–10 minutes, for a total task duration of around 45 minutes to include calibration and breaks.
Figure 2.
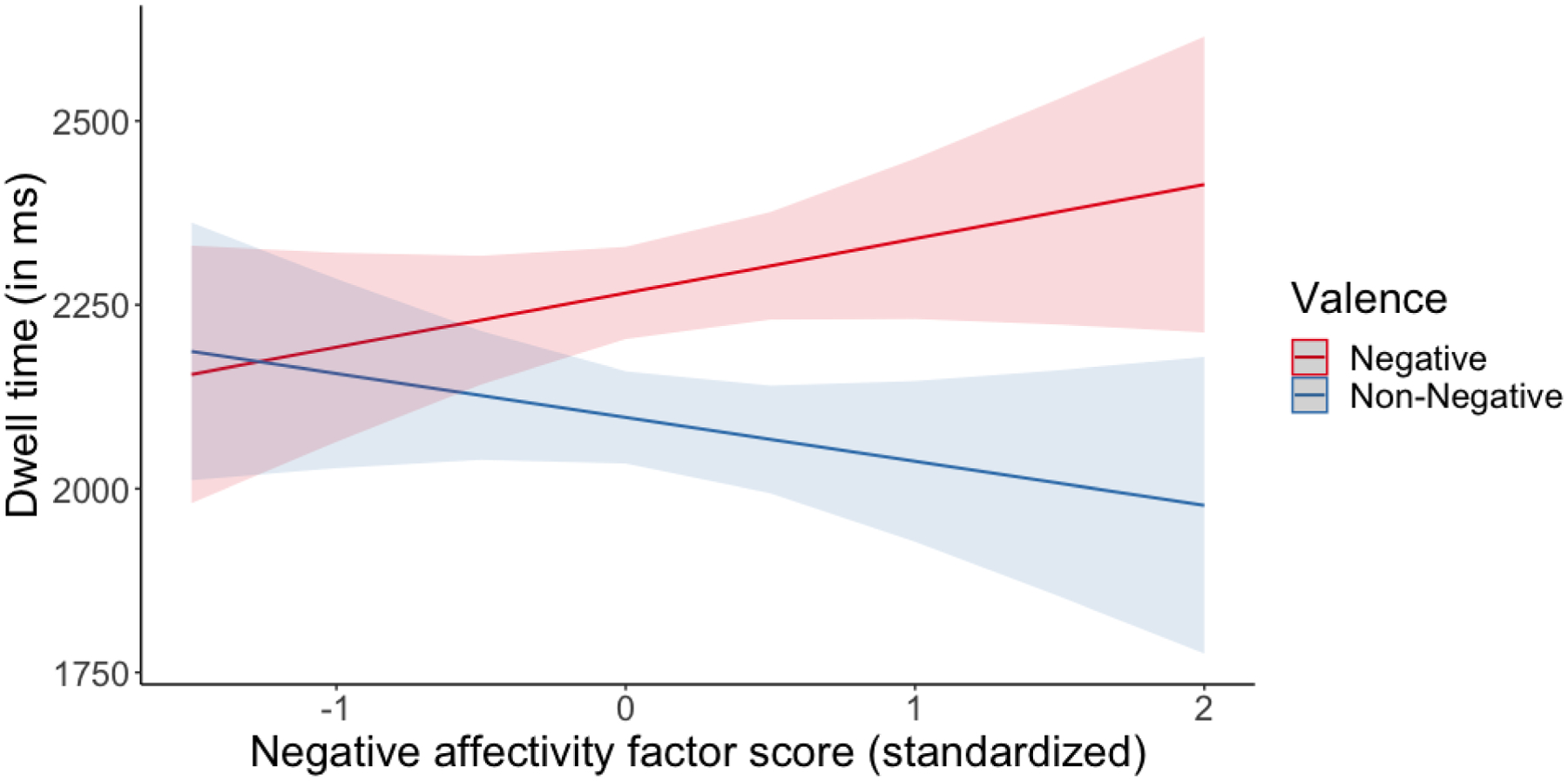
Interaction between negative affectivity factor score and valence on trial-level dwell time (in ms).
Note: Shaded areas represent standard error. Example of a matrix with neutral and disgust faces (adapted from (Abend et al., 2020)). Of note, actual task stimuli utilized the NimStim stimulus set (Tottenham et al., 2009); due to copyright restrictions, stimuli from a different set are shown here for illustrative purposes only. Red and blue boxes around the face stimuli are used to indicate the areas of interest (i.e., negative versus non-negative faces) in the analysis, but the colored boxes were not displayed during the task itself.
Eye-tracking data acquisition and processing
All participants completed the task in the same experimental room with identical lighting. They sat at approximately 52 cm from the desktop mounted eye-tracking camera (EyeLink 1000 Plus eye-tracking camera, SR-research, Ottawa, Ontario, Canada; screen: 47.5 × 27 cm). Real-time binocular eye-tracking data were collected continuously during the task with a 25 mm lens at a 1000 Hz sampling rate, with a 192×1080-pixel display resolution. Before each conditions of the task, we performed a 5-point calibration and a 5-point validation. This calibration procedure was repeated if the average deviation from the calibration was more than 0.5 degrees during the validation or if the maximum error on any of the 5 points was greater than 1 degree. While 97 participants completed the task overall, some participants completed only one (n=15) or two (n=21) task blocks. Data was not recorded on all trials, so the number of trials included in the analysis varied per participant per condition (Supplementary Table 3). The number of trials included in the analysis did not correlate with any of the factor scores (negative affectivity, irritability-parent, irritability-child, anxiety), −0.14 < rs < 0.11, ps > 0.24, and the factor scores did not differ between participants with data from 1, 2, and 3 blocks, Fs > 0.25, ps>0.05.
Eye-tracking data were processed using EyeLink DataViewer software (SR-research, Ottawa, Ontario, Canada; Supplementary Methods). Fixations were defined as at least 100 ms of stable fixation. We defined two areas of interest (AOIs) per matrix: one including the eight faces with a negative expression (anger, disgust, or sad) and one including the eight faces with a non-negative expression (neutral or happy). Total dwell time on negative and non-negative faces was computed as the sum of fixation durations per AOI. Unlike (Abend et al., 2020), we used trial-level data in the group analysis. We also calculated the percentage of time spent on negative faces per trial, computed as total dwell time on negative faces divided by total dwell time on both negative and non-negative faces.
Analysis
To investigate the relation between attention bias to negative faces and negative affectivity, anxiety, irritability-parent, and irritability-child latent factor scores, we ran a linear mixed-effects model in R (nlme package 3.1–139; (Pinheiro et al., 2020)). The following independent variables were included: condition (Happy-Angry, Neutral-Disgust, Sad-Happy), valence (negative, non-negative), negative affectivity factor score, irritability-parent factor score, irritability-child factor score, anxiety factor score, condition-by-valence interaction, and the factor score-by-condition-by-valence interactions. Trial-level dwell time was included as dependent variable, and subject was modeled as random effect. Alpha was set at 0.05. Follow-up analysis for significant interactions were conducted using testInteractions (phia package 0.2–1; (De Rosario-Marinez et al., 2015)) for interactions with only categorical variables and emtrends (emmeans package 1.5.2–1; (Lenth et al., 2020)) for interactions including continuous variables. We repeated the analysis with percentage of time spent on negative faces as dependent variable, including the same independent variables (except valence and its interactions), and subject as random effect.
Results
Complete results of the linear mixed-effects model are reported in Table 2 (variance inflation factors (VIFs) are presented in Supplementary Table 4). The interaction between condition and valence, F(2,13502)=21.68, p<0.001, showed that all children looked longer at negative compared to non-negative faces in Happy-Angry versus Sad-Happy conditions (b=223.79ms, p<0.001), but not in Happy-Angry versus Neutral-Disgust conditions (b=0.14ms, p>0.99; Supplementary Figure 2). Follow-up tests for the interaction between condition and valence confirmed that all children looked longer at negative compared to non-negative faces in the Happy-Angry condition compared to the Sad-Happy condition, X2(1)=38.34, p<0.001, and in the Neutral-Disgust condition compared to the Sad-Happy condition, X2(1)=32.71, p<0.001, whereas there was no difference between the Happy-Angry and Neutral-Disgust conditions, X2(1)=12.22, p=0.758 (Supplementary Figure 2).
Table 2.
Results of the type-III/marginal F-tests on the linear mixed-effects model.
| numDF | denDF | F-value | p-value | |
|---|---|---|---|---|
| Intercept | 1 | 13502 | 4877.69 | < 0.001 |
| Condition | 2 | 13502 | 8.58 | < 0.001 |
| Valence | 1 | 13502 | 36.76 | < 0.001 |
| NA factor score | 1 | 92 | 2.03 | 0.158 |
| IRR-P factor score | 1 | 92 | 2.00 | 0.161 |
| IRR-C factor score | 1 | 92 | 0.14 | 0.711 |
| ANX factor score | 1 | 92 | 0.00 | 0.999 |
| Condition X Valence | 2 | 13502 | 21.68 | < 0.001 |
| Condition X NA factor score | 2 | 13502 | 0.53 | 0.587 |
| Valence X NA factor score | 1 | 13502 | 8.93 | 0.003 |
| Condition X IRR-P factor score | 2 | 13502 | 0.75 | 0.475 |
| Valence: X IRR-P factor score | 1 | 13502 | 0.82 | 0.365 |
| Condition X IRR-C factor score | 2 | 13502 | 0.64 | 0.529 |
| Valence X IRR-C factor score | l | 13502 | 0.02 | 0.889 |
| Condition X ANX factor score | 2 | 13502 | 0.85 | 0.429 |
| Valence X ANX factor score | 1 | 13502 | 0.09 | 0.769 |
| Condition X Valence X NA factor score | 2 | 13502 | 0.94 | 0.393 |
| Condition X Valence X IRR-P factor score | 2 | 13502 | 0.31 | 0.735 |
| Condition X Valence X IRR-C factor score | 2 | 13502 | 1.26 | 0.284 |
| Condition X Valence X ANX factor score | 2 | 13502 | 0.38 | 0.685 |
Marginal R2=0.011 (only fixed effects), conditional R2=0.074 (including random effects) Note: numDF = numerator degrees of freedom; denDF = denominator degrees of freedom; NA = negative affectivity; IRR-P = irritability-parent; IRR-C = irritability-child; ANX = anxiety
Higher negative affectivity factor scores were related to looking longer at negative faces compared to non-negative faces (Figure 2), as indicated by an interaction between valence and negative affectivity factor scores, F(1,13502)=8.93, b=−133.56ms, p=0.003. Follow-up tests revealed that the simple slopes were not significantly different from zero for negative faces (b=76.6ms, 95% CI: −12.4–165.6) and non-negative faces (b=−34.9ms, 95% CI: −123.9–54.1). We repeated the analysis with percentage of time spent on negative faces as dependent variable (Supplementary Results). The main effect of negative affectivity indicated similar findings as the main analysis, F(1,92)=3.10, b=1.53%, p=0.082.
Discussion
This study examined eye-tracking measures of attention bias in relation to the unique and shared features of anxiety and irritability in a transdiagnostic youth sample. Unique and shared features of anxiety and irritability were parsed with bifactor analysis, and eye-tracking measures of attention bias were assessed in a passive viewing task with negative and non-negative faces. Negative affectivity is the derived latent factor reflecting shared variance of anxiety and irritability, based on self- and parent-report measures. We found that higher negative affectivity was associated with looking longer at negative (i.e., angry, sad, disgust) compared to non-negative (i.e., happy, neutral) faces, representing a potential shared mechanism of anxiety and irritability.
The bifactor analysis provides the opportunity to parse unique and shared features of anxiety and irritability. Our finding demonstrates that attention bias might be a more general, transdiagnostic process, and not uniquely related to either anxiety or irritability. We extended the findings from Abend et al. (2020) by suggesting that the attention bias found in children with anxiety disorders might be related to higher negative affectivity. Our finding is consistent with studies demonstrating that both anxiety and irritability are related to attention bias towards negative faces (Dudeney et al., 2015; Hommer et al., 2014) and aberrant threat processing more generally (Brotman et al., 2017; Kircanski et al., 2018; LeDoux and Pine, 2016). Indeed, another study using the bifactor approach also found that negative affectivity was related to attention bias variability as measured with the dot-probe task (Kircanski et al., 2018), which focuses on attention orienting by using shorter trials than the current task.
Our finding could have treatment implications. For example, preliminary research has shown that training children with AD to look at non-negative instead of negative faces reduced clinician- and parent-reported anxiety symptoms (Linetzky et al., 2019). Our findings suggest that this therapy might also be helpful for youth with both anxiety and irritability symptoms.
A few limitations should be noted. First, factor loadings on the irritability-child latent factor were not strong, consistent with previous studies (Cardinale et al., 2019; Kircanski et al., 2018). Second, not all participants completed all conditions of the eye-tracking task. Although linear mixed-effects models account for missing data, this could have influenced the results. Third, we complemented our data with an existing dataset to run a bifactor analysis. However, fit statistics, factor loadings, and distributions of the latent factor scores of our analysis were very similar to those from the (Cardinale et al., 2019) analysis. Fourth, even though VIFs were below 10, some were above 5 for the higher-order interactions. This could indicate standard error inflation, so caution in interpreting these interactions is warranted. Future work should replicate this finding in a larger, more clinically diverse sample. Further, future longitudinal research should clarify whether attention bias is a precursor or a consequence of psychopathology.
To summarize, anxiety and irritability are common in youth and often co-occur (Cornacchio et al., 2016; Shimshoni et al., 2020; Stoddard et al., 2014). However, few studies examine unique and shared features of anxiety and irritability. Our data showed that that higher negative affectivity was associated with looking longer at negative compared to non-negative faces, representing a potential shared mechanism of anxiety and irritability. This might indicate that treatment focused on reducing attention bias to threat might be helpful for youth with both anxiety and irritability symptoms.
Supplementary Material
Highlights.
We studied attention bias as unique or shared mechanisms of anxiety and irritability.
We measured attention bias using eye-tracking in a transdiagnostic youth sample.
Negative affectivity is a bifactor-derived common factor of anxiety and irritability.
Negative affectivity was related to looking longer at negative vs non-negative faces.
This finding might reflect a shared mechanism of anxiety and irritability.
Acknowledgments
This work was supported by the Intramural Research Program at the National Institute of Mental Health, National Institutes of Health (ZIAMH002969 01 for M.A. Brotman and ZIAMH002782 and NCT00018057 for D.S. Pine).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
Declaration of Interest: None
We re-ran the analysis controlling for psychotropic medication use and the results remained the same.
Hierarchical omega was 0.50 for the anxiety factor score, 0.36 for parent-reported irritability, and 0.30 for self-reported irritability. Omegas were estimated using theta parameterization.
References
- Abend R, Bajaj MA, Matsumoto C, Yetter M, Harrewijn A, Cardinale EM, Kircanski K, Lebowitz ER, Silverman WK, Bar-Haim Y, Lazarov A, Leibenluft E, Brotman MA, Pine DS, 2020. Converging multi-modal evidence for implicit threat-related biases in pediatric anxiety disorders. Journal of Abnormal Child Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM, 1997. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatr 36(4), 545–553. [DOI] [PubMed] [Google Scholar]
- Brotman MA, Kircanski K, Stringaris A, Pine DS, Leibenluft E, 2017. Irritability in youths: A translational model. American Journal of Psychiatry 174(6), 520–532. [DOI] [PubMed] [Google Scholar]
- Cardinale EM, Kircanski K, Brooks J, Gold AL, Towbin KE, Pine DS, Leibenluft E, Brotman MA, 2019. Parsing neurodevelopmental features of irritability and anxiety: Replication and validation of a latent variable approach. Development and Psychopathology, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornacchio D, Crum KI, Coxe S, Pincus DB, Corner JS, 2016. Irritability and severity of anxious symptomatology among youth with anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatr 55(1), 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Rosario-Marinez H, Fox J, CoreTeam, 2015. phia: Post-Hoc Interaction Analysis (R package version 0.2–1).
- Dudeney J, Sharpe L, Hunt C, 2015. Attentional bias towards threatening stimuli in children with anxiety: A meta-analysis. Clinical Psychology Review 40, 66–75. [DOI] [PubMed] [Google Scholar]
- Flagel SB, Pine DS, Ahmari SE, First MB, Friston KJ, Mathys C, Redish AD, Schmack K, Smoller JW, Thapar A, 2016. A novel framework for improving psychiatric diagnostic nosology, in: Redish AD, Gordon JA (Eds.), Computational Psychiatry: New Perspectives on Mental Illness. Mit Press, Cambridge, pp. 169–199. [Google Scholar]
- Friston KJ, Redish AD, A., G.J., 2017. Computational nosology and precision psychiatry. Computational Psychiatry 1, 2–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hommer RE, Meyer A, Stoddard J, Connolly ME, Mogg K, Bradley BP, Pine DS, Leibenluft E, Brotman MA, 2014. Attention bias to threat faces in severe mood dysregulation. Depress. Anxiety 31(7), 559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N, 1997. Schedule for Affective Disorders and Schizophrenia for School-Age Children Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatr 36(7), 980–988. [DOI] [PubMed] [Google Scholar]
- Kircanski K, White LK, Tseng WL, Wiggins JL, Frank HR, Sequeira S, Zhang S, Abend R, Towbin KE, Stringaris A, Pine DS, Leibenluft E, Brotman MA, 2018. A latent variable approach to differentiating neural mechanisms of irritability and anxiety in youth. JAMA Psychiatry 75(6), 631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarov A, Abend R, Bar-Haim Y, 2016. Social anxiety is related to increased dwell time on socially threatening faces. Journal of Affective Disorders 193, 282–288. [DOI] [PubMed] [Google Scholar]
- LeDoux JE, Pine DS, 2016. Using neuroscience to help understand fear and anxiety: A two-system framework. American Journal of Psychiatry 173(11), 1083–1093. [DOI] [PubMed] [Google Scholar]
- Lenth R, Buerkner P, Herve M, Love J, Riebl H, Singmann H, 2020. emmeans: Estimated Marginal Means, aka Least-Squares Means (R package version 1.4.6).
- Linetzky M, Kahn M, Lazarov A, Pine DS, Bar-Haim Y, 2019. Gaze-contingent music reward therapy for clinically anxious 7- to 10-year-olds: An open multiple baseline feasibility study. Journal of Clinical Child and Adolescent Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisk S, Vaswani A, Linetzky M, Bar-Haim Y, Lau JYF, 2020. Systematic review and meta-analysis: Eye-tracking of attention to threat in child and adolescent anxiety. Journal of the American Academy of Child & Adolescent Psychiatry 59(1), 88–99. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui LH, Benjet C, Georgiades K, Swendsen J, 2010. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatr 49(10), 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, DebRoy S, Sarkar D, CoreTeam, 2020. nlme: Linear and Nonlinear Mixed Effects Models (R package version 3.1–139).
- Rothbart MK, 2007. Temperament, development, and personality. Current Directions in Psychological Science 16(4), 207–212. [Google Scholar]
- Shimshoni Y, Lebowitz ER, Brotman MA, Pine DS, Leibenluft E, Silverman WK, 2020. Anxious-irritable children: A distinct subtype of childhood anxiety? Behavior Therapy 51(2), 211–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoddard J, Stringaris A, Brotman MA, Montville D, Pine DS, Leibenluft E, 2014. Irritability in child and adolescent anxiety disorders. Depress. Anxiety 31(7), 566–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Goodman R, Ferdinando S, Razdan V, Muhrer E, Leibenluft E, Brotman MA, 2012. The Affective Reactivity Index: a concise irritability scale for clinical and research settings. Journal of Child Psychology and Psychiatry 53(11), 1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry T, Nurse M, Hare TA, Marcus DJ, Westerlund A, Casey BJ, Nelson C, 2009. The NimStim set of facial expressions: Judgments from untrained research participants. Psychiatry Research 168(3), 242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, 1984. Negative affectivity - The disposition to experience aversive emotional states. Psychol. Bull 96(3), 465–490. [PubMed] [Google Scholar]
- Wiggins JL, Brotman MA, Adleman NE, Kim P, Oakes AH, Reynolds RC, Chen G, Pine DS, Leibenluft E, 2016. Neural correlates of irritability in disruptive mood dysregulation and bipolar disorders. American Journal of Psychiatry 173(7), 722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


