Abstract
OBJECTIVE
Investigations of the combined effects of neoadjuvant Onyx embolization and stereotactic radiosurgery (SRS) on brain arteriovenous malformations (AVMs) have not accounted for initial angioarchitectural features prior to neuroendovascular intervention. The aim of this retrospective, multicenter matched cohort study is to compare the outcomes of SRS with versus without upfront Onyx embolization for AVMs using de novo characteristics of the pre-embolized nidus.
METHODS
The International Radiosurgery Research Foundation AVM databases from 1987 to 2018 were retrospectively reviewed. Patients were categorized based on AVM treatment approach into Onyx embolization (OE) and SRS (OE+SRS) or SRS alone (SRS-only) cohorts and then propensity score matched in a 1:1 ratio. The primary outcome was AVM obliteration. Secondary outcomes were post-SRS hemorrhage, all-cause mortality, radiological and symptomatic radiation-induced changes (RICs), and cyst formation. Comparisons were analyzed using crude rates and cumulative probabilities adjusted for competing risk of death.
RESULTS
The matched OE+SRS and SRS-only cohorts each comprised 53 patients. Crude rates (37.7% vs 47.2% for the OE+SRS vs SRS-only cohorts, respectively; OR 0.679, p = 0.327) and cumulative probabilities at 3, 4, 5, and 6 years (33.7%, 44.1%, 57.5%, and 65.7% for the OE+SRS cohort vs 34.8%, 45.5%, 59.0%, and 67.1% for the SRS-only cohort, respectively; subhazard ratio 0.961, p = 0.896) of AVM obliteration were similar between the matched cohorts. The secondary outcomes of the matched cohorts were also similar. Asymptomatic and symptomatic embolization-related complication rates in the matched OE+SRS cohort were 18.9% and 9.4%, respectively.
CONCLUSIONS
Pre-SRS AVM embolization with Onyx does not appear to negatively influence outcomes after SRS. These analyses, based on de novo nidal characteristics, thereby refute previous studies that found detrimental effects of Onyx embolization on SRS-induced AVM obliteration. However, given the risks incurred by nidal embolization using Onyx, this neoadjuvant intervention should be used judiciously in multimodal treatment strategies involving SRS for appropriately selected large-volume or angioarchitecturally high-risk AVMs.
Keywords: arteriovenous malformation, stereotactic radiosurgery, embolization, stroke, endovascular, vascular disorders
Conventional stereotactic radiosurgery (SRS) delivered in a single session struggles to successfully treat large (diameter > 3 cm or volume > 12 ml) brain arteriovenous malformations (AVMs).1–3 Endovascular embolization has been used as a neoadjuvant intervention to render large nidi more amenable to SRS and target high-risk AVM-associated features, such as arterial aneurysms and high-flow intranidal arteriovenous fistulas.4–6 However, the role of upfront AVM embolization has come under scrutiny due to accumulating evidence of its potentially deleterious effect on obliteration rates after SRS.7
The etiology of lower post-SRS obliteration rates in embolized AVMs has been purported to stem from the physical properties of ethylene vinyl alcohol copolymer (Onyx, Medtronic Neurovascular), the most frequently used embolysate in contemporary neurointerventional procedures.8,9 However, previous studies that analyzed the effect of prior embolization on AVM SRS outcomes failed to account for the baseline nidal dimensions and angioarchitectural features before embolization.7,10–12 This represents a fundamental flaw that pervades the available literature pertaining to the relationship between prior Onyx embolization and post-SRS outcomes. The aim of this multicenter, retrospective matched cohort study is to compare the outcomes of SRS with versus without neoadjuvant Onyx embolization using de novo characteristics of the pre-embolized nidus.
Methods
This study follows the guidelines outlined in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement, and it was approved by the IRB of each participating center. Patient consent was waived by each IRB. Institutions within the International Radiosurgery Research Foundation were invited to contribute AVM cases treated between 1987 and 2018. Each respective institution was independently responsible for verification and attestation of data accuracy. Individual patient data from each contributing center were de-identified and pooled by an independent third party.
The inclusion criteria were 1) treatment with single-session SRS (including Gamma Knife radiosurgery and linear accelerator–based radiosurgery) with or without upfront Onyx embolization; 2) available baseline data regarding patient, AVM, SRS, and embolization characteristics; and 3) available outcome data after SRS. Exclusion criteria were 1) AVMs embolized without employing Onyx, and 2) treatment with dose- or volume-staged SRS. AVMs treated with combined endovascular embolization using Onyx as an embolic agent followed by SRS were categorized into the OE+SRS cohort, whereas AVMs treated with SRS alone (i.e., without prior embolization) were categorized into the SRS-only cohort.
Baseline Data and Variables
Patient variables included age, sex, and prior AVM therapy (i.e., before embolization). AVM variables included prior hemorrhage, volume, eloquent location, deep location, and presence of deep venous drainage. AVM nidus volume prior to embolization was measured on catheter digital subtraction angiography (DSA) using the ABC/2 method.13 Eloquent location was defined by Spetzler and Martin as “sensorimotor, language, and visual cortices, hypothalamus and thalamus, internal capsule, brainstem, cerebellar peduncles, and deep cerebellar nuclei.”14 Deep location was defined as thalamus, basal ganglia, and brainstem.15 SRS data included margin dose.
Follow-Up and Outcomes
The primary outcome was AVM obliteration on MRI or DSA. Radiological follow-up was typically performed at 6-month intervals for the first 2 years and then annually thereafter. Patients with evidence of AVM obliteration on follow-up noninvasive neuroimaging were recommended to undergo confirmatory DSA. AVM obliteration was defined as a lack of abnormal flow voids (based on MRI) or an absence of anomalous arteriovenous shunting (based on DSA). In addition to radiological evidence of residual arteriovenous shunting, the AVM was considered to be patent if any additional intervention targeting the nidus was performed after SRS. Time to obliteration was censored at the time of obliteration, additional AVM intervention, or loss to follow-up.
Secondary outcomes were post-SRS hemorrhage, all-cause mortality, radiological and symptomatic radiation-induced changes (RICs), cyst formation, and asymptomatic and symptomatic embolization-related complications. Post-SRS hemorrhage was defined as any AVM-related intracranial hemorrhage during the follow-up period, regardless of associated neurological symptoms or lack thereof. Radiological RIC was defined as the presence of perinidal hyperintensities on T2-weighted or FLAIR MRI sequences. Symptomatic RIC was defined as any new or worsening deterioration of neurological status in a patient with radiological RIC. Clinical and radiological follow-ups were obtained concurrently, when feasible. When in-person follow-up could not be obtained, clinical and neuroimaging data from referring institutions or physicians were acquired and reviewed by the respective treatment center.
Statistical Analysis
All statistical analyses were performed using Stata (version 15.1, StataCorp). Baseline characteristics and follow-up durations were compared between the OE+SRS and SRS-only cohorts using Pearson’s chi-square or Fisher’s exact tests for categorical variables, as appropriate, and the Student t-test for continuous variables. To control for baseline differences, the OE+SRS and SRS-only cohorts were matched, without replacement in a 1:1 ratio, with a caliper of 0.2 standard deviation of the logit of the propensity score using greedy matching. Propensity scores were derived using a logistic regression model accounting for AVM volumes. The PSMATCH2 package developed for Stata was used for propensity score derivation and the matching process.16 Standardized differences were used to assess the balance of baseline data, and differences < 0.20 between pretreatment characteristics of the matched cohorts were considered an adequate balance.
The primary and secondary outcomes between the OE+SRS versus SRS-only cohorts, before and after matching, were compared using binary logistic regression analyses, and each of these comparisons were reported as odds ratios (ORs) with 95% confidence intervals (CIs). Fisher’s exact test was performed for outcomes with zero frequencies. The cumulative rates of AVM obliteration, post-SRS hemorrhage, radiological and symptomatic RICs, and cyst formation were compared between the two cohorts, before and after matching, using cumulative incidence functions (CIFs) and competing-risk regression models adjusting for the competing risk of death, and each of these comparisons was reported as a subhazard ratio (SHR) with a 95% CI.17,18 CIFs and corresponding SHRs were not generated for outcomes with zero frequencies. Statistical significance was defined as p < 0.05, and all tests were two-tailed. Missing data were not imputed.
Results
Overall Cohort Characteristics
The overall study cohort comprised 1178 patients, including 68 and 1110 patients in the OE+SRS and SRS-only cohorts, respectively. Table 1 compares the baseline characteristics and follow-up durations between the unmatched cohorts. Patients in the OE+SRS cohort were significantly older (mean age 41.4 vs 35.7 years, p = 0.008) and more likely to be female (64.7% vs 49.4%, p = 0.014). The OE+SRS cohort had a greater proportion of patients who underwent prior AVM fractionated radiation therapy (4.4% vs 0.4%, p < 0.001). Deep AVM location was more common in the SRS-only cohort (24.9% vs 10.3%, p = 0.006). De novo AVM volume was larger in the OE+SRS cohort (15.5 vs 4.2 ml, p < 0.001), whereas margin dose was higher in the SRS-only cohort (mean 21.0 vs 19.2 Gy, p < 0.001). The clinical follow-up duration was longer in the SRS-only cohort (mean 68.1 vs 47.4 months, p = 0.002).
TABLE 1.
Comparison of baseline characteristics and follow-up durations between the unmatched OE+SRS versus SRS-only cohorts
| Characteristic | OE+SRS Cohort, n = 68 | SRS-Only Cohort, n = 1110 | p Value |
|---|---|---|---|
| Mean age (SD), yrs | 41.4 (17.6) | 35.7 (16.6) | 0.008 |
| Females (%) | 44/68 (64.7) | 548/1110 (49.4) | 0.014 |
| Prior AVM surgery (%) | 8/68 (11.8) | 166/1104 (15.0) | 0.461 |
| Prior AVM fractionated radiation therapy (%) | 3/68 (4.4) | 4/959 (0.4) | <0.001 |
| Prior AVM hemorrhage (%) | 39/68 (57.4) | 571/1110 (51.4) | 0.344 |
| Deep AVM location (%) | 7/68 (10.3) | 276/1109 (24.9) | 0.006 |
| Eloquent AVM location (%) | 35/62 (56.5) | 610/1058 (57.7) | 0.852 |
| Deep venous drainage (%) | 35/68 (51.5) | 444/1109 (40.0) | 0.062 |
| Mean AVM volume (SD), ml | 15.5 (16.4) | 4.2 (7.9) | <0.001 |
| Mean SRS margin dose (SD), Gy | 19.2 (2.7) | 21.0 (3.6) | <0.001 |
| Mean mos radiological follow-up (SD) | 41.7 (40.3) | 49.3 (40.2) | 0.140 |
| Mean mos clinical follow-up (SD) | 47.7 (40.6) | 68.1 (50.3) | 0.002 |
Boldface type indicates statistical significance.
Comparisons of Outcomes Between Unmatched OE+SRS Versus SRS-Only Cohorts
Table 2 compares the outcomes of the unmatched OE+SRS versus SRS-only cohorts. The AVM obliteration rate was lower in the OE+SRS cohort (39.4% vs 64.0%, OR 0.365, 95% CI 0.219–0.607, p < 0.001). However, cumulative probabilities of obliteration at 3, 4, 5, and 6 years were similar between the two cohorts (35.0%, 48.6%, 54.4%, and 58.6% for the OE+SRS cohort vs 43.1%, 58.2%, 64.2%, and 68.5% for the SRS-only cohort, respectively; SHR 0.763, 95% CI 0.533–1.094, p = 0.141; Fig. 1A).
TABLE 2.
Comparison of outcomes between the unmatched OE+SRS versus SRS-only cohorts
| Outcome | OE+SRS Cohort, n = 68 | SRS-Only Cohort, n = 1110 | OR (95% CI) | p Value |
|---|---|---|---|---|
| Primary outcome | ||||
| AVM obliteration (%) | 26/66 (39.4) | 698/1090 (64.0) | 0.365 (0.219–0.607) | <0.001 |
| Secondary outcomes (%) | ||||
| Post-SRS hemorrhage | 5/61 (8.2) | 65/1091 (6.0) | 1.409 (0.546–3.639) | 0.478 |
| All-cause mortality | 1/66 (1.5) | 31/1108 (2.8) | 0.534 (0.072–3.977) | 0.541 |
| Radiological RICs | 20/63 (31.8) | 373/1068 (34.9) | 0.867 (0.502–1.495) | 0.607 |
| Symptomatic RICs | 13/63 (20.6) | 141/1071 (13.2) | 1.715 (0.908–3.237) | 0.096 |
| Cyst formation | 2/63 (3.2) | 13/1079 (1.2) | 2.689 (0.593–12.181) | 0.200 |
| Asymptomatic embolization-related complications | 16/68 (23.5) | — | — | — |
| Symptomatic embolization-related complications | 5/68 (7.4) | — | — | — |
Boldface type indicates statistical significance.
FIG. 1.
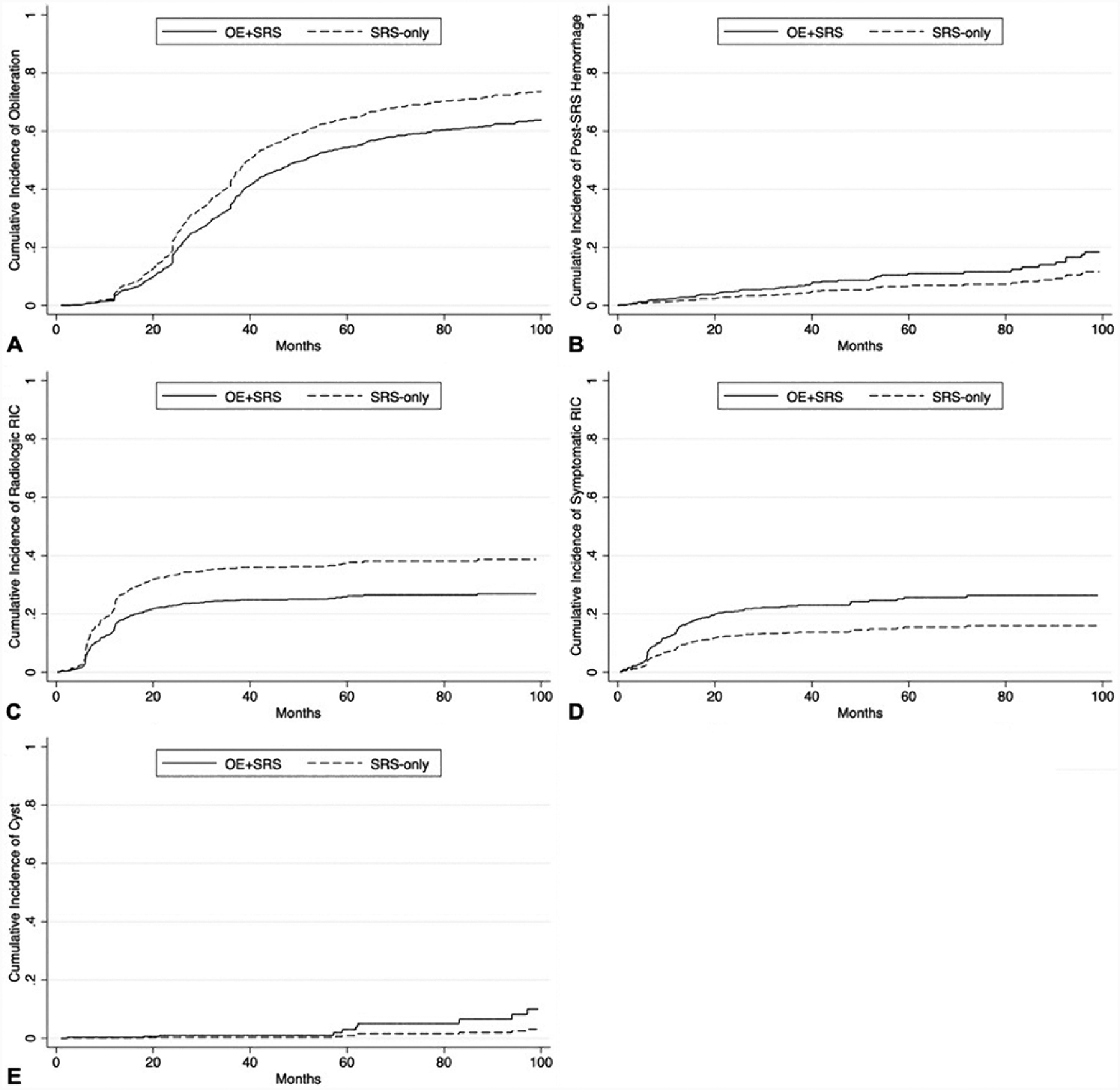
Comparisons of CIFs for AVM obliteration (p = 0.141) (A), post-SRS hemorrhage (p = 0.314) (B), radiological RICs (p = 0.117) (C), symptomatic RICs (p = 0.048) (D), and cyst development (p = 0.115) (E) between the unmatched OE+SRS versus SRS-only cohorts.
The crude rates of each secondary outcome were similar between the unmatched cohorts. Cumulative probabilities at 3, 4, 5, and 6 years of post-SRS hemorrhage (6.5%, 8.7%, 11.0%, and 11.7% for the OE+SRS cohort vs 4.0%, 5.4%, 6.9%, and 7.3% for the SRS-only cohort, respectively; SHR 1.633, 95% CI 0.628–4.250, p = 0.314; Fig. 1B) and radiological RICs (24.5%, 25.0%, 26.1%, and 26.4% for the OE+SRS cohort vs 35.5%, 36.2%, 37.6%, and 38.0% for the SRS-only cohort, respectively; SHR 0.641, 95% CI 0.367–1.118, p = 0.117; Fig. 1C) were similar between the two cohorts. However, cumulative probabilities of symptomatic RICs at 3, 4, 5, and 6 years were significantly higher in the OE+SRS cohort (22.7%, 24.2%, 25.6%, and 26.3% for the OE+SRS cohort vs 13.6%, 14.5%, 15.5%, and 15.9% for the SRS-only cohort, respectively; SHR 1.760, 95% CI 1.004–3.084, p = 0.048; Fig. 1D). Cumulative probabilities of cyst formation at 3, 4, 5, and 6 years were similar between the two cohorts (0.9%, 0.9%, 2.9%, and 5.0% for the OE+SRS cohort vs 0.3%, 0.3%, 0.9%, and 1.5% for the SRS-only cohort, respectively; SHR 3.375, 95% CI 0.745–15.292, p = 0.115; Fig. 1E). Asymptomatic and symptomatic embolization-related complication rates were 23.5% and 7.4%, respectively.
Matched Cohort Characteristics
The matched OE+SRS and SRS-only cohorts each comprised 53 patients. Table 3 compares the baseline characteristics and follow-up durations between the matched cohorts. After matching, patients in the OE+SRS cohort remained significantly older (mean age 43.1 vs 34.4 years, p = 0.013) and more likely to have prior AVM hemorrhage (60.4% vs 39.6%, p = 0.033). The clinical follow-up duration also remained significantly longer in the SRS-only cohort (61.9 vs 43.2 months, p = 0.036).
TABLE 3.
Comparison of baseline characteristics and follow-up durations between the matched OE+SRS versus SRS-only cohorts
| Characteristic | OE+SRS Cohort, n = 53 | SRS-Only Cohort, n = 53 | p Value |
|---|---|---|---|
| Mean age (SD), yrs | 43.1 (18.0) | 34.4 (17.4) | 0.013 |
| Females (%) | 33/53 (62.3) | 27/53 (50.9) | 0.240 |
| Prior AVM surgery (%) | 7/53 (13.2) | 7/53 (13.2) | 1.000 |
| Prior AVM fractionated radiation therapy (%) | 2/53 (3.8) | 0/45 (0) | 0.498 |
| Prior AVM hemorrhage (%) | 32/53 (60.4) | 21/53 (39.6) | 0.033 |
| Deep AVM location (%) | 6/53 (11.3) | 12/53 (22.6) | 0.121 |
| Eloquent AVM location (%) | 29/47 (61.7) | 27/46 (58.7) | 0.767 |
| Deep venous drainage (%) | 28/53 (52.8) | 29/53 (54.7) | 0.846 |
| Mean AVM volume (SD), ml | 10.3 (10.1) | 10.8 (11.4) | 0.794* |
| Mean SRS margin dose (SD), Gy | 19.2 (2.7) | 19.0 (3.4) | 0.663 |
| Mean mos radiological follow-up (SD) | 37.2 (37.4) | 44.4 (36.4) | 0.319 |
| Mean mos clinical follow-up (SD) | 43.2 (37.5) | 61.9 (50.5) | 0.036 |
Boldface type indicates statistical significance.
Matched covariates.
Table 4 summarizes the standardized differences in baseline characteristics between the OE+SRS and SRS-only cohorts before and after propensity score matching. Imbalances in baseline characteristics after matching were noted for age (0.404), prior AVM fractionated radiation therapy (0.209), prior AVM hemorrhage (0.350), and deep location (−0.281). AVM volume and margin dose were well balanced between the matched cohorts. Of the 17 patients in the matched OE+SRS cohort with available embolization results, volume reduction alone, flow reduction alone, flow and volume reduction, flow reduction and aneurysm occlusion, and flow and volume reduction and aneurysm occlusion were achieved in 11.8%, 5.9%, 47.1%, 5.9%, and 29.4%, respectively.
TABLE 4.
Standardized difference of baseline characteristics between OE+SRS versus SRS-only cohorts before and after propensity score matching
| Characteristic | Mean, Before Adjustment | Standardized Difference, Before Adjustment | Mean, After Adjustment | Standardized Difference, After Adjustment | ||
|---|---|---|---|---|---|---|
| OE+SRS Cohort | SRS-Only Cohort | OE+SRS Cohort | SRS-Only Cohort | |||
| Age | 42.21 | 36.36 | 0.346 | 42.18 | 35.35 | 0.404 |
| Sex | 0.40 | 0.51 | −0.223 | 0.41 | 0.46 | −0.101 |
| Prior AVM surgery | 0.13 | 0.15 | −0.052 | 0.14 | 0.19 | −0.150 |
| Prior AVM fractionated radiation therapy | 0.02 | 0.00 | 0.136 | 0.02 | 0.00 | 0.209 |
| Prior AVM hemorrhage | 0.63 | 0.50 | 0.279 | 0.66 | 0.49 | 0.350 |
| Deep AVM location | 0.12 | 0.25 | −0.344 | 0.14 | 0.24 | −0.281 |
| Eloquent AVM location | 0.58 | 0.61 | −0.073 | 0.59 | 0.59 | −0.007 |
| Deep venous drainage | 0.50 | 0.48 | 0.041 | 0.52 | 0.59 | −0.143 |
| AVM volume | 16.43 | 3.94 | 0.944 | 10.88 | 9.12 | 0.133 |
| SRS margin dose | 19.24 | 21.03 | −0.572 | 19.35 | 19.35 | 0.000 |
Boldface type indicates standardized difference ≥ 0.20.
Comparisons of Outcomes Between Matched OE+SRS Versus SRS-Only Cohorts
Table 5 compares the outcomes of the matched OE+SRS versus SRS-only cohorts. Obliteration rates were similar between the matched OE+SRS (37.7%) and SRS-only (47.2%) cohorts (OR 0.679, 95% CI 0.313–1.472, p = 0.327). Cumulative probabilities of obliteration at 3, 4, 5, and 6 years were also similar between the matched cohorts (33.7%, 44.1%, 57.5%, and 65.7% for the OE+SRS cohort vs 34.8%, 45.5%, 59.0%, and 67.1% for the SRS-only cohort, respectively; SHR 0.961, 95% CI 0.530–1.743, p = 0.896; Fig. 2A).
TABLE 5.
Comparison of outcomes between the matched OE+SRS versus SRS-only cohorts
| Outcome | OE+SRS Cohort, n = 53 | SRS-Only Cohort, n = 53 | OR (95% CI) | p Value |
|---|---|---|---|---|
| Primary outcome | ||||
| AVM obliteration (%) | 20/53 (37.7) | 25/53 (47.2) | 0.679(0.313–1.472) | 0.327 |
| Secondary outcomes (%) | ||||
| Post-SRS hemorrhage | 4/50 (8.0) | 6/52 (11.5) | 0.667 (0.176–2.519) | 0.550 |
| All-cause mortality | 1/52 (1.9) | 0/52 (0) | — | 1.000* |
| Radiological RICs | 17/51 (33.3) | 24/50 (48.0) | 0.542 (0.242–1.211) | 0.135 |
| Symptomatic RICs | 11/51 (21.6) | 10/50 (20.0) | 1.100 (0.420–2.879) | 0.846 |
| Cyst | 2/51 (3.9) | 0/51 (0) | — | 0.495* |
| Asymptomatic embolization complications | 10/53 (18.9) | — | — | — |
| Symptomatic embolization complications | 5/53 (9.4) | — | — | — |
Fisher’s exact test
FIG. 2.
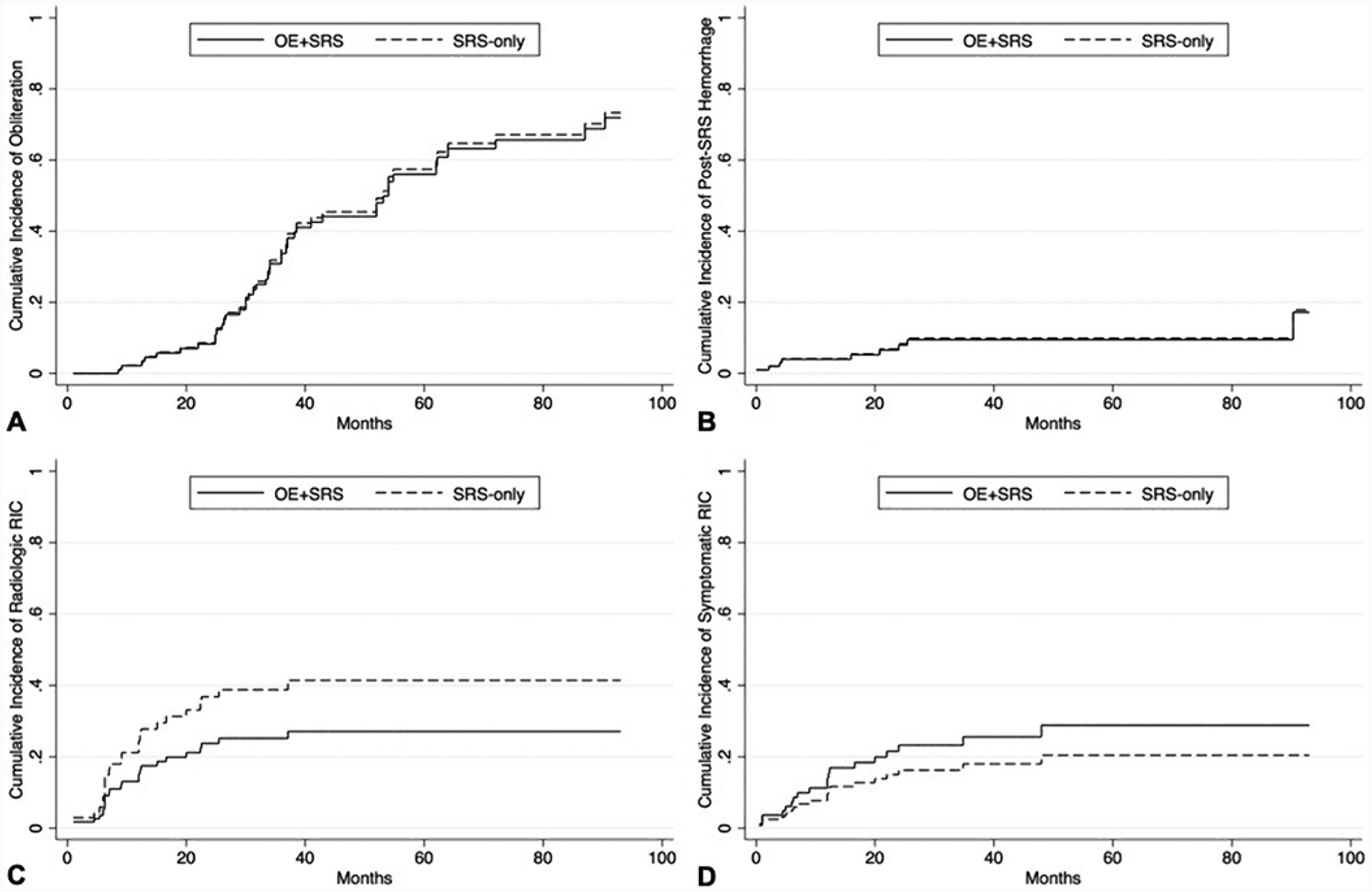
Comparisons of CIFs for AVM obliteration (p = 0.896) (A), post-SRS hemorrhage (p = 0.950) (B), radiological RICs (p = 0.178) (C), and symptomatic RICs (p = 0.392) (D) between the matched OE+SRS versus SRS-only cohorts.
The crude rates of each secondary outcome were similar between the matched cohorts. Cumulative probabilities of post-SRS hemorrhage at 3, 4, 5, and 6 years were similar between the two cohorts (9.5%, 9.5%, 9.5%, and 9.5% for the OE+SRS cohort vs 9.9%, 9.9%, 9.9%, and 9.9% for the SRS-only cohort, respectively; SHR 0.959, 95% CI 0.265–3.478, p = 0.950; Fig. 2B). Cumulative probabilities at 3 and 5 years of radiological (25.2% and 27.1% for the OE+SRS cohort vs 38.8% and 41.4% for the SRS-only cohort; SHR 0.591, 95% CI 0.275–1.270, p = 0.178; Fig. 2C) and symptomatic (25.6% and 28.8% for the OE+SRS cohort vs 18.0% and 20.4% for the SRS-only cohort; SHR 1.487, 95% CI 0.600–3.686, p = 0.392; Fig. 2D) RICs were also similar between the two cohorts. Asymptomatic and symptomatic embolization-related complication rates were 18.9% and 9.4%, respectively.
Discussion
Volumetric reduction of large AVMs using embolization to facilitate subsequent SRS of the smaller residual nidus is a conceptually appealing multimodal treatment, but this combined approach has been reported to yield a lower likelihood of obliteration compared to stand-alone SRS.6,7 As such, pre-SRS embolization has not become a mainstay therapy in AVM management. However, studies supporting this notion performed their comparative analyses with postembolization AVM characteristics, which inherently biased their findings against embolized AVMs. That is, initially larger volumes and more complex angio-architectures of AVMs selected for pre-SRS embolization have not been accounted for by existing reports.
The predominant use of Onyx in contemporary AVM embolization has raised concerns that it could affect AVM SRS outcomes differently from other embolysates. The radiopaque component of Onyx, tantalum, may attenuate the effective radiation dose via a shielding effect. Tantalum’s high atomic number of 73 causes significant image artifacts at typical kilovoltage CT energies, and therefore it could distort radiosurgical dose distribution.9,19 Additionally, extensive beam-hardening artifacts from tantalum on CT angiography and a similar hypointense appearance of Onyx to AVM flow voids on T2-weighted MRI can impair the accuracy of SRS treatment planning by obscuring the borders of the residual nidus. Other plausible mechanisms for lower post-SRS obliteration rates of AVMs embolized with Onyx include embolization-induced angiogenesis, recanalization of embolized portions of a nidus not otherwise targeted by SRS, and pseudoocclusion (i.e., angiographic occlusion of a vessel that is functionally patent).20–26 In contrast, others have argued, based on simulation studies, that Onyx-mediated radiation dose alterations are negligible.19,27–30 As such, the risk-to-benefit profile of Onyx embolization preceding AVM SRS remains controversial.
In this multicenter, retrospective matched cohort study we found no differences between the SRS outcomes of volumetrically comparable Onyx-embolized versus nonembolized AVMs. Our study is distinguished from the flawed design of previous studies by its use of de novo AVM characteristics (i.e., prior to embolization). Although obliteration was more likely in the unmatched SRS-only cohort (p < 0.001), this difference was no longer significant in time-dependent analysis adjusting for competing risk of death. Both crude and time-dependent obliteration rates were similar between the matched OE+SRS and SRS-only cohorts. Therefore, pre-SRS AVM embolization with Onyx does not appear to reduce post-SRS obliteration rates.
Despite our best attempts to balance the OE+SRS and SRS-only cohorts with propensity score matching, age and prior AVM hemorrhage were significantly different between the matched cohorts. Because initial nidus volume is generally accepted to be the most important AVM factor in SRS-induced obliteration, we prioritized this covariate foremost in our matching process.31 Coincidentally, this approach also offered the optimal balance of the remaining baseline covariates between the matched cohorts. Inclusion of other covariates in the derivation of propensity scores did not improve the balance of baseline characteristics relative to using AVM volume alone. Furthermore, the effects of age and prior hemorrhage on obliteration rates after AVM SRS may be inconsequential.32–35
Despite the higher proportion of ruptured AVMs in the OE+SRS cohort, both crude rates and cumulative probabilities of post-SRS hemorrhage were similar between the two cohorts in unmatched and matched analyses. Although the cumulative probability of symptomatic RICs was higher in the unmatched OE+SRS cohort (p = 0.048), cumulative probabilities of both radiological and symptomatic RICs were similar between the matched cohorts. We were unable to elucidate whether the OE+SRS cohort’s higher proportion of prior AVM hemorrhage, which has been shown to protect against RICs, modified the relationship between Onyx embolization and RIC rates in the present analyses.32,33 Despite comparable RIC rates between the matched cohorts, detection of symptomatic SRS-related complications in embolized AVMs could be masked by embolization-related complications, which were symptomatic and asymptomatic in 9% and 19% of the matched OE+SRS cohort, respectively.
Although the present study does not deem Onyx embolization detrimental to AVM SRS outcomes, we also failed to show a discrete benefit from the combination of both AVM therapies. Nevertheless, we believe that pre-SRS AVM embolization with Onyx will retain a role in the treatment of carefully selected patients. Specifically, targeted embolization of a large AVM with multiple compartments could simplify its morphology so as to facilitate treatment of the residual nidus with single-session SRS, thereby averting staged SRS approaches that can require longer implementation periods.36 Embolization can also eliminate AVM-associated arterial aneurysms that, left untreated, can elevate the risk of post-SRS hemorrhage.5,37 Lastly, endovascular occlusion of high-flow intranidal arteriovenous shunts, which are relatively radioresistant, could improve the likelihood of SRS-induced obliteration.38 Although symptomatic complications associated with pre-SRS AVM embolization varied in symptomatology, severity, and duration, they occurred in nearly 10% of our matched OE+SRS cohort. In addition, asymptomatic complications occurred in 19%. Taken together, the pre-SRS embolization-related complication rate was relatively high. Therefore, the added risks of pre-SRS embolization warrant careful consideration, and judicious patient selection is essential. Ultimately, the aggressiveness of pre-SRS embolization should be adjudicated by a multidisciplinary team comprising the operators performing embolization and those performing SRS.
We recognize that limitations of our study could impact its validity and generalizability. The accuracy and reliability of the analyses are dependent upon data reported by respective contributing centers and therefore may be susceptible to reporting bias. Despite our best efforts to balance the pretreatment characteristics of the OE+SRS and SRS-only cohorts through propensity score matching, several measured baseline covariates remained unbalanced and other unmeasured covariates may not be accounted for. The effects of these unbalanced covariates on the primary and secondary outcomes are unquantifiable, but the resultant potential selection bias should be acknowledged. We could not ascertain the criteria or rationale for the utilization of pre-SRS Onyx embolization in each case, which could reflect selection, treatment, and referral biases of the participating centers and treating physicians. However, we were able to balance the most influential baseline characteristics (i.e., nidus volume and margin dose) with respect to AVM SRS outcomes.39
Because pre-embolization MR images were not available for volumetric analysis in some cases, AVM volumes were calculated based on DSA using the ABC/2 method for both cohorts to maintain consistency. This method has been generally accepted for intracerebral hematoma volumetry, but it has yet to be validated for AVMs, especially in those with large nidi and complex morphologies.40,41 Additionally, variations in unrecorded embolysate volume and degree of nidal devascularization may confound the results. Because AVM volume reduction by embolization was not quantified in our data set, its effects on SRS outcomes could not be analyzed. AVM obliteration was determined by MRI alone in 8.3% of the cases, and the lack of angiographic confirmation in a minority of the study cohort could have overestimated the reported obliteration rates. However, MRI has demonstrated reasonable accuracy for assessing obliteration after AVM SRS compared to the gold standard of DSA.42 Importantly, we were unable to detect small differences in outcomes between the matched cohorts due to their modest sample sizes. Lastly, our findings may not be generalizable to small- and medium-volume AVMs or those treated with staged SRS approaches.2,36
Conclusions
After accounting for de novo AVM characteristics, our findings refute previous studies that espoused an adverse effect of Onyx embolization on SRS-induced nidal obliteration. In a matched analysis of morphologically comparable nidi, AVMs embolized with Onyx appeared to have SRS outcomes that were similar to those of nonembolized lesions. However, given the neuroendovascular risks associated with Onyx embolization of AVMs, use of this neoadjuvant intervention should be restricted to carefully selected large-volume or angioarchitecturally high-risk nidi that are deemed appropriate candidates for multimodal treatment strategies employing SRS. Future studies derived from prospective, multicenter registries are necessary to clarify the role of combined embolization and SRS in AVM management, particularly in comparison to staged SRS approaches.
Disclosures
Dr. Liscak reports receiving consultant fees from Elekta AB. Dr. Williams reports receiving consultant fees from Monteris Medical, Inc. Dr. Cockroft reports receiving consultant fees from Medtronic and Minnetronix. Dr. Kondziolka reports receiving research funding from Brainlab.
ABBREVIATIONS
- AVM
arteriovenous malformation
- CI
confidence interval
- CIF
cumulative incidence function
- DSA
digital subtraction angiography
- OE
Onyx embolization
- OR
odds ratio
- RIC
radiation-induced change
- SHR
subhazard ratio
- SRS
stereotactic radiosurgery
References
- 1.Kano H, Kondziolka D, Flickinger JC, et al. Stereotactic radiosurgery for arteriovenous malformations, Part 6: Multistaged volumetric management of large arteriovenous malformations. J Neurosurg. 2012; 116(1): 54–65. [DOI] [PubMed] [Google Scholar]
- 2.Ilyas A, Chen CJ, Ding D, et al. Volume-staged versus dose-staged stereotactic radiosurgery outcomes for large brain arteriovenous malformations: a systematic review. J Neurosurg. 2018; 128(1): 154–164. [DOI] [PubMed] [Google Scholar]
- 3.Patibandla MR, Ding D, Kano H, et al. Stereotactic radiosurgery for Spetzler-Martin Grade IV and V arteriovenous malformations: an international multicenter study. J Neurosurg. 2018; 129(2): 498–507. [DOI] [PubMed] [Google Scholar]
- 4.Solomon RA, Connolly ES Jr. Arteriovenous malformations of the brain. N Engl J Med. 2017; 376(19): 1859–1866. [DOI] [PubMed] [Google Scholar]
- 5.Kano H, Kondziolka D, Flickinger JC, et al. Aneurysms increase the risk of rebleeding after stereotactic radiosurgery for hemorrhagic arteriovenous malformations. Stroke. 2012; 43(10): 2586–2591. [DOI] [PubMed] [Google Scholar]
- 6.Ding D, Ilyas A, Sheehan JP. Contemporary management of high-grade brain arteriovenous malformations. Neurosurgery. 2018; 65(CN_suppl_1): 24–33. [DOI] [PubMed] [Google Scholar]
- 7.Russell D, Peck T, Ding D, et al. Stereotactic radiosurgery alone or combined with embolization for brain arteriovenous malformations: a systematic review and meta-analysis. J Neurosurg. 2018; 128(5): 1338–1348. [DOI] [PubMed] [Google Scholar]
- 8.Lee CC, Chen CJ, Ball B, et al. Stereotactic radiosurgery for arteriovenous malformations after Onyx embolization: a case-control study. J Neurosurg. 2015; 123(1): 126–135. [DOI] [PubMed] [Google Scholar]
- 9.Andrade-Souza YM, Ramani M, Beachey DJ, et al. Liquid embolisation material reduces the delivered radiation dose: a physical experiment. Acta Neurochir (Wien). 2008; 150(2): 161–164. [DOI] [PubMed] [Google Scholar]
- 10.Kano H, Kondziolka D, Flickinger JC, et al. Stereotactic radiosurgery for arteriovenous malformations after embolization: a case-control study. J Neurosurg. 2012; 117(2): 265–275. [DOI] [PubMed] [Google Scholar]
- 11.Oermann EK, Ding D, Yen CP, et al. Effect of prior embolization on cerebral arteriovenous malformation radiosurgery outcomes: a case-control study. Neurosurgery. 2015; 77(3): 406–417. [DOI] [PubMed] [Google Scholar]
- 12.Andrade-Souza YM, Ramani M, Scora D, et al. Embolization before radiosurgery reduces the obliteration rate of arteriovenous malformations. Neurosurgery. 2007; 60(3): 443–452. [DOI] [PubMed] [Google Scholar]
- 13.Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996; 27(8): 1304–1305. [DOI] [PubMed] [Google Scholar]
- 14.Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986; 65(4): 476–483. [DOI] [PubMed] [Google Scholar]
- 15.Wegner RE, Oysul K, Pollock BE, et al. A modified radiosurgery-based arteriovenous malformation grading scale and its correlation with outcomes. Int J Radiat Oncol Biol Phys. 2011; 79(4): 1147–1150. [DOI] [PubMed] [Google Scholar]
- 16.Leuven E, Sianesi B. PSMATCH2: Stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing. 2003. Statistical Software Components. Accessed September 1, 2020. http://ideas.repec.org/c/boc/bocode/s432001.html [Google Scholar]
- 17.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999; 94(446): 496–509. [Google Scholar]
- 18.Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016; 133(6): 601–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roberts DA, Balter JM, Chaudhary N, et al. Dosimetric measurements of Onyx embolization material for stereotactic radiosurgery. Med Phys. 2012; 39(11): 6672–6681. [DOI] [PubMed] [Google Scholar]
- 20.Valle RD, Zenteno M, Jaramillo J, et al. Definition of the key target volume in radiosurgical management of arteriovenous malformations: a new dynamic concept based on angiographic circulation time. J Neurosurg. 2008; 109(suppl): 41–50. [DOI] [PubMed] [Google Scholar]
- 21.Pollock BE, Kondziolka D, Lunsford LD, et al. Repeat stereotactic radiosurgery of arteriovenous malformations: factors associated with incomplete obliteration. Neurosurgery. 1996; 38(2): 318–324. [DOI] [PubMed] [Google Scholar]
- 22.Akakin A, Ozkan A, Akgun E, et al. Endovascular treatment increases but gamma knife radiosurgery decreases angiogenic activity of arteriovenous malformations: an in vivo experimental study using a rat cornea model. Neurosurgery. 2010; 66(1): 121–130. [DOI] [PubMed] [Google Scholar]
- 23.Buell TJ, Ding D, Starke RM, et al. Embolization-induced angiogenesis in cerebral arteriovenous malformations. J Clin Neurosci. 2014; 21(11): 1866–1871. [DOI] [PubMed] [Google Scholar]
- 24.Fournier D, Terbrugge K, Rodesch G, Lasjaunias P. Revascularization of brain arteriovenous malformations after embolization with bucrylate. Neuroradiology. 1990; 32(6): 497–501. [DOI] [PubMed] [Google Scholar]
- 25.Gobin YP, Laurent A, Merienne L, et al. Treatment of brain arteriovenous malformations by embolization and radiosurgery. J Neurosurg. 1996; 85(1): 19–28. [DOI] [PubMed] [Google Scholar]
- 26.Rao VR, Mandalam KR, Gupta AK, et al. Dissolution of isobutyl 2-cyanoacrylate on long-term follow-up. AJNR Am J Neuroradiol. 1989; 10(1): 135–141. [PMC free article] [PubMed] [Google Scholar]
- 27.Bing F, Doucet R, Lacroix F, et al. Liquid embolization material reduces the delivered radiation dose: clinical myth or reality? AJNR Am J Neuroradiol. 2012; 33(2): 320–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mamalui-Hunter M, Jiang T, Rich KM, et al. Effect of liquid embolic agents on Gamma Knife surgery dosimetry for arteriovenous malformations. Clinical article. J Neurosurg. 2011; 115(2): 364–370. [DOI] [PubMed] [Google Scholar]
- 29.Watanabe Y, Sandhu D, Warmington L, et al. Three-dimensional assessment of the effects of high-density embolization material on the absorbed dose in the target for Gamma Knife radiosurgery of arteriovenous malformations. J Neurosurg. 2016; 125(1)(suppl 1): 123–128. [DOI] [PubMed] [Google Scholar]
- 30.Schlesinger DJ, Nordström H, Lundin A, et al. Dosimetric effects of Onyx embolization on Gamma Knife arteriovenous malformation dose distributions. J Neurosurg. 2016; 125(1) (suppl 1): 114–122. [DOI] [PubMed] [Google Scholar]
- 31.Starke RM, Kano H, Ding D, et al. Stereotactic radiosurgery for cerebral arteriovenous malformations: evaluation of long-term outcomes in a multicenter cohort. J Neurosurg. 2017; 126(1): 36–44. [DOI] [PubMed] [Google Scholar]
- 32.Chen CJ, Lee CC, Ding D, et al. Stereotactic radiosurgery for unruptured versus ruptured pediatric brain arteriovenous malformations. Stroke. 2019; 50(10): 2745–2751. [DOI] [PubMed] [Google Scholar]
- 33.Ding D, Yen CP, Starke RM, et al. Effect of prior hemorrhage on intracranial arteriovenous malformation radiosurgery outcomes. Cerebrovasc Dis. 2015; 39(1): 53–62. [DOI] [PubMed] [Google Scholar]
- 34.Chen CJ, Ding D, Kano H, et al. Effect of advanced age on stereotactic radiosurgery outcomes for brain arteriovenous malformations: a multicenter matched cohort study. World Neurosurg. 2018; 119: e429–e440. [DOI] [PubMed] [Google Scholar]
- 35.Chen CJ, Ding D, Kano H, et al. Stereotactic radiosurgery for pediatric versus adult brain arteriovenous malformations. Stroke. 2018; 49(8): 1939–1945. [DOI] [PubMed] [Google Scholar]
- 36.Seymour ZA, Chan JW, Sneed PK, et al. Dose response and architecture in volume staged radiosurgery for large arteriovenous malformations: a multi-institutional study. Radiother Oncol. 2020; 144: 180–188. [DOI] [PubMed] [Google Scholar]
- 37.Ding D, Chen CJ, Starke RM, et al. Risk of brain arteriovenous malformation hemorrhage before and after stereotactic radiosurgery. Stroke. 2019; 50(6): 1384–1391. [DOI] [PubMed] [Google Scholar]
- 38.Taeshineetanakul P, Krings T, Geibprasert S, et al. Angio-architecture determines obliteration rate after radiosurgery in brain arteriovenous malformations. Neurosurgery. 2012; 71(6): 1071–1079. [DOI] [PubMed] [Google Scholar]
- 39.Flickinger JC, Pollock BE, Kondziolka D, Lunsford LD. A dose-response analysis of arteriovenous malformation obliteration after radiosurgery. Int J Radiat Oncol Biol Phys. 1996; 36(4): 873–879. [DOI] [PubMed] [Google Scholar]
- 40.Roark C, Vadlamudi V, Chaudhary N, et al. ABC/2 method does not accurately predict cerebral arteriovenous malformation volume. Neurosurgery. 2018; 82(2): 220–225. [DOI] [PubMed] [Google Scholar]
- 41.Webb AJ, Ullman NL, Morgan TC, et al. Accuracy of the ABC/2 score for intracerebral hemorrhage: systematic review and analysis of MISTIE, CLEAR-IVH, and CLEAR III. Stroke. 2015; 46(9): 2470–2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee CC, Reardon MA, Ball BZ, et al. The predictive value of magnetic resonance imaging in evaluating intracranial arteriovenous malformation obliteration after stereotactic radiosurgery. J Neurosurg. 2015; 123(1): 136–144. [DOI] [PubMed] [Google Scholar]


