Abstract
Background
Total hip arthroplasty (THA) and hip resurfacing arthroplasty (HRA) are already proven good for end-stage arthritis in the older populations but it is challenging in young teenage patients. The primary aim was to assess Hip Disability and Osteoarthritis Outcome Score (HOSS), Harris Hip Score (HHS) and secondary aim for implant survival rate.
Materials and Methods
The details of 33 teenage patients (forty hips) who underwent HRA (21) and THA (19) at our institution (January 2002 to December 2013) with a mean follow-up period of 11.00 years (range 7.00–18.40) were included. The study group had 25 males and eight females.
Results
The overall median HOOSs with interquartile range were 89.00 (87.63–0.00). The median HOOSs at follow-up were as follows: 95.00 (90.00–95.00) for symptoms, 92.00 (90.00–95.00) pain, 87.00 (85.00–90.00) for functions, 81.00 (75.00–85.00) for sports and 94.00 (88.00–95.00) for QOL. HHS improved significantly from 36.88 ± 6.14 to 90.12 ± 6.56 (p < 0.001). The HHS of HRA group improved from 36.29 ± 5.83 to 89.38 ± 5.23 and THA group improved from 37.26 ± 6.22 to 90.94 ± 7.84. The 5-year radiological follow-up X-rays did not show any radiolucent line wider than 2 mm in all three zones of the acetabulum and no progressive subsidence or migration of > 1 mm and divergent radiopaque line in femur. The Implant survival rate for HRA was 100% at 5 years, 100% at 10 years, 92% at 15 years and THA group was 100% at 5 years and 90% at 10 years.
Conclusion
Our study showed a disability rate of zero with improved HOSS and HHS. The overall implant survival rate was good with 100% at 5 years, 97% at 10 years and 89.9% at 15 years in contrast to the previous studies with the use of modern implants and newer standard surgical techniques.
Level of Evidence
A Level II study http://www.spine.org/Documents/LevelsofEvidenceFinal.pdf.
Keywords: Total hip arthroplasty (THA), Hip resurfacing arthroplasty (HRA), Young arthroplasty patients, Hip Disability and Osteoarthritis Outcome Score (HOOS), Harris Hip Score (HHS)
Introduction
Total hip arthroplasty (THA) for end-stage arthritis in the older populations has proven to be a life-altering intervention as evidenced by the excellent long-term survivorship. [1, 2] However, it was not considered a viable option for the same conditions in the very young patients due to concern about the longevity and probable multiple revisions during their lifetime [3]. For several decades, hip arthrodesis and resection arthroplasty were considered as salvage procedures in this population [4]. The loss of stability or mobility at the hip joint in a young growing individual impacts their social and personal development. Uncemented THA in this group has shown excellent survivorship of more than 95% in several reports [5–7]. Hip resurfacing remains one of the viable alternatives in this age group with the following advantages: bone preservation, lower dislocation rate, maintaining the native joint hip biomechanics and the ability to continue in high impact activities [8–11]. The long-term results of Hip Resurfacing Arthroplasty (HRA) certain registries with good survival results makes both THA and HRA viable options in adolescent and very young patients with end-stage arthritis [12–14].
Higher activity level and younger age are well-known risk factors for revision and poor survival of the implant [15, 16]. Recent studies have shown the implant survival rate ranges from 67 to 90% at 10-year follow-up [17–19]. This may be due to the variable inclusion criteria, sample size, etiology, implant type, bearing surface and age groups. There are several studies reporting hip joint-specific implant survival and functional outcome [17–21]. There is a paucity of data in the literature which are patient specific and joint specific. The primary aim of this study is to analyze the patient-related outcome measures including sports activities and the quality of life in patients aged 20 years and younger undergoing HRA and THA. The secondary aim is to access the implant survival including revision rate and to report the long-term outcome.
Materials and Methods
The data of 40 hips in 33 (25 males and eight females) teenage patients of both sexes aged between 13 and 19 less than 20 years who underwent THA or HRA since January 2002 with minimum 7-year follow-up period as of August 2013 were included in this prospective cohort study which was initiated in 2014. Hence, it was not a randomized controlled trial with no power analysis used similar to a study of 2012. The Shapiro–Wilk test was used to check the normality. The p value was equal to 0.001 for the scores in both the groups (THA and HRA). It can be inferred that the sample was not normally distributed. Hence, nonparametric test will be applied. The institutional ethical committee approval and informed consent were obtained from all the participating individuals. Surgical procedure included Neck Capsule Preserving (NCP) Posterior approach for all cases. Transverse Acetabular Ligament (TAL) was used as a landmark to decide on the inclination and version of the acetabular cup [22]. A pretested validated semi-structured questionnaire was prepared to access the following data: demographic profile, age at the time of surgery, past medical or surgical history, primary diagnosis as listed in the operative notes, date of admission, date of surgery, date of discharge, side of surgery, type of surgery, type of bearing surface, type of implant, pre-operative Harris Hip Score (HHS), if relevant, date of revision and type of revision is also noted. Follow-up survey was done with the Hip Disability and Osteoarthritis Outcome Score (HOOS). The HOOS is a self-report questionnaire with forty items and it has 5 subsets—pain, other symptoms including stiffness, function, sports activities and hip-related quality of life. This is a validated and highly reproducible score which is more specific for younger patients. The HOOS was built upon the Western Ontario and MacMaster Universities Index with two additional subsets, viz. sport and recreation and hip-related quality of life [23]. We also assessed the HHS post-operatively and the values at the final follow-up were noted. The HOOS pain and symptom scores were hip joint specific, while the HOOS ADL (Activities of Daily life) and sport scores were patient specific. Both the scores range from 0 to 100, with higher the score related to fewer symptoms. All efforts were made to contact the patients for follow-up using all possible modes of communication including, phone calls, emails, text messaging and snail mail. Minimum of five failed attempts to establish contact classified them as lost to follow-up. In addition to this, patient’s disability status including employment history and school dropouts was also assessed. The forty hips in thirty-three patients were further divided into two groups comprising of HRA and THA; their results were analyzed. The primary outcome is the HOOS and HHS at the final follow-up survey was noted. The secondary outcome measure was implant survival which was calculated by computing the number of years from the date of surgery till to date or date of revision surgery.
Statistical Analysis
The Shapiro–Wilk test was used to check the normality. The p value was equal to 0.001 for the scores in both the groups (THA and HRA). It can be inferred that the sample was not normally distributed. Descriptive statistics was reported as median (IQR) for continuous variables, frequencies (percentage) for categorical variables. An implant survival curve was constructed using life table method. Kaplan–Meier method was used to depict the stratification of implant survival by type of diagnosis. Cox proportion hazard models were then constructed to assess the association between covariates and implant survival. Results thus obtained were subjected to statistical analysis such as Kruskal–Wallis test, Mann–Whitney U test and Wilcoxon sign rank test. p < 0.05 was considered significant. Data were statistically evaluated with IBM SPSS Statistics for Windows, Version 20.0., IBM Corp., Chicago, IL. According to the previous published study our sample size was not less in drawing a conclusion [27].
Results
Thirty-three patients (forty hips) aged between 12 and 20 years who underwent THA/ HRA at our institution from January 2002 to December 2013 were included in our study. No patients were lost in follow-up. The mean follow-up period was 11.00 years (range 7.00–18.40). The study group had 25 males (75.25%) and eight females (24.25%). Out of thirty-three patients, seven had bilateral hip pathology. Diagnosis included ankylosing spondylitis, juvenile chronic arthritis, idiopathic osteonecrosis, postperthes disease secondary arthritis, steroid-induced osteonecrosis, post-traumatic, dysplastic secondary arthritis, idiopathic chondrolysis, post-septic secondary arthritis and enteropathic spondyloarthropathy. Most common were ankylosing spondylitis which contributed to almost 32.5%, juvenile chronic arthritis and idiopathic osteonecrosis of 17.5% each. Out of these patients, 21 (52.2%) underwent HRA and 19 (47.5%) underwent THA, respectively (Table 1).
Table 1.
Demographic profile of study participant and implant data (N = 40)
| Variable | Frequency | Percentage |
|---|---|---|
|
Total number of joint replacement Hip resurfacing arthroplasty (HRA = 21) Total hip arthroplasty (THA = 19) |
40 | |
| Total number of patients (25Male, 8Female) | 33 | |
| Time to follow-up (years) | 11.00 (7.00–18.40) | |
| Average age at time of surgery (Years) | 19.00 (12.00–20.00) | |
| Gender | ||
| Male | 25 | 75.75 |
| Female | 8 | 24.25 |
| Bearing surface | ||
| Hip resurfacing arthroplasty (HRA) | 21 | 52.5 |
| Total hip arthroplasty (THA) | ||
| Ceramic on ceramic | 13 | 32.5 |
| Ceramic on poly | 3 | 7.5 |
| Metal on metal | 3 | 7.5 |
| Diagnosis | ||
| Ankylosing spondylitis | 13 | 32.5 |
| Juvenile chronic arthritis | 7 | 17.5 |
| Idiopathic osteonecrosis | 7 | 17.5 |
| Secondary postperthes | 4 | 10.0 |
| Steroid-induced osteonecrosis | 3 | 7.5 |
| Post-traumatic | 2 | 5.0 |
| Dysplastic secondary arthritis | 1 | 2.5 |
| Idiopathic chondrolysis | 1 | 2.5 |
| Post-septic secondary arthritis | 1 | 2.5 |
| Enteropathicspondlyoarthropathy | 1 | 2.5 |
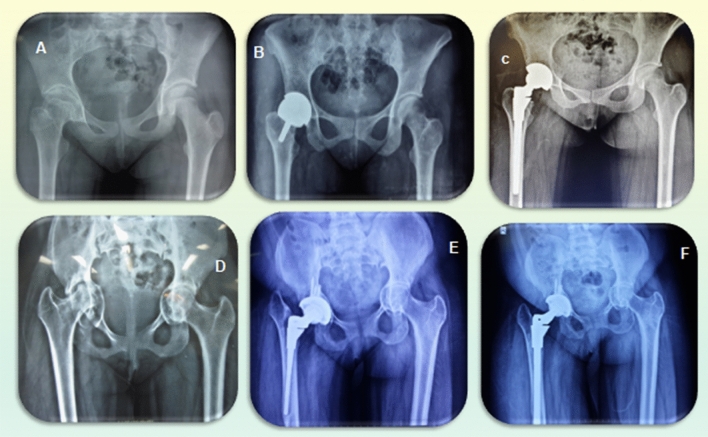
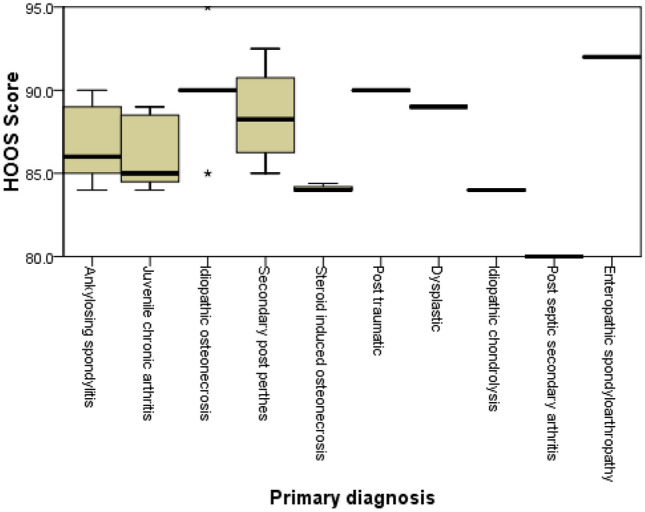
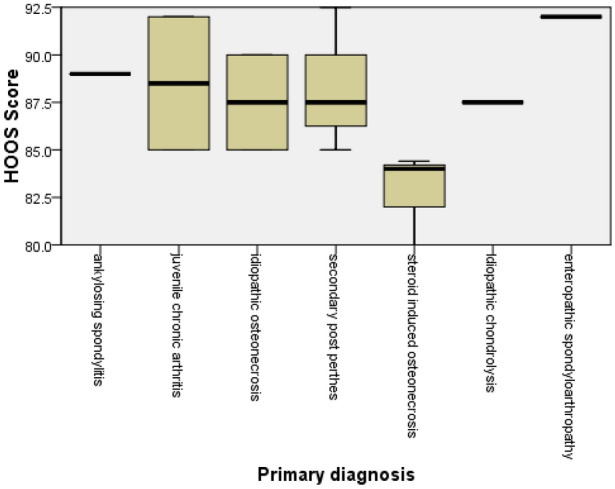
The overall median HOOS with interquartile range was 89.00 (87.63–90.00). The median HOOS at follow-up was as follows: 95.00 (90.00–95.00) for symptoms, 92.00 (90.00–95.00) pain, 87.00 (85.00–90.00) for functions, 81.00 (75.00–85.00) for sports and 94.00 (88.00–95.00) for QOL. There were significant differences in postoperative final follow-up HOOS across all diagnosis groups using one-way ANOVA (p = 0.002) (Fig. 1). The mean postoperative final follow-up HOOS of the HRA group was 87.80 ± 3.21 (Fig. 2). The mean postoperative final follow-up HOOS scores of the THA group was 89.49 ± 1.74 (Fig. 3).
Fig. 1.
Box plot showing overall mean HOOS for all primary arthroplasty stratified by primary diagnosis (N = 40)
Fig. 2.
Box plot showing mean HOOS for, hip resurfacing arthroplasty (HRA) group stratified by primary diagnosis (N = 21)
Fig. 3.
Box plot showing mean HOOS for total hip arthroplasty (THA) group stratified by primary diagnosis (N = 19)
The Mann–Whitney U test revealed that there was statistically significant difference in total HOOS scores between HRA group and THA group (U = 274.50, p = 0.03) with a mean rank of HOOS score of 16.93 for HRA group and 24.45 for THA group. The Mann–Whitney U test revealed that there was no statistically difference in HOOS scores for unilateral cases and bilateral cases, (U = 236.00, p = 0.252) with a mean rank HOOS of 22.26 for unilateral cases and 18.12 for bilateral cases. This might be attributed to the systemic involvement and disease severity in these patients. In our study, there were significant differences in HOOS across all diagnosis groups using Kruskal–Wallis test χ2(7) = 16.69, p = 0.019 (Figs. 1, 2, 3). The individual median HOOS of HRA and THA group was 89.00 (85.00–89.50) and 89.00 (89.00–90.00), respectively (Table 2).
Table 2.
Functional outcome scores (N = 40)
| Postop HOOSa Median (IQR) |
Preop HHSb Median (IQR) |
Postop HHS Median (IQR) |
|
|---|---|---|---|
| Overall (N = 40) | 89.00 (87.63–90.00) | 38.00 (32.00–42.00) | 89.50 (86.00–96.00) |
| Hip Resurfacing (N = 21) | 89.00 (85.00–89.50) | 36.00 (30.00–42.00) | 89.00 (86.00–94.50) |
| Total Hip Arthroplasty (N = 19) | 89.00 (89.00–90.00) | 38.00 (32.00–44.00) | 95.00 (86.00–99.00) |
aHOOS—Hip Disability and Osteoarthritis Outcome Score
bHHS—Harris Hip Score
In our study, there was a significant improvement in HHS following arthroplasty from preoperative 38.00 (32.00–42.00) to postoperative 89.50 (86.00–96.00) [Z = − 5.514, p < 0.001]. The HHS of HRA group improved from 36.00 (30.00–42.00) to 89.00 (86.00–94.50) [Z = − 4.016 p < 0.001] and the THA group improved from 38.00 (32.00–44.00) to 95.00 (86.00–99.00) [Z = − 3.827, p < 0.001]. There was no significant difference between HRA and THA for post-op HHS (U = 239.50, p = 0.03) with a mean rank of HOOS of 18.60 for HRA group and 22.61 for THA group.
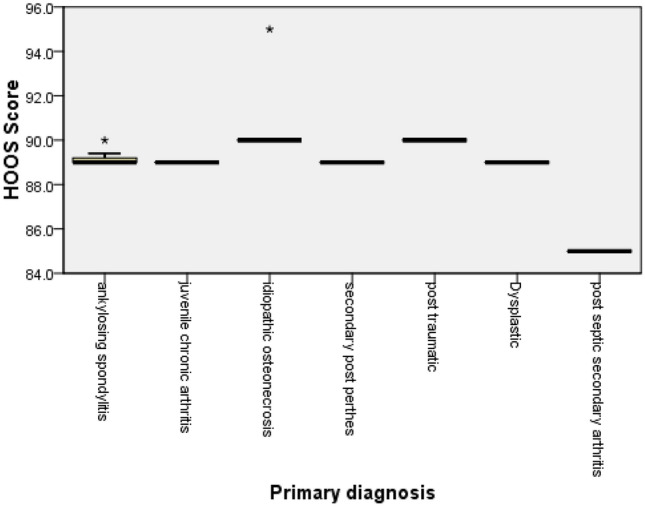
The radiological follow-up X-rays were available for all patients at the end of 5 years, none of them showed radiolucent line wider than 2 mm in all three zones of the acetabulum and no progressive subsidence or migration of > 1 mm and divergent radiopaque line in femur [28, 29]. Further, follow-up X-rays were not available, except for the two patients who came up for revision. The overall implant survival rate (with endpoint being any revision) was 100% at 5 years (CI 91–100%), 97% at 10 years (CI 83–100%) and 89.9% at 15 years (CI 58–99%) (Table 3) (Fig. 4). The implant survival rate (with endpoint being any revision) for hip resurfacing arthroplasty (HRA) group and 95% confidence interval was 100% at 5 years (CI 84–100%), 100% at 10 years (CI 83–100%) and 92% at 15 years (CI 64–99%) (Table 4) (Fig. 5). The implant survival rate (with endpoint being any revision) for total hip arthroplasty (THA) group and 95% confidence interval was 100% at 5 years (CI 82–100%) and 90% at 10 years (CI 59–100%) (Table 5) (Fig. 6). The implant survival rate (with endpoint being any revision) did not differ between the bearing surface (p = 0.28) and between the two groups (p = 0.94). Implant survival was comparatively less among females (p = 0.01), similarly implant survival differed among different diagnosis (p = 0.005) (Fig. 7). Implant survival differed by implant type (p = 0.035). The disability rate was zero.
Table 3.
Overall implant survival rate and 95% confidence interval at 5, 10 and 15 years (N = 40)
| Variable | 5-Year survival, % (95% CI) | 10-Year survival, % (95% CI) | 15-Year survival, % (95% CI) |
|---|---|---|---|
| Overall survival | 100 (91, 100) | 97 (83, 100) | 89.90 (58, 99) |
| Gender | |||
| Male | 100 (88, 100) | 100 (85, 100) | 100 (69, 100) |
| Female | 100 (69, 100) | 89 (52, 100) | 75 (19, 99) |
| Bearing surface | |||
| Resurfacing | 100 (84, 100) | 100 (83, 100) | 92(64, 99) |
| Metal on metal | 100 (29, 100) | 100 (16, 100) | – |
| Ceramic on ceramic | 100 (75, 100) | 100 (60, 100) | – |
| Ceramic on poly | 100 (29, 100) | 50 (2, 98) | – |
| Diagnosis | |||
| Ankylosing spondylitis | 100 (91, 100) | 100 (87, 100) | 100 (84, 100) |
| Juvenile chronic arthritis | 100 (77, 100) | 100 (48, 100) | 100 (3, 100) |
| Idiopathic osteonecrosis | 100 (77, 100) | 100 (16, 100) | – |
| Secondary postperthes | 100 (63, 100) | 100 (39, 100) | 100 (3, 100) |
| Steroid induced osteonecrosis | 100 (54, 100) | 100 (16, 100) | – |
| Post-traumatic | 100 (40, 100) | 100 (3, 98) | – |
| Dysplastic secondary arthritis | 100 (3, 100) | – | – |
| Idiopathic chondrolysis | 100 (3, 100) | 100 (3, 100) | 0 (0, 98) |
| Post-septic secondary arthritis | 100 (3, 100) | 0 (0, 98) | – |
| Enteropathicspondlyoarthropathy | 100 (3, 100) | 100 (3, 100) | 100 (3, 100) |
– Insufficient data
Fig. 4.
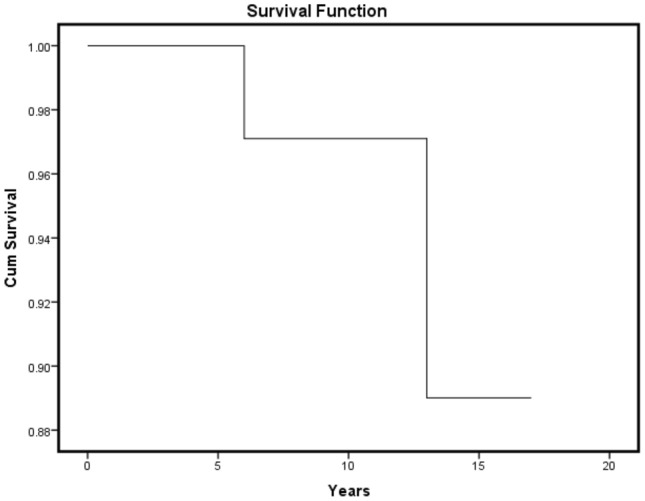
Life table curve of overall implant survival (N = 40)
Table 4.
Implant survival rate for hip resurfacing arthroplasty (HRA) group and 95% confidence interval at 5, 10 and 15 years (N = 21)
| Variable | 5-Year survival, % (95% CI) | 10-Year survival, % (95% CI) | 15-Year survival, % (95% CI) |
|---|---|---|---|
| Overall survival | 100 (84, 100) | 100 (83, 100) | 92 (64, 99) |
| Gender | |||
| Male | 100 (74, 100) | 100 (74, 100) | 100 (66, 100) |
| Female | 100 (66, 100) | 100 (63, 100) | 75 (19, 99) |
| Bearing surface | |||
| Resurfacing | 100 (84, 100) | 100 (83, 100) | 92 (64, 99) |
| Diagnosis | |||
| Ankylosing spondylitis | 100 (48, 100) | 100 (48, 100) | 100 (40, 100) |
| Juvenile chronic arthritis | 100 (54, 100) | 100 (54, 100) | 100 (30, 100) |
| Idiopathic osteonecrosis | 100 (16, 100) | 100 (16, 100) | – |
| Secondary postperthes | 100 (30, 100) | 100 (30, 100) | 100 (16, 100) |
| Steroid induced osteonecrosis | 100 (30, 100) | 100 (30, 100) | – |
| Idiopathic chondrolysis | 100 (3, 100) | 100 (3, 100) | 0 (0, 97) |
| Enteropathicspondlyoarthropathy | 100 (3, 100) | 100 (3, 100) | 100 (3, 100) |
– Insufficient data
Fig. 5.
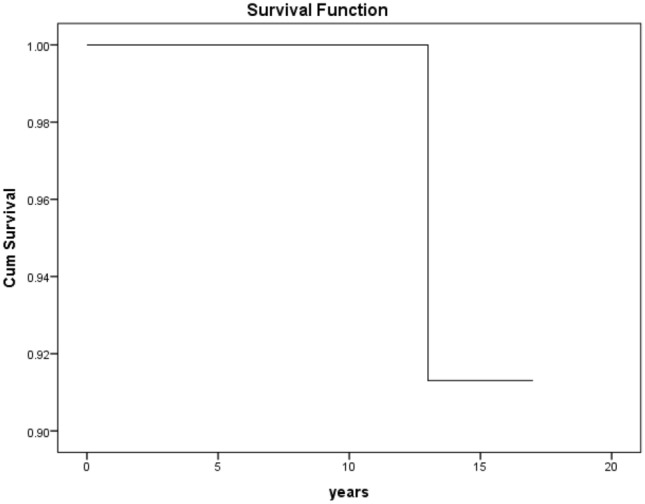
Life table curve of hip resurfacing arthroplasty (HRA) implant survival (N = 21)
Table 5.
Implant survival rate for total hip arthroplasty (THA) group and 95% confidence interval at 5, 10 and 15 years (N = 19)
| Variable | 5-Year survival, % (95% CI) | 10-Year survival, % (95% CI) | 15-Year survival, % (95% CI) |
|---|---|---|---|
| Overall survival | 100 (82, 100) | 90 (59, 100) | – |
| Gender | |||
| Male | 100 (81, 100) | 100 (70, 100) | – |
| Female | 0 (0, 97) | – | |
| Bearing surface | |||
| Metal on metal | 100 (30, 100) | 100(16, 100) | – |
| Ceramic on ceramic | 100 (75, 100) | 100 (59, 100) | – |
| Ceramic on poly | 50 (9.4, 99) | – | – |
| Diagnosis | |||
| Ankylosing spondylitis | 100 (63, 100) | – | – |
| Juvenile chronic arthritis | 100 (3, 100) | – | – |
| Idiopathic osteonecrosis | 100 (48, 100) | – | – |
| Secondary postperthes | 100 (3, 100) | 100 (3, 98) | – |
| Post-traumatic | 100 (16, 100) | 100 (16, 100) | – |
| Dysplastic secondary arthritis | 100 (16, 100) | – | – |
| Post-septic secondary arthritis | 100 (3, 100) | 0 (0, 97) | – |
– Insufficient data
Fig. 6.
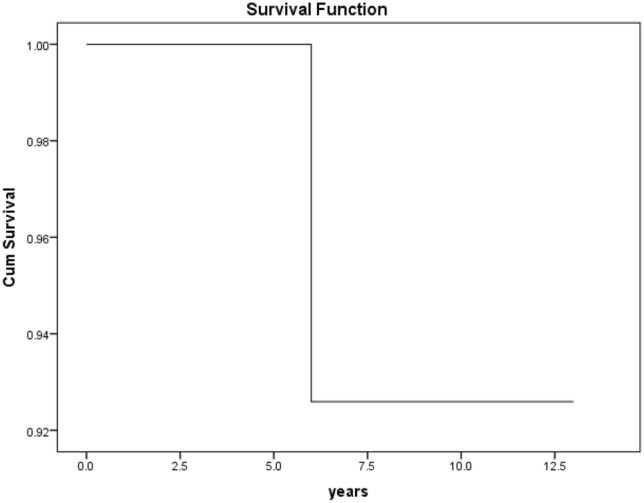
Life table curve of total hip arthroplasty (THA) implant survival (N = 19)
Fig. 7.
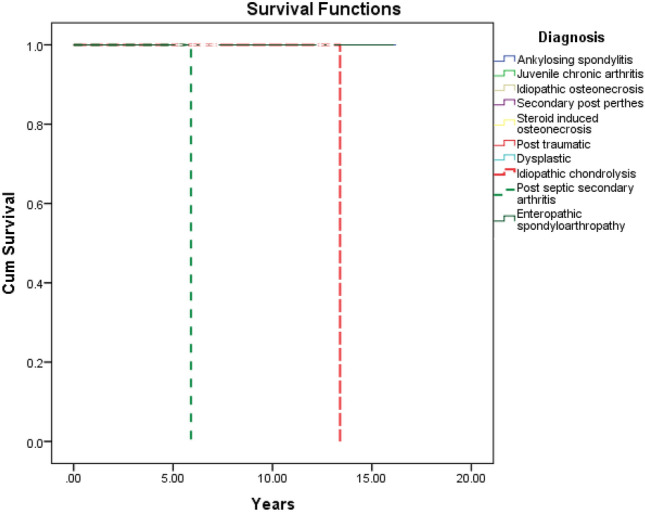
Kaplan–Meier survival curve for all primary arthroplasty stratified by primary diagnosis (N = 40)
Discussion
The principal finding of the present study is that very young patients report good functional outcome measures and hip arthroplasty for unsalvageable hip arthritis significantly improved pain, range of motion, quality of life and ability to participate in sports and recreational activities. The disability rate was zero and all the patients were able to either attend the school or employed at a mean follow-up of 11.84 years. There are only a few studies which have used validated patient-related outcome measures in this age group. Hanouche et al. reported a mean HOOS of 79 at an average follow-up of 8 years in 113 THAs under 20 years of age [24]. Swarup et al. reported a mean HOOS of 83.2 at an average of 14-year follow-up in 548 THAs under the age of 35 years [17]. Our reports are similar to this study and even better than the previous one. There is a significant increase in the HHS during the follow-up period, which is similar to the results of Ambrosi et al [25].
Pain and fatigue both are independent predictors of loss of participation in daily activities and recreational activities marked as the disability rate [25]. In our study population, all the patients had a history of failed conservative measures with severe disability being unable to attend school and work. Post-surgery the disability rate was zero and functional scores improved. All patients were able to either attend the school or employed. The 10 year and 15-year survival rate in our cohort was 97% and 89.9%, respectively, and better than the recent literature in this age group. TAL index used to place the acetabular cup in desired version and inclination, Coaxial stitch technique used to ensure correct offset with no leg length discrepancy and the NCP approach were considered to yield superior result as per the surgeon [22].
Hannouche et al. reported a survival rate of 90.3% at 10-year follow-up for 113 ceramic-on-ceramic THAs in patients younger than 20 years of age [24]. Tsukanaka et al. reported 70% implant survival rate at 10 years after primary THR in patients younger than 20 years of age. This might be attributed to the earlier use of acetabular components (Tropic, Atoll) prior to 2000, which was later shown to have higher revision rates [18]. Maclean et al. reported 90% survival rate at 5 year for a series of 146 resurfacings [19]. He related it to poor bone stock in the acetabulum, soft tissue abnormalities around the hip joint and abnormal muscular forces.
Finkbone et al. showed 96% survival rate at 52 months of follow-up for 24 THAs with ceramic-on-ceramic bearing with only one acetabular component revision in patients younger than 20 years of age [27]. This study shows good midterm follow-up. Our study shows similar results with no cases of failure in ceramic-on-ceramic bearings. In our cohort, only eight patients had 32-mm femoral head and the minimum size for the remaining patients was 36 mm. Large diameter heads are more important in this age group for improved function, stability and with least dislocation rates [30]. Nordsletten et al. (2018) showed a 70% 10-year survival rate after primary THR (with revision as endpoint). The survival rate was much better for the patients who got operated after 1996 (10 years 50% vs. 90%) with improvement in HHS 83 (15–100). 39 patients had at least 1 revision and 16 patients had 2 or more revisions. Follow-up radiographs included osteolysis and atrophy in 19% and 27% of the acetabular cup and 21% and 62% of the femoral stem, respectively [31]. Furthermore, patients in this age group were most likely to undergo more than one revision during their lifetime. Reduction in bone stock is a major concern during revision. Bone conserving methods should be followed and the proponents of resurfacing argue that revision to a THA is easier with HRA and femoral component only revision can be done in situations with a well-fixed cup [32, 33].
In our cohort, two patients underwent revision and both had only femoral component revision. The author has described the bose zones of femur, Zone 1 = femoral head with neck, Zone 2 = proximal third of femur resembling cone shape, Zone 3a = upper middle third of cylindrical femur, Zone 3b = lower middle third of cylindrical femur and Zone 4 = distal third of femur an inverted cone. The author has indicated the ladder of reconstruction during revision in very young patients. The implant fixation during revision must be limited the next zone so that bone is available for successive revision, if required. Choice of stem should be respecting this principle. Hip resurfacing implant indicated for Zone 1, standard primary low-profile taper stem with fixation in zone 2 for failure of hip resurfacing (zone 1), SROM type modular or short distal fitting stem with fixation in zone 3a for failure of primary low-profile taper stems (zone 2) and Long distal fitting stem with fixation in Zone 3b for failure of short revision stem (zone 3a). This is non-validated but is from the experience of the author and that future studies could validate the classification (Fig. 8).
Fig. 8.
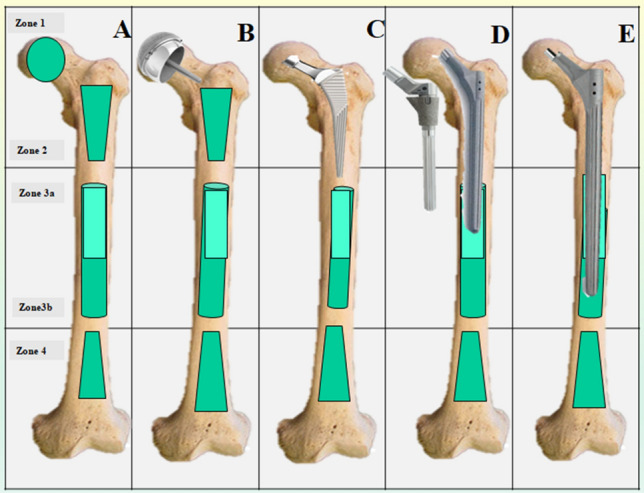
Bose zones of femur indicating the ladder of reconstruction during revision in very young patients. a Diagrammatic representation of implant fixation during revision must be limited to the next zone so that bone is available for successive revision if required. Choice of stem should be respect this principle. Zone 1 = femoral head with neck, Zone 2 = proximal third of femur resembling cone shape, Zone 3a = upper middle third of cylindrical femur, Zone 3b = lower middle third of cylindrical femur, Zone 4 = distal third of femur an inverted cone. b Hip resurfacing indicating fixation only in Zone 1. c Standard primary low-profile taper stem with fixation in zone 2 for failure of hip resurfacing (zone 1). d SROM type modular or short distal fitting stem with fixation in zone 3a for failure of primary low-profile taper stems (zone 2). e Long distal fitting stem with fixation in Zone 3b for failure of short revision stem (zone 3a)
First patient who had THA for post-septic sequelae developed thigh pain after 6 years. There was aseptic loosening of primary S-Rom and was revised with an upsized S-Rom (DePuy Warsaw, IN). The second patient who had HRA for idiopathic chondrolysis developed sudden onset of thigh pain after 13 years. The femoral component was found loose due to global avascular necrosis and was revised with S-Rom over Birmingham hip resurfacing cup with a dual mobility system. Their preoperative blood infection markers ESR (erythrocyte sedimentation rate), CRP (C-reactive protein) and the metal ion values were normal. Intraoperative findings included stable acetabular components with evidence of metallosis with histopathology ALVAL (Aseptic Lymphocyte Vasculitis Associated Lesion) score of 5/10 and 6/10, respectively (Fig. 9).
Fig. 9.
a Preoperative X-ray. b Postoperative X-ray. c Revision X-ray of the first patient. d Preoperative X-ray. e Postoperative X-ray. f Revision X-ray of the second patient who underwent revision
Limitations This study has several limitations. Being a part of an ongoing prospective study with average sample size, further long-term follow-up is needed to draw a final conclusion. Another limitation of our study is the diagnostic heterogeneity of the sample of patients. Other than the inflammatory arthropathies and osteonecrosis, the numbers of patients in other subgroups are lesser. It is difficult to draw a definitive conclusion from our comparative subgroup implant survivorship analysis. The study involves different types of arthroplasty including implant design, and materials, a majority of which are still in use. Furthermore, while reporting a surgery over a period of time, use of different types of implants is inevitable and all were treated by similar protocols in our study. Baseline HOOS data were not collected, so our ability to completely understand outcome measures is limited. Finally, this study included radiographic evaluation only till the end of 5 years and long-term follow-up X-rays regarding prosthesis loosening were missing. There was no randomization and power analysis used with personal bias of the operating surgeon in choosing the surgical procedure.
Conclusion
Our study showed good long-term results in teenage patients who underwent hip arthroplasty. The disability rate was zero with improved HOSS and HHS at the end of 11-year mean follow-up period. The good implant survival rate of 97% and 89.9% at 10 and 15 years, respectively, is in contrast to the previous studies, due to the use of modern implants with superior bearing surface and newer standard surgical techniques.
Acknowledgements
Mr. Raj, Research & Medical Documentation Incharge, Asian Joint Reconstruction Institute @ SIMS Hospitals, Chennai, India (rajdeltapro@gmail.com).
Author Contributions
VCB, MS Ortho: chief operating surgeon. KK, MS Ortho: operating surgeon, manuscript writing, MM, MS Ortho: manuscript writing, data collection, and statistics. AK and PS, MS Ortho: operating surgeon and data collection. SP, MS Ortho: statistics workup and manuscript writing. PS, MS Ortho: chief operating surgeon.
Funding
No specific financial support was received for this study.
Data Availability
Obtained.
Code availability
Obtained.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional Ethical Committee approval was obtained.
Consent for study
The study was approved by SIMS Institutional Review Board and informed consent from patients was obtained.
Consent to participate
Obtained as per institutional policy.
Consent for publication
Obtained as per institutional policy.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. The Lancet. 2007;370(9597):1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.Shan L, Shan B, Graham D, Saxena A. Total hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthritis and Cartilage. 2014;22(3):389–406. doi: 10.1016/j.joca.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 3.Bischel O, Seeger JB, Krüge M, Bitsch BG. Multiple acetabular revisions in THA—poor outcome despite maximum effort. The Open Orthopaedics Journal. 2012;6(1):488–494. doi: 10.2174/1874325001206010488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stover MD, Beaul PE, Matta JM, Mast JW. Hip arthrodesis: a procedure for the new millennium? Clinical Orthopaedics and Related Research. 2004;418:126–133. doi: 10.1097/00003086-200401000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Oryhon JM, Seyler TM, et al. Function and fixation of total hip arthroplasty in patients 25 years of age or younger. Clinical Orthopaedics and Related Research. 2010;468(12):3207–3213. doi: 10.1007/s11999-010-1468-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adelani MA, Keeney JA, Palisch A, Fowler SA, Clohisy JC. Has total hip arthroplasty in patients 30 years or younger improved? A systematic review. Clinical Orthopaedics and Related Research. 2013;471(8):2595–2601. doi: 10.1007/s11999-013-2975-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Restrepo C, Lettich T, Roberts N, Parvizi J, Hozack WJ. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthopaedica Belgica. 2008;74(5):615–622. [PubMed] [Google Scholar]
- 8.Treacy RBC, McBryde CW, Shears E, Pynsent PB. Birmingham hip resurfacing. The Journal of Bone And Joint Surgery British Volume. 2011;93-B(1):27–33. doi: 10.1302/0301-620X.93B1.24134. [DOI] [PubMed] [Google Scholar]
- 9.Daniel J, Pradhan C, Ziaee H, Pynsent PB, McMinn DJW. Results of Birmingham hip resurfacing at 12 to 15 years. The Bone & Joint Journal. 2014;96-B(10):1298–1306. doi: 10.1302/0301-620X.96B10.33695. [DOI] [PubMed] [Google Scholar]
- 10.Multani IS, Cunningham IKT, Walter WL. My current indications for hip resurfacing. Annals of Joint. 2020;5:14. doi: 10.21037/aoj.2019.12.05. [DOI] [Google Scholar]
- 11.McMinn DJ, Daniel J, Ziaee H, Pradhan C. Indications and results of hip resurfacing. International Orthopaedics. 2011;35(2):231–237. doi: 10.1007/s00264-010-1148-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shrader MW. Total hip arthroplasty and hip resurfacing arthroplasty in the very young patient. Orthopedic Clinics of North America. 2012;43(3):359–367. doi: 10.1016/j.ocl.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 13.National Joint Registry for England, Wales, Northern Ireland, and Isles of Man. National Joint Registry NJR 16th Annual Report, 2019
- 14.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2018. https://aoanjrr.sahmri.com/annual-reports-2018
- 15.Flugsrud GB, Nordsletten L, Espehaug B, Havelin LI, Meyer HE. The effect of middle-age body weight and physical activity on the risk of early revision hip arthroplasty: a cohort study of 1,535 individuals. Acta Orthopaedica. 2007;78(1):99–107. doi: 10.1080/17453670610013493. [DOI] [PubMed] [Google Scholar]
- 16.Adelani MA, Crook K, Barrack RL, Maloney WJ, Clohisy JC. What is the prognosis of revision total hip arthroplasty in patients 55 years and younger? Clinical Orthopaedics and Related Research. 2013;472(5):1518–1525. doi: 10.1007/s11999-013-3377-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swarup I, Lee Y-y, Chiu Y-f, Sutherland R, Shields M, Figgie MP. Implant survival and patient-reported outcomes after total hip arthroplasty in young patients. The Journal of Arthroplasty. 2018;33(9):2893–2898. doi: 10.1016/j.arth.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 18.Tsukanaka M, Halvorsen V, Nordsletten L, et al. Implant survival and radiographic outcome of total hip replacement in patients less than 20 years old. Acta Orthopaedica. 2016;87(5):479–484. doi: 10.1080/17453674.2016.1212180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacLean S, Evans S, Pynsent P, O'Hara J. Mid-term results for hip resurfacing in patients under 30 years old with childhood hip disorders. Acta Orthopaedica Belgica. 2015;81(2):264–273. [PubMed] [Google Scholar]
- 20.Walker RP, Gee M, Wong F, et al. Functional outcomes of total hip arthroplasty in patients aged 30 years or less: a systematic review and meta-analysis. HIP International. 2016;26(5):424–431. doi: 10.5301/hipint.5000376. [DOI] [PubMed] [Google Scholar]
- 21.Pakos EE, Paschos NK, Xenakis TA. Long term outcomes of total hip arthroplasty in young patients under 30. The Archives of Bone and Joint Surgery. 2014;2(3):157–162. [PMC free article] [PubMed] [Google Scholar]
- 22.Kanniyan K, Patil S, Ashok Kumar PSA, Suryanaryan P, Bose VC. Does the femoral head size influence outcomes after uncemented total hip arthroplasty for fused hips? A prospective study in ankylosing spondylitis. JOIO. 2020 doi: 10.1007/s43465-020-00210-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nilsdotter, A. K., Lohmander, L. S., Klässbo, M., Roos, E. M. (2003). Hip disability and osteoarthritis outcome score (HOOS)—validity and responsiveness in total hip replacement. BMC Musculoskeletal Disorders, 4(1) [DOI] [PMC free article] [PubMed]
- 24.Hannouche D, Devriese F, Delambre J, et al. Ceramic-on-ceramic THA implants in patients younger than 20 years. Clinical Orthopaedics and Related Research. 2015;474(2):520–527. doi: 10.1007/s11999-015-4546-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.D’Ambrosi R, Marciandi L, Frediani PV, Facchini RM. Uncemented total hip arthroplasty in patients younger than 20 years. Journal of Orthopaedic Science. 2016;21(4):500–506. doi: 10.1016/j.jos.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Backman CL. Arthritis Research & Therapy. 2006;8(6):221. doi: 10.1186/ar2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finkbone PR, Severson EP, Cabanela ME, Trousdale RT. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. The Journal of Arthroplasty. 2012;27(2):213–219. doi: 10.1016/j.arth.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 28.Min B-W, et al. Femoral osteolysis around the unrevised stem during isolated acetabular revision. Clinical Orthopaedics and Related Research. 2009;467(6):1501–1506. doi: 10.1007/s11999-008-0499-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engh CA, Glassman AH, Suthers KE. The case for porous-coated hip implants. The femoral side. Clinical Orthopaedics and Related Research. 1990;261:63–81. [PubMed] [Google Scholar]
- 30.Tsikandylakis G, Mohaddes M, Cnudde P, Eskelinen A, Kärrholm J, Rolfson O. Head size in primary total hip arthroplasty. EFORT Open Reviews. 2018;3(5):225–231. doi: 10.1302/2058-5241.3.170061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nordsletten L, Tsukanaka M, Halvorsen V, Engesaeter I, Engesaeter LB, Fenstad AM, Rohrl SM. Total hip arthroplasty in patients younger than 20 years. Orthopaedic Proceedings. 2018;100-B(SUPP_1):47–47. [Google Scholar]
- 32.Sakellariou VI. Management bone loss of the proximal femur in revision hip arthroplasty: update on reconstructive options. World Journal of Orthopedics. 2014;5(5):614. doi: 10.5312/wjo.v5.i5.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van de Velde SK, Loh B, Donnan L. Total hip arthroplasty in patients 16 years of age or younger. Journal of Children’s Orthopaedics. 2017;11(6):428–433. doi: 10.1302/1863-2548.11.170085.PMID:29263754;PMCID:PMC5725768. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Obtained.
Obtained.