Abstract
Background
The Edinburgh Visual Gait Score (EVGS) is a comprehensive measure of gait abnormalities in children with cerebral palsy (CP) and has good psychometric properties. However, it is cumbersome to administer and requires multiple devices to record and measure its various components. We conducted this study to determine if a smartphone video protocol could be used to improve the usability and reliability of the EVGS for daily use in a clinic setting.
Methods
We used a handheld smartphone camera with slow-motion video technology and a motion analysis application to record and measure the EVGS of 30 ambulatory children with spastic CP. We tested the inter- and intra-rater reliability of various components of the EVGS between two observers.
Results
Average age was 7 years 3 months (range 4–14 years). The mean (range) EVGS scores for the trunk, pelvis, hip, knee, ankle, and foot were 1.18 (0–3), 0.68 (0–3), 1.1 (0–4), 3.95 (1.5–7.5), 1.87 (0–4) and 4.13 (2–6.5) respectively. Total score was 12.92 (7–21.5). The mean (SD) scores for Gross Motor Function Classification System (GMFCS) levels II and III were 10.73 (3.86) and 14.96 (4.2) (p < 0.001). The intra-observer and inter-observer reliability using percentage of complete agreement was 65–98.3% and 61.7–92.5% respectively, with kappa values ranging from 0.15 to 0.87. Reliability was more for distal limb segments as compared to proximal segments.
Conclusion
We have described a simple and reliable method for quantitative OGA of children with CP, using smartphone video technology and motion analysis application, which can be performed by every clinician in an office setting.
Level of Evidence
Level III.
Keywords: Edinburgh Visual Gait Score, Smartphone, Slow-motion video, Motion analysis application, Cerebral palsy, Observational gait analysis
Introduction
Ambulatory children with cerebral palsy (CP) often present with a variety of gait abnormalities. Gait analysis forms an integral part of the clinical workup and treatment plan which is aimed at optimising their walking ability [1]. Instrumented gait analysis (IGA) provides the most accurate understanding of gait deviations in children with CP [1–3]; however, it is expensive, time consuming and requires an elaborate setup with trained personnel, to perform and interpret its results [1–3]. Observational gait analysis (OGA) is simple, quick, and less cumbersome than IGA, and can serve as an alternative to performing 3D gait analysis in places which have limited availability of IGA [2, 4, 5]. OGA has been strengthened by a number of objective and quantifiable gait assessment tools, such as, the Physician Rating Scale [6] and its variants [7], the Visual Gait Assessment Scale [8], the Observational Gait Scale [9], and the Edinburgh Visual Gait score (EVGS) [10], which allow systematisation and quantification of OGA [5]. The EVGS was developed to quantitatively analyse gait parameters in different phases of gait on recorded videos and in archived films, and is one of the most comprehensive OGA scoring systems with good psychometric properties [5, 10].
Despite being shown as a valid and reliable measure of gait abnormalities in children with cerebral palsy [10–14], the EVGS has remained more of a research tool rather than gaining wider acceptance into mainstream clinical practice. The original publication [10] reported on the various items of the EVGS and on the reliability and validity of the new score, but no details were forthcoming on the technical steps of video capture or data analysis. Subsequent reports have focused on confirming the psychometric properties of the score [11–14] or its relationship with other gait assessment tools [15], but there has been very little exploration of its practical implementation in clinical practice [16]. Most of the available literature on EVGS have described its use within the confines of the gait lab [5, 10, 13–15] and requiring multiple devices such as 1–2 video cameras for data acquisition, a computer or laptop to feed in the video data, and a special video software to analyse and measure the various gait parameters [4, 16]. All these factors make the EVGS impractical for daily use in a busy clinic setting.
With the advent of new generation smartphones, equipped with high-definition cameras and various validated applications to accurately measure distances and joint angles [17–19], recent studies have reported on the use of smartphones to record temporospatial parameters and lower limb kinematics in a variety of clinical conditions [19–21]. Slow-motion video recording capability on newer smartphones makes it possible to record high-quality sagittal and coronal gait videos at high frame rates of 120 or 240 frames per second (fps) [22], thus, allowing a more detailed analysis of each phase of gait and with higher precision and accuracy [19]. The aims of this study were to propose a technique of observational gait analysis of children with CP, using slow-motion video capture available in handheld smartphones combined with a motion analysis application to measure various parameters of the EVGS, and to test the inter- and intra-rater reliability of EVGS measurements with this technique.
Methods
We conducted a prospective, observational study in the Department of Paediatric Orthopaedics of a tertiary-care children’s hospital. Since it was a pilot study, a sample size of 30 patients was selected based on feasibility and convenience in place of statistical power. The study was approved by the Institutional Ethics Committee of our hospital (IEC-BJWHC/AP/2020/01-Version 02). Children older than 3 years of age with a diagnosis of cerebral palsy (spastic hemiplegia or diplegia) and who were able to walk with or without support, i.e. Gross Motor Function Classification System (GMFCS) [23] levels I–III were included in our study. Children with ambulatory problems due to causes other than cerebral palsy, children with CP but with higher levels of involvement (GMFCS levels IV and V), and children with motor types other than spastic CP (dystonic/hypotonic/choreoathetoid) were excluded from the study.
-
Patient preparation:
Informed consent from the parent(s) and assent from children > 7 years of age was obtained. Bony landmarks were outlined with a marking pen, including both anterior superior iliac spines, malleoli, patellae, and medial and lateral knee joint lines. We did not use rotational marker blocks at pelvic and thigh levels [10, 24] or any reflective markers over the bony prominences. All participants walked barefoot at self-selected speeds, without their prescribed orthoses.
Technique of video capture:
-
Walkway and camera placement:
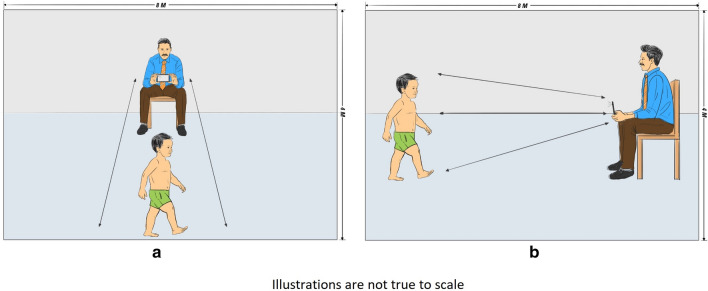
We recorded coronal and sagittal plane videos in a well-lit hallway, measuring 8 m × 4 m in area, adjacent to the outpatient clinic of the Paediatric Orthopaedic department. Thus, the walkway was 8 m long to record sagittal plane videos (Fig. 1a) with the mobile phone at a distance of 3 m from the subject. For recording the coronal plane gait videos (Fig. 1b), the camera was shifted to the opposite side of the hallway, while the participant continued to walk in the same direction. Three to five gait cycles were recorded in both planes for each participant and the best videos were selected for analysis.
-
Smartphone and video-capturing details:
A standard protocol for video recording was followed. Videos were recorded using the rear camera (12 megapixel resolution, f/2.2 aperture, 29 mm standard) of an iPhone 6s smartphone (Apple Inc., CA, USA), using the slow-motion video function at 120 fps in 1080p high definition [22]. All videos were taken from a sitting height with the mobile phone held in the hands of a videographer and level with the pelvis of the subject (Fig. 1). No tripods or stabilising devices were used, and the person recording the video remained seated on a chair for stability. The mobile phone was held still by the videographer and was not rotated or panned to follow the subject, and angles were measured towards the centre of the field to minimise error due to parallax [22].
-
Video analysis and EVGS calculation:
After satisfactory recording, all videos were screened and the best clips were selected for computation of the EVGS. The EVGS consists of 17 gait parameters measured at 6 anatomic levels (foot, ankle, knee, hip, pelvis and trunk) in the sagittal, coronal and transverse planes, that represent key features of pathological gait in children with CP [10]. The slow-motion videos were paused at the following six phases through the gait cycle: initial contact/terminal swing, mid-stance sagittal, terminal stance, mid-swing, mid-stance front, and mid-stance back, as per the described EVGS protocol. Both sides of the patients were scored separately.
To calculate the required joint angles, the selected video clips were imported into the Hudl mobile application (©Agile Sports Technologies Inc., Nebraska, USA) which is available on the Apple App store. This application allows capture of still images within a moving frame by freezing the video at the required phase of gait, and allows lines to be drawn and angles to be measured on the smartphone screen itself (Fig. 2a–f). The joint angles were calculated, and a score was assigned to each parameter as described by Read et al. [10]. Screenshots of the measurements were taken for future reference and, along with the video clips, were archived in a password-protected folder on a cloud-based file storage service (Google Drive) under a unique ID number assigned to each patient. The raw data were then deleted from the smartphone and the application, to protect patient privacy and confidentiality.
Patient preparation, video capture, data analysis and EVGS measurements were performed by two Fellows from the Paediatric Orthopaedic department of our institution. The average time taken to record the videos and score the EVGS for each patient was noted.
-
Inter- and intra-rater reliability testing:
To perform the inter and intra-rater reliability testing, two Paediatric Orthopaedic Fellows with a minimum 1-year experience in managing children with CP were given standardised training of computation of EVGS as described by Read et al. [10]. Both the observers analysed the recorded videos independently, twice at an interval of 4 weeks. The observers were blinded to their previous scores and were presented the videos in a random order each time.
Statistical analysis:
Fig. 1.
Technique of video recording (images are not true to scale). a Recording of sagittal plane videos. b Recording of coronal plane videos
Fig. 2.
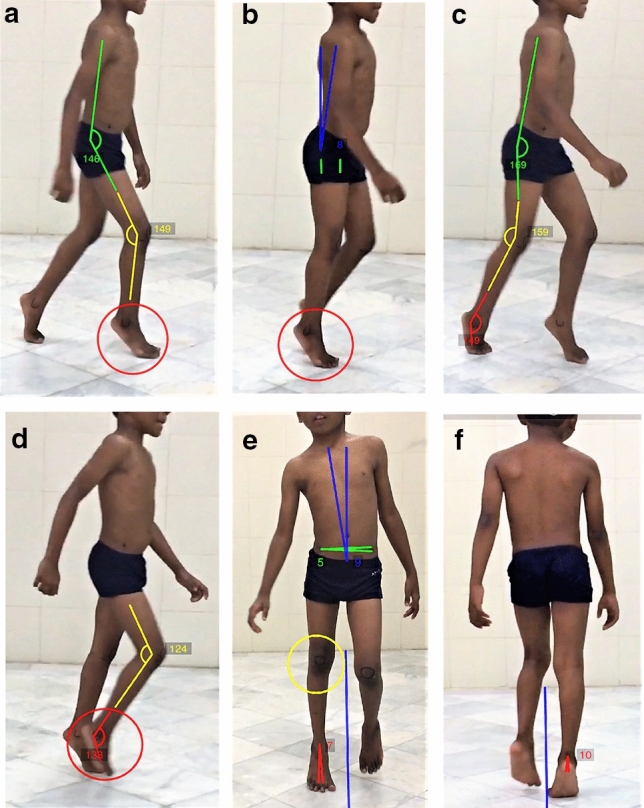
Screenshots of gait videos paused at six phases of gait to record and measure the various parameters of the Edinburgh Visual Gait Score (EVGS) in a 7-year-old child with spastic diplegia and jump gait. The total EVGS of the right side is 18/34. a Parameters of EVGS recorded at initial contact/terminal swing: foot position at initial contact, knee position at terminal swing and peak hip flexion in swing. b Parameters of EVGS recorded at mid-stance sagittal plane: heel lift, pelvic rotation and peak sagittal position of trunk. c Parameters of EVGS recorded at terminal stance: maximum ankle dorsiflexion in stance, peak knee extension in stance and peak hip extension in stance. d Parameters of EVGS recorded at mid-swing: foot clearance in swing, maximum ankle dorsiflexion in swing and peak knee flexion in swing. e Parameters of EVGS recorded at mid-stance coronal plane from front: foot rotation/progression angle, knee progression angle, pelvic obliquity at mid-stance, maximum lateral shift of trunk in stance. f Parameters of EVGS recorded at mid-stance coronal plane from back: hindfoot varus/valgus
The data were entered into an Excel spreadsheet (Microsoft® Excel® for MS Office 365 version 16.0). Statistical analysis was performed with SPSS statistics software (IBM, Armonk, NY, USA, version 20) using mean and standard deviation (SD) for numerical data. Shapiro–Wilk Test was used to determine distribution of population and the Mann–Whitney U test was used for comparison between groups. Intra-observer reliability was performed using Percentage of Complete Agreement and Bland and Altman’s Coefficient of Repeatability (CoR). Inter-observer reliability was tested using the Kappa statistic and Percentage of Complete Agreement. Grading of Kappa scores was carried out according to Landis and Koch.
Results
The salient patient demographics are described in Table 1. Shapiro–Wilk test revealed that the population was not normally distributed (p < 0.001). The EVGS scores for each body segment are summarised in Table 2. The mean (range) of the score for each lower limb segment was 4.13 (2–6.5) for the foot, 1.87 (0–4) for the ankle, 3.95 (1.5–7.5) for the knee, 1.1 (0–4) for the hip, 0.68 (0–3) for the pelvis, and 1.18 (0–3) for the trunk. The mean (SD) of the total score was 12.92 (SD 3.72; range 7–21.5). The mean (SD) gait scores of children increased as their GMFCS levels increased. The mean (SD) score of GMFCS I was 8.5 (SD 3.5), while the mean (SD) scores for GMFCS II and III patients were 10.73 (SD 3.86) and 14.96 (SD 4.2), respectively. There was a statistically significant difference between the EVGS scores of GMFCS Level II and III patients (p < 0.001). The average time to calculate the EVGS, after the videos had been recorded, was 24.7 min (16–55 min).
Table 1.
Patient demographics
| Age (years)* | 7 years 3 months (SD 3 years 3 months; range 4–14 years) | ||
| Male | 21 | ||
| Female | 9 | ||
| Motor type | |||
| Diplegia | 21 | ||
| Hemiplegia | 8 | Right: 5 | Left: 3 |
| Monoplegia | 1 | ||
| GMFCS level# | |||
| I | 1 | ||
| II | 13 | ||
| III | 16 | ||
*Age described as mean (SD; range)
#GMFCS Gross Motor Function Classification System [23]
Table 2.
Edinburgh Visual Gait Score (EVGS) [10] as per body segments
| Body segment | Foot | Ankle | Knee | Hip | Pelvis | Trunk | Total |
|---|---|---|---|---|---|---|---|
| Mean | 4.13 | 1.87 | 3.95 | 1.1 | 0.68 | 1.18 | 12.92 |
| SD | 1.15 | 1.10 | 1.62 | 0.98 | 0.75 | 0.95 | 3.72 |
Intra-Observer Reliability (Table 3)
Table 3.
Intra-observer reliability based on coefficient of repeatability (CoR)* and percentage of complete agreement
| Observer 1 | Observer 2 | |||
|---|---|---|---|---|
| Item | CoR* | % Complete agreement | CoR* | % Complete agreement |
| Foot position initial contact | 0.5 | 93.3 | 0.3 | 98.3 |
| Heel lift in stance | 0.9 | 76.7 | 1 | 80 |
| Foot clearance in swing | 1.1 | 70 | 0.4 | 96.7 |
| Foot progression angle | 1.1 | 78.3 | 0.7 | 86.7 |
| Hindfoot varus/valgus | 1.1 | 66.7 | 0.5 | 93.3 |
| Max ankle dorsiflexion in swing | 0.8 | 86.7 | 0.6 | 91.7 |
| Max ankle dorsiflexion in stance | 0.7 | 86.7 | 0.4 | 96.7 |
| Knee progression angle | 1 | 75 | 0.7 | 88.3 |
| Knee position terminal swing | 0.9 | 85 | 0.4 | 95 |
| Peak knee flexion in swing | 1.1 | 71.7 | 0.6 | 90 |
| Peak knee extension in stance | 0.9 | 85 | 0.4 | 95 |
| Peak hip flexion in swing | 1 | 73.3 | 0.6 | 96.7 |
| Peak hip extension in stance | 0.9 | 80 | 0.5 | 93.3 |
| Pelvic rotation at mid-stance | 1.2 | 80 | 1 | 73.3 |
| Pelvic obliquity at mid-stance | 1 | 73.3 | 1 | 73.3 |
| Max lateral shift of trunk | 1.2 | 68.3 | 0.9 | 80 |
| Peak sagittal position of trunk in stance | 1.3 | 65 | 1.1 | 78.3 |
Intra-observer reliability was satisfactory as seen by the percentage of complete agreement, which for Observer 1 ranged from 65 to 93.3% and for Observer 2 ranged from 73.3 to 98.3%. The mean Coefficient of Repeatability was 0.98 and 0.65 for Observers 1 and 2, respectively. The maximum intra-observer reliability was for foot position at initial contact for both the observers, with percentage of complete agreement of 93.3% and 98.3%.
Inter-Observer Reliability (Table 4)
Table 4.
Inter-observer reliability based on kappa value and percentage of complete agreement
| Item | Kappa value | % of complete agreement | Level of agreement | Rank (by kappa value) |
|---|---|---|---|---|
| Foot position initial contact | 0.87 | 92.5 | Almost perfect | 1 |
| Heel lift in stance | 0.64 | 76.7 | Substantial | 4 |
| Foot clearance in swing | 0.49 | 74.2 | Moderate | 8 |
| Foot progression angle | 0.54 | 75 | Moderate | 6 |
| Hindfoot varus/valgus | 0.45 | 70 | Moderate | 11 |
| Max ankle dorsiflexion in swing | 0.52 | 69.2 | Moderate | 7 |
| Max ankle dorsiflexion in stance | 0.6 | 73.3 | Moderate | 5 |
| Knee progression angle | 0.36 | 65 | Fair | 12 |
| Knee position terminal swing | 0.68 | 79.2 | Substantial | 2 |
| Peak knee flexion in swing | 0.46 | 67.5 | Moderate | 10 |
| Peak knee extension in stance | 0.68 | 79.2 | Substantial | 3 |
| Peak hip flexion in swing | 0.21 | 65 | Fair | 15 |
| Peak hip extension in stance | 0.49 | 68.3 | Moderate | 9 |
| Pelvic rotation at mid-stance | 0.15 | 70 | Slight | 16 |
| Pelvic obliquity at mid-stance | 0.13 | 65.8 | Slight | 17 |
| Max lateral shift of trunk | 0.31 | 70 | Fair | 14 |
| Peak sagittal position of trunk in stance | 0.34 | 61.7 | Fair | 13 |
The percentage of complete agreement for both observers ranged between 61.7 and 92.5%. Here too, the maximum agreement was for foot position at initial contact, with percentage of complete agreement of 92.5% and a kappa value of 0.87 suggesting almost perfect agreement. For individual measurements, the reliability was almost perfect (kappa 0.81–1) for one item, substantial (kappa 0.61–0.80) for three items, moderate (kappa 0.41–0.60) for seven items, fair (0.21–0.60) for four items and slight (0–0.20) for two items of the EVGS.
Discussion
The EVGS has been validated by several studies to be a psychometrically sound, quantitative OGA scale, for use by experienced and non-experienced observers [12–14], with good intra- and inter-observer reliability [10, 13], good concurrent validity with other gait assessments [4, 15, 25], and with adequate sensitivity to detect changes after physiotherapy [16] and multilevel surgery [26]. However, the paucity of information in the literature regarding the technical aspects of video recording and data capture, and lack of practical guidelines have precluded the EVGS from becoming a tool that can be easily implemented in a busy clinical setting [16]. The added requirement of multiple electronic devices and advanced computer-based video software for data acquisition and interpretation [10, 13–16] defeats the intended purpose of making the EVGS a simple, practical, user-friendly and cost-effective tool for daily use.
A few recent studies have reported on the use of smartphone motion analysis applications to record frontal and sagittal plane lower limb kinematics while walking, running or performing other functional activities [19–21]. Finkbiner et al. found no significant differences between measures recorded by the Hudl smartphone application when compared to those recorded by the 3D motion capture system, thus, validating the use of this application to measure sagittal plane kinematics in the clinical setting [19]. Mousavi et al. reported excellent test–retest and inter-rater/intra-rater reliability with the Coach’s Eye (TechSmith Corporation, MI, USA) smartphone motion analysis application in measuring lower limb kinematics during treadmill running in 20 healthy female runners [20]. Borel et al. reported increased inter-rater reliability when using the Dartfish (Fribourg, Switzerland) video analysis software for observational gait analysis in children with CP [27]. However, there is no study till date which has reported on the use of smartphone-based slow-motion video technology and motion analysis applications on a single mobile device, to perform OGA using the EVGS in children with CP.
Smartphones have become ubiquitous and are being used increasingly in clinical practice, education and research across the world [19, 28]. Newer smartphones can record videos in high definition and have a facility of slow-motion video recording [22], allowing a more detailed analysis of each event in the gait cycle [19]. A higher frame rate of > 60 fps allows frame-by-frame analysis of each parameter under scrutiny, thereby improving inter-rater reliability, while also reducing measurement errors of selected gait parameters such as initial contact and toe-off [20]. Over 2000 different models of medium-range and high-end smartphones (both Android and Apple) made by the top-selling smartphone manufacturers in 2019–2020 have availability of built-in slow-motion video technology. The additional use of validated motion analysis applications, which are freely available for smartphones, helps improve the accuracy of kinematic measurements [18–20, 27]. These apps allow video playback at multiple slow-motion speeds, split screen and scrolling facilities for frame-by-frame analysis, and pan and zoom functions that allow access to all important details of the gait video. They also have drawing tools which allow lines to be drawn and angles to be measured on the smartphone screen itself. The use of such comprehensive applications have been shown to enhance the reliability of video gait analysis without much affecting the calculation times [18–20, 27]. While we used the Hudl app, which is ideal for Apple smartphone users, there are several other motion analysis apps such as Coach’s Eye (TechSmith Corporation, MI, USA), CoachNow (Shotzoom LLC, AZ, USA), and myDartfish Express (Fribourg, Switzerland) that are available for the Android platform.
Our study has demonstrated the reliability of recording and analysing the various parameters of the EVGS on a single smartphone device, using slow-motion video technology and mobile-based motion analysis applications that are readily available on current smartphones. The percentage of complete agreement between observers in our study was between 61.7 and 92.5% and our intra-observer reliability was 65–98.3%, which correlates well with the 60–95% reliability reported by previous studies [10, 13, 14]. The reliability of EVGS items in our study was better for distal anatomic levels compared to proximal levels, as reported in previous studies [10–14], with kappa values ranging from 0.45 to 0.87 for the foot and ankle, 0.36–0.68 for the knee and 0.21–0.49 for the hip. Reliability was least at the pelvic level, with kappa values of 0.13 and 0.15 for pelvic obliquity and pelvic rotation in mid-stance, respectively. Sagittal plane parameters demonstrated better reliability (mean kappa = 0.54) than coronal plane (mean kappa = 0.30) and transverse plane parameters (mean kappa = 0.34), which has been borne out in other studies too [10, 13, 14]. The mean Coefficient of Repeatability (CoR) for the two observers in our study was 0.82 compared to mean CoR scores of 5.15 for inexperienced observers and 4.21 for experienced observers, in the study by Ong et al. [12]. Our observers were not particularly experienced in gait analysis and, since our institution lacks a 3D instrumented gait lab, have not had any training in 3D motion analysis. Yet the intra- and inter-observer reliability in our study was substantially higher than that demonstrated by inexperienced observers in the studies by Ong et al. [12] and Orozco et al. [14] across all items of the EVGS. Our study has also demonstrated a correlation between the EVGS and the GMFCS levels of children with CP, with a statistically significant difference between GMFCS levels II and III, as in the study by Robinson et al. [15].
Our study has some limitations. We were unable to establish concurrent validity with instrumented gait analysis which is the ‘gold standard’ for measuring gait deviations in children with CP. We did not have access to a motion analysis laboratory and the incentive to use OGA arose from lack of a 3D gait laboratory to evaluate gait abnormalities in children with CP. However, previous studies have confirmed good validity between most items of the EVGS and 3D gait analysis [10, 12, 14], and the Hudl motion analysis application has been validated as a reliable measure of sagittal plane kinematics in healthy subjects [19]. The reliability of knee progression angle in the transverse plane was the single variable in our study that differed markedly from other studies (0.36 v/s 0.72) [10, 14]. We did not use rotational marker blocks on the pelvis or thighs as recommended by other studies [10, 24], which may have affected the accuracy of this item [13]. However, we wished to simplify the process of OGA and make it practical and cost-effective for daily implementation by avoiding complex patient preparation tools that are not readily available in a clinic setting.
The ability of smartphone technology to record and measure gait videos in a reliable and consistent manner opens up myriad opportunities in the field of OGA. Screenshots of gait deviations recorded and measured on gait videos, paused at appropriate phases of the gait cycle, can be archived and preserved as a permanent record on a patient’s electronic medical file to assist in future assessments. The EVGS has traditionally been used to quantify the severity of gait deviations at different anatomic levels [10–15] and as an outcome measure to evaluate the effectiveness of an intervention [16, 26]. We propose that using our EVGS smartphone protocol, it may be possible to adapt this tool for qualitative analysis of specific gait patterns using the EVGS framework as a template to report key kinematic findings at multiple anatomic levels. This would aid in the decision-making process and thus improve the utility of the EVGS in clinical practice.
Conclusion
By combining the easy availability of smartphones equipped with high-definition slow-motion video technology and motion analysis applications with the strong psychometric properties of EVGS, we have developed a method of OGA that is user-friendly and practical to be implemented by every clinician. We have attempted to simplify and standardise the protocol for consistent and reliable video capture using a smartphone within the clinic space, without the need for additional specialised equipment.
Acknowledgements
The authors thank the administration of Bai Jerbai Wadia Hospital for Children, Mumbai, India for permission to utilize hospital data. We thank Miss Rachita A. Karnik for illustrating Fig. 1a, b and Mr. Ramesh Patil for helping with the statistical analysis.
Author Contributions
AA was responsible for the study conceptualization and design. Material preparation, data collection and analysis were performed by BS and SC. The first draft of the manuscript was written by BS and AA, and SC made major edits, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Funding
This study has no funding support.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
Approval was obtained from the Institutional Ethics Committee—Bai Jerbai Wadia Hospital for Children (IEC-BJWHC/AP/2020/01-Version 02).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that participants provided informed consent for publication of the images in Fig. 2.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Alaric Aroojis, Email: aaroojis@gmail.com.
Bhushan Sagade, Email: sagadebs@gmail.com.
Suresh Chand, Email: sureshdocucms@gmail.com.
References
- 1.Narayanan UG. The role of gait analysis in the orthopaedic management of ambulatory cerebral palsy. Current Opinion in Pediatrics. 2007;19:38–43. doi: 10.1097/MOP.0b013e3280118a6d. [DOI] [PubMed] [Google Scholar]
- 2.Harvey A, Gorter JW. Video gait analysis for ambulatory children with cerebral palsy: why, when, where and how! Gait Posture. 2011;33:501–503. doi: 10.1016/j.gaitpost.2010.11.025. [DOI] [PubMed] [Google Scholar]
- 3.Wright JG. Pro: interobserver variability of gait analysis. Journal of Pediatric Orthopaedics. 2003;23:288–289. [PubMed] [Google Scholar]
- 4.Bella GP, Rodrigues NB, Valenciano PJ, Silva LM, Souza RC. Correlation among the visual gait assessment scale, Edinburgh Visual Gait Scale and observational gait scale in children with spastic diplegic cerebral palsy. Review of Brasil Fisioterap. 2012;16:134–140. doi: 10.1590/S1413-35552012000200009. [DOI] [PubMed] [Google Scholar]
- 5.Rathinam C, Baterman A, Peirson J, Skinner J. Observational gait assessment tools in paediatrics—a systematic review. Gait Posture. 2014;40:279–285. doi: 10.1016/j.gaitpost.2014.04.187. [DOI] [PubMed] [Google Scholar]
- 6.Koman LA, Mooney JF, Smith B, Goodman A, Mulvaney T. Management of cerebral palsy with botulinum-A toxin: preliminary investigation. Journal of Pediatric Orthopedics. 1993;13:489–495. doi: 10.1097/01241398-199307000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Corry IS, Cosgrove AP, Duffy CM, McNeill S, Taylor TC, Graham HK. Botulinum toxin A compared with stretching casts in the treatment of spastic equinus: a randomised prospective trial. Journal of Pediatric Orthopedics. 1998;18:304–311. [PubMed] [Google Scholar]
- 8.Dickens WE, Smith MF. Validation of a visual gait assessment scale for children with hemiplegic cerebral palsy. Gait Posture. 2006;23:78–82. doi: 10.1016/j.gaitpost.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Araújo PA, Kirkwood RN, Figueiredo FM. Validity and intra- and inter-rater reliability of the Observational Gait Scale for children with spastic cerebral palsy. Review of Brasil fisioterap. 2009;13:267–273. doi: 10.1590/S1413-35552009005000033. [DOI] [Google Scholar]
- 10.Read HS, Hazlewood ME, Hillman SJ, Prescott RJ, Robb JE. Edinburgh visual gait score for use in cerebral palsy. Journal of Pediatric Orthopedics. 2003;23:296–301. [PubMed] [Google Scholar]
- 11.Maathuis KG, van der Schans CP, van Iperen A, Rietman HS, Geertzen JH. Gait in children with cerebral palsy: observer reliability of physician rating scale and Edinburgh Visual Gait Analysis Interval Testing scale. Journal of Pediatric Orthopedics. 2005;25:268–272. doi: 10.1097/01.bpo.0000151061.92850.74. [DOI] [PubMed] [Google Scholar]
- 12.Ong AM, Hillman SJ, Robb JE. Reliability and validity of the Edinburgh Visual Gait Score for cerebral palsy when used by inexperienced observers. Gait Posture. 2008;28:323–326. doi: 10.1016/j.gaitpost.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Viehweger E, Zurcher PL, Helix M, Rohon MA, Jacquemier M, Sacvarda D, et al. Influence of clinical and gait analysis experience on reliability of observational gait analysis (Edinburgh Gait Score Reliability) Annal Physical Rehabilitation and Medicine. 2010;53:535–546. doi: 10.1016/j.rehab.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 14.del Pilar Duque M, Orozco O, Abousamra C, Church N, Lennon J, Henley KJR, et al. Reliability and validity of Edinburgh Visual Gait Score as an evaluation tool for children with cerebral palsy. Gait Posture. 2016;49:14–18. doi: 10.1016/j.gaitpost.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 15.Robinson LW, Clement N, Fullarton M, Richardson A, Herman J, Henderson G, et al. The relationship between the Edinburgh Visual Gait Score, the Gait Profile Score and GMFCS levels I-III. Gait Posture. 2015;41:741–743. doi: 10.1016/j.gaitpost.2015.01.022. [DOI] [PubMed] [Google Scholar]
- 16.Tzikalagia T, Ramdharry G. Using the Edinburgh Visual Gait Score to assess gait in children with cerebral palsy: a feasibility evaluation. International Journal of Therapy and Rehabilitation. 2017;24:419–426. doi: 10.12968/ijtr.2017.24.10.419. [DOI] [Google Scholar]
- 17.Vohralik SL, Bowen AR, Burns J, Hiller CE, Nightingale EJ. Reliability and validity of a smartphone app to measure joint range. American Journal of Physical Medicine and Rehabilitation. 2015;94:325–330. doi: 10.1097/PHM.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 18.Maykut JN, Taylor-Haas JA, Paterno MV, DiCesare CA, Ford KR. Concurrent validity and reliability of 2D kinematic analysis of frontal plane motion during running. International Journal of Sport and Physical Theory. 2015;10:136–146. [PMC free article] [PubMed] [Google Scholar]
- 19.Finkbiner MJ, Gaina KM, McRandall MC, Wolf MM, ReidAdams KB, et al. Video movement analysis using smartphones (ViMAS): a pilot study. J Vis Exp. 2017;121:1–7. doi: 10.3791/54659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mousavi SH, Hijmans JM, Moeini F, Rajabi R, Ferber R, van der Worp H, et al. Validity and reliability of a smartphone motion analysis app for lower limb kinematics during treadmill running. Physical Theory and Sport. 2020;43:27–35. doi: 10.1016/j.ptsp.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Neal BS, Lack SD, Barton CJ, Birn-Jeffrey A, Miller S, Morrissey D. Is markerless, smart phone recorded two-dimensional video a clinically useful measure of relevant lower limb kinematics in runners with patellofemoral pain? A validity and reliability study. Physical Theory and Sport. 2020;43:36–42. doi: 10.1016/j.ptsp.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Knight, J., (2019) These are slo-mo specs you should look for in your next phone. Available from: https://smartphones.gadgethacks.com/how-to/these-are-slow-mo-specs-you-should-look-for-your-next-phone-0195741/. Accessed 2 Oct 2020.
- 23.Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH. Content validity of the expanded and revised gross motor function classification system. Developmental Medicine and Child Neurology. 2008;50:744–750. doi: 10.1111/j.1469-8749.2008.03089.x. [DOI] [PubMed] [Google Scholar]
- 24.Hillman SJ, Hazlewood ME, Loudon I, Robb JE. Can transverse plane rotations be estimated from video gait analysis? Gait Posture. 1998;8:87–90. doi: 10.1016/S0966-6362(98)00028-9. [DOI] [PubMed] [Google Scholar]
- 25.Hillman SJ, Hazlewood ME, Schwartz MH, van der Linden ML, Robb JE. Correlation of the Edinburgh gait score with the Gillette gait index, the Gillette functional assessment questionnaire, and dimensionless speed. Journal of Pediatric Orthopedics. 2007;27:11–17. doi: 10.1097/BPO.0b013e31802b7104. [DOI] [PubMed] [Google Scholar]
- 26.Gupta S, Raja K. Responsiveness of Edinburgh Visual Gait Score to orthopedic surgical intervention of the lower limbs in children with cerebral palsy. American Journal of Physical Medicine and Rehabilitation. 2012;91:761–767. doi: 10.1097/PHM.0b013e31825f1c4d. [DOI] [PubMed] [Google Scholar]
- 27.Borel S, Schneider P, Newman CJ. Video analysis software increases the interrater reliability of video gait assessments in children with cerebral palsy. Gait Posture. 2011;33:727–729. doi: 10.1016/j.gaitpost.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 28.Mobasheri MH, King D, Johnston M, Gautama S, Purkayastha S, Darzi A. The ownership and clinical use of smartphones by doctors and nurses in the UK: a multicentre survey study. BMJ Innovations. 2015;1:174–181. doi: 10.1136/bmjinnov-2015-000062. [DOI] [Google Scholar]