Abstract
Aim
The objective of the study is to compare the accuracy of implant positioning and limb alignment achieved in robotic-arm assisted total knee arthroplasty(RATKA) and manual total knee arthroplasty(MTKA) to their respective preoperative plan.
Patients and methods
This was a prospective observational study conducted in a tertiary care centre between August 2018 and January 2020. 143 consecutive RATKA(105 patients) and 151 consecutive MTKA(111 patients) performed by two experienced arthroplasty surgeons were included. Two independent observers evaluated the accuracy of implant positioning by measuring the radiological parameters according to the Knee-Society-Roentgenographic-Evaluation-System and limb alignment from postoperative weight-bearing scanogram. Outcomes were defined, based on the degree of deviation of measurements from the planned position and alignment, as excellent(0–1.99°), acceptable(2.00–2.99°) and outlier(≥ 3.00°).
Results
There were no systematic differences in the demographic and baseline characteristics between RATKA and MTKA. Statistically significant outcomes were observed favouring robotic group for postoperative mechanical axis (p < .001), coronal inclination of the femoral component (p < 0.001), coronal inclination of tibial component (p < 0.001), and sagittal inclination of tibial component (p < 0.001). There was no significant difference in the sagittal inclination of the femoral component (p = 0.566). The percentage of knees in the 'excellent' group were higher in RATKA compared to MTKA. There was absolutely no outlier in terms of limb alignment in the RATKA group versus 23.8% (p < 0.001) in the MTKA group. All the measurements showed high interobserver and intraobserver reliability.
Conclusion
Robotic-arm assisted TKA executed the preoperative plan more accurately with respect to limb alignment and implant positioning compared to manual TKA, even when the surgeons were more experienced in the latter.
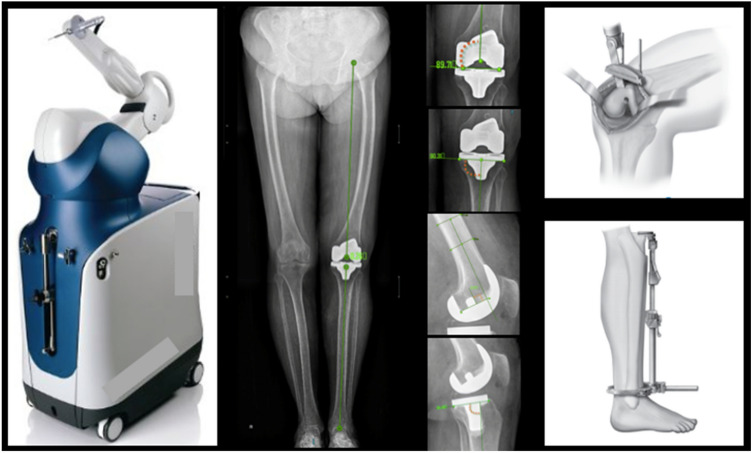
Graphic abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s43465-020-00324-y.
Keywords: Arthroplasty, Robotic surgery, Robotic-arm assisted, Manual, Total knee arthroplasty, Osteoarthritis, Accuracy, Radiology, Implant position, Limb alignment
Introduction
Osteoarthritis is the most common degenerative joint disease and a significant cause of pain and disability in adults [1]. Total knee arthroplasty (TKA) is one of the most commonly performed safe and efficient surgeries for advanced osteoarthritis. Despite the recent advances in the design of the implants and progress in technology, the dissatisfaction rates among patients are still about 15–20% [2–4].
Of many factors, which influence the outcome after a TKA, accurate implant alignment, and soft-tissue balance plays a vital role in treatment success and implant longevity [5]. Not all, but many studies have shown that post-surgical mechanical axis deviation more than three degrees from neutral in the coronal plane is associated with reduced survivability of implants [6–8]. Recently the concept of kinematic alignment has been of great interest. It aims at restoring the tibio-femoral joint line and soft-tissue balance with respect to the pre-arthritic or constitutional state of the knee joint [9, 10]. So, whether the surgeon is aiming for mechanical alignment or the kinematic alignment, the perfect execution of preoperative planning plays a pivotal role in the success of the surgery.
Tools such as computer-assisted navigation have shown to improve the accuracy of implant positioning by providing the patient-specific data to the computer, which provides live kinematic information on-screen during surgery [11]. However, the bone preparation is done manually, and there is no active restraint on the surgeon [12]. Hence, robotic-arm assisted systems were developed, leading to a further reduction in errors. Over the last decade, there were considerable improvements in the robotic systems with different platforms and interfaces compared to their less versatile predecessors [13, 14].
Majority of the studies available in the literature on the precision of implant positioning in robotic-arm assisted TKA had limited sample sizes or were done on cadavers under experimental conditions. To our knowledge, this study appears to be the largest till date and first of its kind done in the Indian subcontinent. Here, we aim to compare the accuracy of implant positioning and limb alignment in robotic-arm assisted total knee arthroplasty (RATKA) and manual total knee arthroplasty (MTKA) with respect to the preoperatively planned position and alignment.
Patients and Methods
We did a prospective observational study of 143 consecutive RATKA (105patients) and 151 MTKA (111 patients) in a tertiary-care centre between August 2018 and January 2020, after obtaining institutional review board approval. The surgeries were performed by two senior arthroplasty surgeons with over twenty years of experience, who had undergone cadaveric RATKA training in 2018. The initial 25 cases of RATKA were not included in the study considering the learning curve involved. Primary osteoarthritis knee patients with mechanical axis measured between 0 and 20° of varus undergoing primary TKA were included. Patients with a history of previous surgeries on knee or hips, neurological issues, body mass index of over 40 kg/m2 and instability, which cannot be treated by cruciate-retaining or cruciate-sacrificing implants, were excluded.
Both groups underwent TKA using a medial parapatellar approach under spinal anaesthesia. We used cemented Triathlon Cruciate Retaining (CR) and Posterior Stabilized (PS) implants (Stryker, Mahwah, New Jersey) for the RATKA group and cemented PS Destiknee (Meril, Vapi, India) implants for the MTKA group.
Operative Techniques
Robotic-arm Assisted Total Knee Arthroplasty
For RATKA, we used the MAKO RIO Robotic Interactive Orthopaedic Arm (Stryker, Mahwah, New Jersey) system. Here the surgeon plans the size and orientation of the implant on a 3D model of the patient's bony anatomy created from preoperative computed tomography (CT) scan. The component positioning with regard to the coronal and the sagittal planes were done on a case-by-case basis. Intraoperatively, after bone registration, the surgeon analyses the kinematic data to make fine adjustments to the preoperative plan before bone preparation. This final plan was recorded and later analysed against postoperative measurements. Bone preparation was done within a virtual haptic boundary, which assists the surgeon in executing resections according to the plan. Once, a satisfactory balance has been achieved, the final implants were manually cemented in place and wound closed in layers.
Manual Total Knee Arthroplasty
For MTKA, we used the preoperative weight-bearing scanogram, lateral knee X-ray, skyline view patella for templating and planning. Valgus correction angle was measured as the angle between the mechanical and anatomical axis of the femur [15]. The distal femoral cut was made accordingly so as to get it perpendicular to the mechanical axis. It was planned to keep the femoral and tibial components perpendicular to the mechanical axis in the coronal plane, the femoral component in the sagittal plane with flexion of zero degrees and the posterior tibial slope at three degrees. The soft tissue balancing was done by gap balancing technique. Bone preparation was done using an intramedullary jig system for the femur and extramedullary set for the tibia. After trialing, once satisfactory balance and alignment have been achieved, the real implants were cemented in place and wound closed in layers.
Radiographic Analysis
Two orthopaedic surgeons other than the surgeons who performed the surgeries assessed the radiological parameters independently. The parameters were measured according to the Knee Society Roentgenographic Evaluation System [16]. The radiographic evaluation was done on the postoperative weight-bearing scanogram and lateral knee X-rays taken at 6 weeks review. The parameters measured were the mechanical axis and the coronal and sagittal alignment of the femoral and tibial component. (Figs. 1, 2 and 3). The outcomes were defined based on the degree of deviation as 'excellent' when it was between 0 and 1.99°, 'acceptable' when between 2 and 2.99° and as an 'outlier' when the deviation is more than or equal to 3° from the preoperatively planned position [17, 18]. Interobserver and intra-observer reliability were tested, with the re-measurements done after one month from the first measurement.
Fig. 1.
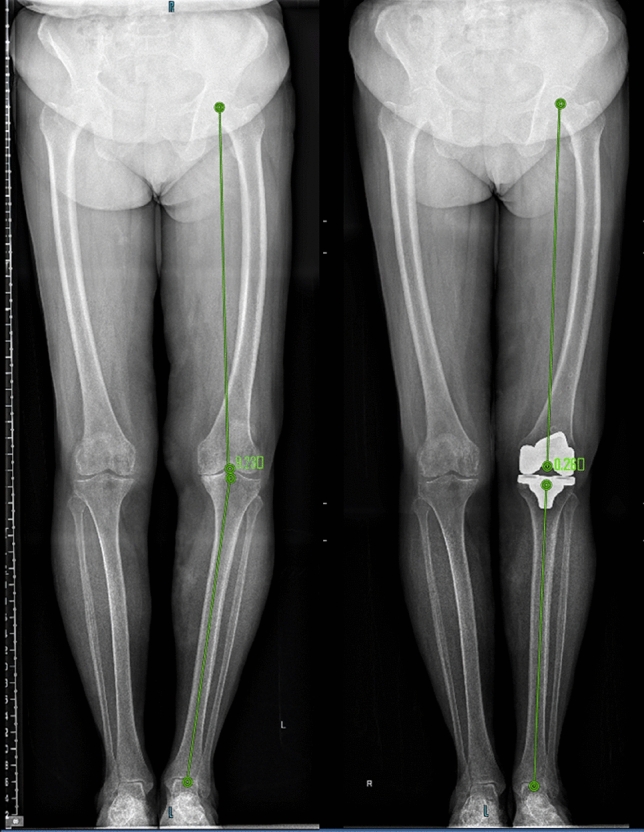
Measurement of Preoperative and Postoperative Mechanical Axis
Fig. 2.
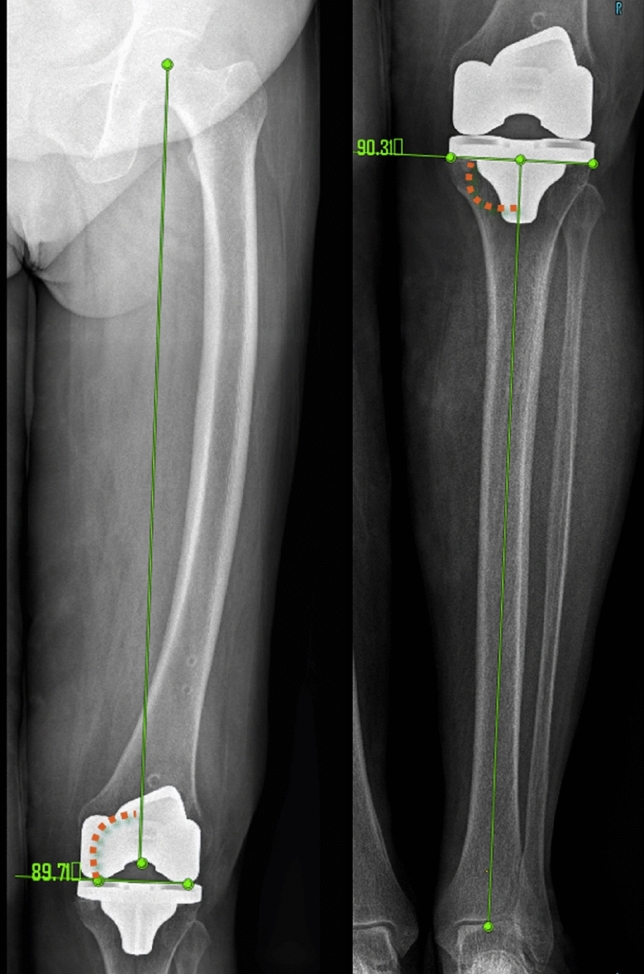
Measurement of coronal inclination of femoral and tibial components
Fig. 3.
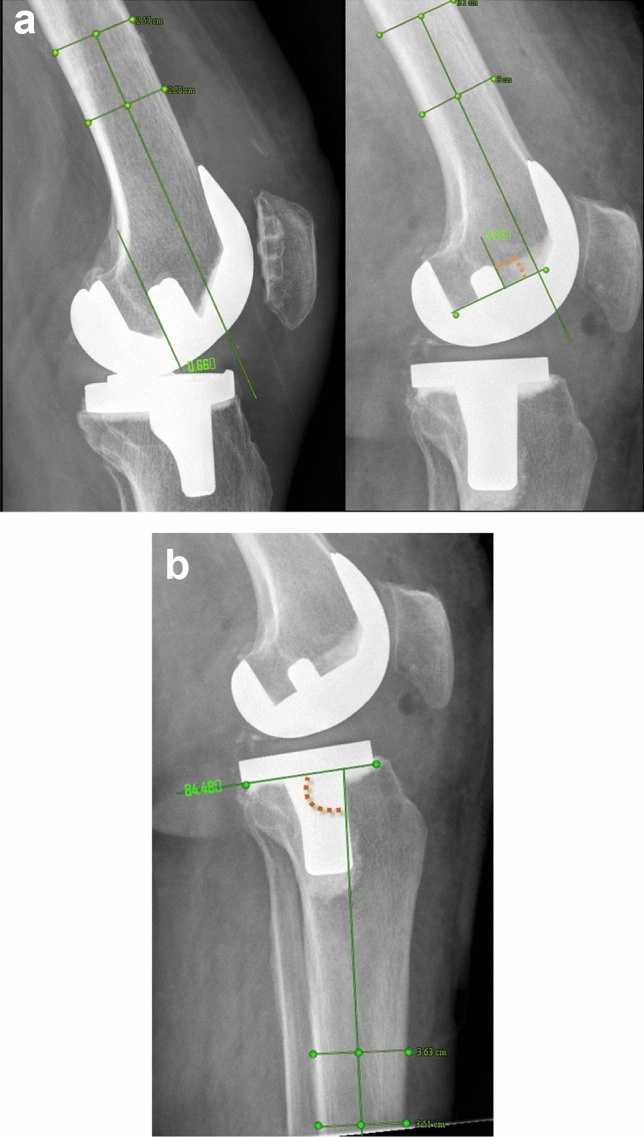
a Measurement of sagittal inclination in CR and PS femoral component. b Measurement of sagittal inclination (of the tibial component
Statistical Analysis
The minimum sample size required for the study is 62 in each group and totalling to 124, calculated using nMaster 1.0 version software based on the study by Song et al. [18] with 95% confidence interval and 80% power of the test. IBM SPSS version 20.0 software was used for all the statistical analysis. Categorical variables are expressed using frequency and percentages and continuous variables using mean and standard deviation. Student's t-test/Mann–Whitney U test was used to test the statistical significance of the difference in mean of mechanical axis before surgery between the two groups. Chi-square test was used to find the significance of error in categories, implant design within groups and between the two surgeons. For testing the intra-observer and interobserver reliability, the intraclass correlation coefficient was performed with 95% confidence interval and standard error of measurement. A p-value < 0.05 was considered as statistically significant.
Results
RATKA group, which included 105 patients (143 knees) and MTKA group with 111 patients (151 knees) had statistically similar demographic characteristics and comparable preoperative mechanical axis (Table 1). We observed that postoperative mechanical axis had absolutely no outliers in RATKA group, whereas MTKA had 23.8% outliers (p < 0.001) with respective to the preoperative plan (Fig. 4). Statistically significant outcomes were seen favouring RATKA group with respect to other parameters also, i.e. coronal inclination of the femoral component (p < 0.001), the coronal inclination of the tibial component (p < 0.001) and sagittal inclination of the tibial component (p < 0.001) (Figs. 5 and 6). We observed comparable results in the sagittal inclination of the femoral component between the two groups (p = 0.566). Moreover, we found that with respect to all parameters measured, the percentage of knees with 'excellent' outcomes were higher in RATKA group compared to MTKA group (Table 2).
Table 1.
Demographic and baseline characteristics of patients included in the study
| Variables | Categories | RATKA (n = 105) | MTKA (n = 111) | p value |
|---|---|---|---|---|
| Mean age (years) | 65.24 (51–81) | 66.29 (52–79) | 0.356 | |
| Gender | F | 84 | 88 | 0.895 |
| M | 21 | 23 | ||
| Mean BMI (kg/m2) | 27.64 (19.29–38.98) | 28.70 (18.91–39.93) | 0.189 | |
| Mean Preoperative mechanical axis(± SD) | 11.56 ± 5.42° (n = 143) |
12.32 ± 5.22° (n = 151) |
0.224 | |
BMI Body mass index; SD Standard deviation
Fig. 4.
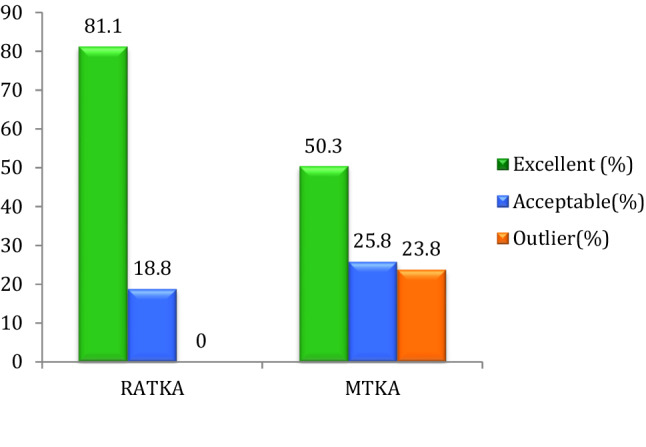
Graph showing comparison of the post-operative mechanical axis between groups
Fig. 5.
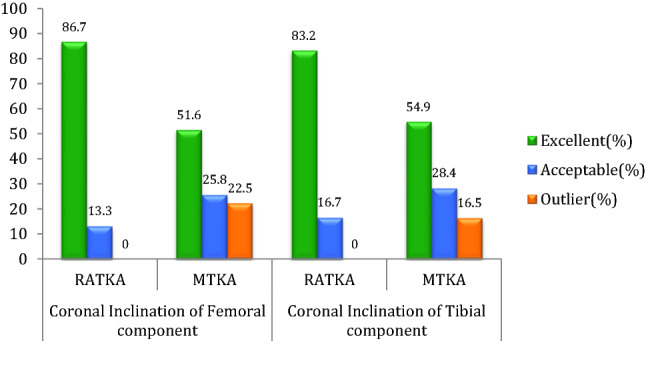
Graph showing comparison of the coronal inclination of femoral and tibial components between groups
Fig. 6.
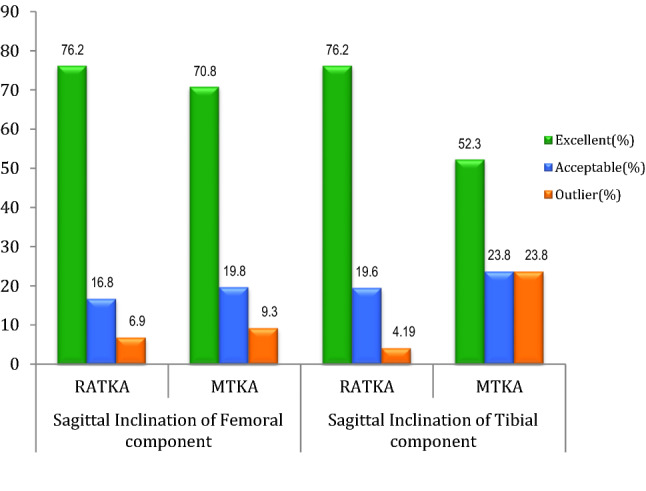
Graph showing comparison of the sagittal inclination of femoral and tibial components between groups
Table 2.
Result of postoperative radiological assessment
| Measurements | Category | RATKA (n = 143) |
MTKA (n = 151) |
p value |
|---|---|---|---|---|
| Postoperative Mechanical axis | Excellent | 116 (81.1%) | 76 (50.3%) | < 0.001 |
| Acceptable | 27 (18.8%) | 39 (25.8%) | ||
| Outlier | 0 (0%) | 36 (23.8%) | ||
| Coronal inclination of femoral component | Excellent | 124 (86.7%) | 78 (51.6%) | < 0.001 |
| Acceptable | 19 (13.3%) | 39 (25.8%) | ||
| Outlier | 0 (0%) | 34 (22.5%) | ||
| Coronal inclination of tibial component | Excellent | 119 (83.2%) | 83 (54.9%) | < 0.001 |
| Acceptable | 24 (16.7%) | 43 (28.4%) | ||
| Outlier | 0 (0%) | 25 (16.5%) | ||
| Sagittal inclination of femoral component | Excellent | 109 (76.2%) | 107 (70.8%) | 0.566 |
| Acceptable | 24 (16.8%) | 30 (19.8%) | ||
| Outlier | 10 (6.9%) | 14 (9.3%) | ||
| Sagittal inclination of tibial component | Excellent | 109 (76.2%) | 79 (52.3%) | < 0.001 |
| Acceptable | 28 (19.6%) | 36 (23.8%) | ||
| Outlier | 6 (4.2%) | 36 (23.8%) |
Excellent—defined when the values were within 0–2° from the planned alignment
Acceptable—defined when the values were > 2° but < 3° from the planned alignment
Outlier—defined when the values were ≥ 3° from the planned alignment
The inter-observer reliability was 0.894 for the postoperative mechanical axis measurements, 0.890 and 0.914 for the coronal inclination of the femoral and tibial component respectively, 0.864 and 0.906 for the sagittal inclination of femoral and tibial component respectively suggesting good agreement between the observers. The intraclass correlation coefficient for the intraobserver measurements was also above 0.8 (0.864–0.910), indicating good reliability. There was no statistically significant difference in the measured parameters between the two surgeons (p > 0.05) and between the CR and PS implants in RATKA group (p > 0.05).
Discussion
Total knee arthroplasty is considered as the most efficient treatment for advanced osteoarthritis of the knee. Postoperative limb alignment and implant positioning are among the crucial factors determining success and longevity [19, 20]. Studies show that the conventional technique which utilises an intramedullary femoral and extramedullary tibial jig, is prone to errors ranging from 13–38% concerning postoperative limb alignment [18, 21–28]. The source of errors can be due to variations in the native bony anatomy such as coronal and sagittal bowing, diameter of the medullary canals and constitutional varus or valgus of the knee [29–32]. Errors may also arise while using the oscillating saws for bone preparation [23, 33]. This may occur when the saw deflects off the dense sclerotic bone or when the cutting block becomes loose as in a case of osteoporosis. Considering all these factors, the probability of erring is more in MTKA even for high volume surgeons [34].
Technological advancement, such as computer-assisted navigation, was later introduced to overcome the errors in the conventional technique. This technique, again uses regular manual oscillating saws for bone preparation, with an error ranging from 0–20%[22–24, 26–28]. Hence to improve precision, robotic devices were developed which had restraints on bone preparation. One of its earliest orthopaedic application was in total hip arthroplasty in 1992 by the ROBODOC (Curexo Technology, Fremont, Ca), which was an active autonomous milling system [35]. Later as designs evolved, many semi-active and passive types of robots came in to use. In our study, a semi-active kind of robot, Mako (Stryker, Mahwah, New Jersey), was used which utilises a preoperative CT scan for planning the implant size and positioning. It gives audio-visual and haptic feedback during bone preparation, controlling the saw within the confines of a haptic boundary. This restraint improves the precision and protects the adjacent tissues, thus reducing iatrogenic bone and soft tissue trauma [36, 37].
It was observed in our study that the execution of the preoperative plan was much more precise in RATKA compared to MTKA, even during the initial phases. Out of the five parameters studied, four were statistically better in the RATKA group. The percentage of knees with excellent outcomes were higher in RATKA, for all the parameters measured. Our results showing no outliers in RATKA compared to 23.8% in MTKA concerning the postoperative mechanical axis, were comparable with the existing literature, where outliers ranged from 0–2% and 19–38% respectively [18, 21, 38–40].
There were several limitations to our study. A CT based assessment of the implant positioning would have been more accurate, which could assess the rotational alignment of the implants as well. However, in view of additional radiation exposure associated with it, we have decided not to perform a postoperative CT scan. We had to use different implants in RATKA, and MTKA due to the new government regulations and manufacturer policy, which resulted in the unavailability of Triathlon (Stryker, Mahwah, New Jersey) implants for MTKA during the study period. However, we focused more on the accuracy of execution of the corresponding preoperative plans with their postoperative measurements, which makes the difference in implants less significant. Still, the possibility of observer bias cannot be ignored.
A recent study by Kayani et al. has shown encouraging results concerning the early functional outcome and time to discharge in robotic-arm assisted TKA [41]. At this point, there is a scarcity of long-term data on the functional outcome and advantages of RATKA. However, recent literature and our study showed that these systems could help a surgeon to get the implant and limb aligned precisely. Nevertheless, each surgeon will have their own "ideal position" of implants, which still need to be determined. The robotics can help in achieving these targets consistently with such accuracy that may not be replicable with manual techniques. Thus, robotics can be a useful research tool to identify "ideal position" of the implants as it removes the surgeon variability in different alignment techniques. Furthermore, because of the versatility of these systems in terms of its capacity to prepare bone; cementless TKA and patient-specific implants may come up encouragingly in the near future.
These benefits in terms of accuracy, precision and reproducibility, can enhance the overall utility of the system, if it further reduces the complications and improves the long-term outcome, thus justifying the added costs.
Conclusion
RATKA significantly reduced the outliers in the mechanical axis, the coronal inclination of femoral and tibial components and sagittal inclination of the tibial components compared to MTKA. Thus RATKA executed the preoperative plan more accurately with respect to limb alignment and implant positioning compared to manual TKA, even when the surgeons were more experienced in the latter.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank Dr Sriraam Rajagopal and Dr Aman Paul George, Resident interns, Department of Orthopaedics, Amrita Institute Of Medical Sciences, Kerala, India for assistance in data procurement.
Compliance with ethical standards
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standards
This study has been approved by the institutional research ethics committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthritis Cartilage. 2013;21(9):1145–1153. doi: 10.1016/j.joca.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gibon E, Goodman MJ, Goodman SB. Patient satisfaction after total knee arthroplasty: a realistic or imaginary goal? Orthopedic Clinics of North America. 2017;48(4):421–431. doi: 10.1016/j.ocl.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Scott CEH, Turnbull GS, MacDonald D, Breusch SJ. Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone Joint J. 2017;99-B(8):1037–1046. doi: 10.1302/0301-620X.99B8.BJJ-2016-1364.R1. [DOI] [PubMed] [Google Scholar]
- 4.Luna IE, Kehlet H, Peterson B, Wede HR, Hoevsgaard SJ, Aasvang EK. Early patient-reported outcomes versus objective function after total hip and knee arthroplasty: a prospective cohort study. Bone Joint J. 2017;99-B(9):1167–1175. doi: 10.1302/0301-620X.99B9.BJJ-2016-1343.R1. [DOI] [PubMed] [Google Scholar]
- 5.Sikorski JM. Alignment in total knee replacement. Journal of Bone and Joint Surgery. British Volume. 2008;90(9):1121–1127. doi: 10.1302/0301-620X.90B9.20793. [DOI] [PubMed] [Google Scholar]
- 6.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. Journal of Bone and Joint Surgery. American Volume. 2010;92(12):2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 7.Lee B-S, Cho H-I, Bin S-I, Kim J-M, Jo B-K. Femoral component varus malposition is associated with tibial aseptic loosening after TKA. Clinical Orthopaedics and Related Research. 2018;476(2):400–407. doi: 10.1007/s11999.0000000000000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu H-X, Shang P, Ying X-Z, Zhang Y. Shorter survival rate in varus-aligned knees after total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(8):2663–2671. doi: 10.1007/s00167-015-3781-7. [DOI] [PubMed] [Google Scholar]
- 9.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clinical Orthopaedics and Related Research. 2013;471(3):1000–1007. doi: 10.1007/s11999-012-2613-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J. 2017;99(5):640–646. doi: 10.1302/0301-620X.99B5.BJJ-2016-0688.R2. [DOI] [PubMed] [Google Scholar]
- 11.Bäthis H, Perlick L, Tingart M, Lüring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty. Journal of Bone and Joint Surgery. British Volume. 2004;86(5):682–687. doi: 10.1302/0301-620x.86b5.14927. [DOI] [PubMed] [Google Scholar]
- 12.Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev. 2019;4(10):611–617. doi: 10.1302/2058-5241.4.190022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthrop. 2016;31(10):2353–2363. doi: 10.1016/j.arth.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 14.Parsley BS. Robotics in orthopedics: a brave new world. J Arthrop. 2018;33(8):2355–2357. doi: 10.1016/j.arth.2018.02.032. [DOI] [PubMed] [Google Scholar]
- 15.Mullaji AB, Shetty GM, Kanna R, Vadapalli RC. The influence of preoperative deformity on valgus correction angle: an analysis of 503 total knee arthroplasties. J Arthrop. 2013;28(1):20–27. doi: 10.1016/j.arth.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 16.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clinical Orthopaedics and Related Research. 1989;248:9–12. [PubMed] [Google Scholar]
- 17.Kim Y-H, Kim J-S, Yoon S-H. Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. Journal of Bone and Joint Surgery. British Volume. 2007;89(4):471–476. doi: 10.1302/0301-620X.89B4.18878. [DOI] [PubMed] [Google Scholar]
- 18.Song E-K, Seon J-K, Park S-J, Jung WB, Park H-W, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19(7):1069–1076. doi: 10.1007/s00167-011-1400-9. [DOI] [PubMed] [Google Scholar]
- 19.Abdel MP, Ledford CK, Kobic A, Taunton MJ, Hanssen AD. Contemporary failure aetiologies of the primary, posterior-stabilised total knee arthroplasty. Bone Joint J. 2017;99-B(5):647–652. doi: 10.1302/0301-620X.99B5.BJJ-2016-0617.R3. [DOI] [PubMed] [Google Scholar]
- 20.Kutzner I, Bender A, Dymke J, Duda G, von Roth P, Bergmann G. Mediolateral force distribution at the knee joint shifts across activities and is driven by tibiofemoral alignment. Bone Joint J. 2017;99-B(6):779–787. doi: 10.1302/0301-620X.99B6.BJJ-2016-0713.R1. [DOI] [PubMed] [Google Scholar]
- 21.Song E-K, Seon J-K, Yim J-H, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clinical Orthopaedics and Related Research. 2013;471(1):118–126. doi: 10.1007/s11999-012-2407-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. Journal of Bone and Joint Surgery. British Volume. 2004;86(3):372–377. doi: 10.1302/0301-620x.86b3.14643. [DOI] [PubMed] [Google Scholar]
- 23.Bäthis H, Perlick L, Tingart M, Perlick C, Lüring C, Grifka J. Intraoperative cutting errors in total knee arthroplasty. Archives of Orthopaedic and Trauma Surgery. 2005;125(1):16–20. doi: 10.1007/s00402-004-0759-1. [DOI] [PubMed] [Google Scholar]
- 24.Confalonieri N, Manzotti A, Pullen C, Ragone V. Computer-assisted technique versus intramedullary and extramedullary alignment systems in total knee replacement: a radiological comparison. Acta Orthopaedica Belgica. 2005;71(6):703–709. [PubMed] [Google Scholar]
- 25.Saragaglia D, Picard F, Chaussard C, Montbarbon E, Leitner F, Cinquin P. Computer-assisted knee arthroplasty: comparison with a conventional procedure. Results of 50 cases in a prospective randomized study. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur. 2001;87(1):18–28. [PubMed] [Google Scholar]
- 26.Oberst M, Bertsch C, Würstlin S, Hol U. [CT analysis of leg alignment after conventional vs. navigated knee prosthesis implantation. Initial results of a controlled, prospective and randomized study] Unfallchirurg. 2003;106(11):941–948. doi: 10.1007/s00113-003-0686-6. [DOI] [PubMed] [Google Scholar]
- 27.Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A. Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. Journal of Bone and Joint Surgery. British Volume. 2003;85(6):830–835. [PubMed] [Google Scholar]
- 28.Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthrop. 2005;20(5):618–626. doi: 10.1016/j.arth.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Bardakos N, Cil A, Thompson B, Stocks G. Mechanical axis cannot be restored in total knee arthroplasty with a fixed valgus resection angle: a radiographic study. J Arthrop. 2007;22(6 Suppl 2):85–89. doi: 10.1016/j.arth.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 30.Kazemi SM, Shafaghi T, Minaei R, Osanloo R, Abrishamkarzadeh H, Safdari F. The effect of sagittal femoral bowing on the femoral component position in total knee arthroplasty. Arch Bone Joint Surg. 2017;5(4):250–254. [PMC free article] [PubMed] [Google Scholar]
- 31.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clinical Orthopaedics and Related Research. 2012;470(1):45–53. doi: 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haruta Y, Kawahara S, Tsuchimochi K, Hamasaki A, Hara T. Deviation of femoral intramedullary alignment rod influences coronal and sagittal alignment during total knee arthroplasty. The Knee. 2018;25(4):644–649. doi: 10.1016/j.knee.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 33.Plaskos C, Hodgson AJ, Inkpen K, McGraw RW. Bone cutting errors in total knee arthroplasty. J Arthrop. 2002;17(6):698–705. doi: 10.1054/arth.2002.33564. [DOI] [PubMed] [Google Scholar]
- 34.Kazarian GS, Lawrie CM, Barrack TN, Donaldson MJ, Miller GM, Haddad FS, et al. The impact of surgeon volume and training status on implant alignment in total knee arthroplasty. Journal of Bone and Joint Surgery. American Volume. 2019;101(19):1713–1723. doi: 10.2106/JBJS.18.01205. [DOI] [PubMed] [Google Scholar]
- 35.Bargar WL, Bauer A, Börner M. Primary and revision total hip replacement using the Robodoc system. Clinical Orthopaedics and Related Research. 1998;354:82–91. doi: 10.1097/00003086-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthrop. 2018;33(8):2496–2501. doi: 10.1016/j.arth.2018.03.042. [DOI] [PubMed] [Google Scholar]
- 37.Thilak J, Thadi M, Mane PP, Sharma A, Mohan V, Babu BC. Accuracy of tibial component positioning in the robotic arm assisted versus conventional unicompartmental knee arthroplasty. J Orthop. 2020;1(22):367–371. doi: 10.1016/j.jor.2020.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clinical Orthopaedics and Related Research. 2007;464:111–116. doi: 10.1097/BLO.0b013e318126c0c0. [DOI] [PubMed] [Google Scholar]
- 39.Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. The Knee. 2002;9(3):173–180. doi: 10.1016/s0968-0160(02)00015-7. [DOI] [PubMed] [Google Scholar]
- 40.Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthopaedica Scandinavica. 2004;75(5):573–579. doi: 10.1080/00016470410001448. [DOI] [PubMed] [Google Scholar]
- 41.Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty. Bone Joint J. 2018;100-B(7):930–937. doi: 10.1302/0301-620X.100B7.BJJ-2017-1449.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.