Abstract
Central studies carried out on vaccines against the severe acute respiratory syndrome coronavirus 2 (SARS-COV2) excluded patients receiving immunosuppressive therapy and those diagnosed with an immunosuppressive condition. Moreover, there are no data on vaccine efficacy regarding older patients with cancer.
Objectives
The primary objective was to evaluate the seroprevalence of the SARS-CoV2 IgG in older patients (aged ≥80 years) diagnosed with solid or hematological malignancies, one month after administering the second dose of the BNT162b2 vaccine.
Materials and methods
We screened 74 older patients with cancer, 45 of them accepted to receive the vaccination and collected serum samples from 36 patients; a group of medical doctors and nurses from our hospital was used as a control in a 1:2 ratio.
Results
The median age was 82 years (range 80–89). Median serum IgG were 2396,10 AU/ml (range 0–32,763,00) in patients with cancer and 8737,49 AU/ml (398.90–976,280,00) in the control group, p < 0.0001. Additional subgroup analyses were performed comparing males and females, patients treated with chemotherapy versus other therapies (immunotherapy, targeted therapy), solid tumors versus hematological malignancies, early (I-II) versus advanced (III-IV) stage of disease, continuative corticosteroid use or not. None of them reached statistical significance.
Conclusion
Our study shows for the first time that patients with cancer aged ≥80 years can have a serological response to the BNT162b2 COVID-19 vaccine one month after vaccination and consequently support the vaccination campaign currently underway in this frail population.
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination campaign started in Europe in December 2020. The BNT162b2 mRNA vaccine developed by BioNTech and Pfizer was the first coronavirus vaccine (COVID-19) approved in Italy.
Efficacy and safety of the BNT162b2 mRNA vaccine was established in a randomized study which enrolled 43,548 patients aged between 16 and 91 years. The median age of the 18,860 patients in the active treatment arm was 52 years (range 16–89) with 42.3% of subjects older than 55. The study demonstrated that efficacy is not influenced by age. This pivotal study excluded patients receiving immunosuppressive therapy and those diagnosed with an immunosuppressive condition [1]. Therefore, there is no specific efficacy data available for older patients with cancer. In Italy the median age of the 106,789 patients who died from COVID-19 was 82 years (range 0–109). Of the 6992 hospitalized patients who died, 16.6% were affected by an active cancer [2]. As recently pointed out, the management of older patients with cancer during COVID-19 pandemic, required major efforts in tailoring and personalizing treatment approach. Recommendation of the Society of Geriatric Oncology (SIOG) COVID-19 working group is to early underline and clearly state the goals of care in this vulnerable population [3].
The Italian Minister of Health identified specific phases and priorities for delivering the vaccine. Priority has been given to health care providers, people older than 80 years, and frail patients. These priority groups were included in the first step of the vaccination campaign.
Considering the important need of real-life data related to COVID-19 vaccination in older patients with cancer [4], we decided to conduct a spontaneous study on this population.
2. Aims
The primary objective of our study was to evaluate the seroprevalence of the SARS-CoV-2 IgG in older outpatients (aged ≥80 years), diagnosed with solid or hematological malignancies, one month after administering the second dose of the BNT162b2 vaccine.
3. Material and methods
This was a spontaneous, not-sponsored, mono-institutional, cross-sectional control study conducted at San Camillo-Forlanini Hospital in Rome. The study was approved by the local ethics committee (Protocol number 216/CE Lazio1, 22nd February 2021) and was conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent before starting any study-related procedure.
3.1. Study population
Older patients (aged ≥80 years) diagnosed with either solid or hematological malignancies, under the care of the Oncology Department at San Camillo Forlanini Hospital, were screened for the study. Major eligibility criteria included: patients with solid or hematological malignancies, early stage or advanced disease, receiving active treatments or having completed treatment within six months before 1st dose of vaccination. Any kind of oncological treatment was allowed (e.g. chemotherapy, targeted therapy, and immunotherapy). Patients with previous SARS-CoV-2 infection, based on anamnestic evaluation, and aged <80 years were excluded. A group of health care workers at our hospital (medical doctors and nurses), aged ≥66 years was used as a control group in a 1:2 ratio. Personal and health data of these subjects were not recorded and serological analyses were conducted anonymously. Previous history of COVID-19 infection was an exclusion criteria for this group.
Study population and control group received two doses of BNT162b2, a lipid nanoparticle–formulated, nucleoside-modified RNA vaccine that encodes a prefusion stabilized, membrane-anchored SARS-CoV-2 full-length spike protein [1]. The vaccine was administered intramuscularly on days 1 and 21, as part of the national vaccination campaign. The first patient was vaccinated on January 4th 2021, the last patient was vaccinated on February 19th 2021.
3.2. Laboratory methods
The serological tests were performed by Abbott IgG anti SARS-CoV-2 Alinity system, an automated immunoassay for the quantitative detection of IgG anti-Spike sub1 antibodies to SARS-CoV-2 in human serum or plasma using chemiluminescent microparticle immunoassay technology (CMIA) [5]. The results of the assay are reported as Arbitrary Units (AU)/ml with a cutoff for positivity of 50 AU/ml. Patient samples were collected one month after administering the second dose of the BNT162b2 vaccine, from 9th to 22nd March 2021.
3.3. Accrual of clinical data
The following data were collected: age, gender, type of cancer or hematological disease, stage, relevant comorbidities, type of treatment, concomitant medication, corticosteroid use and blood cell count. No clinical data were provided for the control sample of health care workers, except for age and serological analyses.
3.4. Statistical analysis
Descriptive statistics was used to analyze patient characteristics. Differences in serological value between vaccinated patients with cancer and control group were tested using the nonparametric Mann-Whitney U test. A p value <0.05 was considered significant. Statistical evaluation was performed using the SPSS 21.0 (SPSS Inc., Chicago, IL, USA) for Windows.
4. Results
We screened 74 older patients with cancer for this study, 45 of them chose to receive the vaccination and serum samples were collected from 36 patients. Median age was 82 years (range: 80–89), 58.4% of patients were female and 41.6% male. The majority were affected by solid tumors (72.2%). Genitourinary tumors followed by gastrointestinal and breast cancer were the most common types. Most patients had an advanced (III-IV) stage of disease (63.9%). Four out of six patients with early stage disease were receiving active treatment: radiotherapy (anal cancer), radiotherapy + chemotherapy (bladder cancer), rituximab (Non-Hodgkin lymphoma), paclitaxel plus trastuzumab (breast cancer). Thirty-one patients (86%) were receiving an active treatment when they were vaccinated: eleven chemotherapy plus monoclonal antibodies, ten chemotherapy, four targeted therapies, and two each for immunotherapy/hormonal therapy/radiotherapy. Only nine patients (25%) were under continuous steroid treatment during vaccination while those receiving steroids as antiemetics were not considered for corticosteroid therapy [Table 1 ].
Table 1.
Patients' data.
| Patients with cancer n = 36 (%) | |
|---|---|
| Median Age (range) | 82 years (80–89) |
| Sex | |
| Female | 21 (58.4) |
| Male | 15 (41.6) |
| Tumor type | |
| Haematologic tumors | 10 (27.3) |
| Solid Tumors | 26 (72.2) |
| Genitourinary | 9 (25.0) |
| Gastrointestinal | 8 (22.2) |
| Breast | 7 (19.4) |
| Others | 2 (5.5) |
| Staging | |
| I-II | 6 (16.7) |
| III-IV | 23 (63.9) |
| NA | 7 (19.4) |
| Comorbidities | |
| Cardiovascular | 25 (69.4) |
| Diabetes | 8 (22.2) |
| Other | 15 (41.7) |
| Cancer Treatment | |
| Active treatment during vaccination | 31 (86.1) |
| Chemotherapy + mAb | 11 (30.5) |
| Chemotherapy | 10 (27.7) |
| Targeted Therapy | 4 (11.1) |
| Hormonal Therapy | 2 (5.5) |
| Immunotherapy | 2 (5.5) |
| Radiotherapy | 2 (5.5) |
| Out of treatment | 5 (13.9) |
| Corticosteroid therapy | |
| Yes | 9 (25.0) |
| No | 26 (72.2) |
| Unknown | 1 (2.8) |
Median serum IgG were 2396,10 AU/ml (range 0–32,763,00) in patients with cancer and 8737,49 AU/ml (398.90–976,280,00) in the control group, p < 0.0001 (Fig. 1 ).
Fig. 1.
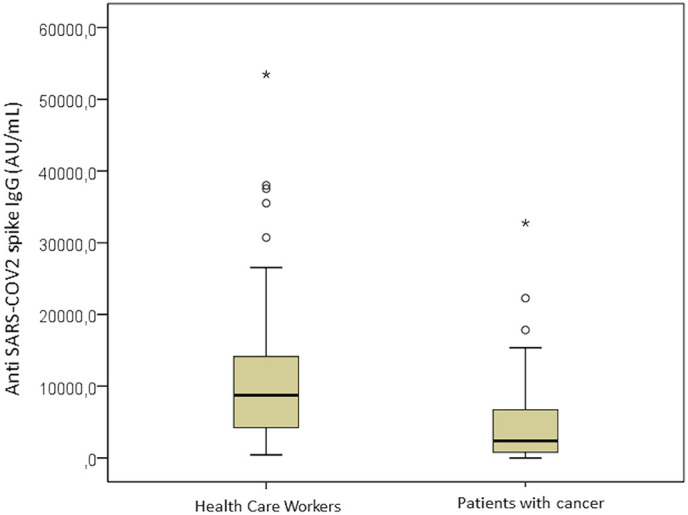
Anti-Spike Immunoglobuline G (IgG) values (positive value > 50 AU/ml) in patients with cancer older than 80 years and control group. Mann-Whitney U test, p < 0,0001.
Additional subgroup analyses were performed comparing males and females, patients treated with chemotherapy to other therapies (immunotherapy, targeted therapy), early (I-II) versus advanced (III-IV) stage of disease, continuative corticosteroid use or not. None of them reached statistical significance. However positivity in serological analyses was not reached in six out of the ten patients with hematological malignancies and in one out of the twenty-six patients with solid tumors.
No major adverse events related to vaccine were recorded.
None of the patients enrolled in this study experienced COVID-19 infection after vaccination, regardless of the level of IgG response.
5. Discussion
Our study shows for the first time that patients with cancer aged ≥80 years can have a substantial serological response to the BNT162b2 COVID-19 vaccine one month after vaccination with increased IgG against the anti-spike sub-1 unit.
If vaccination can avoid COVID-19 infection or if is only able to prevent spread of symptoms and severe clinical disease is still a scientific debate. Moreover the correlation between serological response to COVID-19 vaccination and clinical protection is still not completely documented [6].
Duysburgh et al. recently showed a positive correlation between serological response to vaccination measured with Anti-Spike IgG and presence of neutralising antibodies in cell cultures indicating that serological response is a valid surrogate of efficacy [7].
In our study, none of the patients enrolled experienced COVID-19 infection after vaccination, regardless of the level of IgG response. Based on that it seems that, in our cohort of vulnerable patients, serological response offers a clinical protection.
This trial supports the recommendation recently published by the SIOG COVID-19 Working Group, to prioritize older adults with cancer in vaccination programs [8]. Endorsements for vaccination of patients with cancer have also been promoted by American Association of Clinical Oncology (ASCO) and the European Society of Medical Oncology (ESMO) [9,10]. The recommendation of ASCO is to offer vaccination against COVID-19, as long as components of vaccine are not contraindicated, to patients with cancer, cancer survivors and patients with cancer undergoing active treatment [9].
The European Society of Medical Oncology suggests to continue research in order to generate more data on vaccine efficacy and safety in special populations, including patients with active cancer or history of cancer [10].
Our study has several biases, one of the most relevant is the low number of patients who agreed to undergo serological testing after being vaccinated (45 of 74 were vaccinated and 36 underwent serological testing). Lack of data on vaccine efficacy in this frail population as well as and the lack of information on safety in older patients with cancer contributed to the low accrual. In addition, our follow up is short and we still do not have any data about the duration of the serologic response. Doria-Rose et al. recently showed that antibody persistence after the second dose of mRNA-1273 Vaccine for COVID-19 remains high at day 209 in 33 healthy adults, however it seems less evident with patients aged ≥71 years [11]. These data are also consistent with those obtained in patients with previous COVID-19 infection for up to eight months [12].
Finally we did not perform a geriatric assessment in our population and fitness may have an impact on immune response.
6. Future perspectives
In conclusion, this study has evaluated IgG response to BNT162b2 COVID-19 vaccine in older patients with cancer showing that they are still able to develop an immunological response and consequently support the vaccination campaign currently underway in this frail population. Although this response is significantly lower than that reached in the control group it is indeed of clinical relevance. Immunosenescence could potentially impair immunogenicity of the vaccine in older adults [13]. Recently, Herishanu et al. showed that antibody response to BNT162b2 vaccine in patients with chronic lymphocytic leukemia is markedly impaired by disease activity and treatment [14]. In our experience, even if statistical significance was not reached in the subgroup analyses, there is a difference between hematological and solid tumor immunoresponse and this data could become of clinical relevance with larger numbers.
Additional serological tests will be performed after six and twelve months after vaccination in order to evaluate the duration of immunological response in our patients. A longer follow-up is needed to answer this question and to evaluate a further boost in doses in older patients in order to restore immunity against COVID-19.
Authors' contribution
DI, LC and CG designed the study and significantly contributed in data analyses, interpretation, and writing the article.
DI, LC, LP, EC, RAC,BM and GP contributed to data acquisition.
IS contributed to the statistical analyses and with GP and CG to quality control of data.
All authors reviewed the article.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgements
We‘d like to thank Paola Cioni, Head of nurses of Oncology Day Hospital, for her great collaboration and support during the execution of this research project.
References
- 1.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. NEJM. 2020 Dec 31;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanità I.S.D. 2021. Characteristics of SARS-COV-2patients dying in Italy. (report based on available data on march 30th) [Google Scholar]
- 3.Battisti N.M.L., Mislang A.R., Cooper L., O’Donovan A., Audisio R.A., Cheung K.L., et al. Adapting care for older cancer patients during the COVID-19 pandemic: recommendations from the International Society of Geriatric Oncology (SIOG) COVID-19 working group. J Geriat Oncol. 2020;11:1190–1198. doi: 10.1016/j.jgo.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corti C., Crimini E., Tarantino P., Pravettoni G., Eggermont A.M.M., Delaloge S. G SARS COV 2 vaccines for cancer patients: a call to action. EJC. 2021 Feb 25;148:316–327. doi: 10.1016/j.ejca.2021.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abbott Alinity i SARS-CoV-2 IgG II Quant Reagent Instructions for Use. 2020. [Google Scholar]
- 6.Leshem E., Lopman B.A. Population immunity and vaccine protection against infection. Lancet. 2021;397:1686–1687. doi: 10.1016/S0140-6736(21)00870-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duysburgh E., Mortgat L., Barbezange C., Dierick K., Fischer N., Heyndrickx L., et al. Persistence of IgG response to SARS-COV-2. Lancet Infect Dis. 2021;21:163–164. doi: 10.1016/S1473-3099(20)30943-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mislang A.R., Soto-Perez-de-Celis E., Russo C., Colloca G., Williams G.R., O’Hanlon S., et al. The SIOG COVID-19 working group recommendations on the rollout of COVID-19 vaccines among older adults with cancer. J Geriatr Oncol. 2021 doi: 10.1016/j.go.2021.03.003. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 Vaccines & Patients with Cancer https://www.asco.org/asco-coronavirus-resources/covid-19-vaccines-patients-cancer
- 10.Garassino M.C., Vyas M., de Vries E.G.E., Giuliani R., Peters S., et al. 2021. COVID-19 vaccination in cancer patients: ESMO statements.https://www.esmo.org/covid-19-and-cancer/covid-19-vaccination [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doria-Rose N., Suthar M.S. Antibody persistence trough 6 months after the Second Dose of mRNA-1273 Vaccine for Covid-19. Correspondence. NEJM. 2021;384(23):2259–2261. doi: 10.1056/NEJMc2103916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dan J.M., Mateus J., Kato Y., Hastie K.M., Yu E.D., Faliti C.E., et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021 doi: 10.1126/science.abf4063. Jan 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crooke S.N., Ovsyannikova I.G., Poland G.A. Kennedy RB Immunosenescence and human vaccine immune responses. Immun Ageing. 2019;16:25. doi: 10.1186/s12979-019-0164-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herishanu Y., Avivit I., Aharon A., Shefer G., Levi S., Bronstein Y., et al. Efficacy of the BNT162b2 mRNA COVID-19 vaccine in patients with Chronic Lymphocytic Leukemia. Blood. 2021 doi: 10.1182/blood.2021011568. [DOI] [PMC free article] [PubMed] [Google Scholar]


