Abstract
Stercoral colitis is a rare inflammatory condition involving the large bowel wall secondary to fecal impaction. Stercoral colitis has a clinical course ranging from non-complicated fecaloid impaction to colonic perforation. This case report aims to give a brief review of this condition and discuss its imaging findings.
Case Presentation
We herein report a case 74-year-old female who presented with abdominal pain, abdominal distension, and the absence of gas-feces discharge for a few days. The patient had a one-year history of chronic constipation and recent femoral neck fracture surgery. Physical examination shows abdominal distension with slight tenderness. Abdominal radiographs demonstrated bowel distention and fecal material in the colorectal regions. Computed tomography (CT) images demonstrated abundant fecal material with massive dilatation in the rectosigmoid colon, focal mural thickening, subtle pericolic fat stranding, and minimal free fluid in the abdominal and pelvic cavities. Based on these findings, the diagnosis of stercoral colitis was made. The patient was treated conservatively and eventually discharged with a good health condition.
Conclusion
Stercoral colitis seems to be more common in elderly patients with comorbid diseases. Chronic constipation causing fecal impaction is a major risk factor. CT scan is the most helpful imaging modality for the diagnosis of stercoral colitis. CT findings that should prompt the radiologist to consider this diagnosis include colonic dilatation containing impacted feces, mural thickening, and pericolic fat stranding. If the fecal impaction is not promptly relieved, life-threatening complications such as colonic perforation can occur.
Keywords: Fecal impaction, Stercoral colitis, Constipation, Imaging findings, Computed tomography
Abbreviations: WBC, white blood cell; SC, stercoral colitis; CT, computed tomography
Background
Stercoral colitis (SC) is an inflammatory condition of the large bowel wall related to increased intraluminal pressure secondary to fecal impaction. This rare inflammatory disease was first described in the surgical and gastrointestinal literature in 1894 [1], [2], [3], [4], [5], [6].
Fecal impaction usually occurs after prolonged constipation when the patient is not able to pass stool due to the accumulation of hard stools in the rectum [6], [7], [8], [9]. Risk factors for this condition are obesity, consumption of large amounts of fatty foods, prolonged immobility, low consumption of fluids and dietary fiber, sedentary lifestyle, lack of exercise, stress, travel, and inhibition of excretion, and taking certain medications. Hypothyroidism, neuromuscular diseases, hypokalemia, and intestinal obstruction can also lead to fecal impaction [9], [10], [11], [12].
Fecal impaction may be asymptomatic when there is simple fecaloid impaction but can lead to complications such as bowel wall inflammation and infection, ulcer formation, hemorrhoidal thrombosis, ischemic pressure necrosis, and subsequent colonic perforation, peritonitis, and septic shock. Patients with SC may present with abdominal pain, abdominal distension, absence of gas-feces discharge, nausea and vomiting, and anorexia. When complications occur, symptoms such as fever, chills, bleeding, and hypotension can also be seen [1,18,19]. This case report aims to give a concise review of this condition and discuss its imaging findings.
Case presentation
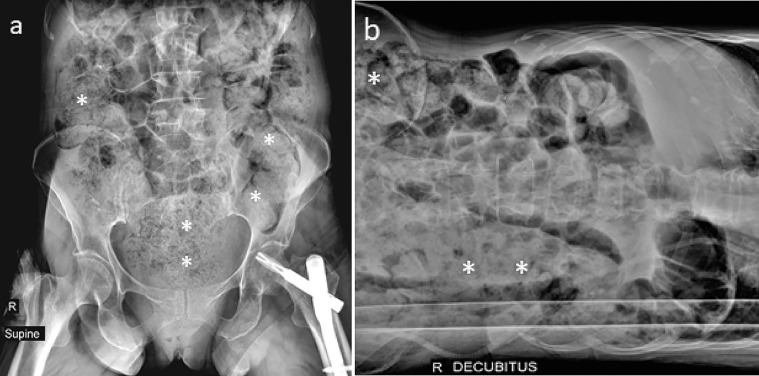
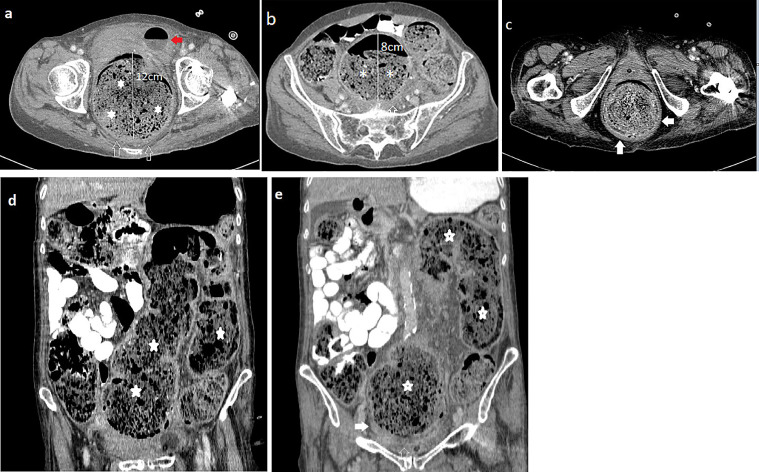
A 74-year-old female was presented to the emergency department of our hospital with abdominal pain, abdominal distension, and the absence of gas-feces discharge for approximately 5 to 7 days. The patient had a one-year history of chronic constipation as well as a history of previous surgery for a left femoral neck fracture. On physical examination, the patient had mild abdominal tenderness to palpation and abdominal distension but no signs of peritonitis. The stool was present in the rectal dome on the digital rectal exam. Her WBC count was slightly higher (12450/mL). The supine and left lateral decubitus abdominal radiographs demonstrated bowel distention and abundant fecal material in the colorectal regions (Figs. 1A-B). CT scan of the abdomen and pelvis was also performed with oral and intravenous contrast. The passage of oral contrast was evident until the beginning of the cecum and there was no evidence of significant small bowel dilatation. Axial and reformatted sagittal and coronal CT images demonstrated abundant fecal material in the colorectal regions causing extensive rectosigmoid dilatation (Figs. 2A-E). The maximum transverse diameter of the sigmoid colon and rectum measured eight and 12cm, respectively (Figs. 2A, B). Focal mural thickening at rectosigmoid regions reaching up to 7.2mm in the distended rectum, with subtle pericolic fat stranding, was also observed (Figs. 2A-C, E). Mild free fluid was seen in the abdominal and pelvic cavities, but no extraluminal free air was depicted. Based on these clinical/imaging findings, the diagnosis of SC secondary to extensive fecal impaction was made. Manual disimpaction was not completely successful, therefore an appropriate bowel regimen consisting of bowel enemas and oral laxatives was also started, which shows evidence of clinical and radiological improvement after 3 days of consecutive treatment. The patient was eventually discharged with a good health condition. Some medications were prescribed and education regarding a proper dietary regimen was given to prevent constipation in the future.
Fig. 1.
A-B. Supine (A) and left lateral decubitus (B) abdominal radiographs show abundant fecal material in the colorectal regions (asterisks).
Fig. 2.
A-E. Axial contrast-enhanced CT images (A-C) showing a voluminous fecal impaction (asterisks) with extensive rectal and sigmoid dilatation measured 12 and 8cm, respectively. Subtle perirectal inflammation manifests with perirectal fat stranding (white hollow arrows) and focal mural thickening, reaching up to 7.2 mm in the distended rectum is also noted (white solid arrows). The round structure with the air-fluid level anterior to the rectum is an inflated balloon of folly catheter within the empty urinary bladder, displaced by the dilated rectum anteriorly (red arrow in fig. A). Coronal CT images (D, E) also demonstrate colorectal dilatation with abundant fecal material (asterisks). Note pericolic fat stranding and inflammation (white hollow arrow) and mural thickening (white solid arrow). (Color version of figure is available online)
Discussion
The term SC refers to an inflammatory condition of the large bowel wall caused by increased intraluminal pressure from impacted fecal material in the colorectum. Fecal impaction and SC are predominantly related to chronic constipation, which is usually seen in elderly patients and those bedbound secondary to dementia or stroke. Occasionally, it may also be seen in young patients who have certain metabolic, neurologic, and/or muscular disorders causing prolong constipation [7,13,14,19]. In our case, the patient was an old female with a history of chronic constipation and recent left femoral neck surgery.
The conglomeration of hard impacted fecaloids is usually seen in the rectosigmoid colon, because of the small diameter of the colon in this region. Fecal material normally becomes more solid and dehydrated forming hard stool fecaloma. The accumulation of these hard stool causes colonic distention and pressure effect on the bowel wall, compromising the blood supply and resulting in ischemia at the antimesenteric side of the colon, which is more vulnerable to ischemia [1,7]. If the pressure effect and vascular compromise persist for a long time without treatment, ischemic necrosis, ulceration, perforation, and peritonitis can occur [4]. SC has a clinical course ranging from non-complicated fecaloid impaction to colonic perforation and peritonitis. Early diagnosis and management can relieve pressure from the colon without any need for surgical intervention. CT findings such as fecaloma and dilatation of the affected colon without associated colonic wall thickening or pericolic fat stranding are seen in non-complicated cases. Thickening of the colonic wall suggesting acute edema or inflammation. Thickening of the colon wall with accompanying pericolic fat stranding is the most helpful imaging finding for the diagnosis of SC [15]. Colonic perforation resulting from SC has been reported to be associated with a high mortality rate [1,7]. Stercoral colonic perforation is not a common cause of acute abdominal pain. Perforations usually occur due to diverticular disease, ulcerative colitis, infectious colitis, malignancy, mesenteric ischemia, and trauma. Dense mucosa signs and mucosal sloughing may also be seen in stercoral colitis. A report from a published article also denotes that, dense mucosa signs in unenhanced CT images and a pericolic abscess had a significant correlation with fatal SC, however, these findings were not statistically significant [16,17]. In our case, the key CT findings of SC were extensive rectosigmoid colon dilatation containing impacted fecal material, focal colonic wall thickening, mild pericolic fat stranding, and minimal extraluminal free fluid.
The differential diagnosis for SC includes diverticulitis, ulcerative colitis, infectious colitis, malignancy, acute mesenteric ischemia, large bowel obstruction, bowel perforation, and intra-abdominal abscess [17,19].
The prognosis of SC is highly dependent on prompt and early diagnosis and management. Length of involvement may also be a good prognostic finding. A study conducted by Ünal E, et al, shows that the finding most related to mortality was the length of the involved colon segment, as 57.1% of patients with >40 cm colon involvement died due to sepsis and deteriorated clinical course (15).
Manual disimpaction, oral regimen, bowel enema, or in some cases surgical methods are used as a treatment. Patients who have no signs/symptoms of peritonitis can be managed non-operatively with manual disimpaction either through the rectum or under endoscopic guidance and oral and/or bowel regimen under close monitoring. Surgical management is usually needed for patients with perforation, when a long bowel segment is involved, or when conservative management fails [7,20]. Patients with chronic constipation or those who have a history of previous fecal impaction or SC should be educated regarding a proper dietary regimen (increasing fiber, vegetables, fruit, and adequate fluid intake) and if needed, pharmacologic therapy such as osmotic and stimulant laxatives should also be given to prevent constipation in the future [21]. In our case, the patient was managed conservatively with a combination of manual fecal disimpaction and an appropriate oral and bowel regimen, therefore a histopathologic diagnosis of SC was not obtained in this case, as a consequence of successful conservative treatment. The patient was eventually discharged with a good health condition and some medications were also prescribed to prevent chronic constipation.
Conclusion
SC seems to be more common in elderly patients with comorbid diseases. Chronic constipation causing fecal impaction is a major risk factor. CT scan is the most helpful imaging modality for diagnosing and differentiating SC from other causes of abdominal pain. CT findings that should prompt the radiologist to consider this diagnosis include colonic dilatation containing impacted fecaloid material, colonic wall thickening, pericolic fat stranding, extraluminal free air, and/or free fluid. If the fecal impaction is not promptly relieved at the time, life-threatening complications such as colonic perforation can occur.
Authors’ contributions
Concept-AT; Radiological diagnosis-AT & DMN; Resources & data collection-AT; Literature research and writing the manuscript-AT; Critical review-DMN. All authors have read and approved the final manuscript.
Footnotes
Acknowledgments: Not applicable
Competing Interest: The authors declare that they have no competing interests and their work is not funded by any institution or organ.
Patient consent: Written informed consent was obtained for publication of this case report and any accompanying images.
References
- 1.Serpell J.W., Nicholls R.J. Stercoral perforation of the colon. Br J Surg. 1990;77:1325–1329. doi: 10.1002/bjs.1800771204. PMID: 2276009. PMID: 2276009. [DOI] [PubMed] [Google Scholar]
- 2.Grinvalsky H.T., Bowerman C.I. Stercoraceous ulcers of the colon: relatively neglected medical and surgical problem. JAMA. 1959;171:1941–1946. doi: 10.1001/jama.1959.03010320031008. PMID: 13829424. [DOI] [PubMed] [Google Scholar]
- 3.Lal S., Brown G.N. Some unusual complications of fecal impaction. Am J Proctol. 1967;18:226–231. PMID: 6046373. [PubMed] [Google Scholar]
- 4.Mauer C.A., Renzulli P., Mazzuchelli L., Egger B., Seiler C.A., Büchler M.W. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Dis Colon Rectum. 2000;43:991–998. doi: 10.1007/BF02237366. PMID: 10910249. [DOI] [PubMed] [Google Scholar]
- 5.Wang S., Sutherlans J.C. Colonic perforation secondary to fecal impaction. Dis Colon Rectum. 1977;20:355–356. doi: 10.1007/BF02586438. PMID: 862497. [DOI] [PubMed] [Google Scholar]
- 6.Rozenblit A.M., Cohen-Schwartz D., Wolf E.L., Foxx M.J., Brenner S. Case reports: stercoral perforation of the sigmoid colon—computed tomography findings. Clin Radiol 2000;55:727–729 the rectum with possible stercoral etiology: report of a case and review of the literature. Surg Today. 1998;28:937–939. doi: 10.1053/crad.1999.0173. PMID: 10988058. [DOI] [PubMed] [Google Scholar]
- 7.Heffernan C., Pachter H.L., Megibow A.J., Macari M. Stercoral colitis leading to fatal peritonitis: CT findings. AJR Am J Roentgenol. 2005;184:1189–1193. doi: 10.2214/ajr.184.4.01841189. PMID: 15788592. [DOI] [PubMed] [Google Scholar]
- 8.Bauer J.J., Weiss M., Dreiling D.A. Stercoraceous perforation of the colon. Surg Clin North Am. 1972;52:1047–1053. doi: 10.1016/s0039-6109(16)39802-4. PMID: 5047522. [DOI] [PubMed] [Google Scholar]
- 9.Hussain Z., Hussain W.D., Hussain L.B., Hussain Fecal impaction. Current gastroenterology reports. 2014 doi: 10.1007/s11894-014-0. PMID: 25119877. [DOI] [PubMed] [Google Scholar]
- 10.Benninga M., Candy D.C., Catto-Smith A.G., Clayden G., Loening-Baucke V., Di Lorenzo C. The Paris consensus on childhood constipation terminology (PACCT) group. J Pediatr Gastroenterol Nutr. 2005;40:273–275. doi: 10.1097/01.mpg.0000158071.24327.88. PMID: 15735478. [DOI] [PubMed] [Google Scholar]
- 11.Forootan M., Bagheri N., Darvishi M. Chronic constipation: A review of literature. Medicine (Baltimore) 2018;97(20):e10631. doi: 10.1097/MD.0000000000010631. PMID: 29768326PMCID: PMC5976340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munjal Y.P., Sharma S.K. ninth edition. Jaypee Brothers Medical Publishers; 2012. API Textbook of Medicine; p. 249. Pages772, 787, 840, 880. ISBN-10: 9350250748, ISBN-13: 978-9350250747. [Google Scholar]
- 13.Hsiao T.F., Chou Y.H. Stercoral perforation of colon: a rare but important mimicker of acute appendicitis. Am J Emerg Med. 2010;28:112.e1–112.e2. doi: 10.1016/j.ajem.2009.02.024. PMID: 20006219. [DOI] [PubMed] [Google Scholar]
- 14.Huang W.S., Wang C.S., Hsieh C.C., Lin P.Y., Chin C.C., Wang J.Y. Management of patients with stercoral perforation of the sigmoid colon: report of five cases. World J Gastroenterol. 2006;12:500–503. doi: 10.3748/wjg.v12.i3.500. PMID: 16489660PMCID: PMC4066079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ünal E., Onur M.R., Balcı S., Görmez A., Akpınar E., Böge M. Stercoral colitis: diagnostic value of CT findings. Diagn Interv Radiol. 2017;23(1):5–9. doi: 10.5152/dir.2016.16002. PMID 27910814PMCID: PMC5214077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu C.H., Huang C.C., Wang L.J., Wong Y.C., Wang C.J., Lo W.C. Value of CT in the discrimination of fatal from non-fatal stercoral colitis. Korean J Radiol. 2012;13:283–289. doi: 10.3348/kjr.2012.13.3.283. PMID: 22563265PMCID: PMC3337864; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar P., Pearce O., Higginson A. Imaging manifestations of fecal impaction and stercoral perforation. Clin Radiol. 2011;66:83–88. doi: 10.1016/j.crad.2010.08.002. PMID: 21147303. [DOI] [PubMed] [Google Scholar]
- 18.Naseer M., Gandhi J., Chams N., Kulairi Z. Stercoral colitis complicated with ischemic colitis: a double-edge sword. BMC Gastroenterol. 2017;17(1):129. doi: 10.1186/s12876-017-0686-6. PMID: 29179680PMCID: PMC5704496; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morano C., Sharman T. StatPearls Publishing; Treasure Island (FL): 2020. Stercoral Colitis. StatPearls [Internet]2021 Jan–. PMID: 32809443. [PubMed] [Google Scholar]
- 20.Tokunaga Y., Hata K., Nishitai R., Kaganoi J., Nanbu H., Ohsumi K. Spontaneous perforation of the rectum with possible stercoral etiology: report of a case and review of the literature. Surg Today. 1998;28(9):937–939. doi: 10.1007/s005950050256. PMID: 9744404. [DOI] [PubMed] [Google Scholar]
- 21.Bae S.H. Diets for constipation. Pediatr Gastroenterol Hepatol Nutr. 2014;17(4):203–208. doi: 10.5223/pghn.2014.17.4.203. PMID: 25587519PMCID: PMC4291444. [DOI] [PMC free article] [PubMed] [Google Scholar]