Highlights
-
•
PA was consistently associated with mental health.
-
•
There were positive associations between PA and overall psychological well-being.
-
•
PA was negatively associated with anxiety and fatigue.
-
•
Unstructured PA showed the most robust relationship with mental health.
-
•
Body composition, sex and age moderated the associations.
Keywords: Physical activity, Mental health, Children and youth, Special educational needs
Abstract
The association between physical activity (PA) and mental health in typically developing children has been amply documented, but little is known about the corresponding association in children with special educational needs (SEN). This systematic review aimed to synthesize the evidence for the association between PA and mental health in children with SEN. A systematic literature search of five databases (PsycINFO, SPORTDiscus, PubMed, Web of Science, and CINAHL) was conducted, and the publication year was between October 2010 and February 2021. Two researchers performed abstract and full text screening and extracted the data independently. Inclusion and exclusion criteria followed the PICOS framework, and the quality of eligible studies was assessed using the McMaster critical review form. Eighteen studies that met the inclusion criteria and had quality ratings ≥ 60% were included in this review. PA was positively associated with overall psychological well-being and its subtypes (including enjoyment, self-worth, self-competence, mental wellness, and quality of life), and negatively associated with anxiety and fatigue. Body composition, age, and sex were moderators of the association. The findings of this review indicated that PA was consistently associated with mental health in children with SEN. These associations were the most powerful when PA was conducted in unstructured types such as free play and recess activities. Structured types including physical education classes were more strongly related to mental health than overall PA (combined structured and unstructured types). Future PA interventions are needed to promote mental health in children with SEN.
1. Introduction
Mental health disorders result in lifelong mental health problems and unhealthy social development in children and adolescents (World Health Organization, 2019), and mental health is defined as a state of well-being in an individual's work and life and enables individuals to contribute to their communities (Downs et al., 2018). Psychological well-being, such as enjoyment, life satisfaction, and self-concept, is considered as efficient psychological functioning; whereas psychological ill-being is reflected in the presence of negative affect and psychological malfunctioning such as stress, anxiety, depression, fatigue, and burnout (Stebbings et al., 2012). Both psychological well-being and psychological ill-being should be considered when assessing mental health (Rodriguez-Ayllon et al., 2019). As far as children with SEN are concerned, nearly 60% of this group have problems in speech and language, emotional-behavioral regulation, or schoolwork (Young et al., 2019). Compared to their typically developing peers, children with SEN are at greater risk of developing mental health problems such as anxiety and self-harm (Downs et al., 2018, Emerson et al., 2010, Licence et al., 2019).
The association of PA with mental health in typically developing children has been extensively studied over the past four decades (Biddle et al., 2019). Evidence shows that regular PA participation is positively associated with self-perception, self-efficacy, self-esteem, and confidence in typically developing children (Ahn and Fedewa, 2011, Martin, 2013). The positive effects of PA on mental health in children could be explained by neurobiological, psychosocial, and behavioral mechanisms (Lubans et al., 2016). Despite these benefits, children or adolescents with SEN tend to engage in much less PA and exhibit far higher sedentary behaviors than their typically developing peers (Corvey et al., 2016, Sit et al., 2020). Sedentary behavior may lead to less PA time, excessive screen-based media exposure, social isolation, and feelings of loneliness, resulting in mental health problems (Rodriguez-Ayllon et al., 2019). Previous studies have shown that PA is positively associated with mental health such as enjoyment (Jin et al., 2018, Martin et al., 2013, PALISANO et al., 2011), self-perception (Batey et al., 2014, Li et al., 2018, Martin et al., 2013, Ng et al., 2014, Te Velde et al., 2018), and mental wellness (Brunes et al., 2015, Giese et al., 2017, Puce et al., 2019); and is negatively associated with anxiety and depression (Brunes et al., 2015, Fiorilli et al., 2016, Gawrilow et al., 2016, Whitney et al., 2019a, Whitney et al., 2019b) and fatigue (Maher et al., 2015) in children with SEN. The strength of the associations varies according to different PA types. This includes out-of-school time PA (Arbour-Nicitopoulos et al., 2018), school-based PA (Hartmann et al., 2010), leisure-time PA (Dahan-Oliel et al., 2012), organized sports (Sahlin & Lexell, 2015), and physical education (Kraft et al., 2019).
Several reviews have focused on the associations between PA and mental health in children with SEN. One review studied the relationship between dance and self-concept in children with SEN but found no associations (May et al., 2021). Another systematic review demonstrated that self-efficacy could be an essential factor associated with PA in children with physical disabilities (Bloemen et al., 2015). Other reviews have found positive effects of PA on several mental health dimensions for children with SEN, including psychological well-being (Arbour-Nicitopoulos et al., 2018), self-efficacy (Kapsal et al., 2019), self-esteem (Dahan-Oliel et al., 2012), anxiety (Cerrillo-Urbina et al., 2015), and depression (Veneri et al., 2018). One review suggested that the effects of PA might be moderated by age, environment, and social factors (Rodriguez-Ayllon et al., 2019). Therefore, a comprehensive assessment of any possible association is required, which covers several types of SEN, mental health dimensions, different PA types, and moderators, to enable more general conclusions to be drawn.
Consequently, the aims of the study were (1) to systematically collate and synthesize the findings of recent observational studies conducted to date, and (2) to examine the evidence for the associations between different PA types and mental health dimensions in children with SEN.
2. Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (Moher et al., 2009). The PRISMA guidelines contain 27 items (see Appendix A) and act as a reference for the critical appraisal of published systematic reviews (Moher et al., 2009). A protocol for this review was registered with PROSPERO (CRD42021238181).
2.1. Search strategy
A systematic search was conducted using PsycINFO (OVID), SPORTDiscus (EBSCO), PubMed (NIBI), CINAHL (EBSCO), and Web of Science databases, and followed the PICOS (population, intervention, comparison, outcome, study design) framework (Stern et al., 2014). The initial search was conducted in October 2019 and then performed again in February 2021, and the publication year was between October 2010 and February 2021. The search strategy followed a previous study (Aromataris & Riitano, 2014), and two researchers (WY and CHPS) were involved in the process. Four terms were used in the search: (1) special educational needs, (2) children and adolescents, (3) physical activity, and (4) mental health. The search strategy in the PubMed database is shown in Appendix B.
2.2. Selection procedure and eligibility criteria
After all duplicates were removed, two reviewers independently screened the titles, abstracts, and full text of the search studies. References were imported and uploaded to Endnote X9, and the reviewers resolved any disagreements through discussion. The inter-rater reliability between the two reviewers was moderate (k = 0.61) for full-text screening.
The inclusion and exclusion criteria followed the PICOS framework (Stern et al., 2014). The PICOS framework was modified, excluding I = interventions and C = comparison. Inclusion criteria for eligible studies were: (1) population: children or adolescents aged 5–17 years with SEN; (2) outcome: measured and reported at least one outcome on PA such as physical education, Special Olympics, exercise, and sports; measured and reported at least one outcome on mental health such as self-perception, enjoyment, mental wellness, anxiety, depression, and fatigue; (3) study design: observational studies (including cross-sectional, longitudinal, cohort, and case-control studies), and published in a peer-reviewed journal with full text in English from October 2010 to February 2021. The exclusion criteria were: (1) outcome: without any outcomes on PA or mental health; (2) study design: case studies, qualitative studies, intervention studies, or reviews; published as a conference poster, conference abstract, protocol, or commentary; or published earlier than October 2010.
2.3. Data extraction
Data extraction followed the Cochrane handbook for systematic reviews of interventions (Higgins et al., 2019). Further, the following data were extracted by two researchers (WY & CHPS) from each of the eligible studies: author, year, country, participant characteristics (i.e., number of participants, age, sex, and disability type), research design, different PA types (i.e., unstructured PA, structured PA, and overall PA [combined]; Kinder et al., 2020), moderators (i.e., body composition, sex, and age), measures of PA, dimensions of mental health (i.e., psychological well-being and psychological ill-being; Rodriguez-Ayllon et al., 2019), measures of mental health, and mental health outcomes (positive association, negative association, no association).
2.4. Quality assessment
The McMaster Critical Review Form (Law et al., 1998) was used to assess the risk of bias in the included studies (see Appendix C). It contains 13 criteria, of which five were chosen in this review: design, sample in detail, outcome measures reliable, valid outcome measures, and analysis method. In ranking the quality of papers numerically, a scoring system was formulated. One mark was allocated for each “yes” answer and no marks for a “no” answer, and the ranking process was conducted by a researcher (WY). The top mark was 5, and only those studies that scored 3 or above (i.e., quality ratings ≥ 60%) could provide the best recommendations.
2.5. Data synthesis
Table 1 shows the method for rating the evidence of the association between PA and mental health (Sallis et al., 2000, Li et al., 2016). If 33% or fewer of the included articles showed significant associations, there was no association "0" in code meaning. If 34–59% of the included articles reported statistically significant outcomes, the result was identified as an inconsistent association "?" in code meaning. If more than 60% of the included articles illustrated significant outcomes, it was classified as positive association "+" or negative association "-" When the number of included articles was over 3, the symbols of "00", "??", "++", "--" could be used in summary code.
Table 1.
The strength of evidence of the association between PA and mental health.
| % of studies supporting the association | Summary code | Code meaning |
|---|---|---|
| 1–33 | 0 | No association |
| 34–59 | ? | Inconsistent association |
| 60–100 | + | Positive association |
| – | Negative association |
3. Results
3.1. Study selection
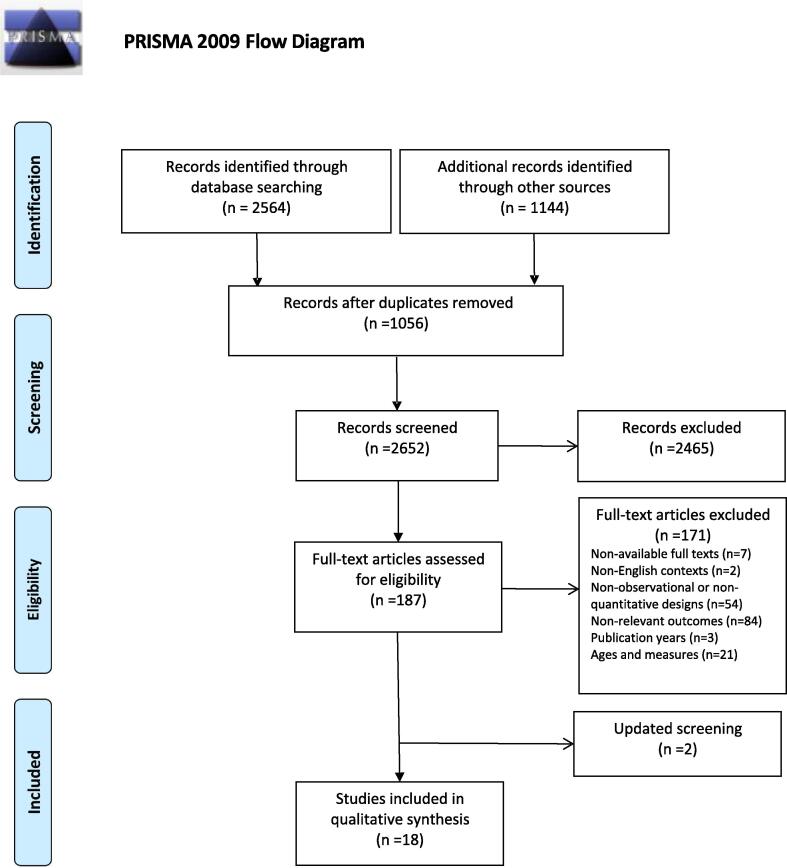
A total of 3,708 original articles were obtained from five databases. After duplicates were removed, 2,652 articles remained, and 2,465 of these articles were excluded after their titles and abstracts were screened. A further 171 articles were removed after their full texts were screened for the following reasons: 7 for non-available full-texts, 2 for non-English contexts, 54 for non-observational or non-quantitative designs, 84 for non-relevant outcomes, 3 for publication years, and 21 for ages and measures. A further screening was performed in February 2021 and two more papers were included. This left us with 18 studies for inclusion in the systematic review. Fig. 1 shows the PRISMA flowchart of the search and screening process.
Fig. 1.
PRISMA flowchart showing the literature searching and screening process.
3.2. Characteristics of included studies
A summary of the author, year, country, participant characteristics, and design is shown in Table 2. The sample size used in the 18 included studies ranged from 29 to 1,059, and 11 studies included more than 100 participants (Giese et al., 2017, Jin et al., 2018, Ng et al., 2014, PALISANO et al., 2011, Puce et al., 2019, Te Velde et al., 2018, Shikako-Thomas et al., 2013, Whitney et al., 2019a, Whitney et al., 2019b, Gür et al., 2020, Gallego-Méndez et al., 2020). The age range of participants was between 5 and 17 years, with the smallest mean age 9.8 ± 2 years (Palisano et al., 2011), and the largest mean age 17.4 ± 3.7 years (Puce et al., 2019). There were 15 cross-sectional studies (Batey et al., 2014, Fiorilli et al., 2016, Giese et al., 2017, Jin et al., 2018, Li et al., 2018, Maher et al., 2015, Martin et al., 2013, Ng et al., 2014, Puce et al., 2019, Te Velde et al., 2018, Shikako-Thomas et al., 2013, Whitney et al., 2019a, Whitney et al., 2019b, Gür et al., 2020, Gallego-Méndez et al., 2020), one longitudinal study (Gawrilow et al., 2016), and two cohort studies (Brunes et al., 2015, PALISANO et al., 2011). The included studies were conducted mainly in Western countries. Six studies were conducted in the USA (Jin et al., 2018, Li et al., 2018, Martin et al., 2013, PALISANO et al., 2011, Whitney et al., 2019a, Whitney et al., 2019b), two in Canada (Batey et al., 2014, Shikako-Thomas et al., 2013), two in Italy (Fiorilli et al., 2016, Puce et al., 2019), two in Germany (Gawrilow et al., 2016, Giese et al., 2017), and one in Norway (Brunes et al., 2015), Finland (Ng et al., 2014), the Netherlands (Te Velde et al., 2018), Australia (Maher et al., 2015), Turkey (Gür et al., 2020), and Spain (Gallego-Méndez et al., 2020). Furthermore, seven types of SEN were included in this review: three included papers discussing physical disability (Maher et al., 2015, Puce et al., 2019, Te Velde et al., 2018), three for intellectual disability (Fiorilli et al., 2016, Puce et al., 2019, Whitney et al., 2019a), three for cerebral palsy (PALISANO et al., 2011, Shikako-Thomas et al., 2013, Whitney et al., 2019b), three for visual impairment (Brunes et al., 2015, Giese et al., 2017, Gür et al., 2020), two for developmental coordination disorder (Batey et al., 2014, Li et al., 2018), two for attention deficit hyperactivity disorder (ADHD) (Gawrilow et al., 2016, Gallego-Méndez et al., 2020), and one for hearing impairment (Martin et al., 2013). Moreover, two studies focused on several types of disabilities (Jin et al., 2018, Ng et al., 2014).
Table 2.
Summary of characteristics of reviewed studies (n = 18).
| No. | Author/Year/Country | Participants’ characteristics | Design | |||
|---|---|---|---|---|---|---|
| N | Age (M ± SD) | Sex (M:F) | Disability type | |||
| 1 | Batey et al. (2014); Canada | 29 | 13.3 ± 0.48 | 19:10 | DCD | Cross-sectional |
| 2 | Brunes et al. (2015); Norway | 46 | 12–17 | 21:25 | VI | Cohort study |
| 3 | Fiorilli et al. (2016); Italy | 93 | PA:16.31 ± 1.55 C:16.06 ± 1.39 |
54:39 | ID | Cross-sectional |
| 4 | Gawrilow et al. (2016); Germany | 38 | 14.37 ± 1.88 | 18:20 | ADHD | Longitudinal |
| 5 | Giese et al. (2017); Germany | 115 | 16 ± 3.1 | 67:48 | VI | Cross-sectional |
| 6 |
Jin et al. (2018); US |
251 | 5–15 | 129:112 | SD | Cross-sectional |
| 7 |
Li et al. (2018); US |
79 | 13.45 ± 0.38 | 30:49 | DCD | Cross-sectional |
| 8 | Maher et al. (2015); Australia | 65 | 8–17 | 35:30 | PD | Cross-sectional |
| 9 | Martin et al. (2013); US | 64 | 14.1 ± 2.1 | 42:22 | HI | Cross-sectional |
| 10 | Ng et al. (2014); Finland | 1059 | 14.76 ± 1.06 | 463:596 | SD | Cross-sectional |
| 11 | Palisano et al. (2011); US | 288 | 9.8 ± 2 | 166:122 | CP | Cohort study |
| 12 | Puce et al. (2019); Italy | 200 | PA:17.4 ± 3.7 C:17 ± 3.7 |
93:107 | PD / ID | Cross-sectional |
| 13 |
Te Velde et al. (2018); Netherlands |
195 | 14.3 ± 2.8 | 116:79 | PD | Cross-sectional |
| 14 |
Shikako-Thomas et al. (2013) Canada |
187 | 15.4 ± 2.2 | 110:75 | CP | Cross-sectional |
| 15 | Whitney et al. (2019a); US | 423 | 6–17 | 268:155 | ID | Cross-sectional |
| 16 | Whitney et al. (2019b); US | 133 | 6–17 | 84:49 | CP | Cross-sectional |
| 17 | Gür et al. (2020); Turkey | 139 | 13.0 ± 1.23 | 78:61 | VI | Cross-sectional |
| 18 | Gallego-Méndez et al. (2020); Spain | 496 | 10.81 ± 2.04 | 274:222 | ADHD | Cross-sectional |
Note: ADHD: attention-deficit/ hyperactivity disorder; C: control group; CP: cerebral palsy; DCD: developmental coordination disorder; HI: hearing impairment; ID: intellectual disorder; PA: physical activity group; PD: physical disorder; SD: several types of disabilities; VI: visual impairment.
A summary of PA, mental health, and outcomes is shown in Table 3. Five studies were restricted to unstructured PA (leisure-time PA, recreational PA, free time PA, and free play), four studies to structured PA (organized sports, Paralympics, Special Olympics, and physical education), and seven studies to overall PA (combined). For the measures of PA, nine studies used self-reported measurements (WHO Health Behavior in School-aged Children Study, National Youth Fitness Survey, Participation Questionnaire, Godin Leisure-Time Exercise Questionnaire, Children’s Assessment of Participation and Enjoyment, Adolescent Lifestyle Profile-Revised 2 Physical Activity subscale, National Health Survey of Spain 2017), four articles were objectively evaluated by accelerometers (RT3 Triaxial Actual Accelerometer, GT3X + Accelerometer) or pedometers (OMRON Pedometers), and three studies used parent-reported measurements (National Survey of Children’s Health, Paediatric Outcome Data Collection Inventory). As for the measures of mental health, that were the most frequently used were scales (Self-efficacy Scales, Spiritual Well-being Scale, 5-point daily diary scale, PedsQL Multidimensional Fatigue Scale, Barrier Self-efficacy Scale, Physical Activity Enjoyment Scale, Rosenberg Self-esteem Scale, Self-perception Profile for Children, Self-perception for Adolescents, Exercise Self-efficacy Scale), and others were questionnaires (Strengths and Difficulties Questionnaire, WHO Five Well-being Index, Hopkins Symptom Checklists, Psychological General Well-being Index), and survey (Short Form 12-Mental Component Summary).
Table 3.
Summary of PA, mental health and outcomes of reviewed studies (n = 18).
| No. | Author/Year | PA | Mental Health | Outcomes | ||
|---|---|---|---|---|---|---|
| Types | Measures | Dimensions | Measures | |||
| 1 | Batey et al. (2014) | Overall PA (Daily PA) |
RT3 Triaxial Actual Accelerometer | Self-efficacy | The self-efficacy scale | Barrier Efficacy 0 Task Efficacy 0 |
| 2 | Brunes et al. (2015) | Unstructured PA (Leisure-time PA) | Self-report (WHO HBSC Study) |
Mental Wellness, Anxiety, Depression | SCL/SWB | Mental Well-being + Anxiety-, Depression - |
| 3 | Fiorilli et al. (2016) | Structured PA (Special Olympic) | Self-report (Special Olympic Swimming) |
Anxiety, Depression | SDQ-SR/ SDQ-P |
Anxiety, Depression: Parent Report - Self-Report 0 |
| 4 | Gawrilow et al. (2016) | Overall PA (Daily PA) |
Pedometer (OMRON HJ-113) |
Depression | Daily diary | Depression: Within Person - Between Person 0 |
| 5 | Giese et al. (2017) | Overall PA (Daily PA) |
OMRON Walking Style Pro Pedometers | Mental Wellness | The WHO-Five Well-being Index | Emotional Well-being + |
| 6 | Jin et al. (2018) | Overall PA (Daily PA) |
Self-report (National Youth Fitness Survey) |
Enjoyment | National Youth Fitness Survey | Enjoyment: 5-11yrs + 12-15yrs + |
| 7 | Li et al. (2018) | Overall PA (Organized Sport and Active Free Play) | Self-report (PQ) |
Self-worth | SPPC | Global Self-worth: Male + Female + |
| 8 | Maher et al. (2015) | Overall PA (Daily PA) |
GT3X + Accelerometer | Fatigue | PedsQL Multidimensional Fatigue Scale | Total Fatigue - Sleep and Rest Fatigue - General Fatigue 0 Cognitive Fatigue 0 |
| 9 | Martin et al. (2013) | Unstructured PA (Leisure-time PA) | Self-report (Godin Leisure-Time Exercise Questionnaire) |
Self-efficacy, Enjoyment |
BSE/PAE | Barrier Self-efficacy 0 PA Enjoyment 0 |
| 10 | Ng et al. (2014) | Overall PA (MVPA) |
Self-report (WHO-HBSC) |
Self-esteem | Rosenberg self-esteem scale | Global Self-esteem: Male 0 Female 0 |
| 11 | Palisano et al. (2011) | Unstructured PA (Leisure and recreational PA) | Parent-report (PODCI) |
Enjoyment | CAPE | Enjoyment + |
| 12 | Puce et al. (2019) | Structured PA (Paralympic) | Self-report (Paralympic Swimming) |
Mental Wellness | PGWBI/ SF12-MCS |
Psychological and General Well-being + Emotional Well-being + |
| 13 | Te Velde et al. (2018) | Structured PA (Organized Sport) | Self-report (RIVM) |
Self-worth | SPPC, SPPA, the Exercise Self-efficacy Scale | Global Self-worth 0 Exercise Self-worth + |
| 14 | Shikako-Thomas et al. (2013) | Unstructured PA (Leisure-time PA) | Self-report (CAPE) |
Self-competence | SPPA | Job Competence + Athletic Competence + |
| 15 | Whitney et al. (2019a) | Overall PA (Daily PA) |
Parent-report (2016 NSCH) |
Anxiety, Depression | 2016 NSCH | Anxiety 0 Depression 0 |
| 16 | Whitney et al. (2019b) | Overall PA (Daily PA) |
Parent-report (2016 NSCH) |
Anxiety, Depression |
2016 NSCH | Anxiety - Depression - |
| 17 | Gür et al. (2020) | Overall PA (Recess and physical education) | ALPS-R2 | Enjoyment | Physical Activity Enjoyment Scale | Enjoyment + |
| 18 | Gallego-Méndez et al. (2020) | Unstructured PA (Free time PA) | K61 in ENSE 2017 | Quality of Life | MAPPING CHU9D; KS9 | Quality of Life: MAPPING CHU9D + KS9 + |
3.3. Quality assessment
Table 4 shows the quality assessment results of the reviewed studies. A total of 10 studies (55.6%) received the maximum score of five, which focused on self-efficacy (Batey et al., 2014, Martin et al., 2013), self-worth (Li et al., 2018, Te Velde et al., 2018), self-competence (Shikako-Thomas et al., 2013), mental wellness (Puce et al., 2019), depression (Gawrilow et al., 2016), anxiety and depression (Brunes et al., 2015), fatigue (Maher et al., 2015) and enjoyment (Palisano et al., 2011). Two studies (11%) received a score of four about self-esteem (Ng et al., 2014) and quality of life (Gallego-Méndez et al., 2020); and six studies (33%) scored three on enjoyment (Jin et al., 2018, Gür et al., 2020), mental wellness (Giese et al., 2017), and anxiety and depression (Fiorilli et al., 2016, Whitney et al., 2019a, Whitney et al., 2019b). All included studies met the criteria of design, sample in detail, and the analysis method. However, five studies did not show outcome measure reliability, and six studies had no outcome measure validity. In general, all of the included studies scored at least 3, indicating that they possessed quality ratings ≥ 60% and met the criteria of quality assessments.
Table 4.
Summary of quality assessment of reviewed studies (n = 18).
| Author & Year | Design | Sample in detail | Outcome measures reliable | Outcome measures valid | Analysis method | Total |
|---|---|---|---|---|---|---|
| Batey et al. (2014) | 1 | 1 | 1 | 1 | 1 | 5 |
| Brunes et al. (2015) | 1 | 1 | 1 | 1 | 1 | 5 |
| Fiorilli et al. (2016) | 1 | 1 | 0 | 0 | 1 | 3 |
| Gawrilow et al. (2016) | 1 | 1 | 1 | 1 | 1 | 5 |
| Giese et al. (2017) | 1 | 1 | 0 | 0 | 1 | 3 |
| Jin et al. (2018) | 1 | 1 | 0 | 0 | 1 | 3 |
| Li et al. (2018) | 1 | 1 | 1 | 1 | 1 | 5 |
| Maher et al. (2015) | 1 | 1 | 1 | 1 | 1 | 5 |
| Martin et al. (2013) | 1 | 1 | 1 | 1 | 1 | 5 |
| Ng et al. (2014) | 1 | 1 | 1 | 0 | 1 | 4 |
| Palisano et al. (2011) | 1 | 1 | 1 | 1 | 1 | 5 |
| Puce et al. (2019) | 1 | 1 | 1 | 1 | 1 | 5 |
| Te Velde et al. (2018) | 1 | 1 | 1 | 1 | 1 | 5 |
| Shikako-Thomas et al. (2013) | 1 | 1 | 1 | 1 | 1 | 5 |
| Whitney et al. (2019a) | 1 | 1 | 0 | 0 | 1 | 3 |
| Whitney et al. (2019b) | 1 | 1 | 0 | 0 | 1 | 3 |
| Gür et al. (2020) | 1 | 1 | 0 | 0 | 1 | 3 |
| Gallego-Méndez et al. (2020) | 0 | 1 | 1 | 1 | 1 | 4 |
Note: 1 = Yes, 2 = No.
3.4. Summary of findings
Table 5 presents the associations between PA and mental health in children with SEN divided by psychological well-being (13 of 19 outcomes, 68%) and psychological ill-being (9 of 16 outcomes, 56%). The evidence of associations between PA and overall psychological well-being was consistent and positive. Among the four psychological well-being outcomes (enjoyment, self-perception, mental wellness, and quality of life), PA was positively associated with enjoyment (3 of 4 outcomes, 75%; Jin et al., 2018, PALISANO et al., 2011, Gür et al., 2020), but not inconsistently associated with self-perception (4 of 9 outcomes, 44%; Li et al., 2018, Te Velde et al., 2018, Shikako-Thomas et al., 2013). Among the self-perception subtypes, PA was positively associated with self-worth (2 of 3 outcomes, 67%; Li et al., 2018, Te Velde et al., 2018) and self-competence (2 of 2 outcomes, 100%; Shikako-Thomas et al., 2013). PA was also found to be positively associated with quality of life (2 of 2 outcomes, 100%; Gallego-Méndez et al., 2020) and mental wellness (4 of 4 outcomes, 100%; Brunes et al., 2015, Giese et al., 2017, PALISANO et al., 2011), which included mental well-being (1 of 1 outcome, 100%; Brunes et al., 2015), psychological and general well-being (1 of 1 outcome, 100%; Puce et al., 2019), and emotional well-being (2 of 2 outcomes, 100%; Giese et al., 2017, Puce et al., 2019).
Table 5.
Summary of associations between PA and mental health (well-being & ill-being) (n = 18).
| Correlates | Related to PA | Unrelated to PA | Summary Code | ||
|---|---|---|---|---|---|
| Bibliography no. | Assoc. (-/+) |
Bibliography no. | % of studies | Assoc. (-/+/?/0) |
|
| Psychological well-being: | 13/19= 68% |
++ | |||
| Enjoyment | 6, 11, 17 | + | 9(1) | 3/4 = 75% | ++ |
| Self-perception | 7, 13(2), 14(1), 14(2) | 1(1), 1(2), 9(2), 10, 13(1) | 4/9 = 44% | ?? | |
| Self-worth | 7, 13(2) | + | 13(1) | 2/3 = 67% | ++ |
| Self-efficacy | 1(1), 1(2), 9(2) | 0/3 = 0% | 00 | ||
| Self-esteem | 10 | 0/1 = 0% | 0 | ||
| Self-competence | 14(1), 14(2) | 2/2 = 100% | + | ||
| Mental wellness | 2(1), 5, 12(1)a1, b1, 12(2) | + | 4/4 = 100% | ++ | |
| Mental well-being | 2(1) | 1/1 = 100% | + | ||
| Emotional well-being | 5, 12(2) | + | 2/2 = 100% | + | |
| Psychological and general well-being | 12(1) | + | 1/1 = 100% | + | |
| Quality of life | 18(1), 18(2) | + | 2/2 = 100% | + | |
| Psychological ill-being: | 9/16= 56% |
?? | |||
| Anxiety | 3(1), 2(2), 16(1) | – | 3(2), 15(1) | 3/5 = 60% | – |
| Depression | 4(1), 16(2), 2(3), 3(3) | – | 4(2), 3(4), 15(2) | 4/7 = 57% | ?? |
| Fatigue (Total) | 8(1)a2, b1 | – | 1/1 = 100% | – | |
| General fatigue | 8(2) | 0/1 = 0% | 0 | ||
| Sleep and rest fatigue | 8(3) | – | 1/1 = 100% | – | |
| Cognitive fatigue | 8(4) | 0/1 = 0% | 0 | ||
| Overall Mental Health | 22/35 = 63% | ||||
Note: 1(1): result of barrier efficacy; 1(2): result of task efficacy; 2(1): result of mental well-being; 2(2): result of anxiety; 2(3): result of depression; 3(1): anxiety result from parent-report; 3(2): depression result from parent-report; ; 3(3): anxiety result from self-report; 3(4): depression result from self-report; 4(1): within-person result of depression; 4(2): between-person result of depression; 8(1): result of total fatigue; 8(2): result of general fatigue; 8(3): result of sleep and rest fatigue; 8(4): result of cognitive fatigue; 9(1): result of physical activity enjoyment; 9(2): result of barrier self-efficacy; 12(1): result of psychological and emotional well-being; 12(2): result of emotional well-being; 13(1): result of global self-worth; 13(2): result of exercise self-worth; 14(1): result of job competence; 14(2): result of exercise competence;15(1): result of anxiety; 15(2): result of depression; 16(1): result of anxiety; 16(2): result of depression; 18(1): results of MAPPING CHU9D; 18(2): results of KS9; a1: male > female; a2: male < female; b1: younger > older; b2: younger < older; +: positive association; -: negative association; ?: inconsistent association; 0: no association.
Three psychological ill-being outcomes (anxiety, depression, and fatigue) were included in the review, and the evidence of associations between PA and overall psychological ill-being was inconsistent. There was a negative association between PA and anxiety (3 of 5 outcomes, 60%; Fiorilli et al., 2016, Brunes et al., 2015, Whitney et al., 2019a, Whitney et al., 2019b), but an inconsistent association between PA and depression (4 of 7 outcomes, 57%; Brunes et al., 2015, Fiorilli et al., 2016, Gawrilow et al., 2016, Whitney et al., 2019a, Whitney et al., 2019b). Only one article studied fatigue, which was divided into three subtypes: sleep and rest fatigue, cognitive fatigue, and general fatigue (Maher et al., 2015). PA was found to be negatively associated with sleep and rest fatigue (1 of 1 outcome, 100%), but not general fatigue (0 of 1 outcome, 0%) and cognitive fatigue (0 of 1 outcome, 0%).
Body composition, sex, and age were used as moderators in our review. It was found that PA was positively associated with body composition values and that better body composition values led to better mental wellness (Giese et al., 2017). There were stronger evidence of PA and mental wellness associations in boys and younger children with SEN than in girls and older children with SEN respectively (Puce et al., 2019). One study reported a higher level of fatigue associated with PA in girls and younger children with SEN than in their male and older counterparts respectively (Maher et al., 2015).
Table 6 illustrates the associations between PA and mental health according to PA types. PA was grouped into unstructured, structured, and overall PA (combined) (Kinder et al., 2020, Mota and Esculcas, 2002). The results showed that unstructured PA and structured PA was positively associated with mental health rather than overall PA (combined). Meanwhile unstructured PA had the strongest evidence with mental health (8 of 10 outcomes, 80%), such as mental wellness, enjoyment, self-competence, quality of life, anxiety, and depression (Brunes et al., 2015, PALISANO et al., 2011, Shikako-Thomas et al., 2013, Gallego-Méndez et al., 2020). The association between structured PA and mental health was stronger such as anxiety, depression, mental wellness, and self-worth (5 of 8 outcomes, 63%; Fiorilli et al., 2016, Puce et al., 2019, Te Velde et al., 2018) than that of overall PA (combined) with anxiety, depression, mental wellness, enjoyment, self-worth, and fatigue (9 of 17 outcomes, 53%; Gawrilow et al., 2016, Giese et al., 2017, Jin et al., 2018, Li et al., 2018, Maher et al., 2015, Whitney et al., 2019b, Gür et al., 2020), and overall PA (combined) was the most frequently studied topic.
Table 6.
Summary of associations between PA and mental health (different PA types) (n = 18).
| Correlates | Related to Mental Health |
Unrelated to Mental Health |
Summary Code |
|
|---|---|---|---|---|
| Well-being | Ill-being | Bibliography no. | % of study | |
| Unstructured PA | 2 (1), 11, 14(1), 14(2), 18(1), 18(2) | 2(2), 2(3) | 9(1), 9(2) | 8/10 = 80% |
| Structured PA | 12(1), 12(2), 13(2) | 3(2), 3(4) | 3(1), 3(3), 13(1) | 5/8 = 63% |
| Overall PA | 5, 6, 7, 17 | 4(1), 8(1), 8(3), 16(1), 16(2) | 1(1), 1(2), 4(2), 8(2), 8(4), 10, 15(1), 15(2) | 9/17 = 53% |
Note: 1(1): result of barrier efficacy; 1(2): result of task efficacy; 2(1): result of mental well-being; 2(2): result of anxiety; 2(3) result of depression; 3(1): anxiety result from parent-report; 3(2): depression result from parent-report; 3(3): anxiety result from self-report; 3(4): depression result from self-report; 4(1): within-person result of depression; 4(2): between-person result of depression; 8(1): result of total fatigue; 8(2): result of general fatigue; 8(3): result of sleep and rest fatigue; 8(4): result of cognitive fatigue; 9(1): result of physical activity enjoyment; 9(2): result of barrier self-efficacy; 12(1): result of psychological and emotional well-being; 12(2): result of emotional well-being; 13(1): result of global self-worth; 13(2): result of exercise self-worth; 14(1): result of job competence; 14(2): result of exercise competence;15(1): result of anxiety; 15(2): result of depression; 16(1): result of anxiety; 16(2): result of depression; 18(1): result of MAPPING CHU9D; 18(2): result of KS9.
4. Discussion
This systematic review aimed to examine the association between PA and mental health in children with SEN. Further, it aimed to synthesize relevant evidence from cross-sectional, longitudinal, and cohort studies. In general, our findings showed consistent associations between PA and mental health, and there were positive and consistent associations between PA and overall psychological well-being. However, the associations between PA and overall psychological ill-being were inconsistent. Meanwhile, unstructured PA showed the strongest associations with mental health including mental wellness, enjoyment, self-competence, and quality of life.
In this present review, we found strong evidence of positive associations between PA and enjoyment, self-worth, self-competence, mental wellness, and quality of life; and negative associations between PA and anxiety, and rest fatigue in children with SEN. A possible mechanism was concluded in a systematic review (Rodriguez-Ayllon et al., 2019), which reported that PA might change the brain's structure and function, such as increasing brain-derived neurotrophic factor (BDNF), brain dopamine, serotonin, and noradrenaline concentrations, not only improve psychological well-being but also protect against psychological ill-being. However, there is a paucity of studies on PA and mental health associations in children with SEN. Previous studies have shown positive effects of PA on self-competence (Sahlin & Lexell, 2015), self-worth (McIntyre et al., 2015), quality of life (Toscano et al., 2018), mental wellness and enjoyment (Dahan-Oliel et al., 2012) in children with SEN. Moreover, there are positive effects of PA on reduced anxiety in children with cerebral palsy (Veneri et al., 2018), ADHD (Cerrillo-Urbina et al., 2015), and special needs (Baron & Faubert, 2005). Concerning fatigue, there is limited evidence, though fatigue is positively associated with functional muscle strength in children with cerebral palsy (Balemans et al., 2015). Future observational studies are needed to investigate the relationship between PA and less-studied mental health in children with SEN.
In our current review, we observed that there was an inconsistent association between PA and depression. Our findings were similar to a review of typically developing children, which reported small or null associations between PA and depression (Biddle & Asare, 2011). This inconsistency between PA and depression might be explained by the interrelationship between physical and psychiatric factors, which could influence mental health indicators (Rodriguez-Ayllon et al., 2019). We also observed that PA was not associated with self-efficacy or self-esteem. This finding, however, was contrary to a systematic review that suggested that PA was positively associated with self-efficacy in children with physical disabilities (Bloemen et al., 2015).
Distinct mental health outcomes were analyzed in groups of unstructured, structured, and overall PA (combined). Unstructured PA and structured PA showed consistent associations with mental health, but overall PA (combined) showed inconsistent associations. Unstructured PA such as leisure-time PA and out-of-school time PA is important for happiness and enjoyment in children with physical disabilities (Arbour-Nicitopoulos et al., 2018), and children with severe disability levels tend to engage more in unstructured PA (Fakolade et al., 2018). In our review, we found that structured PA was associated with mental health, and previous studies also have indicated that structured PA has positive effects on mental health, such as self-control, self-concept, and quality of life in children with ADHD (Choi et al., 2016) and neurological disabilities (Sahlin & Lexell, 2015). Meanwhile overall PA (combined) was the most frequently studied topic in our review, and this was consistent with previous studies, which concluded that both unstructured and structured PA participation types could improve quality of life in children with neurodevelopmental disabilities (Dahan-Oliel et al., 2012). Moreover, both PA types should be applied to maximize PA's positive effects (Kinder et al., 2019), and team sports have stronger mental health associations than individual sports (Rodriguez-Ayllon et al., 2019).
The associations in our present review were influenced by moderators, such as body composition, sex, and age. In a study of children with visual impairment, the better their body composition values during PA, the more positive the association with mental wellness (Giese et al., 2017). A similar association was reported, in that depression and fatigue were common in obese children with SEN, and obesity could influence the disability condition and restrict their PA participation (Reinehr et al., 2010). As for the moderating effects of age and sex, boys and younger children with SEN showed stronger evidence of an association between PA and mental wellness than did girls and older children with SEN (Puce et al., 2019). Meanwhile girls and younger children with SEN have more fatigue associated with PA than their counterparts (Maher et al., 2015). Previous articles also reported that boys have a higher enjoyment level in active PA than girls (Baksjøberget et al., 2017). Due to the lack of observational research, it was impossible to study a range of potential mediators and moderators, such as family socioeconomic status, enjoyment of PA, perceived sport competence, resilience, and social context; more studies are warranted in the future.
Through data synthesis of observational studies assessing PA and mental health associations, we found that some of the psychological well-being and ill-being dimensions were associated with PA. At this time, research on this topic is inadequate, and the paucity of published papers limited the development of PA and mental health of children with SEN. Thus, this finding has some practical implications. Investigators, society, and organizations should pay more attention to PA and children's mental health with SEN. Research funding may help create useful programs and policies to assist children with SEN to improve PA levels and mental health conditions.
Our study has several strengths. First, our present review examined the evidence for the associations between different PA types and mental health dimensions for children with different types of SEN. Second, we performed the review in accordance with the PRISMA guidelines and the PICOS framework, and we availed ourselves of a widely recognized benchmark for the included studies' scientific rigor. Third, the McMaster Critical Review Form was used to examine the quality of the included articles and improve the reliability of our results and conclusions. Nevertheless, this review has several limitations. First, the heterogeneity of types of SEN, PA, mental health, and study designs limited the extent to which the included studies could be integrated and interpreted. Second, we only considered English-language articles in the present review, which may limit the population and cultural differences in the world range. Several questions deserve further study, notably more studies on the wider relationship between PA and mental health. Finally, the bidirectional relationship and meta-analysis of PA and mental health associations could be investigated in the future.
5. Conclusion
Findings from our present review suggested that PA was positively associated with overall psychological well-being, enjoyment, self-worth, self-competence, mental wellness, and quality of life; and was negatively associated with anxiety and fatigue in children with SEN. Concerning the different PA types, unstructured PA showed the strongest relationship with mental health, and structured PA illustrated a stronger relationship with mental health than overall PA (combined). If further progress is to be made in the direction they indicate, greater attention should be given in the future to promote the mental health of children with SEN through participation in unstructured PA.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors wish to thank Dr. Jane Yu, Mr. Xiao Liang, and Mr. Cedric Ho for their assistance in the data search, quality assessment, and synthesis for the systematic review.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2021.101419.
Appendixes. Supplementary data
The following are the Supplementary data to this article:
References
- Ahn S., Fedewa A.L. A meta-analysis of the relationship between children’s physical activity and mental health. J. Pediatr. Psychol. 2011;36(4):385–397. doi: 10.1093/jpepsy/jsq107. [DOI] [PubMed] [Google Scholar]
- Arbour-Nicitopoulos K.P., Grassmann V., Orr K., McPherson A.C., Faulkner G.E., Wright F.V. A scoping review of inclusive out-of-school time physical activity programs for children and youth with physical disabilities. Adapted Physical Activity Quarterly. 2018;35(1):111–138. doi: 10.1123/apaq.2017-0012. [DOI] [PubMed] [Google Scholar]
- Aromataris E., Riitano D. Constructing a search strategy and searching for evidence. A guide to the literature search for a systematic review. The American Journal of Nursing. 2014;114(5):49–56. doi: 10.1097/01.NAJ.0000446779.99522.f6. [DOI] [PubMed] [Google Scholar]
- Balemans A.C., van Wely L., Becher J.G., Dallmeijer A.J. Longitudinal relationship among physical fitness, walking-related physical activity, and fatigue in children with cerebral palsy. Phys. Ther. 2015;95(7):996–1005. doi: 10.2522/ptj.20140270. [DOI] [PubMed] [Google Scholar]
- Baron L.J., Faubert C. The role of Tai Chi Chuan in reducing state anxiety and enhancing mood of children with special needs. Journal of Bodywork and Movement Therapies. 2005;9(2):120–133. [Google Scholar]
- Batey C.A., Missiuna C.A., Timmons B.W., Hay J.A., Faught B.E., Cairney J. Self-efficacy toward physical activity and the physical activity behavior of children with and without developmental coordination disorder. Hum. Mov. Sci. 2014;36:258–271. doi: 10.1016/j.humov.2013.10.003. [DOI] [PubMed] [Google Scholar]
- Baksjøberget P.E., Nyquist A., Moser T., Jahnsen R. Having fun and staying active! Children with disabilities and participation in physical activity: A follow-up study. Physical & Occupational Therapy in Pediatrics. 2017;37(4):347–358. doi: 10.1080/01942638.2017.1281369. [DOI] [PubMed] [Google Scholar]
- Biddle S.J.H., Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br. J. Sports Med. 2011;45(11):886–895. doi: 10.1136/bjsports-2011-090185. [DOI] [PubMed] [Google Scholar]
- Biddle S.J.H., Ciaccioni S., Thomas G., Vergeer I. Physical activity and mental health in children and adolescents: An updated review of reviews and an analysis of causality. Psychol. Sport Exerc. 2019;42:146–155. [Google Scholar]
- Bloemen M.A.T., Backx F.J.G., Takken T., Wittink H., Benner J., Mollema J., Groot J.F. Factors associated with physical activity in children and adolescents with a physical disability: A systematic review. Dev. Med. Child Neurol. 2015;57(2):137–148. doi: 10.1111/dmcn.12624. [DOI] [PubMed] [Google Scholar]
- Brunes A., Flanders W.D., Augestad L.B. The effect of physical activity on mental health among adolescents with and without self-reported visual impairment: The Young-HUNT study. Norway. British Journal of Visual Impairment. 2015;33(3):183–199. [Google Scholar]
- Cerrillo-Urbina A.J., García-Hermoso A., Sánchez-López M., Pardo-Guijarro M.J., Santos Gómez J.L., Martínez-Vizcaíno V. The effects of physical exercise in children with attention deficit hyperactivity disorder: A systematic review and meta-analysis of randomized control trials. Child Care Health Dev. 2015;41(6):779–788. doi: 10.1111/cch.12255. [DOI] [PubMed] [Google Scholar]
- Choi H., Park S., Kim K.K., Lee K., Rhyu H.-S. Acute effects of aerobic stretching, health and happiness improving movement exercise on cortical activity of children. Journal of Exercise Rehabilitation. 2016;12(4):320–327. doi: 10.12965/jer.1632602.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corvey K., Menear K.S., Preskitt J., Goldfarb S., Menachemi N. Obesity, physical activity and sedentary behaviors in children with an autism spectrum disorder. Matern. Child Health J. 2016;20(2):466–476. doi: 10.1007/s10995-015-1844-5. [DOI] [PubMed] [Google Scholar]
- Dahan-Oliel N., Shikako-Thomas K., Majnemer A. Quality of life and leisure participation in children with neurodevelopmental disabilities: a thematic analysis of the literature. Qual. Life Res. 2012;21(3):427–439. doi: 10.1007/s11136-011-0063-9. [DOI] [PubMed] [Google Scholar]
- Downs J., Blackmore A.M., Epstein A., Skoss R., Langdon K., Jacoby P., Whitehouse A.J.O., Leonard H., Rowe P.W., Glasson E.J. The prevalence of mental health disorders and symptoms in children and adolescents with cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2018;60(1):30–38. doi: 10.1111/dmcn.13555. [DOI] [PubMed] [Google Scholar]
- Emerson E., Einfeld S., Stancliffe R.J. The mental health of young children with intellectual disabilities or borderline intellectual functioning. Soc. Psychiatry Psychiatr. Epidemiol. 2010;45(5):579–587. doi: 10.1007/s00127-009-0100-y. [DOI] [PubMed] [Google Scholar]
- Fakolade A., Lamarre J., Latimer-Cheung A., Parsons T., Morrow S.A., Finlayson M. Understanding leisure-time physical activity: Voices of people with MS who have moderate-to-severe disability and their family caregivers. Health Expect. 2018;21(1):181–191. doi: 10.1111/hex.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorilli G., di Cagno A., Iuliano E., Aquino G., Calcagnile G., Calcagno G. Special Olympics swimming: Positive effects on young people with Down syndrome. Sport Sciences for Health. 2016;12(3):339–346. [Google Scholar]
- Gallego-Méndez J., Perez-Gomez J., Calzada-Rodríguez J.I., Denche-Zamorano Á.M., Mendoza-Muñoz M., Carlos-Vivas J., Garcia-Gordillo M.Á., Adsuar J.C. Relationship between health-related quality of life and physical activity in children with hyperactivity. Int. J. Environ. Res. Public Health. 2020;17(8):2804. doi: 10.3390/ijerph17082804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawrilow C., Stadler G., Langguth N., Naumann A., Boeck A. Physical activity, affect, and cognition in children with symptoms of ADHD. Journal of Attention Disorders. 2016;20(2):151–162. doi: 10.1177/1087054713493318. [DOI] [PubMed] [Google Scholar]
- Giese M., Teigland C., Giessing J. Physical activity, body composition, and well-being of school children and youths with visual impairments in Germany. British Journal of Visual Impairment. 2017;35(2):120–129. [Google Scholar]
- Gür K., Beyhan A., Aktan Ç., Akbulut E., Sezer M., Çelik Ş., Çakıcı T. Physical activity levels, enjoyment, and perceptions of barriers to physical activity of adolescents with visual impairments in Turkey. Journal of Visual Impairment & Blindness. 2020;114(6):502–515. [Google Scholar]
- Hartmann T., Zahner L., Pühse U., Puder J.J., Kriemler S. Effects of a school-based physical activity program on physical and psychosocial quality of life in elementary school children: a cluster-randomized trial. Pediatric Exercise Science. 2010;22(4):511–522. doi: 10.1123/pes.22.4.511. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A., editors. Cochrane Handbook for Systematic Reviews of Interventions. Wiley; 2019. [Google Scholar]
- Jin J., Yun J., Agiovlasitis S. Impact of enjoyment on physical activity and health among children with disabilities in schools. Disability and Health Journal. 2018;11(1):14–19. doi: 10.1016/j.dhjo.2017.04.004. [DOI] [PubMed] [Google Scholar]
- Kapsal N.J., Dicke T., Morin A.J., Vasconcellos D., Maïano C., Lee J., Lonsdale C. Effects of physical activity on the physical and psychosocial health of youth with Intellectual disabilities: A systematic review and meta-Analysis. Journal of Physical Activity and Health. 2019;16(12):1187–1195. doi: 10.1123/jpah.2018-0675. [DOI] [PubMed] [Google Scholar]
- Kinder C.J., Gaudreault K.L., Jenkins J.M., Wade C.E., Woods A.M. At-risk youth in an after-school program: Structured vs. unstructured physical activity. Physical Educator. 2019;76(5):1157–1180. [Google Scholar]
- Kinder C.J., Gaudreault K.L., Simonton K. Structured and unstructured contexts in physical education: Promoting activity, learning and motivation. Journal of Physical Education, Recreation & Dance. 2020;91(6):30–35. [Google Scholar]
- Kraft E., Leblanc R., Culver D.M. Strategies for teaching children with autism spectrum disorder in recreational aquatics programs. JOPERD: The Journal of Physical Education, Recreation & Dance. 2019;90(1):24–29. [Google Scholar]
- Law M., Stewart D., Pollock N., Letts L., Bosch J., Westmorland M. McMaster University; Ontario: 1998. Critical Review Form-Quantitative Studies. [Google Scholar]
- Licence L., Oliver C., Moss J.o., Richards C. Prevalence and risk-markers of self-harm in autistic children and adults. J. Autism Dev. Disord. 2019;50(10):3561–3574. doi: 10.1007/s10803-019-04260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R.u., Sit C.H.P., Yu J.J., Duan J.Z.J., Fan T.C.M., McKenzie T.L., Wong S.H.S. Correlates of physical activity in children and adolescents with physical disabilities: A systematic review. Prev. Med. 2016;89:184–193. doi: 10.1016/j.ypmed.2016.05.029. [DOI] [PubMed] [Google Scholar]
- Li Y.-C., Kwan M.Y.W., Clark H.J., Hay J., Faught B.E., Cairney J. A test of the Environmental Stress Hypothesis in children with and without developmental coordination disorder. Psychol. Sport Exerc. 2018;37:244–250. [Google Scholar]
- Lubans, D., Richards, J., Hillman, C., Faulkner, G., Beauchamp, M., Nilsson, M., ... & Biddle, S. (2016). Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics, 138(3). [DOI] [PubMed]
- Maher C., Crettenden A., Evans K., Thiessen M., Toohey M., Watson A., Dollman J. Fatigue is a major issue for children and adolescents with physical disabilities. Dev. Med. Child Neurol. 2015;57(8):742–747. doi: 10.1111/dmcn.12736. [DOI] [PubMed] [Google Scholar]
- Martin J.J. Benefits and barriers to physical activity for individuals with disabilities: a social-relational model of disability perspective. Disabil. Rehabil. 2013;35(24):2030–2037. doi: 10.3109/09638288.2013.802377. [DOI] [PubMed] [Google Scholar]
- Martin J.J., Shapiro D.R., Prokesova E. Predictors of physical activity among Czech and American Children with hearing impairment. European Journal of Adapted Physical Activity. 2013;6(2):38–47. [Google Scholar]
- May T., Chan E.S., Lindor E., McGinley J., Skouteris H., Austin D., McGillivray J., Rinehart N.J. Physical, cognitive, psychological and social effects of dance in children with disabilities: systematic review and meta-analysis. Disabil. Rehabil. 2021;43(1):13–26. doi: 10.1080/09638288.2019.1615139. [DOI] [PubMed] [Google Scholar]
- McIntyre F., Chivers P., Larkin D., Rose E., Hands B. Exercise can improve physical self perceptions in adolescents with low motor competence. Hum. Mov. Sci. 2015;42:333–343. doi: 10.1016/j.humov.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., Altman, D., Antes, G., . . . Berlin, J. A. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Chinese edition). Journal of Chinese Integrative Medicine, 7(9), 889–896.
- Mota, J., & Esculcas, C. (2002). Leisure-time physical activity behavior: structured and unstructured choices according to sex, age, and level of physical activity. International Journal of Behavioral Medicine, 9(2), 111–121. [DOI] [PubMed]
- Ng K., Välimaa R., Rintala P., Tynjälä J., Villberg J., Kannas L. Self-esteem and intentions mediate perceived fitness with physical activity in Finnish adolescents with long-term illness or disabilities. Acta Gymnica. 2014;44(4) [Google Scholar]
- Palisano, R. J., Chiarello, L. A., Orlin, M., Oeffinger, D., Polansky, M., Maggs, J., Bagley, A., Gorton, G., & Children's Activity and Participation Group (2011). Determinants of intensity of participation in leisure and recreational activities by children with cerebral palsy. Developmental Medicine and Child Neurology, 53(2), 142–149. [DOI] [PubMed]
- Puce L., Marinelli L., Girtler N.G., Pallecchi I., Mori L., Simonini M., Trompetto C. Self-perceived psychophysical well-being of young competitive swimmers with physical or intellectual impairment. Percept. Mot. Skills. 2019;126(5):862–885. doi: 10.1177/0031512519865849. [DOI] [PubMed] [Google Scholar]
- Reinehr T., Dobe M., Winkel K., Schaefer A., Hoffmann D. Obesity in disabled children and adolescents: an overlooked group of patients. Deutsches Arzteblatt International. 2010;107(15):268–275. doi: 10.3238/arztebl.2010.0268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Ayllon M., Cadenas-Sánchez C., Estévez-López F., Muñoz N.E., Mora-Gonzalez J., Migueles J.H., Molina-García P., Henriksson H., Mena-Molina A., Martínez-Vizcaíno V., Catena A., Löf M., Erickson K.I., Lubans D.R., Ortega F.B., Esteban-Cornejo I. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: A systematic review and meta-analysis. Sports Medicine (Auckland. N.Z.) 2019;49(9):1383–1410. doi: 10.1007/s40279-019-01099-5. [DOI] [PubMed] [Google Scholar]
- Sahlin K.B., Lexell J. Impact of organized sports on activity, participation, and quality of life in people with neurologic disabilities. PM & R: The Journal of Injury, Function, and Rehabilitation. 2015;7(10):1081–1088. doi: 10.1016/j.pmrj.2015.03.019. [DOI] [PubMed] [Google Scholar]
- Sallis J.F., Prochaska J.J., Taylor W.C. A review of correlates of physical activity of children and adolescents. Med. Sci. Sports Exerc. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- Shikako-Thomas K., Shevell M., Schmitz N., Lach L., Law M., Poulin C., QUALA group Determinants of participation in leisure activities among adolescents with cerebral palsy. Res. Dev. Disabil. 2013;34(9):2621–2634. doi: 10.1016/j.ridd.2013.05.013. [DOI] [PubMed] [Google Scholar]
- Sit C.-P., Yu J.J., Huang W.Y., Wong M.-S., Sum R.-W., Tremblay M.S., Wong S.-S. Results from Hong Kong’s 2019 report card on physical activity for children and youth with special educational needs. Journal of Exercise Science & Fitness. 2020;18(3):177–182. doi: 10.1016/j.jesf.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stebbings J., Taylor I.M., Spray C.M., Ntoumanis N. Antecedents of perceived coach interpersonal behaviors: The coaching environment and coach psychological well-and ill-being. Journal of Sport and Exercise Psychology. 2012;34(4):481–502. doi: 10.1123/jsep.34.4.481. [DOI] [PubMed] [Google Scholar]
- Stern C., Jordan Z., McArthur A. Developing the review question and inclusion criteria. The American Journal of Nursing. 2014;114(4):53–56. doi: 10.1097/01.NAJ.0000445689.67800.86. [DOI] [PubMed] [Google Scholar]
- Te Velde S.J., Lankhorst K., Zwinkels M., Verschuren O., Takken T., de Groot J., HAYS study group Associations of sport participation with self-perception, exercise self-efficacy and quality of life among children and adolescents with a physical disability or chronic disease—a cross-sectional study. Sports Medicine-Open. 2018;4(1):38. doi: 10.1186/s40798-018-0152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toscano C.V.A., Carvalho H.M., Ferreira José.P. Exercise effects for children with autism spectrum disorder: Metabolic health, autistic traits, and quality of life. Percept. Mot. Skills. 2018;125(1):126–146. doi: 10.1177/0031512517743823. [DOI] [PubMed] [Google Scholar]
- Veneri D., Gannotti M., Bertucco M., Fournier Hillman S.E. Using the International Classification of Functioning, Disability, and Health model to gain perspective of the benefits of yoga in stroke, multiple sclerosis, and children to inform practice for children with cerebral palsy: A meta-analysis. The Journal of Alternative and Complementary Medicine. 2018;24(5):439–457. doi: 10.1089/acm.2017.0030. [DOI] [PubMed] [Google Scholar]
- Whitney D.G., Shapiro D.N., Peterson M.D., Warschausky S.A. Factors associated with depression and anxiety in children with intellectual disabilities. J. Intellect. Disabil. Res. 2019;63(5):408–417. doi: 10.1111/jir.12583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitney D.G., Warschausky S.A., Peterson M.D. Mental health disorders and physical risk factors in children with cerebral palsy: A cross-sectional study. Dev. Med. Child Neurol. 2019;61(5):579–585. doi: 10.1111/dmcn.14083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . No. WHO/MSD/19.1. World Health Organization; 2019. (The WHO special initiative for mental health (2019–2023): universal health coverage for mental health). [Google Scholar]
- Young G., Philpott D.F., Butler E., Maich K., Penney S.C. Exploring the impact of quality early child education on special education: Can we prevent placement in special education? Exceptionality Education International. 2019;29(3):6–21. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.