Abstract
Orthodontic retention remains one of the great challenges in orthodontics. In this article, we discuss what is on the horizon to help address this challenge, including biological approaches to reduce relapse, treating patients without using retainers, technological developments, personalised medicine and the impact of COVID-19 on approaches to orthodontic retention.
Key points
As our understanding of biological factors affecting relapse improves, we may be able to harness this knowledge to improve stability after orthodontic treatment.
Developments in new retainer materials, digital workflow and monitoring using artificial intelligence are being investigated in the field of orthodontic retention.
Personalised medicine and patient-centred care is likely to change our approach to reducing orthodontic relapse in the future.
Introduction
Prevention of unwanted post-treatment changes remains one of the biggest challenges in orthodontics. There are a variety of ways of addressing this challenge:
Fitting fixed retainers, which require careful maintenance and monitoring to check for unwanted side effects such as detachments, fractures, unwanted tooth movement and periodontal complications secondary to plaque retention
Asking patients to wear removable retainers, which require excellent long-term adherence to wear and periodic replacement, as a result of degradation and fracture
An acceptance that without provision of retainers in the long term, there will be an unpredictable amount of post-treatment tooth movement, which can either be accepted or corrected with orthodontic re-treatment.
All of these options have associated problems, so it is perhaps not surprising that alternative ways to address this challenge are being investigated. In this article, we provide a brief overview of some of the options on the horizon.
Biological approaches to reduce relapse
The alveolar housings of orthodontically moved teeth remodel. Resorption at the pressure side occurs rapidly and allows the movement of teeth through the bone. After movement is completed, the alveolar housing and periodontal ligament is re-established on the pressure side so that it is similar to an unmoved tooth. On the tension side, where formation of new bone is required, re-establishment of the alveolar housing occurs more slowly and the periodontal ligament maintains tension on the bone, seeking to draw the tooth back to its original position. The challenge for the orthodontist is to establish conditions where the periodontal ligament (PDL) and bone alveolar housing are promptly remodelled, preserving the new position of the tooth.
External agents to reduce relapse
External agents that alter bone remodelling response have been studied with different success levels in animals. These include osteoprotegerin gene transfer, bone morphogenetic protein, systemic and local administration of different pharmacologic agents such as bisphosphonates, statins, aspirin and antibiotics, and the use of low-level laser therapy, cytokines, hormones and mechanical vibration. However, fixed retainers are still needed initially during the application of these external agents, and they can be relatively invasive and may risk systemic effects. Despite many years of experimentation, none of the approaches have reached the point where they are used routinely in the clinic. Two systematic reviews recently discussed these studies in detail.1,2
Biological approaches on the horizon
Factors have emerged recently as vital controllers of bone formation, which may offer promise in preventing relapse, but have yet to be tested in clinical trials. We will briefly examine two which we believe have considerable promise: schlerostin3 and regulatory extracellular vesicles (EVs).4
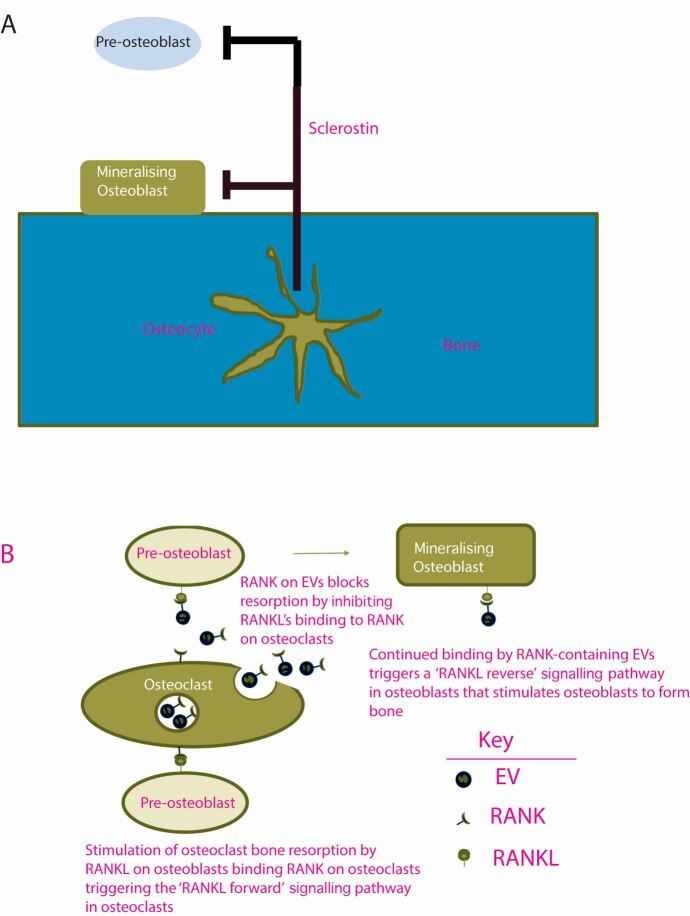
The osteocyte protein sclerostin5,6,7 is vital in bone remodelling and starts a process that inhibits the osteoblastic lineage from forming bone (Fig. 1a). While sclerostin is mostly thought of as a regulatory molecule originating from osteocytes, studies show that sclerostin is also produced by cells of the PDL, particularly on the compression side, presumably to enable resorption.7 Variations in sclerostin levels in the PDL and alveolar housing are associated with tooth movement. Romosozumab, a humanised monoclonal antibody against sclerostin, reduces sclerostin activity (and thus increases bone formation) and is used for the treatment of osteoporosis.8,9 If romosozumab were to be locally directed to the tension side of the tooth, it would be predicted to stimulate bone formation and reduce relapse.
Fig. 1.
New biological approaches to retention. a) Sclerostin is a protein released by osteocytes and cells of the periodontal ligament, which blocks the maturation of pre-osteoblasts into bone-forming osteoblasts. Pre-osteoblasts also express RANKL, which can stimulate osteoclasts to resorb bone. Sclerostin also regulates mineralisation by late osteoblasts. Therefore, blocking sclerostin activity using romosozumab, a humanised monoclonal antibody that inhibits sclerostin, stimulates bone formation. b) Stimulation of RANK on the osteoclast surface by RANKL is essential for osteoclast formation and bone resorption. RANK is also packaged into extracellular vesicles (EVs) and released by osteoclasts. These RANK-EVs can interact with RANKL to competitively inhibit the interaction between RANKL and RANK on the osteoclast surface. In addition, when RANK-EVs interact with RANKL proteins on the pre-osteoblast surface, they stimulate a RANKL reverse signalling pathway that promotes bone formation
The role of EVs as important regulators of bone remodelling has recently been elucidated.4 EVs are tiny (30-150 nm in diameter) vesicles released by cells, including bone cells, and have been identified as crucial and powerful intercellular communicators during the past decade. EV is a term that includes both exosomes (released as multivesicular bodies that fuse with the plasma membrane) and microvesicles (directly from plasma membrane). EVs that contain the protein receptor activator of nuclear factor-kappa B (RANK) are released by osteoclasts and both inhibit bone resorption and stimulate bone formation (Fig. 1b).10,11 Direct application of RANK-containing EVs could enhance bone formation of the tension side. EVs are attractive in that they are natural regulators of bone remodelling.4 In addition, newly described bifunctional therapeutic agents based on RANK-containing EVs released from osteoclasts have been reported. Like RANK-containing EVs, these therapeutic monoclonal antibodies both block bone resorption and stimulate bone formation.11 When (and if) such agents reach clinical use, they would be expected to stimulate tension-side bone formation and to speed the maturation of the post-orthodontic dental alveolar housing.
Caveats
Biological strategies to promote long-term retention of teeth without the use of mechanical retainers warrant further investigation. Agents would ideally increase bone formation on the tension side of the tooth, stabilising the tooth in its new position while still preserving a functional unmineralised PDL, and prevent ankylosis. However, it is also important to recognise that many agents that modify alveolar bone remodelling in the jaw (bisphosphonates are prominent examples) can be associated with an increased risk of medication-related osteonecrosis of the jaw (MRONJ).12 Great care must therefore be taken when using agents that exert biological effects on jaw bone remodelling in an effort to prevent relapse. We hypothesise that agents that subtly modify natural signalling (like antibodies affecting sclerostin and RANK-EV signalling) to enhance retention are less likely to have adverse off-target effects.
No retainers
Based on both research findings13 and through clinical experience, it is apparent that there is a subset of patients who do not comply with retention regimes, yet still have relatively stable outcomes. It would be helpful if we could identify this group of patients who do not appear to need retainers, particularly if they were willing to accept minor changes in their tooth position to avoid wearing retainers.
Reasonable levels of stability in the lower arch have been shown without the use of retainers over a three-year period, provided the lower arch form is maintained and lower incisors are not excessively proclined during active treatment.14 Interestingly, before debond, the authors removed the arch wire for four weeks, but left the brackets in situ to assess tendency for relapse to occur. It was suggested that if there was no relapse in this initial four-week period, significant future relapse was unlikely and appliances could be removed. If relapse occurred in these first four weeks, then excess interdental tooth tissue was removed using interproximal reduction and the teeth realigned with a round wire. Similarly, minimal relapse in the lower arch using interproximal reduction, but without retainers, has been demonstrated in a randomised controlled trial.15 It should be noted that all these patients were treated with extractions and they all initially presented with normal skeletal relationships in all three dimensions.
In a more recent randomised controlled trial, 63 patients that were randomised to either retainers or no retainers were compared, but this time in the maxillary arch.16 At the end of treatment, the patients allocated to 'no retainers' had the wire removed, but the brackets left in situ. They were then monitored firstly after two weeks and then after ten weeks, and if no changes or very minor changes (contact point displacement less than 2 mm) occurred, they were presumed to be relatively stable and the remaining brackets were removed. Only one patient showed a contact displacement greater than 2 mm and, as a result, this patient was judged as unsuitable for no retention; a wire was re-inserted, the teeth realigned and a retainer fitted. All the remaining patients in the 'no retention' group had no retainers fitted at all. One year later, there was slightly more irregularity in the 'no retainer' groups (on average, 1.3 mm irregularity compared to 0.3 mm in the 'retainer' group), which was statistically significant (p <0.001) but was not judged to be clinically significant. Most relapse appeared to happen within the first ten weeks, suggesting that testing the patient with removal of the wire, but maintaining the brackets in place, could be a way of identifying patients who may not need retainers, assuming a minor degree of relapse is acceptable. More research is needed in this area, including long-term effects of no retainers in these patients, and importantly patient satisfaction and acceptance of different levels of relapse, and whether some relapse could be considered more acceptable than the requirement to wear retainers.
Technological developments and retention
New technological developments involving retention are being investigated in the fields of:
Monitoring of retention
Use of different types of retainer materials
Digital workflow to produce retainers.
Monitoring retention
The long-term use of retainers is often recommended to reduce unpredictable and unwanted post-treatment changes.17 However, long-term retainer wear brings the practical challenges of monitoring adherence with removable retainer wear, and checking the integrity and fit of retainers.
Monitoring retention has traditionally entailed visiting a clinician to have retainers reviewed. For removable retainers, this usually involves checking fit, the stability of the dentition and determining the adherence to the prescribed retention regimen. Fixed retainers are checked to determine if they are still in situ and intact, being well maintained and preserving stability. The advent of thermal monitors inserted in removable retainers and the use of artificial intelligence (AI) utilising remote scans has introduced new ways for orthodontists to monitor their patients and their retainers.
Thermal monitors inserted into removable retainers can detect normal intraoral temperature when the appliances are in the mouth and have been used in research to determine how well patients are wearing their retainers.18,19 The technology needs to be further developed to improve their reliability and reduce the size of the devices.20 Furthermore, their data are only accessible when the patient comes for a review appointment. A mobile retainer reminder app was developed to improve adherence to retainers; however, it did not seem to significantly improve objectively assessed adherence levels, stability or patient experiences at three-month follow-up.21 With conventional mobile reminder apps, tracking is dependent on patients entering the usage data themselves and some users perceived this as a 'commitment' and 'time-consuming'.22 To overcome this issue, another pilot study coupling Bluetooth tracking with reminders has shown that this type of compliance tracking has a clinically acceptable level of accuracy and usability, validating its use within future clinical studies.23
AI is the use of computers and software that have the ability to perceive information and reason, and ultimately convert that information into intelligent actions.24 This technology has been harnessed with a product called Dental Monitoring (Paris, France). This software uses intraoral photos taken by patients on smartphones to remotely monitor dentitions. It has most frequently been used to monitor aligner treatment, tracking individual tooth movement, detecting lost attachments and identifying poor oral hygiene. Pre-recorded, customisable instructions are then issued directly to the patients, notifying the supervising orthodontist, but not necessarily needing the clinician's direct input unless desired.25 This can also be used to monitor stability as well as checking dental health issues during the retention phase. Further research will determine if this remote monitoring offers potential advantages for the clinician, with reduced chair time and clinician input, and advantages to patients, helping to reduce the time and financial burden of travelling to the practice, and potentially offering motivation to patients to maintain and adhere to retainer wear.
Use of different retainer materials
Traditionally, retainers have been made with a combination of acrylic and stainless steel wirework (Hawley-type retainers) or clear plastic retainers. Fixed retainers are usually made of stainless steel, constructed in a variety of different thicknesses and configurations to influence flexibility and strength. However, these retainer materials were introduced at a time when it was felt that retainers were only required for a few years to allow the periodontal tissues to adapt to the new tooth position before being discarded. However, as long-term studies of relapse began to show unpredictable but sustained post-treatment change,13 indefinite retention became the norm. However, retainers continued to be manufactured with essentially the same materials. For removable retainers, the acrylic is prone to fracture in the long term and the stainless steel components, such as clasps, can work-harden and fracture. Clear plastic retainers can deteriorate in the mouth as the plastic is porous, leading to discolouration, cracking and wear.
In an attempt to improve the longevity of removable retainers, it has been suggested that cobalt-chrome could be used instead, as it is more resistant to fracture, deformation and scratching, does not absorb moisture and can be cleaned at high temperatures.26 There are challenges to the use of cobalt-chrome, not least the cost and the inherent rigidity, meaning that if settling of the dentition occurs, the fit of the retainer may deteriorate rapidly. However, it demonstrates the ambition to identify alternative and possibly more appropriate materials for long-term removable retainer usage.
One of the risks of using bonded retainers made from stainless steel is that if sufficient force is applied, permanent deformation can occur, which may result in unwanted tooth movement.27 For years, orthodontists have used initial aligning wires made from nickel-titanium to replace the original multi-strand stainless steel wires, not only due to their ability to provide flexibility and their gentle forces, but also to utilise their inherent shape memory. These same attributes may also be useful with a bonded retainer. A nickel-titanium retainer, Memotain (CA Digital, Hilden, Germany), has been described as offering shape memory, flexibility and even the ability to become an 'active' retainer to provide minor tooth alignment if an attachment fails.28 It has a precision fit and, if rebonded to the same place on a tooth that has had a minor relapse, may allow correction of minor irregularities. Further research is needed to test if it is sufficiently fracture-resistant and provides appropriate physiological flexibility.
Digital workflow and retainers
As dentistry moves into an era of digital workflow, retainers are now being produced using a digital approach. The customised nickel-titanium retainer discussed above is digitally planned on a scan of the dentition. It allows positioning of the retainer in the best position on the palatal aspect of the labial segment, which is particularly useful in the upper arch as it ensures that it can be placed clear of occlusal contacts. It is then precision-made using a CAD-CAM process, ensuring close adaptation to the palatal anatomy of the teeth.
For several years, clear plastic retainers have been made on 3D-printed models, produced from intraoral scans, and these have been shown to be as accurate as retainers made on models made from traditional impressions.29 This process still involves thermoforming the clear plastic retainer on a model of the dentition. It has proved more challenging to 3D-print clear plastic retainers directly. Using an additive process of 3D printing, it is possible to directly print a clear plastic retainer, but to date, the properties and accuracy of plastics manufactured using this process have not matched the clear plastic retainers made in the traditional way.30
Changes in patient expectations, personalised medicine and impact of COVID-19 on orthodontic retention
Changes in patient expectations
In another article in this issue, Al-Moghrabi et al.31 discuss how motivation and education at a patient and population level can be used to improve adherence to prescribed retention regimens.32 Lifetime retention requires patient engagement, both in terms of wearing and maintaining retainers as well as attending regular review appointments with related financial costs and time commitments. It is therefore crucial for clinicians to follow scientific, social and technological developments, to be able to serve the needs of new generations and meet contemporary healthcare values.
A Digital Health Consumer Survey carried out in 2019 across different countries including the UK, Australia, USA, Norway, Spain, Finland and Singapore highlighted the rise in patient preference for medical practitioners' use of digital technology, not only for increased communication but also to facilitate remote telemonitoring.33 Future generations may have greater expectations of the use of technology for remote monitoring in orthodontics, as discussed earlier, including during the retention phase of treatment.
Personalised medicine
In recent decades, the concepts of personalised medicine and patient-centred care have become increasingly prominent in individualising healthcare, although these two approaches originate from different background perspectives and values.34 Personalisation stems from a biomedical framework and is an objective view of the patient. It attempts to synthesise patient history, genetic make-up and environmental risk factors to individualise the prevention or treatment of disease.35 So, as our understanding of relapse improves, we may be able to better predict who is likely to experience relapse. This ability to determine a unique relapse potential for each individual may allow us to provide individualised retention regimens to prevent the relapse.
On the other hand, patient-centred care originates from a drive for a more holistic view of patients, taking into account their values, culture and lifestyle.34
This may offer the opportunity to personalise the type of retention according to the patient's lifestyle, values and expectations. Patients can be encouraged to participate in their retention by utilising different monitoring approaches, telehealth and smartphone apps, ensuring full engagement and improved adherence.
Impact of COVID-19
The impact of the COVID-19 pandemic may have a sustained impact on healthcare delivery, including orthodontic retention. Although telemedicine has existed since the late 1950s and early 1960s, it was not used widely until the twenty-first century.36 Lockdowns, increased social distancing and shortages of personal protective equipment (PPE) have accelerated this use of telemedicine in healthcare.
COVID-19 lockdown measures disrupted regular retention check-ups and provision of care to patients with broken or lost retainers. The increased use of digital technology allowed communication and virtual reviews, as well as provision of new retainers manufactured using patients' existing digital scans. As patients and clinicians identify areas of their care that can now be delivered remotely, this will reduce the need for consumables, PPE and patient travel, and will undoubtedly change the way in which we deliver care, including orthodontic retention - not only during a pandemic, but perhaps also in the future.
Conclusions
Traditional approaches to retention have revolved around provision of fixed or removable retainers, with an acceptance that lack of retention will culminate in inevitable post-treatment change. While these tenets continue to apply, our approach to orthodontic retention is evolving due to: advances in biological approaches; developing our understanding of propensity to post-treatment change on an individual basis; and technological developments including those facilitating remote monitoring, as well as material advances. Personalised medicine and patient-centred care may also herald a new dawn in terms of our approach to orthodontic retention in coming decades.
Conflict of interest
The authors do not have any conflicts of interest to declare.
References
- 1.Veginadu P, Tavva S R, Muddada V, Gorantla S. Effect of pharmacological agents on relapse following orthodontic tooth movement: A systematic review of animal studies. Angle Orthod 2020; 90: 598-606. [DOI] [PMC free article] [PubMed]
- 2.Kaklamanos E G, Makrygiannakis M A, Athanasiou A E. Could medications and biologic factors affect post-orthodontic tooth movement changes? A systematic review of animal studies. Orthod Craniofac Res 2021; 24: 39-51. [DOI] [PubMed]
- 3.de Vries T J, Huesa C. The Osteocyte as a Novel Key Player in Understanding Periodontitis through its Expression of RANKL and Sclerostin: a Review. Curr Osteoporos Rep 2019; 17: 116-121. [DOI] [PMC free article] [PubMed]
- 4.Holliday L S, McHugh K P, Zuo J, Aguirre J I, Neubert J K, Rody Jr W J. Exosomes: novel regulators of bone remodelling and potential therapeutic agents for orthodontics. Orthod Craniofac Res 2017; 20 Suppl1: 95-99. [DOI] [PMC free article] [PubMed]
- 5.Samiei M, Janjic K, Cvikl B, Moritz A, Agis H. The role of sclerostin and dickkopf-1 in oral tissues - A review from the perspective of the dental disciplines. F1000Res 2019; 8: 128. [DOI] [PMC free article] [PubMed]
- 6.Yan Y, Wang L, Ge L, Pathak J L. Osteocyte-Mediated Translation of Mechanical Stimuli to Cellular Signalling and Its Role in Bone and Non-bone-Related Clinical Complications. Curr Osteoporos Rep 2020; 18: 67-80. [DOI] [PubMed]
- 7.Odagaki N, Ishihara Y, Wang Z et al. Role of Osteocyte-PDL Crosstalk in Tooth Movement via SOST/Sclerostin. J Dent Res 2018; 97: 1374-1382. [DOI] [PubMed]
- 8.Bandeira L, Lewiecki E M, Bilezikian J P. Romosozumab for the treatment of osteoporosis. Expert Opin Biol Ther 2017; 17: 255-263. [DOI] [PubMed]
- 9.McClung M R. Romosozumab for the treatment of osteoporosis. Osteoporos Sarcopenia 2018; 4: 11-15. [DOI] [PMC free article] [PubMed]
- 10.Huynh N, VonMoss L, Smith D et al. Characterization of regulatory extracellular vesicles from osteoclasts. J Dent Res 2016; 95: 673-679. [DOI] [PMC free article] [PubMed]
- 11.Ikebuchi Y, Aoki S, Honma M et al. Coupling of bone resorption and formation by RANKL reverse signalling. Nature 2018; 561: 195-200. [DOI] [PubMed]
- 12.Pimolbutr K, Porter S, Fedele S. Osteonecrosis of the Jaw Associated with Anti-angiogenics in Antiresorptive-Naive Patient: A Comprehensive Review of the Literature. Biomed Res Int 2018; DOI: 10.1155/2018/8071579. [DOI] [PMC free article] [PubMed]
- 13.Little R M, Wallen T R, Riedel R A. Stability and relapse of mandibular alignment - first four premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod 1981; 80: 349-365. [DOI] [PubMed]
- 14.Aasen T O, Espeland L. An approach to maintain orthodontic alignment of lower incisors without the use of retainers. Eur J Orthod 2005; 27: 209-214. [DOI] [PubMed]
- 15.Edman Tynelius G, Bondemark L, Lilja-Karlander E. A randomized controlled trial of three orthodontic retention methods in Class I four premolar extraction cases - stability after 2 years in retention. Orthod Craniofac Res 2013; 16: 105-115. [DOI] [PubMed]
- 16.Naraghi S, Ganzer N, Bondemark L, Sonesson M. Comparison of post-treatment changes with and without retention in adolescents treated for maxillary impacted canines - a randomized controlled trial. Eur J Orthod 2020; DOI: 10.1093/ejo/cjaa010. [DOI] [PMC free article] [PubMed]
- 17.Littlewood S J, Kandasamy S, Huang G. Retention and relapse in clinical practice. Aust Dent J 2017; 62 Suppl 1: 51-57. [DOI] [PubMed]
- 18.Schott TC, Göz G. Applicative characteristics of New microelectronic sensors smart retainer® and TheraMon® for measuring wear time. J Orofac Orthop 2010; 71: 339-347. [DOI] [PubMed]
- 19.Schott T C, Schlipf C, Glasl B, Schwarzer C L, Weber J, Ludwig B. Quantification of patient compliance with Hawley retainers and removable functional appliances during the retention phase. Am J Orthod Dentofacial Orthop 2013; 144: 533-540. [DOI] [PubMed]
- 20.Brierley C A, Benson P E, Sandler P J. How Accurate Are TheraMon® Microsensors at Measuring Intraoral Wear-Time? Recorded vs. Actual Wear Times in Five Volunteers. J Orthod 2017; 44: 241-224. [DOI] [PubMed]
- 21.Al-Moghrabi D, Pandis N, McLaughlin K, Johal A, Donos N, Fleming P S. Evaluation of the effectiveness of a tailored mobile application in increasing the duration of wear of thermoplastic retainers: a randomized controlled trial. Eur J Orthod 2020; DOI: 10.1093/ejo/cjz088. [DOI] [PubMed]
- 22.Al-Moghrabi D, Colonio-Salazara F B, Johal A, Fleming P S. Development of 'My Retainers' mobile application: Triangulation of two qualitative methods. J Dent 2020; 94: 103281. [DOI] [PubMed]
- 23.Castle E, Chung P, Behfar M H et al. Compliance monitoring via a Bluetooth-enabled retainer: A prospective clinical pilot study. Orthod Craniofac Res 2019; 22 Suppl 1: 149-153. [DOI] [PubMed]
- 24.Asiri S N, Tadlock L P, Schneiderman E, Buschang P H. Applications of artificial intelligence and machine learning in orthodontics. APOS Trends Orthod 2020; 10: 17-24.
- 25.Hansa, I, Semaan, S J, Vaid N R. Clinical outcomes and patient perspectives of Dental Monitoring® GoLive® with Invisalign® - a retrospective cohort study. Prog Orthod 2020; 21: 16. [DOI] [PMC free article] [PubMed]
- 26.Ash S, Singh P, Mizrahi E. Removable cast chrome cobalt retainers for extended or indefinite period clinical use. J Orthod 2015; 42: 248-252. [DOI] [PubMed]
- 27.Kučera J, Marek I. Unexpected complications associated with mandibular fixed retainers: A retrospective study. Am J Orthod Dentofacial Orthop 2016; 149: 202-211. [DOI] [PubMed]
- 28.Kravitz N D, Grauer D, Schumacher P, Jo Y-M. Memotain: A CAD/CAM nickel-titanium lingual retainer. Am J Orthod Dentofacial Orthop 2017; 151: 812-815. [DOI] [PubMed]
- 29.Tahir N M, Hassan W N W, Saub R. Comparing retainers constructed on conventional stone models and on 3D printed models: a randomized crossover clinical study. Eur J Orthod 2019; 41: 370-380. [DOI] [PubMed]
- 30.Nasef A A, El-Beialy A R, Mostafa Y A. Virtual techniques for designing and fabricating a retainer. Am J Orthod Dentofacial Orthop 2014; 146: 394-398. [DOI] [PubMed]
- 31.Al-Moghrabi D, Barber S, Fleming P. Removable retention: enhancing adherence and the remit of shared decision-making. Br Dent J 2021; 230: 765-769. [DOI] [PubMed]
- 32.Bharmal R V, Parker K, Caldwell S et al. A multicentre audit to assess the effectiveness of the British Orthodontic Society 'Hold that Smile' retainer videos. J Orthod 2020, 47: 72-77. [DOI] [PubMed]
- 33.Accenture. Accenture Digital Health Survey. 2019. Available at https://www.accenture.com/_acnmedia/PDF-94/Accenture-2019-Digital-Health-Consumer-Survey.pdf (accessed July 2020).
- 34.El-Alti L, Sandman L, Munthe C. Person Centred Care and Personalized Medicine: Irreconcilable Opposites or Potential Companions? Health Care Anal 2019; 27: 45-59. [DOI] [PubMed]
- 35.Hood L. A systems approach to medicine will transform health care. InPhysical Biology: From Atoms to Medicine. pp 337-366. London: Imperial College Press, 2008.
- 36.Maese J R, Seminara D, Shah Z, Szerszen A. What a Difference a Disaster Makes: The Telehealth Revolution in the Age of COVID-19 Pandemic. Am J Med Qual 2020 35: 429-431. [DOI] [PMC free article] [PubMed]