Abstract
Background:
To date, there have been few studies on the outcomes of anterior cruciate ligament reconstruction (ACLR) using quadriceps tendon–patellar bone (QTPB) autograft.
Purpose:
To evaluate the long-term clinical outcomes of ACLR using QTPB autograft.
Study Design:
Case series; Level of evidence, 4.
Methods:
We retrospectively reviewed 139 patients who underwent primary ACLR with QTPB autografts and had at least 7 years of postoperative follow-up data. Instability, clinical scores, donor-site morbidity, radiographic progression of osteoarthritis, and any associated complications were assessed.
Results:
The proportion of knees classified as grade >1 on the anterior drawer, Lachman, and pivot-shift tests decreased significantly postsurgically (from 47.4% to 5.0%, 48.9% to 4.3%, and 53.3% to 5.0%, respectively; P < .001 for all). The mean clinical scores at the final follow-up were 89.8, 81.0, and 4.4 for the Lysholm, International Knee Documentation Committee, and Tegner Activity Scale, respectively. The results of the Cybex II dynamometer isokinetic test showed decreases in flexion and extension strength at both 60° and 180° per second, which persisted until the final follow-up visit. About one-fifth (19.4%) of the patients had osteoarthritis (Kellgren-Lawrence grade ≥1) before surgery, which increased to 33.8% at the final follow-up. The overall complication rate was 23.2%, and about one-third of the patients who experienced complications underwent revision surgery as a result of graft rupture and residual instability.
Conclusion:
In the current study, ACLR using QTPB autograft provided satisfactory long-term clinical results, with acceptable rates of complication and donor-site morbidity.
Keywords: anterior cruciate ligament, anterior cruciate ligament reconstruction, quadriceps tendon—patellar bone, quadriceps tendon--patellar bone autograft
Anterior cruciate ligament (ACL) ruptures are among the most common orthopaedic injuries, especially in young active patients, with approximately 30 to 40 reconstructions performed per 100,000 people. 10 The incidence of ACL reconstruction (ACLR) is increasing as more people participate in sports while at the same time surgical techniques advance. 11
Over the decades, many types of ACLR grafts have been studied, and the debate continues regarding optimal graft choice. The two most common and well-studied autografts used for ACLR are the bone–patellar tendon–bone (BPTB) graft and hamstring graft. 15 Recently, quadriceps tendon (QT) and quadriceps tendon–patellar bone (QTPB) grafts have emerged as alternative graft choices with comparable function and complication rates. 5,6,8 Despite growing evidence supporting QT and QTPB as excellent graft options in ACLR, in comparision with BPTB or hamstring grafts, they are seldom used, 15 and there have been few studies on the outcomes of ACLR using QT or QTPB autografts. 3
This study was performed to evaluate the long-term clinical results of ACLRs that used QTPB autografts. We postulated that the use of QTPB autografts in ACLR would result in equivalent long-term clinical outcomes to other well-studied graft choices (hamstring and BPTB).
Methods
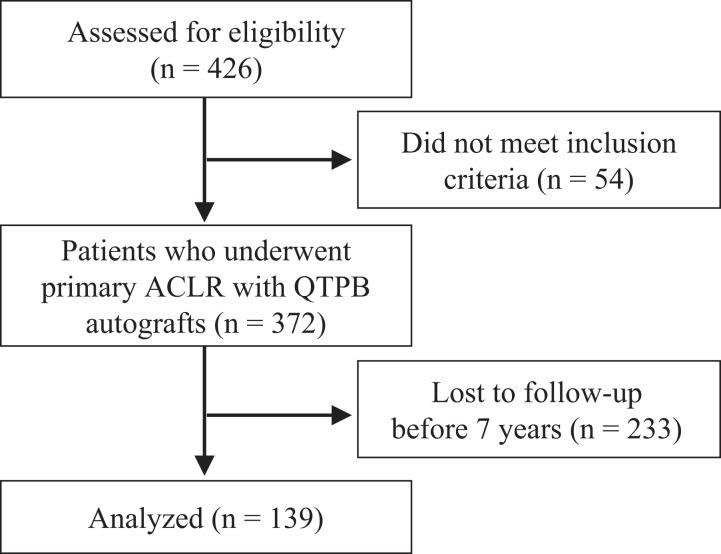
We received institutional review board approval for this retrospective study. From February 1999 to December 2012, 426 patients who underwent primary ACLR with QTPB autografts were screened. Patients who were followed up with for >7 years after ACLR were selected, and the exclusion criteria included previous knee surgery; previous ligamentous injury including chronic ACL tears; and concomitant meniscal or ligamentous injury of the affected knee (other than grade I or II medial collateral ligament injury). Ultimately, 139 patients were included in this study (Figure 1).
Figure 1.
Flowchart of patients screened and grouped. ACLR, anterior cruciate ligament reconstruction; QTPB, quadriceps tendon–patellar bone.
Surgical Technique
Both the harvesting and preparation of QTPB autografts were performed as described previously. 7 A tibial tunnel 10 mm in diameter was drilled, and the intra-articular opening of the tunnel was aligned to the center of the ACL attachment. A 7-mm offset guide was inserted through the tibial tunnel for femoral tunnel placement. Midway through the study (April 2006), modifications to the conventional transtibial (TT) technique were implemented to achieve a more oblique, anatomic trajectory of the femoral tunnel. These modifications included sequential application of the anterior drawer, varus, and external rotation forces to the proximal tibia as well as external rotation of the previously inserted femoral guide. Finally, the drill guide was aimed at the lateral bifurcate ridge on the medial wall of the lateral femoral condyle. In total, 94 ACLRs performed using the TT technique in addition to 45 performed using the modified TT technique, were included in the study.
Rehabilitation Protocol
The postoperative rehabilitation protocol was uniform over the entire study period. Continuous passive motion was started with an assistive device within 2 days of surgery and continued for 1 to 2 days during the hospitalization period. A motion-control brace set at 0° to 90° was applied for 4 weeks. Full flexion was obtained within an additional 2 weeks. Patients were limited to partial weightbearing for 4 to 6 weeks and then progressed to full weightbearing as tolerated. Full sports activities such as jumping, running, and pivoting were allowed 6 months after surgery, once recovery of quadriceps muscle strength had been confirmed by physical examination in the clinic.
Clinical Evaluation
Clinical assessments were performed preoperatively, at 3 months and 1 year postoperatively, and annually thereafter. Clinical variables included instability, clinical scores, donor-site morbidity, radiographic progression of osteoarthritis, and any associated complications. Instability was evaluated via physical examinations (anterior drawer test, Lachman test, and pivot-shift test) and the KT-2000 arthrometer (MEDmetric). Physical examinations were performed in the outpatient clinic by an independent observer. The Lysholm, International Knee Documentation Committee (IKDC), and Tegner Activity Scale scores were obtained. Donor-site morbidity was determined via measurement of quadriceps strength using the Cybex II isokinetic dynamometer (CYBEX) at 60° and 180° per second and Shelbourne and Trumper anterior knee pain questionnaire. 17 The Cybex II results were recorded as percentages relative to the contralateral (normal) side. Furthermore, as a measure of osteoarthritis progression, the Kellgren-Lawrence (K-L) grade at the final follow-up visit was obtained and confirmed by 2 experienced orthopaedic surgeons (S.J. and D.H.R.). Any complications, such as rerupture, residual instability, or cyclops lesion, were recorded in the electronic medical charts.
Statistical Analysis
Continuous variables are presented as means and standard deviations, and categorical variables are presented as frequencies and percentages. The demographics and preoperative clinical variables of the included patients were compared with those who were excluded from the study due to loss of follow-up (control group; n = 233). Continuous and categorical variables were compared using the independent t test and Fisher exact test, respectively. All statistical analyses were performed using SPSS Version 25.0.0 (SPSS). P < .05 indicated statistical significance.
Results
The demographics of the patients included in the study are shown in Table 1. The mean age on the day of surgery was 30.0 years, and the mean follow-up period was 10.2 years (range, 7-19 years). There was a clear male predominance, and the affected side was relatively evenly distributed (right side, 54.0%). The demographics and preoperative clinical scores (Tegner and Lysholm scores) were not significantly different between the study patients and the control group (excluded patients) except for the length of follow-up.
Table 1.
Demographic Data of the Patients a
| Study Patients | Controls | P Value | |
|---|---|---|---|
| No. of knees | 139 | 233 | |
| Age, y | 30.0 ± 6.5 | 31.0 ± 9.6 | .685 |
| Sex, male/female | 119/20 | 248/25 | .108 |
| Side, right/left | 75/64 | 143/130 | .762 |
| BMI, kg/cm2 | 25.1 ± 4.1 | 25.7 ± 3.4 | .782 |
| Follow-up length, y | 10.2 ± 2.6 | 2.2 ± 1.9 | <.001 |
| Preoperative Tegner scale | 3.0 ± 1.8 | 3.5 ± 1.8 | .251 |
| Preoperative Lysholm score | 71.1 ± 12.6 | 68.2 ± 15.5 | .493 |
a Data are reported as n or mean ± SD. Value in bold indicates statistically significant differences between groups (P < .05). BMI, body mass index.
Significant improvements in knee stability were observed postsurgically, as determined by physical examination and arthrometry (Table 2). The proportion of knees classified as grade >1 on the anterior drawer, Lachman, and pivot-shift tests decreased significantly after surgery (from 47.4% to 5.0%, 48.9% to 4.3%, and 53.3% to 5.0%, respectively; all P < .001). In the KT-2000 arthrometer, the overall side-to-side difference was <3 mm in 71.9% of the patients at the final follow-up.
Table 2.
Evaluation of Knee Instability Before Surgery and at the Final Visit a
| Preoperative | Final Visit | P Value | |
|---|---|---|---|
| Anterior drawer test | <.001 | ||
| Grade 0 | 14 (10.1) | 86 (61.9) | |
| Grade 1 | 59 (42.4) | 46 (33.1) | |
| Grade 2 | 54 (38.8) | 7 (5.0) | |
| Grade 3 | 12 (8.6) | 0 (0.0) | |
| Lachman test | <.001 | ||
| Grade 0 | 12 (8.6) | 84 (60.4) | |
| Grade 1 | 59 (42.4) | 49 (35.3) | |
| Grade 2 | 54 (38.8) | 6 (4.3) | |
| Grade 3 | 14 (10.1) | 0 (0.0) | |
| Pivot-shift test | <.001 | ||
| Grade 0 | 11 (7.9) | 80 (57.6) | |
| Grade 1 | 54 (38.8) | 52 (37.4) | |
| Grade 2 | 61 (43.9) | 7 (5.0) | |
| Grade 3 | 13 (9.4) | 0 (0.0) | |
| KT-2000 | 4.4 ± 2.0 | 2.1 ± 1.1 | <.001 |
| <3 mm | 22 (15.8) | 100 (71.9) | |
| 3-5 mm | 84 (60.4) | 39 (28.1) | |
| >5 mm | 32 (23.0) | 0 (0.0) |
a Data are reported as n (%) or mean ± SD. Values in bold indicate statistically significant differences (P < .05).
The Cybex II dynamometer results showed decreases in flexion and extension strength at both 60° and 180° per second, which persisted until the final follow-up visit (Figure 2). Flexion strength was better preserved than extension strength throughout the follow-up period. The proportions of patients who complained of moderate to severe anterior knee pain in association with strenuous work/exercise, stair climbing, prolonged sitting, kneeling, and activities of daily living were 14.4%, 4.3%, 8.6%, 10.1%, and 5%, respectively. Donor-site tenderness was noted in 2.9% of the patients.
Figure 2.
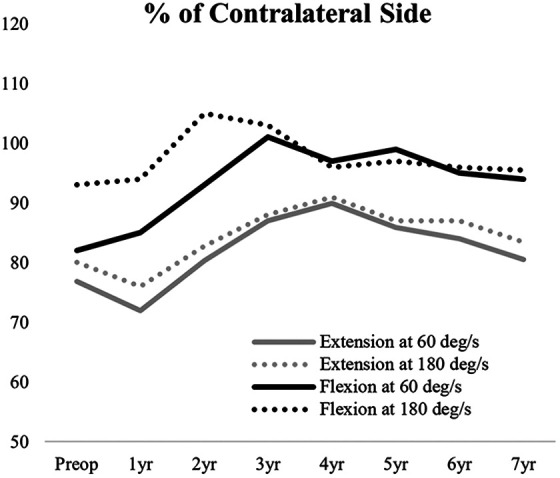
The mean side-to-side ratio of peak torque values according to Cybex II dynamometer isokinetic testing performed at 60° and 180° per second.
Clinical scores improved markedly after ACLR (Table 3). Although the clinical scores decreased slightly over time, 77.3% of the patients had a good to excellent Lysholm score at their final visit.
Table 3.
Clinical Scores of the Study Patients at Each Time Point a
| Time Point | Score |
|---|---|
| Lysholm | |
| Preoperative | 71.2 ± 8.6 |
| 2 years postoperative | 89.8 ± 7.8 |
| 5 years postoperative | 90.2 ± 8.4 |
| Final visit | 89.8 ± 8.3 |
| Subjective IKDC | |
| Preoperative | 56.8 ± 8.1 |
| 2 years postoperative | 90.9 ± 7.7 |
| 5 years postoperative | 84.8 ± 7.6 |
| Final visit | 81.0 ± 8.4 |
| Tegner activity scale | |
| Preoperative | 3.0 ± 1.4 |
| 2 years postoperative | 4.8 ± 1.3 |
| 5 years postoperative | 4.8 ± 1.2 |
| Final visit | 4.4 ± 1.3 |
a Data are reported as mean ± SD. IKDC, International Knee Documentation Committee.
Complications are detailed in Table 4. Patients who were lost to follow-up before 7 years but had definite complications during the follow-up were included in the analysis (n = 16). The overall complication rate was 20.0%, and about one-third of the patients who experienced complications underwent revision surgery due to rerupture and residual instability. About one-fifth (19.4%) of the patients had osteoarthritis (K-L grade ≥1) before surgery, which increased to 33.8% at the final follow-up.
Table 4.
Complications After ACLRs Using Quadriceps Tendon-Patellar Bone Graft a
| Complication Type | Complications | Treatment |
|---|---|---|
| Rerupture | 9 (5.8) | Revision ACLR |
| Residual instability | 2 (1.3) | Revision ACLR |
| Surgical site infection | 2 (1.3) | Arthroscopic synovectomy and debridement |
| Patellar fracture | 6 (3.9) | ORIF |
| Cyclops lesion | 4 (2.6) | Arthroscopic excision |
| Arthrofibrosis | 2 (1.3) | MUA |
| Transient LOM | 6 (3.9) | Physical therapy |
| Total | 31 (20.0) |
a Data are reported as n (%). ACLR, anterior cruciate ligament reconstruction; LOM, limitation of motion; MUA, manipulation under anesthesia; ORIF, open reduction and internal fixation.
Discussion
To our knowledge, to date, this is the largest study reporting the long-term clinical outcomes of ACLR using QT/QTPB autografts. The most important findings were that the QTPB autograft showed fair long-term clinical results. More than 90% of the patients had grade ≤1 knees based on all of the physical examinations (anterior drawer, Lachman, and pivot-shift tests) after ACLR. Moreover, the patients showed satisfactory recovery of quadriceps strength, minimum donor-site morbidity, and good clinical scores.
Barié et al 3 recently reported the long-term follow-up (mean, 7.5 years) results of ACLR using QTPB autografts in 57 patients. The results of the present study showed both similarities and differences to those of Barié et al. The proportions of patients with normal results on physical examination (grade 0) in the Lachman and pivot-shift tests after surgery were 68% and 64.8%, respectively, in the present study, which was quite different from the results of Barié et al (88% and 79%, respectively). The subjective nature of physical examinations (where our evaluation may have been stricter) could explain the discrepancy. In our study, the mean Lysholm and IKDC scores were 89.7 and 90.9, respectively, similar to the scores reported by Barié et al (92 and 90, respectively). The rate of osteoarthritis progression was markedly greater in the present study than in that of Barié et al (24.5% and 3.7%, respectively), but this difference may have been due to the longer mean follow-up period in our study (10.2 years). Complications were very different between the studies: Cyclops lesion was rarer in the present study than the previous study (2.6% and 12%, respectively), although the rerupture rate was higher in our study (5.8% and 0%, respectively). Postoperative infection rates were similar between the 2 studies (1.3% and 1.5%, respectively). Donor-site morbidity of the quadriceps muscle could not be compared, as we used the Cybex II dynamometer isokinetic test and the Shelbourne and Trumper anterior knee pain questionnaire, 17 while Barié et al used thigh circumference and the single-leg triple-hop test.
The long-term outcomes of the present study were also comparable with those of studies of primary ACLRs using other types of autografts (hamstring or BPTB). Leiter et al 9 used hamstring autografts in 68 patients with a mean follow-up of 14.6 years. The mean Lysholm score was 76.7, and 54.5% of the patients showed good to excellent results. The shorter follow-up period (mean, 10.2 years) in the present study may have accounted for the higher mean Lysholm score and percentage of good to excellent results compared with this previous study (89.8 and 77.3%, respectively). The proportion of patients with K-L grade ≥3 knees at the final evaluation in the previous study was 19%, which was much higher than in the present study (2.1%). However, the lower mean age of the patients in the present study (40.2 and 45.8 years, respectively) and lack of preoperative K-L grade in the previous study preclude direct comparison. Systematic reviews comparing QT/QTPB autografts with other types of autografts suggested that the former type provide comparable clinical and functional outcomes, but with reduced donor-site pain. 2,13,14,18 Other comparative studies also advocated the use of QT/QTPB autografts due to the lower rates of sensory loss, 12 stronger extensor mechanism, 1 and superior biomechanical characteristics. 16 Fu et al 4 reported 5 cases of patella fracture (among 57 patients) after harvesting QTPB autografts proposing a problem specific to the graft; similarly, 6 cases of patella fracture (4 intraoperatively and 2 postoperatively) occurred in the present study.
This study had some limitations. First, retrospectively collected data were analyzed, and no comparison with other graft types was performed. Second, despite similar demographics between the included and excluded patients, there was a possibility of selection bias, as only 139 patients were selected among a total of 372 patients due to the requirement of a long follow-up period. Nevertheless, to the authors’ knowledge, this is the largest study on the clinical results of ACLRs using QTPB autografts reported to date; it also has the longest follow-up period.
Conclusion
ACLR using QTPB autograft provides satisfactory long-term clinical results, with acceptable rates of complication and donor-site morbidity.
Footnotes
Final revision submitted December 6, 2020; accepted January 12, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Seoul National University Hospital (No. H-2006-023-113).
References
- 1. Adams DJ, Mazzocca AD, Fulkerson JP. Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Arthroscopy. 2006;22(1):76–79. [DOI] [PubMed] [Google Scholar]
- 2. Ajrawat P, Dwyer T, Whelan D, et al. A comparison of quadriceps tendon autograft with bone-patellar tendon-bone autograft and hamstring tendon autograft for primary anterior cruciate ligament reconstruction: a systematic review and quantitative synthesis. Published online June 19, 2019. Clin J Sport Med. doi:10.1097/JSM.0000000000000765 [DOI] [PubMed] [Google Scholar]
- 3. Barie A, Kopf M, Jaber A, et al. Long-term follow-up after anterior cruciate ligament reconstruction using a press-fit quadriceps tendon-patellar bone autograft. BMC Musculoskelet Disord. 2018;19(1):368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fu FH, Rabuck SJ, West RV, Tashman S, Irrgang JJ. Patellar fractures after the harvest of a quadriceps tendon autograft with a bone block: a case series. Orthop J Sports Med. 2019;7(3):2325967119829051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Han HS, Seong SC, Lee S, Lee MC. Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Clin Orthop Relat Res. 2008;466(1):198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kwak YH, Lee S, Lee MC, Han HS. Anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone allograft: matched case control study. BMC Musculoskelet Disord. 2018;19(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee JK, Lee S, Seong SC, Lee MC. Modified transtibial technique for anterior cruciate ligament reconstruction with quadriceps tendon autograft. JBJS Essent Surg Tech. 2014;4(3):e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee S, Seong SC, Jo CH, et al. Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. J Bone Joint Surg Am. 2007;89)(suppl 3):116–126. [DOI] [PubMed] [Google Scholar]
- 9. Leiter JR, Gourlay R, McRae S, de Korompay N, MacDonald PB. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1061–1069. [DOI] [PubMed] [Google Scholar]
- 10. Lyman S, Koulouvaris P, Sherman S, et al. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. [DOI] [PubMed] [Google Scholar]
- 11. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 12. Mouarbes D, Dagneaux L, Olivier M, et al. Lower donor-site morbidity using QT autografts for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2558–2566. [DOI] [PubMed] [Google Scholar]
- 13. Mouarbes D, Menetrey J, Marot V, et al. Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone–patellar tendon–bone and hamstring-tendon autografts. Am J Sports Med. 2019;47(14):3531–3540. [DOI] [PubMed] [Google Scholar]
- 14. Riaz O, Aqil A, Mannan A, et al. Quadriceps tendon-bone or patellar tendon-bone autografts when reconstructing the anterior cruciate ligament: a meta-analysis. Clin J Sport Med. 2018;28(3):316–324. [DOI] [PubMed] [Google Scholar]
- 15. Shaerf DA, Pastides PS, Sarraf KM, Willis-Owen CA. Anterior cruciate ligament reconstruction best practice: a review of graft choice. World J Orthop. 2014;5(1):23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sheean AJ, Musahl V, Slone HS, et al. Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: use it now, use it often. Br J Sports Med. 2018;52(11):698–701. [DOI] [PubMed] [Google Scholar]
- 17. Shelbourne KD, Trumper RV. Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(1):41–47. [DOI] [PubMed] [Google Scholar]
- 18. Slone HS, Romine SE, Premkumar A, Xerogeanes JW. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31(3):541–554. [DOI] [PubMed] [Google Scholar]