Abstract
Sarcomatoid carcinoma (SC) of the lung is a rare histological subtype of nonsmall cell lung cancer and comprises a diagnostically and therapeutically challenging group of tumors. We report a patient of SC of the lung in an elderly patient who presented with a lung mass. Computed tomography-guided biopsy of the lung mass was done, which clinched the diagnosis. We present this case because of the rarity of this histological subtype and to expand understanding regarding this rare cancer.
KEY WORDS: Carcinoma, lung, sarcoma
INTRODUCTION
Pulmonary sarcomatoid carcinoma (PSC) is defined as poorly differentiated nonsmall cell lung carcinoma (NSCLC) that contains a component of sarcoma or sarcoma-like elements (at least 10% spindle and/or giant cells) or a carcinoma consisting only of spindle and giant cells.[1] Sarcomatoid carcinomas (SCs) of the lung pose a significant challenge due to their rare occurrence, heterogeneous histology, and unclear histogenesis. Since pathological sub-classifications are also important for treatment decisions in lung cancer, clinicians and pathologists should be aware of the rarer tumors.
CASE REPORT
A 75-year-old male,a retired teacher and ex-smoker and a known case of chronic obstructive pulmonary disease for the past 20 years, presented with chief complaints of progressively increasing nonproductive cough and dyspnea for 8 months, loss of weight for 4 months, chest pain for 2 months, and hemoptysis for 1 month. On systemic examination, the patient was hemodynamically stable, had pallor and respiratory failure with a SpO2 of 91% on room air. On local examination, breath sounds were diminished in the left infrascapular, mammary, and infraaxillary fields and rhonchi were present.
Chest X-ray posteroanterior [Figure 1] revealed emphysematous lung fields with flattening of the diaphragm and a homogeneous, irregular margined opacity in the left upper and middle zones suggestive of the mass lesion. Due to the derangement in kidney function test a noncontrast, high resolution computed tomography of the thorax [Figure 2] was done and showed irregular margined, pleura based mass in the anterior segment of the right upper lobe, lingular lobe, and superior segment of the left lower lobe with osteolytic destruction of involved rib and invasion of the chest wall and extensive emphysema.
Figure 1.
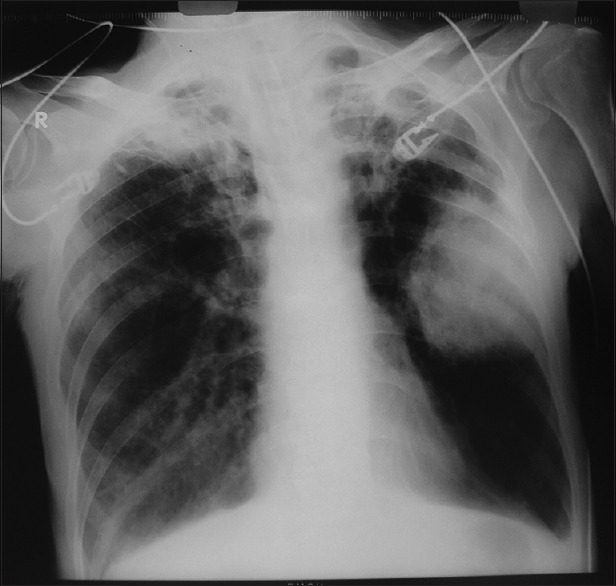
Chest X-ray showing left lung mass
Figure 2.
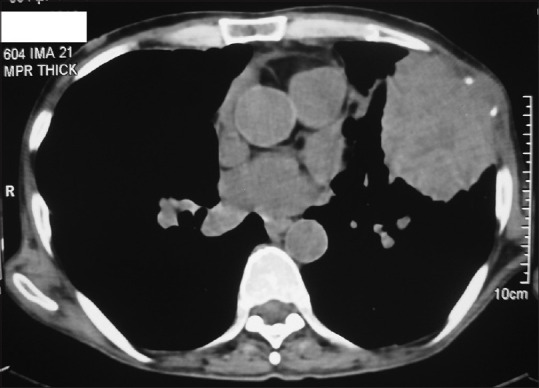
CT thorax showing pleura based mass with rib destruction
A computed tomography guided biopsy of the lung mass was done, and histopathology [Figure 3] was reported as a biphasic appearance composed of carcinomatous areas with areas composed of malignant spindle cells. The carcinomatous area was composed of sheets of polygonal cells with eosinophilic cytoplasm, large vesicular pleomorphic-appearing nuclei, and prominent nucleoli. The malignant spindle cell component consisted of spindle cells arranged in sheets and fascicles with vesicular nuclei and prominent nucleoli. Foci of necrosis, frequent mitotic figures, and inflammatory cell infiltrate were also present. The epithelial component showed Thyroid transcription factor 1 (TTF-1) immunopositivity.and the sarcomatous areas were positive for cytokeratin and vimentin. Immunohistochemistry was negative for epidermal growth factor receptor. A diagnosis of SC was made, and the patient was referred to the Department of Medical Oncology.
Figure 3.
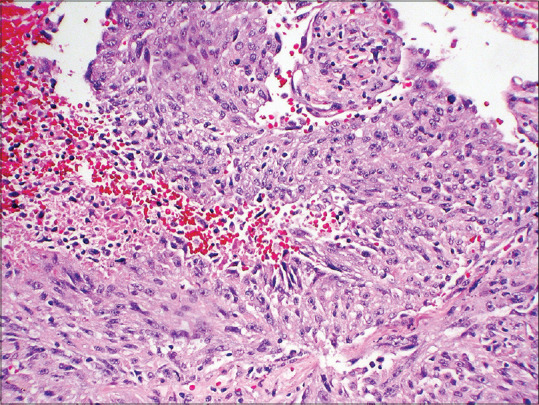
Histopathology of the biopsy showed the biphasic appearance
DISCUSSION
SC, is a relatively uncommon form of cancer whose malignant cells have histological, cytological, or molecular properties of both epithelial tumors (carcinoma) and mesenchymal tumors (sarcoma).[2] SC can occur in different organs such as the thyroid gland, bone, skin, breast, pancreas, liver, urinary tract, and lung.[3] However, SC in the lung is very rare, accounting for 0.1%–0.4% of all lung malignancies.[4]
PSC comprises a distinct clinicopathologic entity on the basis of morphologic, behavioral, and genotypic/phenotypic attributes.[5] The 2015 World Health Organization (WHO) classification of tumors of the lung, pleura, thymus, and heart divides PSC into five histological variants – pleomorphic carcinoma (>50%), spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and pulmonary blastoma.[6]
PSC is a poorly differentiated, aggressive tumor that affects smokers and males predominantly.[7] The average age of individuals at the diagnosis is 65 years, except for the pulmonary blastoma subtype, for which the average age at the diagnosis is 35 years. Multiple risk factors have been associated with SC of the lung, such as smoking cigarettes, cigars, or pipes, and exposure to asbestos in building construction and electrical insulation.[8]
SCs are unique among lung carcinomas in that, although they are considered carcinomas, they contain cytological and tissue architectural features that are usually characteristic of sarcoma. The 1981 WHO histological typing of lung tumors categorized SCs that corresponded to spindle cell, as a variant of squamous cell carcinoma.[9] The 1999 WHO histological typing of lung and pleural tumors, classified carcinomas with spindle and/or giant cells under the heading of “carcinomas with pleomorphic, sarcomatoid, or sarcomatoid elements.”[10] The 2004 WHO classification of lung tumors defined PSCs as “poorly differentiated nonsmall cell carcinoma that have a histological appearance suggesting mesenchymal differentiation.”[11] The 2015 WHO classification of lung tumors had no changes to diagnostic criteria/terminology for these tumors since the 2004 classification, but recommends molecular testing with histological findings.[6]
The location of SC may be central or peripheral. There is no specific clinical presentation, and patients may present with cough, dyspnea, hemoptysis, chest pain, or weight loss.[12] It is characterized by rapid growth, invasion, disease recurrence, and metastases.[5] SC had a median survival of 10 months.[13]
Most of these PSC can be diagnosed by light microscopy alone, although in certain situations, immunohistochemistry can be helpful.[14] The carcinoma components are usually squamous but may be glandular or neuroendocrine. The heterologous sarcomatoid component may comprise rhabdomyosarcoma, osteosarcoma, and chondrosarcoma.
Immunohistochemical analysis must show cytokeratin positivity. Vimentin, carcinoembryonic antigen, and smooth-muscle markers are also positive. Epithelial marker positivity is not essential if histopathological features of cancer are present. Till date, no prospective studies of SC have been done, due to the low incidence, complicated diagnostics needed, and tumor aggressiveness. Retrospective studies that compared PSC to conventional NSCLC reported worse median survival, overall survival, and more disease progression.[15]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Baldovini C, Rossi G, Ciarrocchi A. Approaches to tumor classification in pulmonary sarcomatoid carcinoma. Lung Cancer (Auckl) 2019;10:131–49. doi: 10.2147/LCTT.S186779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ram R, Saadat P, Peng D, Vadmal M. Case report and literature review: Primary cutaneous carcinosarcoma. Ann Clin Lab Sci. 2005;35:189–94. [PubMed] [Google Scholar]
- 3.Arshad HS, Dudekula RA, Niazi M, Malik S, Khaja M. A rare case of sarcomatoid carcinoma of the lung with spine metastasis, including a literature review. Am J Case Rep. 2017;18:760–5. doi: 10.12659/AJCR.904584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karim NA, Schuster J, Eldessouki I, Gaber O, Namad T, Wang J, et al. Pulmonary sarcomatoid carcinoma: University of Cincinnati Experience. Oncotarget. 2017;9:4102–8. doi: 10.18632/oncotarget.23468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pelosi G, Sonzogni A, De Pas T, Galetta D, Veronesi G, Spaggiari L, et al. Review article: Pulmonary sarcomatoid carcinomas: A practical overview. Int J Surg Pathol. 2010;18:103–20. doi: 10.1177/1066896908330049. [DOI] [PubMed] [Google Scholar]
- 6.Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, Beasley MB, et al. The 2015 World Health Organization Classification of lung tumors: Impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10:1243–60. doi: 10.1097/JTO.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 7.Smadhi H, Boudaya MS, Abdannadher M, BenAbdelghaffar H, Kamoun H, Ayadi A, et al. Pulmonary sarcomatoid carcinoma: A surgical diagnosis and prognostic factors. Tunis Med. 2019;97:128–32. [PubMed] [Google Scholar]
- 8.Ishida T, Tateishi M, Kaneko S, Yano T, Mitsudomi T, Sugimachi K, et al. Carcinosarcoma and spindle cell carcinoma of the lung. Clinicopathologic and immunohistochemical studies. J Thorac Cardiovasc Surg. 1990;100:844–52. [PubMed] [Google Scholar]
- 9.The World Health Organization histological typing of lung tumours. Am J Clin Pathol. (Second edition) 1982;77:123–36. doi: 10.1093/ajcp/77.2.123. [DOI] [PubMed] [Google Scholar]
- 10.Travis WD, Colby TV, Corrin B, Shimosato Y, Brambilla E Collaboration with Sobin LH and pathologists from 14 countries. Histological Typing of Lung and Pleural Tumours. 3rd ed. New York: Springer-Verlag; 1999. World Health Organization International Histological Classification of Tumours. [Google Scholar]
- 11.Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol. 2005;40:90–7. doi: 10.1053/j.ro.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Yoshino N, Kubokura H, Yamauchi S, Ohaki Y, Koizumi K, Shimizu K. A true pulmonary carcinosarcoma that required diagnostic differentiation from a pleomorphic adenoma: A case report. Ann Thorac Cardiovasc Surg. 2009;15:42–5. [PubMed] [Google Scholar]
- 13.Ro JY, Chen JL, Lee JS, Sahin AA, Ordóñez NG, Ayala AG. Sarcomatoid carcinoma of the lung. Immunohistochemical and ultrastructural studies of 14 cases. Cancer. 1992;69:376–86. doi: 10.1002/1097-0142(19920115)69:2<376::aid-cncr2820690218>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 14.Travis WD. Sarcomatoid neoplasms of the lung and pleura. Arch Pathol Lab Med. 2010;134:1645–58. doi: 10.5858/2010-0086-RAR.1. [DOI] [PubMed] [Google Scholar]
- 15.Martin LW, Correa AM, Ordonez NG, Roth JA, Swisher SG, Vaporciyan AA, et al. Sarcomatoid carcinoma of the lung: A predictor of poor prognosis. Ann Thorac Surg. 2007;84:973–80. doi: 10.1016/j.athoracsur.2007.03.099. [DOI] [PubMed] [Google Scholar]


