Abstract
Objectives:
The objective is to determine utility of SAPS II, APACHE II, SAPS III, and APACHE IV scoring system in assessing outcome in mechanically ventilated patients in respiratory intensive care unit and to predict duration of mechanical ventilation (MV).
Materials and Methods:
A prospective observational study where 83 mechanically ventilated patients were grouped into Group 1 (n1 = 40, NIV) and Group 2 (n2 = 43, Invasive ventilation) was conducted. SAPS II, APACHE II, SAPS III, and APACHE IV scores based predicted mortality (PM) were collected at day 1, and day 3. Outcomes (on day 7) were grouped into negative and positive. (NIV-negative outcome = Home NIV, intubation or death; positive outcome = NIV free. Invasive group-positive outcome = Extubation; negative outcome = Death). Binary logistic regression was applied to predict duration of MV (> or < 5 days).
Results:
The data were analyzed using SPSS version 17.0 trials comparisons of PM on day 1 with SAPS II (P < 0.05) and APACHE IV (P < 0.007) were significant predictors of clinical outcomes in Group 1 where as in Group 2, none of the system could predict significantly. On day 3, Group 1 analysis revealed SAPS II (P < 0.002), SAPS III (P < 0.03), and APACHE IV (P < 0.004) based PM as significant predictors of outcome. APACHE II (P < 0.05) and APACHE IV (P < 0.02) PM were significant in Group 2. On day 3, APACHE IV could significantly predict (P < 0.05) duration of MV (>5 or < 5) while A-a gradient (P < 0.09) predicted poorly in Group 1. In Group 2, APACHE IV was a poor predictor (P < 0.09). Two full logistic regression models were also formulated for both the groups.
Conclusion:
Study concludes that day 3 severity scores are more significant predictors of outcome and duration. APACHE IV scoring system was found more effective than other systems, not only significantly differentiating outcomes of MV but also predicting duration of NIV.
KEY WORDS: APACHE II, APACHE IV, duration of mechanical ventilation, outcome of mechanical ventilation, SAPS II, SAPS III
INTRODUCTION
Respiratory failure is the one of the most frequent indication of mechanical ventilation (MV); also pulmonary diseases constitute the most common comorbidities on mechanical ventilation.[1,2,3]
Despite advances in therapeutic interventions, mortality has remained high over the years.[4] If outcome and duration of invasive ventilation can be foreseen, early interventions like tracheostomy in case of prolonged MV can be planned which might help in preventing mortality, reducing cost, and counseling patients and relatives. Moreover, there are no standard guidelines to wean off non-invasive ventilation; this leads to prolong use of NIV resulting in extended hospital stay, higher chances of HAI and also cost of healthcare.[5]
Need for a validated indicator to evaluate MV practices has become important in current scenario. Scoring systems have long been used to evaluate delivery of healthcare and to predict outcome of critically ill patients. This study was undertaken to evaluate, if existing severity scores namely SAPS II, APACHE II, SAPS III, and APACHE IV could predict outcome and duration of MV.
MATERIALS AND METHODS
A comparative study was conducted in respiratory intensive care unit (ICU) of a tertiary care center in Central India, over a period of 1 year 2018–2019. Patients >18 years of age, excluding pregnant women and children, who underwent MV for respiratory failure due to various underlying pulmonary etiologies. Out of total (n = 83), 40 patients required noninvasive ventilation (Group 1 = 40) whereas forty three required invasive ventilation (Group 2 = 43). SAPS II, APACHE II, SAPS III, and APACHE IV scores based predicted mortality (PM) were collected at day 1, and day 3 [Figure 1].
Figure 1.
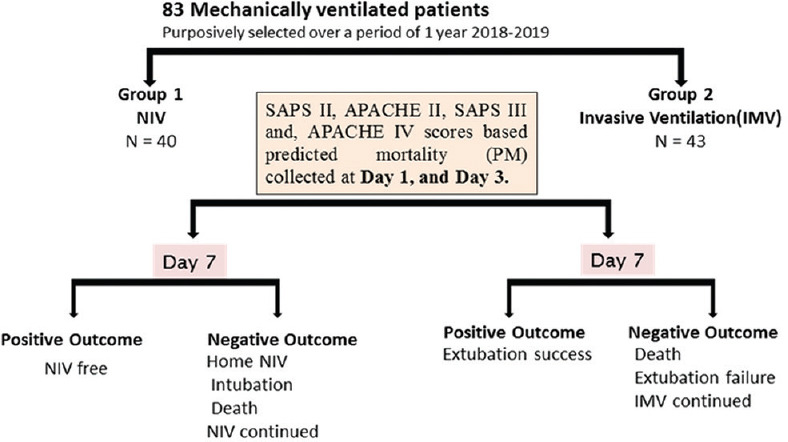
Study scheme
Outcomes were analyzed on day 7 being grouped into negative and positive. Negative outcomes for NIV were patient ending on domiciliary NIV therapy, intubation or death during the course of NIV or continuation of NIV at day 7; whereas positive outcome being freedom from NIV. For Group 2, positive outcome was extubation success; whereas negative were death, extubation failure or continuation of therapy at day 7.
The data were analyzed using SPSS Statistics foe windows, version 17 (SPSS INC., Chicago, Illinois, USA) trials. Descriptive and inferential statistics were used. Results for continuous variables presented as mean ± standard deviation while categorical presented in numbers (%). This was assumed that the observations recorded for a continuous variable had followed a normal distribution.
Significance of scoring systems PM (%) on day 1 and 3 between outcomes (positive/negative) on day 7 was identified using t-test. The P ≤ 0.05 was considered as significant while P ≤ 0.01 and above were considered as highly/strongly significant.
Binary logistic regression was used to predict the days of MV of studied mechanically ventilated patients of Group 1 (noninvasive) and Group 2 (invasive) by employing age, sex, gradient, PaO2/FiO2 ratio, SAPS II, APACHE II, SAPS III, and APACHE IV scoring systems PM (percentage) to model the prediction of days of MV.
RESULTS
Out of a total patients, 65 were (78.3%) male while rests (18, 21.7%) were female. The mean age (mean ± standard deviation) of all mechanically ventilated patients (n = 83) was 54.20 ± 13.06 years, observed within ranges from 18 to 85 years.
Acute exacerbation of chronic obstructive pulmonary disease was found to be the most common diagnosis in Group 1, whereas bacterial pneumonia in Group 2 [Table 1].
Table 1.
Diagnosis among mechanically ventilated patient of two groups
| Diagnosis of mechanically ventilated patient | Noninvasive (Group 1) n (%) n1=40, n (%) | Invasive (Group 2) n2=43, n (%) |
|---|---|---|
| Acute exacerbations of chronic obstructive pulmonary disease | 14 (35.0) | 9 (20.9) |
| Post tuberculosis chronic obstructive pulmonary disease | 2 (5.0) | 2 (4.7) |
| Viral pneumonia | 5 (12.5) | 10 (23.3) |
| Bacterial pneumonia | 5 (12.5) | 14 (32.6) |
| Aspiration pneumonia | 0 (0.0) | 2 (4.7) |
| Disseminated tuberculosis | 0 (0.0) | 1 (2.3) |
| Noncardiogenic pulmonary edema | 1 (2.5) | 1 (2.3) |
| Interstitial lung disease | 3 (7.5) | 1 (2.3) |
| Chronic obstructive pulmonary disease with bronchiectasis | 5 (12.5) | 1 (2.3) |
| Posttuberculosis chronic obstructive Pulmonary disease with posttuberculosis bronchiectasis | 3 (7.5) | 1 (2.3) |
| Chronic obstructive pulmonary disease with community-acquired pneumonia | 2 (5.0) | 1 (2.3) |
Comparisons of PM (%) on day 1 revealed that the severity scoring systems SAPS II and APACHE IV significantly differentiated between clinical outcomes on day 7 among patients supported with noninvasive (Group 1) ventilator. Among patients of Group 2, only APACHE IV-based PM produced acceptable results, such that PM of negative outcome was higher, but did not reach the statistical significance [Table 2].
Table 2.
Comparison of baseline SAPS II, SAPS III, APACHE II, and APACHE IV predicted mortality (%) at day 1 between outcomes (positive/negative) on day 7
| Group and severity scoring system | (n) D1 | Outcome at day 7 | Scatter (%)Mean±SD | Mean difference (%) | t-statistic | P (LOS) | |
|---|---|---|---|---|---|---|---|
| Noninvasive ventilation (Group 1) | SAPS II PM (%) on D1 | 19 | Negative | 13.91±7.89 | 4.67 | 2.04 | P<0.05* |
| 21 | Positive | 9.24±6.56 | |||||
| SAPS III PM (%) on D1 | 19 | Negative | 18.74±10.28 | 2.55 | 0.95 | P>0.05 | |
| 21 | Positive | 16.19±6.38 | |||||
| APACHE II PM (%) on D1 | 19 | Negative | 26.95±11.71 | 5.38 | 1.62 | P>0.05 | |
| 21 | Positive | 21.57±9.20 | |||||
| APACHE IV PM (%) on D1 | 19 | Negative | 11.21±8.32 | 5.96 | 2.83 | P<0.00# | |
| 21 | Positive | 5.24±4.68 | |||||
| Invasive ventilation (Group 2) | SAPS II PM (%) on D1 | 19 | Negative | 27.58±17.41 | 6.60 | 1.11 | N/A |
| 24 | Positive | 34.18±20.71 | |||||
| SAPS III PM (%) on D1 | 19 | Negative | 24.42±14.16 | 8.63 | 1.86 | N/A | |
| 24 | Positive | 33.05±15.77 | |||||
| APACHE II PM (%) on D1 | 19 | Negative | 31.35±14.80 | 6.03 | 1.26 | N/A | |
| 24 | Positive | 37.38±16.25 | |||||
| APACHE IV PM (%) on D1 | 19 | Negative | 27.21±18.69 | 4.26 | 0.75 | P>0.05 | |
| 24 | Positive | 22.95±18.36 | |||||
#The differences are highly significant at the 0.007 level of significance. ∧The differences are poorly/suggestively significant at the 0.07 level of significance. *The mean difference is significant at the 0.03 level of significance. ⊗The differences are not (insignificant) significant at the 0.05 level of significance. The degrees of freedom are 38 and 41. PM: Predicted mortality, LOS: Level of significance, NA: Not available, SD: Standard deviation
Comparisons of PM (%) on day 3 among severity scoring systems revealed that the scoring systems SAPS II, APACHE II and APACHE IV had significantly differentiated clinical outcomes in Group 1 on day 7. Among patients of group 2, comparisons of PM (%) on day 3 revealed that the severity scoring systems SAPS III and APACHE IV PM (%) on day 3 had significantly differentiated clinical outcomes on day 7 [Table 3].
Table 3.
Comparison of baseline SAPS II, SAPS III, APACHE II, and APACHE IV predicted mortality (%) at day 3 between outcomes (positive/negative) on day 7
| Group and severity scoring system | (n) D3 | Outcome at day 7 | Scatter (%)Mean±SD | Mean difference | t-statistic | P (LOS) | |
|---|---|---|---|---|---|---|---|
| Noninvasive Ventilation (Group 1) | SAPS II PM (%) on D1 | 13 | Negative | 13.51±7.68 | 6.54 | 3.31 | P<0.002# |
| 21 | Positive | 6.97±3.86 | |||||
| SAPS III PM (%) on D1 | 13 | Negative | 19.09±14.69 | 5.38 | 1.44 | P>0.05 | |
| 21 | Positive | 13.71±6.99 | |||||
| APACHE II PM (%) on D1 | 13 | Negative | 26.31±8.24 | 6.36 | 2.32 | P<0.03* | |
| 21 | Positive | 19.95±7.49 | |||||
| APACHE IV PM (%) on D1 | 13 | Negative | 11.22±9.35 | 7.18 | 3.11 | P<0.004# | |
| 21 | Positive | 4.04±3.99 | |||||
| Invasive Ventilation (Group 2) | SAPS II PM (%) on D1 | 13 | Negative | 34.01±23.20 | 11.92 | 1.61 | P>0.05 |
| 24 | Positive | 22.09±20.49 | |||||
| SAPS III PM (%) on D1 | 13 | Negative | 35.77±21.68 | 13.64 | 2.13 | P<0.05* | |
| 24 | Positive | 22.13±16.71 | |||||
| APACHE II PM (%) on D1 | 13 | Negative | 42.35±23.18 | 10.76 | 1.47 | P>0.05 | |
| 24 | Positive | 31.59±20.26 | |||||
| APACHE IV PM (%) on D1 | 13 | Negative | 35.31±25.12 | 18.01 | 2.58 | P<0.02* | |
| 24 | Positive | 17.30±17.21 | |||||
#The differences are highly significant at the 0.004 and 0.007 levels of significance. *The mean difference is significant at the 0.02, 0.03 and 0.05 levels of significance. ⊗The differences are not (insignificant) significant at the 0.05 level of significance. The degrees of freedom are 32 and 35. PM: Predictedmortality; LOS: Level of significance, SD: Standard deviation
Since more number of scoring systems was found significant on day 3 in differentiating outcome in Group 1 and Group 2, day 3 scores were used to predict duration of MV. A cut off point for duration of MV (2–14 days) in mechanically ventilated patients (n = 83) on noninvasive (n1 = 40) and invasive (n2 = 43) ventilators was projected by subtracting 2×SE (0.606 days) from mean duration of MV (5.08–0.606 = 4.474 days). To avoid fractions and for simplification, the approximate figure of 5 days was considered as cut off point for the duration of MV.
Tables 4 and 5 report the analysis of binary logistic regression to predict the days of MV of studied patients of Group 1 (noninvasive) and Group 2 (invasive) by employing age, sex, gradient, ratio of partial pressure of oxygen (PaO2), and fraction of inspired oxygen (FiO2), SAPS II, APACHE II, SAPS III, and APACHE IV PM (%) at day 3 model the prediction of days of MV.
Table 4.
Significance of prediction of duration of mechanical ventilation among patients supported with noninvasive (Group 1) ventilator at day 3
| Parameters and scoring system predicted mortality at day 3 | β | SE | P (LOS) | Odds ratio | 95% CI | |
|---|---|---|---|---|---|---|
| Upper | Lower | |||||
| Age (year) | 0.058 | 0.047 | P>0.05 | 1.059 | 0.966 | 1.162 |
| Sex (male) | −0.117 | 1.234 | P>0.05 | 0.890 | 0.079 | 9.994 |
| Gradient | 0.008 | 0.004 | P<0.09 | 1.008 | 0.999 | 1.016 |
| PaO2/FiO2 ratio | −0.001 | 0.002 | P>0.05 | 0.999 | 0.994 | 1.003 |
| SAPS II (predicted mortality %) | −0.061 | 0.122 | P>0.05 | 0.940 | 0.741 | 1.194 |
| APACHE II (predicted mortality %) | −0.069 | 0.064 | P>0.05 | 0.933 | 0.824 | 1.057 |
| SAPS III (predicted mortality %) | −0.051 | 0.093 | P>0.05 | 0.951 | 0.792 | 1.142 |
| APACHE IV (predicted mortality %) | −0.203 | 0.101 | P<0.05* | 0.817 | 0.670 | 0.996 |
*The test variable is significant at the 0.05 level of significance. ⊗The test variable is not (insignificant) significant at the 0.05 level of significance. ^The test variable is poorly/suggestively significant at the 0.07 level of significance. LOS: Level of significance, CI: Confidence interval, SE: Standard error
Table 5.
Significance of prediction of duration of mechanical ventilation among patients supported with invasive (Group 2) ventilator at day 3
| Parameters and scoring system predicted mortality at day 3 | β | SE | P (LOS) | Odds ratio | 95% CI | |
|---|---|---|---|---|---|---|
| Upper | Lower | |||||
| Age (year) | 0.007 | 0.042 | P>0.05 | 1.007 | 0.928 | 1.093 |
| Sex (male) | −0.584 | 1.059 | P>0.05 | 0.558 | 0.070 | 4.443 |
| Gradient | 0.000 | 0.005 | P>0.05 | 0.999 | 0.990 | 1.009 |
| PaO2/FiO2 ratio | 0.001 | 0.008 | P>0.05 | 1.001 | 0.986 | 1.017 |
| SAPS II (predicted mortality, %) | 0.091 | 0.063 | P>0.05 | 1.095 | 0.969 | 1.239 |
| APACHE II (predicted mortality, %) | −0.068 | 0.055 | P>0.05 | 0.934 | 0.839 | 1.040 |
| SAPS III (predicted mortality, %) | 0.027 | 0.034 | P>0.05 | 1.027 | 0.962 | 1.098 |
| APACHE IV (predicted mortality, %) | −0.063 | 0.037 | P<0.09^ | 0.939 | 0.874 | 1.009 |
*The test variable is significant at the 0.05 level of significance. ⊗The test variable is not (insignificant) significant at the 0.05 level of significance. ^The test variable is poorly/suggestively significant at the 0.07 level of significance. LOS: Level of significance, CI: confidence interval, SE: Standard error
Logistic model for the duration of MV (non-invasive) showed that the severity and mortality predictor system APACHE IV to be the significant predictor (P < 0.05) of duration of MV while Alveolar–Arterial Gradient (P < 0.09) predicted poorly whereas age, sex (male), and rest three severity scoring systems were confirmed insignificant predictors of duration of MV.
Logistic model for the duration of MV (invasive) showed that the severity and mortality predictor system APACHE IV to be the poorly significant predictor (P < 0.09) of duration of MV whereas age, sex (male), ratio of PaO2 and FiO2, and rest three severity scoring systems were confirmed insignificant predictors of duration of MV.
The individual full logistic regression model for the duration of noninvasive MV <5 and ≥5 days is as follows;
Log odds of duration of MV (noninvasive) = 0.079 + 0.058 × Age (year)-0.117 × Sex (1 If Male and 0 If female) +0.008 × Gradient (score)–0.001 × ratio of PaO2 and FiO2 (ratio)-0.061 × SAPS II (mortality %)–0.069 × APACHE II (mortality %)-0.051 × SAPS III (mortality %)–0.203 × APACHE IV (mortality %).
The probability of correct prediction was found to be 55.9%. However, the sensitivity of prediction (≥5 days) found to be 89.5% as compared to specificity of prediction (<5 days) was 66.7%.
The individual full logistic regression model for duration of invasive MV <5 and ≥5 days is as follows;
Log odds of duration of MV (invasive) =0.375 + 0.007 × Age (year)-0.584 × Sex (1 If Male and 0 If female) +0.000 × Gradient (score) +0.001 × ratio of PaO2 and FiO2 (ratio) +0.091 × SAPS II (mortality %)–0.068 × APACHE II (mortality %) +0.027 × SAPS III (mortality %)-0.063 × APACHE IV (mortality %).
The probability of correct prediction found to be 56.8%. However, the sensitivity of prediction (≥5 days) found to be 76.2% as compared to specificity of prediction (<5 days) was 62.5%.
DISCUSSION
Clinical outcome is an important measure of efficacy of MV applied to the patients. Our study have attempted to predict outcome and duration of MV by means of existing severity scoring systems, demographic characters, and ventilatory parameters. Scoring systems have not been validated in predicting outcome and duration of mechanically ventilated patients in larger Indian scenario.[6]
The presence of validated indicators of outcome and duration of invasive and non-invasive MV for Indian population, will not only result in better patient care, but also in proper utilization of resources, and will also bring uniformity and standardization of practice patterns in ICU.[7]
In our study, severity scores found at day 3 of initiation of therapy were found to be more significant predictors of outcome as compared to severity scores at initiation, which was also found in study by Hira and Mittal.[8]
APACHE IV scoring system was found more effective than other systems, not only significantly differentiating outcomes of MV but also predicting duration of NIV, which may be the result of consideration of use MV and including a disease specific reason for admission in its risk prediction.[9] The disadvantages of APACHE IV scoring system in an Indian scenario would be higher data abstraction time as compared to other systems, with additional requirement of resources.[10]
Interestingly, SAPS II was also found as a significant indicator of outcomes of NIV group on day 1 and day 3, which correlates with previous studies.[11,12,13]
Therefore, our study suggests APACHE IV as a better predictor of outcome and duration of MV, though this work is preliminary with potential limitations such as being a single center study with very small sample size.
CONCLUSION
The study concludes that day 3 severity scores are more significant predictors of outcome. APACHE IV scoring system was found more effective than other systems, not only significantly differentiating outcomes of MV but also predicting duration of NIV.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cartin-Ceba R, Kojicic M, Li G, Kor DJ, Poulose J, Herasevich V, et al. Epidemiology of critical care syndromes, organ failures, and life-support interventions in a suburban US community. Chest. 2011;140:1447–55. doi: 10.1378/chest.11-1197. [DOI] [PubMed] [Google Scholar]
- 2.Wunsch H, Linde-Zwirble WT, Angus DC, Hartman ME, Milbrandt EB, Kahn JM. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38:1947–53. doi: 10.1097/CCM.0b013e3181ef4460. [DOI] [PubMed] [Google Scholar]
- 3.Khatib KI, Dixit SB, Joshi MM. Factors determining outcomes in adult patient undergoing mechanical ventilation: A “real-world” retrospective study in an Indian intensive care unit. Int J Crit Illn Inj Sci. 2018;8:9–16. doi: 10.4103/IJCIIS.IJCIIS_41_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fialkow L, Farenzena M, Wawrzeniak IC, Brauner JS, Vieira SR, Vigo A, et al. Mechanical ventilation in patients in the intensive care unit of a general university hospital in Southern Brazil: An epidemiological study. Clinics (Sao Paulo) 2016;71:144–51. doi: 10.6061/clinics/2016(03)05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khilnani GC, Jain N. Do we need a protocol for weaning patients from noninvasive ventilation? Indian J Crit Care Med. 2014;18:775–7. doi: 10.4103/0972-5229.146298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sudarsanam TD, Jeyaseelan L, Thomas K, John G. Predictors of mortality in mechanically ventilated patients. Postgrad Med J. 2005;81:780–3. doi: 10.1136/pgmj.2005.033076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seneff MG, Zimmerman JE, Knaus WA, Wagner DP, Draper EA. Predicting the duration of mechanical ventilation. The importance of disease and patient characteristics. Chest. 1996;110:469–79. doi: 10.1378/chest.110.2.469. [DOI] [PubMed] [Google Scholar]
- 8.Hira HS, Mittal A. Evaluation of the predictors for duration of mechanical ventilation in respiratory intensive care unit. Lung India. 2006;23:70–4. [Google Scholar]
- 9.Parajuli BD, Shrestha GS, Pradhan B, Amatya R. Comparison of acute physiology and chronic health evaluation II and acute physiology and chronic health evaluation IV to predict intensive care unit mortality. Indian J Crit Care Med. 2015;19:87–91. doi: 10.4103/0972-5229.151016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuzniewicz MW, Vasilevskis EE, Lane R, Dean ML, Trivedi NG, Rennie DJ, et al. Variation in ICU risk-adjusted mortality: Impact of methods of assessment and potential confounders. Chest. 2008;133:1319–27. doi: 10.1378/chest.07-3061. [DOI] [PubMed] [Google Scholar]
- 11.Stefan MS, Nathanson BH, Higgins TL, Steingrub JS, Lagu T, Rothberg MB, et al. Comparative effectiveness of noninvasive and invasive ventilation in critically ill patients with acute exacerbation of chronic obstructive pulmonary disease. Crit Care Med. 2015;43:1386–94. doi: 10.1097/CCM.0000000000000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoshida Y, Takeda S, Akada S, Hongo T, Tanaka K, Sakamoto A. Factors predicting successful noninvasive ventilation in acute lung injury. J Anesth. 2008;22:201–6. doi: 10.1007/s00540-008-0637-z. [DOI] [PubMed] [Google Scholar]
- 13.Antonelli M, Conti G, Esquinas A, Montini L, Maggiore SM, Bello G, et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med. 2007;35:18–25. doi: 10.1097/01.CCM.0000251821.44259.F3. [DOI] [PubMed] [Google Scholar]


