Abstract
Background
The 10-month timeline from conception to regulatory approval of the Pfizer–BioNTech vaccine against SARS-CoV-2 is unprecedented in modern medicine. However, the climate of the pandemic has also seen anti-vaccination sentiments flourish.
Aims
To determine the intent to accept COVID-19 vaccination among healthcare workers at a London Hospital Trust and examine variation in uptake between demographic groups.
Methods
We conducted a cross-sectional survey open to staff working at the trust. Staff rated on a five-point scale the likelihood of them accepting COVID-19 vaccination.
Results
We received 514 responses, representing 16% of the workforce. About 59% of staff intended to seek vaccination, 24% to reject and 17% were unsure. There was significantly reduced intended uptake in females, younger age groups, healthcare assistants, nurses, staff of black ethnic backgrounds and those who rejected influenza vaccination. Safety was the dominant concern.
Conclusions
Our study finds COVID-19 vaccinate hesitancy is prevalent among healthcare workers at a London Hospital Trust. It is particularly concerning that hesitancy was highest amongst groups most exposed to COVID-19 and most at risk of severe disease. Reasons behind disparities in uptake must be addressed to protect staff and prevent deepening inequalities within the healthcare workforce.
Keywords: Health promotion, infection, NHS workforce, occupational exposure, vaccination
Key learning points.
What is already known about this subject:
Studies in healthcare workers (HCWs) from France and Israel report increased COVID-19 vaccine uptake in men, older age groups, those vaccinated against influenza and those at increased risk of severe infection. Lower uptake was found in nursing and assistant nursing staff compared to doctors [3,4].
One study of the UK general population found 32% considered themselves ‘unlikely’ or ‘very unlikely’ to get vaccinated [2].
What this study adds:
Our study suggests that COVID-19 vaccine hesitancy is prevalent among HCWs at a London Hospital Trust. Only 59% of staff reported intent to accept COVID-19 vaccination, with 24% intending to reject and 17% unsure.
We found reduced intent to seek vaccination in females, younger age groups, nursing staff, HCAs, staff of black ethnicity, those who had rejected the influenza vaccine and those working in COVID-19 areas. Increased intended uptake was seen with management staff and doctors.
Safety concern was the dominant reason for vaccine rejection. Other major themes were availability of trial data and efficacy.
What impact this may have on practice or policy:
It is particularly concerning that hesitancy was highest amongst groups most exposed to COVID-19 and those most at risk of severe disease.
Reasons behind disparities in uptake must be addressed to protect staff and prevent deepening inequalities within the healthcare workforce.
Introduction
The 10-month timeline from conception to regulatory approval of the Pfizer–BioNTech vaccine against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is unprecedented in modern medicine. The breakthrough was hailed as ‘the beginning of the end’ in the battle against COVID-19 [1]. However, the climate of the pandemic has seen anti-vaccination sentiments flourish.
A survey of the UK public found 32% considered themselves ‘unlikely’ or ‘very unlikely’ to seek COVID-19 vaccination [2]. Healthcare workers (HCWs) are not immune to vaccine hesitancy. A study from Israel found 39% of nurses and 22% of doctors intended to reject COVID-19 vaccination [3]. In France, rejection was reported at 35.5% for nurses and 39.9% for assistant nurses [4].
We conducted a cross-sectional survey to determine intent to accept COVID-19 vaccination and examine variation in uptake between demographic groups among HCWs at London North West University Hospital Trust.
Methods
The study was conducted at a large integrated care trust, serving a population of over 1 million people. Approval for the protocol was obtained from the local research governance committee. Formal ethics review was not required as determined by the HRA decisions tool (http://www.hra-decisiontools.org.uk/research/).
Staff were approached in person on site in non-clinical areas and invited to participate. Participants scanned a QR code to access an anonymous online survey. The survey was also disseminated via staff email communications. Responses were collected from 1 to 21 December 2020.
A small-scale pre-test was conducted. Grammatical and typographical corrections were made based on feedback. Staff rated the likelihood of them accepting COVID-19 vaccination on a five-point scale (very unlikely, unlikely, unsure, likely, very likely). Demographic information and explanatory variables including uptake of influenza vaccination were collected.
Data processing and analysis were conducted using IBM SPSS statistics (IBM Corporation, Armonk, NY, USA). Descriptive statistics outlined baseline characteristics. Data were non-parametric and were analysed using the Kruskal–Wallis or Mann–Whitney U-test.
Responses of ‘very likely’ or ‘likely’ were taken as vaccine acceptance, and ‘very unlikely’ or ‘unlikely’ as rejection. Odds ratios were calculated using vaccine acceptance and rejection only.
The survey included the open question: ‘If you would say no to having the vaccine, what other information or factors might influence you to have the vaccine?’. Responses were analysed using qualitative content analysis with inductive category development [5]. Two investigators independently coded responses. Responses coded differently were discussed by coders to reach a consensus.
Results
We received 514 responses, representing 16% of the workforce. About 59% (n = 304) of participants reported intent to accept COVID-19 vaccination, 24% (n = 124) to reject and 17% (n = 86) responded ‘unsure’.
Acceptance was significantly increased amongst hospital management compared to nursing, healthcare assistants (HCAs) and pharmacists (P < 0.05). Increased uptake for doctors was significant compared to nursing (P < 0.001), HCAs (P < 0.001), pharmacists (P < 0.001), allied health professionals (P < 0.01) and administrative staff (P < 0.01).
Acceptance was significantly increased for staff aged 61 plus compared to 18–25, 26–30, 31–40 and 41–50 (P < 0.01). Increased acceptance was significant for staff aged 51–60 compared to 18–25 (P < 0.01), 26–30 (P < 0.05), 31–40 (P < 0.05) and 41–50 (P < 0.05). Intent was significantly decreased amongst black ethnicity staff compared to White (P < 0.001), Indian (P < 0.001) and other Asian backgrounds (P < 0.01). The odds ratio of vaccine rejection was 0.509 for men (95% CI 0.335–0.773) and 1.26 for women (95% CI 1.121–1.416, P < 0.001).
The odds ratio for COVID-19 vaccine rejection was 0.453 (95% CI 0.031–0.96) for those accepting influenza vaccination and 8.320 (95% CI 5.360–12.914, P < 0.001) for those who rejected influenza vaccination.
A summary of results is found in Table 1 (available as Supplementary data at Occupational Medicine Online).
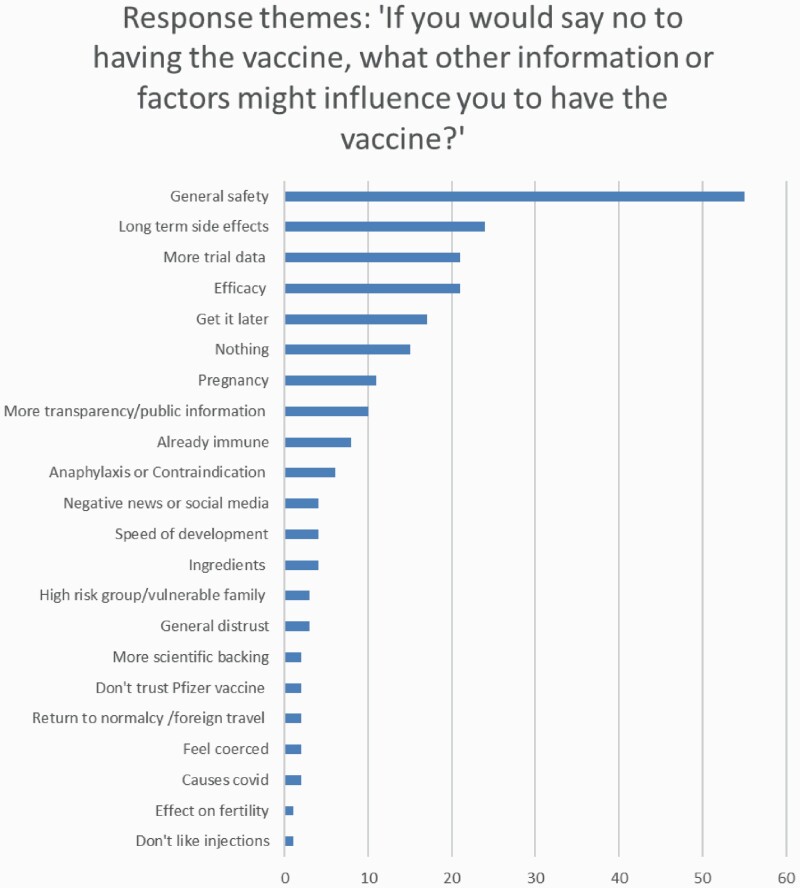
We received a total of 169 short answer responses to the question: ‘If you would say no to having the COVID-19 vaccine, what other information or factors might influence you to have the vaccine?’. A summary of response themes is shown in Figure 1.
Figure 1.
Bar chart of response themes ‘If you would say no to having the vaccine, what other information or factors might influence you to have the vaccine’.
Safety concern was the dominant reason for vaccine rejection. Other major themes were availability of trial data and efficacy. About 15 responded that ‘nothing’ would influence them to seek vaccination. A small number of responses quoted highly publicized online misinformation, including concerns about their ingredients, that they cause COVID-19 illness and reduced fertility.
Discussion
We found reduced intent to seek vaccination in females, younger age groups, nursing staff, HCAs, staff of black ethnicity, those who had rejected influenza vaccination and those working in COVID-19 areas. Doctors and management had increased intent. Safety was the dominant concern.
Vaccine acceptance was lower in staff from black ethnic groups compared to all other ethnic groups. Although our response rate was low (n = 37), this mirrors findings from recent studies of the general population in the UK and USA [6,7]. Black ethnic groups have been disproportionately impacted by COVID-19. In England, they represent 6% of the workforce but 27% of HCW deaths from COVID-19 [8].
HCAs and nursing staff had the lowest vaccine acceptance by staff group, consistent with studies from abroad [3,4]. Nurses and healthcare support workers accounted for the greatest number of COVID-19 HCW deaths in the UK, at 33% and 25% respectively [8].
The strongest predictor of vaccine acceptance was uptake of the influenza vaccine. This is consistent with previous studies in HCWs [3,4,9], suggesting general vaccine hesitancy is a major driver of COVID-19 vaccine rejection.
Despite extensive supportive literature on the vaccine’s safety, this was the dominant reason cited for rejection, consistent with studies from abroad [3,4]. The source for these concerns was rarely specified in our survey responses. Studies in the general population report social media as a significant source of misinformation [10].
Our study finds COVID-19 vaccine hesitancy is prevalent among HCWs at a London hospital Trust. It is particularly concerning that hesitancy was highest amongst groups most exposed to COVID-19 and most at risk of severe disease. Reasons behind disparities in uptake must be addressed to protect staff and prevent deepening inequalities within the healthcare workforce.
Limitations include the low response rate of 16%, particularly in some subgroups. Responses were collected prior to reporting of highly infectious COVID-19 variants and the introduction of a third UK national lockdown.
Funding
No funding was received for this study.
Competing interests
The authors declare no competing interests.
Consent: Consent given by the participant deciding to log on to the survey site after reading the terms of participation on the front page and proceeding to complete the questionnaire.
Data availability
All data were anonymous, and individuals could not be identified by the investigators. The data underlying this article is available on request to the corresponding author.
References
- 1. BBC News. Coronavirus: Vaccine Rollout ‘Marathon not a Sprint’ – Powis. https://www.bbc.co.uk/news/uk-55202093 (21 March 2021, date last accessed).
- 2. A Fifth of People Say They’re Unlikely to Get Vaccinated Against COVID-19. https://www.ucl.ac.uk/news/2020/sep/fifth-people-say-theyre-unlikely-get-vaccinated-against-COVID-19 (retrieved 5 December 2020).
- 3. Dror AA, Eisenbach N, Taiber Set al.. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol 2020;35:775–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gagneux-Brunon A, Detoc M, Bruel Set al.. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross sectional survey. J Hosp Infect 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mayring P. Qualitative content analysis. Forum Qual Soc Res 2000;1. http://nbn-resolving.de/urn:nbn:de:0114-fqs0002204 [Google Scholar]
- 6. Sethi S, Kumar A, Shaikh Met al.. The Uptake Study: Insights and Beliefs of the UK Population on Vaccines During the COVID-19 Pandemic. 2020. Available SSRN: https://ssrn.com/abstract=3723667 or doi: 10.2139/ssrn.3723667 [DOI]
- 7. Malik A, McFadden S, Elharake J, Omer S. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cook T, Kursumovic E, Lennane S. Deaths of NHS Staff from COVID-19 Analysed.https://www.hsj.co.uk/exclusive-deaths-of-nhs-staff-from-COVID-19-analysed/7027471.article (retrieved 5 January 2021).
- 9. Wang K, Wong E, Ho Ket al.. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine 2020;38:7049–7056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Global Health 2020;5:e004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data were anonymous, and individuals could not be identified by the investigators. The data underlying this article is available on request to the corresponding author.