Summary
In India, strict public health measures to suppress COVID-19 transmission and reduce burden have been rapidly adopted. Pandemic containment and confinement measures impact societies and economies; their costs and benefits must be assessed holistically. This study provides an evolving portrait of the health, economic and social consequences of the COVID-19 pandemic on vulnerable populations in India. Our analysis focuses on 100 days early in the pandemic from 13 March to 20 June 2020. We developed a conceptual framework based on the human right to health and the UN Sustainable Development Goals (SDGs). We analysed people’s experiences recorded and shared via mobile phone on the voice platforms operated by the Gram Vaani COVID-19 response network, a service for rural and low-income populations now being deployed to support India’s COVID-19 response. Quantitative and visual methods were used to summarize key features of the data and explore relationships between factors. In its first 100 days, the platform logged over 1.15 million phone calls, of which 793 350 (69%) were outbound calls related largely to health promotion in the context of COVID-19. Analysis of 6636 audio recordings by network users revealed struggles to secure the basic necessities of survival, including food (48%), cash (17%), transportation (10%) and employment or livelihoods (8%). Themes were mapped to shortfalls in 10 SDGs and their associated targets. Pre-existing development deficits and weak social safety nets are driving vulnerability during the COVID-19 crisis. For an effective pandemic response and recovery, these must be addressed through inclusive policy design and institutional reforms.
Keywords: COVID-19, mHealth, social determinants of health, right to health, social justice
INTRODUCTION
The global COVID-19 pandemic is a complex emergency with multidimensional consequences impacting health, economies and societies. These consequences threaten global development trajectories and are expected to be particularly severe for poor countries and people, especially in sub-Saharan Africa and South Asia (World Bank, 2020). According to the World Bank’s latest estimates of the impact of COVID-19 on global poverty, COVID-19 will push 71–100 million people into extreme poverty (<US $1.90 per day), mostly in sub-Saharan Africa, and propel an additional 176–231 million to join the ranks of the poor (calculated at <US $3.20 per day), mostly in South Asia (World Bank, 2020).
A lower-middle-income South Asian country with a population of 1.34 billion, India is the world’s largest democracy. India’s first COVID-19 case was reported on 30 January 2020; by March 11, the date that WHO declared COVID-19 a pandemic, India had 71 confirmed cases. On 25 March, with 497 cumulative cases, in an effort to contain the epidemic and avert a looming crisis, the Government of India introduced a nationwide lockdown (https://www.covid19india.org/ Accessed March 06, 2021).
In parallel, Indian civil society organizations were mobilizing to support the emergency. Used by rural and low-income populations, Gram Vaani is a federated network of voice-based community media platforms now being deployed to support India’s COVID-19 response (https://gramvaani.org/?p=3631 Accessed May 10, 2021). The Gram Vaani COVID-19 response network uses mobile phone technology and a network of ground-level field partners to build awareness, counter misinformation, enable community feedback, and to link those in need (e.g. of food, shelter, transportation, health care) or facing injustice, to critical services. The platform can be accessed using any simple mobile phone. Users can listen to audio recordings and also record their own voice messages, which after a moderation process are published on the platform for other users to listen to. This voice-based approach makes it suitable for less literate populations to participate, access useful information, record their own messages asking for help or simply narrate their own experiences to share with other community members. All services are offered free of charge to end-users.
Based on people’s experiences recorded and shared on the voice platforms operated by the Gram Vaani COVID-19 response network, this article seeks to better understand how the COVID-19 pandemic and mitigation strategies have affected poor and vulnerable groups in India. Due to a range of factors, including generally weaker health systems and lesser fiscal space [commonly defined as the budgetary flexibility that allows a government to provide resources for public aims without undermining fiscal sustainability (World Health Organization, 2021)], developing country governments confronting the pandemic are faced with extremely difficult choices. While COVID-19 disease is inflicting substantial human costs, public health protection measures to suppress transmission and reduce burden severely impact societies and economies (https://www.cgdev.org/blog/resilience-developing-nations Accessed March 06, 2021). It is important to assess the costs and benefits of these measures holistically. This work thus has two aims: (i) to provide an evolving portrait of the health, economic and social consequences of the COVID-19 pandemic on vulnerable populations in India, based on the perspective of the human right to health and the Sustainable Development Goals (SDGs) and (ii) to draw policy lessons to inform a resilient pandemic response and support an inclusive recovery.
Our analysis focuses on 100 days early in the pandemic, from 13 March, 12 days before the national lockdown when India had 91 confirmed cases, to 20 June, 12 days after the national lockdown ended, when the cumulative case count stood at 426 901 (https://www.covid19india.org/ Accessed July 25, 2020). As of 20 June 2020, the Gram Vaani COVID-19 response network included 26+ civil society partner organizations across 10 states and 80+ districts, and had logged over 1 million phone calls and 18 000 user-recorded messages. These are the voices of the poor.
METHODS
Context
Several characteristics make India vulnerable to the effects of COVID-19 and related mitigation measures. Overall economic growth has been strong in recent years, with extreme poverty (US $1.90 per day) dropping from 46% in 1995 to an estimated 15.4% in 2015 (World Bank, 2020). Nonetheless, vulnerability to poverty persists for a large majority of the Indian population; 68% work for US $3.20 or less per day, the World Bank’s new international poverty line for lower-middle-income countries (Kovacevic and Jahic, 2020).
The past decades have also witnessed important reductions in disease burden accompanied by a rapid epidemiological transition; in 2016 all states had a higher burden of disease due to non-communicable diseases and injuries than due to communicable, maternal, neonatal and nutritional conditions (India State-Level Disease Burden Initiative Collaborators, 2017). Population ageing (8% of Indians are over age 65) (Office of the Registrar General and Census Commissioner, 2014) and the high disease burden due to non-communicable diseases may place many Indians at risk of negative outcomes due to SARS-CoV-2 infection. In 2016, the top 20 causes of DALY loss included several known risk factors for severe COVID-19: ischaemic heart disease, chronic obstructive pulmonary disease, cerebrovascular disease, diabetes and chronic kidney disease (India State-Level Disease Burden Initiative Collaborators, 2017). Progress is uneven. Diseases of poverty—for which the relationship to COVID-19 risks is less well understood—such as nutritional deficiencies, diarrhoea, lower respiratory tract infections, tuberculosis and other infectious diseases, remain predominant in some geographies and subpopulations (India State-Level Disease Burden Initiative Collaborators, 2017).
Vulnerability due to structural inequalities, including socioeconomic and demographic factors, health and hygiene conditions is also a key contributing risk (Acharya and Porwal, 2020). Moreover, health system preparedness and response is a critical concern. While countries with high scores on the United Nations Development Program (UNDP) human development index have on average 28.2 doctors, 56 nurses or midwives and 35 hospital beds per 10 000 people, India has only 7.8 doctors, 21 nurses or midwives and 7 hospital beds per 10 000 people (Kovacevic and Jahic, 2020). Compounding problems of limited access to healthcare facilities, in India, health insurance coverage is low and out-of-pocket expenditures are high, ensnaring many citizens in a medical poverty trap (https://www.who.int/gho/countries/ind/country_profiles/en/).
Against this backdrop, India’s public health response to COVID-19 response has been decisive. The Oxford COVID-19 Government Response Tracker gave India’s measures to control the pandemic a stringency score of 100 (out of 100) (Hale et al., 2020).
Conceptual framework
We developed a conceptual framework to monitor the effects of the COVID-19 pandemic and response measures based on the human right to health and the UN 2030 SDGs (Supplementary Figure S1) (Sustainable Development Goals: Sustainable Development Knowledge Platform, 2020). The World Health Organization recommends addressing human rights as a key part of the COVID-19 response (World Health Organization Special Programme for Research Development and Research Training in Human Reproduction, 2020). The human right to health is recognized by law in India (Constitution of India, 1950; Dhar, 2012; Das, 2013; Mathiharan) and internationally. India was a signatory to the Universal Declaration of Human Rights (UDHR), 1948. The Indian constitution, which came into force in 1950, was highly influenced by the UDHR and affirms the population’s right to the highest standard of physical and mental health as well as to protection of life and personal liberty and the right to live with human dignity (Constitution of India, 1950; Dhar, 2012). In 1979, India also ratified the International Covenant on Civil and Political Rights and the International Covenant on Economic, Social and Cultural Rights (Mathiharan). Through its progressive interpretation of the Constitution, the Supreme Court of India has effectively included the right to health as an integral part of the right to life (Article 21), which is a fundamental right (Das, 2013). The Supreme Court has also upheld the importance of providing the key determinants necessary for realizing the right to health (Das, 2013), and recognizes a constitutional obligation to provide health facilities, services and timely access to treatment (Das, 2013; Mathiharan). Unanimously adopted in 2015 by the 193 United Nations Member States, including India, the 17 SDGs provide a global blueprint to end poverty, protect the planet and improve the lives and prospects of everyone, everywhere (United Nations, 2015, 2016).
Categories described entitlements and determinants enshrined in the right to health (The Right to Health. Fact sheet no. 31, 2008) and were refined using a social determinants lens (Working Group for Monitoring Action on the Social Determinants of Health, 2018). The final categorization was mapped to the UN SDG framework (Sustainable Development Goals: Sustainable Development Knowledge Platform, 2020).
Data source
All data came from the Gram Vaani Interactive Voice Response (IVR) system, which automatically logs all outgoing calls and incoming contributions to the COVID-19 response network platform. IVR data stripped of personal identifying information can be disaggregated by various fields including user phone number, date, time, frequency, duration (s), type (outgoing or inbound), content type (e.g. self-assessment of COVID-19 status, information and awareness, news, entertainment, grievances, interviews) and user characteristics.
Data processing for the analysis of user contributions
From 9 June to 26 June 2020, a team of 15 trained field staff performed data screening, extraction, entry and verification. At the screening stage, a single team member listened to each audio file to determine whether it was relevant or irrelevant to this study. Relevant items were those that captured concerns of specific individuals or groups of individuals in relation to the COVID-19 pandemic and public health control measures. Common examples of irrelevant items included general news, announcements or information not about any specific groups or individuals. Relevant contributions were retained for data extraction. During the data extraction phase, relevant contributions were categorized according to a pre-defined coding scheme (Supplementary Table S1). Each field was coded as a binary variable labelled ‘1’ if the code applied and ‘0’ if it did not apply. Data entry was conducted using EPI Info version 7.2.0.1, while data management and analysis pre-processing were performed in Stata Version 15.
Steps were taken to ensure quality at each stage. To minimize subjectivity in relation to data screening, two independent raters scored 107 audio entries; the associated kappa value was 0.85 (almost perfect) (Landis and Koch, 1977). To facilitate data extraction, a detailed data coding form was developed based on a subset of audio files by one author (D.C.) and categories were validated by two other authors (M.J. and A.S.) to ensure that they were easily understandable, comprehensive and mutually exclusive. The coding template was also tested and refined by field staff prior to data extraction. A minimum of 5% of all audio messages were randomly selected for verification. Data mismatches were resolved through repeating the process of audio consultation and extraction with guidance from a supervisor.
Variables
We analysed awareness-related content developed by the Gram Vaani COVID-19 response network partners, termed studio-generated content (SGC), using the continuous metric ‘minutes heard’ to track the outreach achieved by this authoritatively developed content. To analyse user-generated contributions (UGC), we took two approaches: (i) we summarized the raw data and (ii) we recoded data to represent the UN 2030 SDGs. To construct the SDG variables, two authors (D.C. and M.J.) mapped each relevant variable in the coding template to at most one SDG category (Supplementary Table S2). To represent SDG5 (gender equality), we repeated analyses stratifying on caller gender.
Statistical methods
We used quantitative (counts, frequencies, proportions) and visual methods to summarize key features of the data and explore relationships between factors. Data visualizations were programmed in Python using the Folium and Plotly data visualization libraries and refined using Draw.io software. Location coordinates were generated using Map My India’s geocoding library. Analyses focused on the first 100 days of operation.
RESULTS
Total activity logged by the COVID-19 IVR platform
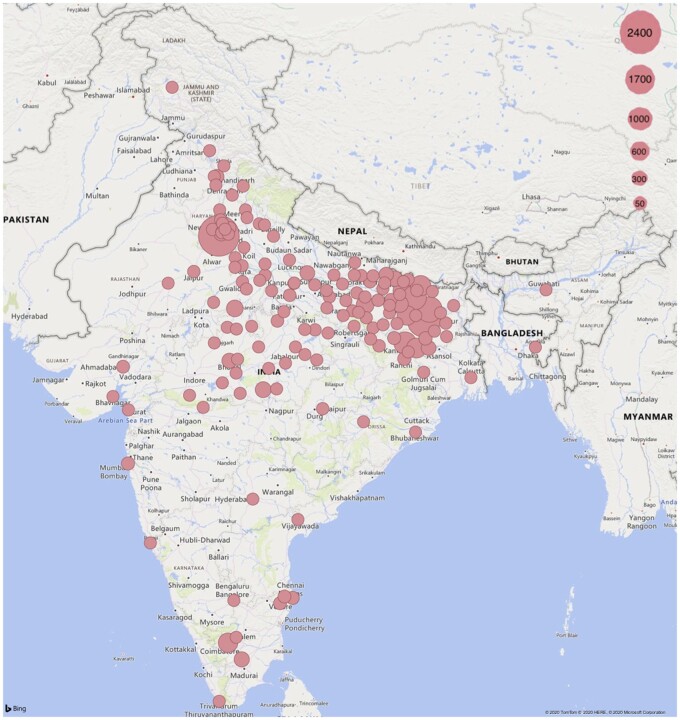
In the 100 days from 13 March to 20 June 2020, the COVID-19 IVR platform logged 1 153 249 total interactions linked to 917 587 unique phone numbers (callers). Of this total, 793 350 were outbound calls offering SGC related to COVID-19 information, awareness-building and service linkages and 359 899 were incoming calls made by users to the IVR platform. These incoming calls led to 19 832 recorded UGC. An SOS functionality enabled callers to signal situations of extreme distress or danger; fully 4931 (24.86%) of user contributions were SOS messages, most of which were followed-up by the Gram Vaani COVID-19 response network to provide relief assistance to the people. Figure 1 shows the spatial distribution of contributions within India; activity distribution reflects the presence of COVID-19 response network partner organizations in a given geography, as well as factors related to the pandemic response and local conditions. Supplementary Figures S2 and S3 present the temporal distribution of total calls, callers, contributions and SOS messages over the 100-day analysis period.
Fig. 1:
Spatial distribution of contributions to the COVID-19 response network, 13 March–20 June 2020.
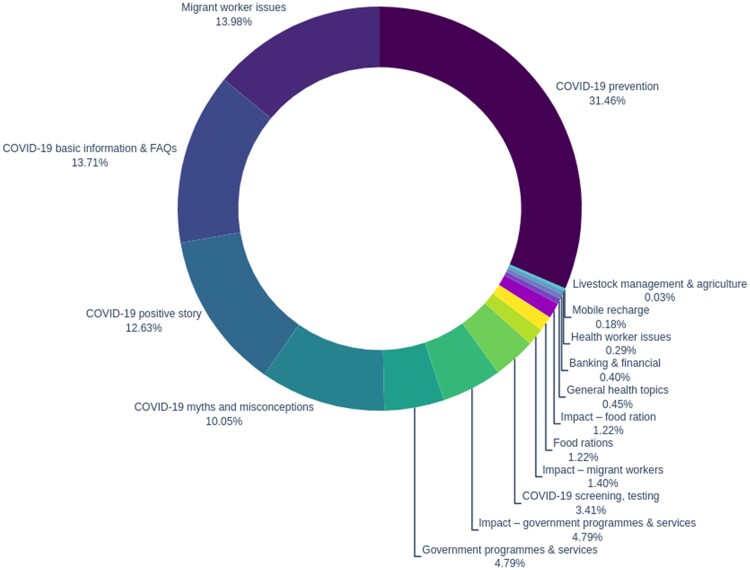
Uptake of SGC
Figure 2 illustrates the relative proportions of themes accessed by listeners in 793 350 SGC calls representing 1 417 276 total minutes heard over the 100-day analysis period. Basic health promotion (COVID-19 prevention, COVID-19 basic information and FAQs, COVID-19 positive story, COVID-19 myths and misconceptions) accounted for 67.91% (961 737 min) of SGC.
Fig. 2:
Thematic analysis of studio-generated content for the COVID-19 response network, 13 March–20 June 2020. Percentages represent the number of minutes heard by category (N = 1 417 276 total minutes).
Analysis of UGC
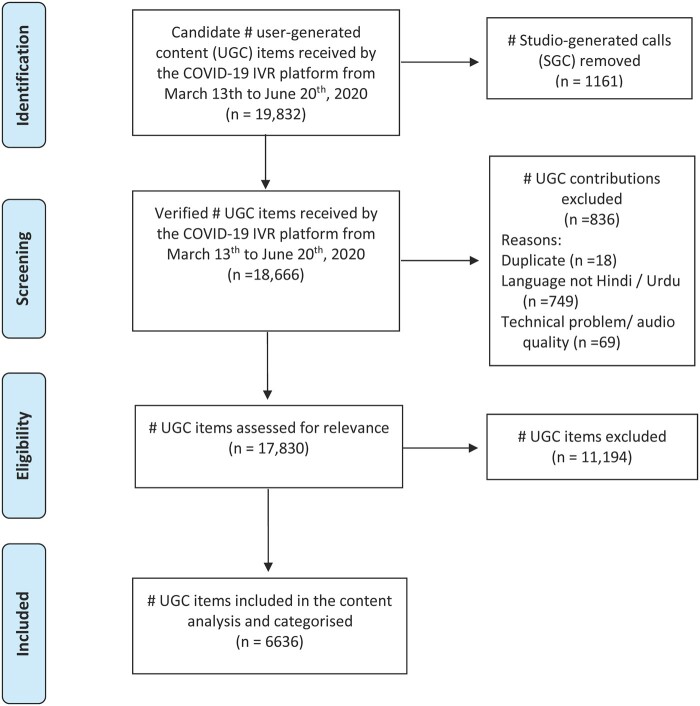
The COVID-19 IVR platform recorded a total of 19 832 UGC items between 13 March and 20 June 2020. Of these, 1161 were miscategorized SGC; these audio files were removed from the data set. Of the 18 666 true user contributions, 836 additional items were excluded for the following reasons: 18 were duplicates, 749 were not in Hindi or Urdu and 69 had a technical or audio quality problem, leaving a total of 17 830 contributions for data screening, extraction, entry and verification. After exclusion of 11 194 non-relevant items, 6636 UGC contributions were retained for analysis. Figure 3 describes the construction of the UGC sample.
Fig. 3:
User-generated contributions included in the content analysis.
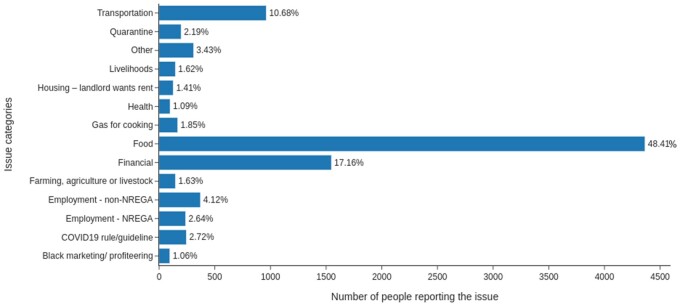
The issues raised by callers to the COVID-19 IVR platform focused overwhelmingly on basic necessities of survival (Figure 4). Analysis of the 6636 UGC contributions reporting 9015 issues found that 48% (4364) recounted shortages of food or problems in accessing food entitlements, 17% (1547) had insufficient funds, were out of cash or faced problems in accessing cash transfer related relief measures initiated by the government, 10% (963) required transport and 8% (755) related concerns about employment or livelihoods. These problems were particularly acute during the first two lockdown phases (Supplementary Figures S4 and S5).
Fig. 4:
Issues raised by callers to the COVID-19 IVR platform, 13 March–20 June 2020.
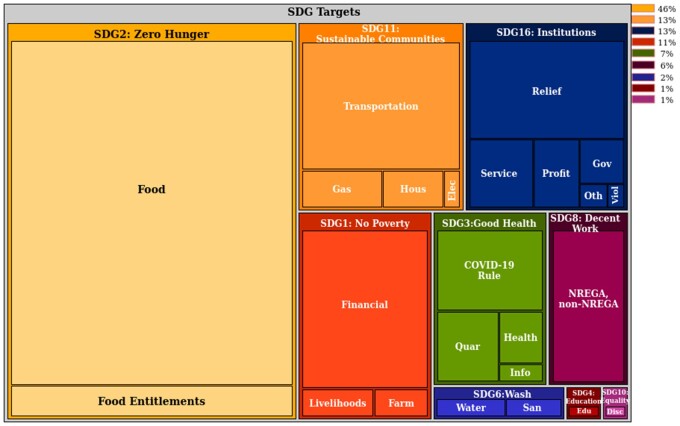
We also mapped issues raised by callers to deficits in attaining the SDGs (Figure 5). Analysis of 6636 UGC contributions representing 18 764 issues related to the SDGs revealed the following top 5 shortfalls: SDG2: zero hunger (48%); SDG1: no poverty (acute financial distress and concerns over livelihoods; 15%); SDG11: sustainable cities and communities (basic living conditions, such as transport, electricity, housing and cooking fuel; 13%); SDG16: peace, justice and strong institutions (problems with corruption and difficulties in accessing government relief measures; 7%); and SDG3: good health and well-being (health issues such as COVID-19 rules or quarantine conditions; 7%). Patterns of SDG deficits differed by gender (Supplementary Figures S6 and S7); for example, female callers expressed more frequent concerns over food shortages.
Fig. 5:
Issues raised by callers categorized according to the UN 2030 Sustainable Development Goals. Elec—electricity; Farm—farming, agriculture or livestock; Gas—Ujjwala yojana—gas for cooking; Gov—local governance (Panchayat); Hous—housing; Profit—black marketing and profiteering/price rises; Relief—relief measures/financial services not working; Viol—violence, domestic or communal.
DISCUSSION
In India, stringent public health measures, including a complete nationwide lockdown, were taken early on in the hopes of slowing the speed of SARS-CoV-2 spread, giving the health system time to adjust, and mitigating harms to the population. On 26 March 2020, at the start of the lockdown, the Government of India additionally announced a range of measures under the Pradhan Mantri Garib Kalyan Yojana (PMGKY, the Prime Minister’s welfare initiative for the poor) to alleviate impending financial hardships that would arise due to the lockdown. Notwithstanding, the lockdown is widely considered to have sparked India’s biggest humanitarian crisis since the country gained independence in 1947. How did this happen, and what can we learn from it?
The data presented in this article were generated through uptake of an emergency response service and did not follow a pre-established sampling design. They constitute a very large convenience sample offering a unique window into this humanitarian crisis from the standpoint of the disenfranchised.
Individuals availing the services of the Gram Vaani COVID-19 response network represent the poorer segments of society, choosing a communications medium that is free of cost and does not require access to the internet, a smartphone or literacy. One of the network’s key functions is to offer basic health promotion for individuals excluded from other information sources. That more than 1 million calls were logged in just 100 days is testimony to the importance of this service, which was a spontaneous and initially self-funded effort of key Indian civil society organizations. While government health promotion focused on communications channels oriented to the middle and elite classes such as television, internet and newspapers, health promotion for the most vulnerable was largely an afterthought.
Audio recordings made by network users spoke of profound distress over struggles to secure the basic necessities of survival. Analysis of these recordings shows that, for a large segment of the Gram Vaani COVID-19 response network callers, stringent public health measures to counter COVID-19 compromised the right to health by threatening its essential determinants and entitlements.
In India, due to a scarcity of jobs in rural areas and growing agrarian distress, an estimated 100 million people are regularly away from their homes, working as labourers in the construction and manufacturing industries in urban industrialized centres of the country. With the sudden announcement of a lockdown, these migrant workers found themselves overnight with no source of income and no means to travel back to their homes (Srivastava, 2020a). They soon ran out of food and cash, and, as revealed by the intensity of SOS cries for help on the Gram Vaani Interactive Voice IVR platforms, the food kits and community kitchens run by the government soon proved inadequate. Many went hungry or undertook perilous journeys on foot or bicycles, to reach their homes hundreds of kilometres away (Ruthven, 2020). Many of these harms, including violations of human rights enshrined in the Indian constitution, could have been substantially mitigated through a better consideration of the needs of the marginalized. We illustrate gaps in three areas:
India’s Public Distribution System (PDS) scheme provides subsidized food and non-food items to poor households. While the government announced doubling of the subsidized food grains distributed via PDS to support the poor whose meagre incomes had been impacted due to the lockdown, many people in rural and urban areas remained excluded. The PDS in India is not yet portable across states, and migrant workers are thus unable to avail these benefits (Srivastava, 2020b). Among non-migrants, an estimated 100 million people are also unable to avail these benefits because they are not enrolled under the PDS, either due to long pending applications, or failed applications due to missing documents, or because they were excluded from the population survey which last happened in 2011 (Special Correspondent, 2020).
The government also announced several cash transfer benefits to aid the poor during the lockdown, but many could not avail these benefits due to implementation failures. We highlight difficulties related to the technological approach adopted to operationalize these transfers. Over the last few years, the use of digital technology and biometric-based authentication has steadily increased as a means for people to access social welfare schemes in India, both for in-kind benefits like PDS, as well as cash transfers directly to people’s bank accounts. Network connectivity issues at bank branches and Point of Service machines for authentication and recording of transactions, transaction failures due to server capacity bottlenecks, inactive bank accounts because of discrepancies in identity documents provided by the people, and a lack of physical banking infrastructure in remote areas for people to be able to withdraw cash, caused many to be needlessly excluded from these programmes and led to significant distress(Gupta et al., 2020; Raghavan, 2020).
The Indian health system, including community health workers who operate in remote areas with underserved populations, was diverted to focus exclusively on COVID-19-related issues such as contact tracing and door-to-door surveys. This came at the cost of routine healthcare delivery, including access for the emergency treatment of physical injuries, suspension of routine immunization sessions, suspension of nutrition programmes for pre-school and school-going children and other health programmes related to chronic conditions such as tuberculosis and diabetes (Population Council Institute, 2020). The disruption of primary health care and nutrition services is expected to have a significant impact on the future health of children and mothers (Roberton et al., 2020).
In ‘Listening as governance’, Indian Nobel prize winning economist and philosopher Amartya Sen describes the need to address the COVID-19 pandemic by strengthening participatory democracy and listening to the poor (Sen, 2020). The experiences of callers to the Gram Vaani COVID-19 response network reveal that it is in fact pre-existing development deficits, such as failures in establishing an effective social safety net, that are driving vulnerability during the COVID-19 crisis.
To build an inclusive recovery, the needs of the marginalized must be placed at the heart of policy design. First, public policy must avoid exacerbating structural drivers of exclusion, inequalities and discrimination. If a sudden and strictly enforced lockdown was required, logistics to ensure provision of essentials such as transport, food and cash, should have been mobilized to help vulnerable groups such as migrant workers and day labourers deal more easily with the situation. Second, as we rebuild institutions, we must reinforce social protection measures and be vigilant about the dangers of wrongful exclusion. During the COVID-19 lockdown, a universalization of benefits such as subsidized food should have been seriously considered as a useful measure to reduce the suffering of the poor, while relying on self-selection by people to keep inclusion errors low (Sen et al., 2020). In planning for the post-pandemic recovery, adequate attention should be paid to reasons for exclusion from social protection benefits, including technology-related failures, and to have clear protocols to handle these cases (Seth, 2020). Moving forward, there is a need for documentation of workers especially in the unorganized sector, as a gateway to ensure access to portable welfare benefits, unemployment benefits, skills-based job matching and employment-based social security such as workplace health insurance (Tiwari, 2020).
The COVID-19 pandemic is both a crisis and an opportunity to reimagine more just institutions and policies. The voices of the marginalized must become central to this dialogue.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Health Promotion International online.
AUTHORS’ CONTRIBUTIONS
Mira Johri: Conceptualization, Methodology, Writing—Original Draft, Funding acquisition; Sumeet Agarwal: Methodology, Writing—Review & Editing; Aman Khullar: Visualization, Formal analysis; Writing—Review & Editing; Dinesh Chandra: Supervision, Data curation, Investigation, Writing—Review & Editing; Vijay Sai Pratap: Project administration, Funding acquisition, Writing—Review & Editing; Aaditeshwar Seth: Conceptualization, Methodology, Writing—Original Draft, Funding acquisition; Gram Vaani Team: Supervision, Investigation, Resources, Software. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplementary Material
ACKNOWLEDGEMENTS
Our sincere thanks to the COVID-19 response network partners, the Tika Vaani team and Gram Vaani Community Media for their extraordinary generosity and dedication.
FUNDING
We gratefully acknowledge the support of the Omidyar Network India (ONI, as part of the COVID19 Rapid Response Funding Initiative) to fund the COVID-19 response network operations, Laudes Foundation, the Bill and Melinda Gates Foundation for top-up funds on project #INV-002938 to extend the scope to COVID-19 relief and awareness efforts and the IC-IMPACTS Innovative Technologies Demonstration Projects initiative for research funding. The study sponsors played no role in study design, in the collection, analysis and interpretation of data, in the writing of the report or the decision to submit the paper for publication.
ETHICS APPROVALS
Research ethics approval for this study was granted by the Institutional Committee for Ethics and Review of Research, Onion Dev Technologies Pvt. Ltd. (No. TV-OS/01-2020).
REFERENCES
- Acharya R., Porwal A. (2020) A vulnerability index for the management of and response to the COVID-19 epidemic in India: an ecological study. The Lancet Global Health, 8, e1142–e1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constitution of India (1950) Government of India Ministry of Law and Justice Legislative Department. https://legislative.gov.in/constitution-of-india Accessed May 10, 2021.
- Das A. (2013) Right to health in India: contemporary issues and concerns. Journal of the National Human Rights Commission, 12, 37-57. [Google Scholar]
- Dhar K. (2012) Domestic Implementation of Human Rights (February 19, 2012). Available at SSRN: https://ssrn.com/abstract=2007967.
- Gupta A., Kumar A., Janani A. P. (2020) Last-mile delivery of PM Garib Kalyan Yojana benefits during the COVID-19 pandemic. In Dvara Research. https://www.dvara.com/research/wp-content/uploads/2020/05/Last-mile-Delivery-of-PM-Garib-Kalyan-Yojana-Benefits-during-the-COVID-19-Pandemic.pdf Accessed May 10, 2021.
- Hale T., Webster S., Petherick A., Phillips T., Kira B. (2020) Oxford COVID-19 government response tracker. www.bsg.ox.ac.uk/covidtracker Accessed July 25, 2020. [DOI] [PubMed]
- India State-Level Disease Burden Initiative Collaborators (2017) Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet, 390, 2437–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacevic M., Jahic A. (2020) COVID-19 and human development: exploring global preparedness and vulnerability. https://datastudio.google.com/reporting/abd4128c-7d8d-4411-b49a-ac04ab074e69/page/QYXLB.
- Landis J. R., Koch G. G. (1977) The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. [PubMed] [Google Scholar]
- Mathiharan K. The fundamental right to health care. Indian Journal of Medical Ethics, [S.l.], v. 11, n. 4, p. 123, nov. 2016. ISSN 0975-5691.. [PubMed] [Google Scholar]
- Office of the Registrar General and Census Commissioner (2014) India: census 2011. New Delhi. http://censusindia.gov.in/pca/cdb_pca_census/Houselisting-housing-UP.html.
- Population Council Institute (2020) Access to RCH services during the COVID-19 crisis: insights from Bihar and Uttar Pradesh. https://www.popcouncil.org/uploads/pdfs/2020PGY_CovidIndiaKAP_RCHServicesBrief.pdf Accessed July 25, 2020.
- Raghavan M. (2020) Transaction failure rates in the Aadhaar enabled Payment System: Urgent issues for consideration and proposed solutions. In Dvara Research. https://www.dvara.com/research/wp-content/uploads/2020/05/Transaction-failure-rates-in-the-Aadhaar-enabled-Payment-System-Urgent-issues-for-consideration-and-proposed-solutions.pdf Accessed May 10, 2021.
- Roberton T., Carter E. D., Chou V. B., Stegmuller A. R., Jackson B. D., Tam Y.. et al. (2020) Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. The Lancet Global Health, 8, e901–e908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruthven O. (2020) Lockdown chronicle: the story of a migrant workers’ platform across India’s lockdown. Agrarian Questions. https://www.aqs.org.uk/lockdown-chronicle-the-story-of-a-migrant-workers-platform-across-indias-lockdown/ Accessed July 25, 2020.
- Sen A. (2020) Listening as governance. The Indian Express, 8 April. https://indianexpress.com/article/opinion/columns/coronavirus-india-lockdown-amartya-sen-economy-migrants-6352132/ Accessed July 25, 2020.
- Sen A., Rajan R., Banerjee A. (2020) Huge numbers may be pushed into dire poverty or starvation…we need to secure them. The Indian Express, 18 July.
- Seth A. (2020) Learning to listen: building an empathetic state. The India Forum, 22 May. https://www.theindiaforum.in/article/learning-listen Accessed July 25, 2020.
- Special Correspondent (2020) Outdated census data deprives over 10 crore of PDS: economists. The Hindu, 15 April.
- Srivastava R. (2020a) Understanding circular migration in India: its nature and dimensions, the crisis under lockdown and the response of the state. New Delhi. http://www.ihdindia.org/Working%20Ppaers/2020/IHD-CES_WP_04_2020.pdf Accessed July 25, 2020.
- Srivastava R. (2020b) Vulnerable internal migrants in India and portability of social security and entitlements. New Delhi. http://www.ihdindia.org/Working%20Ppaers/2020/IHD-CES_WP_02_2020.pdf Accessed July 25, 2020.
- Sustainable Development Goals: Sustainable Development Knowledge Platform (2020) https://sustainabledevelopment.un.org/?menu=1300 Accessed July 25, 2020.
- The Right to Health. Fact sheet no. 31 (2008).
- The World Bank (2020) The World Bank: India overview. https://www.worldbank.org/en/country/india/overview Accessed July 25, 2020.
- Tiwari S. (2020) No documents, no benefits: how India’s invisible workforce is left to fend for itself. India Spend, 21 June. https://www.indiaspend.com/no-documents-no-benefits-how-indias-invisible-workforce-is-left-to-fend-for-itself/ Accessed July 25, 2020.
- United Nations (2015) Transforming our world: the 2030 agenda for sustainable development. http://webcache.googleusercontent.com/search?q=cache:G5YqmceTNJQJ; https://sustainabledevelopment.un.org/post2015/transformingourworld+&cd=1&hl=en&ct=clnk&gl=us Accessed July 25, 2020.
- United Nations (2016) Sustainable development goals: 17 goals to transform our world. http://www.un.org/sustainabledevelopment/hunger/ Accessed July 25, 2020.
- Working Group for Monitoring Action on the Social Determinants of Health (2018) Towards a global monitoring system for implementing the Rio Political Declaration on Social Determinants of Health: developing a core set of indicators for government action on the social determinants of health to improve health equity. International Journal for Equity in Health, 17, 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank (2020) Updated estimates of the impact of COVID-19 on global poverty. https://blogs.worldbank.org/opendata/updated-estimates-impact-covid-19-global-poverty Accessed July 25, 2020.
- World Health Organization (2021) Health financing for universal coverage: what is ‘fiscal space’ and why does it matter? https://www.who.int/health_financing/topics/fiscal-space/why-it-matter/en/ Accessed March 10, 2021.
- World Health Organization Special Programme for Research Development and Research Training in Human Reproduction (2020) Addressing human rights as key to the COVID-19 response (WHO/2019-nCoV/SRH/Rights/2020.1). https://www.who.int/publications-detail/addressing-human-rights-as-key-to-the-covid-19-response?fbclid=IwAR1NKbpOxUCodHvNh4tyRDBAU1WlLGpl7GTDyZFxBZwXMLs_bEpG90HLt0I Accessed July 25, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.