This editorial refers to ‘Early cardiac involvement in patients with acute COVID-19 infection identified by multiparametric cardiovascular magnetic resonance imaging’, by Chen et al. pp. 844–851.
In battle, in a war, a soldier sees only a tiny fragment of what is available to be seen. The soldier is not a photographic machine. He is not a camera. He registers, so to speak, only those few items that he is predisposed to register and not a single thing more. Do you understand this? So I am saying to you that after a battle each soldier will have different stories to tell, vastly different stories, and that when a war is ended it is as if there have been a million wars, or as many wars as there were soldiers.
—Tim O'Brien, Going After Cacciato
The pandemic has ravaged through our lives in so many ways that we readily believe it scars our hearts as well. Patients complain of cardiac symptoms long after recovery, seemingly unrelated to COVID-19 severity.1 Observational cardiac magnetic resonance (CMR) studies have found a plethora of abnormalities with remarkable variation between groups.2–9 The only consistent findings seem to be a paucity of classical myocarditis and no clear relation between abnormalities and symptoms. Pathologic studies showed increased numbers of macrophages in the myocardium of many patients, a high prevalence of thrombotic complications but few cases of lymphocytic myocarditis.10–13
Chen et al.14 add another brick to the house of COVID-19. While previous CMR studies have focused on recovered COVID-19 patients, this is the first CMR study in acute COVID-19 patients. The authors deserve our great respect for putting themselves at risk by scanning patients that are still infectious. From a collective of 120 hospitalized COVID-19 cases, the authors selected 25 patients based on symptoms and clinical findings, thus maximizing pre-test probability of cardiac involvement. The authors further stratified patients by Troponin elevation and compared both groups to age- and sex-matched healthy controls.
Their main findings were:
overall slight impairment of left ventricular systolic function by volumetry and strain analysis (right ventricular function was not assessed),
high prevalence of myocardial oedema on T2-weighted imaging (56%) and T2 mapping,
low prevalence of irreversible focal necrosis (one patient with late gadolinium enhancement), and
patients with elevated Troponin scored worse in all categories.
Out of 120 patients who were sick enough to warrant hospitalization, the authors identified only one case of ‘classical’ myocarditis with focal necrosis. While findings of functional impairment and myocardial oedema warrant follow-up, studies at later intervals post-COVID-19 showed little functional impairment of the left ventricle even in troponin-positive patients.2–9
Open questions remain regarding the specificity of the findings. Transient cardiac dysfunction is apparent in a substantial number of patients with severe infections irrespective of the causative organism.15 Vasodilation and redistribution of fluid into the extracellular space are basic features of our systemic inflammatory response, which might explain elevations in the mapping parameters native T1, T2, and extracellular volume (ECV).16 Most of us have encountered the perils of high-sensitivity troponin in our residency and we are familiar with the concept of ‘type 2 myocardial infarction’, namely a rise in troponin due to causes other than acute coronary artery occlusion. Are we heading in the same direction with high-sensitive CMR, diagnosing ‘type 2 myocarditis’?
The CMR diagnosis of myocarditis relies strongly on the Lake–Louise–Criteria (LLC), which require evidence of both oedema and myocardial damage. While the LLC show good sensitivity and specificity for the detection of acute myocarditis in patients with reasonable clinical suspicion, their diagnostic accuracy for chronical conditions has not been established. Furthermore, the LCC were recently updated to include the mapping-parameters native T1, T2, and ECV.17 T1 and T2 relaxation times of protons are the main determinants of native tissue contrast in magnetic resonance imaging, while the ECV determines uptake of extracellular contrast agents. Modern mapping methods allow direct quantification of these underlying tissue properties, comparable to the Hounsfield-Units in computer tomography. All three parameters are elevated in myocardial oedema and necrosis, whereas T1 and ECV are also elevated in fibrosis.17
While the original LLC required evidence of necrosis or scar on late enhancement imaging, the updated criteria accept elevated native T1 or ECV as a surrogate, effectively expanding the CMR diagnosis of myocarditis to myocardial oedema without myocardial damage. The resulting increase in sensitivity is welcome for well-selected patients with a high pre-test probability of myocarditis and greatly facilitates follow-up. However, this comes at a cost of decreased specificity. Applying the updated LLC to patients with low pre-test probability, especially in the presence of possibly confounding conditions, inevitably increases the number of false positives. It will produce a barrage of unspecific elevations in parameters that check the boxes for myocarditis but might just resemble systemic inflammation. We have yet to understand the prognostic relevance of these findings and their relation to the patients’ symptoms and long-term follow-up data are needed. Furthermore, we need comparisons with patients with other pulmonary and systemic infections to differentiate COVID-19-specific pathology from physiological inflammatory response.
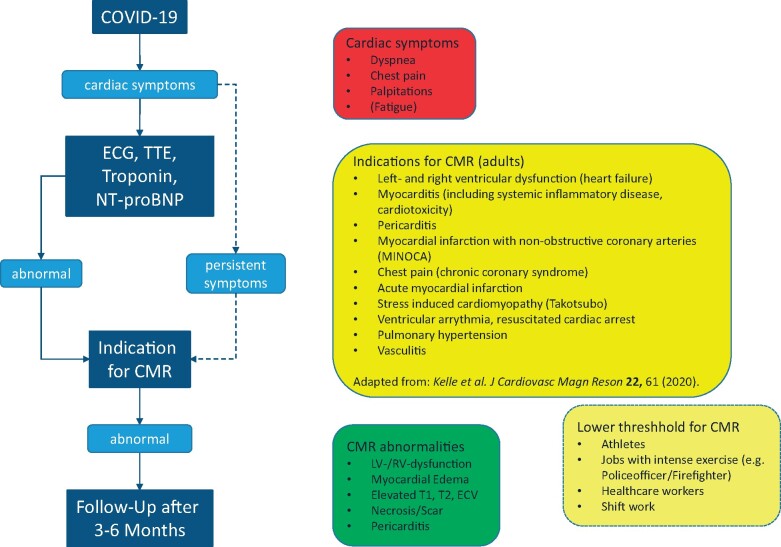
Currently, there is no evidence for routine clinical use of CMR during or after COVID-19 in the absence of symptoms or signs suggestive of a cardiac pathology. In our clinic, we choose a pragmatic, symptom-oriented approach, depicted in Figure 1.18 For certain high-risk occupations, a lower threshold for imaging might be appropriate depending on symptoms and the clinical course. Ultimately, the decision lies on us as clinical cardiologists to use diagnostic procedures wisely as a guide to treatment. As always, diagnostic procedures have harms that we need to weigh against their benefits.
Figure 1.
Recommendation for a symptoms-oriented approach towards CMR in patients with suspected cardiac involvement post COVID-19. CMR, cardiac magnetic resonance; COVID-19, coronavirus infectious disease 2019; ECG, electrocardiogram; LV, left ventricle; NT-proBNP, N-terminal pro-brain natriuretic peptide; RV, right ventricle; T1, T1 relaxation time; T2, T2 relaxation time; TTE, transthoracic echocardiography.
Because COVID-19 is an international disease, we recommend that researchers and clinicians share their anonymized data in international registries to allow for independent assessment of their findings and epidemiological analyses that might shed light on the missing links. As an example for CMR, the Society for Cardiovascular Magnetic Resonance (SCMR) offers a registry with extensive data reporting options (https://scmr.org/page/COVID-19Registry). With mutual collegial assistance, maybe one day our individual fragments will combine to form a comprehensive picture of what COVID-19 does or does not do to our hearts and lead to a better understanding of not just COVID-19-related inflammatory cardiac diseases.
Conflict of interest: P.D. owns stock of Siemens and Bayer. S.K. is the past-Chair of the Advocacy Committee of the Society for Cardiovascular Magnetic Resonance (SCMR) and current member of the SCMR COVID-19 Registry Task Force and is supported by Philips Health Care.
The opinions expressed in this article are not necessarily those of the Editors of EHJCI, the European Heart Rhythm Association or the European Society of Cardiology.
References
- 1. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X. et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021;397:220–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brito D, Meester S, Yanamala N, Patel HB, Balcik BJ, Casaclang-Verzosa G. et al. High prevalence of pericardial involvement in college student athletes recovering from COVID-19. JACC Cardiovasc Imaging 2020;14:541–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Clark DE, Parikh A, Dendy JM, Diamond AB, George-Durrett K, Fish FA. et al. COVID-19 myocardial pathology evaluation in athletes with cardiac magnetic resonance (COMPETE CMR). Circulation 2021;143:609–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C. et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging 2020;13:2330–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J. et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020;5:1265–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP. et al. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol 2021;6:116–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Starekova J, Bluemke DA, Bradham WS, Eckhardt LL, Grist TM, Kusmirek JE. et al. Evaluation for myocarditis in competitive student athletes recovering from coronavirus disease 2019 with cardiac magnetic resonance imaging. JAMA Cardiol 2021; Jan 14;e207444. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Martinez MW, Tucker AM, Bloom OJ, Green G, DiFiori JP, Solomon G. et al. Prevalence of inflammatory heart disease among professional athletes with prior COVID-19 infection who received systematic return-to-play cardiac screening. JAMA Cardiol 2021; Mar 4;e210565. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G. et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J 2021;42(19):1866–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Basso C, Leone O, Rizzo S, De Gaspari M, van der Wal AC, Aubry MC. et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J 2020;41:3827–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Halushka MK, Vander Heide RS.. Myocarditis is rare in COVID-19 autopsies: cardiovascular findings across 277 postmortem examinations. Cardiovasc Pathol 2021;50:107300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lindner D, Fitzek A, Brauninger H, Aleshcheva G, Edler C, Meissner K. et al. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol 2020;5:1281–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Edler C, Schroder AS, Aepfelbacher M, Fitzek A, Heinemann A, Heinrich F. et al. Dying with SARS-CoV-2 infection-an autopsy study of the first consecutive 80 cases in Hamburg, Germany. Int J Legal Med 2020;134:1275–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen B-C, Shi N-N, Wu C-W, An D-A, Shi Y-X, Wesemann LD. et al. Early cardiac involvement in patients with acute COVID-19 infection identified by multiparametric cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging 2021;3:Mar 4;jeab042.online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beesley SJ, Weber G, Sarge T, Nikravan S, Grissom CK, Lanspa MJ. et al. Septic cardiomyopathy. Crit Care Med 2018;46:625–34. [DOI] [PubMed] [Google Scholar]
- 16. Merx MW, Weber C.. Sepsis and the heart. Circulation 2007;116:793–802. [DOI] [PubMed] [Google Scholar]
- 17. Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U. et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol 2018;72:3158–76. [DOI] [PubMed] [Google Scholar]
- 18. Kelle S, Bucciarelli-Ducci C, Judd RM, Kwong RY, Simonetti O, Plein S. et al. Society for Cardiovascular Magnetic Resonance (SCMR) recommended CMR protocols for scanning patients with active or convalescent phase COVID-19 infection. J Cardiovasc Magn Reson 2020;22:61. [DOI] [PMC free article] [PubMed] [Google Scholar]