Abstract
We reviewed publicly available data from major US health jurisdictions to compare severe acute respiratory syndrome coronavirus 2 case fatality rates in people experiencing homelessness with the general population. The case fatality rate among people experiencing homelessness was 1.3 times (95% CI, 1.1–1.5) that of the general population, suggesting that people experiencing homelessness should be prioritized for vaccination.
Keywords: case fatality rate, COVID-19, homelessness, public health surveillance
People experiencing homelessness (PEH) are highly vulnerable to coronavirus disease 2019 (COVID-19) due to numerous factors including increased risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exposure and infection. Lacking permanent shelter, PEH are less able to mitigate exposures through social distancing, often living doubled-up with friends and family, in crowded shelter facilities, or in densely populated encampments. Preventing infection may be challenging for PEH, as access to high-quality masks may be limited and inconsistent access to running water impedes hand hygiene. Throughout the pandemic, health authorities have reported high seroprevalence among PEH [1] and large outbreaks at homeless shelters and encampments [2–4]. Relatedly, research has linked evictions to community-level COVID-19 risk [5].
Once infected, PEH may be at elevated risk of COVID-19 morbidity and mortality. Homelessness takes a dramatic toll on health, with life expectancies among the chronically homeless estimated to be as low as 42–52 years [6]. Weathering homelessness means that PEH develop age-related health problems decades earlier than their housed counterparts [7, 8]. Many of these conditions may increase risk for severe COVID-19 illness and death. For example, the prevalence of chronic obstructive pulmonary disease among PEH is 2–3 times that of the general population [8, 9]. Based on this underlying risk, a modeling study projected that 4% of the US homeless population would require hospitalization due to COVID-19 and that nearly 1% would die [10].
Despite substantial vulnerability to COVID-19 among PEH, few data exist to gauge the impact of homelessness on COVID-19 outcomes. We reviewed publicly available data in US health jurisdictions to compare case fatality rates among PEH with population-wide case fatality rates.
METHODS
We queried publicly available online data from government websites of public health agencies with jurisdiction over the 25 most populous US counties, the 25 most populous US cities (n = 12 additional), and the most populous city in each state (n = 39 additional) to identify PEH-specific COVID-19 case and mortality data. We included data from March 1, 2020, to February 28, 2021.
If PEH-specific data were available, we extracted the most recent cumulative case and death counts for PEH, as well as jurisdiction-wide case and death counts. Where possible, we also extracted data by age.
Statistical Analysis
For each jurisdiction, we calculated PEH case fatality rates (CFRs; defined as deaths per 100 cases) and jurisdiction-wide CFRs and compared these via relative risk (a ratio of PEH CFR over jurisdiction-wide CFR). We summarized CFRs and relative risk estimates across all jurisdictions as a population-weighted average. For jurisdictions with age-stratified data, we calculated age-specific CFRs and relative risk.
Patient Consent
All analyses were based on publicly available, aggregate data collected by jurisdictions through routine public health surveillance. For this reason, our study is not considered human subjects research and was exempted from institutional review board review and from requirements to obtain written consent.
RESULTS
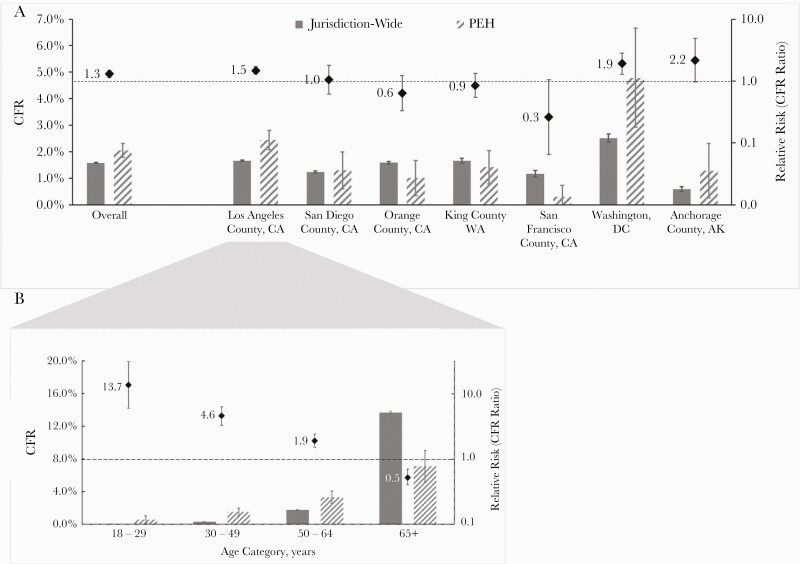
Of the 76 jurisdictions reviewed, 7 (9.2%) included data on PEH. In these jurisdictions the CFR for PEH ranged from 0.3% to 4.8%, compared with the jurisdiction-wide CFRs, which ranged from 0.6% to 2.5% (relative risks ranged from 0.3% to 2.2%) (Figure 1A). Across jurisdictions, the overall CFR was 2.1% (95% CI, 1.8%–2.3%) among PEH and 1.6% (95% CI, 1.6%–1.6%) for the general population (relative risk, 1.3%; 95% CI, 1.1%–1.5%).
Figure 1.
COVID-19 case fatality in US health jurisdictions: PEH vs jurisdiction-wide March 1, 2020–February 28, 2021. CFRs for each jurisdiction and age category appear on the primary (left) y-axis, with estimates for PEH appearing in solid gray bars and jurisdiction-wide estimates appearing in hatched gray. The relative risk (ratio of PEH vs jurisdiction-wide CFR) appears on the secondary (right) y-axis, represented via forest plot. Abbreviations: CFR, case fatality rate; COVID-19, coronavirus disease 2019; PEH, people experiencing homelessness.
Only Los Angeles County stratified PEH data by age (Figure 1B). CFRs were significantly increased for PEH under 65 compared with the county population, with relative risks of 13.7% (95% CI, 6.0%–31.1%), 4.6% (95% CI, 3.3%–6.3%), and 1.9% (95% CI, 1.5%–2.4%) for 18–29, 30–49, and 50–64-year-olds, respectively. Among adults aged 65 and over, this trend was reversed, with a relative risk of 0.5% (95% CI, 0.4%–0.7%).
DISCUSSION
We identified few jurisdictions reporting on COVID-19 among PEH; however, among jurisdictions that did report these data, PEH with COVID-19 had a 30% higher risk of death than the overall population. This increased risk was especially pronounced in younger age groups. Our findings underscore the need to prioritize PEH for COVID-19 prevention interventions, including vaccination.
Despite expanded COVID-19 vaccine eligibility throughout the United States, PEH are at risk of being left behind in settings implementing appointment-based vaccination at hospitals, pharmacies, and mass vaccination centers. Leveraging homeless outreach and health care personnel to offer vaccines to PEH in encampments and shelters will prevent COVID-19 morbidity and mortality while promoting health equity. In addition to promoting vaccination, interventions such as isolation and quarantine rooms, along with more permanent housing options for PEH, should be central to discussions of pandemic mitigation moving forward.
We found substantial heterogeneity in case fatality and CFR ratios across jurisdictions, likely reflecting local differences in COVID-19 dynamics, surveillance and testing practices, homeless services, PEH living conditions (eg, crowding, indoor vs outdoor), and reporting. Careful evaluation of local COVID-19 prevention and control programs is important to identify effective strategies to reduce the burden of COVID-19 in PEH. Interestingly, we found that PEH cases >65 years had a lower risk of COVID-19 mortality than cases in Los Angeles’ overall >65 population. The most likely explanation for this finding is survivor bias: on average, PEH who survive to age 65 without shelter may be less frail than older adults in the general population. Given low life expectancy among PEH [6], we also hypothesize differing age distributions, with fewer PEH aged ≥80. Importantly, however, older PEH remained at substantially elevated mortality risk compared with younger PEH.
There are several limitations to our study. Because so few jurisdictions published PEH-specific data and all but 1 of these jurisdictions were on the West Coast, the generalizability of our estimates may be limited. As available PEH data were rarely disaggregated, we were not able to account for underlying differences such as age structure in our comparisons of PEH vs jurisdiction-wide cases. Additionally, PEH status is prone to misclassification and differential classification across jurisdictions. Specifically, we expect that PEH not accessing homeless services would be misclassified as not PEH. Furthermore, screening programs by homeless services and health departments may increase detection of mild COVID-19 cases and asymptomatic SARS-CoV-2 infections among PEH compared with the general population. Finally, deaths from substance use represent a substantial competing risk in our study. In particular, fentanyl-involved deaths have increased leading up to and during the COVID-19 pandemic, disproportionately rising among PEH [11, 12]. Importantly, these limitations would likely lead to underestimation of the degree to which homelessness increases COVID-19 case fatality, strengthening our conclusion that PEH are a highly vulnerable population in need of effective interventions to prevent COVID-19.
Only 7 of 76 jurisdictions reviewed published data on COVID-19 among PEH, likely because housing status is not routinely collected as part of public health surveillance. The paucity of COVID-19 data specific to PEH represents a limitation not just for our study, but for public health surveillance as a whole. Disaggregated data allow for development of targeted public health interventions that prioritize high-risk populations for case finding and public health interventions such as vaccination. Moreover, these data allow for monitoring of health inequities, documenting the degree to which PEH are disproportionately burdened by COVID-19. Moving forward, it is essential that data on homelessness be made available to understand the degree to which structural failures such as insufficient housing have compromised US pandemic preparedness. Routinely collecting housing status as part of disease surveillance may pose logistical challenges in some jurisdictions; however, we see this as an important step for the control of COVID-19 and other infectious diseases in this high-risk and underserved population.
CONCLUSIONS
As COVID-19 vaccines bring new signs of hope, we urge public agencies to prioritize PEH for vaccination and other public health interventions. Past outbreaks and seroprevalence studies have shown that exposure and infection risk are extremely high among PEH. Our analyses suggest that COVID-19 may also be particularly deadly for this population, independent of age. By prioritizing PEH for interventions, public health agencies can prevent deaths, promote health equity, and reduce community transmission of COVID-19 in many of the country’s hardest hit cities [13].
Acknowledgments
Financial support. K. M. Leifheit was supported by postdoctoral training grant number T32HS000046 from the Agency for Healthcare Research and Quality (AHRQ).
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ.
Potential conflicts of interest. K.M.L., L.H.C., J.A.M., and R.N.W. have no conflicts of interest or financial disclosures to declare. C.L.S. was previously employed as a contractor with the Los Angeles County Department of Public Health, a health jurisdiction included in our analysis. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Author contributions. K.M.L. and C.L.S. conceived, designed, and performed the analysis. K.M.L., J.A.M., R.N.W., and C.L.S. collected the data. K.M.L., L.H.C., and C.L.S. prepared an original draft of the paper. J.A.M. and R.N.W. reviewed and edited the paper. C.L.S. supervised and provided project administration.
References
- 1. Roederer T, Mollo B, Vincent C, Nikolay B. Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: a cross-sectional study. Lancet Public Heal 2021; 6:E202–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maxmen A. Coronavirus is spreading under the radar in US homeless shelters. Nature 2020; 581:129–30. [DOI] [PubMed] [Google Scholar]
- 3. Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA 2020; 323:2191–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Imbert E, Kinley PM, Scarborough A, et al. . Coronavirus disease 2019 outbreak in a San Francisco homeless shelter. Clin Infect Dis. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Leifheit KM, Linton SL, Raifman J, et al. . Expiring eviction moratoriums and COVID-19 incidence and mortality. Am J Epidemiol 2021. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. O’Connell J. Premature Mortality in Homeless Populations: A Review of the Literature. Nashville: National Health Care for the Homeless Council, Inc., 2005. [Google Scholar]
- 7. Adams J, Rosenheck R, Gee L, Seibyl CL, Kushel M. Hospitalized younger: a comparison of a national sample of homeless and housed inpatient veterans. J Health Care Poor Underserved 2007; 18:173–84. [DOI] [PubMed] [Google Scholar]
- 8. Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric syndromes in older homeless adults. J Gen Intern Med 2012; 27:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Snyder LD, Eisner MD. Obstructive lung disease among the urban homeless. Chest 2004; 125:1719–25. [DOI] [PubMed] [Google Scholar]
- 10. Culhane D, Treglia D, Steif K, et al. . Estimated emergency and observational/quarantine capacity need for the US homeless population related to COVID-19 exposure by county; projected hospitalizations, intensive care units and mortality. 2020. Available at: https://endhomelessness.org/wp-content/uploads/2020/03/COVID-paper_clean-636pm.pdf. Accessed 1 March 2021. [Google Scholar]
- 11. Shover CL, Falasinnu TO, Dwyer CL, et al. . Steep increases in fentanyl-related mortality west of the Mississippi River: recent evidence from county and state surveillance. Drug Alcohol Depend 2020; 216:108314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Los Angeles County Department of Public Health Center for Health Impact Evaluation. Recent trends in mortality rates and causes of death among people experiencing homelessness in Los Angeles County.2021. Available at: http://www.publichealth.lacounty.gov/chie/reports/HomelessMortality2020_CHIEBrief_Final.pdfA. Accessed 1 March 2021.
- 13. Bibbins-Domingo K, Petersen M, Havlir D. Taking vaccine to where the virus is—equity and effectiveness in coronavirus vaccinations. JAMA Heal Forum 2021; 2:e210213. [DOI] [PubMed] [Google Scholar]