Abstract
Purpose:
Delirium occurs frequently in critically ill children, with highest rates reported in children under five years of age. The objective of this study was to measure the residual effect of delirium on quality of life at one- and three-months after hospital discharge.
Methods:
In this prospective observational cohort study, all children were screened for delirium (using the Cornell Assessment for Pediatric Delirium) throughout their stay in the pediatric intensive care unit (PICU). Quality of life was measured using the Infant-Toddler Quality of Life questionnaire (IT-QOL) at three time-points: baseline, 1-month, and 3-months after hospital discharge. IT-QOL scores were compared between children who did and did not develop delirium.
Results:
207 children were enrolled. 122 completed the 1-month follow-up, and 117 completed the 3-month follow-up. Fifty-six children (27%) developed delirium during their PICU stay. At follow-up, IT-QOL scores for the PICU cohort overall were consistently lower than age-related norms. When analyzed by delirium status, children who had experienced delirium scored lower in every QOL domain when compared to children who did not experience delirium. Even after controlling for severity of illness, delirious patients demonstrated an average 11-point lower general health score than non-delirious patients (p=0.029).
Conclusion:
This pilot study shows an independent association between delirium and decreased quality of life after hospital discharge in young children.
Keywords: pediatric delirium, quality of life, outcomes, critical care, phenotype
Tweet:
Delirium has residual effects on quality of life in children under five years of age that can persist up to 3 months after ICU discharge.
Background
Delirium is a neuropsychiatric syndrome with decompensation of cerebral functioning and temporary disruption of neuronal pathways, which results from a serious underlying medical condition or side-effects of treatment (1,2). Delirium has been recognized as a major public health problem in adults, with a prevalence as high as 87% in high-risk critically ill populations (3–5). Delirium in adults is associated with increased mortality, prolonged hospital stay, post-discharge morbidity, neurocognitive diminution, and a decline in health-related quality of life (3,6–11).
Similar concern has been raised regarding children (12). Research demonstrates that greater than 25% of children in the pediatric intensive care unit (PICU) are affected by delirium, and that delirium may be independently associated with excess mortality (13–19). However, the long-term consequences of pediatric delirium have not been broadly investigated and there is a lack of rigorous assessment of post-discharge outcomes in PICU survivors.
A critically-ill child is often subjected to multiple procedures, exposed to sedating medication, and at risk for delusional imagery and altered thinking (17,20,21). The experience of delirium during critical illness may therefore prevent children and their families from returning to their normal activities, and expose them to ongoing worries and altered expectations for the future. The child may also have subtle lingering perceptual-motor and behavior impairments that persist after the acute delirium resolves (22,23). Therefore, we hypothesized that delirium would adversely impact the quality of life of the child and family members in the three months after hospital discharge. The primary objective of this study was to explore the effect of delirium, with respect to quality of life and adaptive behavior, at one month after discharge in children less than five years of age. A secondary objective was to explore the possible lingering effects of delirium up to three months after hospital discharge.
Methods
Study Design:
This is a prospective longitudinal cohort study, including all patients under the age of five years at time of admission to the PICU at New York-Presbyterian-Weill Cornell Medical Center. Only children of caregivers who did not speak English or Spanish were excluded from the study. Caregivers were approached in the PICU by study coordinators, typically 24-hours after admission, and invited to participate. Informed consent was obtained. This study was approved by the Institutional Review Board at Weill Cornell Medical College, and was performed in accordance with ethical standards.
Baseline Data Collection:
After informed consent was obtained, caregivers were asked to complete the Infant-Toddler Quality of Life Questionnaire (IT-QOL). The IT-QOL was designed for use in children two-months to five-years of age and is well-validated in both healthy children and those with chronic disease (24). A short form (ITQOL-SF47) was published in 2013 and is reliable, valid, and precise. It measures physical function, growth and development, bodily pain, temperament and moods, behavior, and general health perceptions. It also includes a parent-specific scale to assess emotional and time impact of the child’s status on the caregiver’s needs. It consists of 47 items scored on a Likert-type scale, which are converted into a 0 (worst health) to 100 (best health) continuum (25). Domain scores for eight scales were analyzed in this study. The scales consisted of the Physical Abilities Scale (PA), the Satisfaction with Overall Growth and Development Scale (GD), the Discomfort and Pain Scale (BP), the Temperament and Mood Scale (TM), the Combined Behavior Scale (CBE), the General Health Perceptions Scale (GH), the Parent Impact-Emotional Scale (PE), and the Parent Impact-Time Scale (PT). Caregivers were asked to answer the IT-QOL questions to reflect how their child was behaving prior to the acute illness that led to the hospitalization, in order to provide a benchmark assessment.
In-Hospital Data Collection:
All patients in the PICU at New York Presbyterian Hospital-Weill Cornell Medical College are screened for delirium twice daily by nurses, as standard of care, using the validated Cornell Assessment of Pediatric Delirium (CAPD) (26). The CAPD is a rapid, 8-item observational tool, recommended by the European Society of Pediatric and Neonatal Intensive Care (ESPNIC) for routine use by the bedside nurse to reliably detect delirium in all critically ill children (27). The operational definition of delirium for this study was a positive CAPD (score of nine or higher) at any time during the PICU stay. The CAPD has been shown to be consistent with the gold-standard psychiatric diagnosis of delirium, even in extremely young children (28,29). In addition to twice-daily delirium scores, other demographic and clinical information was extracted from the electronic medical record, including age, gender, admitting diagnosis, and severity of illness (as scored by the Pediatric Index of Mortality III [PIM3]) (30).
Post-Discharge Data Collection:
At one- and three-months after hospital discharge, parents were contacted via email and asked to repeat the IT-QOL questionnaire. They were given a secure link created by REDCap, a web-based application used to manage surveys and data (31). They were instructed to have the same caregiver fill out the IT-QOL survey each time to maintain consistency. As an incentive to complete the follow-up surveys, caregivers were given a reloadable debit card upon enrollment, and five dollars were added to the card with each survey completed.
Statistical Analyses
Children were divided into two groups: ever delirious vs. never delirious. Data are described as N (%), mean (sd), or median (IQR), by delirium status. Demographic characteristics and baseline ITQOL domain scores were compared between patients who did and did not develop delirium in the PICU by Chi-squared/Fisher’s Exact tests or independent two-sample t-tests, as appropriate. IT-QOL domain scores in the entire cohort were compared to norms validated by the IT-QOL research team (32). Domain scores at one-month and three-months after hospital discharge were analyzed similarly. Severity of illness was calculated by the probability of mortality generated by the PIM3 score upon PICU admission. Because of the skewed distribution, PIM3 scores were dichotomized as above or below the median. Multivariable linear regressions modeling one-month IT-QOL domain scores were constructed with ever delirious as the primary predictor, controlling for severity of illness. All p-values were two-sided with statistical significance evaluated at the 0.05 alpha level. Analyses were performed in R version 3.5.0 (Vienna, Austria).
Results
207 children were enrolled in this study, and completed the baseline IT-QOL. 122 families (59%) completed the 1-month survey, and 117 families (57%) completed the 3-month follow-up survey.
See Table I for demographics of the included population. In brief, median age was 13 months (IQR 5–29 months), and 59% were male. The most common admitting diagnosis category was respiratory insufficiency/failure (59%), and the mean probability of mortality on admission was 3% (SD 9%). Forty-seven percent of the cohort was exposed to opiates, 29% to benzodiazepines, and 80% to anticholinergics. Only 5% of the children received neuroleptics.
Table I:
Subject Demographics and Delirium Status
| Overall (n=207) | Delirium (n=56) | No delirium (n=151) | p-value | |
|---|---|---|---|---|
| Age (months; median, IQR) | 13 (5–29) | 12 (3–32) | 14 (6–29) | 0.27 |
| Gender (n, %): | ||||
| Male | 121 (59%) | 36 (64%) | 85 (56%) | 0.38 |
| Female | 86 (41%) | 20 (36%) | 66 (44%) | |
| Diagnosis categories (n, %): | ||||
| Respiratory insufficiency/failure | 121 (59%) | 28 (50%) | 93 (62%) | 0.058 |
| Neurologic disease | 44 (21%) | 12 (21%) | 32 (21%) | |
| Cardiac disease | 19 (9%) | 10 (18%) | 9 (6%) | |
| Infectious/inflammatory | 14 (7%) | 3 (5%) | 11 (7%) | |
| Renal/Metabolic | 4 (2%) | 0 (0%) | 4 (3%) | |
| Hematologic/Oncologic | 3 (1%) | 2 (4%) | 1 (1%) | |
| Other | 2 (1%) | 1 (2%) | 1 (1%) | |
| Severity of Illness*(mean, SD) | 3% (SD 9%) | 6% (SD 17%) | 1% (SD 2%) | 0.024 |
as defined by the Paediatric Index of Mortality III probability of mortality score.
Fifty-six children (27%) developed delirium. Median duration of delirium was three days, with an interquartile range of 1–5 days. With respect to delirium subtype, eleven percent of days with delirium were characterized as hyperactive, 48% were hypoactive, and 40% were mixed. Most children with delirium experienced more than one delirium subtype throughout their ICU stay. No child experienced only hyperactive delirium, and only 5% experienced purely hypoactive delirium. Delirium resolved in all subjects prior to PICU discharge. There were no significant differences in age or gender between children who did and did not develop delirium. In bivariate analysis, children with higher severity of illness upon admission (defined by PIM3 score) were more likely to become delirious (p=0.024) (Table I).
IT-QOL scores at pre-hospital baseline were no different between children who did and did not go on to develop delirium. At one-month follow-up, the domain scores for the PICU cohort overall were consistently lower than the age-related norms (Table II). When analyzed by delirium status, children who had experienced delirium scored lower in every domain when compared to children who did not experience delirium (Figure 1). The children with purely hypoactive delirium had lower IT-QOL scores than the children with mixed-type delirium, but this difference did not achieve statistical significance.
Table II:
Quality of Life Scores at 1 month after hospital discharge
| IT-QOL domains | US Norms (mean) | PICU cohort (baseline, n=207) | 1-mo follow-up (no delirium, n=94) |
1-mo follow-up (yes delirium, n=28) |
|---|---|---|---|---|
| PA | 96 | 84 | 85 | 76 |
| GD | 95 | 86 | 88 | 75* |
| BP | 83 | 70 | 77 | 69 |
| TM | 83 | 75 | 77 | 69* |
| CBE | 77 | 74 | 74 | 64* |
| GH | 78 | 59 | 56 | 47* |
| PE | 90 | 68 | 69 | 51* |
| PT | 93 | 79 | 77 | 58* |
Scores reported as means. Legend: IT-QOL= Infant Toddler Quality of Life Questionnaire; PICU = pediatric intensive care unit; PA=physical abilities; GD=satisfaction with growth and development; BP=bodily pain; TM=temperament and mood; CBE=combined behavior/getting along; GH=general health perceptions; PE=parent impact/emotional; PT=parent impact/time. *p<0.05
Figure 1:
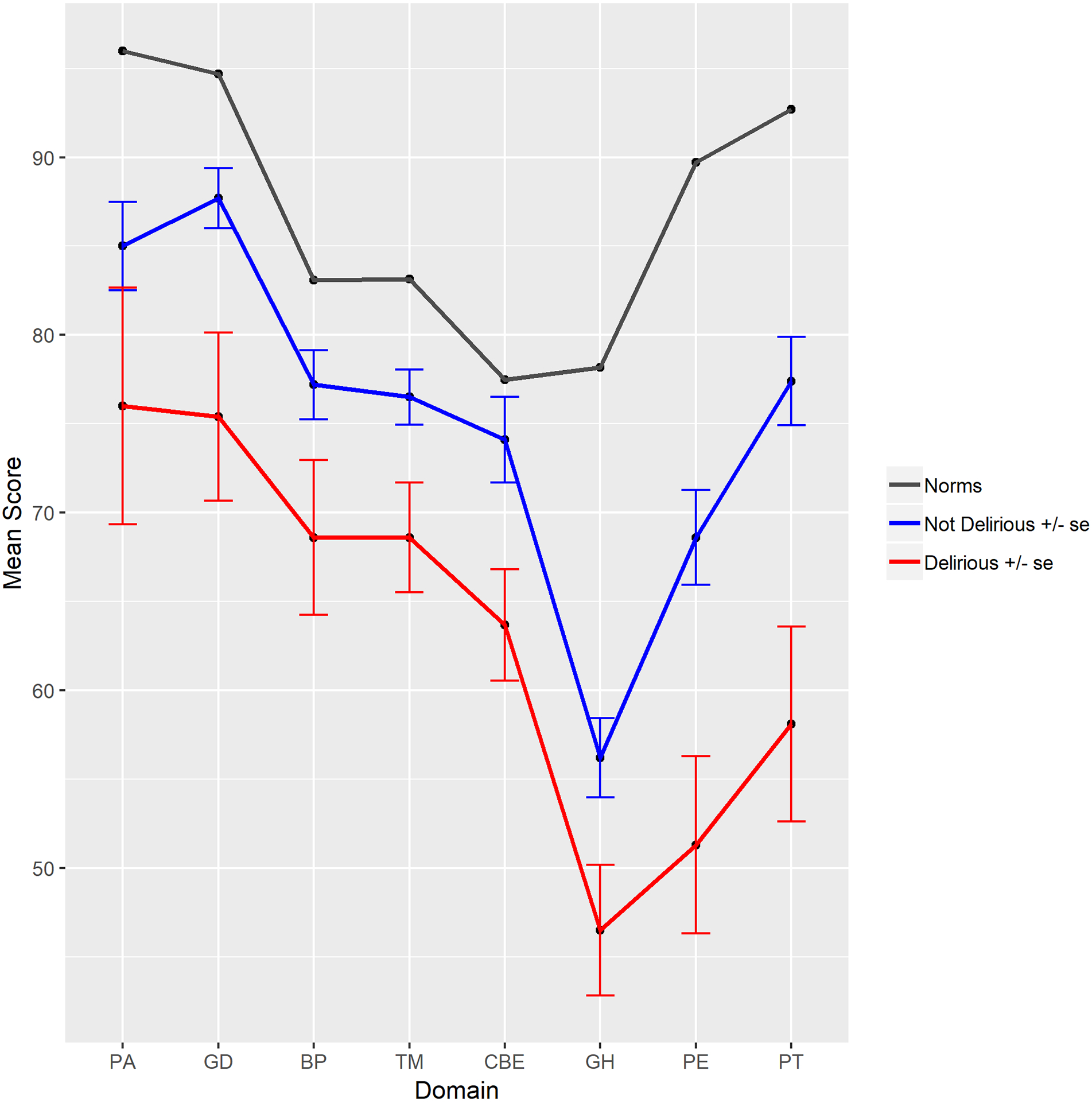
Quality of life scores were significantly lower at one-month after hospital discharge in the cohort of children who experienced delirium during their stay in the pediatric intensive care unit.
(Scores reported as means. Domains as defined by the Infant-Toddler Quality of Life (IT-QOL) Questionnaire: PA=physical abilities; GD=satisfaction with growth and development; BP=bodily pain; TM=temperament and mood; CBE=combined behavior/getting along; GH=general health perceptions; PE=parent impact/emotional; PT=parent impact/time. See text for details).
In multivariable analyses, after controlling for severity of illness, adjusted scores for delirious patients remained significantly lower in six out of eight domains. As an example, children who experienced delirium during their hospitalization demonstrated an average 11-point lower GH score than non-delirious patients one-month after discharge (p=0.029). It is notable that scores were also lower on the parent-related domains (assessing emotional impact and time impact) in children who experienced delirium (Figure 2).
Figure 2:
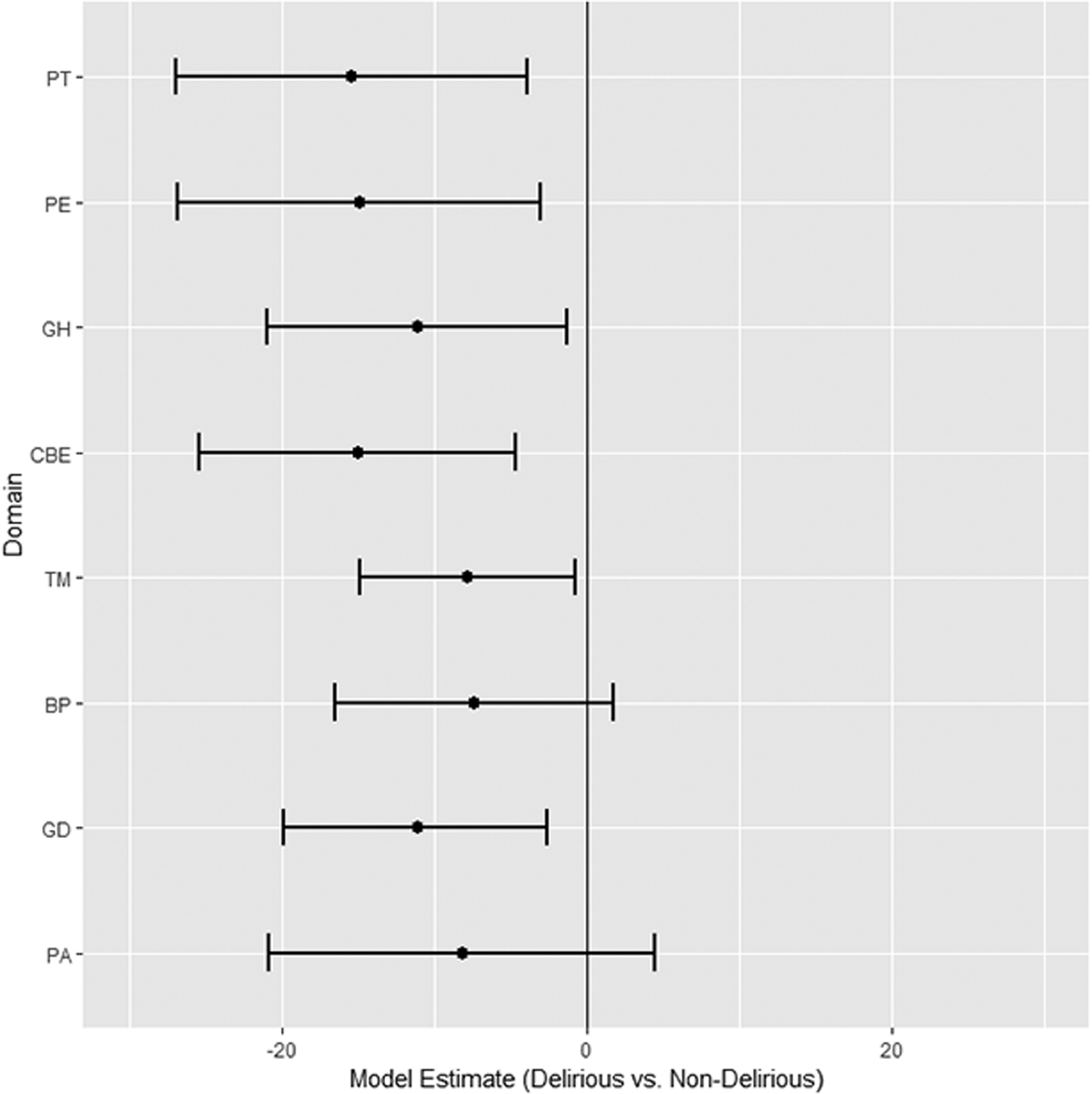
In multivariable analysis, quality of life was significantly lower in most domains for the cohort of children who experienced delirium.
(X-axis represents estimates and confidence limits for each domain score at 1-month after discharge, after adjusting for severity of PICU illness. Y-axis represents IT-QOL domains as defined in the text).
Three-month follow-up data was available for 117 children. Again, when analyzed by delirium status, children who had been diagnosed with delirium during the PICU stay scored lower in every IT-QOL domain when compared to children who were not diagnosed with delirium (Table III).
Table III:
Quality of Life Scores at 3 months after hospital discharge
| IT-QOL domains | 3-mo follow-up (no delirium, n=88) |
3-mo follow-up (yes delirium, n=29) |
|---|---|---|
| PA | 84 | 83 |
| GD | 84 | 78 |
| BP | 76 | 72 |
| TM | 77 | 74 |
| CBE | 73 | 67 |
| GH | 55 | 47 |
| PE | 72 | 67 |
| PT | 82 | 70* |
Scores reported as means. Legend: IT-QOL= Infant Toddler Quality of Life Questionnaire; PICU = pediatric intensive care unit; PA=physical abilities; GD=satisfaction with growth and development; BP=bodily pain; TM=temperament and mood; CBE=combined behavior/getting along; GH=general health perceptions; PE=parent impact/emotional; PT=parent impact/time. *p<0.05
Discussion
Delirium is a frequent complication of pediatric critical illness, especially prevalent in children less than five years of age (15). Pediatric delirium has been independently associated with excess mortality, and in-hospital morbidity, but little is known about the longer-term effects of delirium on PICU survivors, and the contribution of delirium to Post Intensive Care Syndrome in pediatrics (PICS-p) (14,33,34). Fortunately, emerging research has shown that pediatric delirium is preventable, and treatable (35,36).
Consistent with prior research, our data demonstrate that PICU survivors overall have lower quality of life scores when compared to age-adjusted norms (23,37). However, this study is the first to explore the contribution of delirium to this measured decrement in QOL. Since young children are in a vital period of developmental maturation, we hypothesized that they may be exceptionally vulnerable to the disruption of normal cognition and awareness posed by delirium (29,38). In adults, delirium has been independently associated with residual impairments in QOL up to six-months after hospital discharge (9,10). Similarly, this study demonstrated a consistent decrease in QOL measures in young children who experienced delirium. Importantly, the parents’ general health perception of the children with delirium remained substantially lower at one-month after hospital discharge– even after controlling for severity of illness during the PICU stay. Adjusted scores were an average of 11 points less, which is not merely statistically significant, but also clinically meaningful. Although this study was not powered for further multivariable analyses, the data at three months after discharge continue to trend in the hypothesized direction, suggesting that the effect of delirium on young children may persist long after the delirium itself resolves.
However, it is important not to assume a causal relationship in this observational pilot study. Although the data demonstrate an association between pediatric delirium and QOL after PICU discharge, it is possible that delirium is merely a marker for children who are already more vulnerable to poor outcomes – in effect, the stress of the critical illness unmasks those children with least reserve, and these children present with delirium. But if this were the case, we would expect lower QOL scores at baseline for those children who would go on to develop delirium. However, baseline IT-QOL scores were not statistically different between the cohort of children who did and did not develop delirium. Therefore, it is possible that delirium itself may have a direct negative effect on long-term QOL in PICU patients. Further research will be necessary to explore this relationship.
This study demonstrated that delirium affected not just the child, but also the parent. There is a growing body of research looking at the reciprocal processes involved with parent-child functioning (39,40). It is possible that the measured decrement in the child’s QOL and behavior placed an additional emotional and time burden on the parent. On the other hand, it is conceivable that witnessing the child’s delirium in-and-of-itself negatively impacted the parent. The frightening experience of seeing the child’s altered mental status may have provoked greater anxiety in the caregiver, which could result in an altered perception of the child’s health and vulnerability. An anxious parent may further affect the child’s QOL and behavior after discharge. Future research will be necessary to better delineate the complex interplay between delirium, parent, and child outcomes.
This study has some noteworthy limitations. Baseline data was obtained from the parent after the child had already been admitted to the PICU. This presents the possibility of recall bias, as the parent’s answers may have been influenced by the child’s acute illness, and could result in falsely lower baseline scores. To mitigate against this possibility, parents were asked to complete the initial IT-QOL questionnaire soon after PICU admission (within 24–48 hours). There is also the risk of selection bias – perhaps this study selected for children with poor outcomes, as parents whose children were still not completely recovered from their PICU stay may have been more likely to take the time to complete the follow-up questionnaires. However, there were no statistically significant differences when comparing the demographics of the patients lost to follow-up with the larger cohort. Lastly (and most importantly), this pilot study is limited by a relatively small sample size, restricting the ability to control for multiple confounders that may affect quality of life in PICU survivors (especially medication exposure and psychological health of parent), or to analyze the differential effects of delirium subtype and/or duration on outcomes. Nevertheless, it is compelling that delirious children consistently demonstrated lower mean scores after discharge at both time points and across all eight domains.
Conclusion
Critically ill children under five years of age are at high risk for developing delirium. This pilot study shows an association between delirium and decreased quality of life after hospital discharge, after controlling for severity of illness while in the PICU. Further research is necessary to define the lingering effects of delirium on PICU survivors in order to target interventions to optimize recovery and improve long-term health in these vulnerable young children.
Take-Home Message:
Delirium has a measurable impact on post-discharge quality of life in children under five years of age. Delirium may contribute to Post-Intensive Care Syndrome in young children.
Financial support:
This research was supported, in part, by the Department of Pediatrics at Weill Cornell Medical Center, as well as the Clinical Translational Science Center, grant number UL1-TR000457-06.
Compliance with ethical standards:
Dr. Traube received support for article research from the National Institutes of Health. None of the other authors have any potential conflicts of interest to disclose. This research was approved by the Institutional Review Board at Weill Cornell Medical College. Informed consent was obtained from all participants.
Footnotes
Name of Institution where the work was performed:
NY Presbyterian Hospital, Weill Cornell Medical College
References
- 1.Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. American Psychiatric Association; 2013. [Google Scholar]
- 2.Salluh JIF, Sharshar T, Kress JP. Does this patient have delirium? Intensive Care Med. 2017. May;43(5):693–5. [DOI] [PubMed] [Google Scholar]
- 3.Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intensive Care Unit. Crit Care Med. 2013. January;41(1):278–80. [DOI] [PubMed] [Google Scholar]
- 4.Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2006. November 11;33(1):66–73. [DOI] [PubMed] [Google Scholar]
- 5.Dubois MJN|Dumont M|Dial S|Skrobik Y. Delirium in an intensive care unit: a study of risk factors. Intensive Care Med. 2001;27(8):1297–304. [DOI] [PubMed] [Google Scholar]
- 6.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. Jama. 2004;291(14):1753–1762. [DOI] [PubMed] [Google Scholar]
- 7.Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010. July;38(7):1513–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basinski JR, Alfano CM, Katon WJ, Syrjala KL, Fann JR. Impact of Delirium on Distress, Health-Related Quality of Life, and Cognition 6 Months and 1 Year after Hematopoietic Cell Transplant. Biol Blood Marrow Transplant. 2010. June;16(6):824–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duppils GS, Wikblad K. Cognitive Function and Health-Related Quality of Life After Delirium in Connection With Hip Surgery: A Six-Month Follow-Up. Orthop Nurs. 2004. May;23(3):195–203. [DOI] [PubMed] [Google Scholar]
- 10.Kim S-Y, Kim J-M, Kim S-W, Kang H-J, Lee J-Y, Bae K-Y, et al. Perceived Stigma and Quality of Life in Patients Following Recovery From Delirium. J Clin Psychiatry. 2017. August 23;78(7):e744–9. [DOI] [PubMed] [Google Scholar]
- 11.Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001. December;27(12):1892–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schieveld JN, Janssen NJ. Delirium in the Pediatric Patient: On the Growing Awareness of Its Clinical Interdisciplinary Importance. JAMA Pediatr. 2014;168(7):595–596. [DOI] [PubMed] [Google Scholar]
- 13.Traube C, Silver G, Reeder RW, Doyle H, Hegel E, Wolfe HA, et al. Delirium in Critically Ill Children: An International Point Prevalence Study. Crit Care Med. 2017. April;45(4):584–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Traube C, Silver G, Gerber LM, Kaur S, Mauer EA, Kerson A, et al. Delirium and Mortality in Critically Ill Children: Epidemiology and Outcomes of Pediatric Delirium. Crit Care Med. 2017. May;45(5):891–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith HAB, Gangopadhyay M, Goben CM, Jacobowski NL, Chestnut MH, Savage S, et al. The Preschool Confusion Assessment Method for the ICU: Valid and Reliable Delirium Monitoring for Critically Ill Infants and Children. Crit Care Med. 2016. March;44(3):592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyburg J, Dill M-L, Traube C, Silver G, von Haken R. Patterns of Postoperative Delirium in Children. Pediatr Crit Care Med. 2017. February;18(2):128–33. [DOI] [PubMed] [Google Scholar]
- 17.Patel AK, Biagas KV, Clarke EC, Gerber LM, Mauer E, Silver G, et al. Delirium in Children After Cardiac Bypass Surgery. Pediatr Crit Care Med. 2017. February;18(2):165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alvarez RV, Palmer C, Czaja AS, Peyton C, Silver G, Traube C, et al. Delirium is a Common and Early Finding in Patients in the Pediatric Cardiac Intensive Care Unit. J Pediatr. 2018. April;195:206–12. [DOI] [PubMed] [Google Scholar]
- 19.Dervan LA, Di Gennaro JL, Farris RWD, Watson RS. Delirium in a Tertiary PICU: Risk Factors and Outcomes. Pediatr Crit Care Med. 2019. September;1. [DOI] [PubMed] [Google Scholar]
- 20.Colville G, Kerry S, Pierce C. Children’s Factual and Delusional Memories of Intensive Care. Am J Respir Crit Care Med. 2008. May;177(9):976–82. [DOI] [PubMed] [Google Scholar]
- 21.Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ, Needham DM. Posttraumatic Stress Disorder in Critical Illness Survivors: A Metaanalysis. Crit Care Med. 2015. February;1. [DOI] [PubMed] [Google Scholar]
- 22.Schieveld JNM, van Tuijl S, Pikhard T. On Nontraumatic Brain Injury in Pediatric Critical Illness, Neuropsychologic Short-Term Outcome, Delirium, and Resilience*. Crit Care Med. 2013. April;41(4):1160–1. [DOI] [PubMed] [Google Scholar]
- 23.Colville GA, Pierce CM. Children’s Self-Reported Quality of Life After Intensive Care Treatment*: Pediatr Crit Care Med. 2013. February;14(2):e85–92. [DOI] [PubMed] [Google Scholar]
- 24.Raat H, Landgraf JM, Oostenbrink R, Moll HA, Essink-Bot M-L. Reliability and validity of the Infant and Toddler Quality of Life Questionnaire (ITQOL) in a general population and respiratory disease sample. Qual Life Res. 2007. April;16(3):445–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landgraf JM, Vogel I, Oostenbrink R, van Baar ME, Raat H. Parent-reported health outcomes in infants/toddlers: measurement properties and clinical validity of the ITQOL-SF47. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2013. April;22(3):635–46. [DOI] [PubMed] [Google Scholar]
- 26.Traube C, Silver G, Kearney J, Patel A, Atkinson TM, Yoon MJ, et al. Cornell Assessment of Pediatric Delirium: A Valid, Rapid, Observational Tool for Screening Delirium in the PICU. Crit Care Med. 2014. March;42(3):656–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris J, Ramelet A-S, van Dijk M, Pokorna P, Wielenga J, Tume L, et al. Clinical recommendations for pain, sedation, withdrawal and delirium assessment in critically ill infants and children: an ESPNIC position statement for healthcare professionals. Intensive Care Med. 2016. June;42(6):972–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silver G, Kearney J, Traube C, Atkinson TM, Wyka KE, Walkup J. Pediatric delirium: Evaluating the gold standard. Palliat Support Care. 2014. April 24;1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silver G, Kearney J, Traube C, Hertzig M. Delirium screening anchored in child development: The Cornell Assessment for Pediatric Delirium. Palliat Support Care. 2014. August 15;1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Straney L, Clements A, Parslow RC, Pearson G, Shann F, Alexander J, et al. Paediatric Index of Mortality 3: An Updated Model for Predicting Mortality in Pediatric Intensive Care*. Pediatr Crit Care Med. 2013. September;14(7):673–81. [DOI] [PubMed] [Google Scholar]
- 31.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. April;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.HealthActCHQ. Child Health Questionnaire Scoring and Interpretation Manual. 2013. HealthActCHQ Inc., Boston MA USA. [Google Scholar]
- 33.Manning JC, Pinto NP, Rennick JE, Colville G, Curley MAQ. Conceptualizing Post Intensive Care Syndrome in Children—The PICS-p Framework: Pediatr Crit Care Med. 2018. February;1. [DOI] [PubMed] [Google Scholar]
- 34.Spentzas T Long-Term Sequelae of Pediatric Delirium: Pediatr Crit Care Med. 2019. March;20(3):307–8. [DOI] [PubMed] [Google Scholar]
- 35.Simone S, Edwards S, Lardieri A, Walker LK, Graciano AL, Kishk OA, et al. Implementation of an ICU Bundle: An Interprofessional Quality Improvement Project to Enhance Delirium Management and Monitor Delirium Prevalence in a Single PICU. Pediatr Crit Care Med. 2017. June;18(6):531–40. [DOI] [PubMed] [Google Scholar]
- 36.Groves A, Traube C, Silver G. Detection and Management of Delirium in the Neonatal Unit: A Case Series. Pediatrics. 2016. March;137(3):e20153369. [DOI] [PubMed] [Google Scholar]
- 37.Ebrahim S, Singh S, Hutchison JS, Kulkarni AV, Sananes R, Bowman KW, et al. Adaptive Behavior, Functional Outcomes, and Quality of Life Outcomes of Children Requiring Urgent ICU Admission*: Pediatr Crit Care Med. 2013. January;14(1):10–8. [DOI] [PubMed] [Google Scholar]
- 38.Silver GH, Kearney JA, Kutko MC, Bartell AS. Infant delirium in pediatric critical care settings. Am J Psychiatry. 2010;167(10):1172–1177. [DOI] [PubMed] [Google Scholar]
- 39.Briegel W, Greuel J, Stroth S, Heinrichs N. Parents’ Perception of Their 2–10-Year-Old Children’s Contribution to The Dyadic Parent-Child Relationship in Terms of Positive and Negative Behaviors. Int J Environ Res Public Health. 2019. January;16(7):1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yan N, Ansari A. Child Adjustment and Parent Functioning: Considering the Role of Child Driven Effects. J Fam Psychol JFP J Div Fam Psychol Am Psychol Assoc Div 43. 2016. April;30(3):297–308. [DOI] [PMC free article] [PubMed] [Google Scholar]


