We read with great interest the interesting and timely paper by Nedelcu et al. [1]. Although we share the authors’ conclusions, a 4-week interval between a coronavirus disease 2019 (COVID-19) infection and bariatric surgery is probably not safe. Herein, we report 2 cases of unexpected and asymptomatic pulmonary abnormalities discovered during the preoperative assessment of patients with recent infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
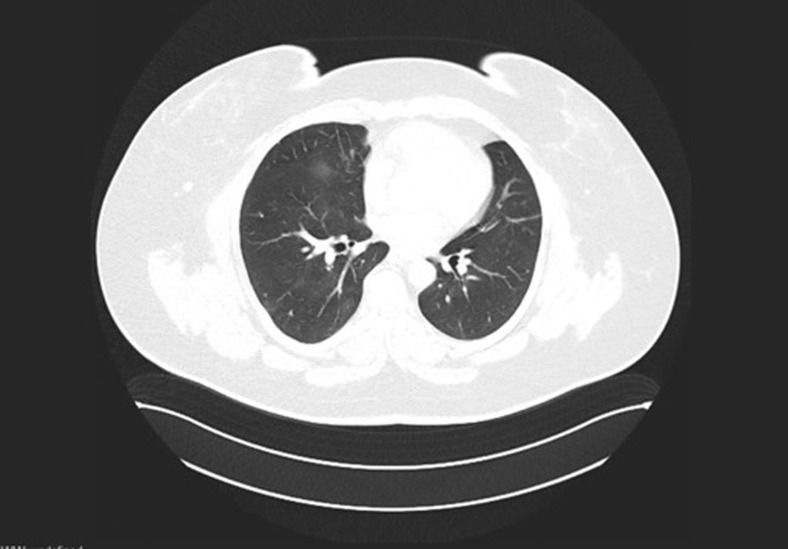
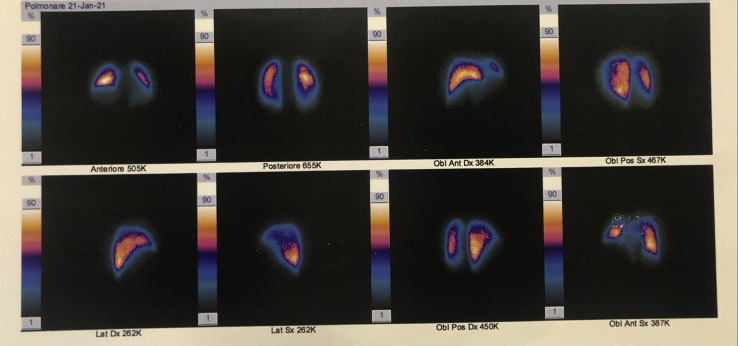
The first patient was a female aged 44 years with a body mass index (BMI) of 47.7 kg/m2 with laparoscopic adjustable gastric band scheduled for removal and conversion to 1-anastomosis gastric bypass/mini gastric bypass (OAGB/MGB). Unfortunately, the patient was diagnosed with a COVID-19 infection and the intervention had to be cancelled. She did not develop severe clinical symptoms (only mild fever and cough) and did not start any therapy. A nasopharyngeal swab tested negative after 10 days and she was rescheduled for surgery after an interval of 2 months. A preoperative chest computed tomography (CT) angiography (Fig. 1 ) showed sequelae of bilateral pneumonia with ground glass opacities; a CT with ventilation/perfusion scintigraphy demonstrated multiple areas of hypoperfusion bilaterally (Fig. 2 ) with signs of thrombo-embolism.
Fig. 1.
Preoperative chest computed tomography angiography of patient number 1.
Fig. 2.
Preoperative computed tomography with ventilation/perfusion scintigraphy of patient number 1.
The second case was a male patient aged 46 years with a BMI of 60.8 kg/m2 scheduled for an OAGB/MGB. The patient had a COVID-19 infection 3 months before the planned surgery, with bilateral pneumonia requiring oxygen therapy and azithromycin by mouth. However, admission to a hospital was not required. Symptoms resolved in 10 days and a nasopharyngeal swab tested negative after 20 days. The subject was rescheduled for surgery at 3 months after complete recovery, but a preoperative chest CT showed residual bilateral abnormalities.
Even if 30-day morbidity and mortality rates following bariatric surgery did not change during the COVID-19 epidemic [2], asymptomatic patients may present focal unilateral or diffuse bilateral opacities that progress within 1–3 weeks.
Patients with a recent history of symptomatic or asymptomatic COVID-19 infection that are scheduled for bariatric surgery should undergo a full preoperative pulmonary evaluation with chest CT angiography [3]. Adequate therapy with low–molecular weight heparin is recommended to avoid risks of intraoperative desaturation and postoperative thromboembolism.
References
- 1.Nedelcu M., Marx L., Lutfi R.E. Bariatric surgery in patients with previous COVID-19 infection. Surg Obes Relat Dis. 2021;17(7):1244–1248. doi: 10.1016/j.soard.2021.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singhal R., Tahrani A.A., Ludwig C., Mahawar K. GENEVA collaborators. Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinol. 2021;9(1):7–9. doi: 10.1016/S2213-8587(20)30375-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navarra G., Komaei I., Currò G. Bariatric surgery and the COVID-19 pandemic: SICOB recommendations on how to perform surgery during the outbreak and when to resume the activities in phase 2 of lockdown. Updates Surg. 2020;72(2):259–268. doi: 10.1007/s13304-020-00821-7. [DOI] [PMC free article] [PubMed] [Google Scholar]