Abstract
Purpose
We compared a restrictive fluid management strategy to usual care among critically ill patients with acute kidney injury (AKI) who had received initial fluid resuscitation.
Methods
This multicenter feasibility trial randomized 100 AKI patients 1:1 in seven ICUs in Europe and Australia. Restrictive fluid management included targeting negative or neutral daily fluid balance by minimizing fluid input and/or enhancing urine output with diuretics administered at the discretion of the clinician. Fluid boluses were administered as clinically indicated. The primary endpoint was cumulative fluid balance 72 h from randomization.
Results
Mean (SD) cumulative fluid balance at 72 h from randomization was − 1080 mL (2003 mL) in the restrictive fluid management arm and 61 mL (3131 mL) in the usual care arm, mean difference (95% CI) − 1148 mL (− 2200 to − 96) mL, P = 0.033. Median [IQR] duration of AKI was 2 [1–3] and 3 [2–7] days, respectively (median difference − 1.0 [− 3.0 to 0.0], P = 0.071). Altogether, 6 out of 46 (13%) patients in the restrictive fluid management arm and 15 out of 50 (30%) in the usual care arm received renal replacement therapy (RR 0.42; 95% CI 0.16–0.91), P = 0.043. Cumulative fluid balance at 24 h and 7 days was lower in the restrictive fluid management arm. The dose of diuretics was not different between the groups. Adverse events occurred more frequently in the usual care arm.
Conclusions
In critically ill patients with AKI, a restrictive fluid management regimen resulted in lower cumulative fluid balance and less adverse events compared to usual care. Larger trials of this intervention are justified.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00134-021-06401-6.
Keywords: Acute kidney injury, Critically ill, Fluid balance, Restrictive fluid management
Take-home message
| Among critically ill patients with acute kidney injury, a fluid restrictive management regimen as compared to usual care led to a lower cumulative fluid balance after 72 h from randomization. Adverse events were more frequent in the usual care arm. |
Introduction
Many critically ill patients develop acute kidney injury (AKI). AKI is associated with an increased risk of adverse outcomes [1, 2]. Current management of AKI remains supportive and includes optimization of hemodynamics and fluid status, avoidance of nephrotoxins [3] and, in severe cases, renal replacement therapy (RRT) [1, 2]. Novel therapies are being evaluated in cardiac surgical [4] and septic patients [5], but no specific pharmacological therapies for general intensive care unit (ICU) patients are currently available.
While fluid therapy is the traditional cornerstone of AKI prevention and treatment [6], patients with AKI are also especially prone to develop fluid overload [7]. Such fluid overload is associated with increased mortality [7–11] and progression of AKI [12, 13]. Thus, a more restrictive fluid management approach among adequately resuscitated patients with AKI might improve outcomes by reducing congestion and improving kidney and other organ function. Notably, a feasibility trial in septic shock patients comparing restrictive fluid resuscitation versus usual care reported a lower risk of worsening of AKI in the restrictive group [14].
Trials among general ICU patients [15], or those with sepsis [14, 16] or acute respiratory distress syndrome (ARDS) [17] have found various fluid restrictive strategies to be safe. Among patients undergoing major abdominal surgery, however, restrictive intra- and post-operative fluid resuscitation and management compared to usual care increased the risk of AKI [18]. Thus, research investigating the role of restrictive fluid management specifically in critically ill patients with AKI has been identified as a research priority [3, 19, 20]. To date, such trials have not been performed.
Accordingly, we conducted a multinational, unblinded, randomized, controlled, feasibility pilot trial comparing a restrictive fluid management (RFM) regimen to usual care among ICU patients with AKI to study the feasibility of such intervention in terms of separation, safety, and compliance. We tested the hypothesis that the proposed RFM regimen would lead to a lower cumulative fluid balance at 72 h post-randomization.
Methods
Trial design
We conducted an investigator-initiated, multicenter, unblinded, randomized, controlled, parallel pilot feasibility study (clinicaltrials.gov identifier NCT03251131) in five European and two Australian ICUs. The trial protocol and statistical analysis plan were published prior to completion of data collection [21]. In each participating site, the trial was approved by the relevant research ethics committee prior to commencing screening. Depending on local practices and ethics approval, we obtained written informed consent either prior to enrollment from patient or proxy, or alternatively a deferred consent with written informed consent obtained from patient or proxy as soon as possible. If consent was not granted or withdrawn, approval of using data collected that far was sought. Trial was performed according to the Declaration of Helsinki and its later amendments.
We randomized patients to either RFM or usual care using an electronic platform with allocation ratio of 1:1. Severity of AKI (stage 1 vs stage 2 or 3 according to the Kidney Diseases: Improving Global Outcomes (KDIGO) criteria [3]) and presence of clinical signs of fluid accumulation (defined by peripheral pitting edema and/or positive fluid balance with P/F ratio less than 200 mmHg) served as stratification variables. We used permuted blocks of varying size (2–4). Due to the nature of intervention, only the statistician conducting the data analysis remained blinded to treatment allocation.
Patients
We included patients who (1) were 18 years or older and admitted to critical care with an arterial line in place, (2) were in critical care for at least 12 but no more than 72 h (3) had AKI but were not receiving RRT, (4) were judged by the treating clinician not to be hypovolemic, and (5) were likely to remain in critical care for 48 h after randomization.
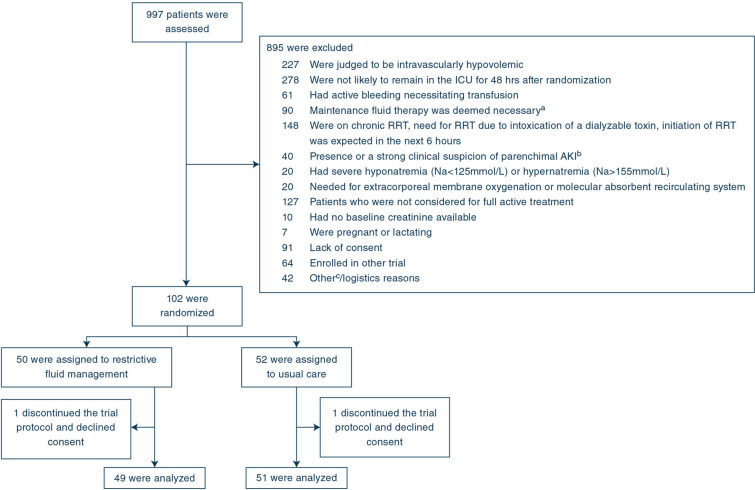
We defined AKI according to the following criteria: (1) increase in plasma creatinine 1.5 times or more above baseline without a decline of 27umol/L or more from the last preceding measurement and/or (2) overall urine output less than 0.5 ml/kg/h (or 6 ml/kg) for the previous 12 h. Exclusion criteria are listed in Fig. 1. The Electronic Supplementary Material (ESM) Tables S1 and S2 present detailed definitions of the eligibility criteria.
Fig. 1.
Flowchart of trial patients. ICU intensive care unit, RRT renal replacement therapy. a Diabetic ketoacidosis, non-ketotic coma, severe burns or other clinical reason determined by the medical staff. b Glomerulonephritis, vasculitis, acute interstitial nephritis, or post-renal obstruction. c Including two exclusion criteria that were removed in a protocol amendment in April 2018 (1) Metformin-induced lactic acidosis or acute liver failure (n = 8) (2) AKI stage 2 or greater is known to have been present for > 48 h (n = 14). These criteria were amended to clarify the exclusion criteria
Interventions
The trial intervention (RFM) consisted of a bundle of treatment recommendations for clinicians treating the trial patients. The overall aim was to reach negative fluid balance on the days following randomization. These recommendations included, first, restricting total daily fluid input only to medications and nutritional fluids (enteral or parenteral) and blood products (if clinically necessary). Second, use of maintenance intravenous fluids was permitted only if enteral nutrition was not tolerated and parenteral nutrition contraindicated. Third, fluid bolus therapy could be given as clinically deemed necessary. Fourth, matching fluid output (with unrestricted use of diuretics) to fluid input whenever possible to achieve a preferably negative cumulative fluid balance but always less than 300 mL/day. Fifth, if the fluid balance target could not be achieved by such means, consideration of RRT to remove the required fluid. Commencing RRT was not mandated in the trial and, if RRT was not considered clinically desirable, the protocol indicated acceptance of a less than targeted fluid balance temporarily (for 24 h) up to 900 mL.
In the usual care group, fluid management was at the discretion of the treating clinical team.
Fluid balance was calculated by subtracting total fluid output (urine output, losses to drains, losses from gastrointestinal tract, ultrafiltration by RRT) from total fluid input (intravenous and oral). Insensible losses were not considered. The intervention period was 7 days from randomization or until ICU discharge whatever occurred first.
Outcomes
The primary outcome was cumulative fluid balance at 72 h after randomization adjusted for stratification variables [21, 22]. Secondary outcomes included duration of AKI in days defined by the KDIGO creatinine and urine output criteria (truncated at ICU discharge or 14 days whichever came first), number of patients requiring RRT (truncated at 14 days, including initiation of RRT after ICU discharge), cumulative fluid balance at 24 h after randomization and at ICU discharge (or truncated at 7 days if ICU stay exceeded 7 days), and cumulative dose of diuretics (furosemide) during the intervention period (while in the ICU, maximum of 7 days) adjusted for the duration of the observation period.
Exploratory outcomes included days free of mechanical ventilation and alive at 14 days, days free of vasopressors and alive at 14 days, days free of ICU and alive at 14 days, days free of RRT and alive (assessed at 90 days), 90-days dialysis dependence and 90-days mortality. The safety and feasibility outcomes included the number of patients with one or more (serious) adverse events (AE) and reactions in both arms (detailed definitions are provided in Table S3), screened versus recruited patients ratio, recruitment rate (patients/center/month), and protocol compliance (number of patients with protocol violations in both arms).
Statistical analysis
Details of statistical analysis plan have been published [21]. We estimated that 50 patients per arm would be required to show a difference of 1200 mL in the primary outcome between treatment arms with a two-sided alpha of 0.05 and power exceeding 80%. Based on unpublished data among AKI patients in the FINNAKI study [1], we estimated that cumulative fluid balance at 72 h would be 2700 mL in the usual care group, and thus 1500 mL in the fluid restrictive group (both with a SD of 2000 mL).
We performed the primary analysis on the intention-to-treat (ITT) population defined as all randomized subjects with consent to use data in the analysis. An additional sensitivity analysis was conducted in the per-protocol population, defined as the ITT population after exclusion of subjects who experienced protocol violation(s) or stayed in the ICU for less than 48 h post-randomization.
The primary, secondary, and exploratory outcomes were adjusted for the stratification variables [22] (mild vs severe AKI and presence/absence of clinical signs of fluid accumulation) using two-tailed logistic regression (dichotomous outcomes) or a linear model (continuous outcome variables, mean or median regression model). We report risk ratios (RR) with 95% confidence intervals (CIs) or difference in means/median with 95% CIs.
We used Shapiro–Wilk test for continuous variables to assess assumption of normality. We set the statistical significance to 0.05 and report two-sided P values. Analyses were conducted using R statistical software version 3.6.2 and SPSS 24.
Results
Patients
Between October 2017 and January 2020, we screened 997 patients and randomized 102 patients. One patient in each group declined consent leaving 100 patients for analysis. Randomization occurred at a median [IQR] 30.7 [20.4–46.2] hours after ICU admission. Forty-nine patients (49%) were assigned to the RFM arm and 51 (51%) to the usual care arm. Figure 1 presents the patient flow. Further, two patients in the RFM arm and three patients in usual care arm withdrew consent and their data obtained until withdrawal were included in the analysis.
Patient baseline characteristics and status at randomization were well-balanced (Table 1). The most frequent reasons for ICU admission were cardiac arrest (8.2%), septic shock (7.2%), and gastrointestinal perforation/rupture (7.2%). Suspected etiology of AKI was multifactorial in 55 (55%) patients. Table S5 presents the observed AKI risk factors.
Table 1.
Patient characteristics
| Characteristic | Restrictive fluid management (n = 49) |
Usual care (n = 51) |
|---|---|---|
| Age, median [IQR], years | 71 [60–77] | 64.5 [56.2–74] |
| Male sex, n (%) | 30 (62.5) | 36 (70.6) |
| Body mass index, median [IQR], kg/m2 | 25.6 [22.8–29.5] | 26.4 [22.7–31.1] |
| Hypertension, n (%) | 26 (54.2) | 32 (65.3) |
| Diabetes, n (%) | 24 (50) | 33 (66) |
| Chronic heart failure, n (%) | 6 (12.5) | 7 (14) |
| Coronary artery disease, n (%) | 9 (18.8) | 16 (31.4) |
| Chronic obstructive pulmonary disease, n (%) | 8 (16.7) | 14 (27.5) |
| Chronic kidney disease, n (%) | 5 (10.6) | 6 (11.8) |
| Chronic liver disease, n (%) | 4 (8.3) | 3 (5.9) |
| Surgical ICU admission, n (%) | 22 (44.9) | 20 (40) |
| Emergency ICU admission, n (%) | 37 (75.5) | 41 (82) |
| Time from hospital admission to ICU admission, median [IQR], days | 1 (0.1–4) | 0.9 (0.2–2.9) |
| Time from ICU admission to randomization, median [IQR], h | 33.3 (21.4–45.9) | 30 (20.3–46) |
| Data at randomization | ||
| AKI inclusion criteria | ||
| Creatinine | 25 (51) | 28 (54.9) |
| Urine output | 10 (20.4) | 8 (15.7) |
| Creatinine and urine output | 14 (28.6) | 15 (29.4) |
| SAPS II score, median [IQR]a | 41.5 [31.3–51.5] | 43 [30–50] |
| SOFA score, median [IQR]b | 9 [8–11] | 9 [7–11] |
| AKI stage 2 to 3 (stratification), n (%) | 31 (63.3) | 33 (64.7) |
| Fluid overload present (stratification), n (%)c | 21 (42.9) | 22 (43.1) |
| Respiratory supportmechanical ventilation, n (%) | 24 (49) | 33 (66) |
| Vasoactives, n (%) | 30 (61.2) | 37 (72.5) |
| Sepsis, n (%) | 27 (55.1) | 30 (58.8) |
| Septic shock, n (%) | 5 (10.2) | 9 (17.7) |
| Cumulative fluid balance from ICU admission to randomization, mean (SD), mL | 2437 (2103) | 1982 (2434) |
The number of missing data is presented in Table S4 in the Electronic Supplementary Material
AKI acute kidney injury, SAPS simplified acute physiology score, SOFA sequential organ failure assessment
aData of one or several SAPS II score subcomponents were missing from 11 patients in the RFM group and 15 in the usual care group. Their scores are omitted here
bThe hepatic subcomponent score was assumed to be 0 in those 4 in RFM group and 3 in the control group with missing bilirubin values
cDefinition of the stratification variable: presence of peripheral pitting edema and/or positive fluid balance with P/F ratio less than 200 mmHg
Primary, secondary, and exploratory outcomes
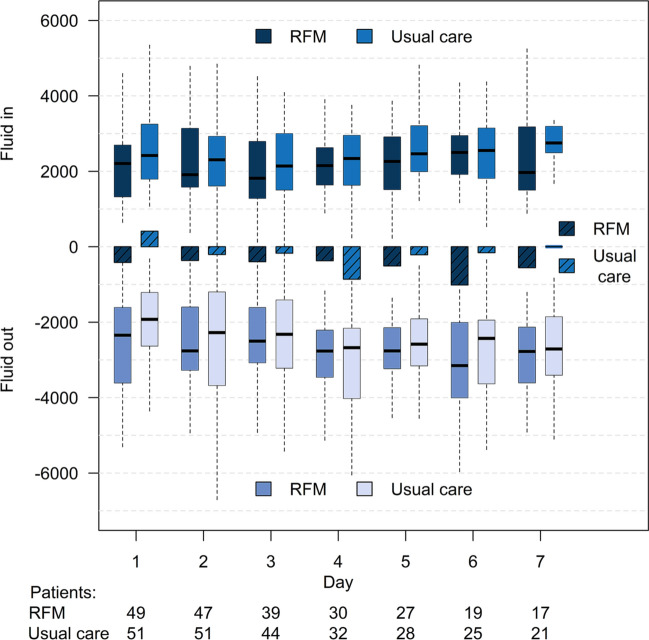
At 72 h, 66 (66%) patients were still in ICU, while 29 (29%) were discharged, four were deceased (one in RFM arm and three in usual care), and one had withdrawn consent for further data collection. The median length of stay from randomization to discharge among these 34 patients was 49.2 [32.6–51.9] in RFM arm and 51.0 [29.3–60.2] hours in the usual care arm. The primary outcome was assessed after a median [IQR] 72.0 [53.9–72] hours from randomization. Figure 2 presents fluid input and output data along with daily fluid balance in both arms. Table 2 presents the primary and secondary outcomes. The mean difference (95% CI) in cumulative fluid balance at 72 h was − 1148 (− 2200 to − 96) mL, P = 0.033. There was no difference in duration of AKI but fewer patients in the RFM group received RRT compared to the usual care group. Two additional patients in the usual care arm commenced RRT after day 14. Cumulative fluid balance at 24 h and at ICU discharge or on day 7 were significantly lower in the RFM group. Diuretics were administered to 35 (71.4%) in the RFM group and 38 (74.5%) in the usual care group. The median [IQR] day number of first administration of diuretics was 1 [1] in both groups. There were no differences in the cumulative doses of diuretics adjusted for observation days. The crude primary outcome was in line with the adjusted analysis (Table S6). There were no significant differences in the adjusted or unadjusted exploratory outcomes (adjusted in Table 3, crude in Table S7). Figure S1 presents the daily SOFA score according to treatment allocation.
Fig. 2.
Daily fluid input, fluid output and daily fluid balance from randomization in restrictive versus usual care. Boxplots represent median with IQR and range in mL. Bars present the daily balance (not cumulative) in mL. RFM restrictive fluid management
Table 2.
Primary and secondary outcomes (adjusted for stratification variables)
| Outcome | Restrictive fluid management (n = 49) | Usual care (n = 51) | Restrictive fluid management vs usual care (95% CI)a | P valueb |
|---|---|---|---|---|
| Cumulative fluid balance at 72 h from randomization, mean (SD) mLc | − 1080 (2003) | 61 (3131) | − 1148 (− 2200; − 97) | 0.033 |
| Duration of AKI (days), median [IQR]d | 2 [1–3] | 3 [2–7] | − 1 (− 3; 0) | 0.071 |
| Number of patients-receiving RRT, n (%)e | 6/46 (13) | 15/50 (30) | 0.42 (0.16; 0.91) | 0.043 |
| Cumulative fluid balance at 24 h from randomization, mean (SD) mLc | − 416 (1194) | 409 (1566) | − 822 ( − 1381; − 264) | 0.004 |
| Cumulative fluid balance at ICU discharge/day 7, mean (SD) mLc | − 2166 (2988) | − 650 (4469) | − 1532 (− 3036; − 29) | 0.046 |
| Cumulative dose of furosemide per day, median [IQR] mgf | 0 (0–19) | 1.4 (0–26.2) | 0 (− 11; 5.7) | 0.700 |
AKI acute kidney injury, RRT renal replacement therapy
aAdjusted (severity of AKI and presence of fluid overload) difference in means/median or risk ratio with 95% CIs
bP value derived from regression model adjusted for stratification variables (severity of AKI and presence of fluid accumulation)
cThe last available value for cumulative balance was analyzed for all patients even if ICU discharge or consent withdrawal would have occurred before endpoint was fulfilled
dTruncated at 7 days, ICU discharge, or consent withdrawal. Data missing for three patients-receiving restricted fluid management and one in usual care
eTruncated at 14 days (RRT provided post-ICU discharge included)
fPer oral furosemide dose divided by 2 to make it comparable to intravenous doses
Table 3.
Exploratory outcomes (adjusted for stratification variables)
| Outcome | Restrictive fluid management | Usual care | Restrictive fluid management vs usual care (95% CI)a | P valueb |
|---|---|---|---|---|
| Days alive and free of mechanical ventilation, median [IQR]c | 13 (9–14) | 11.5 (1.5–14) | 0 (− 1; 6) | 0.284 |
| Days alive and free of vasopressors, median [IQR] c | 12 (10–14) | 11.5 (7–13) | 1 (0; 2) | 0.072 |
| Days alive and free of ICU treatment, median [IQR] c | 8 (3–11) | 2.5 (0–11) | 2 (0; 6) | 0.106 |
| Days alive and free of RRT at 90 days, median [IQR]d | 90 (85–90) | 90 (33–90) | 0 (0; 14) | 0.145 |
| Dialysis dependence at 90-days, n (%) | 0/46 (0) | 1/49 (2) | 0.34 (0.01; 8.55) | 1.000 |
| 90-day mortality, n (%) | 9/46 (19.6) | 13/49 (26.5) | 0.74 (0.35; 1.46) | 0.387 |
aAdjusted (severity of AKI and presence of fluid overload) difference in means/median with 95% CIs
bP value derived from regression model adjusted for stratification variables (severity of acute kidney injury and presence of fluid accumulation)
cTruncated at 14 days or ICU discharge. Potential ICU readmissions not included. Data not available for two patients-receiving restrictive fluid management and for one receiving usual care
dData not available for two patients in both groups
Safety and feasibility outcomes
Eleven (22.4%) patients in the RFM group and 25 (49%) in the usual care group experienced one or more AE (risk ratio 0.46; 95% CI 0.36–0.63, P = 0.001). Serious adverse events (SAE) were observed in six (12.2%) patients randomized to RFM group and in 16 (31.4%) randomized to usual care group (RR 0.39; 95% CI 0.15–0.86, P = 0.031). Table S8 provides a detailed description of AEs and SAEs. Most events were related to disturbances in serum electrolyte concentrations and RRT. The median [IQR] number of patients recruited per center/month was 0.8 [0.5–1.7] (Figure S2).
Fluid protocol and protocol violations
Protocol violations occurred in 18 (36.7%) in the RFM arm and in 5 (9.8%) in the usual care arm. In the RFM arm, use of excess maintenance fluid was the most frequently observed protocol violation in 9 (18.4%) patients (Table S9). Moreover, five patients in the RFM arm had a protocol suspension for the following reasons: hypernatremia (n = 2), need for surgery (n = 1), complete heart block (not considered to be attributable to study intervention) (n = 1), and withdrawal of consent (n = 1). One patient in the usual care arm had protocol suspension as overall ICU care was withdrawn.
Per-protocol analysis
Twenty-three patients (46.9% of 49) in the RFM arm and 37 (72.5% of 51) in the usual care arm were included in the per-protocol analysis. The primary or secondary outcome variables were not different in the per-protocol population except for fluid balance at 24 h (Table S10).
Discussion
Key findings
In this multicenter, multinational, unblinded, randomized, controlled, feasibility pilot study involving 100 critically ill patients with AKI who were considered adequately resuscitated, we assessed whether, compared to usual care, a restrictive fluid management regimen would lead to a meaningful difference in cumulative fluid balance after 72 h from randomization without signals of harm. We found the RFM protocol to be effective in terms of achieving a lower cumulative fluid balance at 72 h compared to usual care. Moreover, patients in the RFM arm received RRT less frequently and had fewer adverse events than patients in the usual care arm.
Relationship with previous studies
No randomized controlled trial has studied a RFM regimen among critically ill patients with AKI.
The FACTT trial, conducted from 2000 to 2005, compared conservative fluid management to liberal therapy in patients with ARDS and found no difference in 60-day mortality, but reported shorter duration of mechanical ventilation and a trend toward less RRT in the conservative arm [17]. Furthermore, a sub-analysis of patients with AKI found an association with high cumulative fluid balance and mortality [9]. In the FACTT, the cumulative fluid balance on day three (corresponding to the primary endpoint in the current analysis) was about 150 mL in the conservative arm and about 5000 mL in the liberal arm, both more positive than in our study [23]. Moreover, we observed a much lower actual fluid balance in the usual care group than we had assumed based on data collected in 2011–2012. Such a shift towards more restrictive fluid management practices among the critically ill has been reported also in another RFM pilot trial [24].
Most interventional fluid trials in the critically ill have concentrated on modifying fluid administration [14, 15, 25–28] or enhancing fluid output with diuretics and/or ultrafiltration [29]. Our approach of combining the two sides of the coin in one trial gave the treating clinician more tools to individualize fluid therapy while still successfully targeting a clinically meaningful outcome measure. For example, the CLASSIC pilot trial among patients with septic shock achieved a difference in the administered resuscitation fluid but not in the total fluid balance [14]. Notably, fluids other than resuscitation fluid represent the largest proportion of the administered fluids [30, 31] even in patients with shock [32].
A dynamic intervention bundle such as ours may be more suitable for AKI patients who represent a heterogeneous group of patients with some having severely reduced urine output significantly affecting the achievable fluid output while others have a creatinine rise but preserved urine output. A French stepped wedge cluster RCT is assessing another dynamic approach among general ICU patients [33]. The trial intervention involves fluid restriction and/or enhancement of fluid output to achieve a daily weight loss of 0.5 kg in patients with increasing daily weight [33]. However, no results are yet available. A pilot study among septic shock patients reported a rather large but non-significant difference between restrictive and usual care without any signals of harm, but the trial was stopped early as the predefined endpoint of a—500 mL—difference in mean daily fluid balance was not met [24].
Study implications
Our results showed that, in ICU patients with AKI who are considered not to be hypovolemic, using a combined strategy targeting control of daily fluid balance is both feasible and safe. Adverse events were more frequent in the usual care arm, possibly related to more frequent use of RRT in this group. Moreover, the trial provides initial support to the hypothesis that fluid accumulation is linked to important outcomes among AKI patients such as need for RRT, a hypothesis that should be studied in larger clinical trials.
A quarter of excluded patients were ineligible due to being still considered intravascularly hypovolemic albeit having stayed in the ICU for at least 12 h. This is an important patient cohort that should be considered when designing future RFM trials. Potentially, these patients could be enrolled, if the RFM protocol included a well-defined starting trigger after correction of hypovolemia such as using passive leg raising or other dynamic tests to assess fluid responsiveness [34, 35].
Strengths and limitations
Obvious strengths to our study include randomization to minimize selection bias and a multinational approach allowing simultaneous feasibility assessment in multiple locations with potentially different fluid treatment practices and increasing external validity. In addition, we used a treatment bundle targeting both fluid input and output to maximize the efficacy of the intervention, a dynamic two-pronged approach, which increased flexibility and allowed for individualization of treatment according to perceived patients’ needs. Moreover, we collected data on multiple potential adverse events daily to be able to reliably identify any signal of harm potentially associated with RFM.
We acknowledge several limitations. First, blinding of the intervention was not possible due to its nature. Second, calculated fluid balance is not an exact measure, as measurement of fluid output in patients with high insensible losses (such as losses to wound dressing) is not exact. Thus, the actual fluid balance of the included patients in both groups may be lower than reported here. Third, we observed protocol violations in terms of use of excessive maintenance fluid. This may signal the presence of local practices [30, 32] that need to be better addressed in future trials. Fourth, we excluded patients with treatment limitations albeit many from this heterogenous group could potentially have been enrolled. Nonetheless, we observed a signal for positive patient-centered outcomes in the frequency of RRT, which implies that fluid restriction may have an effect on clinical outcomes.
Conclusions
In a pilot multicenter, international, randomized, controlled trial of critically ill patients with AKI who were considered adequately fluid resuscitated, a restrictive fluid management regimen was feasible, resulted in fewer adverse events than usual care, and delivered a significant separation in fluid balance. The results also suggested benefit in terms of patient-centered outcomes implying that this intervention should now be studied in larger trials.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We warmly thank the patients and their families for participating. We are grateful to the clinical staff at participating ICUs for their contributions. The REVERSE-AKI study team: Austin Hospital: Rinaldo Bellomo, Suvi Vaara, Laurent Bitker, Glenn Eastwood. Canberra Hospital: Frank van Haren, Liam Byrne, Mary Nourse, Samantha Adam, Clare Robertson, Josie Russell-Brown, Shakira Spiller. Ghent University Hospital: Eric Hoste, Jan Fierens, Pieter Nepuydt, Daisy Vermeiren, Ingrid Herck, Druwe Patrick, Luc De Crop, Stephanie Bracke. Guys and St Thomas’ Hospital: Marlies Ostermann, Andy Retter, Sara Campos, Gill Arbane, Andrea Kelly, Neus Grau Novellas, Rosario Lim, Martina Marotti, Aneta Bociek, Tim Jones, Christopher Whitton, Andrew Slack, Luigi Camporota, Simon Sparkes, Duncan Wyncoll. Helsinki University Hospital: Suvi Vaara, Minna Bäcklund, Ville Pettilä, Jonna Heinonen, Leena Pettilä, Sari Sutinen, Elina Lappi. Lausanne University Hospital Antoine Schneider, Elettra Poli, Marco Altarelli, Michel Thibault, Philippe Eckert, Madeleine Schnorf. Royal London Hospital: John Prowle, Ryan Haines, Richard Cashmore, Alex Fowler, Filipa Dos Santos, Amaia Garcia, Maria Fernandez, Tim Martin, Ruzena Uddin.
Funding
Open access funding provided by University of Helsinki including Helsinki University Central Hospital. The trial has received support from the Academy of Finland (317061), Orion Research Foundation, and state funding for university-level health research (TYH2017241). STV has received a Fellowship grant from the Sigrid Juselius Foundation. In the UK, the study was supported by an investigator-initiated research grant from Fresenius Medical Care. The funders had no role in the trial design, conduction, or interpretation of the results.
Data availability
A dataset is available as supplemental information.
Declarartions
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
The members of the The REVERSE-AKI study team are listed in the acknowledgements section.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Suvi T. Vaara, Email: suvi.vaara@helsinki.fi
on behalf of the REVERSE-AKI study team:
Rinaldo Bellomo, Suvi Vaara, Laurent Bitker, Glenn Eastwood, Frank van Haren, Liam Byrne, Mary Nourse, Samantha Adam, Clare Robertson, Josie Russell-Brown, Shakira Spiller, Eric Hoste, Jan Fierens, Pieter Nepuydt, Daisy Vermeiren, Ingrid Herck, Druwe Patrick, Luc De Crop, Stephanie Bracke, Marlies Ostermann, Andy Retter, Sara Campos, Gill Arbane, Andrea Kelly, Neus Grau Novellas, Rosario Lim, Martina Marotti, Aneta Bociek, Tim Jones, Christopher Whitton, Andrew Slack, Luigi Camporota, Simon Sparkes, Duncan Wyncoll, Suvi Vaara, Minna Bäcklund, Ville Pettilä, Jonna Heinonen, Leena Pettilä, Sari Sutinen, Elina Lappi, Antoine Schneider, Elettra Poli, Marco Altarelli, Michel Thibault, Philippe Eckert, Madeleine Schnorf, John Prowle, Ryan Haines, Richard Cashmore, Alex Fowler, Filipa Dos Santos, Amaia Garcia, Maria Fernandez, Tim Martin, and Ruzena Uddin
References
- 1.Nisula S, Kaukonen KM, Vaara ST, Korhonen AM, Poukkanen M, Karlsson S, et al. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med. 2013;39:420–428. doi: 10.1007/s00134-012-2796-5. [DOI] [PubMed] [Google Scholar]
- 2.Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41:1411–1423. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 3.KDIGO (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Inter Suppl 1–138
- 4.Meersch M, Schmidt C, Hoffmeier A, Van Aken H, Wempe C, Gerss J, et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med. 2017;43:1551–1561. doi: 10.1007/s00134-016-4670-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pickkers P, Mehta RL, Murray PT, Joannidis M, Molitoris BA, Kellum JA, et al. Effect of human recombinant alkaline phosphatase on 7-day creatinine clearance in patients with sepsis-associated acute kidney injury: a randomized clinical trial. JAMA. 2018;320:1998–2009. doi: 10.1001/jama.2018.14283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prowle JR, Kirwan CJ, Bellomo R. Fluid management for the prevention and attenuation of acute kidney injury. Nat Rev Nephrol. 2014;10:37–47. doi: 10.1038/nrneph.2013.232. [DOI] [PubMed] [Google Scholar]
- 7.RENAL Replacement Therapy Study Investigators An observational study fluid balance and patient outcomes in the randomized evaluation of normal vs. augmented level of replacement therapy trial*. Crit Care Med. 2012;40:1753–1760. doi: 10.1097/CCM.0b013e318246b9c6. [DOI] [PubMed] [Google Scholar]
- 8.Vaara ST, Korhonen AM, Kaukonen KM, Nisula S, Inkinen O, Hoppu S, et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care. 2012;16:R197. doi: 10.1186/cc11682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grams ME, Estrella MM, Coresh J, Brower RG, Liu KD. Fluid balance, diuretic use, and mortality in acute kidney injury. Clin J Am Soc Nephrol. 2011;6:966–973. doi: 10.2215/CJN.08781010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422–427. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- 11.Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid overload and mortality in adult critical care patients—a systematic review and meta-analysis of observational studies. Crit Care Med. 2020;48:1862–1870. doi: 10.1097/CCM.0000000000004617. [DOI] [PubMed] [Google Scholar]
- 12.Raimundo M, Crichton S, Martin JR, Syed Y, Varrier M, Wyncoll D, et al. Increased fluid administration after early acute kidney injury is associated with less renal recovery. Shock. 2015;44:431–437. doi: 10.1097/SHK.0000000000000453. [DOI] [PubMed] [Google Scholar]
- 13.Zhang J, Crichton S, Dixon A, Seylanova N, Peng ZY, Ostermann M. Cumulative fluid accumulation is associated with the development of acute kidney injury and non-recovery of renal function: a retrospective analysis. Crit Care. 2019;23:392. doi: 10.1186/s13054-019-2673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettila V, et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med. 2016;42:1695–1705. doi: 10.1007/s00134-016-4500-7. [DOI] [PubMed] [Google Scholar]
- 15.Martensson J, Bihari S, Bannard-Smith J, Glassford NJ, Lloyd-Donald P, Cioccari L, et al. Small volume resuscitation with 20% albumin in intensive care: physiological effects: the SWIPE randomised clinical trial. Intensive Care Med. 2018;44:1797–1806. doi: 10.1007/s00134-018-5253-2. [DOI] [PubMed] [Google Scholar]
- 16.Chen C, Kollef MH. Targeted fluid minimization following initial resuscitation in septic shock: a pilot study. Chest. 2015;148:1462–1469. doi: 10.1378/chest.15-1525. [DOI] [PubMed] [Google Scholar]
- 17.Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 18.Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, et al. Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med. 2018;378:2263–2274. doi: 10.1056/NEJMoa1801601. [DOI] [PubMed] [Google Scholar]
- 19.Pickkers P, Ostermann M, Joannidis M, Zarbock A, Hoste E, Bellomo R, et al. The intensive care medicine agenda on acute kidney injury. Intensive Care Med. 2017;43:1198–1209. doi: 10.1007/s00134-017-4687-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ostermann M, Bellomo R, Burdmann EA, Doi K, Endre ZH, Goldstein SL, et al. Controversies in acute kidney injury: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) conference. Kidney Int. 2020;98:294–309. doi: 10.1016/j.kint.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaara ST, Ostermann M, Selander T, Bitker L, Schneider A, Poli E, et al. Protocol and statistical analysis plan for the restricted fluid therapy versus standard treatment in acute kidney injury—REVERSE-AKI randomized controlled pilot trial. Acta Anaesthesiol Scand. 2020;64:831–838. doi: 10.1111/aas.13557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahan BC, Morris TP. Reporting and analysis of trials using stratified randomisation in leading medical journals: review and reanalysis. BMJ. 2012;345:e5840. doi: 10.1136/bmj.e5840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grissom CK, Hirshberg EL, Dickerson JB, Brown SM, Lanspa MJ, Liu KD, et al. Fluid management with a simplified conservative protocol for the acute respiratory distress syndrome*. Crit Care Med. 2015;43:288–295. doi: 10.1097/CCM.0000000000000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Semler MW, Janz DR, Casey JD, Self WH, Rice TW. Conservative fluid management after sepsis resuscitation: a pilot randomized trial. J Intensive Care Med. 2020;35:1374–1382. doi: 10.1177/0885066618823183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meyhoff TS, Hjortrup PB, Moller MH, Wetterslev J, Lange T, Kjaer MN, et al. Conservative vs liberal fluid therapy in septic shock (CLASSIC) trial-protocol and statistical analysis plan. Acta Anaesthesiol Scand. 2019;63:1262–1271. doi: 10.1111/aas.13434. [DOI] [PubMed] [Google Scholar]
- 26.Self WH, Semler MW, Bellomo R, Brown SM, deBoisblanc BP, Exline MC, et al. Liberal versus restrictive intravenous fluid therapy for early septic shock: rationale for a randomized trial. Ann Emerg Med. 2018;72:457–466. doi: 10.1016/j.annemergmed.2018.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Macdonald SPJ, Keijzers G, Taylor DM, Kinnear F, Arendts G, Fatovich DM, et al. Restricted fluid resuscitation in suspected sepsis associated hypotension (REFRESH): a pilot randomised controlled trial. Intensive Care Med. 2018;44:2070–2078. doi: 10.1007/s00134-018-5433-0. [DOI] [PubMed] [Google Scholar]
- 28.Corl KA, Prodromou M, Merchant RC, Gareen I, Marks S, Banerjee D, et al. The restrictive IV fluid trial in severe sepsis and septic shock (RIFTS): a randomized pilot study. Crit Care Med. 2019;47:951–959. doi: 10.1097/CCM.0000000000003779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berthelsen RE, Perner A, Jensen AK, Rasmussen BS, Jensen JU, Wiis J, et al. Forced fluid removal in intensive care patients with acute kidney injury: the randomised FFAKI feasibility trial. Acta Anaesthesiol Scand. 2018;62:936–944. doi: 10.1111/aas.13124. [DOI] [PubMed] [Google Scholar]
- 30.Silversides JA, Fitzgerald E, Manickavasagam US, Lapinsky SE, Nisenbaum R, Hemmings N, et al. Deresuscitation of patients with iatrogenic fluid overload is associated with reduced mortality in critical illness. Crit Care Med. 2018;46:1600–1607. doi: 10.1097/CCM.0000000000003276. [DOI] [PubMed] [Google Scholar]
- 31.Van Regenmortel N, Verbrugghe W, Roelant E, Van den Wyngaert T, Jorens PG. Maintenance fluid therapy and fluid creep impose more significant fluid, sodium, and chloride burdens than resuscitation fluids in critically ill patients: a retrospective study in a tertiary mixed ICU population. Intensive Care Med. 2018;44:409–417. doi: 10.1007/s00134-018-5147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lindén-Søndersø A, Jungner M, Spångfors M, Jan M, Oscarson A, Choi S, et al. Survey of non-resuscitation fluids administered during septic shock: a multicenter prospective observational study. Ann Intensive Care. 2019;9:132. doi: 10.1186/s13613-019-0607-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agrinier N, Monnier A, Argaud L, Bemer M, Virion JM, Alleyrat C, et al. Effect of fluid balance control in critically ill patients: design of the stepped wedge trial POINCARE-2. Contemp Clin Trials. 2019;83:109–116. doi: 10.1016/j.cct.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 34.Douglas IS, Alapat PM, Corl KA, Exline MC, Forni LG, Holder AL, et al. Fluid response evaluation in sepsis hypotension and shock: a randomized clinical trial. Chest. 2020;158:1431–1445. doi: 10.1016/j.chest.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vignon P, Evrard B, Asfar P, Busana M, Calfee CS, Coppola S, et al. Fluid administration and monitoring in ARDS: which management? Intensive Care Med. 2020;46:2252–2264. doi: 10.1007/s00134-020-06310-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
A dataset is available as supplemental information.