Abstract
Purpose: This analysis was designed to characterize the pre-exposure prophylaxis (PrEP) cascade in a U.S. national sample of transgender men and trans masculine adults who have sex with cisgender men (trans MSM) at-risk for HIV acquisition.
Methods: From November to December 2017, 843 HIV-negative trans MSM self-reporting past-6-month receptive sex with a cisgender man were recruited via peer referrals, dating apps, listservs, and social media. A computer-assisted self-interview assessed demographics, health care, and the PrEP cascade. Descriptive statistics and multivariable regression models evaluated factors associated with PrEP uptake and persistence.
Results: Mean age was 28.1 years (standard deviation = 7.1); 4.8% were Black, 21.7% Latinx, and 25.6% another race/ethnicity. A total of 84.1% had heard of PrEP, with 67.3% reporting interest. More than half (55.2%) were PrEP indicated, of which 50.8% were PrEP naive. Approximately 1/4 (28.0%) reported PrEP use, of which 65.3% were PrEP persistent. PrEP modality preferences were injectable (51.2%), daily oral pill (22.1%), and anal gel/lube (14.6%). Reasons for PrEP noninterest were no HIV risk (68.5%), cost (24.2%), and side effects (20.1%). Surgical gender affirmation, no health care discrimination, and social media as a primary health information source were associated with increased odds of PrEP uptake and persistence (all p < 0.05). PrEP adherence difficulties were reported by 52.6%, due to busy/inconsistent schedule (53.1%), side effects (27.4%), and too many medical visits (11.6%).
Conclusion: PrEP uptake was modest among the trans MSM sampled, given prevalent HIV risk behaviors. The limited PrEP uptake in at-risk trans MSM suggests the need to develop culturally tailored community education and interventions.
Keywords: HIV prevention, MSM, PrEP, transgender
Introduction
Transgender men and other trans masculine adults who have sex with men (trans MSM) are at-risk for HIV infection when they have condomless anal or frontal/vaginal intercourse with cisgender (cis) MSM partners or share needles for hormone or recreational drug injection.1 Pre-exposure prophylaxis (PrEP) has been shown to be a safe and effective method of HIV prevention for cis MSM.2,3 However, data are limited on PrEP effectiveness and use in trans MSM.4,5 Studies demonstrate high rates of condomless sex and suboptimal recent HIV testing behaviors among trans MSM.6–8 Information is needed about PrEP awareness, indications, uptake, and persistence in this at-risk MSM subgroup for service delivery planning.
The PrEP cascade is a heuristic framework utilized to understand steps or stages of PrEP care and implementation, from identifying individuals at highest risk of HIV acquisition to retaining individuals in PrEP care.9,10 To date, research applying the PrEP cascade framework to evaluate PrEP-related outcomes in trans MSM is scarce.4 The current study sought to fill this gap. In cis MSM, many factors impact PrEP cascade outcomes. For example, differences in PrEP uptake have been found by geographic region, age, race, ethnicity, and insurance.11–13 Perceived HIV risk, HIV testing history, sexual risk behaviors, and PrEP indications have also been associated with PrEP outcomes.13–17 In addition, psychosocial factors such as mental health challenges influence PrEP utilization behaviors.18,19
For trans MSM, added factors warrant consideration in the PrEP cascade. A binary gender identity or a gay sexual orientation identity may each confer vulnerability due to pressures to conform to social norms surrounding gender roles (e.g., what it means to be a man) or sexual identity (e.g., what it means to be a gay man).20 PrEP education programs for MSM have generally focused on cis MSM, leaving trans MSM with the impression that they might not be candidates for PrEP. Medical gender affirmation (e.g., hormones, surgeries) is linked with improved mental health functioning21; however, the association of these therapies with PrEP cascade outcomes is unknown. Stigma due to being gender minority and sexual minority is also an important concern for trans MSM in navigating sexual partnerships and with health care systems.22 Furthermore, understanding preferred sources of health information, such as online social media, will aid the design, implementation, and scale-up of future PrEP interventions for trans MSM.
The objective of this study was to characterize the PrEP cascade in a national sample of trans MSM in the United States and examine factors associated with PrEP to characterize the PrEP cascade and product preferences in a national sample of trans MSM in the United States and examine factors associated with PrEP uptake and persistence, and product preferences.
Methods
Participants and procedures
A U.S. national sample of 857 trans MSM was recruited and completed an online one-time computer-assisted self-interview survey from November to December 2017. Nonprobability sampling methods were used for recruitment (e.g., peer referral, dating apps, listservs, and other social media). Eligibility criteria for participation were as follows: ages 18 years or older, assigned female sex at birth, current gender identity on the trans masculine spectrum, English-speaking, and self-reporting receptive anal or frontal/vaginal sex, with or without a condom, with a cisgender male sex partner in the past 6 months. Trans MSM living with HIV (n = 14; 1.6% of the sample) were excluded from this PrEP analysis. All study activities were approved by the Fenway Health Institutional Review Board (FWA00000145). Written consent was waived to preserve anonymity. Participants reviewed an electronic informed consent page and agreed to participate before completing the survey. Additional study details can be found elsewhere.23
Survey measures
The survey included source questions from the U.S. Behavioral Risk Factor Surveillance System24 and previous transgender research.25 Geographic region was assessed via self-reported zip code and coded as Northeast, Midwest, South, West, or Other/Unknown Geography. Age group was assessed continuously and coded as 18–24, 25–29, 30–39, and 40–60 years. Race was assessed by asking participants to describe their race or ethnic background and was coded as White, Black, and other (Asian, Pacific Islander, American Indian/Alaskan, Multiracial, other). Ethnicity was coded as Latinx or not Latinx. Education was assessed as low (<high school diploma/some college) or high (4-year college degree, graduate degree).
Participants were asked to select the response that best described their current gender identity. Binary gender identity was coded as binary (male, man, transgender man, female-to-male, trans man, man of transgender experience) or nonbinary (trans masculine, gender queer, gender nonconforming, nonbinary, agender, bigender, other gender). Participants were asked to describe their sexual orientation identity and responses were coded as gay (gay, homosexual, same-gender attraction) or other (bisexual, queer, pansexual, other). A series of items were asked about medical gender affirmation, including lifetime hormone use (testosterone use) and a list of surgical interventions (e.g., chest, genital). Participants were coded as having had any surgery, top surgery (those indicating chest surgery, e.g., mastectomy, chest reconstruction), lower surgery (those indicating genital surgery, e.g., metoidioplasty, phalloplasty), or no surgery.
HIV acquisition sexual risk behavior was assessed by asking participants separate questions about whether or not they had engaged in condomless receptive anal and frontal sex with a male partner in the last 6 months. PrEP indications (yes, no) were evaluated by applying the adapted Centers for Disease Control and Prevention criteria.26 Access to health services was queried, including questions about health insurance (public, private, or none) and lifetime and past 6-month HIV testing history (coded as ever tested, tested in the last 6 months, or never tested). PrEP cascade variables were assessed, including PrEP awareness, interest, uptake, side effects, reasons for nonuse, adherence, persistence, and product preferences.9,10
Psychosocial factors were measured including substance use in the last 6 months, coded as alcohol, drugs, both alcohol and drugs, neither.27 Psychological distress in the last 30 days was evaluated using the validated Kessler-6, which asked participants to rate the frequency with which they felt different symptoms (e.g., “nervous,” “hopeless,” “worthless”) on a scale from 0 (none of the time) to 4 (most of the time). Scores ranged from 0 to 24 and were grouped into quartiles based on the sample distribution as no distress, low, moderate, or high distress.28 Experiencing stigma in the context of sex with a cisgender male in the last 6 months was measured using a four-item scale designed and validated specifically for the study population.29 Items pertained to gender nonaffirmation in the context of a sexual encounter with a cisgender male, such as being referred to with the incorrect pronouns/misgendered during sex and dealing with a sex partner questioning his own sexual orientation after having sex. Responses ranged from 1 (never) to 4 (many times) and were summed (theoretical range from 4 to 16), then grouped into quartiles based on sample distribution as none, low, moderate, or high stigma. Lifetime discrimination in health care was asked and coded as any discrimination or none.30 Participants were asked about their primary source of health information, which was coded as online social media or another source.
Statistical analyses
Missing data on all survey items used to measure the PrEP cascade and statistical predictors exceeded 10.0%. All analyses were conducted on multiply imputed data (five data sets) obtained via multiple imputation by chained equations with random forests in R. Pooled statistics were obtained by combining estimates from each data set into a single parameter estimate using appropriate methodology (PROC MIANALYZE in SAS). Descriptive statistics were used to characterize the sample. Logistic regression models were fit with PrEP uptake (yes/no) and PrEP persistence (yes/no) as outcome variables. Bivariate models were followed by multivariable models. A single multivariable model was fit for PrEP uptake. The denominator for the PrEP outcome was HIV-negative trans MSM who had ever heard of PrEP (n = 709). For PrEP persistence, separate multivariable models were fit, adjusted for geographic location only, to ensure model convergence. These models were restricted to HIV-negative trans MSM who reported having heard of PrEP and had ever taken PrEP (n = 236).
Results
Sociodemographic and clinical characteristics
Table 1 presents sample characteristics overall and stratified by PrEP uptake. Table 2 displays the sample stratified by PrEP persistence. The mean age was 28.1 years (standard deviation = 7.1 years) and 4.8% were Black, 21.7% Latinx, 25.6% another race/ethnicity. A total of 86.8% endorsed a binary gender identity (e.g., man, male, trans man). One-third (32.7%) identified as gay. The majority had medically affirmed their gender: 82.6% testosterone, 56.1% surgery (48.8% chest, 19.9% genital).
Table 1.
Descriptive Characteristics of Trans MSM Sampled by PrEP Uptake and Logistic Regression Models of PrEP Uptake in Trans MSM Who Reported Having Heard of PrEP (n = 709)
| |
Among all HIV-negative trans MSM (N = 843) |
PrEP uptake (among HIV-negative trans MSM who reported knowing about [having heard of] PrEP) (N = 709) |
||||||
|---|---|---|---|---|---|---|---|---|
| Total sample |
PrEP uptake (N = 236) |
No PrEP uptake (N = 473) |
Crude models and adjusted multivariable model |
|||||
| Characteristic | n | % | n | % | n | % | OR (95% CI) | aOR (95% CI) |
| Geographic location | ||||||||
| Northeast | 165 | 19.57 | 48 | 20.34 | 94 | 19.87 | 1.29 (0.69–2.42) | 1.02 (0.51–2.04) |
| Midwest | 121 | 14.35 | 27 | 11.44 | 71 | 15.01 | Ref. | Ref. |
| South | 206 | 24.44 | 56 | 23.73 | 122 | 25.79 | 1.18 (0.66–2.12) | 0.94 (0.49–1.83) |
| West | 188 | 22.30 | 58 | 24.58 | 96 | 20.30 | 1.58 (0.86–2.90) | 0.95 (0.46–1.97) |
| Other/unknown geography | 163 | 19.34 | 47 | 19.92 | 90 | 19.03 | 1.35 (0.72–2.52) | 1.14 (0.54–2.44) |
| Age group (years) | ||||||||
| 18–24 | 271 | 32.15 | 31 | 13.14 | 183 | 38.69 | Ref. | Ref. |
| 25–29 | 280 | 33.21 | 94 | 39.83 | 142 | 30.02 | 3.96 (2.26–6.93) | 3.40 (1.71–6.76) |
| 30–39 | 241 | 28.59 | 96 | 40.68 | 116 | 24.52 | 4.95 (2.99–8.20) | 3.29 (1.69–6.39) |
| 40–60 | 51 | 6.05 | 15 | 6.35 | 32 | 6.77 | 2.79 (1.35–5.80) | 1.97 (0.83–4.69) |
| Race | ||||||||
| White | 587 | 69.63 | 182 | 77.12 | 315 | 66.60 | 2.06 (0.89–4.77) | 3.58 (1.28–10.00) |
| Black | 40 | 4.75 | 8 | 3.39 | 27 | 5.71 | Ref. | Ref. |
| Other | 216 | 25.62 | 46 | 19.49 | 131 | 27.70 | 1.24 (0.51–3.02) | 2.32 (0.74–7.23) |
| Ethnicity | ||||||||
| Latinx | 183 | 21.71 | 70 | 29.66 | 75 | 15.86 | 2.24 (1.50–3.34) | 3.00 (1.80–5.00) |
| Not Latinx | 660 | 78.29 | 166 | 70.34 | 398 | 84.14 | Ref. | Ref. |
| Education | ||||||||
| High | 315 | 37.37 | 100 | 42.37 | 186 | 39.32 | 1.12 (0.80–1.59) | 1.00 (0.62–1.60) |
| Low | 528 | 62.63 | 136 | 57.63 | 287 | 60.68 | Ref. | Ref. |
| Gender identity | ||||||||
| Binary | 732 | 86.83 | 217 | 91.95 | 397 | 83.93 | 2.20 (1.27–3.80) | 1.70 (0.90–3.20) |
| Nonbinary | 111 | 13.17 | 19 | 8.05 | 76 | 16.07 | Ref. | Ref. |
| Sexual orientation | ||||||||
| Gay | 276 | 32.74 | 119 | 50.42 | 107 | 22.62 | 3.48 (2.41–5.04) | 2.23 (1.39–3.58) |
| Other | 567 | 67.26 | 117 | 49.58 | 366 | 77.38 | Ref. | Ref. |
| Medical affirmationa,b | ||||||||
| Testosterone use | 696 | 82.56 | 211 | 89.41 | 399 | 84.36 | 1.56 (0.86–2.84) | — |
| Any surgery | 473 | 56.11 | 178 | 75.42 | 245 | 51.80 | 2.86 (1.95–4.19) | 2.28 (1.42–3.65) |
| Top surgery | 411 | 48.75 | 152 | 64.41 | 226 | 47.78 | 1.98 (1.33–2.93) | — |
| Lower surgery | 168 | 19.93 | 96 | 40.68 | 50 | 10.57 | 5.81 (3.84–8.79) | — |
| Health insurance | ||||||||
| Public | 262 | 31.08 | 102 | 43.22 | 109 | 23.04 | 3.02 (1.76–5.18) | 2.30 (1.21–4.36) |
| Private | 414 | 49.11 | 101 | 42.80 | 259 | 54.76 | 1.26 (0.70–2.27) | 1.13 (0.57–2.26) |
| None | 167 | 19.81 | 33 | 13.98 | 105 | 22.20 | Ref. | Ref. |
| HIV testedb | ||||||||
| Ever | 672 | 79.72 | 193 | 81.78 | 404 | 85.41 | 0.77 (0.50–1.20) | — |
| Last 6 months | 666 | 79.00 | 190 | 80.51 | 402 | 84.99 | 1.10 (0.79–1.54) | — |
| Never | 171 | 20.28 | 43 | 18.22 | 69 | 14.59 | Ref. | — |
| PrEP indicated, last 6 months | ||||||||
| Yes | 465 | 55.16 | 162 | 68.64 | 236 | 49.89 | 2.20 (1.46–3.32) | 2.72 (1.52–4.88) |
| No | 378 | 44.84 | 74 | 31.36 | 237 | 50.11 | Ref. | Ref. |
| Substance use, last 6 months | ||||||||
| Alcohol | 169 | 20.05 | 64 | 27.12 | 78 | 16.49 | 3.51 (0.84–14.63) | — |
| Drugs | 66 | 7.83 | 15 | 6.36 | 39 | 8.25 | 1.63 (0.36–7.46) | — |
| Both alcohol and drugs | 561 | 66.55 | 152 | 64.41 | 334 | 70.61 | 1.96 (0.47–8.19) | — |
| Neither | 47 | 5.57 | 5 | 2.12 | 22 | 4.65 | Ref. | — |
| Psychological distress | ||||||||
| No distress | 147 | 17.44 | 54 | 22.88 | 69 | 14.59 | 2.06 (1.15–3.68) | — |
| Low levels of distress | 297 | 35.23 | 81 | 34.32 | 173 | 36.58 | 1.24 (0.74–2.06) | — |
| Moderate levels of distress | 232 | 27.52 | 63 | 26.69 | 130 | 27.48 | 1.29 (0.78–2.14) | — |
| High levels of distress | 167 | 19.81 | 38 | 16.10 | 101 | 21.35 | Ref. | — |
| Cisgender male sexual partner stigma | ||||||||
| None | 188 | 22.30 | 53 | 22.46 | 118 | 24.95 | Ref. | Ref. |
| Low | 280 | 33.21 | 73 | 30.93 | 171 | 36.15 | 0.95 (0.62–1.46) | 1.28 (0.71–2.29) |
| Moderate | 258 | 30.60 | 72 | 30.51 | 137 | 28.96 | 1.17 (0.70–1.95) | 1.55 (0.76–3.13) |
| High | 117 | 13.89 | 38 | 16.10 | 47 | 9.94 | 1.79 (1.04–3.08) | 2.00 (0.89–4.51) |
| Discrimination in health care | ||||||||
| Any | 719 | 85.29 | 187 | 79.24 | 424 | 89.64 | Ref. | Ref. |
| None | 124 | 14.71 | 49 | 20.76 | 49 | 10.36 | 2.27 (1.46–3.54) | 2.62 (1.31–5.24) |
| Primary source of health information | ||||||||
| Other | 606 | 71.89 | 143 | 60.59 | 362 | 76.53 | Ref. | Ref. |
| Social media | 237 | 28.11 | 93 | 39.41 | 111 | 23.47 | 2.09 (1.48–2.95) | 1.90 (1.23–2.93) |
| HIV acquisition sexual risk behavior, last 6 monthsb | ||||||||
| Condomless receptive anal sex | 294 | 34.87 | 119 | 50.42 | 132 | 27.91 | 2.64 (1.88–3.72) | — |
| Condomless receptive frontal sex | 461 | 54.69 | 154 | 65.25 | 238 | 50.32 | 1.85 (1.31–2.61) | — |
Bold indicates statistical significance at the alpha 0.05 level.
Medical affirmation: the surgery variable was operationalized as binary (surgery yes/no) for the final multivariable model of PrEP uptake to assess the overall association of any surgery with PrEP uptake.
Total does not sum to 100% because response options were not mutually exclusive.
aOR, adjusted odds ratio; CI, confidence interval; MSM, men who have sex with men; OR, odds ratio; PrEP, pre-exposure prophylaxis.
Table 2.
Descriptive Characteristics and Logistic Regression Models of PrEP Persistence in Trans MSM Who Reported Having Heard of PrEP and Ever Taken PrEP (n = 236)
| |
PrEP persistence (among HIV-negative trans MSM who reported knowing about [having heard of] PrEP and ever taken PrEP) (N = 236) |
|||||
|---|---|---|---|---|---|---|
| PrEP persistence (N = 154) |
No PrEP persistence (N = 82) |
Crude and geographically adjusted multivariable models |
||||
| Characteristic | n | % | n | % | OR (95% CI) | aOR (95% CI) |
| Geographic location | ||||||
| Northeast | 34 | 22.08 | 12 | 14.63 | 2.10 (0.91–4.85) | a |
| Midwest | 20 | 12.99 | 8 | 9.76 | 1.98 (0.70–5.61) | a |
| South | 31 | 20.13 | 25 | 30.49 | Ref. | a |
| West | 42 | 27.27 | 17 | 20.73 | 1.97 (0.88–4.41) | a |
| Other/unknown geography | 27 | 17.53 | 20 | 24.39 | 1.10 (0.46–2.60) | a |
| Age group (years) | ||||||
| 18–24 | 16 | 10.39 | 15 | 18.29 | 1.14 (0.32–4.10) | 1.16 (0.32–4.28) |
| 25–29 | 70 | 45.45 | 25 | 30.49 | 2.89 (0.92–9.09) | 2.84 (0.84–9.56) |
| 30–39 | 61 | 39.61 | 34 | 41.46 | 1.81 (0.58–5.71) | 1.78 (0.54–5.88) |
| 40–60 | 7 | 4.55 | 8 | 9.76 | Ref. | Ref. |
| Race | ||||||
| White | 118 | 76.62 | 64 | 78.05 | Ref. | Ref. |
| Black | 7 | 4.55 | 1 | 1.22 | 3.52 (0.41–30.09) | 4.10 (0.47–36.14) |
| Other | 29 | 18.83 | 17 | 20.73 | 0.93 (0.43–2.01) | 0.97 (0.45–2.10) |
| Ethnicity | ||||||
| Latinx | 42 | 27.27 | 28 | 34.15 | 1.44 (0.80–2.60) | 1.24 (0.66–2.34) |
| Not Latinx | 112 | 72.73 | 54 | 65.85 | Ref. | Ref. |
| Education | ||||||
| High | 74 | 48.05 | 26 | 31.71 | 1.96 (1.10–3.51) | 1.80 (0.98–3.30) |
| Low | 80 | 51.95 | 56 | 68.29 | Ref. | Ref. |
| Gender identity | ||||||
| Binary | 143 | 92.86 | 74 | 90.24 | 1.56 (0.56–4.37) | 1.39 (0.49–3.98) |
| Nonbinary | 11 | 7.14 | 8 | 9.76 | Ref. | Ref. |
| Sexual orientation | ||||||
| Gay | 69 | 44.81 | 34 | 41.46 | 1.73 (0.99–3.02) | 1.76 (0.99–3.10) |
| Other | 85 | 55.19 | 48 | 58.54 | Ref. | Ref. |
| Medical affirmationb | ||||||
| Testosterone use | 140 | 90.91 | 71 | 86.59 | 1.39 (0.53–3.64) | 1.34 (0.51–3.53) |
| Any surgery | 125 | 81.17 | 53 | 64.63 | 2.22 (1.16–4.25) | 2.13 (1.09–4.16) |
| Top surgery | 108 | 70.13 | 43 | 52.44 | 2.06 (0.88–4.79) | 1.97 (0.81–4.78) |
| Lower surgery | 74 | 48.05 | 23 | 28.05 | 2.39 (1.12–5.11) | 2.57 (1.15–5.71) |
| Health insurance | ||||||
| Public | 64 | 41.56 | 38 | 46.34 | 1.29 (0.49–3.39) | 1.23 (0.45–3.37) |
| Private | 72 | 46.75 | 30 | 36.59 | 1.86 (0.65–5.32) | 1.74 (0.60–5.06) |
| None | 18 | 11.69 | 14 | 17.07 | Ref. | Ref. |
| HIV testedb | ||||||
| Ever | 129 | 83.77 | 64 | 78.05 | 1.43 (0.71–2.89) | 1.31 (0.65–2.65) |
| Last 6 months | 89 | 57.79 | 45 | 54.88 | 1.11 (0.62–1.98) | 1.03 (0.56–1.88) |
| Never | 25 | 16.23 | 18 | 21.95 | Ref. | |
| PrEP indicated, last 6 months | ||||||
| Yes | 100 | 64.94 | 62 | 75.61 | 0.58 (0.30–1.13) | 0.55 (0.27–1.12) |
| No | 54 | 35.06 | 20 | 24.39 | Ref. | Ref. |
| Substance use, last 6 months | ||||||
| Alcohol | 51 | 33.12 | 12 | 14.63 | 2.84 (1.38–5.84) | 2.63 (1.27–5.47) |
| Drugs | 9 | 5.84 | 6 | 7.32 | 1.09 (0.30–4.03) | 0.99 (0.26–3.73) |
| Both alcohol and drugs | 90 | 58.44 | 62 | 75.61 | Ref. | Ref. |
| Neither | 4 | 2.60 | 2 | 2.44 | — | — |
| Psychological distress | ||||||
| No distress | 43 | 27.92 | 10 | 12.20 | 3.49 (1.30–9.38) | 3.40 (1.23–9.45) |
| Low levels of distress | 51 | 33.12 | 30 | 36.59 | 1.42 (0.63–3.21) | 1.43 (0.63–3.26) |
| Moderate levels of distress | 39 | 25.32 | 25 | 30.49 | 1.27 (0.55–2.89) | 1.25 (0.53–2.92) |
| High levels of distress | 21 | 13.64 | 17 | 20.73 | Ref. | Ref. |
| Cisgender male sexual partner stigma | ||||||
| None | 44 | 28.57 | 8 | 9.76 | 3.85 (1.33–11.15) | 3.90 (1.30–11.69) |
| Low | 43 | 27.92 | 31 | 37.80 | 1.03 (0.45–2.34) | 1.04 (0.47–2.39) |
| Moderate | 45 | 29.22 | 27 | 32.93 | 1.17 (0.47–2.94) | 1.23 (0.49–3.13) |
| High | 22 | 14.29 | 16 | 19.51 | Ref. | Ref. |
| Discrimination in health care | ||||||
| Any | 108 | 70.13 | 78 | 95.12 | Ref. | Ref. |
| None | 46 | 29.87 | 4 | 4.88 | 10.82 (2.62–44.71) | 11.78 (2.73–50.82) |
| Primary source of health information | ||||||
| Other | 85 | 55.19 | 58 | 70.73 | Ref. | Ref. |
| Social media | 69 | 44.81 | 24 | 29.27 | 1.94 (1.05–3.59) | 1.93 (1.02–3.67) |
| HIV acquisition sexual risk behavior, last 6 monthsb | ||||||
| Condomless receptive anal sex | 78 | 50.65 | 41 | 50.00 | 1.01 (0.49–2.07) | 1.00 (0.49–2.05) |
| Condomless receptive frontal sex | 98 | 63.64 | 56 | 68.29 | 0.81 (0.37–1.76) | 0.79 (0.36–1.73) |
Bold indicates statistical significance at the alpha 0.05-level.
Geographic location was adjusted for in each model of PrEP persistence; thus, no single-parameter estimates are presented in the aOR (95% CI) column for geographic location.
Total does not sum to 100% because response options were not mutually exclusive.
Nearly one-third (31.1%) had public insurance, 49.1% private, and 19.8% no health insurance. Overall, 20.3% had never been tested for HIV in their lifetime, and 21.0% had not been tested for HIV in the last 6 months. Past 6-month HIV risk behavior, condomless receptive sex with a cis male partner, was reported by 34.9% for anal sex and 54.7% for frontal/vaginal sex. Experiencing stigma in the last 6 months in the context of an interaction with a cisgender male sexual partner was reported by 77.7%. Lifetime discrimination in health care was reported by 85.3%.
The PrEP cascade
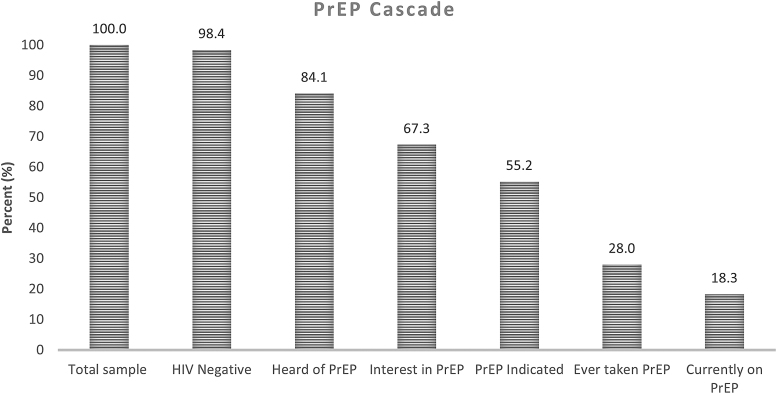
The PrEP cascade in this sample of trans MSM is shown in Figure 1.
FIG. 1.
The pre-exposure prophylaxis cascade in transgender men who have sex with men (n = 857).
PrEP awareness and interest
PrEP awareness was high, with 84.1% (709/843) having heard of PrEP. Of those, 67.3% reported interest in PrEP as a daily oral pill.
PrEP uptake
Overall, 28.0% (236/843) of HIV-negative trans MSM had taken PrEP, 18.3% (154/843) were currently on PrEP, and 9.7% (82/843) had stopped taking PrEP. Thus, 65.3% (154/236) of those who had ever taken PrEP were PrEP persistent (currently taking PrEP), but they were a minority of the men who met PrEP indications (see below). PrEP was most often obtained from a primary care provider (61.4%), followed by a sexual partner (19.9%), STI clinic (9.5%), OB/GYN (9.4%), another source (8.5%), or an endocrinologist (5.5%).
PrEP indications
Approximately half (55.2%; 465/843) of the sample had one or more PrEP indications, of which 50.8% (236/465) had never taken PrEP. The most common reasons why trans MSM were not interested in PrEP were feeling they are not at risk (68.5%), being concerned about cost (24.2%), concerned about side effects (20.1%), and concerned about interference with hormones (14.6%).
PrEP adherence
Among trans MSM who had taken PrEP (n = 236), 52.6% reported adherence difficulties. Reasons for suboptimal adherence were as follows: being busy or having an inconsistent schedule (53.1%), reporting side effects (27.4%), too many medical visits (11.6%), and being worried PrEP may cause harm (11.4%). Side effects reported by trans MSM who had ever taken PrEP were as follows: diarrhea (34.4%), abdominal discomfort/bloating (29.1%), weight loss (26.0%), bone density (21.6%), and nausea (20.7%).
Interest in other PrEP modalities
Trans MSM were asked about other PrEP modalities and were “very” or “somewhat” interested in injectable PrEP (70.0%), blood transfusions with antibodies (54.8%), anal gel/lube (39.6%), and anal douche (31.8%). When asked to rank their preferred PrEP method, they preferred injectable PrEP (51.2%), PrEP as a daily oral pill (22.1%), anal gel/lube (14.6%), blood transfusions with antibodies (9.1%), and anal douche (3.0%).
Logistic regression models: PrEP uptake and PrEP persistence
Results from multivariable logistic regression models are shown in Table 1 for PrEP uptake and Table 2 for PrEP persistence.
PrEP uptake
Factors associated with increased odds of PrEP uptake were being aged 25–29 years and 30–39 years (vs. aged 18–24 years), being White (vs. Black), being Latinx (vs. not), identifying as gay (vs. another sexual identity), having had surgical medical affirmation (vs. none), having public health insurance (vs. no insurance), being PrEP indicated in the last 6 months (vs. not), never having experienced discrimination in health care (vs. discrimination), and using social media as the primary source of health information (vs. some other source) (all p < 0.05).
PrEP persistence
Elevated odds of PrEP persistence were statistically predicted by having had a surgical medical affirmation (vs. not), alcohol use (vs. not), not having any psychological distress (vs. high distress), not experiencing any cisgender male partner stigma (vs. high stigma), never having experienced discrimination in health care (vs. discrimination), and using social media as the primary source of health information (vs. another source) (all p < 0.05).
Discussion
Although research documents that trans MSM are at-risk for HIV acquisition,31,32 this group often gets ignored when it comes to HIV prevention. In this U.S. national sample of trans MSM, PrEP uptake was limited considering the high prevalence of HIV risk behaviors. Although 55.2% of trans MSM reported PrEP indications, the majority were not using PrEP, suggesting that further research, intervention development, and community education are needed to enhance uptake. However, the study found that trans MSM with PrEP indications were more likely to use PrEP than others, highlighting that PrEP may be reaching some trans MSM who need it most. The results support full inclusion of trans MSM in biomedical HIV prevention efforts, including research on long-acting injectable PrEP and other new modalities, which were endorsed by approximately half of the sample.
Three overlapping factors were associated with both PrEP uptake and persistence in regression models. First, not reporting discrimination in health care was associated with PrEP care engagement. Discrimination in health care can have long-term impacts on health care utilization for transgender people.30 More than 8 in 10 trans MSM in this sample indicated that they experienced enacted stigma in health care. It is therefore vital to consider discrimination and stigma-reduction in PrEP care provision for this population. National educational resources are available to train clinicians in the provision of culturally responsive care.33
Second, trans MSM with any surgical gender affirmation were more likely to report PrEP use and continuation than those without. Medical and surgical gender affirmation improves mental health functioning, including gender dysphoria.21 Thus, surgically affirmed trans MSM may engage in health behaviors, such as PrEP to prevent HIV infection, to protect their bodies that now feel comfortable to them. Furthermore, trans MSM with surgery, compared with those without surgery, may access different MSM spaces and partnership pools, perhaps MSM networks with more supportive norms surrounding PrEP use, which may support uptake, or with higher HIV rates which may confer increased vulnerability for HIV acquisition. In addition, this finding may reflect the targeted marketing of PrEP to MSM and the masculine gendering of PrEP to male consumers. PrEP may be perceived of as both socially acceptable and gender-affirming for trans MSM, particularly those who have undergone medical and surgical gender affirmation. Last, this finding suggests the importance of linking PrEP and gender affirmation for trans MSM. PrEP care delivery models for trans MSM may benefit from PrEP providers linking patients to gender-affirming services and trans health providers offering comprehensive PrEP care.
Third, trans MSM who used online social media as their primary source of health information were more likely to report both PrEP uptake and persistence relative to those who utilized other information sources. The internet and online spaces are important resources for transgender people.34,35 This finding demonstrates the potential power of social media as a health outreach tool and the key role it may play in HIV prevention for trans MSM in the era of biobehavioral prevention. Additional research is needed to assess social media exposure and engagement for service delivery.
Limitations
Limitations of this study are the convenience sampling method. PrEP use was higher than anticipated, which may partly be a function of recruitment methods (e.g., recruitment included outreach to HIV prevention listservs). This may also be the reason why trans MSM who endorsed online social media as their primary source of health information had higher odds of PrEP uptake and persistence than those who did not. Another limitation pertains to the relatively low proportion of Black participants in the sample. This could be the result of the nonprobability sampling methods utilized in this study or to other factors that could influence participation, such as stigma. Future research that overcomes this limitation is warranted, including studies that oversample racial/ethnic minority communities. All data are self-report; future research would benefit from gathering biospecimens (e.g., dried blood spots for PrEP adherence). It is not known whether trans MSM experienced discrimination in health care due to their gender identity, sexual orientation, or some other factor. Additional representative data are needed to characterize the PrEP cascade in the trans MSM population (e.g., barriers and facilitators to PrEP uptake, longitudinal studies modeling the PrEP cascade in trans MSM).
Conclusion
PrEP uptake was modest in this U.S. national study of trans MSM, despite that more than half of those sampled were PrEP indicated and HIV acquisition risk sexual behaviors were highly prevalent. In addition, trans MSM experience multiple HIV-related vulnerabilities due to being both a gender minority and a sexual minority. Findings from this research can be used to design, tailor, and implement HIV prevention research, programming, and services for trans MSM. Evidence-based interventions are needed that incorporate culturally specific vulnerabilities, such as stigma in health care, medical gender affirmation, and social media, to improve PrEP cascade outcomes for trans MSM.
Acknowledgments
We thank our Community Task Force for their input and guidance in designing and implementing the study. We also thank those who participated in the study and shared their experiences with us: “Nothing about us without us.”
Authors' Contributions
S.L.R. conceptualized the study, oversaw data acquisition, data analysis, and interpretation, drafted sections of the article, and revised it critically for important intellectual content. C.S.M. conducted data analysis and interpretation and drafted sections of the article. A.A. and D.J.P. implemented data collection, conducted a literature review, interpreted findings, and drafted sections of the article. K.H.M. revised the work critically for important intellectual content. All authors reviewed and approved the article before submission.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was supported by an unrestricted research grant from Gilead Sciences awarded to K.H.M.
References
- 1. Poteat T, Scheim A, Xavier J, et al. : Global epidemiology of HIV infection and related syndemics affecting transgender people. J Acquir Immune Defic Syndr 2016;72:S210–S219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grant RM, Lama JR, Anderson PL, et al. : Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010;363:2587–2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hare CB, Coll J, Ruane P, et al. : The Phase 3 DISCOVER study: Daily F/TAF or F/TDF for HIV preexposure prophylaxis. Abstract no. 104. Conference on Retroviruses and Opportunistic Infections (CROI); March 2019; Seattle, Washington. Available at https://www.croiconference.org/abstract/phase-3-discover-study-daily-ftaf-or-ftdf-hiv-preexposure-prophylaxis/ Accessed December20, 2020
- 4. Golub SA, Fikslin RA, Starbuck L, Klein A: High rates of PrEP eligibility but low rates of PrEP access among a national sample of transmasculine individuals. J Acquir Immune Defic Syndr 2019;82:e1–e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rowniak S, Ong-Flaherty C, Selix N, Kowell N: Attitudes, beliefs, and barriers to PrEP among trans men. AIDS Educ Prev 2017;29:302–314 [DOI] [PubMed] [Google Scholar]
- 6. Scheim AI, Santos GM, Arreola S, et al. : Inequities in access to HIV prevention services for transgender men: Results of a global survey of men who have sex with men. J Int AIDS Soc 2016;19:20779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Scheim AI, Travers R: Barriers and facilitators to HIV and sexually transmitted infections testing for gay, bisexual, and other transgender men who have sex with men. AIDS Care 2017;29:990–995 [DOI] [PubMed] [Google Scholar]
- 8. Sevelius J: “There's no pamphlet for the kind of sex I have”: HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. J Assoc Nurses AIDS Care 2009;20:398–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, et al. : Defining the HIV pre-exposure prophylaxis care continuum. AIDS 2017;31:731–734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McNairy ML, El-Sadr WM: A paradigm shift: Focus on the HIV prevention continuum. Clin Infect Dis 2014;59 Suppl 1:S12–S15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Finlayson T, Cha S, Xia M, et al. : Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men - 20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep 2019;68:597–603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kanny D, Jeffries WL, 4th, Chapin-Bardales J, et al. : Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men - 23 urban areas, 2017. MMWR Morb Mortal Wkly Rep 2019;68:801–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sullivan PS, Sanchez TH, Zlotorzynska M, et al. : National trends in HIV pre-exposure prophylaxis awareness, willingness and use among United States men who have sex with men recruited online, 2013 through 2017. J Int AIDS Soc 2020;23:e25461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Coy KC, Hazen RJ, Kirkham HS, et al. : Persistence on HIV preexposure prophylaxis medication over a 2-year period among a national sample of 7148 PrEP users, United States, 2015 to 2017. J Int AIDS Soc 2019;22:e25252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chan PA, Mena L, Patel R, et al. : Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc 2016;19:20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kelley CF, Kahle E, Siegler A, et al. : Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis 2015;61:1590–1597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Goedel WC, Halkitis PN, Greene RE, Duncan DT: Correlates of awareness of and willingness to use pre-exposure prophylaxis (PrEP) in gay, bisexual, and other men who have sex with men who use geosocial-networking smartphone applications in New York City. AIDS Behav 2016;20:1435–1442 [DOI] [PubMed] [Google Scholar]
- 18. Spinelli MA, Laborde N, Kinley P, et al. : Missed opportunities to prevent HIV infections among pre-exposure prophylaxis users: A population-based mixed methods study, San Francisco, United States. J Int AIDS Soc 2020;23:e25472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Krakower D, Maloney KM, Powell VE, et al. : Patterns and clinical consequences of discontinuing HIV preexposure prophylaxis during primary care. J Int AIDS Soc 2019;22:e25250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reisner SL, Perkovich B, Mimiaga MJ: A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDS 2010;24:501–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Murad MH, Elamin MB, Garcia MZ, et al. : Hormonal therapy and sex reassignment: A systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol (Oxf) 2010;72:214–231 [DOI] [PubMed] [Google Scholar]
- 22. White Hughto JM, Reisner SL, Pachankis JE: Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med 2015;147:222–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reisner SL, Moore CS, Asquith A, et al. : High risk and low uptake of pre-exposure prophylaxis to prevent HIV acquisition in a national online sample of transgender men who have sex with men in the United States. J Int AIDS Soc 2019;22:e25391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Centers for Disease Control and Prevention (CDC): 2017 Behavioral Risk Factor Surveillance System Questionnaire. Atlanta, GA: CDC, 2016 [Google Scholar]
- 25. James SE, Herman JL, Rankin S, et al. : The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC, National Center for Transgender Equality [Google Scholar]
- 26. Centers for Disease Control and Prevention (CDC). US Public Health Service: Preexposure Prophylaxis for the Prevention of HIV Infection in the United States—2017 Update: A Clinical Practice Guideline. Atlanta, GA: CDC, 2018 [Google Scholar]
- 27. Bush K, Kivlahan DR, McDonell MB, et al. : The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 1998;158:1789–1795 [DOI] [PubMed] [Google Scholar]
- 28. Kessler RC, Green JG, Gruber MJ, et al. : Screening for serious mental illness in the general population with the K6 screening scale: Results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res 2010;19 Suppl 1:4–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Reisner SL, Moore CS, Asquith A, et al. : Gender non-affirmation from cisgender male partners: Development and validation of a brief stigma scale for HIV research with transgender men who have sex with men (trans MSM). AIDS Behav 2020;24:331–343 [DOI] [PubMed] [Google Scholar]
- 30. Reisner SL, Hughto JM, Dunham EE, et al. : Legal protections in public accommodations settings: A critical public health issue for transgender and gender-nonconforming people. Milbank Q 2015;93:484–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Scheim AI, Bauer GR, Travers R: HIV-related sexual risk among transgender men who are gay, bisexual, or have sex with men. J Acquir Immune Defic Syndr 2017;74:e89–e96 [DOI] [PubMed] [Google Scholar]
- 32. Becasen JS, Denard CL, Mullins MM, et al. : Estimating the prevalence of HIV and sexual behaviors among the US transgender population: A systematic review and meta-analysis, 2006–2017. Am J Public Health 2019;109:e1–e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. The Fenway Institute: National LGBTQIA+ Health Education Center. Fenway Health. 2020. Available at https://www.lgbthealtheducation.org Accessed May28, 2020
- 34. Austin A, Craig SL, Navega N, McInroy LB: It's my safe space: The life-saving role of the internet in the lives of transgender and gender diverse youth. Int J Transgend Health 2020;21:33–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cipolletta S, Votadoro R, Faccio E: Online support for transgender people: An analysis of forums and social networks. Health Soc Care Community 2017;25:1542–1551 [DOI] [PubMed] [Google Scholar]