Abstract
Background
There is a paucity of literature addressing COVID-19 case-fatality ratios (CFR) by zip code (ZC). We aim to analyze trends in COVID-19 CFR, population density, and socioeconomic status (SES) indicators (unemployment, median household income) to identify ZCs heavily burdened by COVID-19.
Methods
Cross-sectional study to investigate the US prevalence of COVD-19 fatalities by ZC and SES. CFRs were calculated from state/county Departments of Health. Inclusion criteria were counties that reported cases/deaths by ZC and a CFR≥2%. This study was reported in line with the STROCSS criteria.
Results
609/1,853 ZCs, spanning 327 counties in 7 states had CFRs ≥2%. A significant positive correlation was found between the CFR and median household income (Pearson correlation:0.107; 95% CI [289.1,1937.9]; p < 0.001). No significant correlations exist between the CFR, and population/mi (Sen-Crowe et al., 2020) [2] or unemployment rate. Significant associations exist between the CFR and young males and elderly females without public insurance. CFR was inversely associated with persons aged <44 and individuals aged ≥65. The percentage of nursing homes (NHs) within cities residing within high CFR ZCs range from 8.7% to 67.6%.
Conclusion
Significant positive association was found between the CFR and median household income. Population/mi (Sen-Crowe et al., 2020) [2] and unemployment rates, did not correlate to CFR. NHs were heavily distributed in high CFR zip codes. We recommend the targeted vaccination of zip codes with a large proportion of long-term care facilities. Finally, we recommend for improved screening and safety guidelines for vulnerable populations (e.g nursing home residents) and established protocols for when there is evidence of substantial infectious spread.
Keywords: COVID-19, Case fatality rate, COVID-19 vaccination, Socio-economic status, Zip codes
Highlights
-
•
First national sampling of COVID-19 Case Fatality Ratio (CFR) at the zip code level.
-
•
Population density and unemployment rate did not correlate to COVID-19 CFR.
-
•
Significant positive correlation was found between CFR and median household income.
-
•
Nursing homes were concentrated in zip codes with high COVID-19 CFR.
-
•
States should make COVID-19 data available at the zip code level.
1. Background
The impact of COVID-19 on the United States (US) will likely plague the country longer than we anticipate [[1], [2], [3], [4], [5], [6], [7], [8]]. As of April 2nd, 2021, 554,069 COVID-19-related deaths out of 30,606,648 total confirmed cases, corresponds to a 1.8% case fatality ratio (CFR) [9]. Both acute and chronic health conditions disproportionately affect low socioeconomic status (SES) individuals [3,10,11] These findings may be related to distributional inhabitance [[12], [13], [14]].
Studies evaluating individual states and local areas have noted significant disparities among individuals who live in socioeconomically disadvantaged areas and have been able to analyze COVID-19 data at the county and zip code (ZC) level. Many studies found correlations between lower SES and higher infection rates and poorer outcomes. ZCs in South Florida, New York City, and Illinois, with particularly low SES and low mean household income (MHI saw an increased incidence rate ratio for COVID-19 compared to ZCs with higher SES and increased mean household income [15,16]. This trend of increased incidence rate ratio was also noted in ZCs in New York City and Michigan with an increased population of Black and Hispanic residents [17,18]. Studies have been able to highlight some specific factors that may attribute to the rapid spread of the virus, particularly percent crowding metrics for ZCs with lower SES. Areas with higher population densities saw amongst the highest rates of COVID-19 infection rates, as did areas with the most socioeconomic strain [16].
Furthermore, access to healthcare is a problem seen in low SES regions. Data collected before and during the pandemic revealed that there was a substantial difference between average number of ICU beds per population between predominantly White, higher SES neighborhoods and predominantly Black and Hispanic, lower SES neighborhoods in New York City [[19], [20], [21]]. Additionally, increased primary care physician density per county has been associated with lower COVID-19 death rates [22].
We hypothesized that there would be associations between COVID-19 CFR and population density, SES, other demographic variables and to our knowledge this is the first study to investigate this in a national sampling. This study will further apply these findings to the proportion of nursing homes that reside within zip codes heavily burdened by COVID-19 in order to determine if there are any trends in CFR and indicators of the elderly population.
2. Methods
2.1. Study design
Cross-sectional study utilizing publicly available data to investigate associations between CFR and SES indicators and demographics. We aim to identify ZCs heavily burdened by COVID-19 fatalities with consideration of the proportion of long-term care facilities for allocation of transmission prevention actions. This study was reported in line with the STOCSS criteria [23]. This work was submitted to the Research registry (UIN #: researchregistry6856) which can be found via the following link (https://www.researchregistry.com/browse-the-registry#home/registrationdetails/60abe32e274cad001ee00791/):
2.2. Zip code data collection & selection criteria
COVID-19 cases and fatalities were obtained by ZC via the state/county Department of Health (DOH) and/or state/county public health department as of December 23, 2020. Areas containing ZCs where the total number of COVID-19 cases and/or COVID-19 deaths were not available were excluded.
ZCs with a case-fatality ratio (CFR), the number of COVID-19 cases divided by the number of COVID-19 deaths, ≥2.0% were included in this study, as they represent areas experiencing greater COVID-19 burden compared to the national average of 1.8% at the time this data was collected [9].
2.3. Socioeconomic status (SES) and population data
Unemployment rates and MHI were obtained from the American Community Survey (AmCoS) 5-year data profiles, 2015–2019 [24]. The MHI and unemployment rates of the county the ZC resided within was used to indicate the SES status, according to the classification system set by the US Census Bureau. All SES and demographic attributes were linked to their respective ZC via their associated geographic identification codes (GEOIDs). Finally, population and ZC land area data were obtained from the Census Bureau ZC Tabulation Area (ZCTA) database and used to calculate population density defined as population/square mile (mi [2]) [25].
2.4. Nursing home data
Nursing home (NH) facilities were searched by using the Medicare website by ZC and classification system. These results were compared to compiled NH lists in individual local (state/county/city) DOH resources and simple percentages were calculated for included ZCs in the study [26].
2.5. Geospatial informational system (GIS) mapping
Blue Marble Geographics Global Mapper v20.0 was used for GIS mapping. We defined heavily COVID-19 burdened ZCs as those experiencing a CFR greater than the national average. ZC locations were plotted according to the ZCTAs. ZCTAs are generalized representations of ZCs that have been assigned to census blocks and representative of the geographic locations of populated areas [25]. ZCTA boundaries were constructed utilizing shapefiles (.shp) and geodatabases (.gdb) from TIGER/Line Shapefiles [25,27]. In addition, the TIGER/Line Database was utilized to stratify county areas including/surrounding the ZCs as the following: urban cluster areas (2,500-<50,000 population), urbanized areas (50,000–99,999 population), and metropolitan areas (≥100,000 population). Demographic, population, and SES (e.g. unemployment rate, MHI, etc.) attributes obtained from the AmCoS were linked to the ZCTAs via their associated GEOIDs. Attributes (e.g. CFR, population, urbanized areas, ZCTA boundaries, etc.) were superimposed in layers in order to generate a geospatial representation of ZCs heavily burdened with COVID-19. Finally, ZC locations were further classified by US region (Northeast, Midwest, South, West) as defined by the US Census Bureau.
2.6. Statistical analysis
IBM SPSS Statistics v26.0 (Armonk, NY) was used for statistical analysis. Analysis of variance (ANOVA) was used to evaluate differences in CFR, MHI, Unemployment Rate, and Population/mi [2], and corresponding US Census Bureau region. In addition, linear regression analysis was used in order to determine any significant correlations between the four analyzed variables. Significance was defined as p < 0.05. This study was conducted in compliance with ethical standards and deemed exempt by our Institutional Review Board.
3. Results
Fourteen states offered data by ZC of which only three states (North Carolina, Oklahoma, and New Jersey) reported both total cases and total deaths by ZC for the entire state. Apart from those, four states (California, Illinois, Washington, and New York) reported total cases and total deaths by ZC for ≥1 county, which were also included in this study.
In total, we included 327 counties that spanned the above seven states. 609/1,853 (32.9%) total ZCs had CFRs ≥2% and were included in subsequent analyses.
3.1. Northeast region
A total of 328 ZCs in New York City, NY (168) and New Jersey (160) represented the Northeast region. All ZCs were contained within metropolitan divisions (Fig. 1, Fig. 2). The average CFR and population/mi [2] were 5.9% and 25,635, respectively. (Fig. 1ab,2 ab) In addition, the average MHI was $78,925, and the unemployment rate was 6.0%. (Fig. 1cd,2cd).
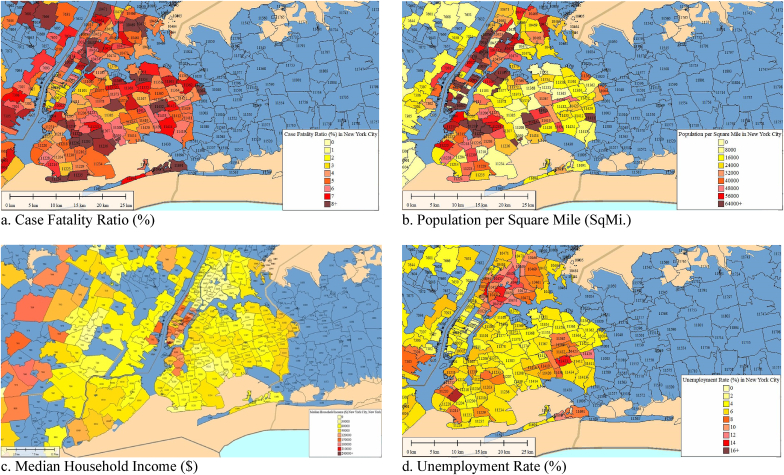
Fig. 1.
Case-Fatality Ratio, Population/mi2, Median Household Income, and Unemployment Rate in New York City, New York. A total of 168 zip codes were included. The average CFR was 5.6% and ranged from 1.5% to 6.2%. The population/mi2 ranged from 12,944–128,616, with an average of 43,469. Additionally, the average median household income and unemployment rate was $73,980 (Range: $21,447-$250,000) and 6.2% (Range: 0.4%–15.2%), respectively.
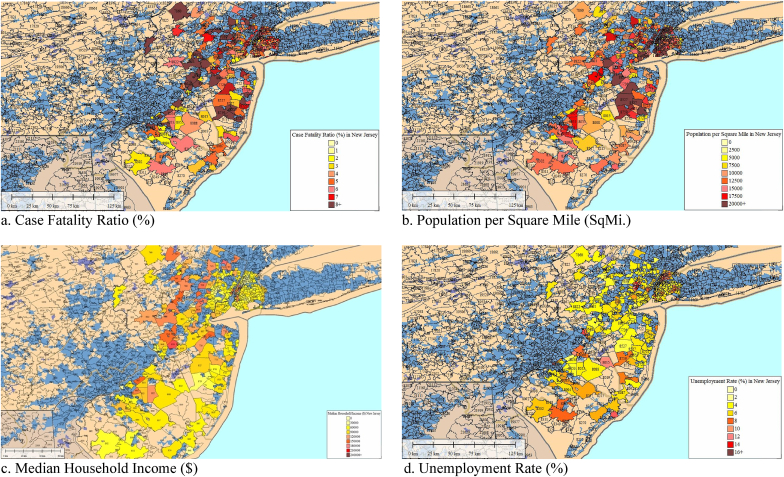
Fig. 2.
Case-Fatality Ratio, Population/mi2, Median Household Income, and Unemployment Rate in New Jersey. A total of 160 zip codes were included. The average CFR was 6.1% and ranged from 2.0% to 17.8%. The population/mi2 ranged from 173 to 53,316, with an average of 6,909. Additionally, the average median household income and unemployment rate was $80,763 (Range: $29,232-$154,688) and 5.8% (Range: 2.7%–17.4%), respectively.
3.2. West region
A total of 51 ZCs in King County, Washington (26) and Orange County, California (25) represented the West region. All analyzed ZCs were contained within a metropolitan division (Fig. 3, Fig. 4). The average CFR and population/mi [2] was 5.2% and 6,134, respectively. (Fig. 3ab,4 ab) In addition, the average MHI was $103,132 and the unemployment rate was 4.0%. (Fig. 3cd,4cd).
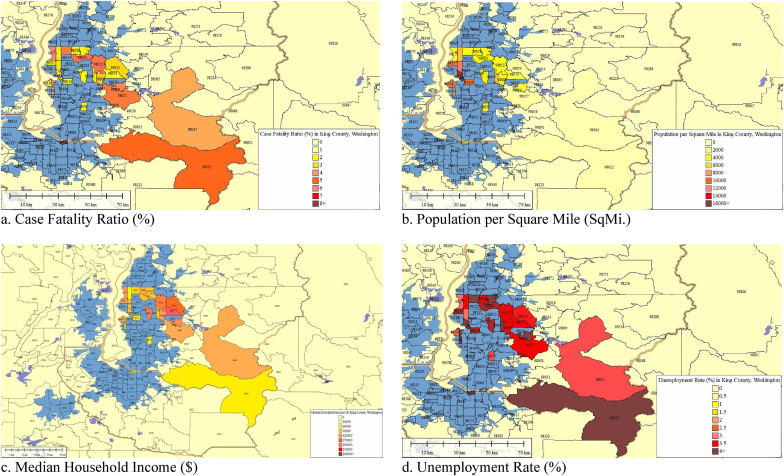
Fig. 3.
Case-Fatality Ratio, Population/mi2, Median Household Income, and Unemployment Rate in King County, Washington. A total of 26 zip codes were included. The average CFR was 3.6% and ranged from 2.0% to 9.1%. The population/mi2 ranged from 45.5 to 26,984, with an average of 6,568 population/mi2. Additionally, the average median household income and unemployment rate was $105,633 (Range: $68,994-$188,900) and 3.7% (Range: 2.7%–4.6%), respectively.
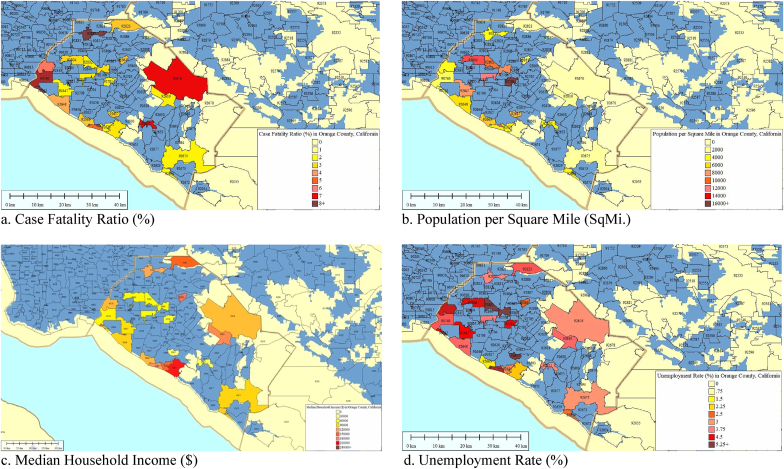
Fig. 4.
Case-Fatality Ratio, Population/mi2, Median Household Income, and Unemployment Rate in Orange County, California. A total of 25 zip codes were included. The average CFR was 6.9% and ranged from 2.2% to 57.1%. The population/mi2 ranged from 31.2 to 16,684, with an average of 2,682 population/mi2. Additionally, the average median household income and unemployment rate was $100,531 (Range: $36,824-$204,291) and 4.3% (Range: 1.9%–8.9%), respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
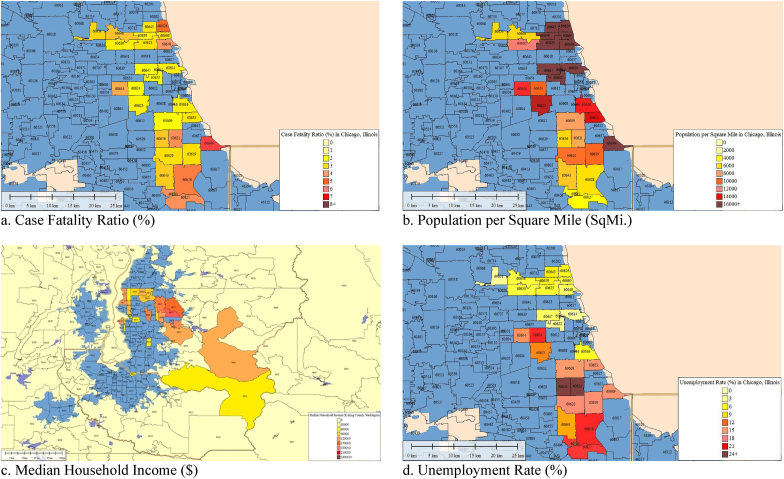
3.3. Midwest region
A total of 26 ZCs within Chicago, Illinois, represented the Midwest region. All ZCs were contained within a metropolitan division (Fig. 5). The average CFR and population/mi [2] was 3.22% and 14,823, respectively. (Fig. 5ab) In addition, the average MHI was $53,259 and the unemployment rate was 11.0%. (Fig. 5cd).
Fig. 5.
Case-Fatality Ratio, Population/mi2, Median Household Income, and Unemployment Rate in Chicago, Illinois. A total of 26 zip codes were included. The average CFR was 3.2% and ranged from 2.0% to 6.5%. The population/mi2 ranged from 4,069–34,229, with an average of 14,823 population/mi2. Additionally, the average median household income and unemployment rate was $53,259 (Range: $22,158-$117,138) and 11.0% (Range: 2.5%–27.2%), respectively.
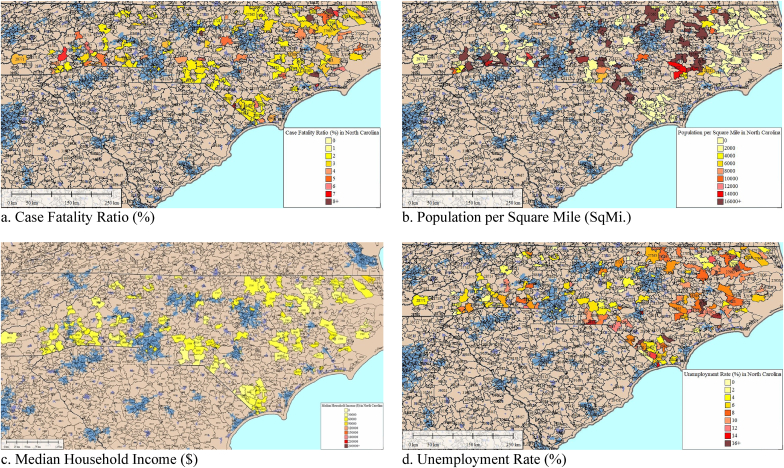
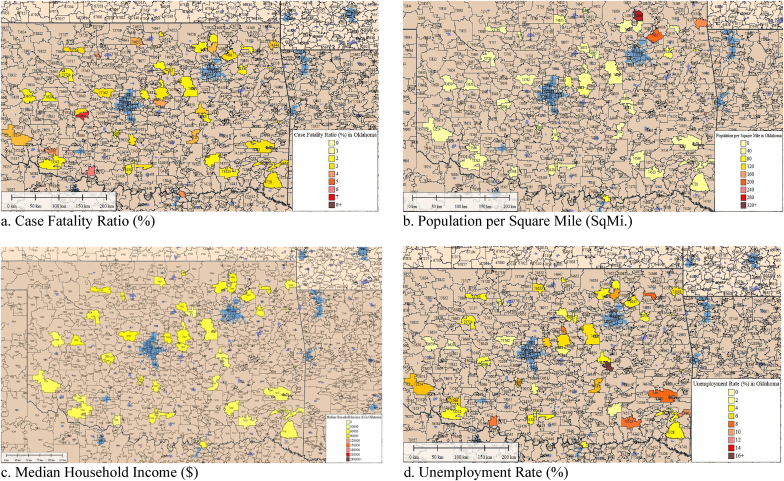
3.4. South region
A total of 204 ZCs in Oklahoma (43) and North Carolina (161) represented the South region. 97 ZCs are contained within urbanized areas and 22 ZCs contained in an urbanized cluster. The remaining 85 ZCs were not contained within an urban cluster, urbanized area, or metropolitan division. Oklahoma did not contain any ZCs within metropolitan divisions or urbanized areas (Fig. 6, Fig. 7). The average CFR and population/mi [2] was 3.19% and 19,506, respectively. (Fig. 6ab,7 ab) In addition, the average MHI was $46,432 and the unemployment rate was 6.7%. (Fig. 6cd,7cd).
Fig. 6.
Case-Fatality Ratio, Population/mi2, Median Household Income, and Unemployment Rate in North Carolina. A total of 161 zip codes were included. The average CFR was 3.3% and ranged from 2.0% to 9.8%. The average population/mi2 was 25,239. Additionally, the average median household income and unemployment rate was $46,316 (Range: $19,954-$86,250) and 7.1% (Range: 0.0%–36.0%), respectively.
Fig. 7.
Case-Fatality Ratio, Population/mi2, Median Household Income, and Unemployment Rate in Oklahoma. A total of 43 zip codes were included. The average CFR was 3.0% and ranged from 2.0% to 6.6%. The average population/mi2 was 42.4 and ranged from 5.0 to 302.9. Additionally, the average median household income and unemployment rate was $46,863 (Range: $31,923-$66,323) and 5.4% (Range: 0.0%–29.5%), respectively.
3.5. Nursing homes
The percentage of NHs within a city that reside within the ZCs included in this study range from 8.7% to 67.6%. In New York City, 169/250 (67.6%) NHs resided within heavily burdened ZCs. 234/366 (63.9%) of NHs in New Jersey resided within heavily burdened ZCs, followed by Chicago (64/129 = 49.6%), King County, Washington (25/52 = 48.0%), Orange County, California (32/75 = 42.7%), North Carolina (147/423 = 34.8%), and Oklahoma (25/288 = 8.7%).
Multiple significant differences in regional CFR (f(3,95.4) = 82.8; p < 0.001), population/mi [2] (f(3,128.3) = 47.1; p < 0.001), MHI (f(3,83.8) = 117.4; p < 0.001), and Unemployment Rate (f(3,97.0) = 38.8; p < 0.001) exist.
3.6. Case fatality rate
The overall mean CFR across all regions was 4.7%. The Northeast region (μ = 5.9%) exhibited a significantly higher mean CFR than the South (μ = 3.2%) and Midwest regions (μ = 3.2%) (Table 1). Significant inverse correlations were found between CFRs and the proportion of persons aged <44 years old (Pearson Correlation = −0.049; 95% CI [-0.193,-0.025]; p = 0.011) and the proportion of elderly individuals aged ≥65 (Pearson Correlation = −0.033; 95% CI [-0.222,-0.046]; p = 0.011). These results are consistent with the regional CFRs, as the Midwest region exhibited significantly larger proportions of persons aged <44 than all other regions and would be expected to demonstrate an inverse correlation. Similarly, the South region exhibited significantly larger proportions of elderly individuals than the Midwest and Northeast regions, but not the West region.
Table 1.
Comparison of the case fatality ratio (%) by U.S. Region.
| Census Region | Mean Difference | 95% Confidence Interval of Mean |
Significance | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| South Region | Midwest Region | 0.022 | −0.58 | 0.63 | 1.000 |
| West Region | −2.01 | −4.98 | 0.96 | 0.286 | |
| Northeast Region | −2.65 | −3.09 | −2.20 | 0.0001 | |
| Midwest Region | South Region | −0.022 | −0.63 | 0.58 | 1.000 |
| West Region | −2.03 | −5.03 | 0.97 | 0.287 | |
| Northeast Region | −2.67 | −3.33 | −2.01 | 0.0001 | |
| West Region | South Region | 2.01 | −0.96 | 4.98 | 0.286 |
| Midwest Region | 2.03 | −0.97 | 5.03 | 0.287 | |
| Northeast Region | −0.64 | −3.62 | 2.34 | 0.941 | |
| Northeast Region | South Region | 2.65 | 2.20 | 3.09 | 0.0001 |
| Midwest Region | 2.67 | 2.01 | 3.33 | 0.0001 | |
| West Region | 0.64 | −2.34 | 3.62 | 0.941 | |
A significant inverse correlation was found between CFR and males aged <44 without public health insurance (Pearson Correlation = −0.134; 95% CI [0.014,0.351]; p = 0.034). The Northeast displayed significantly smaller proportions of young males aged <44 without health insurance than all other regions and is consistent with the regional CFR and inverse association. In contrast, the West displayed significantly larger proportions of persons aged ≥65 than all other regions.
However, a significant direct correlation was found between CFR and females over the age of 65 who did not have public health insurance (Pearson Correlation = 0.142; 95% CI [0.262,2.792]; p = 0.018). Consistent with these results, the Northeast region displayed significantly larger proportions of elderly females without public health insurance than all other regions. No significant correlations were found between CFRs and race.
3.7. Population/square mile
The nationwide mean was 21,537 population/mi [2]. The Northeast region (μ = 25,634.8 population/mi [2]) exhibited a significantly larger population/mi [2] than the Midwest region (μ = 14,823.1 population/mi [2]). In addition, the Northeast, South (μ = 19,506.3 population/mi [2]) and Midwest regions displayed a significantly larger population/mi [2] than the West region (μ = 6,133.8 population/mi [2]). (Table 2)
Table 2.
Comparison of the population per square mile by U.S. Region.
| Census Region | Mean Difference | 95% Confidence Interval of Mean |
Significance | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| South Region | Midwest Region | 4683.24 | −5303.37 | 14669.84 | 0.618 |
| West Region | 13372.46 | 4125.14 | 22619.78 | 0.001 | |
| Northeast Region | −6128.50 | −16024.57 | 3767.58 | 0.380 | |
| Midwest Region | South Region | −4683.24 | −14669.84 | 5303.37 | 0.618 |
| West Region | 8689.22 | 3870.02 | 13508.42 | 0.0001 | |
| Northeast Region | −10811.74 | −16729.97 | −4893.50 | 0.0001 | |
| West Region | South Region | −13372.46 | −22619.78 | −4125.14 | 0.001 |
| Midwest Region | −8689.22 | −13508.42 | −3870.02 | 0.0001 | |
| Northeast Region | −19500.96 | −23957.66 | −15044.25 | 0.0001 | |
| Northeast Region | South Region | 6128.50 | −3767.58 | 16024.57 | 0.380 |
| Midwest Region | 10811.74 | 4893.4993 | 16729.97 | 0.0001 | |
| West Region | 19500.96 | 15044.25 | 23957.66 | 0.0001 | |
3.8. Median household income
The overall MHI across all ZCs was $69,030. The West region (μ = $103,132) displayed a significantly higher MHI than the Northeast (μ = $78,925), South (μ = $46,432), and Midwest regions (μ = $53,259). In addition, the Northeast region exhibited a significantly higher average MHI than the Midwest and South regions (Table 3). No significant associations exist between the Midwest and South regions.
Table 3.
Comparison of the median household income ($) by U.S. Region.
| Census Region | Mean Difference | 95% Confidence Interval of Mean |
Significance | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| South Region | Midwest Region | −6,827.13 | −21,226.88 | 7,572.62 | 0.571 |
| West Region | −56,699.88 | −69,837.68 | −43,562.09 | 0.0001 | |
| Northeast Region | −32,492.43 | −37,774.93 | −27,209.93 | 0.0001 | |
| Midwest Region | South Region | 6,827.13 | −7,572.62 | 21,226.88 | 0.571 |
| West Region | −49,872.75 | −68,646.47 | −31,099.04 | 0.0001 | |
| Northeast Region | −25,665.30 | −40,585.62 | −10,744.99 | 0.0001 | |
| West Region | South Region | 56,699.88 | 43,562.09 | 69,837.68 | 0.0001 |
| Midwest Region | 49,872.75 | 31,099.04 | 68,646.47 | 0.0001 | |
| Northeast Region | 24,207.45 | 10,449.21 | 37,965.69 | 0.0001 | |
| Northeast Region | South Region | 32,492.43 | 27,209.93 | 37,774.93 | 0.0001 |
| Midwest Region | 25,665.30 | 10,744.99 | 40,585.62 | 0.0001 | |
| West Region | −24,207.45 | −37,965.69 | −10,449.21 | 0.0001 | |
3.9. Unemployment rate
The average unemployment rate was 6.3%. The Midwest region (μ = 11.0%) exhibited a significantly larger average unemployment rate than the South (μ = 6.7%), West (μ = 4.0%), and Northeast regions (μ = 6.0%). In addition, the Northeast region displayed a significantly higher average unemployment rate than the West region. No significant difference existed between the Northeast and South region (Table 4).
Table 4.
Comparison of the unemployment rate (%) by U.S. Region.
| Census Region | Mean Difference | 95% Confidence Interval of Mean |
Significance | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| South Region | Midwest Region | −4.32 | −8.39 | −0.26 | 0.034 |
| West Region | 2.72 | 1.75 | 3.68 | 0.0001 | |
| Northeast Region | 0.66 | −0.28 | 1.61 | 0.269 | |
| Midwest Region | South Region | 4.32 | 0.26 | 8.39 | 0.034 |
| West Region | 7.04 | 3.03 | 11.05 | 0.0001 | |
| Northeast Region | 4.99 | 0.98 | 8.99 | 0.011 | |
| West Region | South Region | −2.72 | −3.68 | −1.75 | 0.0001 |
| Midwest Region | −7.04 | −11.05 | −3.03 | 0.0001 | |
| Northeast Region | −2.05 | −2.64 | −1.46 | 0.0001 | |
| Northeast Region | South Region | −0.66 | −1.61 | 0.28 | 0.269 |
| Midwest Region | −4.99 | −8.99 | −0.98 | 0.011 | |
| West Region | 2.05 | 1.46 | 2.64 | 0.0001 | |
A weak but significant positive correlation was found between CFRs and MHI (Pearson correlation:0.107; 95% CI [289.1,1937.9]; p < 0.001). In addition, there was a moderate negative and significant correlation between the unemployment rate and MHI (Pearson correlation: −0.336; 95% CI [-3492.3,-2214.4]; p < 0.001). No significant correlations exist between CFRs, and population/mi [2] or unemployment rate.
4. Discussion
The Northeast region exhibited the largest CFR (5.9%), then the West (5.2%), Midwest (3.22%), and South (3.19%) region. The Northeast mean CFR was significantly larger than the Midwest and South regions. The Northeast exhibited the largest population/mi [2] (25,635), followed by the South (19,506), Midwest (14,823), and West (6,134) region. Our results varied slightly from other studies. Another study found the Northeast exhibited the largest CFR (5.9%), then the Midwest (5.6%), West (5.1%) and South (5.05%) [28]. One possible explanation of this inconsistency is the ZCs representing the West region reside within metropolitan areas, where larger population densities can facilitate increased spread and elevated CFRs. On the other hand, our data may suggest that some COVID-19 data interpretations at the county level may mask harder hit communities and trends in local infection rates and mortality.
In contrast to other studies, we did not find significant associations between CFR and race [29]. Our study was limited by the small sample size and narrow area designations (metropolitan vs. urban vs. rural). We recommend states make CFR reporting consistent at ZC levels for more granular analysis.
Our study found a significant inverse correlation between CFR and individuals aged <44 as well as CFR and individuals aged ≥65. When controlled by gender, there was a significant direct correlation between CFR and females with no public insurance aged ≥65. The association seen between CFR and elderly individuals is inconsistent with previous studies; however, the association seen between CFR and young individuals is consistent with prior literature [[30], [31], [32]]. This inconsistency may be due to a limited sample size. Our study also did not control for comorbid health conditions, which would likely affect CFR.
The West region displayed significantly higher MHIs than the other regions. In addition, the Northeast region exhibited a significantly higher MHI than the South and Midwest regions. A statistically significant weak positive correlation was found between CFRs and average MHI. This correlation is inconsistent with other studies that concluded death rates to be significantly higher, in areas with substantially non-White populations with substantially low measures of SES [33]. Likewise, other studies have related higher SES with reduced risk of mortality [34]. As the only national sampling of US ZCs, this could be novel information not found in smaller studies. This disparity could also be due to two other factors. First, the majority of ZCs with available COVID-19 data resided within metropolitan areas which may facilitate increased rates of infection, leading to greater CFRs. Additionally, individuals in metropolitan areas have been shown to have larger incomes than those in nonmetropolitan areas and, therefore a higher SES [35]. Thus, it is possible that this inconsistency is a result of sampling bias due to the limited availability of COVID-19 data by ZC. Second, our sample size only comprises ~1.5% (609/42,000) of all US ZCs [36]. It is possible that the relatively small number of ZCs with available data were not representative of their respective US region.
The Midwest region exhibited a significantly larger unemployment rate than other regions. In addition, the Northeast region displayed a significantly higher average unemployment rate than the West region. There was a statistically significant moderate negative correlation between unemployment rate and MHI. This is expected, as higher unemployment rates inversely correlate with MHI across an area [37]. The ZCs we identified to be heavily burdened by COVID-19 contain a substantial percentage of the respective state's NHs. The percentage of NHs included in the ZCs analyzed are most apparent in the states representing the Northeast and Midwest regions. The increased CFR demonstrated in ZCs with a high density of NHs is consistent with previous literature demonstrated significantly higher CFRs in the elderly, sometimes almost four times that of the average population, and worsen after age 60 [38,39].
The reasons behind this increased CFR are likely multifactorial. As we age, the immune system becomes less robust, with diminished function and production of lymphocytes and other components [40]. However, this effect has been well-demonstrated across many viral illnesses, such as influenza, and is not something easily prevented [41]. The elderly population is also significantly more likely to have comorbid health conditions, such as hypertension, diabetes, pulmonary disease, and heart disease, all of which have been shown to correlate with increased rates of severe disease and increased mortality in Covid-19 patients.[[42], [43], [44]]
Most importantly, the CDC reports that there has been increased incidence of Covid-19 both in nursing homes and communities surrounding nursing homes when compared to the average population [45]. Increased incidence was attributed to insufficient contact and safety guidelines - over one-third of high-risk exposures for staff members involved household or social contacts, which indicated lapses in masking and other social distancing guidelines. Also, limited supplies of personal protective equipment and their proper use may factor into the high transmission rates that were largely preventable in the early stages of the pandemic. In the light of new masking guidelines, we feel that it is important to continue educating NH staff members about community exposure risks, the importance of masking in high-risk exposure environments, and stringent screening protocols in nursing homes including continued routine testing, COVID-19 status, and temperature screening. We recommend for improved education of staff members working in nursing homes regarding the risks of community exposures and the importance of adhering to safety and social distancing guidelines, in accordance with the recommendations of the CDC [45].
Our study has limitations. First, 36/50 (72%) states do not offer comprehensive COVID-19 data at ZC levels. The majority of ZCs analyzed resided within metropolitan divisions and are not representative of entire regions. Moreover, when considering the available data regarding the number of NHs in each state, our search relied on Medicare.gov and local DOH resources, where inconsistencies in how they define NHs or reported NHs deaths may exist. Furthermore, our relatively small sample size limits our ability to generalize trends across the US. Additionally, it is important to contemplate that patients may seek care outside of their residential areas, affecting ZC data.
We have several recommendations. First, we recommend for states to make data publicly available at ZC levels. Second, future investigations should include demographic characteristics by ZC, which could provide for a more specific targeted strategy. Third, states are encouraged to provide information NHs within their state. In the event of another public health emergency, we recommend for nationwide prioritization of the vaccination of high-risk populations, particularly those residing in long-term care facilities and for all SES members [12,31,32,46,47]. Finally, we recommend for improved, consistent health screening and safety protocols for vulnerable populations, such as NH residents in future emergency situations. In addition, safety protocols may include specific guidelines for those working in nursing homes who may place the residents at risk of infection. Our study demonstrates correlations between CFR with those aged 65 and older and revealed high proportions of nursing homes within these zip codes. These results provide evidence for the substantial risk placed on these populations and call for improved safety protocols to match the elevated risk. By learning from the past year and a half and implementing aggressive preventative guidelines, we can minimize the number of preventable deaths early on in the event of another tremendous surge in COVID-19 cases.
5. Conclusion
CFRs ranged from 3.1% in the West region to 5.9% in the Northeast region. The West region displayed a significantly larger median household income than other regions and the lowest population density, whereas the Northeast exhibited the highest population density. A significant weak positive correlation was found between CFRs and median household income and no correlation was found between population density and unemployment status. These novel findings may be due to a lack of available COVID-19 data at the zip code level nationwide, which is required to make generalizable claims about regions as a whole. This study emphasizes the need for states to make COVID-19 data available at the zip code level. In addition, the percentage of a state's nursing homes residing within zip codes heavily burdened by COVID-19 ranged from 8.7%, up to 67.6% in New York City. Zip code analysis can help with identifying COVID-19 risk groups and locations, including long-term care facilities towards targeted vaccine distribution. Most importantly, we recommend for improved and more stringent screening and safety practices, such as distancing protocols and sanitation guidelines for those living and working in nursing homes when there is evidence of infectious spread.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
This study was conducted in compliance with ethical standards, reviewed by our institutional review board and deemed exempt.
Source of funding
None.
Author contribution
Study design and conception: AE. Data collection, interpretation and analysis: BS, IL, RA, MM, AE. Manuscript preparation: BS, IL, RA, MM, AE. Critical revision of manuscript: BS, IL, RA, MM, AE. All authors read and approved the final manuscript.
Trial registry number
Not applicable.
Guarantor
Mark McKenney.
Adel Elkbuli.
Declaration of competing interest
Authors declare no competing interests.
References
- 1.Boserup B., McKenney M., Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sen-Crowe B., McKenney M., Elkbuli A. Social distancing during the COVID-19 pandemic: staying home save lives. Am. J. Emerg. Med. 2020;38(7):1519–1520. doi: 10.1016/j.ajem.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boserup B., McKenney M., Elkbuli A. The financial strain placed on America's hospitals in the wake of the COVID-19 pandemic [published online ahead of print, 2020 Jul 9] Am. J. Emerg. Med. 2020;S0735–6757(20):30601–X. doi: 10.1016/j.ajem.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sen-Crowe B., Sutherland M., McKenney M., Elkbuli A. A closer look into global hospital beds capacity and resource shortages during the COVID-19 pandemic. J. Surg. Res. 2021;260:56–63. doi: 10.1016/j.jss.2020.11.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sutherland M., McKenney M., Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: what has changed? Am. J. Emerg. Med. 2020;38(9):1710–1714. doi: 10.1016/j.ajem.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Sutherland M., McKenney M., Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York city, Chicago, los angeles and baltimore. Am. J. Emerg. Med. 2021;39:225–226. doi: 10.1016/j.ajem.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 Map. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html. Published January 22, 2020. Accessed April 2nd, 2021.
- 10.Populations and Vulnerabilities . 2020 Apr 29. Centers for Disease Control and Prevention.https://ephtracking.cdc.gov/showPcMain.action#:~:text=Socioeconomics,birth%20and%20throughout%20their%20lives [Google Scholar]
- 11.Price J.H., Khubchandani J., Webb F.J. Poverty and health disparities: what can public health professionals do? Health Promot. Pract. 2018 Mar;19(2):170–174. doi: 10.1177/1524839918755143. Epub 2018 Jan 24. PMID: 29363333. [DOI] [PubMed] [Google Scholar]
- 12.Williams D.R. Miles to go before we sleep: racial inequities in health. J. Health Soc. Behav. 2012 Sep;53(3):279–295. doi: 10.1177/0022146512455804. PMID: 22940811; PMCID: PMC3712789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United States Census Bureau . United States Census Bureau; 2018. American Community Survey 5-year Estimate.https://www.census.gov/en.html Available at: Published 2018. Accessed 2020. [Google Scholar]
- 14.Diez Roux A.V. Investigating neighborhood and area effects on health. Am. J. Publ. Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palacio A., Tamariz L. Social determinants of health mediate COVID-19 disparities in South Florida. J. Gen. Intern. Med. 2020:1–6. doi: 10.1007/s11606-020-06341-9. Epub ahead of print. PMID: 33206324; PMCID: PMC7673244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen J.T., Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J. Publ. Health Manag. Pract. 2021;27(Suppl 1):S43–S56. doi: 10.1097/PHH.0000000000001263. COVID-19 and Public Health: Looking Back, Moving Forward. PMID: 32956299. [DOI] [PubMed] [Google Scholar]
- 17.Whittle R.S., Diaz-Artiles A. An ecological study of socioeconomic predictors in detection of COVID-19 cases across neighborhoods in New York City. BMC Med. 2020 Sep 4;18(1):271. doi: 10.1186/s12916-020-01731-6. PMID: 32883276; PMCID: PMC7471585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akanbi M.O., Rivera A.S., Akanbi F.O., Shoyinka A. An ecologic study of disparities in COVID-19 incidence and case fatality in oakland county, MI, USA, during a state-mandated shutdown. J Racial Ethn Health Disparities. 2020:1–8. doi: 10.1007/s40615-020-00909-1. Epub ahead of print. PMID: 33124003; PMCID: PMC7595050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guha A., Bonsu J., Dey A., Addison D. Community and Socioeconomic Factors Associated with COVID-19 in the United States: zip code level cross sectional analysis. medRxiv [Preprint] 2020 doi: 10.1101/2020.04.19.20071944. Apr 22:2020.04.19.20071944. PMID: 32511646; PMCID: PMC7277002. [DOI] [Google Scholar]
- 20.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. J. Am. Med. Assoc. 2020 Jun 23;323(24):2466–2467. doi: 10.1001/jama.2020.8598. PMID: 32391864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Douglas J.A., Subica A.M. COVID-19 treatment resource disparities and social disadvantage in New York City. Prev. Med. 2020 Dec;141:106282. doi: 10.1016/j.ypmed.2020.106282. Epub 2020 Oct 6. PMID: 33035550; PMCID: PMC7536513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ojinnaka C.O., Adepoju O.E., Burgess A.V., Woodard L. Factors associated with COVID-related mortality: the case of Texas. J Racial Ethn Health Disparities. 2020 doi: 10.1007/s40615-020-00913-5. Epub ahead of print. PMID: 33169310; PMCID: PMC7651831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., for the STROCSS Group The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. https://www.census.gov/programs-surveys/acs Data Tables & Tools. American Community Survey. Accessed December 23, 2020. [DOI] [PubMed] [Google Scholar]
- 24.Zip Code Tabulation Areas (ZCTAs). United States Census Bureau. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/zctas.html? Accessed December 23, 2020.
- 25.Medicare Nursing Home Provider List. Medicare.gov. https://www.medicare.gov/care-compare/Accessed December 23, 2020.
- 26.TIGER/Line Shapefiles. United States Census Bureau. https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.html. Accessed December 23, 2020.
- 27.Ahmed R., Williamson M., Hamid M.A., Ashraf N. United States county-level COVID-19 death rates and case fatality rates vary by region and urban status. Healthcare (Basel) 2020;8(3):330. doi: 10.3390/healthcare8030330. Published 2020 Sep. 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boserup B., McKenney M., Elkbuli A. Disproportionate impact of COVID-19 pandemic on racial and ethnic minorities. Am. Surg. 2020;86(12):1615–1622. doi: 10.1177/0003134820973356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levin A.T., Hanage W.P., Owusu-Boaitey N., Cochran K.B., Walsh S.P., Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur. J. Epidemiol. 2020 Dec;35(12):1123–1138. doi: 10.1007/s10654-020-00698-1. Epub 2020 Dec 8. PMID: 33289900; PMCID: PMC7721859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghisolfi S., Almås I., Sandefur J.C., von Carnap T., Heitner J., Bold T. Predicted COVID-19 fatality rates based on age, sex, comorbidities and health system capacity. BMJ Glob Health. 2020 Sep;5(9) doi: 10.1136/bmjgh-2020-003094. PMID: 32912856; PMCID: PMC7482102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. J. Am. Med. Assoc. 2020 May 12;323(18):1775–1776. doi: 10.1001/jama.2020.4683. Erratum in: JAMA. 2020 Apr 28;323(16):1619. PMID: 32203977. [DOI] [PubMed] [Google Scholar]
- 32.Adhikari S., Pantaleo N.P., Feldman J.M., Ogedegbe O., Thorpe L., Troxel A.B. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw Open. 2020 Jul 1;3(7) doi: 10.1001/jamanetworkopen.2020.16938. PMID: 32721027; PMCID: PMC7388025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hawkins R.B., Charles E.J., Mehaffey J.H. Socio-economic status and COVID-19-related cases and fatalities. Publ. Health. 2020 Dec;189:129–134. doi: 10.1016/j.puhe.2020.09.016. Epub 2020 Oct 17. PMID: 33227595; PMCID: PMC7568122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Personal Income by County and Metropolitan Area. Bureau of Economic Analysis; 2019. https://www.bea.gov/news/2020/personal-income-county-and-metropolitan-area-2019 November 17, 2020. Accessed January 8, 2020. [Google Scholar]
- 35.Postal Facts. United States Postal Service. https://facts.usps.com/42000-zip-codes/. Accessed January 8, 2020.
- 36.Terry S. Unemployment and its effect on family income in 1980. Mon. Labor Rev. 1982:35–43. https://www.bls.gov/opub/mlr/1982/04/art5full.pdf [Google Scholar]
- 37.Kang S.J., Jung S.I. Age-related morbidity and mortality among patients with COVID-19. Infect Chemother. 2020;52(2):154–164. doi: 10.3947/ic.2020.52.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Montecino-Rodriguez E., Berent-Maoz B., Dorshkind K. Causes, consequences, and reversal of immune system aging. J. Clin. Invest. 2013;123(3):958–965. doi: 10.1172/JCI64096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Freitas A.R.R., Donalisio M.R. Excess of mortality in adults and elderly and circulation of subtypes of influenza virus in southern Brazil. Front. Immunol. 2018;8:1903. doi: 10.3389/fimmu.2017.01903. Published 2018 Jan 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davis J.W., Chung R., Juarez D.T. Prevalence of comorbid conditions with aging among patients with diabetes and cardiovascular disease. Hawaii Med. J. 2011;70(10):209–213. [PMC free article] [PubMed] [Google Scholar]
- 42.Dai S.P., Zhao X., Wu Jh. Effects of comorbidities on the elderly patients with COVID-19: clinical characteristics of elderly patients infected with COVID-19 from sichuan, China. J. Nutr. Health Aging. 2021;25:18–24. doi: 10.1007/s12603-020-1486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Makary M. Risk factors for COVID-19 mortality among privately insured patients. FAIR Health White Paper. 2020 [Google Scholar]
- 44.Bagchi S., Mak J., Li Q. Rates of COVID-19 among residents and staff members in nursing homes — United States, may 25–november 22, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021;70:52–55. doi: 10.15585/mmwr.mm7002e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.States Plan for Vaccinating their Populations against COVID-19 . 2020. National Academy for State Health Policy.https://www.nashp.org/each-states-plan-for-vaccinating-its-populations-against-covid-19/ Updated December 18. Accessed January 4, 2021. [Google Scholar]
- 46.ACIP Presentation Slides . vol. 1. 2020. Meeting. Centers for Disease Control and Prevention.https://www.cdc.gov/vaccines/acip/meetings/slides-2020-12.html Accessed January 4, 2021. [Google Scholar]
- 47.Resources Vaccination Planning. American College of Physicians. January. 2021. https://assets.acponline.org/coronavirus/scormcontent/?&_ga=2.59967405.1227884443.1608736866-1332072176.1608736866#/lessons/kwJbUTKXK1SULXbRPFsZbpMAMKMMXgV9 4. Accessed January 4, 2021.