Abstract
An online questionnaire survey was used to assess the application of noninvasive strategies in the management of COVID-19 patients. We found a marked increase in the proportion of facilities using high flow nasal cannula (HFNC) oxygen therapy successfully in the 3rd epidemic wave as compared to the 1st wave (49% vs. 12%) and rare reports of associated nosocomial infection in the medical personnel. Furthermore, the proportion of facilities using HFNC as first-line therapy for half or more than half of their patients who did not respond to conventional oxygen therapy increased from 9% in the first to 33% in the second survey. Conversely, the rate of mechanical ventilation with intubation usage following conventional oxygen therapy failure decreased from 62% to 54%. These changes could be due to the limited medical resources available during the larger 3rd wave coupled with increased internal reports on the success of HFNC.
Keywords: High flow nasal cannula (HFNC), NPPV, CPAP, COVID-19, COVID-19 management
1. Introduction
Noninvasive ventilation (NIV), which includes noninvasive positive pressure ventilation (NPPV), continuous positive airway pressure (CPAP) therapy, and high flow nasal cannula oxygen therapy (HFNC), has been frequently used in daily medical care for patients with acute respiratory failure. However, in the case of coronavirus disease (COVID-19), there are concerns about the risk of aerosol dispersion that may infect the medical personnel. Therefore, at the beginning of the 1st epidemic wave, the Japan COVID-19 ECMOnet [1] suggested that these supporting measures should not be used for COVID-19 patients. However, several foreign guidelines [2,3] support the use of HFNC. Due to these conflicting recommendations, the decision of their usage was left to the discretion of each facility.
Therefore, we conducted two identical questionnaire surveys to assess the actual rate and trend of NIV and HFNC usage in COVID-19 patients in Japan in June 2020 and February 2021.
2. Facilities and methods
Internet-based surveys (Table 1 ) covering the main and relevant facilities of the Japanese Respiratory Society (JRS) Specialty Program were performed twice with the same questions regarding the use of noninvasive strategies for the management of COVID-19 patients. The first survey was conducted after the end of the 1st Japanese COVID-19 epidemic wave (from June 8 to June 29, 2020) and the second one in the middle of the 3rd wave (from February 3 to February 24, 2021). This study was planned and conducted by members of the respiratory care assembly of the JRS and supported by the JRS.
Table 1.
Questions in the survey.
| Questions: |
|---|
|
3. Results
The first questionnaire was sent to 756 facilities, and responses were received from 156 facilities (20.6%), which included 26 university hospitals, 56 national and public hospitals, 65 community hospitals, and 16 anonymous hospitals. The second survey was sent to 725 facilities, and responses were received from 139 facilities (19.2%), which included 21 university hospitals, 48 national and public hospitals, 63 community hospitals, and 7 anonymous hospitals. The number of facilities that responded to both surveys was 71 (15 university hospitals, 30 national and public hospitals, and 26 community hospitals).
3.1. NPPV (Bilevel PAP) usage
NPPV was used in 7% (11/156) of the facilities in the first survey and 13% (18/139) in the second survey. NPPV was assessed to be effective in treating COVID-19 by 40% (4/10) of the facilities in the first survey, excluding one non-respondent, and 28% (5/18) in the second survey. Full personal protective equipment (PPE), which included N95 mask, goggles or face-shield, cap, gown, and gloves, were used in 82% (9/11) of the facilities in the first survey. Of the 18 facilities utilizing NPPV in the second survey, 15 responded, and 14 of them reported the use of full PPE. Nosocomial infection associated with NPPV usage in the medical personnel of the hospital was reported in one facility (1/11; 9%) in the first survey. In the second survey, 12 facilities responded, and 2 (13%) of them reported that they could not determine whether the nosocomial infection had occurred.
3.2. CPAP (for acute respiratory failure) usage
CPAP was used in 3% (5/154) and 4% (6/137) of the hospitals during the 1st and 3rd waves, respectively. CPAP was assessed to be effective by 25% (1/4), excluding one non-respondent, and 34% (2/6) of the facilities in the 1st and 3rd waves, respectively. Full PPE was used in 75% (3/4) and 83% (5/6) of the hospitals in the 1st and 3rd waves, respectively. None of the facilities in the first and second surveys reported nosocomial COVID-19 infection associated with CPAP usage in the medical personnel of the hospital.
3.3. HFNC usage
According to the first and second surveys, HFNC was used in 12% (18/156) and 49% (68/139) of the facilities, respectively. HFNC was assessed to be effective by 71% (12/17), excluding one non-respondent, and 85% (58/68) of the facilities in the 1st and 3rd waves, respectively. Full PPE was used in 100% (17/17) and 97% (66/68) of the hospitals in the 1st and 3rd waves, respectively. Among the 71 facilities that responded to both surveys, 28 facilities (39%) reported the first use of HFNC in the second survey. None of the facilities in the first survey reported the incidence of nosocomial COVID-19 infection associated with HFNC usage in the medical personnel of the hospital. However, in the second survey, 1 facility (1/68; 1.5%) reported its occurrence, while 3 (3/68; 4%) reported that they could not determine whether it had occurred.
3.4. First-line therapy for COVID-19 patients, including suspected cases, after failure of conventional oxygen therapy
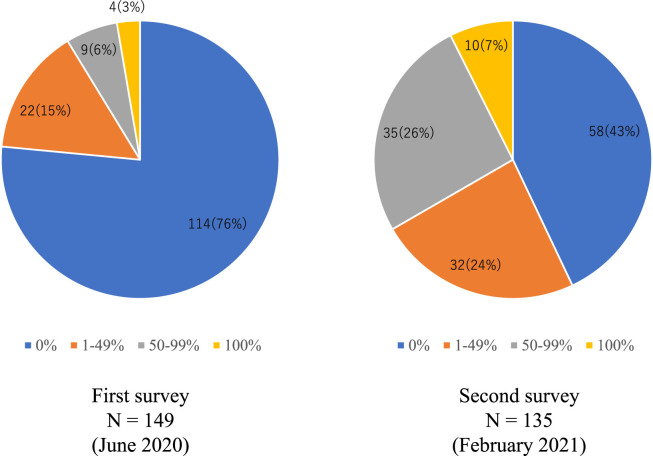
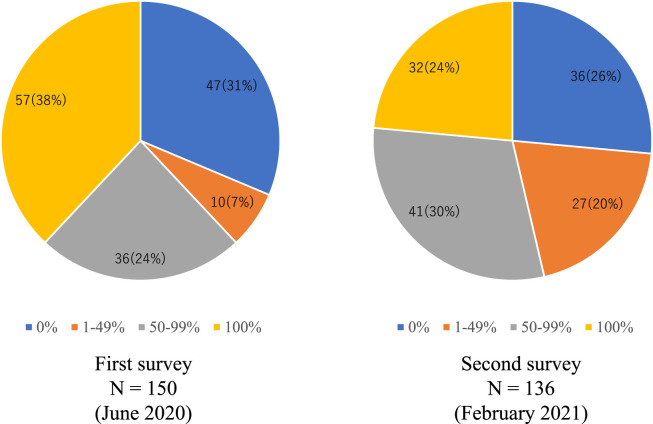
As the first-line therapy following failure of conventional oxygen therapy, NPPV, CPAP, and HFNC were used in all qualifying patients in 1%, 0%, and 3% of the facilities responding to the first survey and in 0%, 0%, and 7% of the facilities responding to the second survey, respectively. For 50%–99% of the qualifying patients in the facilities responding to the first and second surveys, NPPV was used in 3% and 6%, CPAP in 3% and 4%, and HFNC in 6% and 26%, respectively. For 1%–49% of the qualifying patients in the facilities responding to the first and second surveys, NPPV was used in 11% and 8%, CPAP in 6% and 5%, and HFNC in 15% and 24%, respectively (Fig. 1 ). Mechanical ventilation with intubation was performed as the first-line therapy after conventional oxygen therapy for all the patients in 38% and 24% of the facilities responding to the first survey and second survey, respectively. In the 50%–99% of qualifying patients, it was used in 24% and 30% of the facilities responding to the first and second surveys, respectively. In the 1%–49% of qualifying patients, it was used in 7% and 20% of the facilities responding to the first and second surveys, respectively. Furthermore, it was not used at all in 31% and 26% of the facilities responding to the first and second surveys, respectively (Fig. 2 ).
Fig. 1.
Rate of use of high flow nasal cannula as first-line therapy. Left: First survey (June 2020); Right: Second survey (February 2021). The rate of use of HFNC as the first-line therapy in COVID-19 patients, including suspected cases, after the failure of conventional oxygen therapy is illustrated here. For more than half of the patients, HFNC was first applied in 9% of the facilities in the first survey and in 33% in the second survey. (HFNC, high flow nasal cannula; COVID-19, coronavirus disease).
Fig. 2.
Rate of performing invasive mechanical ventilation as first-line therapy. Left: First survey (June 2020); Right: Second survey (February 2021). The rate of performing invasive mechanical ventilation as the first-line therapy in COVID-19 patients, including suspected cases, after the failure of conventional oxygen therapy is illustrated here. For more than half of the patients, invasive ventilation was first applied in 62% of the facilities in the first survey and in 54% in the second survey. (COVID-19, coronavirus disease).
4. Discussion
This is the first report showing the usage trends of noninvasive strategies for the management of COVID-19 in Japan. NPPV was initially used in 7% of the facilities in the first survey, which increased to 13% in the second survey, but it was used rather exceptionally as a first-line therapy after failure of conventional oxygen therapy. CPAP usage was below 5% in both surveys, and no changes were observed between them. On the other hand, HFNC usage increased markedly from its use in 12% of the facilities in the first to 49% in the second survey, and the proportion of facilities that reported using HFNC as a first-line therapy for more than half of the patients increased from 9% to 33%. With the increased usage of HFNC, the proportion of facilities using mechanical ventilation with intubation as a first-line treatment for more than half of the patients decreased from 62% to 54%.
There could be several reasons for the change to HFNC usage. First, accumulating experimental studies have shown that HFNC therapy does not result in significant droplet and aerosol dispersion as compared to conventional oxygen supplementation devices if it is properly fitted [[4], [5], [6]]. Moreover, it has been proven that a surgical mask covering the nasal cannula can block most of the droplets and aerosol dispersion from the HFNC [7]. Second, real-world data from countries outside Japan referring to HFNC usage for COVID-19 [8,9] have shown a decreased intubation ratio, tendency for improved prognosis, and no evident nosocomial infection when used in a negative pressure environment and with full PPE. Third, the 3rd epidemic wave in Japan was significantly larger than the 1st, and the peak number of mechanical ventilations in Japan had doubled [10]. Thus, as intensive medical care resources were severely limited, some facilities needed to reconsider and adopt the use of HFNC.
One case of nosocomial COVID-19 infection of medical personnel associated with HFNC was reported in the second survey. Unfortunately, we cannot specify the details of the case from the survey. Nevertheless, we should continue to pay full attention to infection prevention even with HFNC and full PPE, and a negative pressure room should be mandatory.
These surveys were conducted in the main and relevant facilities of the JRS Specialty Program; hence, the results cannot be generalized to all of Japan. However, these results can provide useful information to the frontline respiratory physicians.
5. Conclusion
The proportion of facilities using HFNC increased from the 1st wave to the 3rd wave of the Japanese COVID-19 epidemic. This could be attributed to the limited medical resources; however, further studies are warranted to reveal the effectiveness of HFNC as compared to the other interventions.
Conflict of interest
K.T. received lecture fees from Boehringer Ingelheim Japan Inc., AstraZeneca K.K, GlaxoSmithKline K.K, Eli Lilly Japan K.K, and Teijin Pharma Ltd. J.T. received research funding from Teijin Pharma Ltd. K.C. belonged to endowed departments supported by Phillips-Japan, Resmed, Fukuda Denshi, Fukuda Lifetec.
Acknowledgements
We sincerely thank all the doctors for responding to the questionnaires during these difficult days and Ms. Yurie Ogawa and other JRS staff for their help in conducting the internet surveys.
References
- 1.Japan ECMOnet for COVID-19. Respiratory support in covid-19-related critically ill patients. http://square.umin.ac.jp/jrcm/pdf/info20200312.pdf (Accessed 27 March 2021).
- 2.The Australian and New Zealand Intensive Care Society (ANZICS) COVID-19 guidelines version 1. March 2020. pp. 1–35. [Google Scholar]
- 3.Alhazzani W., Møller M.H., Arabi Y.M., Loeb M., Gong M.N., Fan E. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus Disease 2019 (COVID-19) Crit Care Med. 2020;48:e440–e469. doi: 10.1097/CCM.0000000000004363. Online First:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hui D.S., Chow B.K., Lo T., Tsang O.T., Ko F.W., Ng S.S. Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks. Eur Respir J. 2019;53:1–11. doi: 10.1183/13993003.02339-2018. [DOI] [PubMed] [Google Scholar]
- 5.Loh N.W., Tan Y., Taculod J., Gorospe B., Teope A.S., Somani J. The impact of high-flow nasal cannula (HFNC) on coughing distance: implications on its use during the novel coronavirus disease outbreak. Can J Anesth. 2020;67:893–894. doi: 10.1007/s12630-020-01634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gaeckle N.T., Lee J., Park Y., Kreykes G., Evans M.D., Hogan C.J. Aerosol generation from the respiratory tract with various modes of oxygen delivery. Am J Respir Crit Care Med. 2020;202:1115–1124. doi: 10.1164/rccm.202006-2309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leonard S., Strasser W., Whittle J.S., Volakis L.I., DeBellis R.J., Prichard R. Reducing aerosol dispersion by high flow therapy in COVID-19: high resolution computational fluid dynamics simulations of particle behavior during high velocity nasal insufflation with a simple surgical mask. J Am Coll Emerg Physicians Open. 2020;1:578–591. doi: 10.1002/emp2.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel M., Gangemi A., Marron R., Chowdhury J., Yousef I., Zheng M. Retrospective analysis of high flow nasal therapy in COVID-19-related moderate-to-severe hypoxaemic respiratory failure. BMJ Open Respir Res. 2020;7 doi: 10.1136/bmjresp-2020-000650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Demoule A., Baron A.V., Darmon M., Beurton A., Geri G., Voiriot G. High-flow nasal canula in critically ill severe COVID-19 patients. Am J Respir Crit Care Med. 2020 doi: 10.1164/rccm.202005-2007LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Japan ECMOnet for COVID-19. Survey of critically ill COVID-19 patients in Japan. https://crisis.ecmonet.jp/(Accessed 27 March 2021).