Abstract
Background
Substance misuse is a global public health problem. In addition to social and economic concerns, consumption of tobacco and alcohol is associated with susceptibility to cardiovascular, respiratory, and infectious diseases, cancers, and risk of transition to substance use disorders. African data suggest regional differences in the prevalence and patterns of substance use, but a number of key questions remain. This cross-sectional population-based study of middle-aged adults aims to examine prevalence and socio-demographic correlates of substance use in four sub-Saharan African countries, in rural and urban settings.
Methods
Participants aged between 40 and 60 years were recruited from six research centres as part of the Africa Wits-INDEPTH partnership for Genomic Research study. Data on patterns of tobacco and alcohol consumption was captured, and the latter further assessed using the CAGE (cut-annoyed-guilty-eye) questionnaire.
Results
Data from 10,703 participants suggested that more men (68.4%) than women (33.3%) were current substance users. The prevalence of current smoking was significantly higher in men than in women (34.5% vs 2.1%, p < 0.001). Smokeless tobacco was used more by women than men (14.4% vs 5.3%, p < 0.001). Current smoking was associated with alcohol consumption in men, and smoking cessation in men was associated with being a former drinker, having higher socio-economic status, and if married or cohabiting. Current alcohol consumption was higher in men, compared to women (60.3% vs 29.3%), and highest in men from Soweto (70.8%) and women from Nanoro (59.8%). The overall prevalence of problematic alcohol consumption among men was 18.9%, and women 7.3%. Men were significantly more likely to develop problematic drinking patterns, and this was more common in those who were divorced or widowed, and in current smokers.
Conclusions
Regional variation in the patterns and prevalence of substance use was observed across study sites, and in rural and urban settings. The high levels of substance use recorded in this study are of concern due to the increased risk of associated morbidities. Further longitudinal data will be valuable in determining trends in substance misuse in Africa.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-11084-1.
Keywords: Alcohol use, Tobacco use, Sub-Saharan Africa, Prevalence, Cross-sectional study, Adults, Socio-demographic correlates, AWI-gen
Background
Global data suggest that the prevalence of substance use (tobacco, alcohol, and recreational drugs) is increasing, especially in low and middle income countries (LMICs) [1–5]. On the African continent, there are few studies estimating prevalence and correlates of substance use, and data examining the socio-demographic correlates of substance use in African countries is sparse. Sreeramareddy and colleagues (2014) examined Demographic and Health Survey Data from 30 African countries to determine the prevalence and social correlates of smoking and smokeless tobacco [6]. Overall their findings suggest that the prevalence of smoking was higher in men than in women, and that tobacco use was more common among the poor, those with lower education, and working in occupations that required fewer skills. There are also studies that suggest that the prevalence of substance use varies regionally and between urban and rural settings, for example in Kenya, Ethiopia, and South Africa (SA) [3, 6–20]. Importantly, African studies examining the prevalence of substance use are not necessarily nationally representative and are often restricted to specific groups, such as among people living with HIV, homeless people, people suffering from mental disorders, or university students [3, 11, 15, 17, 19–22]. Socio-demographic correlates that have emerged from these studies include sex (i.e. men being more likely to engage in harmful substance use than women) and a range of physical and mental health outcomes associated with substance use [8, 10, 13, 17, 21, 23–26]. It is therefore important to examine prevalence and correlates of substance use, including sex, education, and area of residence (rural vs urban). Investigating these relationships may lead to a better understanding of the trajectory of substance use and pathways to various outcomes, and when best to intervene.
The Africa Wits-INDEPTH Partnership for Genomic Research (AWI-Gen) study was initiated in order to assess the genomic and environmental factors associated with susceptibility to cardiometabolic disease [27, 28]. Our secondary analysis addresses the paucity of data on prevalence and patterns of substance use in Africa, and examines demographic correlates of substance use in four sub-Saharan African (SSA) countries: South Africa (South), Kenya (East), Ghana and Burkina Faso (West). Our aim was to examine prevalence of substance use in rural and urban regions, including patterns of alcohol and tobacco consumption.
Methods
Study design and participants
The participants were recruited for the primary cross-sectional study, AWI-Gen, a Collaborative Centre of the Human Heredity and Health in Africa (H3Africa) Consortium, to examine genetic and environmental factors that contribute to cardiometabolic diseases in African populations [27, 28]. Participants were recruited among residents from six study sites in four SSA countries between 2013 and 2016. In SA, the sites were the MRC/Wits Agincourt Health and Demographic Surveillance System Site (HDSS) in Bushbuckridge (referred to as Agincourt), the Dikgale HDSS (now referred to as DIMAMO), and the Soweto cohort from the MRC/Wits Developmental Pathways for Health Research Unit [29–31]. In Kenya, representing East Africa, the study was conducted within two Nairobi slums by the African Population and Health Research Center (APHRC) HDSS in Nairobi [32]. In West Africa, in Ghana, at the Navrongo HDSS, Navrongo Health Research Centre, and Burkina Faso at the Nanoro HDSS, Institut de Recherche en Sciences de la Santé/ Clinical Research Unit of Nanoro [33, 34].
Participants of African descent aged between 40 and 60 years, and residing in the areas monitored by these sites were included in this cross-sectional population-based study in compliance with established recruitment procedures at each of the research centres [27–31, 33, 34]. Exclusion criteria included: closely related individuals, pregnant women, and non-residents [27, 28]. Participants were invited to complete a questionnaire requesting information on demography, family composition, marital status, education, employment, household attributes, substance use, and medical and biological variables not applicable to this study [28].
Ethical considerations
All participants provided written informed consent prior to enrollment into the study [28]. Ethics clearance for each of the study sites was approved through their relevant institutional and national ethics boards, and the AWI-Gen study as a whole was approved by the Human Research Ethics Committee (HREC) (Medical) of the University of the Witwatersrand (approval number M121029, and renewal M170880). Participant identity was protected by assigning unique study identifiers and the key linking them was securely stored at the collection site.
Measures
Overall substance use was defined as; ‘current substance user’ versus ‘current non-user’ (a user was defined as a person currently consuming alcohol and/or currently consuming tobacco products (smoking, chewing, or using snuff)).
Tobacco use variables included smoking categorised as; never used, current user, or former user, based on participant responses. Age at smoking initiation and type of tobacco smoked (cigarettes, pipe, hand rolled cigarettes, and cigars - note that participants could report more than one) were also recorded. The frequency of smoking was captured as; daily (5–6 days per week), 1–4 days per week, 1–3 days per month, or less than once per month. All participants were asked if they used smokeless tobacco and if so; was it chewing tobacco, or snuff.
Alcohol use was categorised as; never consumed, current non-problematic consumer, current problematic consumer, or former consumer. Problematic alcohol use was determined according to the CAGE (cut-annoyed-guilty-eye) questionnaire [35]. If the participant responded yes to at least two of the following questions they were categorised as being problematic drinkers: Have you ever felt that you should cut down on your drinking? Have people annoyed you by criticising your drinking? Have you ever felt bad or guilty about your drinking? Have you ever had an alcoholic drink first thing in the morning to steady your nerves, or get rid of a hangover? In the past year, did you ever have 6 or more alcoholic drinks in a single morning, afternoon, or night? Data were collected on the type of alcohol consumed (spirits, beer, homebrew, wine, or other) and the frequency of alcohol consumption (daily, 5–6 days per week, 1–4 days per week, 1–3 days per month, or less than once per month). It is important to point out that ‘Other’ for the type of alcohol refers to locally brewed alcohol ranging from home brewed sorghum beer in Nanoro and Navrongo, Changaa (traditional home-brewed spirit from maize, millet, or sorghum) in Nairobi, to fermented cider in Dikgale, and cider and spirits in Soweto.
Household goods were used as a proxy for socioeconomic status (SES), using a method developed by the Demographic and Health Surveys (DHS) Program [36]. This method involves a principal component analysis of the SES variables (household attributes) where factor scores (factor loadings) are used to predict wealth indices (from the first principal component or factor) which in turn are categorised into quintiles [37]. The partnership status of participants was categorised as; never married/co-habited, married/living with partner, or divorced/widowed. Education was reported as no formal education, primary, secondary, or tertiary education. Employment status was considered as either employed, or unemployed.
Statistical analyses
Data were captured into REDCap and underwent basic quality control (QC) [38]. Further QC was completed in a PostgreSQL database after exportation. Descriptive statistics were used to summarise the socio-demographic variables in current substance users and non-users of alcohol and/or tobacco, and the distributions were compared. Continuous variables were reported as medians and inter-quartile ranges, and categorical variables were reported as percentages. The data on the consumption of alcohol and tobacco were analysed separately for each site according to sex, and for the combined dataset. The Kruskal-Wallis test was used to compare continuous variables between the sites. Two group comparisons for continuous and non-normally distributed variables were performed using the Mann-Whitney test, and Pearson Chi-squared test or Fisher’s exact test for categorical variables to assess differences between the sexes.
To assess the correlates with alcohol use of the participants according to current use (current consumer of tobacco and/or alcohol) or current non-use (individuals who never consumed or are former consumers of tobacco and/or alcohol), abuse (problematic alcohol use vs non-problematic alcohol use), and smoking cessation (for men); multivariable logistic regression was used to calculate adjusted Odds Ratios (aORs) with 95% Confidence Intervals. We adjusted for ethnicity based on recruitment site for all logistic regressions. Some analyses were performed only for men because the number of women who smoked tobacco was negligible. The analyses were performed using Stata 14.2© (45).
Results
Participants: description of socio-demographic variables in current users and current non-users of tobacco and alcohol
The study included 10,703 participants aged between 40 and 60 years, of whom 5895 were women (55.1%). Table 1 presents the characteristics of the participants according to current use (current consumer of tobacco and/or alcohol) or current non-use (individuals who never consumed or are former consumer of tobacco and/or alcohol), stratified by study site, and for the combined sample. The overall median age was 50 years. In the combined dataset, age was significantly associated with substance use, although age was not significant in four of the six study sites. Similarly level of education was significantly associated with substance use in the combined dataset, although the distribution of education levels differed across sites and was only significantly associated with substance use in three of the six sites. Overall, there were more substance users among those with no formal education. SES (assessed using quintiles) showed differences in the distribution between substance users and non-users across sites. Substance use was variable across SES quintiles, and significantly associated across all study sites. There were more substance users among participants who had never married/cohabited or married/living with partner, than among those who were divorced/widowed. More employed participants were substance users than those that were unemployed. Complete data regarding substance use was not available for Soweto, as alcohol consumption was not recorded for Soweto women.
Table 1.
Socio-demographic characteristics of the AWI-Gen cohort according to study site and for the combined dataset (All sites), stratified according to substance use (current alcohol consumption and/or current tobacco use, including smoking, chewing, and using snuff)
| Agincourt | Digkale | Nairobi | Nanoro | Navrongo | Soweto | All sites | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Current users | Current non-users | p-value | Current users | Current non-users | p-value | Current users | Current non-users | p-value | Current users | Current non-users | p-value | Current users | Current non-users | p-value | Current users | Current non-users | p-value | Current users | Current non-users | p-value | |
| N(%) | 358 (24.40%) | 1107 (75.60%) | 655 (43.90%) | 512 (56.10%) | 485 (25.00%) | 1457 (75.00%) | 1467 (70.40%) | 617 (29.60%) | 1410 (70.00%) | 604 (30.00%) | 872 (42.90%) | 1159 (57.00%) | 5247 (49.00%) | 5456 (51.00%) | |||||||
| Age (years) | 52 (10) | 51 (10) | 0.1782 | 51 (10) | 40.0 (10.5) | < 0.001 | 47 (9) | 48 (9) | 0.8415 | 50 (10) | 49 (10) | < 0.001 | 51 (10) | 51 (10) | 0.3125 | 49 (10) | 49 (10) | 0.4236 | 50 (10) | 49 (10) | < 0.001 |
| Sex | < 0.001 | < 0.001 | < 0.001 | 0.674 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||
| Women | 85 (9.53%) | 807 (90.47%) | 380 (46.86%) | 431 (53.14%) | 91 (8.62%) | 965 (91.38%) | 727 (63.97%) | 312 (30.03%) | 628 (57.56%) | 463 (42.44)% | 49 (4.87%)a | 957 (95.13%)a | 1960 (33.25%) | 3935 (66.75%) | |||||||
| Men | 273 (47.64%) | 300 (52.36%) | 275 (77.25%) | 81 (22.75%) | 394 (44.47%) | 492 (55.53%) | 741 (70.81%) | 305 (29.19%) | 782 (84.72%) | 141 (15.28%) | 823 (80.29%) | 202 (19.71%) | 3287 (68.37%) | 1521 (31.63%) | |||||||
| Socioeconomic Status (Lowest to highest) | < 0.001 | 0.025 | 0.023 | < 0.001 | 0.023 | < 0.001 | < 0.001 | ||||||||||||||
| 1st Quintile | 82 (36.28%) | 144 (63.72%) | 93 (63.27%) | 54 (36.73%) | 78 (33.19%) | 157 (66.81%) | 246 (73.21%) | 90 (26.79%) | 243 (65.32%) | 129 (34.68%) | 36 (15.52%) | 196 (84.48%) | 778 (50.26%) | 770 (49.74%) | |||||||
| 2nd Quintile | 103 (29.68%) | 244 (70.32%) | 155 (58.49%) | 110 (41.51%) | 107 (24.77%) | 325 (75.23%) | 303 (75.00%) | 101 (25.00%) | 250 (69.44%) | 110 (30.56%) | 100 (20.49%) | 388 (79.51%) | 1018 (44.34%) | 1278 (55.66%) | |||||||
| 3rd Quintile | 42 (22.95%) | 141 (77.05%) | 89 (58.17%) | 64 (41.83%) | 112 (24.89%) | 338 (75.11%) | 303 (74.81%) | 102 (25.19%) | 288 (74.42%) | 99 (25.58%) | 132 (40.87%) | 191 (59.13%) | 966 (50.82%) | 935 (49.18%) | |||||||
| 4th Quintile | 80 (22.99%) | 268 (77.01%) | 148 (58.04%) | 107 (41.96%) | 85 (21.46%) | 311 (78.54%) | 282 (73.06%) | 104 (26.94%) | 346 (73.15%) | 127 (26.85%) | 221 (63.51%) | 127 (36.49%) | 1162 (52.67%) | 1044 (47.33%) | |||||||
| 5th Quintile | 51 (14.13%) | 310 (85.87%) | 170 (49.13%) | 176 (50.87%) | 103 (24.01%) | 326 (75.99%) | 331 (60.62%) | 215 (39.38%) | 283 (67.22%) | 138 (32.78%) | 373 (76.59%) | 114 (23.41%) | 1311 (50.62%) | 1279 (49.38%) | |||||||
| Marital status | < 0.001 | 0.016 | < 0.001 | 0.140 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||
| Never married or co-habited | 49 (36.57%) | 85 (63.43%) | 156 (54.17%) | 132 (45.83%) | 13 (15.66%) | 70 (84.34%) | 10 (58.82%) | 7 (41.18%) | 16 (80.00%) | 4 (20.00%) | 239 (75.63%) | 77 (24.37%) | 483 (56.29%) | 375 (43.71%) | |||||||
| Married/living with partner | 252 (25.66%) | 730 (74.34%) | 324 (53.64%) | 280 (46.36%) | 374 (28.90%) | 920 (71.10%) | 1271 (70.03%) | 544 (29.97%) | 1067 (72.05%) | 414 (27.95%) | 446 (53.35%) | 390 (46.65%) | 3734 (53.25%) | 3278 (46.75%) | |||||||
| Divorced/Widowed | 57 (16.33%) | 292 (83.67%) | 175 (63.64%) | 100 (36.36%) | 98 (17.38%) | 466 (82.62%) | 185 (75.20%) | 61 (24.80%) | 327 (63.87%) | 185 (36.13%) | 165 (30.78%) | 371 (69.22%) | 1007 (40.57%) | 1475 (59.43%) | |||||||
| Highest education completed | 0.060 | < 0.001 | 0.006 | 0.086 | 0.403 | < 0.001 | < 0.001 | ||||||||||||||
| No Formal education | 106 (26.30%) | 297 (73.70%) | 63 (65.62%) | 33 (34.38%) | 25 (17.01%) | 122 (82.99%) | 1229 (71.54%) | 489 (28.46%) | 980 (69.36%) | 433 (30.64%) | 7 (70.00%) | 3 (30.00%) | 2410 (63.64%) | 1377 (36.36%) | |||||||
| Primary | 148 (25.74%) | 427 (74.26%) | 250 (64.77%) | 136 (35.23%) | 263 (23.69%) | 847 (76.31%) | 157 (65.69%) | 82 (34.31%) | 282 (73.63%) | 101 (26.37%) | 122 (16.18%) | 632 (83.82%) | 1222 (35.45%) | 2225 (64.55%) | |||||||
| Secondary | 91 (22.86%) | 307 (77.14%) | 328 (51.01%) | 315 (48.99%) | 187 (28.38%) | 472 (71.62%) | 62 (64.58%) | 34 (35.42%) | 121 (69.14%) | 54 (30.86%) | 620 (69.27%) | 275 (30.73%) | 1409 (49.16%) | 1457 (50.84%) | |||||||
| Tertiary | 12 (13.64%) | 76 (86.36%) | 14 (34.15%) | 27 (65.85%) | 10 (38.46%) | 16 (61.54%) | 15 (83.33%) | 3 (16.67%) | 24 (66.67%) | 12 (33.33%) | 106 (69.28%) | 47 (30.72%) | 181 (50.00%) | 181 (50.00%) | |||||||
| Employment status | 0.700 | 0.259 | 0.168 | 0.380 | < 0.001 | 0.018 | < 0.001 | ||||||||||||||
| Unemployed | 215 (24.32%) | 669 (75.68%) | 396 (54.70%) | 328 (45.30%) | 22 (19.47%) | 91 (80.53%) | 13 (61.90%) | 8 (38.10%) | 564 (75.20%) | 186 (24.80%) | 322 (39.75%) | 488 (60.25%) | 1532 (46.40%) | 1770 (53.60%) | |||||||
| Employed | 117 (23.40%) | 383 (76.60$) | 255 (58.09%) | 184 (41.91%) | 461 (25.25%) | 1365 (74.75%) | 1453 (70.67%) | 603 (29.33%) | 842 (66.93%) | 416 (33.07%) | 550 (45.05%) | 671 (54.95%) | 3678 (50.38%) | 3622 (49.62%) | |||||||
Continuous variables are presented as medians and interquartile range. Mann-Whitney Wilcoxon test has been used to assess differences
Categorical variables are presented as number and percentage. Chi-squared or Fisher’s exact test (when Chi-squared test conditions were not fulfilled) were used to assess differences
aThis only accounts for smoking since alcohol consumption data have not been collected for women in Soweto
Tobacco use
The prevalence of current smoking was significantly higher in men than in women (34.5% vs 2.1%, p < 0.001). There were differences observed between the sites with the lowest prevalence of current smoking in Nanoro for both men and women (13.6 and 0% respectively), and the highest in Dikgale for men (63.4%) and in Soweto for women (4.9%) (Table 2). The median age of smoking initiation was 20 (Q1-Q3: 17–24) years old for both sexes. Cigarettes were the most consumed type of smoking tobacco, followed by hand-rolled cigarettes and pipes. For men, Nairobi had the highest prevalence of former smokers (29.3%), and Nanoro had the lowest percentage of former smokers (11.7%). Smokeless tobacco was used more by women overall (14.4% vs 5.3%, p < 0.001), and chewing tobacco (7.1%) more than snuff (5.4%) for women across all sites. The type and frequency of smoked tobacco was not available for Agincourt and Soweto, and smokeless tobacco data was unavailable for Soweto.
Table 2.
Prevalence and characteristics of tobacco consumption per site and per gender
| Agincourt | Digkale | Nairobi | Nanoro | Navrongo | Soweto | All men | All women | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men (573) | Women (892) | p-value | Men (355) | Women (810) | p-value | Men (886) | Women (1056) | p-value | Men (1045) | Women (1039) | p-value | Men (923) | Women (1091) | p-value | Men (1025) | Women (1005) | p-value | N = 4807 | N = 5893 | p-value | |
| Smoking status | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||
| Never Smoked | 291 (50.96%) | 882 (98.88%) | 54 (15.21%) | 756 (93.33%) | 418 (47.33%) | 975 (92.33%) | 779 (74.69%) | 1033 (99.81%) | 332 (35.97%) | 1052 (96.6%) | 311 (30.40%) | 897 (89.97%) | 2185 (45.52%) | 5595 (95.17%) | |||||||
| Current smoker | 155 (27.15%) | 3 (0.34%) | 224 (63.38%) | 25 (03.09%) | 208 (23.50%) | 27 (02.56%) | 142 (13.61%) | 0 (0.00%) | 388 (42.04%) | 21 (01.93%) | 540 (52.79%) | 49 (4.91%) | 1658 (34.54%) | 125 (02.13%) | |||||||
| Former smoke | 125 (21.89%) | 7 (0.78%) | 76 (21.41%) | 29 (03.58%) | 259 (29.27%) | 54 (05.11%) | 122 (11.70%) | 2 (0.19%) | 203 (21.99%) | 16 (01.47%) | 172 (16.81%) | 51 (5.12%) | 957 (19.94%) | 159 (02.70%) | |||||||
| Age started smoking | 20 (17–27) | 23 (20–30) | 0.4103 | 19 (16–23) | 19 (16–22) | 0.7572 | 19 (16–22) | 20 (17–23) | 0.1457 | 20 (18–25) | 24.5 (21–28) | 0.3333 | 20 (20–25) | 20 (18–30) | 0.8061 | NA | NA | 20 (17–25) | 20 (17–24) | 0.3125 | |
| Type of smoked tobacco Use | |||||||||||||||||||||
| Cigarettes (Yes) | NA | NA | – | 118 (33.15%) | 14 (01.73%) | < 0.001 | 208 (23.48%) | 25 (02.37%) | < 0.001 | 140 (13.40%) | 0 (0.00%) | < 0.001 | 262 (28.39%) | 12 (01.10%) | < 0.001 | 535 (52.20%) | 49 (04.87%) | < 0.001 | 1263 (26.27%) | 100 (01.70%) | < 0.001 |
| Pipe (Yes) | NA | NA | – | 39 (10.96%) | 5 (0.62%) | < 0.001 | 0 (0.00%) | 1 (0.09%) | 0.360 | 1 (0.10%) | 0 (0.00%) | 0.321 | 5 (0.54%) | 1 (0.09%) | 0.034 | 3 (0.29%) | 0 (0.00%) | 0.086 | 48 (01.00%) | 7 (0.12%) | < 0.001 |
| Hand rolled (Yes) | NA | NA | 77 (21.63%) | 6 (0.74%) | < 0.001 | 0 (0.00%) | 1 (0.09%) | 0.360 | 0 (0.00%) | 0 (0.00%) | 164 (17.77%) | 11 (1.01%) | < 0.001 | NA | NA | 241 (05.01%) | 18 (0.31%) | < 0.001 | |||
| Cigars (Yes) | NA | NA | – | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 2 (0.22%) | 0 (0.00%) | 0.124 | NA | NA | 2 (0.04%) | 0 (0.00%) | |||||
| Frequency of smoked tobacco use | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||||||
| Current Non-smokers | 131 (36.8%) | 786 (96.92%) | 678 (76.52%) | 1029 (97.44%) | 903 (86.41%) | 1039 (100%) | 535 (57.96%) | 1070 (98.08%) | NA | NA | 2665 (70.45%) | 4813 (98.45%) | |||||||||
| Daily smokers | NA | NA | 194 (54.49%) | 20 (02.47%) | 182 (20.54%) | 21 (01.99%) | 126 (12.06%) | 0 (0.00%) | 343 (37.16%) | 18 (01.65%) | NA | NA | 845 (22.34%) | 59 (01.21%) | |||||||
| 5–6 days per week | NA | NA | 3 (0.84%) | 0 (0.00%) | 2 (0.23%) | 0 (0.00%) | 7 (0.67%) | 0 (0.00%) | 17 (01.84%) | 0 (0.00%) | NA | NA | 29 (0.77%) | 0 (0.00%) | |||||||
| 1–4 days per week | NA | NA | 23 (06.46%) | 4 (0.49%) | 21 (02.37%) | 6 (0.57%) | 6 (0.57%) | 0 (0.00%) | 17 (01.84%) | 0 (0.00%) | NA | NA | 67 (01.77%) | 10 (0.20%) | |||||||
| 1–3 days per month | NA | NA | 4 (1.12%) | 1 (0.12%) | 0 (0.00%) | 0 (0.00%) | 2 (0.19%) | 0 (0.00%) | 3 (0.33%) | 1 (0.09%) | NA | NA | 9 (0.24%) | 2 (0.04%) | |||||||
| Less than once per month | NA | NA | 1 (0.28%) | 0 (0.00%) | 3 (0.34%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | NA | NA | 4 (0.11%) | 0 (0.00%) | |||||||
| Smokeless tobacco status (Yes) | 13 (02.27%) | 51 (05.72%) | 0.002 | 32 (08.99%) | 337 (41.55%) | < 0.001 | 48 (05.42%) | 20 (01.89%) | < 0.001 | 67 (06.41%) | 326 (31.38%) | < 0.001 | 95 (10.29%) | 114 (10.45%) | 0.735 | NA | NA | 255 (05.30%) | 848 (14.39%) | < 0.001 | |
| Type of smokeless tobacco Use | |||||||||||||||||||||
| Snuff (Yes) | 4 (0.70%) | 31 (03.48%) | 0.002 | 18 (05.06%) | 253 (31.20%) | < 0.001 | 35 (03.95%) | 16 (01.52%) | < 0.001 | 3 (0.29%) | 4 (0.38%) | < 0.001 | 30 (03.25%) | 12 (01.10%) | 0.002 | 0 (0.00%) | 0 (0.00%) | – | 90 (01.87%) | 316 (05.36%) | < 0.001 |
| Chewing tobacco use (Yes) | 0 (0.00%) | 0 (0.00%) | – | 0 (0.00%) | 12 (01.48%) | < 0.001 | 4 (0.45%) | 4 (0.38%) | < 0.001 | 64 (06.12%) | 307 (29.55%) | < 0.001 | 58 (06.28%) | 93 (08.52%) | < 0.001 | 0 (0.00%) | 0 (0.00%) | – | 126 (02.62%) | 416 (07.06%) | < 0.001 |
Categorical variables are presented as number and percentage. Chi-squared or Fisher’s exact test (when Chi-squared test conditions were not fulfilled) were used to assess differences
NA For variables not available at site
Alcohol consumption
The patterns of alcohol consumption per site, and for the combined sample (All) are presented in Table 3. In the combined sample, the percentage of lifetime abstainers (never consumed) was more than twofold higher among women than men (52.4% vs 23.8%). Overall, current consumers were more likely to be men. The lowest prevalence of current alcohol consumption was observed in Nairobi (33.9% of men and 5.9% of women). Consumers of alcohol were highest in Soweto (70.8%) for men, and in Nanoro (59.8%) for women. Navrongo had the highest rate of problematic drinking (50.1% men and 15.3% women). Former consumers were highest in Nairobi (37.1%) for men, and Navrongo for women (24.3%). Among the sites, Nanoro had the highest prevalence of daily alcohol consumption, whilst Dikgale had the lowest. There were differences in the types of alcoholic beverages consumed at each site, despite homebrewed alcohol and beer being most popular in most sites (Table 3). Approximately 21.7% of men felt that they should cut down on alcohol consumption, and 8.6% of women felt the same. Alcohol consumption-based guilt was felt by 16.9% of men and 5.1% of women. Binge drinking (> 6 alcoholic drinks) was observed at a higher prevalence in men than in women (9.6% vs 2.5%, p < 0.001) (Table 3). Data on alcohol consumption was not collected for Soweto women, nor was the frequency of consumption and CAGE questionnaire responses available for Soweto men.
Table 3.
Prevalence and characteristics of alcohol consumption per site and per gender
| Agincourt | Digkale | Nairobi | Nanoro | Navrongo | Soweto | All Men | All Women | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men (573) | Women (892) | p-value | Men (355) | Women (810) | p-value | Men (886) | Women (1056) | p-value | Men (1045) | Women (1039) | p-value | Men (923) | Women (1091) | p-value | Men (1025) | Women (1005) | p-value | N = 4807 | N = 5893 | p-value | |
| Alcohol use | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||||||||||||||
| Never Consumed | 187 (32.64%) | 731 (81.95%) | 55 (15.45%) | 561 (69.43%) | 257 (29.01%) | 758 (71.78%) | 273 (26.22%) | 277 (26.74%) | 71 (7.71%) | 231 (21.21%) | 299 (29.17%) | – | 1142 (23.79%) | 2558 (52.41%) | |||||||
| Current non-problematic | 218 (38.08%) | 52 (05.83%) | 77 (21.63%) | 45 (05.57%) | 174 (19.64%) | 32 (03.03%) | 544 (52.26%) | 521 (50.19%) | 252 (27.36%) | 426 (39.12%) | 726 (70.83%) | – | 1991 (41.97%) | 1075 (22.02%) | |||||||
| Current problematic | 18 (03.14%) | 2 (0.22%) | 142 (39.89%) | 57 (07.05%) | 126 (14.22%) | 30 (02.84%) | 160 (15.37%) | 100 (09.65%) | 461 (50.05%) | 167 (15.34%) | – | – | 906 (18.87%) | 356 (07.29%) | |||||||
| Former consumer | 150 (26.18%) | 107 (12.00%) | 82 (23.03%) | 145 (17.95%) | 329 (37.13%) | 236 (22.35%) | 64 (06.15%) | 139 (13.42%) | 137 (14.88%) | 265 (24.33%) | – | – | 762 (15.87%) | 892 (18.27%) | |||||||
| Problems with drinking | |||||||||||||||||||||
| Felt should cut down? | 17 (02.97%) | 2 (0.22%) | < 0.001 | 140 (39.33%) | 65 (08.01%) | < 0.001 | 137 (15.46%) | 31 (02.94%) | < 0.001 | 208 (19.90%) | 126 (12.13%) | < 0.001 | 543 (58.83%) | 282 (25.85%) | < 0.001 | NA | NA | 1045 (21.73%) | 506 (08.58%) | < 0.001 | |
| People have criticized | 8 (01.40%) | 1 (0.11%) | 0.002 | 90 (25.28%) | 33 (04.07%) | < 0.001 | 95 (10.72%) | 27 (02.56%) | < 0.001 | 136 (13.01%) | 94 (09.05%) | 0.010 | 347 (37.59%) | 117 (10.72%) | < 0.001 | NA | NA | 676 (14.06%) | 272 (04.62%) | < 0.001 | |
| Guilty? | 10 (01.75%) | 1 (0.11%) | < 0.001 | 121 (33.99%) | 54 (06.66%) | < 0.001 | 127 (14.33%) | 27 (02.56%) | < 0.001 | 111 (10.62%) | 51 (04.91%) | < 0.001 | 441 (47.78%) | 170 (15.58%) | < 0.001 | NA | NA | 810 (16.85%) | 303 (05.14%) | < 0.001 | |
| Alcohol first in the morning? | 30 (05.24%) | 3 (0.34%) | < 0.001 | 121 (33.99%) | 20 (02.47%) | < 0.001 | 51 (05.76%) | 10 (0.95%) | < 0.001 | 87 (08.33%) | 63 (06.06%) | 0.136 | 229 (24.81%) | 49 (04.49%) | < 0.001 | NA | NA | 518 (10.77%) | 145 (02.46%) | < 0.001 | |
| > 6 alcoholic drinks | 98 (17.10) | 11 (01.23%) | < 0.001 | 136 (38.20%) | 49 (06.04%) | < 0.001 | 43 (04.85%) | 9 (0.85%) | < 0.001 | 166 (15.89%) | 74 (07.12%) | < 0.001 | 18 (01.95%) | 5 (0.46%) | 0.007 | NA | NA | 461 (09.59%) | 148 (02.51%) | < 0.001 | |
| Type of consumption | |||||||||||||||||||||
| Beer | 139 (24.26%) | 24 (02.69%) | < 0.001 | 217 (60.96%) | 98 (12.08%) | < 0.001 | 334 (37.70%) | 190 (17.99%) | < 0.001 | 154 (14.74%) | 13 (01.25%) | < 0.001 | 250 (27.09%) | 158 (14.48%) | < 0.001 | 593 (57.85%) | NA | 1687 (35.09%) | 483 (08.19%) | < 0.001 | |
| Home brew | 85 (14.83%) | 22 (02.47%) | < 0.001 | 73 (20.51%) | 34 (04.19%) | < 0.001 | 361 (40.74%) | 120 (11.36%) | < 0.001 | 223 (21.34%) | 393 (37.82%) | < 0.001 | 675 (73.13%) | 772 (70.76%) | < 0.001 | 25 (02.44%) | NA | 1442 (29.99%) | 1341 (22.75%) | < 0.001 | |
| Spirits | 7 (01.22%) | 1 (0.11%) | < 0.001 | 3 (0.85%) | 2 (0.25%) | < 0.001 | 25 (02.82%) | 7 (0.66%) | < 0.001 | 60 (05.74%) | 7 (0.67%) | < 0.001 | 629 (68.15%) | 391 (35.84%) | < 0.001 | 59 (05.76%) | NA | 783 (16.29%) | 408 (06.92%) | < 0.001 | |
| Wine | 3 (0.52%) | 3 (0.34%) | < 0.001 | 2 (0.56%) | 25 (03.08%) | < 0.001 | 5 (0.56%) | 4 (0.38%) | < 0.001 | 5 (0.48%) | 7 (0.67%) | 0.803 | 33 (03.58%) | 11 (01.01%) | < 0.001 | 41 (04.00%) | NA | 89 (01.85%) | 50 (0.85%) | < 0.001 | |
| Other | 1 (0.17%) | 4 (0.45%) | 0.380 | 11 (03.10%) | 87 (10.74%) | < 0.001 | 1 (0.11%) | 0 (0.00%) | 0.275 | 411 (39.33%) | 345 (33.21%) | 0.007 | 4 (0.43%) | 3 (0.27%) | < 0.001 | 54 (05.27%) | NA | 482 (10.02%) | 439 (07.45%) | < 0.001 | |
| Frequency of consumption | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||||||||||||||
| Current Non-consumers | 337 (58.81%) | 838 (93.95%) | 137 (38.59%) | 710 (87.65%) | 588 (66.37%) | 994 (94.13%) | 345 (33.01%) | 423 (40.71%) | 211 (22.86%) | 506 (46.38%) | NA | NA | 2643 (54.98%) | 4476 (75.95%) | |||||||
| Daily | 37 (06.46%) | 4 (0.45%) | 12 (03.38%) | 0 (0.00%) | 78 (08.80%) | 12 (01.14%) | 284 (27.18%) | 107 (10.30%) | 125 (13.54%) | 60 (05.50%) | NA | NA | 536 (11.15%) | 183 (03.11%) | |||||||
| 5–6 days per week | 35 (06.11%) | 3 (0.34%) | 7 (01.97%) | 0 (0.00%) | 6 (0.68%) | 1 (0.09%) | 97 (09.28%) | 44 (04.23%) | 263 (28.39%) | 128 (11.73%) | NA | NA | 407 (08.47%) | 176 (02.99%) | |||||||
| 1–4 days per week | 66 (11.52%) | 7 (0.78%) | 137 (38.59%) | 35 (04.32%) | 129 (14.56%) | 28 (02.65%) | 268 (25.65%) | 354 (34.07%) | 272 (29.47%) | 312 (28.60%) | NA | NA | 872 (18.14%) | 736 (12.49%) | |||||||
| 1–3 days per month | 60 (10.47%) | 18 (02.02%) | 61 (17.18%) | 59 (07.28%) | 58 (06.55%) | 12 (01.14%) | 43 (04.11%) | 93 (08.95%) | 43 (04.66%) | 65 (05.96%) | NA | NA | 265 (05.51%) | 247 (04.19%) | |||||||
| Less than once per month | 38 (06.63%) | 22 (02.47%) | 1 (0.28%) | 6 (0.74%) | 27 (03.05%) | 9 (0.85%) | 8 (0.77%) | 18 (01.73%) | 10 (01.08%) | 20 (01.83%) | NA | NA | 84 (01.75%) | 75 (01.27%) | |||||||
Categorical variables are presented as number and percentage. Chi-squared or Fisher’s exact test (when Chi-squared test conditions were not fulfilled) were used to assess differences
NA Variables not available at site
Multivariable logistic regression analysis of problematic drinking
In the site (proxy for ethnicity) adjusted analysis; SES, age, level of education, and employment status were not associated with problematic alcohol use when pooling data from all of the sites (Fig. 1; Supplementary Table 1). Being male, and being divorced/widowed was associated with increased likelihood of alcohol abuse with respective aOR of 3.23 (95% IC [2.72–3.82]) and 1.61 (95% IC [1.12–2.32]) (Supplementary Table 1). These associations differed at site level, and being male was the only consistent risk factor across all sites with aOR ranging from 1.91 (95% IC [1.36–2.69]) in Nanoro, to 8.15 (95% IC [1.34–49.66]) in Agincourt. Higher SES was associated with reduced odds in Nairobi, whereas in Nanoro it was associated with increased odds of having a drinking problem. When assessing the effects of tobacco consumption on problematic drinking, tobacco users showed increased likelihood of problematic alcohol consumption with aOR = 3.84 (95% IC [3.24–4.57]) for current smokers, and aOR = 2.07 (95% IC [1.70–2.52]) for smokeless tobacco users.
Fig. 1.
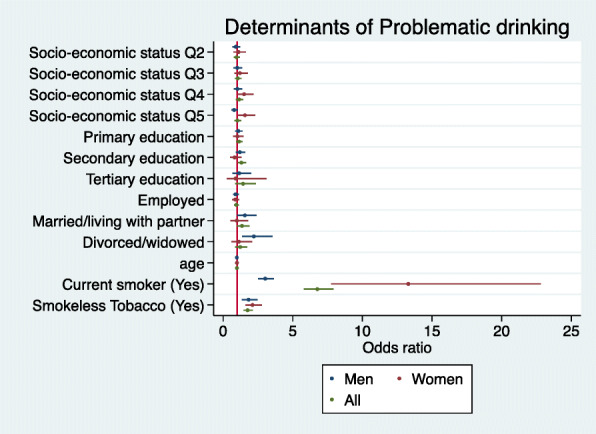
Forest plot depicting the aORs for the determinants of problematic alcohol consumption in men and women for the combined dataset. (Legend) Forest plot of multivariable logistic regression coefficients (95% Confidence Intervals) for the association of problematic drinking with socio-economic status (SES quintiles) (Reference = Q1), highest education level (Reference = No formal education), sex (Reference = Women), employment status (Reference = Not employed), marital status (Reference = Single), age, smoking status (Reference = current non-smokers), smokeless tobacco use (Reference = smokeless tobacco non-user). The model adjusted for site as a proxy for ethnicity based on location of research centre (N = 8486)
Analysis of current smoking in men
There were too few women smokers for meaningful analysis, so only men were included in this analysis. Multivariable logistic regression suggests that SES (4th and 5th quintiles), being married/living with partner, and tertiary education were significantly associated with a reduced likelihood of being a current smoker (Fig. 2). In men, alcohol consumption and having only primary school education were associated with statistically increased odds of being a current smoker, while age was associated with reduced likelihood of being a current smoker, which although statistically significant had a small effect in our cohort of older adults (Fig. 2, Supplementary Table 2).
Fig. 2.
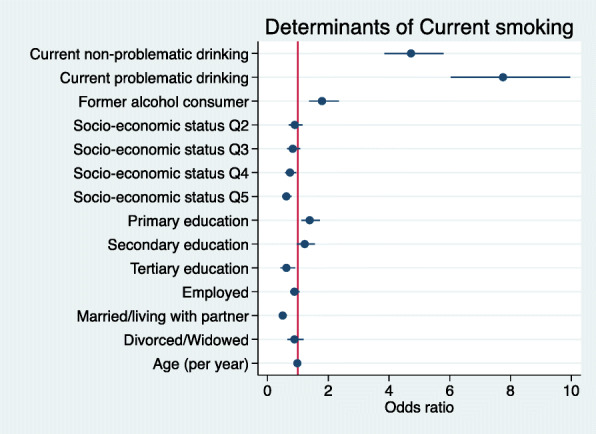
Forest plot showing the correlates of current tobacco smoking for men only. (Legend) Forest plot of regression coefficients (95% Confidence Intervals) for the association of current smoking in men with socio-economic status (SES quintiles) (Reference = Q1), highest level of education (Reference = No formal education), employment (Reference = Not employed), marital status (Reference = Single), age, alcohol consumption (Reference = never consumed). Model adjusted for site as a proxy for ethnicity. Estimates for men only (N = 4734)
Correlates of smokeless tobacco use
Overall results across all sites suggest that smokeless tobacco use was more likely if the participant consumed alcohol (current non-problematic alcohol consumer aOR = 2.99 95% CI [2.41–3.70]; current problematic aOR = 4.52 [3.50–5.83]; former consumer aOR = 2.74 [2.21–3.39]) or were former smokers (aOR = 1.58, 95% IC [1.20–2.09]) (Fig. 3, Supplementary Table 3). On the other hand, current smokers were less likely to use smokeless tobacco (aOR = 0.37, 95% IC [0.26–0.51]) and men were significantly less likely to use smokeless tobacco (aOR = 0.30, 95% IC [0.24–0.37]). Figure 3 provides a graphic summary of the results from the multivariable logistic regression performed.
Fig. 3.
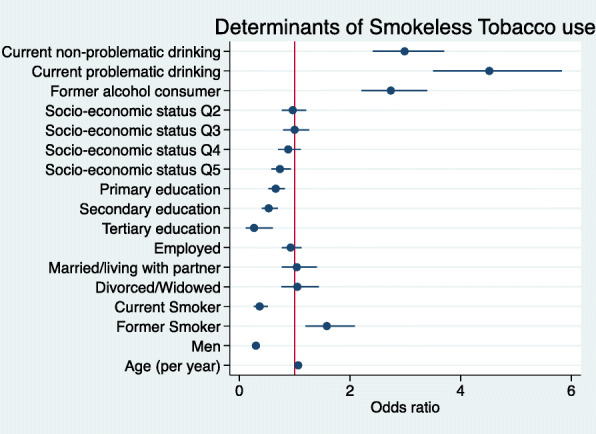
Forest plot indicating the site aORs for the correlates of smokeless tobacco consumption. (Legend) Forest plot of regression coefficients (95% Confidence Intervals) for the association of smokeless tobacco use with socio-economic status (SES quintiles) (Reference = Q1), highest level of education (Reference = No formal education), employment (Reference = Not employed), marital status (Reference = Single), age, sex (Reference = Women), alcohol consumption (Reference = never consumed), smoking status (Reference = Never smoked). Model adjusted for site as a proxy for ethnicity. (N = 8485)
Multivariable logistic regression analysis of smoking cessation in men
Results suggest that the adjusted odds ratio (aOR) for smoking cessation increased with age, higher SES (4th and 5th quintiles), being married/living with partner, and having stopped drinking (Fig. 4). Current alcohol consumption was correlated with a lower likelihood of smoking cessation (Fig. 4; Supplementary Table 4).
Fig. 4.
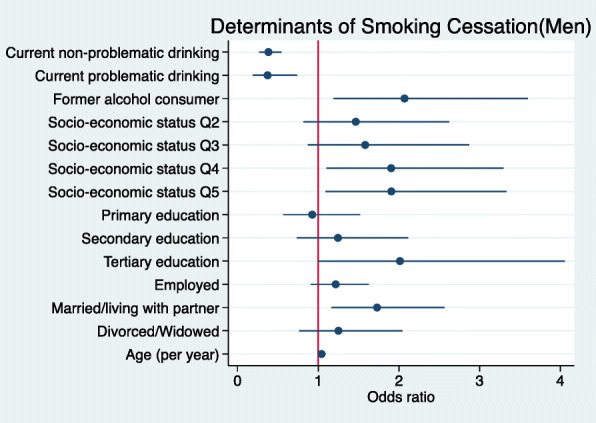
Forest plot showing the correlates of smoking cessation in men. (Legend) Forest plots of regression coefficients (95% Confidence Intervals) for the association of smoking cessation in men with socio-economic status (SES quintiles) (Reference = Q1), highest level of education (Reference = No formal education), employment (Reference = Not employed), marital status (Reference = Single), age, alcohol consumption (Reference = never consumed), smoking status (Reference = Never smoked). Model adjusted for site as a proxy for ethnicity. Estimates for men only (N = 2102)
Discussion
In this study we reveal complex regional patterns of tobacco and alcohol consumption in six communities across four SSA countries. First, in the total cohort, almost half (49%) of all participants, men and women, either consumed tobacco products, alcohol, or both. Secondly, men were more likely to be current smokers than women (34.5% vs 2.1%), in line with global studies, but more women (14.4%) used smokeless tobacco (snuff and chewing tobacco) than men (5.3%), with some regional variation [2, 3, 5, 6]. Third, overall, being a current smoker was associated with alcohol consumption, lower education levels, and was less common among married individuals or those living with partners. Fourth, alcohol consumption was also more common among men, but had higher prevalence than smoking in both sexes (60.8% of men and 29.3% of women). And lastly, problematic alcohol use was associated with being male, widowed or divorced, and using tobacco products (smoking and smokeless use).
Prevalence estimates of current smoking among men from almost all the AWI-Gen sites were much higher when compared to the age-adjusted prevalence for daily smoking among men in their respective countries in a study conducted in 2015 [2]. A reason for this difference might be that the previous study to which we compare our findings was based on the prevalence of daily smoking, whereas our smoking variable was ‘current smoking’ with some men reporting that they were occasional current smokers. However, the direct comparison of prevalence of daily smokers is still higher in AWI-Gen and these differences could be due to several other factors including age distribution, and selection of specific communities in AWI-Gen, whereas Reitsma et al. (2017) may have used publications with small participant numbers, or specific co-morbidities from different communities to develop country-specific prevalence estimates. Patterns of tobacco use were highly sex-specific, with smoking tobacco most common among men, and women preferring snuff or chewing tobacco supporting previous findings in SA, Ethiopia, the Gambia, Kenya and Angola [3, 9, 10, 13, 15, 21, 25, 39]. In the combined sample, more than half of the men ever smoked, and 34.5% were current smokers. A similarly high prevalence of current smoking was previously reported in men from other African countries [3, 6, 9, 10, 13, 15, 21, 25, 39]. In our study, age was associated with current smoking in men (aOR = 0.98 (95%CI 0.97–0.99)) and smokeless tobacco consumption across both sexes (aOR = 1.06 (1.05–1.08)), and while statistically significant in the full dataset, the effects were small (per year of age) and in opposite directions. Adults in the highest wealth categories and those who had attained higher education levels were less likely to use tobacco products, in concordance with the findings of previous studies in Africa [3, 6, 9, 10, 13, 15, 21, 25, 39]. Alcohol consumption was strongly associated with tobacco use. Furthermore, former smokers appeared to be more likely to consume some form of smokeless tobacco, which suggests that there may be a substitution process at play. Smoking cessation was significantly associated with the highest SES quintiles, being married/living with a partner, and ceasing to consume alcohol. Within the AWI-Gen study, smoking was less common among adults with tertiary education and if they did smoke, they were more likely to stop smoking than those with lower levels of education.
Overall current alcohol consumption (both problematic and non-problematic) was present in 40.5% of the AWI-Gen cohort. The lower prevalence of alcohol consumption among women, as well as the decreased likelihood to engage in harmful alcohol consumption has been attributed to socio-cultural stigmas surrounding women who consume alcohol. This finding is supported by several studies in different African contexts [7–9, 17, 18, 20, 24]. Lifetime alcohol abstainers were more prevalent in East and South (Kenya and South Africa) Africa, compared to West Africa (Burkina Faso and Ghana). This difference was found to be more defined among women, with women in Nairobi (Kenya), Agincourt, Dikgale, and Soweto (South Africa) more likely to abstain from alcohol than participants in Navrongo (Ghana) and Nanoro (Burkina Faso). The frequency of daily alcohol consumption was highest among men in Nanoro (27.2%) and 10.3% of women were daily consumers. This trend of high daily alcohol consumption in both sexes was also observed during the national WHO-STEPS survey in 2013 in Nanoro where 26.2% of men and 16.7% of women were identified as daily alcohol consumers [36].
Differences in alcohol use were observed between the West African sites, Nanoro and Navrongo, despite having similar rates of alcohol consumption. Navrongo reported a much higher prevalence of problematic alcohol consumption (31.2%) than Nanoro (12.5%). In Navrongo, spirits were also more popular than in Nanoro. Binge drinking was found to be highest among men in Dikgale and Agincourt, corroborating previous data suggesting that SA has one of the highest rates of alcohol consumption per capita in the world [7, 17, 18, 40]. Binge drinking was the main feature of problematic alcohol consumption together with the feeling of needing to “cut down”. It also appears that social pressure through criticism (“people criticising you”) was most prevalent in Navrongo, followed by Dikgale. In Agincourt however, fewer surveyed drinkers reported facing criticism and feeling guilty related to their drinking patterns. In this study of adults aged 40 to 60 years, age was significantly associated with problematic alcohol consumption, where older people in this age range were less likely to drink, but the effect was small. Age effects related to drinking behaviour were observed in other African studies [12, 13, 16, 41]. Across the combined dataset, problematic drinking was not significantly correlated with SES, but SES associations were complex and varied at site level. A recent cross-sectional study examining correlates of alcohol use in the slums in Kenya suggested that alcohol use was associated with higher income, whereas the reverse relationship was found for problematic drinking in the Nairobi sample of this study (with lower odds of problematic drinking in association with higher SES) [10]. In our study, alcohol consumption was highly correlated with tobacco use, likely reflecting addictive behavior, rather than a preference for one substance above the other. This correlation has been observed in many cross-sectional studies that were also not specifically designed to reveal the likely sequence of substance use behaviours [9, 10, 13, 14, 16, 21, 39]. Current (problematic and non-problematic) and former drinkers were more likely to use tobacco products than those who had never consumed alcohol.
To our knowledge, this is one of the larger cross-sectional African population studies of multi-site comparisons of the prevalence of tobacco and alcohol consumption with related socio-demographic correlates. Patterns of tobacco and alcohol consumption show sex specific, regional (East, West, South Africa), as well as within-region differences. These differences may be due to differences in socio-economic transition across regions, but may also be affected by different national policies related to the regulation and taxation of tobacco and alcohol products, in turn affecting accessibility to those substances [2, 42, 43]. In addition, there are differences across religions and cultural beliefs which are known to influence patterns of tobacco and/or alcohol consumption [9, 10, 15, 17, 19, 24, 36].
Limitations
This cross-sectional study was not designed to infer causality and there is no data to assess the temporal sequence of substance use. Our study was limited to persons aged 40 to 60 years, which is not representative of the general population, and data generated from a single community is not necessarily generalisable to be representative of the geographic region or an entire country. The missing data from Soweto limited inference for this site. Under-reporting of substance use may have occurred due to cultural differences within regions, as women would be less likely to report substance use due to potential stigmatisation, and because the CAGE questionnaire asks sensitive questions which participants may have found difficult to answer honestly and objectively.
Conclusion
This study reports the prevalence and socio-demographic correlates of alcohol and tobacco consumption in four SSA countries (Burkina Faso, Ghana, Kenya, and South Africa). Our results showed differences in the prevalence of substance use, sex-differences in the type of tobacco products consumed, and the patterns of alcohol consumption across the study sites. Sex, SES, and education had varying effects on tobacco and alcohol consumption both regionally and by study site. The high prevalence of alcohol consumption and problematic alcohol use is of concern and policies should be strengthened on a macro level in order to combat this high prevalence of substance use in SSA [2, 42]. Individual behavioural changes may be more difficult to achieve without addressing them from a broader perspective, such as product-specific taxation, proactive monitoring and regulation, and limiting access to substances. Our results provide insight and understanding into patterns of tobacco and alcohol consumption in African communities in rural and urban settings, which is vital for the development of policies and interventions which may assist in reducing the burden of disease and mortality associated with substance use in Africa.
Supplementary Information
Acknowledgements
We acknowledge the contribution of Freedom Mukomana from the SBIMB for curating and doing quality control on the AWI-Gen data used for analysis, and all of the fieldworkers across the research sites for their hard work during data collection, and we extend our gratitude to every research participant for being a part of this study.
Abbreviations
- aOR
Adjusted odds ratio
- AWI-Gen
Africa Wits-INDEPTH Partnership for Genomic Research Study
- HDSS
Health and Demographic Surveillance System
- HIV
Human Immunodeficiency Virus
- LMIC
Low and middle income countries
- Q1-Q5
First to fifth quintile for socio-economic status
- QC
Quality control
- SES
Socio-economic status
- SA
South Africa
- SSA
Sub-Saharan Africa
- TB
Tuberculosis
Authors’ contributions
PRB analysed the data, interpreted the results, and co-drafted the manuscript. He was also part of the Nanoro research team as study-coordinator during data collection. CCS performed the literature review and co-drafted the manuscript. She contributed to the original development of the AWI-Gen questionnaire. CD interpreted the results and gave input regarding data from Navrongo. SN provided an expert interpretation and background of substance use in South Africa. IM, SFM, SC, AO, GA, LKM, FXG, and HS contributed to the original design of the study and to the acquisition and interpretation of data. They provided inputs and edits to the paper. SM helped draft and lay out the manuscript as senior author along with MR who is the principal investigator for AWI-Gen. Both senior authors (SM and MR) and PRB and CCS developed the research questions and related hypotheses. The authors read and approved the final manuscript.
Funding
AWI-Gen was funded by the National Human Genome Research Institute (NHGRI), Office of the Director (OD), Eunice Kennedy Shriver National Institute Of Child Health & Human Development (NICHD), the National Institute of Environmental Health Sciences (NIEHS), the Office of AIDS research (OAR) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), of the National Institutes of Health (NIH) (U54HG006938) and its supplements, as part of the H3Africa Consortium. Additional funding from the Department of Science and Technology, South Africa, (DST/CON 0056/2014). Government of Ghana provided additional funding for the NHRC. SM has had research support from an early career research award from the Claude Leon Foundation, a self-initiated research fellowship from the South African Medical Research Council and incentive funding for rated researchers from the South African National Research Foundation (grant number 119375). The funders had no role in the design or any other part of the study. They approved the original application and funded the study.
Availability of data and materials
AWI-Gen phenotype data variables have been deposited in the European Genome-Phenome Archive (Accession number: EGAD00001006425). The datasets generated and/or analysed during the current study are available and accessible from the corresponding author Palwende Romuald Boua (romyboua@gmail.com) on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval was obtained from the University of the Witwatersrand (Wits) Human Research Ethics Committee (HREC) for AWI-Gen which included approval for the Wits sites at DPHRU (Soweto) and Agincourt (M121029, Renewal M170880)/South Africa. Each of the research centres outside of Wits applied for ethics approval in accordance with their national regulations. Dikgale (DIMAMO) (University of Limpopo, Medunsa Research and Ethics Committee (MREC) MREC/HS/195/2014:CR)/ South Africa, APHRC (The Ethics and Scientific Review Committee AMREF P114/2014)/Kenya, Nanoro (The Institutional Ethics Committee of Centre Muraz 015–2014/CE-CM)/Burkina Faso, and Navrongo (Ghana Health Service Ethical Review Committee GHS-ERC 05/05/14)/Ghana. All participants were required to sign an informed consent document stating their willingness to share and have stored both their anonymised collected data and biospecimens. A withdrawal clause was included which makes provision for participants to withdraw from the study. It also specifies that any anonymised data already within the public sphere cannot be withdrawn.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sumaya Mall and Michèle Ramsay joint senior authors.
References
- 1.Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, Giovino GA, West R, Hall W, Griffiths P, Ali R, Gowing L, Marsden J, Ferrari AJ, Grebely J, Farrell M, Degenhardt L. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018;113(10):1905–1926. doi: 10.1111/add.14234. [DOI] [PubMed] [Google Scholar]
- 2.Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, Abate KH, Abbafati C, Abera SF, Abraham B, Abyu GY, Adebiyi AO, al-Aly Z, Aleman AV, Ali R, al Alkerwi A', Allebeck P, al-Raddadi RM, Amare AT, Amberbir A, Ammar W, Amrock SM, Antonio CAT, Asayesh H, Atnafu NT, Azzopardi P, Banerjee A, Barac A, Barrientos-Gutierrez T, Basto-Abreu AC, Bazargan-Hejazi S, Bedi N, Bell B, Bello AK, Bensenor IM, Beyene AS, Bhala N, Biryukov S, Bolt K, Brenner H, Butt Z, Cavalleri F, Cercy K, Chen H, Christopher DJ, Ciobanu LG, Colistro V, Colomar M, Cornaby L, Dai X, Damtew SA, Dandona L, Dandona R, Dansereau E, Davletov K, Dayama A, Degfie TT, Deribew A, Dharmaratne SD, Dimtsu BD, Doyle KE, Endries AY, Ermakov SP, Estep K, Faraon EJA, Farzadfar F, Feigin VL, Feigl AB, Fischer F, Friedman J, G/hiwot TT, Gall SL, Gao W, Gillum RF, Gold AL, Gopalani SV, Gotay CC, Gupta R, Gupta R, Gupta V, Hamadeh RR, Hankey G, Harb HL, Hay SI, Horino M, Horita N, Hosgood HD, Husseini A, Ileanu BV, Islami F, Jiang G, Jiang Y, Jonas JB, Kabir Z, Kamal R, Kasaeian A, Kesavachandran CN, Khader YS, Khalil I, Khang YH, Khera S, Khubchandani J, Kim D, Kim YJ, Kimokoti RW, Kinfu Y, Knibbs LD, Kokubo Y, Kolte D, Kopec J, Kosen S, Kotsakis GA, Koul PA, Koyanagi A, Krohn KJ, Krueger H, Defo BK, Bicer BK, Kulkarni C, Kumar GA, Leasher JL, Lee A, Leinsalu M, Li T, Linn S, Liu P, Liu S, Lo LT, Lopez AD, Ma S, el Razek HMA, Majeed A, Malekzadeh R, Malta DC, Manamo WA, Martinez-Raga J, Mekonnen AB, Mendoza W, Miller TR, Mohammad KA, Morawska L, Musa KI, Nagel G, Neupane SP, Nguyen Q, Nguyen G, Oh IH, Oyekale AS, PA M, Pana A, Park EK, Patil ST, Patton GC, Pedro J, Qorbani M, Rafay A, Rahman M, Rai RK, Ram U, Ranabhat CL, Refaat AH, Reinig N, Roba HS, Rodriguez A, Roman Y, Roth G, Roy A, Sagar R, Salomon JA, Sanabria J, de Souza Santos I, Sartorius B, Satpathy M, Sawhney M, Sawyer S, Saylan M, Schaub MP, Schluger N, Schutte AE, Sepanlou SG, Serdar B, Shaikh MA, She J, Shin MJ, Shiri R, Shishani K, Shiue I, Sigfusdottir ID, Silverberg JI, Singh J, Singh V, Slepak EL, Soneji S, Soriano JB, Soshnikov S, Sreeramareddy CT, Stein DJ, Stranges S, Subart ML, Swaminathan S, Szoeke CEI, Tefera WM, Topor-Madry R, Tran B, Tsilimparis N, Tymeson H, Ukwaja KN, Updike R, Uthman OA, Violante FS, Vladimirov SK, Vlassov V, Vollset SE, Vos T, Weiderpass E, Wen CP, Werdecker A, Wilson S, Wubshet M, Xiao L, Yakob B, Yano Y, Ye P, Yonemoto N, Yoon SJ, Younis MZ, Yu C, Zaidi Z, el Sayed Zaki M, Zhang AL, Zipkin B, Murray CJL, Forouzanfar MH, Gakidou E. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the global burden of disease study 2015. Lancet. 2017;389(10082):1885–1906. doi: 10.1016/S0140-6736(17)30819-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mdege ND, Shah S, Ayo-Yusuf OA, Hakim J, Siddiqi K. Tobacco use among people living with HIV: analysis of data from demographic and health surveys from 28 low-income and middle-income countries. Lancet Glob Heal. 2017;5(6):e578–e592. doi: 10.1016/S2214-109X(17)30170-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degenhardt L, Charlson F, Ferrari A, Santomauro D, Erskine H, Mantilla-Herrara A, et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987-1012. 10.1016/S2215-0366(18)30337-7. Epub 2018 Nov 1. [DOI] [PMC free article] [PubMed]
- 5.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng ATA, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FGR, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, III, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Memish ZA, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Hanafiah KM, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CDH, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, III, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJC, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJL, Ezzati M. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sreeramareddy CT, Pradhan PM, Sin S. Prevalence , distribution , and social determinants of tobacco use in 30 sub-Saharan African countries. 2014. pp. 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andersson LMC, Twum-Antwi A, Staland-Nyman C, van Rooyen DRM. Prevalence and socioeconomic characteristics of alcohol disorders among men and women in the eastern Cape Province, South Africa. Heal Soc Care Commun. 2018;26(1):e143–e153. doi: 10.1111/hsc.12487. [DOI] [PubMed] [Google Scholar]
- 8.Magidson JF, Dietrich J, Otwombe KN, Sikkema KJ, Katz IT, Gray GE. Psychosocial correlates of alcohol and other substance use among low-income adolescents in peri-urban Johannesburg, South Africa: a focus on gender differences. J Health Psychol. 2017;22(11):1415–1425. doi: 10.1177/1359105316628739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gedif T, Azale T, Nigusie A. Substance use and associated factors among Gumuz people in Benishangul-Gumuz regional state, Mandura woreda, Northwest Ethiopia. Subst Abus Treat Prev Policy. 2019;14(1):36. 10.1186/s13011-019-0225-2. [DOI] [PMC free article] [PubMed]
- 10.Takahashi R, Wilunda C, Magutah K, Mwaura-Tenambergen W, Wilunda B, Perngparn U. Correlates of alcohol consumption in rural western Kenya: a cross-sectional study. BMC Psychiatry. 2017;17(1):175. 10.1186/s12888-017-1344-9. [DOI] [PMC free article] [PubMed]
- 11.Gebremariam TB, Mruts KB, Neway TK. Substance use and associated factors among Debre Berhan University students, Central Ethiopia. Subst Abus Treat Prev Policy. 2018;13(1):13. 10.1186/s13011-018-0150-9. [DOI] [PMC free article] [PubMed]
- 12.Peltzer K, Phaswana-Mafuya N. Drug use among youth and adults in a population-based survey in South Africa. South Afr J Psychiatry. 2018;24:1139. 10.4102/sajpsychiatry.v24i0.1139. eCollection 2018. [DOI] [PMC free article] [PubMed]
- 13.Peltzer K, Chao LW, Ramlagan S, Szrek H. Daily tobacco use and problem drinking among urban adults in South Africa: a longitudinal study. Pan Afr Med J. 2019;1:32. doi: 10.11604/pamj.2019.32.51.17256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuteesa MO, Seeley J, Cook S, Webb EL. Multi-level experiences and determinants of alcohol misuse and illicit drug use among occupational groups at high-risk of HIV in sub-Saharan Africa: a thematic synthesis of qualitative findings. Glob Public Health. 2020;15(5):715-33. 10.1080/17441692.2019.1679216. Epub 2019 Oct 23. [DOI] [PMC free article] [PubMed]
- 15.Molla Z, Dube L, Krahl W, Soboka M. Tobacco dependence among people with mental illness: a facility-based cross sectional study from Southwest Ethiopia. BMC Res Notes. 2017;10(1):289. 10.1186/s13104-017-2608-7. [DOI] [PMC free article] [PubMed]
- 16.Jenkins R, Othieno C, Ongeri L, Kiima D, Sifuna P, Kingora J, et al. Alcohol consumption and hazardous drinking in western Kenya — a household survey in a health and demographic surveillance site. 2015. pp. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nkoana S, Sodi T, Darikwa TB. Heavy episodic alcohol drinking among students from a rural south African university: correlates with personal-social variables. J Psychol Africa. 2016;26(4):368–372. doi: 10.1080/14330237.2016.1208949. [DOI] [Google Scholar]
- 18.National Department of Health (NDoH), South African Medical Research Council (SAMRC) and I . South Africa Demographic and Health Survery 2016. 2019. [Google Scholar]
- 19.Kassa A, Wakgari N, Taddesse F. Determinants of alcohol use and khat chewing among Hawassa university students, Ethiopia: a cross sectional study. Afr Health Sci. 2016;16(3):822–830. doi: 10.4314/ahs.v16i3.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayano G, Assefa D, Haile K, Chaka A, Solomon H, Hagos P, et al. Mental, neurologic, and substance use (MNS) disorders among street homeless people in Ethiopia. Ann General Psychiatry. 2017;16:40. 10.1186/s12991-017-0163-1. eCollection 2017. [DOI] [PMC free article] [PubMed]
- 21.Elf JL, Variava E, Chon S, Lebina L, Motlhaoleng K, Gupte N, Niaura R, Abrams D, Golub JE, Martinson N. Prevalence and correlates of smoking among people living with HIV in South Africa. Nicotine Tob Res. 2018;20(9):1124–1131. doi: 10.1093/ntr/ntx145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kagee A, Saal W, Bantjes J. The relationship between symptoms of common mental disorders and drug and alcohol misuse among persons seeking an HIV test. AIDS Care Psychol Socio-Medical Asp AIDS/HIV. 2018;30(2):219–223. doi: 10.1080/09540121.2017.1361510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oppong AK. Cannabis and amphetamine use and its psychosocial correlates among school-going adolescents in Ghana. Child Adolesc Psychiatry Ment Health. 2019;29:13(1). doi: 10.1186/s13034-019-0293-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riva K, Allen-Taylor L, Schupmann WD, Mphele S, Moshashane N, Lowenthal ED. Prevalence and predictors of alcohol and drug use among secondary school students in Botswana: a cross-sectional study. BMC Public Health. 2018;18(1):1396.10.1186/s12889-018-6263-2. [DOI] [PMC free article] [PubMed]
- 25.Jallow IK, Britton J, Langley T. Prevalence and determinants of susceptibility to tobacco smoking among students in the Gambia. Nicotine Tob Res. 2019;21(8):1113–1121. doi: 10.1093/ntr/nty128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wesonga R, Guwatudde D, Bahendeka SK, Mutungi G, Nabugoomu F, Muwonge J. Burden of cumulative risk factors associated with non-communicable diseases among adults in Uganda: evidence from a national baseline survey. Vol. 15. London: International Journal for Equity in Health; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramsay M, Crowther N, Tambo E, Agongo G, Baloyi V, Dikotope S, et al. H3Africa AWI-gen collaborative Centre: a resource to study the interplay between genomic and environmental risk factors for cardiometabolic diseases in four sub-Saharan African countries. Glob Heal Epidemiol Genomics. 2016;1:e20. 10.1017/gheg.2016.17. eCollection 2016. [DOI] [PMC free article] [PubMed]
- 28.Ali SA, Soo C, Agongo G, Alberts M, Amenga-Etego L, Boua RP, Choudhury A, Crowther NJ, Depuur C, Gómez-Olivé FX, Guiraud I, Haregu TN, Hazelhurst S, Kahn K, Khayeka-Wandabwa C, Kyobutungi C, Lombard Z, Mashinya F, Micklesfield L, Mohamed SF, Mukomana F, Nakanabo-Diallo S, Natama HM, Ngomi N, Nonterah EA, Norris SA, Oduro AR, Somé AM, Sorgho H, Tindana P, Tinto H, Tollman S, Twine R, Wade A, Sankoh O, Ramsay M. Genomic and environmental risk factors for cardiometabolic diseases in Africa: methods used for phase 1 of the AWI-gen population cross-sectional study. Glob Health Action. 2018;11(sup2):1507133. doi: 10.1080/16549716.2018.1507133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Richter L, Norris S, Pettifor J, Yach D, Cameron N. Cohort profile: Mandela’s children: The 1990 birth to twenty study in South Africa. Int J Epidemiol. 2007;36(3):504–511. doi: 10.1093/ije/dym016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kahn K, Collinson MA, Xavier Gómez-olivé F, Mokoena O, Twine R, Mee P, et al. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol. 2012;41(4):988–1001. doi: 10.1093/ije/dys115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kanjala C, Alberts M, Byass P, Burger S. Spatial and temporal clustering of mortality in Digkale HDSS in rural northern South Africa. Glob Health Action. 2010;3. 10.3402/gha.v3i0.5236. [DOI] [PMC free article] [PubMed]
- 32.Beguy D, Elung’ata P, Mberu B, Oduor C, Wamukoya M, Nganyi B, et al. Health & demographic surveillance system profile: The Nairobi urban health and demographic surveillance system (NUHDSS) Int J Epidemiol. 2015;44(2):462–471. doi: 10.1093/ije/dyu251. [DOI] [PubMed] [Google Scholar]
- 33.Oduro AR, Wak G, Azongo D, Debpuur C, Wontuo P, Kondayire F, Welaga P, Bawah A, Nazzar A, Williams J, Hodgson A, Binka F. Profile of the Navrongo health and demographic surveillance system. Int J Epidemiol. 2012;41(4):968–976. doi: 10.1093/ije/dys111. [DOI] [PubMed] [Google Scholar]
- 34.Derra K, Rouamba E, Kazienga A, Ouedraogo S, Tahita MC, Sorgho H, Valea I, Tinto H. Profile: Nanoro health and demographic surveillance system. Int J Epidemiol. 2012;41(5):1293–1301. doi: 10.1093/ije/dys159. [DOI] [PubMed] [Google Scholar]
- 35.Ewing JA. Detecting Alcoholism: The CAGE Questionnaire. JAMA. 1984;252(14):1905–1907. doi: 10.1001/jama.1984.03350140051025. [DOI] [PubMed] [Google Scholar]
- 36.Ministere De La Sante Burkina Faso . Rapport de l’enquête STEPS. 2013. p. 1973. [Google Scholar]
- 37.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459–468. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 38.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pedro JM, Brito M, Barros H. Tobacco consumption and nicotine dependence in Bengo Province, Angola: A community-based survey. PLoS One. 2017;12(11):e0188586. 10.1371/journal.pone.0188586. eCollection 2017. [DOI] [PMC free article] [PubMed]
- 40.Ferreira-Borges C, Parry CDH, Babor TF. Harmful Use of Alcohol: A Shadow over Sub-Saharan Africa in Need of Workable Solutions. Int J Environ Res Public Health. 2017;14(4):346. 10.3390/ijerph14040346. [DOI] [PMC free article] [PubMed]
- 41.Ward CL, Mertens JR, Flisher AJ, Bresick GF, Sterling SA, Little F, Weisner CM. Prevalence and correlates of substance use among south African primary care clinic patients. Subst Use Misuse. 2008;43(10):1395–1410. doi: 10.1080/10826080801922744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ndinda C, Ndhlovu TP, Juma P, Asiki G, Kyobutungi C. The evolution of non-communicable diseases policies in post-apartheid South Africa. BMC Public Health. 2018;18(Suppl 1):956. 10.1186/s12889-018-5832-8. [DOI] [PMC free article] [PubMed]
- 43.Drope J, Schluger NW, Cahn Z, Drope J, Hamill S, Islami F, et al. The tobacco atlas. Choice Rev Online. 2018;50(05):50–2422. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
AWI-Gen phenotype data variables have been deposited in the European Genome-Phenome Archive (Accession number: EGAD00001006425). The datasets generated and/or analysed during the current study are available and accessible from the corresponding author Palwende Romuald Boua (romyboua@gmail.com) on reasonable request.


