Abstract
Background
During the COVID-19 pandemic, visiting restrictions of different extents have been implemented. However, despite the long history of visiting restrictions in health care systems, little is known about their effects.
Objectives
This review sought to explore the consequences of visitor restrictions in health care services during the COVID-19 pandemic.
Methods
A systematic, integrative review was conducted in accordance with the PRISMA guidelines, based on a systematic search in PubMed, CHINAL full plus, Web of Science, PsychInfo, Scopus and the Cochrane Library.
Results
A total of 17 scientific papers covering intensive care, pediatric care, general medical care, hospital care, palliative care and nursing home settings were included. Although appreciation for the technical solutions enabling remote meetings was reported, visiting restrictions had several consequences, mainly negative, for the patient's health, the health and wellbeing of family members and the provision of care. Among physical health consequences, reduced nutrition intake, decreased activities of daily living and increased physical pain and symptoms were reported. Among mental health consequences for the patient, loneliness, depressive symptoms, agitation, aggression, reduced cognitive ability and overall dissatisfaction were observed. For family members, worry, anxiety and uncertainty occurred, and they reported an increased need for information from care providers. Family members of neonatal intensive care unit patients reported less bonding with their child and family relation disturbances due to the restrictions. For care providers, visiting restrictions added the burdens of ethical dilemmas, learning new technical means to enable social interaction and an increased demand for communication with families and providing social support to both family members and patients.
Conclusions
When implementing visiting restrictions in health care services, decision makers and nurses need to be aware of their potential negative effects and adapt the provision of care to compensate for such effects. Nurses in all sectors should be aware that visiting restrictions may affect patients, families, and health care services for longer than the actual pandemic. Since the level of evidence regarding effect from visiting restrictions is low, further studies is strongly needed.
Keywords: COVID-19, Integrative review, Mental health, Nursing, Pandemic, Visiting restrictions
What is already known
-
•
Visiting restrictions have a long history in health care services. During the COVID-19 pandemic, such restrictions were implemented in most countries and health care sectors.
-
•
Little is known about the effects of visiting restrictions, either from a virus transmission perspective or as to their impact on everyday care from the perspectives of patients, families or nurses.
What this paper adds
-
•
This review has indicated that visiting restrictions during the COVID-19 pandemic had several impacts on patient health, the health and wellbeing of family members and the provision of care.
-
•
Nurses in all sectors should be aware of be aware of potential negative effects and adapt the provision of care to compensate for such effects these effects.
-
•
Since visiting restrictions have profound effects on the entire health care system, their effects from both a virus transmission and a wellbeing perspective need further investigation.
1. Introduction
On January 30th, 2020, the World Health Organization declared the COVID-19 pandemic a Public Health Emergency of International Concern, its highest level of alarm. The pandemic forced health care systems worldwide to introduce mitigating measures to reduce the impact of the disease. One of the recommendations was that “numbers of visitors and visiting periods should be highly restricted” (World Health Organization (WHO) 2020, p. 10). Following this recommendation and similar guidance, visitor restrictions at hospitals and nursing homes were introduced in many countries. During the COVID-19 pandemic, different visiting restrictions were applied in different countries and regions, ranging from an absolute ban on all visits in all kinds of care facilities to comparatively liberal visiting policies, allowing visitors during certain circumstances or with mitigating procedures. These restrictions and policies also changed over time as the pandemic developed and the knowledge of spread-reducing strategies increased.
The actual effects of visitor restriction as an intervention to reduce the spread of infections in general is not fully known, and the existing evidence is unclear (Jeffersson et al. 2020). The knowledge on the spread of COVID-19, and visiting restrictions is still limited, and multiple possible routes of in-hospital COVID-19 transmission has been identified (Rickman et al., 2021). Since visiting restrictions has been one out of many precautions for infection control implemented within the healthcare services during the pandemic, no study that has distinguished the effects from such precaution measures have been found. However, visitor restrictions during the winter in a pediatric hospital were found to reduce hospital transmission of respiratory viruses (not specifically SARS COv-2) compared with when no restrictions were in place (Forkpa et al., 2020). Another study reported a significant reduction in health care-acquired respiratory viral infections when implementing year around visiting restrictions (Washam et al., 2018).
The role of families and loved ones in the care of a hospital-admitted patient or resident at a nursing home can be viewed from many perspectives in several nursing theories and concepts, such as family-based nursing or person-centered nursing. Visiting restrictions have existed since the very first hospitals were established in the early 1800s and have been used not only with the aim of reducing the spread of disease but also to protect both patient and family from stress (Smith et al., 2009). Since then, knowledge regarding the effects of visiting restrictions and the desire to enable a calm environment to promote healing has increased; in the 1960s, the value of social interaction between the hospitalized patient and the family was highlighted, and liberal visiting policies were implemented in many caring facilities (Bellou and Gerogianni, 2010). Today, relations with and the role of family members are seen as an essential part of nursing (Gaugler, 2005). Visits from family and close friends has been found to have several positive health and wellbeing effects for the hospitalized patient or resident at a nursing home (Gillick, 2013; Weinberg et al., 2007).
Despite the long history of visiting restrictions, there is no consensus about visiting restrictions or their impact in everyday care (Smith et al., 2009). In times when the world faces a previously unknown disease, causing uncertainty, fear and an extreme load on health care systems, interventions that are effective in reducing the spread of that disease are essential. However, all mitigating procedures need to be evaluated in the light of potential other effects from a holistic perspective; this review was conducted to contribute to the possibility of making well-informed decisions and to fill existing gaps in knowledge.
2. The review
2.1. Aim
This review aimed to explore the consequences of visitor restrictions in health care services during the COVID-19 pandemic.
2.2. Design
A systematic, integrative review (Whittemore and Knafl, 2005) was conducted.
2.3. Search methods
A systematic search in PubMed, Chinal plus with full text, Web of Science, PsychInfo, Scopus and the Cochrane Library was conducted by one of the authors (KH) and an academic librarian on the November 30, 2020. Search terms used were “Covid 19*”, “SARS Cov 19*”, “visitor restriction*”, “visiting restriction”, “visitor”. For a detailed description of the search, including search terms and outcomes, see Supplementary Table 1.
The following eligibility criteria were used to select studies: (a) reporting visitor or family restrictions at hospitals or nursing homes during the COVID-19 pandemic; (b) full-text articles published in English; (c) using a qualitative, quantitative or mixed method design or published as a case report; and (d) presenting a patient and/or family member and/or caring perspective. Studies were excluded if they (a) were published as editorial or similar texts, (b) were review studies, (c) reported only on technical aspects of telemedicine use, (d) consisted only of inventories of restriction protocols or (e) reported on infections other than COVID-19. The selection of papers to include were conducted by two authors (KH and MM), using the Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). Disagreements were resolved by discussion or referral to the third author (NH).
2.4. Search outcome
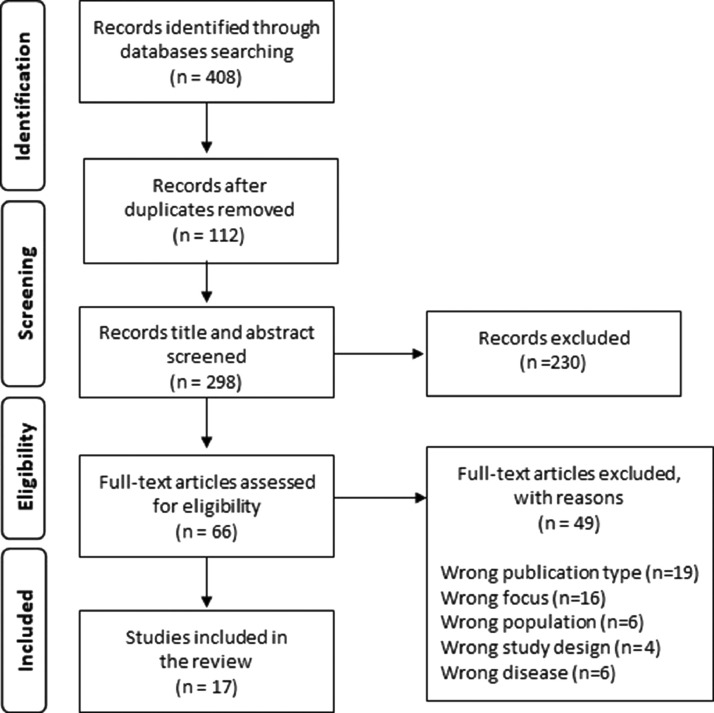
The search resulted in retrieving 408 papers from PubMed (n = 134), Chinal Plus with full text (n = 41), PsychInfo (n = 6), Web of Science (n = 89), Scopus (n = 132) and the Cochrane Library (n = 6; see Table 1). After duplicates were removed, 296 articles remained and were screened by title and abstract. Of these, 230 did not meet the inclusion criteria and were excluded. The full text of 66 articles was screened. Of these, 49 were excluded due to publication type (n = 19), study focus (n = 16), population (n = 6), study design (n = 4) or disease (n = 6). Ultimately, 17 articles were included; a manual search of the reference lists of those 17 articles did not yield any further articles that would merit inclusion. The detailed selection process is shown in the PRISMA flowchart in Fig. 1 .
Table 2.
Overview of quality appraisal of included studies and CASP checklist used.
| CASP Qualitative Studies Checklist* | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author/s and year | Was there a clear statement of the aims of the research? | Is a qualitative methodology appropriate? | Was the research design appropriate to address the aims of the research? | Was the recruitment strategy appropriate to the aims of the research? | Was the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethical issues been taken into consideration? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | How valuable is the research? | Overall Quality Assessment | |||
| Anneser et al. 2020 | Y | Y | Y | C | C | C | C | Y | Y | Y | L | |||
| Bembich et al., 2020 | Y | Y | Y | C | C | C | Y | Y | Y | Y | M | |||
| Creutzfeldt et al., 2020 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | M | |||
| Sizoo et al., 2020 | Y | Y | C | Y | Y | C | Y | Y | Y | Y | M | |||
| Verbeek et al., 2020 | Y | Y | Y | Y | Y | C | Y | Y | Y | Y | M | |||
| Virani et al., 2020 | C | C | C | C | C | C | C | N | N | Y | L | |||
| CASP Cohort Studies Checklist*, ⁎⁎ | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Did the study address a clearly focused issue? | Was the cohort recruited in an acceptable way? | Was the exposure accurately measured to minimize bias? | Was the outcome accurately measured to minimize bias? | Have the authors identified all important confounding factors? | Have they taken account of the confounding factors in the design and/or analysis? | Was the follow up of subjects complete enough? | Was the follow up of subjects long enough? | How precise are the results? | Do you believe the results? | Can the results be applied to the local population? | Do the results of this study fit with other available evidence? | What are the implications of this study for practice? | Overall quality assessment | |
| Heat et al. 2020 | Y | Y | Y | Y | N | N | N | N | Y | Y | C | C | C | M |
| Mahoney et al. 2020 | Y | Y | Y | Y | N/A | N/A | N/A | N/A | Y | Y | Y | C | C | M |
| Mercadante et al., 2020 | Y | Y | Y | Y | N/A | N/A | N/A | N/A | Y | Y | C | C | C | M |
| Muniraman et al., 2020 | Y | C | Y | Y | N/A | N/A | N/A | N/A | Y | Y | C | Y | Y | M |
| O'Caoimh et al. 2020 | Y | C | Y | Y | N | N | C | N | Y | Y | C | Y | C | M |
| Ostacoli et al., 2020 | Y | Y | Y | Y | N | N | C | N | Y | Y | C | Y | C | M |
| Piscatello et al. 2020 | Y | Y | Y | Y | C | C | Y | N | Y | Y | C | C | C | M |
| Shum et al., 2020 | Y | C | C | C | N | N | C | N | C | Y | C | C | C | M |
| Wammes et al., 2020 | Y | Y | C | Y | C | C | Y | N | Y | Y | C | Y | C | M |
| Yeh et al. 2020 | Y | Y | Y | Y | N/A | N/A | N/A | N/A | Y | Y | C | C | N | M |
| Zeh et al., 2020 | Y | Y | Y | Y | C | C | Y | C | Y | Y | C | C | N | M |
In accordance with the CASP checklist guidelines, the following gradings were used: Y= yes, C= Can´t tell, N No. N/A= not applicable. M = moderate overall quality, L = low overall quality.
The question “What were the results of this study?” has been presented in Table 3 and is therefore not included in this table.
Fig. 1.
Selection process of included articles.
2.5. Quality appraisal
The CASP Cohort Study Checklists (CASP 2020) (the Qualitative Studies Checklist or Cohort Study Checklist, depending on study design) were used to inform the quality appraisal of the papers (Long et al., 2020). All studies were comprehensively assessed with regard to both their methodological or theoretical rigor and data relevance and an overall quality appraisal as ‘moderate quality’ or ‘low quality’ was used (Whittemore and Knafl, 2005; Long et al., 2020). Due to the limited number of scientific publications available, the nature of the research question and the need for timely results given the ongoing pandemic, case studies and studies with only a brief description of the methodology used, sample, instruments and/ or analysis used included and assessed as ‘low quality’. Studies with a more rigor and adequate reporting on methods used were assessed as moderate quality. Each study was independently assessed by two authors (KH and MM). Disagreements were resolved by discussion or referral to the third author (NH). The results of the quality appraisal is shown in Table 2 .
2.6. Data abstraction and synthesis
As suggested in the integrative literature review, the analysis was based on the results and conclusions of each study. As a first step, relevant results were extracted, sorted and examined to identify subthemes and themes. These were internally and externally compared and placed into a table to enable synthesizing the results. Finally, the synthesized results were reflected on with regard to previous studies and nursing science in general. The entire process of analysis was carried out by all authors, first independently and then in a discussion.
3. Results
The 17 papers published in scientific journals covered different perspectives on visiting restrictions as a main or additional finding. As to method, quantitative (n = 10), qualitative (n = 3) and mixed methods designs (n = 2) were represented, as were case reports (n = 2). The studies were conducted in the United States (n = 5, including one multi-center study featuring neonatal intensive care units in Saudi Arabia, Spain, Canada, France, India, the United States and the United Kingdom), the Netherlands (n = 3), Italy (n = 2), Taiwan (n = 1), Hong Kong (n = 1), Japan (n = 1), Ireland (n = 1), Canada (n = 1), Germany (n = 1) and the United Kingdom (n = 1). The study contexts were nursing homes (n = 5), palliative care units in hospitals (n = 3), neonatal intensive care units (n = 3), intensive care units (n = 2) or other hospital care (n = 4). Six of the studies had a patient perspective, eight a family member perspective and two a care provider perspective. Only two studies included or focused specifically on COVID-19-positive patients and/or their family members. Of the included studies, some were conducted during complete visiting restriction policy (n = 9), some during a partial visiting restriction policy (n = 4) and in some studies, the study compared or combined different degrees of visiting restriction policies (n = 3). An overview of the studies included is provided in Table 3 .
Table 3.
Overview of included studies settings, method, and main findings of relevance for this review.
| Author/s and year | Study setting | Country | Study population | Focus of the study | Visiting restrictions studied | Design | Methods | Main findings of relevance |
|---|---|---|---|---|---|---|---|---|
| Anneser et al. 2020 | Palliative care unit | Germany | Case report of a palliative care patient (n = 1) | Report and discuss challenges in palliative care during Covid 19 | One 30 min visit once permitted | Case report | Case report | Specific demands on the palliative care during the Covid 19 pandemic |
| Bembich et al., 2020 | Neonatal intensive care unit | Italy | Parents of the hospitalised infants (n = 10) | Experiences from visitor restrictions in the neonatal intensive care unit | One parent, one hour per day permitted | Qualitative study | Individual interviews | Visiting restrictions lead to dysphoric emotions, relations suffering and adaptive strategies. Long term effects are unknown. |
| Creutzfeldt et al., 2020 | Intensive care unit | USA | Family members of ICU patients with traumatic brain injury (n = 22) | Family member experiences from visiting restrictions | No physical visits allowed | Qualitative study | Individual interviews | Visiting restrictions had serious negative impact on family members wellbeing and health. |
| Heat et al. 2020 | Hospital palliative care unit | UK | Covid 19 patients referred to the hospital palliative care service (n = 31) | Symptoms, management, and family presence in palliative care of Covid 19 patients | One family member allowed to be present in dying phase, no other visits permitted | Descriptive retrospective cohort study | Analysis of medical records. | About 80% of the patients included did not have a loved one or relative present when dying. The effects from this are unknown. |
| Mahoney et al. 2020 | Neonatal intensive care unit | Multiple | Neonatal intensive care units in USA, Saudi Arabia, United Kingdom, Spain, Canada, France and India (n = 277) | Policy for family presence in neonatal intensive care units during COVID-19 | No physical visits allowed (2%), one parent at the bedside at any time (85%), a single parent to be allowed for the entire hospital stay | Cross-sectional descriptive quantitative study | Survey | Hospital restrictions significantly limited parental presence in neonatal intensive care units. A decrease in full parental participation in rounds was reported (71–32%, p < 0.001). |
| Mercadante et al., 2020 | Palliative care unit | Italy | Family members of hospitalized palliative care patients (n = 16) | Experiences from using mobile technology to communicate with loved ones. | No physical visits allowed | Retrospective cohort study | Interviews | Some of the problems related to visitor restrictions could be overcome with technology. However, such solutions cannot substitute the real presence. |
| Muniraman et al., 2020 | Neonatal intensive care unit | UK and USA | Parents and families of infants (n = 231) | To assess parental perceptions of restricted visiting policies in the unit. | One parent at the bedside at any time (63%), two parents at the bedside at any time (19%), one parent at the bedside with time restrictions (16%) | Cross-sectional study | Survey | Visiting restrictions had impacts on the ability to visit, care for and bond with their infants. Respondents subject to restrictions of one parent were more likely to perceive a severe impact compared with those facing less austere restrictions (p = 0.02) |
| O'Caoimh et al. 2020 | Nursing home | Ireland | Visitors of residents in nursing homes (n = 225) | Emotional wellbeing among family members of nursing homes residents | No physical visits allowed | Cross-sectional study | Survey | Many visitors experienced low psychosocial and emotional well-being |
| Ostacoli et al., 2020 | Other hospital care | Italy | Women who had given birth during the Covid 19 pandemic (n = 163) | Prevalence of depressive and post-traumatic stress symptoms in women giving birth during the Covid-19 pandemic | No physical visits allowed | Cross-sectional study | Survey | Reported distress seemed to be associated more with the prenatal experience and other individual factors than with the pandemic hospital restrictions. The absence of visitors during hospitalization resulted in quiet wards that protected women from risk of developing postpartum PTSS. |
| Piscatello et al. 2020 | Intensive care unit | USA | ICU patients suffering from Covid 19 with lacked alert mental status and a documented request of family meetings (n = 61) | Evaluation of distance family meetings for ICU patients unable of decision making on their own care | No physical visits allowed | Retrospective cohort study | Analysis of charts and medical records | Fewer changes in patient goals of care occurred following video meetings compared to in-person meetings. Visitor restriction policies may increase the risk for inadequate and unequal communication with family members. |
| Shum et al., 2020 | Other hospital care | Hong-Kong | Elderly patients with advanced dementia (Covid 19 negative) (n = 24) | Visiting restrictions effects for feeding among elderly living in nursing homes | No physical visits allowed | Retrospective cohort study | Analysis of medical records | Oral feeding in patients with advanced dementia could deteriorate during periods of visitor restrictions (in 2020) compared with the same time period in 2019. |
| Sizoo et al., 2020 | Nursing home | The Netherlands | Physicians (n = 76) | To investigate dilemmas experienced by medical doctors in nursing homes due to visitor restrictions | No physical visits allowed | Qualitative study | An open-ended questionnaire | Visiting restrictions effected both patients, family members and health professionals. Ethical dilemmas, challenges related to the dying phase, emotional impacts and the use of technical means to enable social interaction were discussed. |
| Verbeek et al., 2020 | Nursing home | The Netherlands | Nursing homes representants (n = 23) and nurses (n = 30) | Compliance and experiences of visitors nursing homes | No physical visits allowed (8 weeks) and thereafter one visitor per resident with specific protocols | Mixed methods study | Survey, telephone interviews and descriptive analyses of documents | Residents, visitors, and staff were in general compliant with the local protocol guidelines. However, the workload of staff increased due to the restrictions. Personal interactions are crucial for the residents’ quality of life and staff cannot replace family members. |
| Virani et al., 2020 | Other hospital care | Canada | Case reports of hospitalized children (n = 3) | Highlight situations in which health care teams must decide how to apply visitor restrictions and whether | Not reported | Case report | Case report | Aspects of how visiting restrictions affect hospitalized children and their family members |
| Wammes et al., 2020 | Nursing home | The Netherlands | Family members of nursing home residents (n = 1997) | Describe perspectives from relatives of nursing home residents on visiting restrictions | No physical visits allowed | Cross sectional study | Survey | Adverse health effects among residents in nursing homes were reported. Communication needs between staff and family increased during visiting restrictions. |
| Yeh et al. 2020 | Nursing home | Taiwan | Family members to residents of nursing homes (n = 157) | Explore family members’ concerns for their relatives during the lockdown | No physical visits allowed | Cross sectional study | Telephone interview survey | Most family members (85%) accepted the restrictions. Staff members need to provide more psychological information about residents to their family members during lockdown compared to other times. |
| Zeh et al., 2020 | Other hospital care | USA | Non Covid 19 patients undergoing planned surgery (n = 117) | Impact of visitor restriction rules on the postoperative experience of patients undergoing surgery | No physical visits allowed | Mixed methods study | Survey and individual interviews | Patients lacking visitors were less satisfied with their overall hospital experiences and had lower psychosocial well-being than patients with visitors (80.7% vs 66.0%, p = 0.044). |
Four themes (health consequences for the patient, health consequences for family members, consequences for social relations within the family and consequences for the provision of care) and eight subthemes (physical health, mental health, interaction between patients and family members, interaction within families, technical means to enable social interaction, understanding patient condition, interaction between care providers and families and workload and ways to provide care) emerged. The representation of the studies in each theme is shown in Table 4 .
Table 4.
Overview of the representation of data from each included paper in the themes.
| Authors and year of publication | Themes |
|||
|---|---|---|---|---|
| Health consequences for the patient | Health consequences for the family members | Consequences for the relations within the family | Consequence for the providing of care | |
| Anneser et al. 2020 | X | |||
| Bembich et al., 2020 | X | X | ||
| Creutzfeldt et al., 2020 | X | X | ||
| Heat et al. 2020 | X | X | ||
| Mahoney et al. 2020 | X | X | ||
| Mercadante et al., 2020 | X | X | ||
| Muniraman et al., 2020 | X | X | X | |
| O'Caoimh et al. 2020 | X | X | ||
| Ostacoli et al., 2020 | X | |||
| Piscatello et al. 2020 | X | |||
| Shum et al., 2020 | X | X | ||
| Sizoo et al., 2020 | X | X | ||
| Verbeek et al., 2020 | X | X | X | |
| Virani et al., 2020 | X | X | X | |
| Wammes et al., 2020 | X | X | X | |
| Yeh et al. 2020 | X | |||
| Zeh et al., 2020 | X | X | ||
The findings reported below describe the consequences of visitor restrictions during the COVID-19 pandemic from patient, family and caregiver perspectives. Since the visiting restrictions within the health care services were general and the number of available papers limited, no distinction was made between patients and family members of patients infected with COVID-19 and other patients.
3.1. Health consequences for patients
The visiting restrictions affected the physical health of patients suffering from both COVID-19 and other conditions. An increased level of observed body pain was reported (Sizoo et al., 2020) and a reduced ability to care for oneself, such as personal hygiene maintenance (O'Caoimh et al., 2020; Wammes et al., 2020), were reported among nursing home residents due to the visiting restrictions. In geriatric care, the nutritional status of long-term patients decreased due to reduced oral intake during the visiting-restriction period (O'Caoimh et al., 2020; Shum et al., 2020). Non-COVID-19 patients who had been hospitalized and undergone surgery of different kinds while visiting was restricted reported less timely access to analgesics, nausea medication and other medications than postoperative patients under normal visiting routines (84.5% vs 69.0%, p = 0.048) (Zeh et al., 2020a).
As to mental health consequences, increased levels of perceived loneliness, depressive symptoms, agitation and aggression were found among residents in nursing homes during the visiting-restriction period when compared to periods with normal visiting procedures (O'Caoimh et al., 2020; Sizoo et al., 2020; Wammes et al., 2020). In addition, reduced cognitive functions like loss of memory were reported (O'Caoimh et al., 2020; Wammes et al., 2020; Verbeek et al., 2020). Reduced access to their parents during hospitalization was considered to affect perceived fundamental trust among children (Virani et al., 2020). Factors associated with postpartum depression and post-traumatic stress symptoms was quiet on the ward related to the absence of visitors (OR 0.525 95% CI 0.308–0.896) whereas distress related to the absence of partner was insignificant risk factor (Ostacoli et al., 2020). Surgery patients who were not infected with COVID-19 were less satisfied with their overall experiences while hospitalized during visitor restrictions than in non-restriction periods (80.7% vs 66.0%, p = 0.044), (Zeh et al., 2020b).
3.2. Health consequences for family members
Not being physically present for their hospitalized family member created worries, anxiety, sadness and a need for more information and updates on the family member's condition (Creutzfeldt et al., 2020; Muniraman et al., 2020; Wammes et al., 2020; Yeh et al., 2020). A lower score of general psychosocial wellbeing of family members was reported both among family members of residents in nursing homes (O'Caoimh et al., 2020) and parents of children in neonatal intensive care units (Muniraman et al., 2020). Sadness and anger were expressed among parents of hospitalized children (Bembich et al., 2020). Many family members reported stress due to uncertainty (Creutzfeldt et al., 2020; Muniraman et al., 2020). Not being allowed to be present in the hospital created moral concerns and a feeling of failing to support and protect their loved ones among family members of intensive care patients who were not infected with COVID-19 (Creutzfeldt et al., 2020). Being present at the patient's side, on the other hand, supported family members in understanding and coping with the situation (Creutzfeldt et al., 2020). In addition, family members had positive experiences from “virtual visits”, using telecommunication solutions to “see” their loved ones (Mercadante et al., 2020). Several studies noted the unknown long-term consequences for family members who had lost someone close during the COVID-19 pandemic. Complicated or prolonged sorrow might be an increasing mental health problem due to the limited possibilities to understand and be involved in the care of a dying family member (Sizoo et al., 2020; Heath et al., 2020).
3.3. Consequences for the relations within the family
Visiting restrictions affected the social relations between family members in different ways. During visiting restrictions, the number of visits of family members such as siblings or elderly family members to neonatal intensive care units were reduced compared to before the pandemic. The long-term effects of this is unknown (Darcy Mahoney et al., 2020; Yeh et al., 2020). Despite exceptions to the visiting restrictions that enabled visits from family members at the end of life, few palliative care patients actually had a family member present when dying (Heath et al., 2020). When nursing homes reopened for visitors, activities such as having a cup of coffee together caused deeply emotional reactions among patients, showing the value of such social contact (Verbeek et al., 2020). Despite technological solutions, it was common for patients not to be well enough to participate in video calls or chats, which reduced the possibility of maintaining social relations within the family (Heath et al., 2020). Enabling physical, safe meetings such as outdoor visits or meetings behind glass were more appreciated for social interaction within the family than digital solutions by family members of relatives in nursing homes (Wammes et al., 2020). A reasonable compromise between full and no access might be more acceptable and better than the no-access alterative for both patients and family members, contributing to promoting a sense of being a family (Virani et al., 2020).
Parents caring for a child in the neonatal intensive care units found their relations as a couple were negatively affected, since their time together was reduced by visitor restrictions that allowed only one parent at a time in the neonatal intensive care unit (Bembich et al., 2020). In addition, the separation of child and parent seriously interrupted the social relationship within the family (Bembich et al., 2020), led to less bonding between parents and children and decreased breast feeding (Muniraman et al., 2020). The long-term consequences of the separation of parents and children in the neonatal intensive care units cannot yet be determined (Muniraman et al., 2020; Bembich et al., 2020).
3.4. Consequence for the provision of care
Visiting restrictions caused ethical dilemmas in balancing the protection of the public and the wellbeing of patients and their family members (Anneser, 2020). From a caring perspective, family members can be seen as external partners or an essential and internal part of a patient's care team, as in pediatric care (Virani et al., 2020). Despite this perspective, the visitor restrictions had several direct and indirect impacts on the care provided in all health care settings in this review. If the patient was positive for COVID-19, any family member living with the patient was most likely already exposed to the virus (Virani et al., 2020), but after nursing homes were reopened to visitors, no transmission of COVID-19 was detected (Verbeek et al., 2020). Nevertheless, several studies demonstrated that family members accepted and followed the visiting restrictions to reduce the transmission of COVID-19, even if their own wellbeing was affected (Mercadante et al., 2020; Muniraman et al., 2020; Verbeek et al., 2020).
Many health care facilities tried to replace physical visits with a variety of digital and technical means. However, these kinds of meetings had certain limitations. Video or telephone meetings with family members led to fewer changes of goals than in-person meetings in palliative care settings (Piscitello et al., 2020). Also, despite substitute methods such as video visits, the visiting restrictions reduced the adequacy of family members’ understanding of their loved ones’ condition and thus their understanding of the overall situation and the care provided (Piscitello et al., 2020; Shum et al., 2020). This not only caused problems in the dialog between health care professionals and family members but also reduced the possibilities to provide consensus-based care (Creutzfeldt et al., 2020; Muniraman et al., 2020; Piscitello et al., 2020). As an example, a decrease in full parental participation in rounds at neonatal intensive care units, from71% to 32% (p < 0.001) was reported due to visiting restrictions (Mahoney et al. 2020).
When families were not able to visit patients, an increased need for information and regular updates from health care professionals on patients’ conditions was reported (Creutzfeldt et al., 2020; Muniraman et al., 2020; Verbeek et al., 2020; Wammes et al., 2020). As a consequence, health professionals were expected to provide more detailed and frequent communications with family members than when such information could be gained through physical visits and face-to-face communication (Wammes et al., 2020). This communication was vital to establishing vitally needed trust for the health care services (Yeh et al., 2020). This physical distance also made the information and frequent updates on their loved ones’ condition more important than the normal emotional support from the health professionals to family members, placing new demands on health care professionals (Creutzfeldt et al., 2020; Yeh et al., 2020). An increased need for psychosocial support of family members during the visiting-restriction period was also found in the neonatal intensive care unit context (Bembich et al., 2020). Together with visiting protocols such as demonstrating the use of personal protective gear or digital solutions, the increased demand for communication and supplying information to family members caused an increased workload among health care staff (Verbeek et al., 2020; Wammes et al., 2020). Even though digital solutions and efforts by health care professionals to maintain appropriately distanced relationships between patients and family member were appreciated digital visits could not substitute for the physical presence of family members. Therefore, some of the included studies suggested that such solutions should be used as a last resort to enable social contacts (Creutzfeldt et al., 2020; Mercadante et al., 2020).
4. Discussion
The results of this review indicate that visiting restrictions imposed during the COVID-19 pandemic have had several negative consequences for both patients and family members, despite efforts to use technical solutions to substitute for physical visits. In addition, social relations within families were affected. However, this should be seen in the light of lack of knowledge of visiting restriction decreased the number of infected people. Efforts to mitigate the negative effects and the demands to change the ways of providing care due to visiting restrictions placed an increased burden on health care professionals.
Several studies reported on technical and digital solutions to enable social contacts for hospitalized patients or nursing home residents. Such solutions are appreciated by both patients and families when they offer new possibilities to interact free of concerns regarding physical distance, visiting hours or the spread of disease. Therefore, such services might add value to care even when the pandemic is over and could be seen as a “new normal” in many ways. Telemedicine was introduced to healthcare in the 1960s, and its use has since increased, along with technological advances. The effectiveness of telemedicine has been demonstrated by multiple meta-analyses in various settings (Fu et al., 2020). While telemedicine was mostly used in rural areas or countries with scarce medical and health care resources, the COVID-19 pandemic has forced resource-rich institutions to shift from conventional to technology-assisted medical practice. On the other hand, family involvement in both acute and long-term care settings contributes to favourable patient outcomes and family member experiences (Kelley et al., 2019; Mackie et al., 2018). Technical solutions might not replace the physical contact enabled by face-to-face meetings or provide the same impressions and comprehensive understanding of patient condition as would be found in a real-life visit. Therefore, some of the included studies suggested that such solutions should be used as a last resort to enable social contacts (Creutzfeldt et al., 2020; Mercadante et al., 2020). To deal with the positive and negative sides of remote visiting, nurses could ensure the quality of remote visiting by using knowledge gained through telemedicine. For example, proper device setting, lighting and noise management are all essential for better examinations in telemedicine, factors that could be applied to virtual meetings between hospitalized patients and family members.
The findings in this review show that visiting restrictions increased mental health problems and caused distress and worry among both patients and family members. Nurses, regardless of their assigned departments, would regularly check for symptoms of psychiatric problems such as depressive mood or diminished motivation for recovery commonly observed in patients. Social support from the normal social network, including family and close friends, has been found crucial in mitigating distress (Southwick et al., 2016). Therefore, whenever visiting restrictions are implemented, nurses and social workers need to be aware of the increased need to provide professional psychosocial support for both patients and family members. Acknowledging their distress and negative feelings, normalizing the emotional turmoil expressed and providing basic comfort are all elements of essential care for these patients.
The visiting restrictions had several impacts on palliative and end-of-life care. Low-quality or scant communication between care providers and families causes distress that can affect both the quality of dying for the patient and complicate or prolong grief for the family members (Anderson-Shaw and Zar, 2020, Feder et al., 2020; Wallace et al., 2020).
Several studies reported on the effects of visiting restrictions in pediatric care. In neonatal intensive care units, family members are deeply integrated into the caring team and contribute to both the physiological and psychological wellbeing of their children (Page, 2016). Therefore, the absence of one or both parents from the bedside of a neonate may have consequences for the development of that child and for the functionality of the family that cannot be anticipated at the present time (Murray and Swanson, 2020). The presence of family members has been shown to be essential, especially for patients in critical condition (Page, 2016). In intensive care units, the presence of family members has been described as a “lifeline to reality” (Page, 2016) and is often a strong motivation to stay alive and to continue the struggle to recover (Engström and Söderberg, 2007).
This review has revealed that visiting restrictions place extra burdens on care providers by increasing the need for communication with family members, imposing social distancing between patients and family members and modifying established ways to provide psychosocial support. The response to COVID-19 has brought clinically significant psychological burdens and mental health problems for healthcare providers around the globe (Preti et al., 2020). The COVID-19 pandemic has caused care providers to suffer moral injury, which refers to the psychosocial, behavioural and even spiritual impacts of “failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations” (Anderson-Shaw and Zar, 2020, Litz et al., 2009). Moral injury carries a sense of guilt, powerlessness and insufficiency that can lead to burnout in health care professions (Ruotsalainen et al., 2015). In order to prevent moral injury among nurses, which can be amplified by visiting restrictions, managers need to proactively develop protect measures, remain open to and candid in communication and periodically screen mental health among their staff, along with providing them with support and evidence-based treatments (Greenberg et al., 2020).
4.1. Limitations
Most of the studies included in this review rely on a quantitative design. To some extent, this is not surprising, since the pandemic reduced the opportunities to conduct face-to-face interviews or observations. In addition, many of the papers used study-specific surveys instead of standardized instruments to measure, for example, depression symptoms or quality of life. That reduces the ability to compare different settings or populations and to evaluate the effects of nursing interventions such as different kinds of visiting restrictions. Case reports and brief reports were included in this review, given the recent appearance of the phenomena studied and the lack of studies within the field. Most studies had a descriptive design, and none used a control group nor baseline data. This reduced the possibilities to judge if the health problems and symptoms reported were related to the visiting restrictions or could be a result of the overall stress and impact that the pandemic in general caused. Also, the design and methodology used in the included studies imply that the level of evidence must be considered as low. Nevertheless, all articles aimed to provide knowledge on visiting restrictions caused by COVID-19 and this presenting article is to assemble current state of science and art in caring COVDI-19 patients in timely fashion.
This study has highlighted several effects of visiting restrictions. It can be concluded that the restrictions had profound effects on the whole health care system, from intensive care settings to nursing homes. However, just two of the studies covered specifically COVID-19-positive patients and their families. Only one reported on the actual transmission of the virus with regard to the restrictions. Since COVID-19 was not the first and will not be the last time that visiting restrictions are implemented, greater scientific knowledge of their effects not only from a disease-spreading perspective but also from patient, family and caring perspectives is urgently needed so that the best possible decisions can be made. In addition, further research on how to mitigate the negative effects found and specific nursing interventions that can enable safe physical visits in all kinds of care settings, such as the use of personal protection gear or outdoor visits, is an imperative for the nursing research community.
5. Conclusions
When implementing visiting restrictions in health care services, decision makers and nurses need to be aware of their potential negative effects and adapt the provision of care to compensate for such effects. Nurses in all sectors should be aware that visiting restrictions may affect patients, families and health care services for longer than the actual pandemic. Since the level of evidence regarding consequences of visiting restrictions is low, further studies is strongly needed.
Declaration of Competing Interest
None
Acknowledgments
Funding
No external funding
CRediT authorship contribution statement
Planning the study: KH, NH, MM; Data collection: KH, MM; Analysis: KH, NH, MM, Data summarizing: KH, NH, MM. Writing of manuscript: KH, NH, MM. Revision of manuscript: KH, NH, MM. Editing of manuscript: KH.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnurstu.2021.104000.
Appendix. Supplementary materials
References
- Anderson-Shaw L.K., Zar F.A. COVID-19, moral conflict, distress, and dying alone. J. Bioeth. Inq. 2020;17:777–782. doi: 10.1007/s11673-020-10040-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anneser J. Dying patients with COVID-19: what should hospital palliative care teams (HPCTs) be prepared for? Palliative Support Care. 2020;18(4):382–384. doi: 10.1017/S1478951520000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellou P., Gerogianni K.G. The contribution of family in the care of patient in the hospital. Health Sci. J. 2010;1(3):4–9. http://62.217.125.154/xmlui/bitstream/handle/11400/1173/family.pdf?sequence=1 [Google Scholar]
- Bembich S., Tripani A., Mastromarino S., Di Risio G., Castelpietra E., Risso F.M. Parents experiencing NICU visit restrictions due to COVID-19 pandemic. Acta Paediatr. 2020 doi: 10.1111/apa.15620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASP CASP Cohort Study Checklist. 2020 https://casp-uk.net/casp-tools-checklists/ [Google Scholar]
- Creutzfeldt C.J., Schutz R.E.C., Zahuranec D.B., Lutz B.J., Curtis J.R., Engelberg R.A. Family presence for patients with severe acute brain injury and the influence of the COVID-19 pandemic. J. Palliat. Med. 2020 doi: 10.1089/jpm.2020.0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darcy Mahoney A., White R.D., Velasquez A., Barrett T.S., Clark R.H., Ahmad K.A. Impact of restrictions on parental presence in neonatal intensive care units related to coronavirus disease 2019. J. Perinatol. 2020;40(Suppl 1):36–46. doi: 10.1038/s41372-020-0753-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engström A., Söderberg S. Receiving power through confirmation: the meaning of close relatives for people who have been critically ill. J. Adv. Nurs. 2007;59(6):569–576. doi: 10.1111/j.1365-2648.2007.04336.x. [DOI] [PubMed] [Google Scholar]
- Feder S., Smith D., Griffin H., Shreve S.T., Kinder D., Kutney-Lee A., et al. Why couldn't I go in to see him?” Bereaved families' perceptions of end-of-life communication during COVID-19. J. Am. Geriatric Soc. 2020 doi: 10.1111/jgs.16993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forkpa H., Rupp A.H., Shulman S.T., Patel S.J., Gray E.L., Zheng X., Bovee M., Kociolek L.K. Association between children's hospital visitor restrictions and healthcare-associated viral respiratory infections: a quasi-experimental study. J. Pediatric. Infect. Dis. Soc. 2020;9(2):240–243. doi: 10.1093/jpids/piz023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Z., Burger H., Arjadi R., Bockting C.L.H. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(10):851–864. doi: 10.1016/s2215-0366(20)30256-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler J.E. Family involvement in residential long-term care: a synthesis and critical review. Aging Ment. Health. 2005;9(2):105–118. doi: 10.1080/13607860412331310245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillick M.R. The critical role of caregivers in achieving patient-centred care. JAMA. 2013;310(6):575–576. doi: 10.1001/jama.2013.7310. [DOI] [PubMed] [Google Scholar]
- Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- Heath L., Yates S., Carey M., Miller M. Palliative care during COVID-19: data and visits from loved ones. Am. J. Hospice and Palliative Med. 2020;37(11):988–991. doi: 10.1177/2F1049909120943577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson T., Del Mar C.B., Dooley L., Ferroni E., Al-Ansary L.A., Bawazeer G.A., van Driel M.L., Jones M.A., Thorning S., Beller E.M., Clark J., Hoffmann T.C., Glasziou P.P., Conly J. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of System. Rev. 2020;11 doi: 10.1002/14651858.CD006207.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley R., Godfrey M., Young J. The impacts of family involvement on general hospital care experiences for people living with dementia: an ethnographic study. Int. J. Nurs. Stud. 2019;96:72–81. doi: 10.1016/j.ijnurstu.2019.04.004. [DOI] [PubMed] [Google Scholar]
- Litz B.T., Stein N., Delaney E., Lebowitz L., Nash W.P., Silva C., Maguen S. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Long H., French D., Brooks J. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res. Methods in Med. Health Sci. 2020;1(1):31–42. doi: 10.1177/2632084320947559. [DOI] [Google Scholar]
- Mackie B.R., Mitchell M., Marshall A. The impact of interventions that promote family involvement in care on adult acute-care wards: an integrative review. Collegian. 2018;25(1):131–140. [Google Scholar]
- Mercadante S., Adile C., Ferrera P., Giuliana F., Terruso L., Piccione T. Palliative care in the time of COVID-19. J. Pain Symptom Manag. 2020;60(2):e79–e80. doi: 10.1016/j.jpainsymman.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muniraman H., Ali M., Cawley P., Hillyer J., Heathcote A., Ponnusamy V., Coleman Z., Hammonds K., Raiyani C., Gait-Carr E., Myers S., Hunt K., Govande V., Jain A., Clark R., Doherty C., Raju V., Clarke P. Parental perceptions of the impact of neonatal unit visitation policies during COVID-19 pandemic. BMJ Paediatrics Open. 2020;4 doi: 10.1136/2Fbmjpo-2020-000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray P.D., Swanson J.R. Visitation restrictions: is it right and how do we support families in the NICU during COVID-19? J. Perinatol. 2020;40(10):1576–1581. doi: 10.1038/s41372-020-00781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Caoimh R., O'Donovan M.R., Monahan M.P., Dalton O'Connor C., Buckley C., Kilty C., Fitzgerald S., Hartigan I., Cornally N. Psychosocial impact of COVID-19 nursing home restrictions on visitors of residents with cognitive impairment: a cross-sectional study as part of the Engaging Remotely in Care (ERiC) Project. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.585373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostacoli L., Cosma S., Bevilacqua F., Berchialla P., Bovetti M., Carosso A.R., et al. Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703–711. doi: 10.1186/s12884-020-03399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page P. Critical illness trajectory for patients, families and nurses: a literature review. Nurs. Crit. Care. 2016;21(4):195–205. doi: 10.1111/nicc.12199. [DOI] [PubMed] [Google Scholar]
- Piscitello, G.M., Fukushima, C.M., Saulitis, A.K., Tian, K.T., Hwang, J., Gupta S., & Sheldon, M. 2020 Family meetings in the intensive care unit during the coronavirus disease 2019 pandemic. Am. J. Hospice and Palliative Med.. 10.1177/2F1049909120973431. [DOI] [PMC free article] [PubMed]
- Preti E., Di Mattei V., Perego G., Ferrari F., Mazzetti M., Taranto P., Di Pierro R., Madeddu F., Calati R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr. Psychiatry Rep. 2020;22(8):43. doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickman H., Rampling T., Shaw K., Martinez-Garcia K., Hail L., Coen P., Shahmanesh M., Yen Shin G., Nastouli E., Houlihan C. Nosocomial Transmission of Coronavirus Disease 2019: a Retrospective Study of 66 Hospital-acquired Cases in a London Teaching Hospital. Clin. Infect. Dis. 2021;72(4):690–693. doi: 10.1093/cid/ciaa816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruotsalainen J.H., Verbeek J.H., Mariné A., Serra C. Preventing occupational stress in healthcare workers. Cochrane Database System. Rev. 2015;2015(4) doi: 10.1002/14651858.CD002892.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shum C.K., Shea Y.F., Tang M., Wan W.H., Chan M.M.K. Poor feeding due to visitor restrictions in long-term care facilities during the coronavirus disease 2019 pandemic. Psychogeriatrics. 2020;20(6):929–930. doi: 10.1111/psyg.12623. [DOI] [PubMed] [Google Scholar]
- Sizoo E.M., Monnier A.A., Bloemen M., Hertogh C., Smalbrugge M. Dilemmas with restrictive visiting policies in Dutch nursing homes during the COVID-19 pandemic: a qualitative analysis of an open-ended questionnaire with elderly care physicians. J. Am. Med. Directors Assoc. 2020;21(12):1774–1781. doi: 10.1016/j.jamda.2020.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L., Medves J., Harrison M.B., Tranmer J., Waytuck B. The impact of hospital visiting hour policies on pediatric and adult patients and their visitors. JBI Library of System. Rev. 2009;7(2):38–79. doi: 10.11124/jbisrir-2009-181. [DOI] [PubMed] [Google Scholar]
- Southwick S.M., Sippel L., Krystal J., Charney D.S., Mayes L., Pietrzak R.H. Why are some individuals more resilient than other: the role of social support. World Psychiatry. 2016;15(1):77–79. doi: 10.1002/wps.20282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeek H., Gerritsen D.L., Backhaus R., de Boer B.S., Koopmans R.T.C.M., Hamers J.P.H. Allowing visitors back in the nursing home during the COVID-19 crisis: a Dutch national study into first experiences and impact on well-being. J. Am. Medical Directors Assoc. 2020;21(7):900–904. doi: 10.1016/j.jamda.2020.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virani A.K., Puls H.T., Mitsos R., Longstaff H., Goldman R.D., Lantos J.D. Benefits and risks of visitor restrictions for hospitalized children during the COVID pandemic. Pediatrics. 2020;146(2):1–6. doi: 10.1542/peds.2020-000786. [DOI] [PubMed] [Google Scholar]
- Wallace C.L., Wladkowski S.P., Gibson A., White P. Grief during the COVID-19 pandemic: considerations for palliative care providers. J. Pain Symptom Manage. 2020;60(1):e70–ee6. doi: 10.1016/j.jpainsymman.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wammes J.D., Kolk M.D., van den Besselaar J.H., MacNeil-Vroomen J.L., Buurman-van Es B.M., van Rijn M. Evaluating perspectives of relatives of nursing home residents on the nursing home visiting restrictions during the COVID-19 crisis: a Dutch cross-sectional survey study. J. Am. Medical Directors Assoc. 2020;12(2):1746–1750. doi: 10.1016/j.jamda.2020.09.031. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washam M., Woltmann J., Ankrum A., Connelly B. Association of visitation policy and health care-acquired respiratory viral infections in hospitalized children. Am. J. Infect. Control. 2018;46(3):353–355. doi: 10.1016/j.ajic.2017.09.007. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg D.B., Lusenhop R.W., Gittell J.H., Kautz C.M. Coordination between formal providers and informal caregivers. Health Care Manage. Rev. 2007;32(2):140–149. doi: 10.1097/01.HMR.0000267790.24933.4c. [DOI] [PubMed] [Google Scholar]
- Whittemore R., Knafl K. The integrative review: updated methodology. J. Adv. Nurs. 2005;52(5):546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2020, June 1). Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance, 1 June 2020. https://apps.who.int/iris/handle/10665/332240
- Yeh, T.C., Huang, H.C., Yeh, T.Y., Huang, W.T., Huang, H.C., Chang, Y.M., & Chen, W. Family members’ concerns about relatives in long-term care facilities: acceptance of visiting restriction policy amid the COVID-19 pandemic. Geriatrics & Gerontol., 20(10), 938–942. 10.1111/ggi.14022. [DOI] [PubMed]
- Zeh R.D., Santry H.P., Monsour C., Sumski A.A., Bridges J.F.P., Tsung A., Pawlik T.P., Cloyd J.M. Impact of visitor restriction rules on the postoperative experience of COVID-19 negative patients undergoing surgery. Surgery. 2020;168(5):770–776. doi: 10.1016/j.surg.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.